ABSTRACT
Acupuncture is a popular alternative therapy worldwide and is generally safe. However, serious acupuncture-related complications can occur. Intracranial complications caused by a migrated acupuncture needle are extremely rare. Herein we report a surgical case of intracranial acupuncture needle migration and discuss the key technical aspects of the procedure. We additionally performed a review of the relevant literature. A 55-year-old woman presented with migration of a broken acupuncture needle via the posterior cervical skin. Computed tomography (CT) showed that the needle migrated intra- and extradurally via the atlanto-occipital junction. CT angiography revealed that the needle tail was located adjacent to the right distal horizontal loop of the vertebral artery. Meanwhile, the needle tip was positioned in the premedullary cistern adjacent to the medulla oblongata via the right lateral medullary cistern. Emergent surgical removal was conducted. Intradural exploration was required as the needle was not found in the epidural space. The needle penetrated the adventitia of the right intradural vertebral artery. We failed to pull out the needle toward the epidural space. After the needle was completely pulled into the intradural space, it was successfully removed without bleeding complication. Postoperative CT showed no evidence of residual needle fragment. The patient was discharged home without any sequelae. To the best of our knowledge, this is the first case of penetrating vertebral artery injury caused by radiologically confirmed acupuncture needle migration. An intracranially migrated needle should be removed urgently to prevent further migration causing brainstem, cranial nerve, and vessel injuries. The surgical strategy should be selected according to needle location and direction.
Key Words: acupuncture-related complication, foreign body, intracranial complication, penetrating injury, vertebral artery injury
INTRODUCTION
Acupuncture is the stimulation of specific points on the skin (acupuncture points) commonly via the insertion of fine needles. Currently, it is increasingly used worldwide as an alternative and complementary medical modality for pain control. Acupuncture is usually safe; however, serious complications, including pneumothorax, cardiac tamponade, and transverse myelopathy, can occur.1-3 To date, intracranial complications caused by acupuncture needle migration is extremely rare.4-8 Herein we describe a surgical case involving penetrating injury of the intradural vertebral artery (VA) caused by an intracranially migrated acupuncture needle. A literature review about intracranial complications caused by radiologically confirmed acupuncture needle migration was performed.
CASE REPORT
A 55-year-old woman with no significant medical history presented to our hospital immediately after migration of a broken needle via the posterior cervical skin (day 0). To relieve headache and stiff neck, the patient had repeatedly undergone self-acupuncture on the posterior neck using a disposable, fine 4-cm stainless steel needle with a shaft. However, the joint between the needle and shaft had accidentally detached during self-acupuncture, followed by complete needle migration into the posterior neck region. On day 0, her vital signs and neurological findings were normal. A needle puncture mark was not found on the posterior cervical skin. The initial computed tomography (CT) on day 0 revealed that the needle migrated intra- and extradurally via the atlanto-occipital junction. There was no evidence of hemorrhage and cerebrospinal fluid (CSF) leakage. CT angiography (CTA) on day 0 showed that the right distal horizontal loop of the V3 segment of the VA was surrounded by the vertebral venous plexus. The needle penetrated the vertebral venous plexus (Fig. 1). The needle tip was positioned in the premedullary cistern adjacent to the medulla oblongata via the right lateral medullary cistern (Fig. 1).
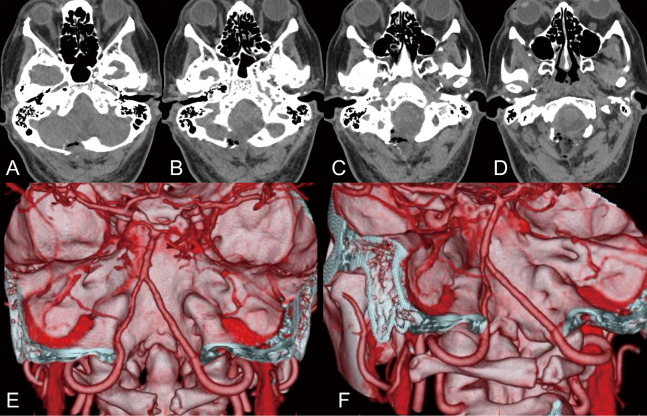
Fig. 1.
Preoperative computed tomography angiography
Fig. 1A: The needle tip (arrow) was positioned in the premedullary cistern adjacent to the medulla oblongata.
Fig. 1B: The needle (arrow) was located in the right lateral medullary cistern.
Fig. 1C, 1D: The right distal horizontal loop of the V3 segment of the vertebral artery (arrowheads) was surrounded by the vertebral venous plexus (asterisks). The needle (arrows) penetrated the vertebral venous plexus.
Three-dimensional CTA on day 0 showed that the needle was adjacent to the proximal right V4 segment (Fig. 2A, B). The tail of the needle was located between the right distal horizontal loop and the posterior arch of the atlas (Fig. 2C). The lengths of the needle located in the intradural space and epidural space were about 2.5 and 1.5 cm, respectively. The left VA was located in the long axis direction of the migrated needle (Fig. 2B). To prevent further needle migration and infection, emergent surgical removal was performed on day 0. This study was approved by the institutional review board, and a written informed consent for treatment was obtained from the patient.
Fig. 2.
Preoperative three-dimensional computed tomography angiography
Fig. 2A, 2B: The needle was adjacent to the proximal right V4 segment (arrows).
Fig. 2C: The needle tail was located between the right distal horizontal loop and the posterior arch of the atlas (arrowhead). Notably, the left VA was located in the long axis direction of the migrated needle.
Surgical removal
Caution was taken not to cause further needle migration during surgery. Under general anesthesia, midline suboccipital craniotomy with C1 laminectomy was performed. The right side of the posterior atlanto-occipital membrane was dissected. However, the needle could not be found in the extradural space. After dural incision, the needle was identified in the right lateral medullary cistern (Fig. 3A). The lower cranial nerves were intact. However, the needle penetrated the adventitia of the right V4 segment (Fig. 3B). First, we attempted to pull out the needle toward the epidural space using a microforceps. Nevertheless, the needle did not move at all. Second, the needle was cut with a microscissors in the intradural space; however, this procedure was not successful because the needle was stiff. Thus, the needle was cautiously pulled in caudally toward the intradural space using a microforceps (Fig. 3C). After the needle was completely pulled into the intradural space (Fig. 3D), it was removed without causing bleeding in the VA.
Fig. 3.

Intraoperative images captured with a video
Fig. 3A: The needle (arrowhead) was found in the right lateral medullary cistern. The right intradural vertebral artery (VA) (single asterisk), accessary nerve (double asterisks), and medulla oblongata (triple asterisks) were visualized.
Fig. 3B: The needle penetrated the adventitia of the right VA (arrowhead).
Fig. 3C, 3D: The needle (arrowheads) was cautiously pulled in caudally toward the intradural space using a microforceps. Consequently, the needle (arrowheads) was completely pulled into the intradural space without causing bleeding complication.
Primary dural closure was performed in which the total operative time was 228 min and estimated blood loss was 150 ml. The needle length was about 4 cm. The needle tip remained sharp, and the needle tail was dull (Fig. 4).
Fig. 4.
Photograph of the acupuncture needle
Removed acupuncture needle in the current case (upper) and unused identical needle (lower).
Postoperative course
Immediate postoperative CT confirmed no evidence of residual needle fragment and intracranial hemorrhage (Fig. 5A–D). The patient did not develop postoperative neurological deficits. On day 15, CTA showed no evidence of VA dissection/pseudoaneurysm formation (Fig. 5E, F). On day 30, the patient required surgical repair for postoperative CSF leakage due to inadequate dural closure. Watertight dural closure was achieved using pericranium and fibrin glue. On day 52, magnetic resonance imaging revealed no evidence of metal artifacts, brainstem injury, hemorrhagic lesion, ischemic stroke, and CSF leakage. No evidence of VA dissection/pseudoaneurysm formation was obtained on magnetic resonance angiography. On day 69, the patient was discharged home without any sequelae. The patient is doing well 2 years after the surgery.
Fig. 5.
Postoperative computed tomography (CT) and three-dimensional CT angiography (3D-CTA)
Fig. 5A–D: No evidence of residual needle fragment or intracranial hemorrhage was obtained on immediate postoperative CT.
Fig. 5E, 5F: No evidence of vertebral artery dissection or pseudoaneurysm formation was obtained on 3D-CTA (day 15).
DISCUSSION
Acupuncture has been practiced in China for over 3,000 years and is currently gaining popularity worldwide as a complementary medicine for various health conditions, such as low back pain, neck pain, osteoarthritis/knee pain, and headache.9 In most countries, acupuncture is performed by licensed acupuncturists or medically trained professionals (eg, medical doctors, physiotherapists, nurses, and midwives).10 In Japan, this treatment is only provided by licensed acupuncturists.11 Acupuncture for low back pain, frozen shoulder, neuralgia, rheumatoid arthritis, cervico-brachial syndrome, and/or neck sprain are covered by public health insurance when the treatment is advised or approved by a medical doctor.11
Acupuncture is generally considered safe when performed by an experienced, well-trained practitioner using sterile needles. However, improperly performed acupuncture can cause serious adverse events.1-8 To date, there is no law that allows self-acupuncture in Japan. Moreover, the reality is that acupuncture needles are easily obtained via the internet.6
Some studies have reported about acupuncture-related spinal complications, including spinal infection, subarachnoid hemorrhage, and spinal cord/nerve root injury.12,13 However, intracranial complications caused by radiologically confirmed acupuncture needle migration are extremely rare.4-8 Only six cases, including ours, have been reported in the literature (Table 1). Three patients presented with penetrating injury to the medulla oblongata,4,7,8 one with injury in the cervical spinal cord and medulla oblongata,5 one with penetrating injury in the cerebellar tonsil and medulla oblongata,6 and one with penetrating injury in the VA.
Table 1.
Cases involving intracranial injury caused by radiologically confirmed acupuncture needle migration
| Abumi et al4
(1996) |
Hama et al5
(2004) |
Miyamoto et al6
(2010) |
Fukaya et al7
(2011) |
El-Wahsh et al8
(2018) |
Current case | |
| Age (years)/sex | 60/F | 70/M | 47/M | 44/M | NA/M | 55/F |
| Acupuncture point | Posterior neck | Posterior neck | Posterior neck | Posterior neck | Posterior neck | Posterior neck |
| Further needle migration | No | No | Yes | No | Yes | No |
| Access | Atlanto-occipital junction | Atlanto-axial junction | Atlanto-occipital junction | Atlanto-occipital junction | Atlanto-occipital junction | Atlanto-occipital junction |
| Needle location | Intradural | Intradural | Intradural | Intra- and extradural | Intra- and extradural | Intra- and extradural |
| Needle direction | Left posterolateral to right anterolateral | Left posterolateral to right anterolateral | Left posterolateral to right anterolateral | Midline | Midline | Right posterolateral to left anterolateral |
| Injury site | Medulla oblongata | Cervical spinal cord / medulla oblongata | Cerebellar tonsil / medulla oblongata | Medulla oblongata | Medulla oblongata | VA |
| Intracranial hemorrhage | None | None | Small subpial hemorrhage | Small subpial hemorrhage | None | None |
| Ischemic stroke | None | NA | None | None | None | None |
| Symptoms | Motor and sensory disturbances in the right upper extremitya | Left facial paresthesiab | Discomfort in the posterior neck | Pain in the left face / lower extremity and dysesthesia in the left lower extremity | None | None |
| Removal surgery | Yes | No | Yes | Yes | Yes | Yes |
| Surgery-related complication | No | NA | No | No | No | CSF leakagec |
| Outcome | Recovered | Deteriorated | Recovered | Improved | Without neurological deficits | Without neurological deficits |
CSF: cerebrospinal fluid
F: female
M: male
NA: not applicable or not available
VA: vertebral artery
aThese symptoms developed 18 years after acupuncture treatment.
bThe symptom appeared 1 year after the needle penetrated the cervical spinal cord and medulla oblongata.
cSurgical repair was required for postoperative CSF leakage.
Figure 6 shows the estimated needle entry point and needle trajectory in the present case. To the best of our knowledge, this is the first case report of penetrating VA injury caused by radiologically confirmed acupuncture needle migration.
Fig. 6.

Schematic diagrams indicating estimated needle entry point (A), and estimated needle trajectory (B, C) in the present case
Fig. 6A: The blue circle indicates the estimated needle entry point.
Fig. 6B: The blue arrow indicates the estimated needle trajectory.
Fig. 6C: Schematic diagram presenting axial plane at the level of the estimated needle trajectory. The acupuncture needle tip may have migrated into the intradural space after penetrating the splenius capitis (SPC), semispinalis capitis (SSC), and rectus capitis posterior major (RCPM) muscles.
OCS: oblique capitis superior muscle
SCM: sternocleidomastoid muscle
T: trapezius muscle
The posterior neck is the common site of acupuncture-related spinal complications.6 Similarly, in all patients with intracranial complications, the acupuncture point is the posterior neck. This may be attributed to the following: First, headache and stiff neck, as in the current case, are the most typical complaints among patients seeking acupuncture.6 Second, the nuchal acupuncture points are used as they are effective for headache and stiff neck.6 Third, neck movements can lead to needle migration.4,6 In cases of spinal complications, the acupuncture needle mainly migrated into the spinal canal via the atlanto-axial junction.6 Meanwhile, in five of six cases involving intracranial complications, the needle migrated into the cranium via the atlanto-occipital junction (Table 1). This may be attributed to the fact that the atlanto-occipital junction is anatomically closer to the cranium than the atlanto-axial junction.
An intracranial migrated needle should ideally be removed urgently to prevent acute-onset complications (such as further needle migration that can cause brainstem injury, cranial nerve injury, and/or vessel injury) and delayed-onset complications (such as secondary gliosis, cavity formation, infection, and/or granuloma in the surrounding nerve tissue).6 A review article showed that patients with central nervous system complications associated with acupuncture needle migration who underwent surgical removal had a significantly better outcome than those who did not.6 Indeed, in two of six cases involving intracranial complications, further needle migration was radiologically observed, and two patients developed delayed-onset neurological deficits (Table 1). Five patients who underwent surgical removal had favorable outcomes. In contrast, one patient who was treated conservatively developed delayed progressive neurological deterioration (Table 1).
To safely remove intracranially migrated needles, operators should confirm the needle location and direction via preoperative radiological imaging. Magnetic resonance imaging as a preoperative diagnostic tool must be avoided because acupuncture needles are commonly made of stainless steel.8 Thus, non-contrast CT and three-dimensional CTA are useful diagnostic modalities for patients with acupuncture-related intracranial complications. Surgical removal may be anatomically straightforward in patients with intracranial needle migration via the posteromedial dura at the foramen magnum level. However, in patients with intracranial needle migration via the posterolateral dura at the level of the foramen magnum, surgical removal can be technically challenging because there are intra- and extradural anatomical structures that can complicate surgery, including the VA, posterior inferior cerebellar artery, lower cranial nerves, and vertebral venous plexus. Meanwhile, in patients with intra- and extradural needle migration, the pull-out maneuver in the epidural space will be a simple and reliable method. El-Wahsh et al showed that the pull-out maneuver in the epidural space under direct visualization via durotomy was a useful option because it can facilitate immediate hemostasis during removal.8 However, in the current case, intradural manipulation was required as the needle was not found in the epidural space. The needle tail might have migrated in the vertebral venous plexus. The pull-out maneuver in the intradural space could have failed due the following reasons: 1) the end of the needle tail was dull, and 2) the needle tail was not exposed. Moreover, operators should be aware that it is technically difficult to cut a stainless steel needle in a limited intradural surgical field. In the current case, the migrated needle could be removed from the intradural space with the pull-in maneuver, and several technical strategies can be used. First, operators should be aware about the length of the needles that migrated to the epidural space (ie, the length of the needle that must be pulled in). If the needle located in the epidural space is longer, the procedure can be more challenging. Second, operators must simulate the direction in which the needle is pulled in. In our case, the contralateral VA could be injured if the needle was pulled in along the long axis direction of the migrated needle. The VA union and/or ipsilateral VA could be injured if the needle was pulled in cranially. Therefore, the migrated needle was pulled in caudally toward a space without major arteries, resulting in its successful removal.
A retrospective review of patients with penetrating spinal injuries showed that the development of CSF leakage was more common in patients who underwent intradural exploration than in those managed conservatively.14 Additionally, posterior fossa surgeries are more frequently associated with CSF leakage compared to supratentorial surgeries.15 In our case, the patients experienced postoperative CSF leakage requiring surgical repair due to inadequate dural closure. The dura must be repaired with great caution during the surgical removal of the infratentorial intracranial migrated needle.
AUTHOR CONTRIBUTION
DA and YH served as co-first authors and contributed equally to this work.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
ETHICS APPROVAL
This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Abbreviations
- CSF
cerebrospinal fluid
- CT
computed tomography
- CTA
computed tomography angiography
- VA
vertebral artery
REFERENCES
- 1.Goldberg I. Pneumothorax associated with acupuncture. Med J Aust. 1973;1(19):941–942. doi: 10.5694/j.1326-5377.1973.tb128849.x. [DOI] [PubMed]
- 2.Halvorsen TB, Anda SS, Naess AB, Levang OW. Fatal cardiac tamponade after acupuncture through congenital sternal foramen. Lancet. 1995;345(8958):1175. doi: 10.1016/s0140-6736(95)91004-2. [DOI] [PubMed]
- 3.Ilhan A, Alioğlu Z, Adanir M, Ozmenoğlu M. Transverse myelopathy after acupuncture therapy: A case report. Acupunct Electrother Res. 1995;20(3-4):191–194. doi: 10.3727/036012995816357078. [DOI] [PubMed]
- 4.Abumi K, Anbo H, Kaneda K. Migration of an acupuncture needle into the medulla oblongata. Eur Spine J. 1996;5(2):137–139. doi: 10.1007/BF00298396. [DOI] [PubMed]
- 5.Hama Y, Kaji T. A migrated acupuncture needle in the medulla oblongata. Arch Neurol. 2004;61(10):1608. doi: 10.1001/archneur.61.10.1608. [DOI] [PubMed]
- 6.Miyamoto S, Ide T, Takemura N. Risks and causes of cervical cord and medulla oblongata injuries due to acupuncture. World Neurosurg. 2010;73(6):735–741. doi: 10.1016/j.wneu.2010.03.020. [DOI] [PubMed]
- 7.Fukaya S, Kimura T, Sora S, Morita A. Medulla oblongata injury caused by an acupuncture needle; Warning for serious complications due to a common method of alternative medicine. J Neurol. 2011;258(11):2093–2094. doi: 10.1007/s00415-011-6072-3. [DOI] [PubMed]
- 8.El-Wahsh S, Efendy J, Sheridan M. Migration of self-introduced acupuncture needle into the brainstem. J Neurosci Rural Pract. 2018;9(3):434–436. doi: 10.4103/jnrp.jnrp_480_17. [DOI] [PMC free article] [PubMed]
- 9.Urits I, Wang JK, Yancey K, et al. Acupuncture for the management of low back pain. Curr Pain Headache Rep. 2021;25(1):2. doi: 10.1007/s11916-020-00919-y. [DOI] [PubMed]
- 10.Bleck RR, Gold MA, Westhoff CL. Training hour requirements to provide acupuncture in the United States. Acupunct Med. 2021;39(4):327–333. doi: 10.1177/0964528420939576. [DOI] [PubMed]
- 11.Ishizaki N, Yano T, Kawakita K. Public status and prevalence of acupuncture in Japan. Evid Based Complement Alternat Med. 2010;7(4):493–500. doi: 10.1093/ecam/nen037. [DOI] [PMC free article] [PubMed]
- 12.Hadden WA, Swanson AJ. Spinal infection caused by acupuncture mimicking a prolapsed intervertebral disc. A case report. J Bone Joint Surg Am. 1982;64(4):624–626. [PubMed]
- 13.Murata K, Nishio A, Nishikawa M, Ohinata Y, Sakaguchi M, Nishimura S. Subarachnoid hemorrhage and spinal root injury caused by acupuncture needle--Case report. Neurol Med Chir (Tokyo). 1990;30(12):956–959. doi: 10.2176/nmc.30.956. [DOI] [PubMed]
- 14.Simpson RK Jr, Venger BH, Narayan RK. Treatment of acute penetrating injuries of the spine: A retrospective analysis. J Trauma. 1989;29(1):42–46. [PubMed]
- 15.Sawaya R, Hammoud M, Schoppa D, et al. Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery. 1998;42(5):1044–1055; discussion 1055–1056. doi: 10.1097/00006123-199805000-00054. [DOI] [PubMed]