ABSTRACT
We aimed to investigate the impact of post-discharge scheduled hospital visits on readmission due to heart failure (HF). In this retrospective study, a total of 245 patients (N = 101 in the scheduled hospital visit group, N = 144 in the non-scheduled hospital visit group) who were alive with free from readmission due to HF for 90 days after discharge were enrolled. The patients had been hospitalized with acute decompensated HF between August 2018 and July 2019. Scheduled hospital visits were recommended 90 days after the patients had been discharged. After checking their self-care adherence, nurse-led self-care maintenance and monitoring were provided. To determine the effectiveness of the scheduled hospital visits, we conducted landmark analyses divided into two periods: Scheduled visits within 180 days, and after 180 days. The readmission rate due to HF within 180 days was lower in the scheduled visit group. In the landmark analysis, the 1-year incidence rate of readmission was significantly lower in patients with a scheduled hospital visit than in those without, in the period within 180 days (2.0% vs 9.0%, P = 0.029) but not after 180 days. After adjusting for age and estimated glomerular filtration rate as confounders, scheduled hospital visits tended to reduce readmission due to HF (P = 0.060); however, readmission was significantly reduced in the period within 180 days (P = 0.007). In conclusion, scheduled hospital visits at 90 days after discharge may be beneficial in delaying readmission due to HF by reducing risk of readmission during the early post-visit period.
Key Words: heart failure, scheduled hospital visit, readmission
INTRODUCTION
In aging populations worldwide, the prevalence of heart failure (HF) is increasing.1,2 Despite recent advances in management and therapy, HF still poses challenges for real clinical practice, with high mortality and readmission rates.3,4 Recent reports have shown that various comorbidities are present in older patients with HF, which lead to poor outcomes.5-8 Given that more heterogeneous and complicated conditions are accompanied by comorbid conditions, a multidisciplinary approach will be a prerequisite to manage older patients well. A post-discharge multidisciplinary approach including post-discharge hospital visiting programs, rehabilitation, nurse-led care, and self-care management (including telephone calls) has been proposed9-11; however, a confirmed post-discharge visiting program to prevent HF readmission has not yet been established in Japan.
Thus, we performed this study to examine whether a post-discharge scheduled visiting program effectively prevents hospitalizations in patients with HF.
METHODS
Study population
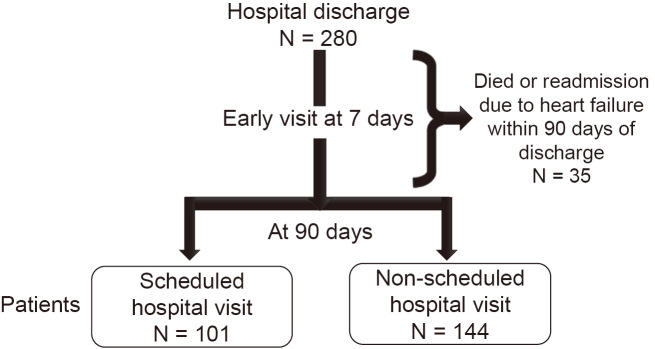
In this retrospective study, a total of 245 patients were enrolled who had been discharged from hospital after admission due to HF and had not been readmitted within the first 90 days post-discharge (Figure 1). The patients had been hospitalized for acute decompensated HF at Kasugai Municipal Hospital between August 2018 and July 2019. We excluded subjects who were undergoing hemodialysis, who had undergone multiple hospitalizations due to HF within the study period, and those with HF caused by acute myocardial infarction. The study protocol complies with the Declaration of Helsinki and was approved by the Committee of Ethics at Kasugai Municipal Hospital. We also offered each patient the opportunity to opt-out, (https://www.hospital.kasugai.aichi.jp/byouin/torikumi/rinsho/rinri/documents/rinri355-3.pdf). No subject decided to opt-out.
Fig. 1.
Study population
Definitions
HF was defined according to the guidelines set by the American College of Cardiology/American Heart Association, which include the signs and symptoms of HF, as well as confirmed left ventricular systolic or diastolic dysfunction.12 Anemia was defined as hemoglobin levels ≤ 13 g/dL (if male) or 12 g/dL (if female) in accordance with the WHO committee.13 The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.14
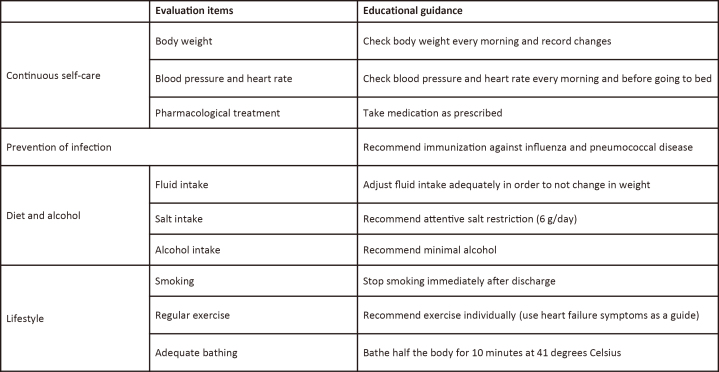
The post-discharge scheduled visiting program consisted of predetermined visits to deliver repetitive self-care support adapted to patients with HF who had been discharged from the Department of Cardiology at Kasugai Municipal Hospital after August 2018. Each patient was recommended to visit the outpatient clinic of our department, or a general physician, 7 days after they were discharged. Following this early visit, each subject visited our department or a general physician. Furthermore, all patients with HF were strongly recommended to attend a scheduled hospital visit after 90 days (± 14 days). Although some patients met this recommendation, others did as per their request or other circumstance. All patients who attended the scheduled visit were all delivered self-care support. Those who visited without a reservation and those who visited outside the predetermined period could not receive self-care support because of lack of information or nurse availability. Scheduled hospital visits 90 days after discharge were determined based on our clinical practice. Out of the patients who were discharged between January and December 2016, the proportion who were rehospitalized during each period to the total number rehospitalized in 1 year, were as follows: 47.3% within 90 days, 26.3% between 90 and 179 days, 21.1% between 180 and 269 days, and 5.3% between 270 and 365 days (Figure 2). HF rehospitalization between 90 and 179 days was relatively high despite the early post-discharge visits after the first week. For this reason, we defined scheduled hospital visits 90 days after discharge to prevent HF rehospitalization in the period between 90 and 179 days. The scheduled visits included the following: First, an attending cardiologist checked the patient’s condition and self-care adherence (including home blood pressure, heart rate, and body weight). Second, nurses provided self-care maintenance via point-by-point interviews, and further promoted self-care monitoring (Figure 3). Finally, all information was sent to the patients’ general physicians.
Fig. 2.
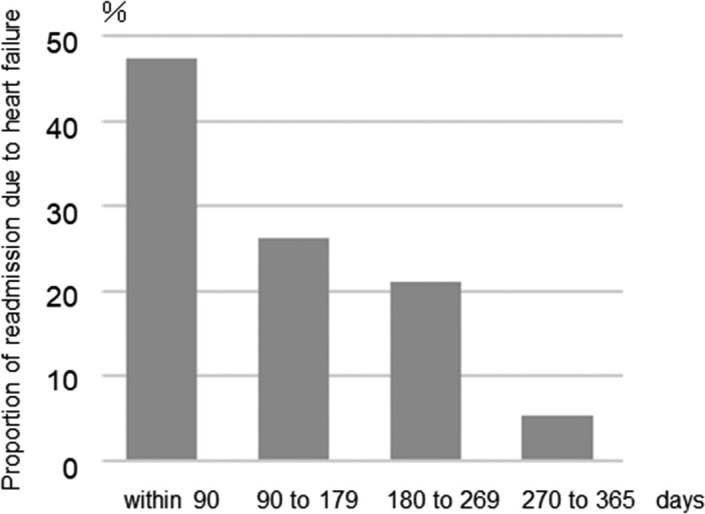
The proportion of heart failure rehospitalization at each period to total rehospitalization within 1-year
Fig. 3.
Evaluating items and educational guidance provided by an attending nurse at the scheduled hospital visit
Data collection
The following clinical characteristics were assessed by retrospective chart review: Age, sex, height, weight, medical history, functional classification according to the New York Heart Association, etiology, non-cardiac comorbidities, vital signs, laboratory data, in-hospital treatment, medication provided before discharge, and 1-year outcomes (mortality and readmission due to HF). Echocardiographic data during hospitalization was also collected. Left ventricular ejection fraction was derived according to the Modified Simpson’s rule.
Statistical analysis
SAS software (version 9.4; SAS Institute Inc. Cary, NC, USA), JMP (version 5.1; SAS Institute Inc. Cary, NC, USA), and EZR (graphical user interface for R, Saitama Medical Center, Jichi Medical University, Saitama, Japan),15 were used to perform statistical analyses. Categorical variables were expressed as counts and percentages, and continuous variables were expressed as medians with interquartile ranges or as a mean ± standard deviation. Categorical variables were compared using the chi-squared test, while distributions of continuous variables were examined using the Shapiro-Wilk test. Continuous variables were compared using the Mann–Whitney U test. Cumulative incidence rates of readmission due to HF were estimated using the cumulative incidence function, and the differences between the two groups were evaluated by Gray test for a competing risk model. Thereafter, a landmark analysis was performed for each period: 90 to 179 days and 180 to 365 days after discharge. Univariate and multivariate Cox regression analyses were used to determine predictors of readmission due to HF and were performed according to each period. Variables with a P-value < 0.05 on univariate analysis, were entered into the multivariate model. All variables that were statistically significant on univariate analysis were considered as potential covariates, and P-values, hazard ratios (HRs), and 95% confidence intervals (CIs) were calculated. Statistical significance was set at P-value < 0.05.
RESULTS
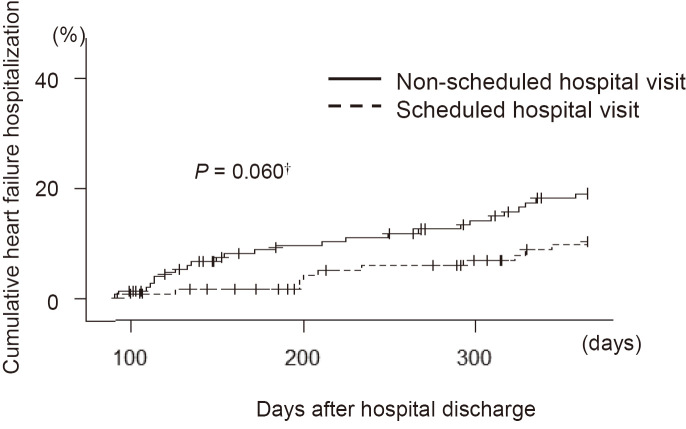
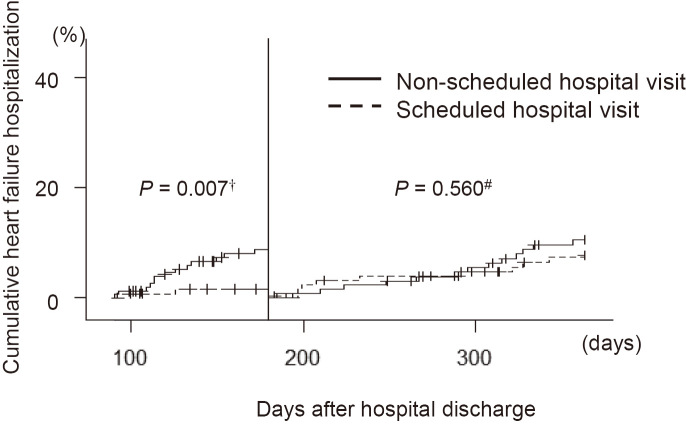
The characteristics of the enrolled patients (N = 101 in the scheduled hospital visit group, N = 144 in the non-scheduled hospital visit group) are shown in Table 1. The median age was 80 years (interquartile range, 72–87 years), and 50.2% of the subjects were male. Non-cardiac comorbidities were observed in descending order: Reduced eGFR (75%), hypertension (73%), and anemia (60%). Angiotensin-converting enzyme or angiotensin II receptor 1 blocker use was significantly higher in the scheduled hospital visit group than in the non-scheduled hospital visit group, and patients were significantly younger in the scheduled hospital visit group. Other variables were similar between the two groups. During the follow-up period (median of 358 days), the cumulative incidence of readmission due to HF was 15.5% (N=38) (Table 2). The readmission rate due to HF within 180 days was lower in the scheduled hospital visit group. In the landmark analysis, the 1-year incidence rate of readmission was significantly lower in patients with scheduled hospital visits than in those without in the period within 180 days (2.0% vs 9.0%, P = 0.029) but not after 180 days (10.1% vs 9.9%, P = 1.000). The univariate Cox regression model identified that scheduled hospital visits, eGFR, and age were significant predictors of 1-year readmission due to HF during the entire period (HR 0.70, 95% CI 0.49−0.97, P = 0.033; HR 0.97, 95% CI 0.95−0.99, P < 0.001; HR 1.04, 95% CI 1.01−1.08, P = 0.019, respectively) (Table 3). After adjusting for age and eGFR as confounders, scheduled hospital visits tended to reduce readmission due to HF (HR 0.73, 95% CI 0.51−1.01, P = 0.060). To determine the effectiveness of the scheduled hospital visits, we conducted landmark analyses by dividing the two periods. Scheduled hospital visits was a significant and independent predictor of 1-year readmission due to HF with adjustment for age and eGFR within 180 days after discharge (HR 0.43, 95% CI 0.17−0.81, P = 0.007). Figures 4 and 5 show the cumulative incident curves for 1-year readmission due to HF during the entire period, and during each period after the landmark analyses.
Table 1.
Characteristics of study patients
| Characteristic | Scheduled hospital visit | Non-scheduled hospital visit | P |
| No. of subjects | 101 | 144 | |
| Age (years) | 78 (71–84) | 82 (72–88) | 0.018 |
| Sex (male/female, %) | 46.5/53.5 | 52.8/47.2 | 0.336 |
| Body mass index (kg/m2) | 23.3 (21.1–25.7) | 22.6 (19.8–25.3) | 0.138 |
| Current or former smoker (%) | 46.5 | 47.2 | 0.916 |
| Type 2 diabetes mellitus (%) | 47.5 | 36.1 | 0.074 |
| Hypertension (%) | 79.2 | 70.8 | 0.140 |
| Dyslipidemia (%) | 59.4 | 49.3 | 0.119 |
| Reduced eGFR (<60 mL·min–1·1.73 m–2) (%) | 77.2 | 73.6 | 0.519 |
| Atrial fibrillation or atrial flutter (%) | 35.6 | 38.2 | 0.684 |
| Previous myocardial infarction (%) | 12.9 | 21.5 | 0.082 |
| Previous stroke (%) | 5.9 | 7.6 | 0.799 |
| Previous heart failure hospitalization before the study period (%) | 20.8 | 29.9 | 0.112 |
| Ischemic etiology (%) | 27.8 | 21.3 | 0.244 |
Categorical variables are described as percentages and continuous variables are given as medians and 25th–75th percentile ranges.
eGFR: estimated glomerular filtration rate
Table 2.
1-year outcomes
| Characteristic | Scheduled hospital visit | Non-scheduled hospital visit | P |
| No. of subjects | 101 | 144 | |
| 1-year outcomes | |||
| All-cause death, n (%) | 5 (5.0) | 13 (9.0) | 0.321 |
| Readmission due to heart failure, n (%) | 12 (11.9) | 26 (18.1) | 0.213 |
| Period within 180 days, n | 2 | 13 | 0.029 |
| Period after 180 days, n | 10 | 13 | 1.000 |
Table 3.
Impact of scheduled hospital visits on 1-year readmission due to heart failure during the entire period or during a sub-period within or after 180 days after discharge
| Univariate | Multivariate | ||||
| HR (95%CI) | P | HR (95%CI) | P | ||
| Entire period | |||||
| Scheduled hospital visit | 0.70 (0.49–0.97) | 0.033 | 0.73 (0.51–1.01) | 0.060 | |
| eGFR | 0.97 (0.95–0.99) | <0.001 | 0.97 (0.96–0.99) | <0.001 | |
| Age | 1.04 (1.01–1.08) | 0.019 | 1.03 (1.00–1.07) | 0.078 | |
| Period within 180 days | |||||
| Scheduled hospital visit | 0.41 (0.16–0.79) | 0.005 | 0.43 (0.17–0.81) | 0.007 | |
| eGFR | 0.97 (0.94–1.00) | 0.025 | 0.97 (0.94–1.00) | 0.034 | |
| Age | 1.02 (0.98–1.08) | 0.319 | 1.01 (0.97–1.07) | 0.589 | |
| Period after 180 days | |||||
| Scheduled hospital visit | 0.89 (0.58–1.33) | 0.560 | 0.93 (0.60–1.40) | 0.716 | |
| eGFR | 0.97 (0.95–0.99) | 0.005 | 0.97 (0.95–0.99) | 0.011 | |
| Age | 1.05 (1.01–1.10) | 0.026 | 1.04 (1.00–1.09) | 0.071 | |
CI: confidence interval
eGFR: estimated glomerular filtration rate
HR: hazard ratio
Fig. 4.
Cumulative incident curves for readmission due to heart failure
†P-value was analyzed in the multivariable Cox regression model with adjustment for eGFR and age.
Fig. 5.
Cumulative incident curves for readmission due to heart failure after landmark analyses
†Value was calculated in the multivariable Cox regression model with adjustment for eGFR and age.
#Value was analyzed in the univariate Cox regression model.
Ninety days after hospital discharge, 57.4% of patients in the scheduled hospital visit group and 75.7% of patients in the non-scheduled hospital visit group were monitored by general physicians (P = 0.003). There was no statistically significant difference in the cumulative incidence of readmission due to HF according to the medical setting (P = 0.063). Among the patients in the non-scheduled hospital visit group and those who were monitored by general physicians, hospital visits 90 days after discharge were at 12.3% between 105 and 179 days, 14.2% between 180 and 365 days, and 73.5% after 1 year or no visit.
DISCUSSION
Our study provides suggestive and observationally derived evidence suggesting that post-discharge scheduled visiting programs might be beneficial in delaying readmission due to HF. Post-discharge visits 90 days after hospital discharge were associated with a significantly reduced risk of readmission during the early post-visit period (within 180 days) in patients with HF.
Recent estimates in Japan have shown that the prevalence of HF will steadily increase until 2035, as the population ages.16 HF has already been recognized as a common disease, therefore, detailed planning against high rates of mortality and readmission as well as against significant post-discharge impairments in quality of life is essential. However, specific characteristics frequently observed in the elderly, such as multiple comorbidities (eg, frailty, cognitive impairment, falls, depression, and disability) make it more difficult for us to develop a uniform disease management program for patients with HF.17 Given that age was an independent clinical factor for patients receiving a scheduled visiting program in our study, there is a possibility that a feasible post-discharge visiting program that is stratified by age could be provided. Despite our results, it is still unclear what can be done for subjects in the non-scheduled hospital group (average age: 82 years).
There is a lurking risk in the transition from hospital stays to home, especially during the vulnerable period. Therefore, a clear pre-discharge planning is pivotal in order to attempt preventable readmissions, especially during this period.18 According to the guidelines published by the European Society of Cardiology, early assessment with a general physician within 1 week of discharge and with a cardiologist within 2 weeks of discharge has been proposed for patients with HF.9 Protocol-driven post-discharge programs have successfully reduced readmission due to HF,19 however, whether subsequent visits in order to prevent readmission due to worsening HF is required, remains unclear. From a large-scale survey performed by Maggioni et al, the rate of readmission due to HF continued to grow after the vulnerable period.20 A similar tendency was observed in the Japanese registry among patients with HF irrespective of their left ventricular ejection fraction or ischemic etiology.21 Therefore, post-discharge continuous management, including self-care maintenance and monitoring, medication adherence, natriuretic peptide measurement, and contingency planning, is necessary for the prevention of HF readmission.12 As far as we investigated, our study is the first to characterize the efficacy of post-discharge scheduled hospital visits in addition to early visits to the outpatient clinic of core hospitals. Although scheduled hospital visits 90 days after hospital discharge showed a significant reduction in readmission within 180 days, this beneficial effect was not sustainable after 180 days.
Multidisciplinary post-discharge strategies, including self-care support, were reported to be effective in managing patients with HF.22 Sato et al emphasized the importance of self-care support as part of a comprehensive multidisciplinary program. Medication taking, symptom monitoring, dietary prudence, fluid and alcohol limitations, weight loss due to cachexia, daily exercise, smoking cessation, and preventive measures were all mentioned in the guidelines.9,23 However, studies have shown that unfavorable HF patient prognoses are attributable to poor adherence to self-care recommendations.24,25 In addition, no specific program consistently showed improved prognoses, but longer durations seemed to improve the effects of self-management interventions on the prognosis of patients with HF.26 A post-discharge outpatient visit has been proposed as a fulcrum for the multidisciplinary services available to patients with HF, as well as an opportunity to fill any gaps that might have occurred in the evidence-based care of the patients. Determining what should be done at the visit or who should do what, remains to be established.11 Although the variety of characteristics of patients with HF and the multiple possible comorbidities might complicate the integrated strategies, repetitive self-care support using planned post-discharge scheduled hospital visits should be valid in daily clinical practice. We especially valued nurse-led education to improve self-care and monitoring of individual patients at the post-discharge scheduled hospital visit in this study. Given that self-care support has already been established to be effective in the management of HF, it is possible that repeated delivery of this opportunity through the post-discharge scheduled hospital visits brought the contribution to the delay of readmission due to HF.
The present study has some limitations: (i) The results presented here are only from a single hospital with a relatively small sample size, therefore, replication with larger sample sizes will be needed. (ii) Clinical factors not collected from our medical records, such as dietary lifestyle and adherence to medications, could have influenced our findings. (iii) We did not evaluate the clinical efficacy of the post-discharge visit randomly. Accordingly, study subjects between the scheduled hospital visit group and non-scheduled visit group were heterogeneous. (iv) We scheduled a post-discharge hospital visit only 90 days in addition to an early visit after discharge. However, we did not taken into consideration the possibility of other schedules that could be effective. (v) Patients who had died or who were readmitted within 90 days after discharge were excluded; these results cannot be adapted for critically ill patients or patients at high risk of readmission. (vi) It is possible that patients who did not get with the recommended medical programs could tend to refuse other physician’s instructions. In conclusion, this study suggests that post-discharge scheduled hospital visits at 90 days after discharge might be beneficial for delaying readmission due to HF.
ACKNOWLEDGEMENTS
We gratefully acknowledge the work of past and present members of our department for their helpful discussions, and their comments on the manuscript. And we especially wish to thank S. Ito for collecting the medical data.
CONFLICT OF INTEREST
This study received no grants from any funding agency within the public, commercial, or non-profit sectors.
Abbreviations
- CI
confidence interval
- eGFR
estimated glomerular filtration rate
- HF
heart failure
- HR
hazard ratio
REFERENCES
- 1.Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63(12):1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed]
- 2.Shimokawa H, Miura M, Nochioka K, Sakata Y. Heart failure as a general pandemic in Asia. Eur J Heart Fail. 2015;17(9):884–892. doi: 10.1002/ejhf.319. [DOI] [PubMed]
- 3.Shiraishi Y, Kohsaka S, Sato N, et al. 9-Year Trend in the Management of Acute Heart Failure in Japan: A Report From the National Consortium of Acute Heart Failure Registries. J Am Heart Assoc. 2018;7(18):e008687. doi: 10.1161/JAHA.118.008687. [DOI] [PMC free article] [PubMed]
- 4.Yaku H, Ozasa N, Morimoto T, et al. Demographics, Management, and In-Hospital Outcome of Hospitalized Acute Heart Failure Syndrome Patients in Contemporary Real Clinical Practice in Japan – Observations From the Prospective, Multicenter Kyoto Congestive Heart Failure (KCHF) Registry. Circ J. 2018;82(11):2811–2819. doi: 10.1253/circj.CJ-17-1386. [DOI] [PubMed]
- 5.Paolillo S, Scardovi AB, Campodonico J. Role of comorbidities in heart failure prognosis Part I: Anaemia, iron deficiency, diabetes, atrial fibrillation. Eur J Prev Cardiol. 2020;27(2_suppl):27–34. doi: 10.1177/2047487320960288. [DOI] [PMC free article] [PubMed]
- 6.Tedeschi A, Agostoni P, Pezzuto B, et al. Role of comorbidities in heart failure prognosis Part 2: Chronic kidney disease, elevated serum uric acid. Eur J Prev Cardiol. 2020;27(2_suppl):35–45. doi: 10.1177/2047487320957793. [DOI] [PMC free article] [PubMed]
- 7.van Deursen VM, Urso R, Laroche C, et al. Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16(1):103–111. doi: 10.1002/ejhf.30. [DOI] [PubMed]
- 8.Braunstein JB, Anderson GF, Gerstenblith G, et al. Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J Am Coll Cardiol. 2003;42(7):1226–1233. doi: 10.1016/s0735-1097(03)00947-1. [DOI] [PubMed]
- 9.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed]
- 10.Lainscak M, Blue L, Clark AL, et al. Self-care management of heart failure: practical recommendations from the Patient Care Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2011;13(2):115–126. doi: 10.1093/eurjhf/hfq219. [DOI] [PubMed]
- 11.Gheorghiade M, Bonow RO. Heart failure: Early follow-up after hospitalization for heart failure. Nat Rev Cardiol. 2010;7(8):422–424. doi: 10.1038/nrcardio.2010.102. [DOI] [PubMed]
- 12.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137–e161. doi: 10.1161/CIR.0000000000000509. [DOI] [PubMed]
- 13.WHO Scientific Group on Nutritional Anaemias & World Health Organization. Nutritional anaemias: report of a WHO Scientific Group. World Health Organ Tech Rep Ser. 1968;405:5–37. [PubMed]
- 14.Levey AS, Stevens LA, Schmid CH, et al. A New Equation to Estimate Glomerular Filtration Rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed]
- 15.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed]
- 16.Okura Y, Ramadan MM, Ohno Y, et al. Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J. 2008;72(3): 489–491. doi: 10.1253/circj.72.489. [DOI] [PubMed]
- 17.Matsue Y, Kamiya K, Saito H, et al. Prevalence and prognostic impact of the coexistence of multiple frailty domains in elderly patients with heart failure: the FRAGILE-HF cohort study. Eur J Heart Fail. 2020;22(11):2112–2119. doi: 10.1002/ejhf.1926. [DOI] [PubMed]
- 18.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol. 2013;61(4):391–403. doi: 10.1016/j.jacc.2012.09.038. [DOI] [PubMed]
- 19.Donaho EK, Hall AC, Gass JA, et al. Protocol-Driven Allied Health Post-Discharge Transition Clinic to Reduce Hospital Readmissions in Heart Failure. J Am Heart Assoc. 2015;4(12):e002296. doi: 10.1161/JAHA.115.002296. [DOI] [PMC free article] [PubMed]
- 20.Maggioni AP, Dahlström U, Filippatos G, et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail. 2013;15(7):808–817. doi: 10.1093/eurjhf/hft050. [DOI] [PubMed]
- 21.Ushigome R, Sakata Y, Nochioka K, et al. Temporal trends in clinical characteristics, management, and prognosis of patients with symptomatic heart failure in Japan — report from the CHART Studies. Circ J. 2015;79(11):2396–2407. doi: 10.1253/circj.CJ-15-0514. [DOI] [PubMed]
- 22.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810–819. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed]
- 23.Sato Y. Multidisciplinary management of heart failure just beginning in Japan. J Cardiol. 2015;66(3):181–188. doi: 10.1016/j.jjcc.2015.01.007. [DOI] [PubMed]
- 24.Seid MA, Abdela OA, Zeleke EG. Adherence to self-care recommendations and associated factors among adult heart failure patients. From the patients’ point of view. PLoS One. 2019;14(2):e0211768. doi: 10.1371/journal.pone.0211768. [DOI] [PMC free article] [PubMed]
- 25.van der Wal MH, Jaarsma T, van Veldhuisen DJ. Non-compliance in patients with heart failure; how can we manage it? Eur J Heart Fail. 2005;7(1):5–17. doi: 10.1016/j.ejheart.2004.04.007. [DOI] [PubMed]
- 26.Jonkman NH, Westland H, Groenwold RH, et al. What Are Effective Program Characteristics of Self-Management Interventions in Patients With Heart Failure? An Individual Patient Data Meta-analysis. J Card Fail. 2016;22(11):861–871. doi: 10.1016/j.cardfail.2016.06.422. [DOI] [PMC free article] [PubMed]