Abstract
Purpose of Review
Social determinants of health (SDH) are factors that affect patient health outcomes outside the hospital. SDH are “conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.” Current literature has shown SDH affecting patient reported outcomes in various specialties; however, there is a dearth in research relating spine surgery with SDH. The aim of this review article is to identify connections between SDH and post-operative outcomes in spine surgery. These are important, yet understudied predictors that can impact health outcomes and affect health equity.
Recent Findings
Few studies have shown associations between SDH pillars (environment, race, healthcare, economic, and education) and spine surgery outcomes. The most notable relationships demonstrate increased disability, return to work time, and pain with lower income, education, environmental locations, healthcare status and/or provider. Despite these findings, there remains a significant lack of understanding between SDH and spine surgery.
Summary
Our manuscript reviews the available literature comparing SDH with various spine conditions and surgeries. We organized our findings into the following narrative themes: 1) education, 2) geography, 3) race, 4) healthcare access, and 5) economics.
Keywords: Social determinants of health, Education, Geography, Healthcare access, Race, Spine surgery
Introduction
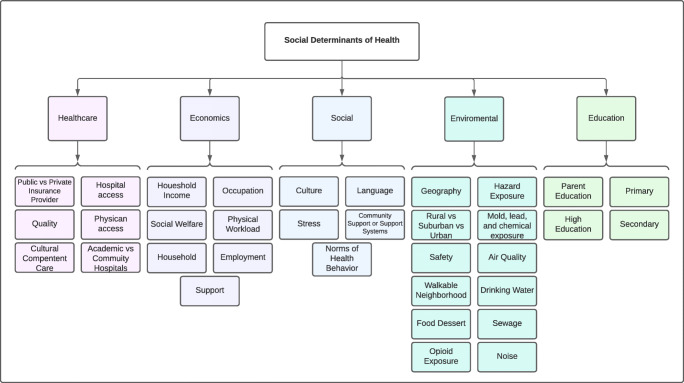
According to the World Health Organization, health is more than the absence or presence of disease but encompasses the complete physical, mental, and social well-being of a person [1]. To address these, physicians must understand the social determinants of health (SDH) to deliver quality healthcare. SDH can be defined as the “conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks ” [2]. SDH affect patient health and well-being in multiple capacities. Education, race, geography, healthcare access, and economic factors are fundamental aspects of SDH leading to health inequalities between different patient groups (Fig. 1) [2–5]. These pillars of SDH have been documented in various medical specialties ranging from pediatrics to neurosurgery. [6–18]. Even in the present day of the SARS-CoV-2 pandemic, COVID-19 mortality has been associated with SDH [12, 18]. Within the field of orthopedic surgery, research has shown that various subspecialities including shoulder, elbow, hand, and hip post-surgical outcomes have been affected by SDH [13–17]. However, the question still remains: how does SDH affect outcomes in spine surgery?
Fig. 1.
The pillars of social determinants of health and subcategories
Much of the current literature regarding SDH in spine surgery has focused on lower back pain in lower education and income cohorts leading to poor post-operative outcomes [19, 20]. The interplay of individual SDH and surgical outcomes in spine surgery is not well studied in the literature. It is fundamentally important to understand and analyze relationships between spine surgery and SDH to redress health inequality amongst marginalized patient populations. The aim of this review is to highlight studies identifying the relationship between spine surgery and SDH, focusing on the aforementioned pillars.
Education
The importance of education in SDH has been widely accepted as a pivotal factor affecting patient longevity, with more years of schooling correlating to longer lifespans [21]. Each year of education attained by a patient is associated with 1.37 years gained in life expectancy [22••]. Numerous measurable metrics have demonstrated the impact that education can have on return to work (RTW), Oswestry Disability Index (ODI), and post-operative pain.
Several studies have evaluated the impact of education when investigating RTW. Using a large database, Macki et al. found that patients undergoing lumbar surgeries for degenerative disease with any college education was a strong predictor of minimal clinically important difference (MCID) for ODI (p-value = 0.003) as well as RTW at 1 year (p-value = 0.001) [23, 24]. Another study analyzing predictive factors of RTW examined 4,694 patients who underwent spine surgery for degenerative lumbar disease, and found that higher education levels (post-college degree) significantly increased the likelihood of RTW compared to patients with less than a high-school level education [25]. These findings are further supported by Zieger et al., who retrospectively evaluated 305 patients undergoing surgery for disc herniation and noted that the RTW cohort had significantly higher education (college or university) compared to non-RTW cohort [26]. Notably, these studies acknowledge a potential selection bias due to patients not responding to the questionnaires/interviews at specific follow-up time points.
When assessing pain and disability after lumbar decompression for spinal stenosis, Elsayed et al. found that patients with no college education had significantly greater back and leg pain visual analog scale (VAS) scores compared to patients with formal college education pre-operatively [27]. Despite differences in VAS, both cohorts showed improvement in functional outcomes at 3 and 12 months post-operatively. In another study, Soriano et al. analyzed 203 lumbar deformity correction cases from 2002 to 2006 and found that patients with higher education levels had more favorable post-operative VAS scores and ODI scores [28]. It should be noted Soriano’s criteria for higher education combined both high school and other higher levels of education such as college/university. Interestingly, in a 5-year prospective study on patients undergoing lumbar microdiscectomy in Greece, only patients with primary education had worse VAS, ODI, Roland Morris Disability Questionnaire (RMDQ) and Short Form 36 Health Survey (SF-36) scores compared to secondary (p-value < 0.05) and university level education (p-value < 0.05) [29]. In another study reviewing clinical outcomes in 13,406 patients undergoing decompression for lumbar spinal stenosis from 2008 to 2012 in Sweden, Iderberg et al. noted that the higher education cohort (university level or higher) had lower ODI scores at 1 year after surgery [30]. Similar findings were observed in a study performed by Kim et al. that examined 155 patients diagnosed with lumbar spinal stenosis at a Korean tertiary care center [31]. Kim et al. reported that higher education was correlated with lower leg VAS, back VAS, ODI, and less catastrophizing. This study’s findings are in accordance with the studies by Soriano, Iderberg, and Gelalis et al., which also showed that higher VAS scores correlated with lower education levels.
When considering long-term employment as an outcome measure, Furnes et al. found that a higher level of education significantly impacted employment status (p-value = 0.03) in a randomized controlled trial of 82 patients undergoing lumbar disc replacement [32]. These results support the impact of higher education on long term employment, whereas the studies by Macki et al. and Asher et al. highlight the impact of higher education on shorter term employment (2 years and 3 months, respectively).
Education levels affect disability, pain, and RTW timing of patients undergoing lumbar surgery. These findings suggest that surgeons should consider patients’ education level and anticipate perioperative support if needed. Future studies should employ a standardized cutoff to define higher education from lower education, as one of the main drawbacks from the current literature is the varying definition of higher education.
Geography
The interplay between patients and their environment is paramount to public health as location can have a significant impact on mortality rates [33–35]. The World Urbanization Prospect 2018 Revision reported that health outcomes differ among patients within rural and urban communities [36]. For example, an urban environment impacts the amount of physical activity acquired during adolescence [37]. The role of environment as a factor in SDH is multifaceted—encompassing physical, chemical, and biological factors—which make an impact at the regional and national levels [38]. The interactions between the environment and spine surgery have yet to be clearly examined.
In the context of cervical spinal surgery, Angevine et al. analyzed national and regional rates of anterior cervical discectomy and fusions (ACDF) performed from the National Hospital Discharge Survey between 1990 and 1999 [39]. They reported that the Northeast had the lowest number of ACDFs performed (19 per 100,000) while the South had the highest rates of ACDFs performed (42 per 100,000). Another study reviewed medical beneficiaries enrolled in Medicare from 1992 to 2005 [40]. Wang et al. found the highest rates of cervical fusions were performed in the Northwest and South-Central US. These differences suggest slight disparities in care and clinical decision making based upon geographic location. The authors attribute these differences to increases in the prevalence of cervical disc disease, increase in density of spine surgeons, extending candidacy for surgery, and surgical techniques [39, 40]. Regional differences for lumbar fusions have been well documented with variations based on city and county [41, 42]. When searching the PearlDiver database between 2004 and 2009, Pannell et al. found higher rates of lumbar fusion surgeries in the Midwest and South while the lowest rates were in the Northeast [41]. Pannell et al. suggest that the variability among regions is possibly linked to differences in knowledge, experience, and understanding of the current literature by spine surgeons [41].
An understudied area of research within the current literature is the differences between rural and urban environments. In a cross-sectional study for Medicare beneficiaries in 2006, Francis et al. reported rural patients were more likely to undergo lumbar fusion compared to urban beneficiaries [43]. According to Francis et al. the differences in rural vs urban populations could be attributed to cultural or behavior differences, access to healthcare, or rural communities having a higher burden of disease. In comparison, a study using the National Inpatient Sample with a cohort of 84,953 patients, Kim et al. found urban hospitals were less likely to perform lumbar decompression with or without fusion compared to rural hospitals (p-value < 0.001) [44••]. Additionally, hospitals located in suburban areas were more likely to perform decompression compared to urban locations (p-value = 0.03). [44••]. Among all of the above mentioned studies, the differences between urban, rural, and suburban hospitals have been attributed to variability of cost, reimbursement, surgeon characteristics, or resource allocation [41, 43–45].
Another important factor in spine surgery that has been demonstrated to impact outcomes is prescribing patterns in pre-operative opioids. Current literature reports a strong association between prolonged pre-operative opioid use and poor post-operative outcomes; however, regional differences exist [46–55]. In a retrospective database study reviewing 13,257 patients who underwent lumbar decompression and fusion from 2007-2016, Adogwa et al. reported that patients living in Western and Southern states had a higher likelihood of prolonged (>1 year) postoperative opioid use (West: OR 1.26, 95% CI: 1.095–1.452 South: OR 1.18, 95% CI: 1.074–1.287) [46, 56]. Of note, sampling bias may be present as there was a disproportionate number of patients in the South (63.1%) and Midwest (24.3%) cohorts compared to the West (10.5%) and Northeast cohorts (2.1%). In another study assessing 25,329 patients from 2010 to 2015, Massie et al. reported that patients who underwent a spinal procedure (anterior or posterior cervical fusion, lumbar decompression, or lumbar fusion) and lived in the Northeast were significantly less likely to refill their opioid prescription post-operatively (p-value = 0.008) [57•]. Patients living in the Midwest (p-value < 0.001) and West (p-value = 0.019) were significantly more likely to refill opioid prescriptions compared to patients in the South. Again, risk of sampling bias should be noted for the study since a higher number of patients were living in the South (39.1%) and North Central regions (26.3%) compared to the Northeast (18.3%) and West regions (15.8%). Adogwa et al. suggested that the regional variation in opioid use may not be affected solely by discrete patient characteristics (i.e., employment, insurance status, or invasiveness of procedure) but rather a combination of patient characteristics, lack of consensus for optimum post-operative opioid use, and possibly practice variations due to varying levels of policy (local, regional, or state level) [56]. In a study utilizing an insurance claims database from 2010 to 2015, Harris et al. analyzed 28,813 patients and reported data on US regional differences in opioid prescriptions in patients undergoing ACDF [58]. Similar to studies published by Adogwa et al. and Massie et al., Harris et al. found that the rates and duration of chronic opioid use were highest in the Western US (p-value < 0.001). Additionally, pre-operative opioid, drug abuse, depression, and anxiety were all risks factors of chronic opioid use [53, 59, 60].
In conclusion, the environment in which patients live affects the rate of fusion, opioid exposure, as well as other psychiatric comorbidities (anxiety/depression). It should be recognized that environmental factors within SDH cover a wide variety of elements [61–68]. Future research focused on analyzing patient outcomes should consider important environmental/geographical variables.
Race
Racial disparities in patient care have been shown to significantly impede equitable healthcare delivery. Racial minorities reportedly receive lower quality of care and face greater morbidity for different chronic diseases compared to non-minorities [69–74]. In fact, the infant mortality rate per 1000 livebirths for Black, non-Hispanic children (10.8) is more than double the rate for White, non-Hispanic children (4.9) [75]. While the cause of such disparities remain in question, the presence of such disparities is not.
Disparities in post-operative outcomes after spine surgery have also been well-documented [76–84]. Khan et al. investigated patient outcomes after surgery for degenerative spine disease and found that Black patients had a 55% higher chance of death relative to White patients [RR = 1.55, 95% CI = 1.28–1.87, I2 = 70%] [76]. Also, Black patients had a higher risk of non-home discharge (RR 1.63; 95% CI, 1.47–1.81; I2 = 89%), 30-day readmission (RR 1.45; 95% CI, 1.03–2.04; I2 = 96%), and longer average length of stay by 0.93 days (95% CI, 0.75–1.10; I2 = 73%). When examining post-operative hospital readmissions, Martin et al. found that Black patients were at greater risk of 30-day readmission as well (OR: 2.20, C.I. 95% (1.04, 4.64)) [77]. Schoenfeld et al. compiled studies that investigated complications and mortality among different racial groups following spine surgery, joint replacement, or other orthopedic procedures; approximately 64% of the studies analyzed reported disparities among racial minorities [78]. Similar trends are observed when analyzing specific spinal surgeries. Skolasky et al. found that while there were no differences in mortality or complications between Caucasian and Hispanic patients following cervical spine surgery, African American patients had a higher inpatient mortality (OR 1.59; 95% CI, 1.30–1.96) and in-hospital complications (OR 1.37; 95% CI 1.27–1.48) [79]. Furthermore, Elsamadicy et al. concluded that African American patients had lower baseline and follow-up patient-reported outcomes (PROs) after elective lumbar spine surgery—specifically ODI (p-value < 0.0001), VAS-LP (p-value = 0.0007), and VAS-BP scores (p-value = 0.0002) [80]. Additionally, in terms of patient-reported satisfaction measures, African American patients were less likely to report that the surgery met their expectations (3 months: 47.2% vs 65.5%, p = 0.01; 12 months: 35.7% vs 62.7%, p = 0.007). Reyes et al. found that when comparing procedural types, fusions were generally similar amongst racial/ethnic groups. However, for many fusion procedures, more medical complications and longer lengths of stay were observed for African American and Hispanic patients compared to White patients [81•]. Kim et al. found that Hispanic and Asian/Pacific Islander patients were less likely to receive a fusion for a similar diagnosis compared to White patients (p-value < 0.001) [82]. However, in a different study using institutional data, Elsamadicy et al. found no significant difference among Black and White patients with regards to neck disability index, VAS, or SF-12 at 3-months and 12-months after ACDF [83]. Finally, Wang et al. studied racial disparities in the setting of adult spinal deformity [84]. Using a nationwide sample, they discovered that from 2004 to 2014, adult spinal deformity surgery usage among Black patients increased from 24.0 to 50.9 per 1,000,000 people, whereas usage amongst White patients increased from 29.9 to 73.1 per 1,000,000 people, which was a greater proportional increase, indicating increased racial disparities in adult spinal deformity surgery utilization.
In conclusion, race has been shown to affect health outcomes across a multitude of spine surgeries, including degenerative cervical and lumbar spine surgery, as well as deformity cases. It should be noted that not all studies controlled for socioeconomic factors such as household income. However, most if not all studies included some type of control for various confounders. Racial minorities tend to face worse outcomes and higher mortality post-operatively. Finally, it is important to note that many of the studies acknowledge how different, complex societal factors may serve as potential confounders. Future studies must attempt to control further societal factors (e.g. access to vehicle) to clearly explore how race may affect health outcomes in spine surgery.
Healthcare Access
Different insurance plans provide patients varying types of healthcare access and quality. In 2020, according to the US Census Bureau, approximately 91.4% of individuals had health insurance for at least a portion of the year [85]. Private health insurance (66.5%) was more common than public health insurance (34.8%) [85]. The two most prevalent types of public health insurance include Medicaid and Medicare [85, 86]. Uninsured individuals, who represented about 8.6% of the population in 2020, often lack primary care providers and face financial barriers to critical health care operations and medications [85, 87]. Moreover, disparities in health outcomes between individuals of different health insurance groups—including private insurance, public insurance, and uninsured—have been shown to exist[83]
Specifically for spinal fusion operations, there is conflicting evidence over the presence of health outcome disparities between payer groups [88–95]. Tanenbaum et al. conducted a study to determine the association between insurance status and adverse quality metrics after cervical fusion procedures. Using Nationwide Inpatient Sample data from 1998–2011, they concluded that Medicaid and self-pay patients were at higher risk of hospital-acquired, post-operative conditions relative to privately insured patients [88]. In a different study in patients that underwent lumbar spinal fusions, Tanenbaum et al. found that both Medicaid and self-pay patients were at higher risk of adverse events in the postoperative period compared to privately insured patients (OR 1.16, 95% CI 1.07–1.27) [89]. Along the same lines, Rasouli et al. determined that relative to privately insured patients, Medicaid patients had longer lengths of stay (p-value = 0.004) and higher rates of 30-day (p-value = 0.0009) and 90-day (p-value = 0.0009) emergency department visits following ACDF [90•]. However, Bhandarkar et al. found that hospitals which have a higher proportion of ACDF patients billed as self-pay, Medicaid, or charity care faced greater inpatient costs, but did not have increased adverse patient events [91]. In light of the aforementioned contradicting findings, the impact of insurance on outcome disparities in ACDF patients is still unclear.
Orhurhu et al. investigated disparities in the use of spine augmentation (vertebroplasty or kyphoplasty) for patients who sustained osteoporotic fractures; they determined that patients under Medicaid (p-value < 0.001), self-pay (p-value < 0.001), and private insurance (p-value = 0.001) all were significantly less likely to receive spine augmentation procedures relative to patients under Medicare [92]. Based on these studies, the presence of healthcare disparities for patients following fracture treatment is also inconclusive.
Finally, the results of studies investigating the association between insurance plan and outcomes after decompression or fusion for lumbar spinal stenosis appear to be more consistent. Lad et al. determined that Medicaid patients had significantly lower reoperation rates at 2 years relative to commercially insured patients (7.22% vs 10.30%, p-value = 0.0002) [93]. A similar trend persisted after 2 years (13.92% vs 16.89%, p-value < 0.0001). Furthermore, Medicaid patients were much less likely to undergo reoperation with fusion (p-value < 0.0001). Elsayed et al. also found that patients with public insurance reported slightly worse outcomes and quality of life after decompression surgery for lumbar spinal stenosis compared to patients with private insurance [94]. Both these studies support the presence of disparities among different payer groups for lumbar spinal stenosis operations.
In conclusion, the presence of disparities in health outcomes among different payer groups is currently inconclusive for spinal fusions, however, there seems to be more conclusive evidence of healthcare-based disparities for lumbar decompression surgeries. It is important to note that many of the studies cite potential confounding variables, including supplemental insurance plans and different baseline levels of age and sex between insurance groups—such variables should be considered and more rigorously controlled in future studies.
Economics
Economic stability is necessary for optimizing health equity and minimizing adverse health outcomes [95]. Currently, there is scarcity of literature involving the impact of economic status on health outcomes in spine surgery. Jackson et al. demonstrated a higher prevalence of established surgical risk factors such as obesity, smoking, sedentary lifestyles, and low-quality diets in low- and middle-income adolescents [96].
To our knowledge, in one of the only studies to date examining occupation type and outcomes of elective lumbar surgery, Khan et al. investigated the relationship between type of work and return to work within 1-year post-surgery. The authors determined that patients with more physically demanding occupations, a workers’ compensation claim, or on short-term disability leave at the time of surgery all had lower RTW rates, independent of medical complications and readmissions [97]. It is important to note that the physical demand of an occupation is not a perfect proxy for income, and the results must not be interpreted as such. To date, there are few studies that have assessed socioeconomic or occupational disparities in spine surgery, necessitating further research in this field.
Conclusion
The concept of SDH is not new. Rather the incorporation of these various factors—education, race, insurance status, economics, and environment—under one umbrella term is novel to the field of research. The connection between them all is best explained by the conceptual framework outlined by the World Health Organization [98]. For example, the social, economic, and political systems within society set up socioeconomic positions. These socioeconomic positions break down populations based on social class, gender, race/ethnicity, culture, education, and income amongst many others. It’s important to note that differences in education lead to variability in occupation; therefore, leading to differences in income. All these factors lead to a wide spectrum of social support, lifestyle, living and working conditions impacting the health of patients.
To date, some evidence exists suggesting the impact of education, race, geography, healthcare, and economic factors can affect the outcomes of spine surgery. However, there are increasingly clear gaps within our current understanding. Future studies examining patient outcomes should not only include SDH elements but controls in statistical analysis. We propose the inclusion of a questionary or survey (i.e., Accountability Health Communities Screen Tool) along with propensity matching to more accurately incorporate reliable SDH qualities within spine surgery [99].
With this new knowledge, spine surgeons should consider patients SDH factors more when treating patients post-operatively. For example, the incorporation of community health workers into the care team can help reduce hospitalization while improving patient quality of care [100].
Acknowledgments
Code availability
N/A
Institution information
From, Northwestern Feinberg School of Medicine
Author Contribution
All authors reviewed the manuscript, approved the final manuscript, and agree to be held responsible for all aspects of the work.
Data availability
N/A
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of interest
Samuel Reyes, Pranav Bajaj, Bejan Alvandi, Steven Kurapaty, Alpesh Patel, and Srikanth Divi declare that they have no conflict of interest.
Footnotes
This article is part of the Topical Collection on Updates in Spine Surgery - Techniques, Biologics, and Non-Operative Management
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Samuel G. Reyes, Email: samuel.reyes@northwestern.edu
Pranav M. Bajaj, Email: pranav.bajaj@northwestern.edu
Bejan A. Alvandi, Email: bejan.alvandi@gmail.com
Steven S. Kurapaty, Email: steven.kurapaty@northwestern.edu
Alpesh A. Patel, Email: alpesh.patel@nm.org
Srikanth N Divi, Email: srikanth.divi@nm.org.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Forty-ninth edition (including amendments adopted up to 31 May 2019). License: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization. 2020.
- 2.Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved 2021, from https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
- 3.Spruce L. Back to Basics: Social Determinants of Health. AORN J. 2019;110:60–69. doi: 10.1002/aorn.12722. [DOI] [PubMed] [Google Scholar]
- 4.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 129(Suppl 2):19–31. [DOI] [PMC free article] [PubMed]
- 5.Fuchs VR. Social Determinants of Health: Caveats and Nuances. JAMA. 2017;317:25–26. doi: 10.1001/jama.2016.17335. [DOI] [PubMed] [Google Scholar]
- 6.Reno R, Hyder A. The Evidence Base for Social Determinants of Health as Risk Factors for Infant Mortality: A Systematic Scoping Review. J Health Care Poor Underserved. 2018;29:1188–1208. doi: 10.1353/hpu.2018.0091. [DOI] [PubMed] [Google Scholar]
- 7.Quiñones J, Hammad Z. Social Determinants of Health and Chronic Kidney Disease. Cureus. 2020;12:e10266. doi: 10.7759/cureus.10266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkman JM, Dallas J, Lim J, Bhatia R, Gaulden A, Gannon SR, Shannon CN, Esbenshade AJ, Wellons JC. Social determinants of health affecting treatment of pediatric brain tumors. J Neurosurg Pediatr. 2019;24:159–165. doi: 10.3171/2019.4.PEDS18594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DInur-Schejter Y, Stepensky P. Social determinants of health and primary immunodeficiency. Ann Allergy Asthma Immunol. 2022;128:12–18. doi: 10.1016/j.anai.2021.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Hoyler MM, Abramovitz MD, Ma X, Khatib D, Thalappillil R, Tam CW, Samuels JD, White RS. Social determinants of health affect unplanned readmissions following acute myocardial infarction. J Comp Eff Res. 2021;10:39–54. doi: 10.2217/cer-2020-0135. [DOI] [PubMed] [Google Scholar]
- 11.Dang S, Shinn JR, Campbell BR, Garrett G, Wootten C, Gelbard A. The impact of social determinants of health on laryngotracheal stenosis development and outcomes. Laryngoscope. 2020;130:1000–1006. doi: 10.1002/lary.28208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. 2020;8:659–661. doi: 10.1016/S2213-2600(20)30234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jayakumar P, Teunis T, Vranceanu A-M, Moore MG, Williams M, Lamb S, Ring D, Gwilym S. Psychosocial factors affecting variation in patient-reported outcomes after elbow fractures. J Shoulder Elb Surg. 2019;28:1431–1440. doi: 10.1016/j.jse.2019.04.045. [DOI] [PubMed] [Google Scholar]
- 14.Crijns TJ, Bernstein DN, Ring D, Gonzalez R, Wilbur D, Hammert WC. Factors Associated With a Discretionary Upper-Extremity Surgery. J Hand Surg [Am] 2019;44:155.e1–155.e7. doi: 10.1016/j.jhsa.2018.04.028. [DOI] [PubMed] [Google Scholar]
- 15.Rubenstein WJ, Harris AHS, Hwang KM, Giori NJ, Kuo AC. Social Determinants of Health and Patient-Reported Outcomes Following Total Hip and Knee Arthroplasty in Veterans. J Arthroplast. 2020;35:2357–2362. doi: 10.1016/j.arth.2020.04.095. [DOI] [PubMed] [Google Scholar]
- 16.Suleiman LI, Manista GC, Sherman AE, Adhia AH, Karas V, Sporer SM, Levine BR. The Impact of Race and Socioeconomic Status on Total Joint Arthroplasty Care. J Arthroplast. 2021;36:2729–2733. doi: 10.1016/j.arth.2021.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Auais M, Al-Zoubi F, Matheson A, Brown K, Magaziner J, French SD. Understanding the role of social factors in recovery after hip fractures: A structured scoping review. Health Soc Care Community. 2019;27:1375–1387. doi: 10.1111/hsc.12830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schold JD, King KL, Husain SA, Poggio ED, Buccini LD, Mohan S. COVID-19 mortality among kidney transplant candidates is strongly associated with social determinants of health. Am J Transplant. 2021;21:2563–2572. doi: 10.1111/ajt.16578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yap ZL, Summers SJ, Grant AR, Moseley GL, Karran EL. The role of the social determinants of health in outcomes of surgery for low back pain: a systematic review and narrative synthesis. Spine J. 2022;22:793–809. doi: 10.1016/j.spinee.2021.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Karran EL, Grant AR, Moseley GL. Low back pain and the social determinants of health: a systematic review and narrative synthesis. Pain. 2020;161:2476–2493. doi: 10.1097/j.pain.0000000000001944. [DOI] [PubMed] [Google Scholar]
- 21.Zajacova A, Lawrence EM. The Relationship Between Education and Health: Reducing Disparities Through a Contextual Approach. Annu Rev Public Health. 2018;39:273–289. doi: 10.1146/annurev-publhealth-031816-044628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.•• Roy B, Kiefe CI, Jacobs DR, Goff DC, Lloyd-Jones D, Shikany JM, et al. Education, Race/Ethnicity, and Causes of Premature Mortality Among Middle-Aged Adults in 4 US Urban Communities: Results From CARDIA, 1985–2017. Am J Public Health. 2020;110:530–6 Study analyzes the effect of education on life expectancy with every year of education adding 1.37 years of life. [DOI] [PMC free article] [PubMed]
- 23.• Macki M, Hamilton T, Lim S, Telemi E, Bazydlo M, Nerenz DR, et al. Disparities in outcomes after spine surgery: a Michigan Spine Surgery Improvement Collaborative study. J Neurosurg Spine. 2021:1–9 Study analyzed large database and found some college experience had a statically significant effect on ODI. [DOI] [PubMed]
- 24.Hung M, Saltzman CL, Kendall R, Bounsanga J, Voss MW, Lawrence B, Spiker R, Brodke D. What Are the MCIDs for PROMIS, NDI, and ODI Instruments Among Patients With Spinal Conditions? Clin Orthop Relat Res. 2018;476:2027–2036. doi: 10.1097/CORR.0000000000000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asher AL, Devin CJ, Archer KR, Chotai S, Parker SL, Bydon M, Nian H, Harrell FE, Speroff T, Dittus RS, Philips SE, Shaffrey CI, Foley KT, McGirt MJ. An analysis from the Quality Outcomes Database, Part 2. Predictive model for return to work after elective surgery for lumbar degenerative disease. J Neurosurg Spine. 2017;27:370–381. doi: 10.3171/2016.8.SPINE16527. [DOI] [PubMed] [Google Scholar]
- 26.Zieger M, Luppa M, Meisel HJ, Günther L, Winkler D, Toussaint R, Stengler K, Angermeyer MC, König HH, Riedel-Heller SG. The Impact of Psychiatric Comorbidity on the Return to Work in Patients Undergoing Herniated Disc Surgery. J Occup Rehabil. 2011;21:54–65. doi: 10.1007/s10926-010-9257-1. [DOI] [PubMed] [Google Scholar]
- 27.Elsayed GA, Dupépé EB, Erwood MS, Davis MC, McClugage SG, Szerlip P, et al. Education level as a prognostic indicator at 12 months following decompression surgery for symptomatic lumbar spinal stenosis. J Neurosurg Spine. 2019;30:60–68. doi: 10.3171/2018.6.SPINE18226. [DOI] [PubMed] [Google Scholar]
- 28.Cobo Soriano J, Sendino Revuelta M, Fabregate Fuente M, Cimarra Díaz I, Martínez Ureña P, Deglané Meneses R. Predictors of outcome after decompressive lumbar surgery and instrumented posterolateral fusion. Eur Spine J. 2010;19:1841–1848. doi: 10.1007/s00586-010-1284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gelalis ID, Papanastasiou EI, Pakos EE, Ploumis A, Papadopoulos D, Mantzari M, Gkiatas IS, Vekris MD, Korompilias AV. Clinical outcomes after lumbar spine microdiscectomy: a 5-year follow-up prospective study in 100 patients. Eur J Orthop Surg Traumatol. 2019;29:321–327. doi: 10.1007/s00590-018-2359-8. [DOI] [PubMed] [Google Scholar]
- 30.Iderberg H, Willers C, Borgström F, Hedlund R, Hägg O, Möller H, Ornstein E, Sandén B, Stalberg H, Torevall-Larsson H, Tullberg T, Fritzell P. Predicting clinical outcome and length of sick leave after surgery for lumbar spinal stenosis in Sweden: a multi-register evaluation. Eur Spine J. 2019;28:1423–1432. doi: 10.1007/s00586-018-5842-3. [DOI] [PubMed] [Google Scholar]
- 31.Kim H-J, Kim S-C, Kang K-T, Chang B-S, Lee C-K, Yeom JS. Influence of Educational Attainment on Pain Intensity and Disability in Patients With Lumbar Spinal Stenosis. Spine (Phila Pa 1976) 2014;39:E637–E644. doi: 10.1097/BRS.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 32.Furunes H, Hellum C, Brox JI, Rossvoll I, Espeland A, Berg L, Brøgger HM, Småstuen MC, Storheim K. Lumbar total disc replacement: predictors for long-term outcome. Eur Spine J. 2018;27:709–718. doi: 10.1007/s00586-017-5375-1. [DOI] [PubMed] [Google Scholar]
- 33.Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, Fat DM, Boerma T, Temmerman M, Mathers C, Say L, United Nations Maternal Mortality Estimation Inter-Agency Group collaborators and technical advisory group Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387:462–474. doi: 10.1016/S0140-6736(15)00838-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hug L, You D, Blencowe H, Mishra A, Wang Z, Fix MJ, Wakefield J, Moran AC, Gaigbe-Togbe V, Suzuki E, Blau DM, Cousens S, Creanga A, Croft T, Hill K, Joseph KS, Maswime S, McClure E, Pattinson R, Pedersen J, Smith LK, Zeitlin J, Alkema L, UN Inter-agency Group for Child Mortality Estimation and its Core Stillbirth Estimation Group Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: a systematic assessment. Lancet. 2021;398:772–785. doi: 10.1016/S0140-6736(21)01112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fink G, Günther I, Hill K. Slum Residence and Child Health in Developing Countries. Demography. 2014;51:1175–1197. doi: 10.1007/s13524-014-0302-0. [DOI] [PubMed] [Google Scholar]
- 36.United Nations, Department of Economic and Social Affairs, Population Division . World Urbanization Prospects: The 2018 Revision (ST/ESA/SER.A/420) New York: United Nations; 2019. [Google Scholar]
- 37.Magalhães APT d F, Pina M d FRP d, Ramos E d CP. The Role of Urban Environment, Social and Health Determinants in the Tracking of Leisure-Time Physical Activity Throughout Adolescence. J Adolesc Health. 2017;60:100–106. doi: 10.1016/j.jadohealth.2016.08.015. [DOI] [PubMed] [Google Scholar]
- 38.Schulz A, Northridge ME. Social Determinants of Health: Implications for Environmental Health Promotion. Health Educ Behav. 2004;31:455–471. doi: 10.1177/1090198104265598. [DOI] [PubMed] [Google Scholar]
- 39.Angevine PD, Arons RR, McCormick PC. National and Regional Rates and Variation of Cervical Discectomy With and Without Anterior Fusion, 1990–1999. Spine (Phila Pa 1976) 2003;28:931–939. doi: 10.1097/01.BRS.0000058880.89444.A9. [DOI] [PubMed] [Google Scholar]
- 40.Wang MC, Kreuter W, Wolfla CE, Maiman DJ, Deyo RA. Trends and Variations in Cervical Spine Surgery in the United States. Spine (Phila Pa 1976) 2009;34:955–961. doi: 10.1097/BRS.0b013e31819e2fd5. [DOI] [PubMed] [Google Scholar]
- 41.Pannell WC, Savin DD, Scott TP, Wang JC, Daubs MD. Trends in the surgical treatment of lumbar spine disease in the United States. Spine J. 2015;15:1719–1727. doi: 10.1016/j.spinee.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 42.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ Trends and Regional Variations in Lumbar Spine Surgery: 1992–2003. Spine (Phila Pa 1976) 2006;31:2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Francis ML. Rural-Urban Differences in Surgical Procedures for Medicare Beneficiaries. Arch Surg. 2011;146:579–583. doi: 10.1001/archsurg.2010.306. [DOI] [PubMed] [Google Scholar]
- 44.•• Kim S, Ryoo JS, Ostrov PB, Reddy AK, Behbahani M, Mehta AI. Disparities in Rates of Fusions in Lumbar Disc Pathologies. Global Spine Journal. 2022;12:278–88 Study includes a large cohort which demonstrates rural populations more likely to undergo lumbar decompression compared to urban locations. [DOI] [PMC free article] [PubMed]
- 45.Huang M, Buchholz A, Goyal A, Bisson E, Ghogawala Z, Potts E, Knightly J, Coric D, Asher A, Foley K, Mummaneni PV, Park P, Shaffrey M, Fu KM, Slotkin J, Glassman S, Bydon M, Wang M. Impact of surgeon and hospital factors on surgical decision-making for grade 1 degenerative lumbar spondylolisthesis: a Quality Outcomes Database analysis. J Neurosurg Spine. 2021;34:768–778. doi: 10.3171/2020.8.SPINE201015. [DOI] [PubMed] [Google Scholar]
- 46.Adogwa O, Davison MA, Vuong V, Desai SA, Lilly DT, Moreno J, et al. Sex Differences in Opioid Use in Patients With Symptomatic Lumbar Stenosis or Spondylolisthesis Undergoing Lumbar Decompression and Fusion. Spine (Phila Pa 1976) 2019;44:E800–E807. doi: 10.1097/BRS.0000000000002965. [DOI] [PubMed] [Google Scholar]
- 47.Kha ST, Scheman J, Davin S, Benzel EC. The Impact of Preoperative Chronic Opioid Therapy in Patients Undergoing Decompression Laminectomy of the Lumbar Spine. Spine (Phila Pa 1976) 2020;45:438–443. doi: 10.1097/BRS.0000000000003297. [DOI] [PubMed] [Google Scholar]
- 48.Berkman RA, Wright AH, Sivaganesan A. Opioid-free spine surgery: a prospective study of 244 consecutive cases by a single surgeon. Spine J. 2020;20:1176–1183. doi: 10.1016/j.spinee.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 49.Sharma M, Ugiliweneza B, Aljuboori Z, Nuño MA, Drazin D, Boakye M. Factors predicting opioid dependence in patients undergoing surgery for degenerative spondylolisthesis: analysis from the MarketScan databases. J Neurosurg Spine. 2018;29:271–278. doi: 10.3171/2018.1.SPINE171258. [DOI] [PubMed] [Google Scholar]
- 50.Goyal A, Payne S, Sangaralingham LR, Jeffery MM, Naessens JM, Gazelka HM, Habermann EB, Krauss W, Spinner RJ, Bydon M. Incidence and risk factors for prolonged postoperative opioid use following lumbar spine surgery: a cohort study. J Neurosurg Spine. 2021:1–9. [DOI] [PubMed]
- 51.Ge DH, Hockley A, Vasquez-Montes D, Moawad MA, Passias PG, Errico TJ, et al. Total Inpatient Morphine Milligram Equivalents Can Predict Long-term Opioid Use After Transforaminal Lumbar Interbody Fusion. Spine (Phila Pa 1976) 2019;44:1465–1470. doi: 10.1097/BRS.0000000000003106. [DOI] [PubMed] [Google Scholar]
- 52.Schoenfeld AJ, Belmont PJ, Blucher JA, Jiang W, Chaudhary MA, Koehlmoos T, Kang JD, Haider AH. Sustained Preoperative Opioid Use Is a Predictor of Continued Use Following Spine Surgery. J Bone Joint Surg. 2018;100:914–921. doi: 10.2106/JBJS.17.00862. [DOI] [PubMed] [Google Scholar]
- 53.Berg J, Wahood W, Zreik J, Yolcu YU, Alvi MA, Jeffery M, Bydon M. Economic Burden of Hospitalizations Associated with Opioid Dependence Among Patients Undergoing Spinal Fusion. World Neurosurgery. 2021;151:e738–e746. doi: 10.1016/j.wneu.2021.04.116. [DOI] [PubMed] [Google Scholar]
- 54.O’Donnell JA, Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, et al. Preoperative Opioid Use is a Predictor of Poor Return to Work in Workers’ Compensation Patients After Lumbar Diskectomy. Spine (Phila Pa 1976) 2018;43:594–602. doi: 10.1097/BRS.0000000000002385. [DOI] [PubMed] [Google Scholar]
- 55.Tye EY, Anderson JT, Faour M, Haas AR, Percy R, Woods ST, et al. Prolonged Preoperative Opioid Therapy in Patients With Degenerative Lumbar Stenosis in a Workers’ Compensation Setting. Spine (Phila Pa 1976) 2017;42:E1140–E1146. doi: 10.1097/BRS.0000000000002112. [DOI] [PubMed] [Google Scholar]
- 56.Adogwa O, Davison MA, Vuong VD, Desai SA, Lilly DT, Moreno J, Cheng J, Bagley C. Regional Variation in Opioid Use After Lumbar Spine Surgery. World Neurosurgery. 2019;121:e691–e699. doi: 10.1016/j.wneu.2018.09.192. [DOI] [PubMed] [Google Scholar]
- 57.Massie L, Gunaseelan V, Waljee J, Brummett C, Schwalb JM. Relationship between initial opioid prescription size and likelihood of refill after spine surgery. Spine J. 2021;21:772–778. doi: 10.1016/j.spinee.2021.01.016. [DOI] [PubMed] [Google Scholar]
- 58.Harris AB, Marrache M, Jami M, Raad M, Puvanesarajah V, Hassanzadeh H, Lee SH, Skolasky R, Bicket M, Jain A. Chronic opioid use following anterior cervical discectomy and fusion surgery for degenerative cervical pathology. Spine J. 2020;20:78–86. doi: 10.1016/j.spinee.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 59.Reyes AA, Canseco JA, Mangan JJ, Divi SN, Goyal DKC, Bowles DR, et al. Risk Factors for Prolonged Opioid Use and Effects of Opioid Tolerance on Clinical Outcomes After Anterior Cervical Discectomy and Fusion Surgery. Spine (Phila Pa 1976) 2020;45:968–975. doi: 10.1097/BRS.0000000000003511. [DOI] [PubMed] [Google Scholar]
- 60.Kalakoti P, Volkmar AJ, Bedard NA, Eisenberg JM, Hendrickson NR, Pugely AJ. Preoperative Chronic Opioid Therapy Negatively Impacts Long-term Outcomes Following Cervical Fusion Surgery. Spine (Phila Pa 1976) 2019;44:1279–1286. doi: 10.1097/BRS.0000000000003064. [DOI] [PubMed] [Google Scholar]
- 61.Dworkin ER, Menon SV, Bystrynski J, Allen NE. Sexual assault victimization and psychopathology: A review and meta-analysis. Clin Psychol Rev. 2017;56:65–81. doi: 10.1016/j.cpr.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Levallois P, Barn P, Valcke M, Gauvin D, Kosatsky T. Public Health Consequences of Lead in Drinking Water. Curr Environ Health Rep. 2018;5:255–262. doi: 10.1007/s40572-018-0193-0. [DOI] [PubMed] [Google Scholar]
- 63.Lie A, Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby K-C, Engdahl B, Tambs K. Occupational noise exposure and hearing: a systematic review. Int Arch Occup Environ Health. 2016;89:351–372. doi: 10.1007/s00420-015-1083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The Long-Term Health Consequences of Child Physical Abuse, Emotional Abuse, and Neglect: A Systematic Review and Meta-Analysis. PLoS Med. 2012;9:e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Novak Babič M, Gostinčar C, Gunde-Cimerman N. Microorganisms populating the water-related indoor biome. Appl Microbiol Biotechnol. 2020;104:6443–6462. doi: 10.1007/s00253-020-10719-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Orru H, Ebi KL, Forsberg B. The Interplay of Climate Change and Air Pollution on Health. Curr Environ Health Rep. 2017;4:504–513. doi: 10.1007/s40572-017-0168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Satyanarayana VA, Chandra PS, Vaddiparti K. Mental health consequences of violence against women and girls. Curr Opin Psychiatry. 2015;28:350–356. doi: 10.1097/YCO.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 68.Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21:667–669. doi: 10.1111/j.1525-1497.2006.0512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kalantar-Zadeh K, Kovesdy CP, Derose SF, Horwich TB, Fonarow GC. Racial and survival paradoxes in chronic kidney disease. Nat Clin Pract Nephrol. 2007;3:493–506. doi: 10.1038/ncpneph0570. [DOI] [PubMed] [Google Scholar]
- 70.Rymer JA, Li S, Pun PH, Thomas L, Wang TY. Racial Disparities in Invasive Management for Patients With Acute Myocardial Infarction With Chronic Kidney Disease. Circ Cardiovasc Interv. 2022;15:e011171. doi: 10.1161/CIRCINTERVENTIONS.121.011171. [DOI] [PubMed] [Google Scholar]
- 71.Clark-Cutaia MN, Rivera E, Iroegbu C, Squires A. Disparities in chronic kidney disease-the state of the evidence. Curr Opin Nephrol Hypertens. 2021;30:208–214. doi: 10.1097/MNH.0000000000000688. [DOI] [PubMed] [Google Scholar]
- 72.Crews DC, Pfaff T, Powe NR. Socioeconomic Factors and Racial Disparities in Kidney Disease Outcomes. Semin Nephrol. 2013;33:468–475. doi: 10.1016/j.semnephrol.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 73.Karnati SA, Wee A, Shirke MM, Harky A. Racial disparities and cardiovascular disease: One size fits all approach? J Card Surg. 2020;35:3530–3538. doi: 10.1111/jocs.15047. [DOI] [PubMed] [Google Scholar]
- 74.Warren CM, Turner PJ, Chinthrajah RS, Gupta RS. Advancing Food Allergy Through Epidemiology: Understanding and Addressing Disparities in Food Allergy Management and Outcomes. J Allergy Clin Immunol Pract. 2021;9:110–118. doi: 10.1016/j.jaip.2020.09.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Infant mortality. Centers for Disease Control and Prevention. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm. Published September 8, 2021. Accessed January 3, 2022. .
- 76.Khan IS, Huang E, Maeder-York W, Yen RW, Simmons NE, Ball PA, Ryken TC. Racial Disparities in Outcomes After Spine Surgery: A Systematic Review and Meta-Analysis. World Neurosurgery. 2022;157:e232–e244. doi: 10.1016/j.wneu.2021.09.140. [DOI] [PubMed] [Google Scholar]
- 77.Martin JR, Wang TY, Loriaux D, Desai R, Kuchibhatla M, Karikari IO, Bagley CA, Gottfried ON. Race as a predictor of postoperative hospital readmission after spine surgery. J Clin Neurosci. 2017;46:21–25. doi: 10.1016/j.jocn.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 78.Schoenfeld AJ, Tipirneni R, Nelson JH, Carpenter JE, Iwashyna TJ. The Influence of Race and Ethnicity on Complications and Mortality After Orthopedic Surgery. Med Care. 2014;52:842–851. doi: 10.1097/MLR.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 79.Skolasky RL, Thorpe RJ, Wegener ST, Riley LH. Complications and Mortality in Cervical Spine Surgery. Spine (Phila Pa 1976) 2014;39:1506–1512. doi: 10.1097/BRS.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 80.Elsamadicy AA, Kemeny H, Adogwa O, Sankey EW, Goodwin CR, Yarbrough CK, Lad SP, Karikari IO, Gottfried ON. Influence of racial disparities on patient-reported satisfaction and short- and long-term perception of health status after elective lumbar spine surgery. J Neurosurg Spine. 2018;29:40–45. doi: 10.3171/2017.12.SPINE171079. [DOI] [PubMed] [Google Scholar]
- 81.Reyes AM, Katz JN, Schoenfeld AJ, Kang JD, Losina E, Chang Y. National utilization and inpatient safety measures of lumbar spinal fusion methods by race/ethnicity. Spine J. 2021;21:785–794. doi: 10.1016/j.spinee.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim S, Ryoo JS, Ostrov PB, Reddy AK, Behbahani M, Mehta AI. Disparities in Rates of Fusions in Lumbar Disc Pathologies. Global Spine J. 2022;12:278–288. doi: 10.1177/2192568220951137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Elsamadicy A, Adogwa O, Reiser E, Fatemi P, Cheng J, Bagley C. The Effect of Patient Race on Extent of Functional Improvement After Cervical Spine Surgery. SPINE. 2016;41:822–826. doi: 10.1097/BRS.0000000000001346. [DOI] [PubMed] [Google Scholar]
- 84.Wang KY, Puvanesarajah V, Xu A, Zhang B, Raad M, Hassanzadeh H, et al. Growing Racial Disparities in the Utilization of Adult Spinal Deformity Surgery. Spine (Phila Pa 1976) 2022;47:E283–E289. doi: 10.1097/BRS.0000000000004180. [DOI] [PubMed] [Google Scholar]
- 85.Bureau USC. Health insurance coverage in the United States: 2020. Census.gov. https://www.census.gov/library/publications/2021/demo/p60-274.html. Published October 18, 2021. Accessed January 3, 2022.
- 86.Differences between Medicare and Medicaid. Medicare Interactive. https://www.medicareinteractive.org/get-answers/medicare-basics/medicare-coverage-overview/differences-between-medicare-and-medicaid. Published January 13, 2022. Accessed January 15, 2022.
- 87.Health Care Access and Quality. Health Care Access and Quality - Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-care-access-and-quality. Accessed January 3, 2022.
- 88.Tanenbaum JE, Miller JA, Alentado VJ, Lubelski D, Rosenbaum BP, Benzel EC, Mroz TE. Insurance status and reportable quality metrics in the cervical spine fusion population. Spine J. 2017;17:62–69. doi: 10.1016/j.spinee.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tanenbaum JE, Alentado VJ, Miller JA, Lubelski D, Benzel EC, Mroz TE. Association between insurance status and patient safety in the lumbar spine fusion population. Spine J. 2017;17:338–345. doi: 10.1016/j.spinee.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.• Rasouli JJ, Neifert SN, Gal JS, Snyder DJ, Deutsch BC, Steinberger J, et al. Disparities in Outcomes by Insurance Payer Groups for Patients Undergoing Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976). 2020;45:770–5 Study supports literature regarding Medicaid users are higher risk of postoperative complications. [DOI] [PubMed]
- 91.Bhandarkar AR, Alvi MA, Naessens JM, Bydon M. Disparities in inpatient costs and outcomes after elective anterior cervical discectomy and fusion at safety-net hospitals. Clin Neurol Neurosurg. 2020;198:106223. doi: 10.1016/j.clineuro.2020.106223. [DOI] [PubMed] [Google Scholar]
- 92.Orhurhu V, Agudile E, Chu R, Urits I, Orhurhu MS, Viswanath O, Ohuabunwa E, Simopoulos T, Hirsch J, Gill J. Socioeconomic disparities in the utilization of spine augmentation for patients with osteoporotic fractures: an analysis of National Inpatient Sample from 2011 to 2015. Spine J. 2020;20:547–555. doi: 10.1016/j.spinee.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 93.Lad SP, Huang KT, Bagley JH, Hazzard MA, Babu R, Owens TR, et al. Disparities in the Outcomes of Lumbar Spinal Stenosis Surgery Based on Insurance Status. Spine (Phila Pa 1976) 2013;38:1119–1127. doi: 10.1097/BRS.0b013e318287f04e. [DOI] [PubMed] [Google Scholar]
- 94.Elsayed G, McClugage SG, Erwood MS, Davis MC, Dupépé EB, Szerlip P, et al. Association between payer status and patient-reported outcomes in adult patients with lumbar spinal stenosis treated with decompression surgery. J Neurosurg Spine. 2019;30:198–210. doi: 10.3171/2018.7.SPINE18294. [DOI] [PubMed] [Google Scholar]
- 95.Economic stability. Economic Stability - Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/browse-objectives/economic-stability. Accessed January 3, 2022.
- 96.Jackson SL, Yang EC, Zhang Z. Income Disparities and Cardiovascular Risk Factors Among Adolescents. Pediatrics. 2018;142. [DOI] [PMC free article] [PubMed]
- 97.Khan I, Bydon M, Archer KR, Sivaganesan A, Asher AM, Alvi MA, Kerezoudis P, Knightly JJ, Foley KT, Bisson EF, Shaffrey C, Asher AL, Spengler DM, Devin CJ. Impact of occupational characteristics on return to work for employed patients after elective lumbar spine surgery. Spine J. 2019;19:1969–1976. doi: 10.1016/j.spinee.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 98.Closing the gap in a generation: health equity through action on the social determinants of health - Final report of the commission on social determinants of health. 2008 [DOI] [PubMed]
- 99.Drake C, Lian T, Trogdon JG, Edelman D, Eisenson H, Weinberger M, Reiter K, Shea CM. Evaluating the association of social needs assessment data with cardiometabolic health status in a federally qualified community health center patient population. BMC Cardiovasc Disord. 2021;21:342. doi: 10.1186/s12872-021-02149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kangovi S, Mitra N, Norton L, Harte R, Zhao X, Carter T, Grande D, Long JA. Effect of Community Health Worker Support on Clinical Outcomes of Low-Income Patients Across Primary Care Facilities: A Randomized Clinical Trial. JAMA Intern Med. 2018;178:1635–1643. doi: 10.1001/jamainternmed.2018.4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
N/A