Abstract
Acquired benign trachea-oesophageal fistula is a rare benign pathological entity with varying aetiologies that most often occurs post-intubation. This case report presents the case of a female patient, 31 years old, admitted to the emergency room with sepsis syndrome following bilateral aspiration pneumonia caused by a large trachea-oesophageal fistula. The fistula was the result of intra-tracheal migration of an oesophageal stent placed for post lye ingestion stenosis. Esophageal diversion and partial resection with oesophageal patch to repair the tracheal defect, under general anaesthesia with ventilation using rigid bronchoscopy and high frequency jet ventilation (HFJV), followed at a later date by esophageal replacement with colic graft were the procedures performed with a view to curing the patient. In conclusion, complex cases always require a tailored approach. It is important to note that HFJV may be applied for a longer period of time and the oesophagus can be used as patch for the posterior tracheal wall in selected cases. Staged surgery is also an option when the patients' poor health status does not permit major surgery.
Keywords: trachea-esophageal fistula, esophageal stenting, high frequency jet ventilation, acquired fistula, lye ingestion, stenosis
Introduction
Acquired benign trachea-oesophageal fistula is a rare pathological entity that concerns the occurrence of an abnormal connection between the oesophagus and the trachea that does not involve the presence of local neoplastic pathology (1). This fistula is common in patients that were mechanically ventilated for longer periods of time during which, most often, the hyperinflated cuff of the endotracheal or tracheostomy tube is in contact with a nasogastric tube placed in the oesophagus (1). Other causes for this type of fistula are rare, but regardless of the aetiology, the treatment is rather the same, aimed at closing the tracheoesophageal connection and restoring the separate permeability of the airways and digestive tube so as to avoid pulmonary contamination and aspiration pneumonia (2). Certain cases required a tailored approach, e.g. patients with complex local and pathological issues, patients regarding whom we should try to ‘think outside the box’; a rich experience in tracheal and oesophageal surgery is always conducive to obtaining good results. Using an oesophageal patch for the posterior tracheal wall, staged surgery and extending the duration of high frequency jet ventilation (HFJV) anaesthesia are among the strategies used in order to successfully treat the case presented below.
Case report
A 31-year old female patient was admitted to the Department of Thoracic Surgery, ‘Marius Nasta’ National Institute of Pneumology (Bucharest, Romania) with quasi-complete dysphagia, severe cough exacerbated with deglutition, purulent sputum and fever, namely symptoms that began ~1 week before and got worse in time.
The patient's history is relevant, as she was known to have cicatricial oesophageal stenosis after accidentally ingesting lye ~10 years ago. At the time, she received conservative treatment, with the patient only requiring regular oesophageal dilatations approximately once a year in the first 6 years. Subsequently, as the stenosis relapsed more often and extended on longer stretches of the oesophagus, the dilatation treatment had come to be needed 3-4 times per year, so 2 years prior to this admission, the decision was made to insert an oesophageal stent.
It is important to note that the surgical option (oesophageal plasty) was also offered to the patient, who refused such treatment. The first fully covered metallic expandable stent inserted was kept in place for ~2 months before it was removed, following which the oesophagus restenosis (~3 months), another similar, but longer stent was placed in the oesophagus. This procedure was repeated four times. The last time, during the same digestive endoscopy, the patient was also subject to percutaneous gastrostomy; we do not know the actual reason for this procedure, but it suggests that the gastroenterologist performing this procedure was clearly unsatisfied with the results. This last manoeuvre was performed 2 weeks before the symptoms started and 3 weeks before the patient was admitted to our clinic.
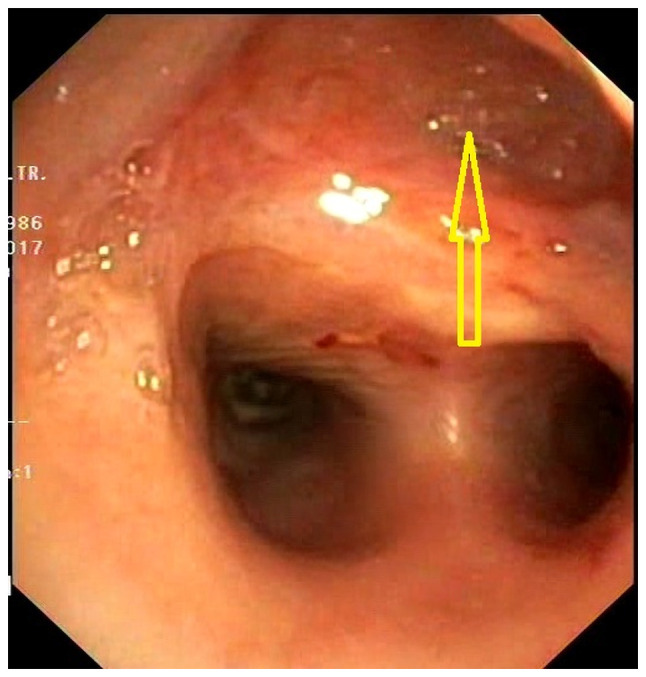
When she arrived, the patient was septic (fever and cough with mucopurulent expectoration) and severely dehydrated, and had been unable to properly swallow for several days. The imagistic tests showed bilateral lung lesions (aspiration pneumonia), and the additional bronchoscopy exam indicated a tracheoesophageal fistula right above the carina, ~2.5 cm long, with the intratracheal migration of the oesophageal stent (Fig. 1). The attempts to remove the stent through the trachea or the oesophagus failed because of its size, in the first case, and also because the proximal stenosis of the oesophagus and, when pulled, the stent would cling to the tracheal fistula. A rigorous cleaning of the trachea-bronchial tree was conducted by means of bronchoaspiration.
Figure 1.

Fibrobronchoscopy image on admission. Oesophageal stent had migrated into the trachea. Yellow arrow, oesophageal lumen; green arrow, tracheal lumen.
The first steps taken consisted of completely interrupting oral alimentation and through the gastrostomy tube-the oesophageal reflux of the gastric content through the stent would end up in the trachea, then in the lungs, and of starting total parenteral nutrition. Measures were taken to correct the acid-base and hydroelectrolyte balances, which were severely imbalanced; broad spectrum antibiotics were administered to control the sepsis. Practically, this first step was intended to simply improve the health condition and reduce the effects of post-sepsis syndrome with a view to conducting a surgery that would resolve the connection between the airway and the digestive tube.
Following discussions about the case, it was decided that oesophagectomy was the surgical option at the time. Also, given the poor health status of the patient (BMI, 13.6; height, 165 cm; weight, 37 kg) who was also suffering from hypoproteinemia and 6 kg weight loss in the few weeks prior to admission (a significant percentage) it was decided that the oesophagoplasty would be performed at a later time, once the nutritional status of the patient had improved.
Surgery was performed under general and epidural anaesthesia while the patient was ventilated in a rather unconventional manner; she was intubated using a rigid bronchoscope and the ventilation on separate areas was performed with HFJV associated with a bronchial blocker.
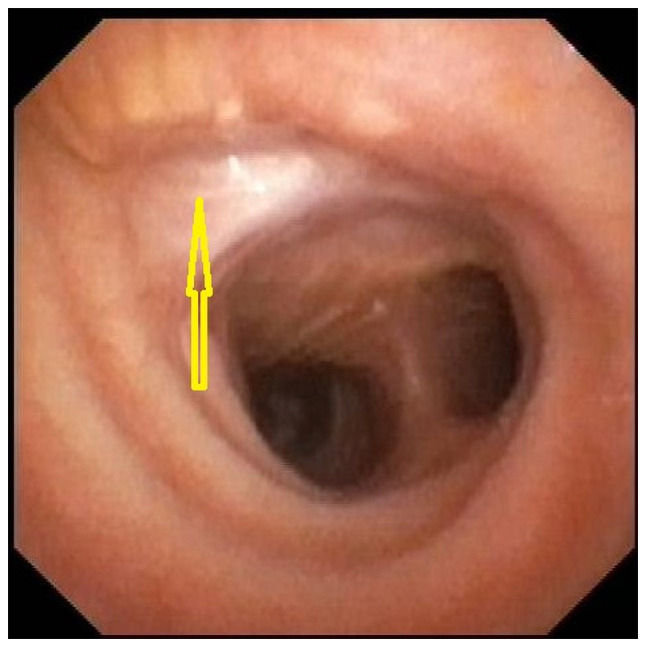
A standard posterolateral thoracotomy was used to gain access to the right pleural cavity. First, an oesophagectomy was performed to remove the bulky oesophageal stent that interfered with the dissection. Prior to the surgery, the initial intent was to conduct a total oesophagectomy and a standard lower tracheal anastomosis resection. The peritracheal fibrosis and the very tight existing adhesions turned the surgery into a partial oesophagectomy, distal and proximal to the fistulous opening. Practically, an ~4-cm long oesophagus fragment was left stuck to the posterior trachea next to the fistulous opening, forming a sort of tracheal diverticulum (Fig. 2). A cervical esophagostomy completed the surgery.
Figure 2.
Fibrobronchoscopy image immediately post-operation. Yellow arrow, posterior tracheal pseudodiverticulum (oesophageal patch).
The post-operative recovery was simple, the patient was discharged on day 10 after surgery, with resolving aspiration pneumonia and the inflammatory sepsis syndrome under control once the lung contamination was stopped. It was jointly agreed that, for ~3 months, food should be administered through the existing gastrostomy, while the patient was put on a nutritional and respiratory recovery program before the oesophageal reconstruction.
According to the agreement, after the set period, the patient was admitted in order to restore the digestive tube continuity. On admission, the nutritional status had improved (5 kg weight gain), and the patient did not show hypoproteinemia; the bilateral aspiration pneumonia was fully resolved during the recovery period. Since the patient was young, with a benign pathology, the oesophageal reconstruction was conducted with an iso-peristaltic colonic loop vascularized on the middle colic pedicle, with the graft in retrosternal position. The surgery was successful, with standard post-operative recovery and discharge 10 days after surgery; this time, the patient was able to feed normally.
The images and bronchoscopy tests showed a reduction to almost disappearance of the tracheal pseudo-diverticulum, with complete scarring of the posterior side of the trachea (Fig. 3, Fig. 4 and Fig. 5). Three years after surgery, the patient is in good health and has reintegrated socio-professionally, with only minor feeding issues, which are somehow normal in a patient with oesophageal plasty.
Figure 3.
Fibrobronchoscopy image at the late post-operative stage. The posterior tracheal pseudodiverticulum had almost disappeared, as shown by the yellow arrow.
Figure 4.

Computerized tomography scan image at the late post-operative stage. The posterior tracheal pseudodiverticulum had almost disappeared, as shown by the arrow.
Figure 5.
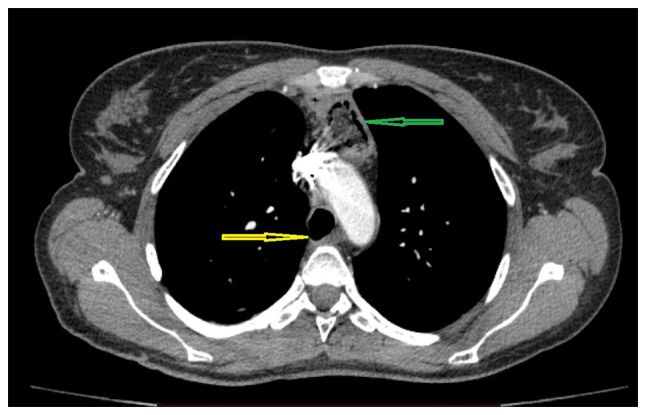
Computed tomography scanning image at the late post-operative stage demonstrating the presence of the retrosternal colic graft. The posterior tracheal pseudodiverticulum had almost disappeared, as indicated by the yellow arrow. Retrosternal colic graft is indicated by the green arrow.
Discussion
Several aspects should be discussed in this case. Post lye ingestion oesophageal stenoses are rather rare injuries and it cannot be said there is an ideal or even standardized treatment strategy. It depends on numerous factors, such as injury size (meaning the length of the oesophagus that was affected), organs involved (stenosis of the pharynx and stomach or laryngeal problems may be associated), time since the initial injury (knowing that it is an evolving condition) and type of ingested substance (2). Thus, the management of post lye ingestion oesophageal stenoses must be individualized to consider all these factors, so it is more complex than it may look at first glance.
Evidently, oesophageal resection surgery as the first procedure is no longer an option without the acute post-ingestion perforation; endoscopic follow-up with repetitive dilatation is feasible as long as the need and frequency of the procedures do not severely impair the patient's quality of life. Inserting oesophageal stents may also be an option in certain conditions, but keeping them in place long-term is not recommended, as their presence may lead to complications, the most severe ones being, just like we had in this case, the formation of fistulas, particularly with the airway, but also with other intra-thoracic organs (3-5).
Regarding the general anaesthesia that the patient underwent for the first surgery, the airway could only be secured by using a rigid bronchoscope as inserting a double-lumen tube was impossible because the stent almost completely blocked the tracheal lumen and could not be mobilized through flexible bronchoscopy since it was encroached in the fistula opening. As ventilation on separate areas is advisable in chest surgery, it was performed using a bronchial blocker introduced through the rigid bronchoscope in the right main bronchus.
The HFJV allowed for the ventilation of the left lung during surgery, the total duration of the ventilation being 4 h. There is no time limit for using this type of ventilation, but there is a risk of developing hypercapnia, a risk that increases with the duration. Hypercapnia is caused by certain risk factors, such as obesity and bronchospasm, which were absent in our patient, as well as by ventilation parameters, specifically those that are flow-related, which should be large enough to ‘wash’ CO2 (6). The patient showed no hypercapnia at any moment during the 4 h of surgery and the blood gases were monitored every 30 min using an arterial catheter. Our department's extensive experience in tracheal surgery enabled us to do all these technical methods (6-8), the anaesthesia posed no distinct problems, even though the long duration of the HFJV was unusual.
The partial oesophagectomy above and below the fistula was not a technical first as we have performed this type of surgery on other occasions too, but this was usually when the fistula had extreme sizes that would not allow for the tracheal resection, practically turning the oesophagus into a posterior wall of the trachea; this procedure has also been successfully described by other teams (1,9,10). This was not our initial plan, but during the surgery, the fibrosis found was extremely severe, not allowing for the safe dissection of the oesophagus from the trachea. It is important to note that the severity of the adhesions is linked to the repetitive dilatation treatment and repetitive stenting rather than the lye injury itself because oesophagectomies for lye stenoses have been performed before in the clinic, but the peri-oesophageal adhesions have not been comparable in severity.
There is great variability of practice worldwide when it comes to oesophageal resection and reconstruction (11). Resections are mostly performed for oesophageal malignancies and very rarely for benign diseases. Most procedures performed are minimally invasive and we are aware of the benefits brought by such a surgical approach (12). The stomach is commonly used as the organ for oesophagoplasty and the surgery is performed in one go. In our case, the open approach was used in order to associate a potential lower tracheal resection, but even without it, performing the partial oesophagectomy through a minimally invasive procedure under the given circumstances, with extended fibrosis and very tight adhesions, would have likely been extremely difficult.
At present, staged surgery, namely performing resection and interval oesophageal reconstruction is very rarely considered. The patient's poor health and the fact that we planned to perform the oesophageal reconstructions using the colon, which meant a more laborious procedure than the usual one where the reconstruction is performed with the stomach, steered us towards this decision. Using the colon as the oesophageal substitute is an option when replacing the oesophagus for a benign disease in a young patient, in which case it is assumed the graft will be kept in place long-term.
To conclude, complex cases always require a tailored approach. This case demonstrated that ventilating a patient with HFJV for a long period of time (4 h in this case) is possible, provided that blood gases are carefully monitored to correct hypercapnia if required. Replacing the posterior tracheal wall with an oesophageal patch proved once again to be a feasible option in selected cases. Splitting the procedure into a resection stage followed by subsequent reconstruction (staged surgery) should be considered when the patient is not healthy enough to undergo serious reconstructive surgery.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
CB and IC were involved in the study conception and design, data collection and analysis and the writing of the manuscript. IB, NB and AM participated in the writing of the manuscript, data collection and data analysis. FF and CP were involved in the study design and data analysis. MA, GCa and FG were involved in data analysis. AB, GCo, IB, AM and DR were involved in study conception and design. All authors have read and approved the final manuscript. CB, IC and NB confirm the authenticity of the raw data.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of ‘Marius Nasta’ National Institute of Pneumology (approval no. 292/12.06.2020; Bucharest, Romania). Informed consent was obtained and signed by the patient on 11.06.2020.
Patient consent for publication
The patient provided written informed consent for the publication of the case details and associated images.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003;13:271–289. doi: 10.1016/s1052-3359(03)00030-9. [DOI] [PubMed] [Google Scholar]
- 2.Shu YS, Sun C, Shi WP, Shi HC, Lu SC, Wang K. Tubular stomach or whole stomach for esophagectomy through cervico-thoraco-abdominal approach: A comparative clinical study on anastomotic leakage. Ir J Med Sci. 2013;182:477–480. doi: 10.1007/s11845-013-0917-y. [DOI] [PubMed] [Google Scholar]
- 3.Bakken JC, Wong Kee Song LM, de Groen PC, Baron TH. Use of a fully covered self-expandable metal stent for the treatment of benign esophageal diseases. Gastrointest Endosc. 2010;72:712–720. doi: 10.1016/j.gie.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Farkas ZC, Pal S, Jolly GP, Lim MMD, Malik A, Malekan R. Esophagopericardial fistula and pneumopericardium from caustic ingestion and esophageal stent. Ann Thorac Surg. 2019;107:e207–e208. doi: 10.1016/j.athoracsur.2018.06.087. [DOI] [PubMed] [Google Scholar]
- 5.Aneeshkumar S, Sundararajan L, Santosham R, Palaniappan R, Dhus U. Erosion of esophageal stent into left main bronchus causing airway compromise. Lung India. 2017;34:76–78. doi: 10.4103/0970-2113.197114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cordos I, Bolca C, Paleru C, Posea R, Stoica R. Sixty tracheal resections-single center experience. Interact Cardiovasc Thorac Surg. 2009;8:62–65. doi: 10.1510/icvts.2008.184747. [DOI] [PubMed] [Google Scholar]
- 7.Couraud L, Jougon JB, Velly JF. Surgical treatment of nontumoral stenoses of the upper airway. Ann Thorac Surg. 1995;60:250–260. doi: 10.1016/0003-4975(95)00464-v. [DOI] [PubMed] [Google Scholar]
- 8.Stoica RT, Cordos I, Popescu WM. Anesthetic considerations for tracheobronchial resection in oncologic surgery. Curr Opin Anaesthesiol. 2020;33:55–63. doi: 10.1097/ACO.0000000000000821. [DOI] [PubMed] [Google Scholar]
- 9.He J, Chen M, Shao W, Wang D. Surgical management of huge tracheo-oesophageal fistula with oesophagus segment in situ as replacement of the posterior membranous wall of the trachea. Eur J Cardiothorac Surg. 2009;36:600–602. doi: 10.1016/j.ejcts.2009.05.047. [DOI] [PubMed] [Google Scholar]
- 10.de Castro G, Iribarren M, Rivo E, Meléndez R, Nóvoa E, Cañizares M, Gil P. Tracheoesophageal fistula in an intubated patient. Treatment through exclusion and esophageal patch. Cir Esp. 2005;77:230–232. doi: 10.1016/s0009-739x(05)70843-5. (In Spanish) [DOI] [PubMed] [Google Scholar]
- 11.Oesophago-Gastric Anastomosis Study Group on behalf of the West Midlands Research Collaborative. International variation in surgical practices in units performing oesophagectomy for oesophageal cancer: A unit survey from the oesophago-gastric anastomosis audit (OGAA) World J Surg. 2019;43:2874–2884. doi: 10.1007/s00268-019-05080-1. [DOI] [PubMed] [Google Scholar]
- 12.Erus S, Öztürk AB, Albayrak Ö, İncir S, Kapdağlı MH, Cesur EE, Yavuz Ö, Tanju S, Dilege Ş. Immune profiling after minimally invasive lobectomy. Interact Cardiovasc Thorac Surg. 2021;32:291–297. doi: 10.1093/icvts/ivaa296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


