Abstract
Background
The number of MitraClip® implantations increased significantly in recent years. Data regarding the impact of weight class on survival are sparse.
Hypothesis
We hypothesized that weight class influences survival of patients treated with MitraClip® implantation.
Methods
We investigated in‐hospital, 1‐year, 3‐year, and long‐term survival of patients successfully treated with isolated MitraClip® implantation for mitral valve regurgitation (MR) (June 2010–March 2018). Patients were categorized by weight classes, and the impact of weight classes on survival was analyzed.
Results
Of 617 patients (aged 79.2 years; 47.3% females) treated with MitraClip® implantation (June 2010–March 2018), 12 patients were underweight (2.2%), 220 normal weight (40.1%), 237 overweight (43.2%), and 64 obesity class I (11.7%), 12 class II (2.2%), and 4 class III (0.7%). Preprocedural Logistic EuroScore (21.1 points [IQR 14.0–37.1]; 26.0 [18.5–38.5]; 26.0 [18.4–39.9]; 24.8 [16.8–33.8]; 33.0 [25.9–49.2]; 31.6 [13.1–47.6]; p = .291) was comparable between groups. Weight class had no impact on in‐hospital death (0.0%; 4.1%; 1.5%; 0.0%; 7.7%; 0.0%; p = .189), 1‐year survival (75.0%; 72.0%; 76.9%; 75.0%; 75.0%; 33.3%; p = .542), and 3‐year survival (40.0%; 36.8%; 38.2%; 48.6%; 20.0%; 33.3%; p = .661). Compared to normal weight, underweight (hazard ratio [HR]: 1.35 [95% confidence interval [CI]: 0.65–2.79], p = .419), obesity‐class I (HR: 0.93 [95% CI: 0.65–1.34], p = .705), class II (HR: 0.39 [95% CI: 0.12–1.24], p = .112), and class III (HR: 1.28 [95% CI: 0.32–5.21], p = .726) did not affect long‐term survival. In contrast, overweight was associated with better survival (HR: 1.32 [95% CI: 1.04–1.68], p = .023).
Conclusion
Overweight affected the long‐term survival of patients undergoing MitraClip® implantation beneficially compared to normal weight.
Keywords: edge‐to‐edge repair, MitraClip, mitral valve regurgitation, obesity, survival, transcatheter mitral valve repair
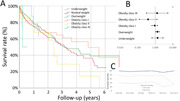
Long‐term survival stratified for weight classes illustrated by Hazard plot for patients treated with MitraClip® implantation stratified for weight classes. Association of weight class compared to normal‐weight with long‐term survival (adjusted for Logistic EuroScore). Survival rate at discharge, 1‐year follow‐up, and 3‐year follow‐up stratified for weight classes.
Abbreviations
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular diseases
- DMR
degenerative mitral valve regurgitation
- FMR
functional mitral valve regurgitation
- HR
hazard ratio
- IQR
interquartile range
- MR
mitral valve regurgitation
- OR
odds ratio
- TEER
transcatheter edge‐to‐edge repair (new term of the ACC/AHA guidelines)
- WHO
World Health Organization
1. INTRODUCTION
Mitral valve regurgitation (MR) is a common heart valve disease in the developed countries 1 , 2 , 3 , 4 accompanied by substantial morbidity and mortality. 3 , 5 , 6 , 7 , 8 , 9 , 10 , 11 The prevalence of MR increases substantially with age 9 , 10 , 12 and patients with MR are frequently referred for surgical or interventional treatment. 2 , 8 , 10 , 12 , 13 Transcatheter mitral valve repair (TMVr) using MitraClip® technique or transcatheter edge‐to‐edge repair (TEER) therapy is an established treatment for patients suffering from MR with both primary etiology, who are at high or prohibitive surgical risk, and secondary etiology in a broader range of risk classes and age groups according to current guidelines. 4 , 6 , 10 , 13 , 14 , 15 , 16 TMVr with MitraClip® implantation has been shown to reduce patients’ symptoms and to improve survival in selected patients. 16 Thus, the number of TMVr is increasing in Germany and worldwide. 6 , 10 , 11 , 13 , 14 Studies indicated that MitraClip® implantations are accompanied by low rates of adverse events. 10 , 11 , 12 However, comorbidities and patient baseline factors potentially influencing long‐term outcomes are still under investigation. Studies have suggested an obesity survival paradox in patients with cardiovascular diseases (CVDs) 17 , 18 , 19 and one recently published study reported an obesity paradox regarding in‐hospital major adverse cardiac events even in TMVR, but failed to confirm an obesity paradox for in‐hospital survival, while data for long‐term follow‐up are entirely missing. 20 Thus, the objective of the present study was to investigate the impact of nutritional status at the baseline of MitraClip® implantation on patients in short‐term outcomes, and in particular long‐term outcomes.
2. PATIENTS AND METHODS
Patients successfully treated for MR (regardless of the underlying pathomechanism, functional MR [FMR] vs. degenerative MR [DMR]) with TEER by MitraClip® implantation in our University Department for Cardiology between June 9, 2010 and March 8, 2018 were included in the present study. Those patients undergoing MitraClip® implantation simultaneously in combination with other forms of TMVr (e.g., direct or indirect mitral valve annuloplasty or chordal reconstruction as COMBO therapy), as well as patients with procedural failure (defined as failure of clip placement due to anatomical reasons or other operator‐reported reasons [e.g., resulting relevant mitral valve stenosis during grasping of the leaflets, leading to the removal of the device and aborting the procedure]), were excluded from this study. All treated patients were aged ≥18 years with moderate to high‐grade or high‐grade MR despite optimal medical treatment and cardiac resynchronization therapy—if indicated—and estimated to be at high risk for valve surgery by an interdisciplinary board (Heart Valve Team). 21
The individual risk for alternative surgical treatments was calculated with scoring systems (e.g., Logistic EuroScore I, for details and online calculator, see http://www.euroscore.org), and other individual factors such as frailty and comorbidities were taken into account. 21 All MitraClip® procedures and implantations were guided by fluoroscopy and three‐dimensional transesophageal echocardiography. Procedures were performed under general anesthesia or deep sedation. Long‐term survival or date of death, respectively, were assessed based on entries in our hospital's patients’ records, data from routine follow‐up visits, and an enquiry at the Rhineland‐Palatinate bureau of vital statistics as of March 8, 2018. 21
2.1. Study endpoint
Primary outcome was survival at the following time periods: in‐hospital stay, and 1‐year, 3‐year, and long‐term follow‐up.
2.2. Definitions
Based on current guideline recommendations, MR was quantified/categorized into four grades 22 , 23 : Grade 0 for no or trace MR, Grade I for mild, Grade II for moderate, and Grade III for severe MR. Renal insufficiency was defined as a glomerular filtration rate <60 ml/min·kg. According to the World Health Organization (WHO), underweight was categorized as body mass index (BMI) < 18.5 kg/m2, normal‐weight ranges between 18.5 and <25 kg/m2, overweight was defined as BMI ≥ 25 and <30 kg/m2, obesity class I was defined as BMI between ≥30 and <35kg/m2, obesity class II between ≥35 and <40 kg/m2, and highest class was obesity class III≥ 40 kg/m2. Echocardiographic left‐ and right‐ventricular analysis and quantification were based on transthoracic echocardiography measurements and evaluated in accordance with ASE/EACVI recommendations. 24
2.3. Ethical aspects and study oversight
The study involved only anonymized, retrospective analysis of diagnostic standard data, and thus, individual consent for inclusion was waived according to German law. The study was approved by the local ethics committee on human research and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
2.4. Statistics
The included patients were stratified according to the mentioned WHO weight classes and the groups were compared regarding baseline parameters.
Descriptive statistics for the relevant comparisons regarding baseline characteristics of the weight‐class groups were provided with median and interquartile range (IQR), or absolute numbers and corresponding percentages. Continuous variables were compared using the Kruskal–Wallis test and categorical variables with Fisher's exact or χ 2 test, as appropriate. Univariable logistic regression models were calculated to examine the impact of the different patients’ weight classes in comparison to the normal‐weight group (as the reference group) on in‐hospital mortality, and 1‐year and 3‐year survival. Results were presented as odds ratios (OR) and 95% confidence interval (CI). All of these analyses were performed in a univariable as well as a multivariable manner. Multivariate logistic regression analyses were adjusted for Logistic EuroScore. In addition, Cox regression models were computed to examine the impact of patients’ weight classes in comparison to the normal‐weight group on long‐term survival. These results were presented as hazard ratios (HRs) with 95% CI in a univariable manner as well as in a multivariable manner adjusted for Logistic EuroScore. p Values <.05 (two‐sided) were considered to be statistically significant. The software SPSS® (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 25.0: IBM Corp.) was used for computerised analysis.
3. RESULTS
Overall, 617 patients (aged 79.2 years in the median; 47.3% females) treated with TMVr using MitraClip® implantations between June 9, 2010 and March 8, 2018, who could be categorized in weight classes, were included in the present study.
3.1. Baseline parameters
Patients were categorized as follows: 12 patients were classified as underweight (2.2%), 220 as normal weight (40.1%), 237 as overweight (43.2%), and 64 patients were categorized as obesity class I (11.7%), 12 as obesity class II (2.2%), and 4 as obesity class III (0.7%).
Despite higher age in the weight classes underweight and normal weight (underweight: 79.8 [IQR: 72.8–85.8]; normal weight: 80.4 [75.4–84.9]; overweight: 78.7 [74.3–83.5]; obesity class I: 78.7 [72.9–82.9]; obesity class II: 73.3 [70.6–79.0]; obesity class III: 72.5 [70.0–73.1]; p < .001), the preprocedural Logistic EuroScore values (21.1 [IQR: 14.0–37.1]; 26.0 [18.5–38.5]; 26.0 [18.4–39.9]; 24.8 [16.8–33.8]; 33.0 [25.9–49.2]; 31.6 [13.1–47.6]; p = .291) were comparable between the groups (Table 1). Prevalence of the cardiovascular risk factors arterial hypertension and diabetes mellitus increased in higher weight classes. Additionally, the frequency of renal insufficiency was higher in obese individuals (Table 1). However, the administration of medication for heart failure was similar between the groups. The left ventricular function was more commonly reduced in obese patients of the obesity classes I and II compared to normal‐weight and overweight patients (Table 1 and Figure 1). Figure 2 illustrates the MR grade reduction from pre‐ to postinterventional. Residual MR grades at discharge were comparable between underweight (p = .187) and normal weight, overweight (p = .528) and normal weight, and class II and normal weight (p = .663), as well as class III and normal weight (p = .451), whereas patients with obesity class I (p = .005) revealed lower residual MR grades at discharge in comparison to normal‐weight patients.
Table 1.
Baseline characteristics of all patients included in the retrospective analysis stratified for survival status at 1‐year follow‐up
| Parameter | Underweight (n = 12; 2.2%) | Normal weight (n = 220; 40.1%) | Overweight (n = 237; 43.2%) | Obesity class I (n = 64; 11.7%) | Obesity class II (n = 12; 2.2%) | Obesity class III (n = 4; 0.7%) | p Value |
|---|---|---|---|---|---|---|---|
| Age at procedure (years) | 79.8 (72.8–85.8) | 80.4 (75.4–84.9) | 78.7 (74.3–83.5) | 78.7 (72.9–82.9) | 73.3 (70.6–79.0) | 72.5 (70.0–73.1) | <.001 |
| Age >70 years | 10 (83.3%) | 227 (93.3%) | 238 (87.8%) | 56 (80.0%) | 10 (76.9%) | 4 (80.0%) | .056 |
| Female sex | 10 (83.2%) | 135 (54.9%) | 104 (38.4%) | 33 (47.1%) | 7 (53.8%) | 3 (60.0%) | .001 |
| In‐hospital stay (days) after the procedure | 5.0 (3.3–6.5) | 5.0 (4.0–7.0) | 5.0 (4.0–6.0) | 5.0 (4.0–7.0) | 6.0 (4.5–7.0) | 7.0 (5.3–8.8) | .223 |
| NYHA III or IV | 10 (83.3%) | 190 (86.4%) | 211 (89.0%) | 63 (98.4%) | 12 (100.0%) | 3 (75.0%) | .072 |
| Cardiovascular risk factors | |||||||
| Art. hypertension | 8 (66.7%) | 200 (81.3%) | 244 (90.0%) | 60 (85.7%) | 13 (100.0%) | 5 (100.0%) | .012 |
| Diabetes mellitus | 0 (0.0%) | 40 (16.3%) | 85 (31.4%) | 35 (50.0%) | 9 (69.2%) | 3 (60.0%) | <.001 |
| Intervention parameters | |||||||
| FMR | 4 (33.3%) | 139 (56.5%) | 155 (57.2%) | 47 (67.1%) | 8 (61.5%) | 2 (40.0%) | .541 |
| DMR | 6 (50.0%) | 78 (31.7%) | 82 (30.3%) | 15 (21.4%) | 3 (23.1%) | 3 (60.0%) | |
| Mixed etiology | 2 (16.7%) | 29 (11.8%) | 34 (12.5%) | 8 (11.4%) | 2 (15.4%) | 0 (0.0%) | |
| Number of implanted clips >1 | 3 (25.0%) | 114 (46.3%) | 146 (53.9%) | 24 (34.3%) | 7 (53.8%) | 4 (80.0%) | .126 |
| Logistic EuroScore I (points) | 21.1 (14.0–37.1) | 26.0 (18.5–38.5) | 26.0 (18.4–39.9) | 24.8 (16.8–33.8) | 33.0 (25.9–49.2) | 31.6 (13.1–47.6) | .291 |
| Comorbidities | |||||||
| COPD | 6 (50.0%) | 38 (15.4%) | 29 (10.7%) | 8 (11.4%) | 4 (30.8%) | 2 (40.0%) | .001 |
| Atrial fibrillation | 7 (58.3%) | 181 (73.6%) | 191 (70.5%) | 55 (78.6%) | 10 (76.9%) | 4 (80.0%) | .627 |
| Renal insufficiency | 4 (33.3%) | 112 (45.5%) | 133 (49.3%) | 40 (57.1%) | 12 (92.3%) | 3 (60.0%) | .014 |
| Coronary artery disease | 5 (41.7%) | 154 (62.6%) | 172 (63.5%) | 53 (76.8%) | 8 (61.5%) | 4 (80.0%) | .138 |
| Peripheral artery disease | 2 (16.7%) | 25 (10.2%) | 26 (9.6%) | 6 (8.6%) | 3 (23.1%) | 1 (20.0%) | .588 |
| History of stroke | 0 (0.0%) | 30 (12.2%) | 31 (11.4%) | 8 (11.4%) | 2 (15.4%) | 1 (20.0%) | .824 |
| History of aortic valve surgery | 1 (8.3%) | 15 (6.1%) | 24 (8.9%) | 5 (7.2%) | 2 (15.4%) | 1 (20.0%) | .674 |
| Medication | |||||||
| Diuretics | 9 (75.0%) | 232 (94.7%) | 247 (91.5%) | 66 (94.3%) | 12 (92.3%) | 5 (100.0%) | .137 |
| RAS blockers | 9 (75.0%) | 200 (81.6%) | 223 (82.6%) | 59 (84.3%) | 11 (84.6%) | 4 (80.0%) | .978 |
| Beta‐blockers | 7 (58.3%) | 206 (84.1%) | 224 (83.0%) | 55 (78.6%) | 10 (76.9%) | 4 (80.0%) | .280 |
| Echocardiography | |||||||
| LVEF (%) pre | 52.0 (40.0–55.0) | 45.0 (30.0–55.0) | 43.0 (30.0–55.0) | 35.0 (30.0–50.0) | 35.0 (30.0–50.0) | 50.0 (50.0–50.0) | .003 |
| MR (grade)a preprocedure | 3 (3–3) | 3 (3–3) | 3 (3–3) | 3 (3–3) | 3 (3–3) | 3 (3–3) | .684 |
| MR (grade)a at discharge | 2 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–1) | .003 |
| TAPSE < 1.8 cm | 3 (60%) | 62 (54.4%) | 64 (52.5%) | 21 (65.6%) | 0 (0%) | 1 (100%) | .566 |
| sPAP > 30 mm Hg | 8 (100%) | 183 (96.3%) | 197 (98.5%) | 55 (98.2%) | 7 (100%) | 2 (100%) | .767 |
| Laboratory examinations | |||||||
| BNP (pg/ml) preprocedure | 453.0 (110.3–812.3) | 564.0 (276.0–1478.5) | 582.5 (275.0–1142.0) | 444.0 (219.5–980.5) | 888.0 (736.0–1497.0) | 357.5 (147.0–888.3) | .040 |
| hsTnI (pg/ml) preprocedure | 9.2 (4.6–35.5) | 19.1 (7.8–46.6) | 18.8 (8.2–43.8) | 19.2 (6.8–47.3) | 32.8 (14.9–73.0) | 11.8 (5.1–58.1) | .667 |
Note: Bold values considered to be statistically significant at p < .05 (two‐sided).
Abbreviations: BNP, brain natriuretic peptide; COPD, chronic obstructive pulmonary disease; DMR, degenerative mitral valve regurgitation; FMR, functional mitral valve regurgitation; hsTnI, high sensitive troponin I; LVEF, left ventricular ejection fraction; MR, mitral valve regurgitation (aclassified into four grades: 0 = no/trace, 1 = mild, 2 = moderate or moderate‐severe, 3 = severe); NYHA, New York Heart Association; RAS, renin–angiotensin system; sPAP, systolic pulmonary artery pressure; TAPSE, tricuspid annular plane systolic excursion.
Figure 1.

LVEF graduation of the LVEF at baseline of the patients treated with MitraClip® implantation stratified for the different weight classes. LVEF, left ventricular ejection fraction.
Figure 2.

Changes in MR regurgitation severity grades from baseline to discharge in the different weight classes. MR, mitral valve.
3.2. Impact of weight classes on survival
The weight class had no impact on in‐hospital death (underweight: 0.0%; normal weight: 4.1%; overweight: 1.5%; obesity class I: 0.0%; obesity class II: 7.7%; obesity class III: 0.0%; p = .189), 1‐year survival (75.0%; 72.0%; 76.9%; 75.0%; 75.0%; 33.3%; p = .542) and 3‐year survival (40.0%; 36.8%; 38.2%; 48.6%; 20.0%; 33.3%; p = .661) (Figure 3A).
Figure 3.

Survival rate at discharge, 1‐year follow‐up, and 3‐year follow‐up stratified for weight classes. (A) Survival rate at discharge (dark blue line), 1‐year follow‐up (orange line), and 3‐year follow‐up (light blue line) stratified for weight classes. (B) Association of weight class compared to normal weight with 1‐year survival (adjusted for Log EuroScore). (C) Association of weight class compared to normal weight with 3‐year survival (adjusted for Log EuroScore).
Underweight (univariable: OR: 1.17 [95% CI: 0.23–5.95], p = .854; multivariable: OR: 0.82 [95% CI: 0.15–4.40], p = .813), overweight (univariable: OR: 1.30 [95% CI: 0.82–2.05], p = .269; multivariable: OR: 1.25 [95% CI: 0.76–2.04], p = .386), obesity class I (univariable: OR: 1.17 [95% CI: 0.58–2.35], p = .669; multivariable: OR: 0.93 [95% CI: 0.43–2.04], p = .864), obesity class II (univariable: OR: 1.17 [95% CI: 0.30–4.47], p = .823; multivariable: OR: 1.38 [95% CI: 0.35–5.51], p = .649) and obesity class III (univariable: OR: 0.19 [95% CI: 0.02–2.19], p = .185; multivariable: OR: 0.23 [95% CI: 0.02–2.78], p = .249) were all not associated with 1‐year survival in comparison to the reference group of patients with normal weight (Figure 3B).
Similarly, the 3‐year survival of the patients treated with MitraClip® was not affected by underweight (univariable: OR: 1.14 [95% CI: 0.19–7.08], p = .886; multivariable: OR: 1.00 [95% CI: 0.15–6.67], p = .997), overweight (univariable: OR: 1.06 [95% CI: 0.65–1.74], p = .814; multivariable: OR: 1.00 [95% CI: 0.57–1.75], p = .998), obesity class I (univariable: OR: 1.62 [95% CI: 0.78–3.39], p = .196; multivariable: OR: 1.45 [95% CI: 0.65–3.27], p = .366), obesity class II (univariable: OR: 0.43 [95% CI: 0.09–2.10], p = .296; multivariable: OR: 0.42 [95% CI: 0.08–2.09], p = .286) or obesity class III (univariable: OR: 0.86 [95% CI: 0.08–9.70], p = .901; multivariable: OR: 1.13 [95% CI: 0.09–13.87], p = .924) in comparison to individuals with normal weight (Figure 3C).
Regarding long‐term survival, underweight (univariable: HR: 1.68 [95% CI: 0.82–3.44], p = .159; multivariable: HR: 1.35 [95% CI: 0.65–2.79], p = .419) was not associated with lower long‐term survival in comparison to normal weight. In addition, obesity class I (univariable: HR: 1.01 [95% CI: 0.72–1.43], p = .950; multivariable: HR: 0.93 [95% CI: 0.65–1.34], p = .705), obesity class II (univariable: HR: 0.37 [95% CI: 0.12–1.17], p = .092; multivariable: HR: 0.39 [95% CI: 0.12–1.24], p = .112) as well as obesity class III (univariable: HR: 1.46 [95% CI: 0.36–5.94], p = .594; multivariable: HR: 1.28 [95% CI: 0.32–5.21], p = .726) did also not affect long‐term survival significantly. In contrast, overweight was independently associated with improved survival (univariable: HR: 1.18 [95% CI: 0.94–1.48], p = .151; multivariable: HR: 1.32 [95% CI: 1.04–1.68], p = .023) in comparison to the reference group with normal weight in the adjusted regression model (Figure 4).
Figure 4.

Long‐term survival stratified for weight classes. (A) Hazard plot for patients treated with MitraClip® implantation stratified for weight classes. (B) Association of weight class compared to normal‐weight with long‐term survival (adjusted for Logistic EuroScore).
4. DISCUSSION
Epidemiological studies and surveys reported an alarming increase in the prevalence of obesity worldwide. 17 , 20 , 25 , 26 Obesity was associated with poor long‐term outcomes in the healthy general population and was identified as an important risk factor for the development of cardiovascular diseases (CVD), occurrence of CVD events, and increased mortality. 20 , 25 , 27 , 28 Based on this burden of knowledge, the American joint guidelines of the American Heart Association (AHA) and the American College of Cardiology Foundation of 2011 29 recommend a weight management and optimization with the primary aim to maintain or achieve a BMI within the normal range between 18.5 and 24.9 kg/m2 in particular for patients with CVD. 29 Despite the unfavorable consequences of obesity on the development of CVD and long‐term outcomes, 25 , 27 , 30 several studies demonstrated that obese patients with CVD, 17 , 18 , 19 such as coronary artery disease as well as myocardial infarction, 17 , 18 , 31 , 32 pulmonary embolism, 33 heart failure, 17 , 34 and atrial fibrillation 35 revealed a better prognosis compared to their leaner counterparts. 19 This phenomenon with a survival discrepancy has been referred to as the term “obesity paradox.” 17 , 18 , 19 , 25 , 31 , 36
Data about the impact of obesity as well as weight classes on mitral valve disease are sparse. One study demonstrated an association between low BMI and the presence of mitral valve prolapse, 37 whereas the influence of obesity on the development of MR is widely unknown. 20 While an obesity survival paradox was demonstrated for patients with transcatheter aortic valve implantations, 25 , 38 , 39 , 40 , 41 one study failed to confirm an influence of obesity on the outcomes after mitral valve surgery 42 and one recently published large study was also not able to confirm an obesity survival paradox for the in‐hospital stay of patients treated with MitraClip® implantations. 20
The results of the present study demonstrated for the first time that overweight affected survival beneficially regarding the long‐term survival of patients treated with TEER, and therefore, the presence of an overweight survival paradox in these patients. The long‐term survival of overweight patients was 1.3‐fold higher than that of the normal‐weight reference group independently of the parameters of the Logistic EuroScore. In contrast, obesity was not associated with better survival.
The reasons underlying the obesity or overweight paradox have still not been fully elucidated and understood. 20 , 28 , 43 , 44 , 45 , 46 Regarding the obesity/overweight paradox, it has to be considered that obesity and overweight might prevent malnutrition and energy wastage. 20 In this context, it should not be overlooked that patients treated with TEER caused by severe MR with high surgical risk are frequently affected by an end‐stage CVD. 6 , 13 , 20 , 47 Patients with severe MR often suffer from heart failure (symptoms) and have often a poor prognosis. 47
Obesity and overweight represent a nutritional reserve, which might particularly become important in older patients with frailty when comorbidities and lower homeostatic reserves coexist. 48 In addition, overweight and obesity may protect against malnutrition and energy wastage during acute CVD events, surgeries, or interventions based on alterations with respect to the neuroendocrine status that may subsequently have an impact on the modulation of pathologic cardiovascular remodeling. 28 , 48 , 49 , 50 , 51 Higher BMI and obesity may protect patients against inflammatory cytokines by an enhanced production of “buffering” lipoproteins. 28 , 43
Another hypothesis for the obesity paradox consists of the assumption that normal weight in older individuals with CVD is largely uncommon in Western populations, insinuating that normal weight may reflect the presence of unknown or serious comorbid conditions. 28 , 52 , 53
The apparent discrepancy that overweight affected the long‐term survival of patients treated by TEER for MR beneficially, but obesity did not, might be attributed to the fact that indeed both weight classes (overweight as well as obesity) are related to a nutritional reserve, but obesity might be affiliated to other unfavorable periprocedural and long‐term effects. The higher rate of reduced left ventricular function in obese patients (obesity classes I and II) as well as the higher rate of the postprocedural remaining unfavorable moderate and severe MR in patients with obesity class II might in part be an explanation for a similar long‐term survival of obese patients despite better nutritional reserve of obesity in comparison to normal weight. This finding might outline the specific anatomical challenges and efforts in non‐normal weight patients to achieve optimal MR reduction by TMVr and underlines the importance of a careful patient selection. 54
4.1. Limitations
Some limitations regarding our study merit consideration: First, the design of the study is a monocentric retrospective analysis on an all‐comer sample of patients undergoing interventional edge‐to‐edge repair for MR without any control group. The follow‐up rate was almost complete (96.7%); thus, selection bias can widely be excluded. Second, the potential impact of weight classes on prognosis has to be interpreted with caution since some weight class groups were small.
5. FUTURE DIRECTIONS
Although TMVr using MitraClip® technique or TEER therapy is an established treatment for patients suffering from MR with both primary etiology, who are at high or prohibitive surgical risk, and secondary etiology in a broader range of risk classes and age groups according to current guidelines, 4 , 6 , 10 , 13 , 14 , 15 , 16 identification of patients at higher risk of complications and mortality as well as identification of specific risk factors of poor outcome is of outstanding interest. 54
6. CONCLUSION
Our results demonstrated a long‐term survival benefit for patients undergoing MitraClip® procedure with overweight in comparison to normal weight patients.
CONFLICTS OF INTEREST
Lukas Hobohm reports having received lecture honoraria from MSD. Felix Kreidel reports having received consultancy and lecture honoraria from Abbott, Cardiac Implants, Edwards Lifesciences. Eberhard Schulz reports lecture honoraria from Edwards Lifesciences and Medtronic. Ralph Stephan von Bardeleben reports having received lecture honoraria from Abbott Structural Heart, Bioventrix, Boehringer Ingelheim, Cardiac Dimensions, Edwards Lifesciences and Philips Healthcare outside the current paper. Unpaid IIT and trial participation as Global or local PI and steering team member to Abbott Structural Heart, Cardiac Dimensions, Edwards Lifesciences, IZKS University of Göttingen, LMU Munich and DZHK Germany. The remaining authors declare no conflict of interest.
ACKNOWLEDGMENTS
This work contains results that are part of the doctoral thesis of Kevin Bachmann and Sonja Born. Thomas Münzel is PI of the DZHK (German Center for Cardiovascular Research), Partner Site Rhine‐Main, Mainz, Germany. Open Access funding enabled and organized by Projekt DEAL.
Keller K, Geyer M, Hobohm L, et al. Survival benefit of overweight patients undergoing MitraClip® procedure in comparison to normal‐weight patients. Clin Cardiol. 2022;45:1236‐1245. 10.1002/clc.23897
Karsten Keller and Martin Geyer contributed equally to this study and should be considered as co‐shared first authors.
Contributor Information
Karsten Keller, Email: karsten.keller@unimedizin-mainz.de.
Martin Geyer, Email: Martin.Geyer@unimedizin-mainz.de.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
REFERENCES
- 1. Lancellotti P, Moura L, Pierard LA, et al. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010;11(4):307‐332. [DOI] [PubMed] [Google Scholar]
- 2. Stone GW, Vahanian AS, Adams DH, et al. Mitral Valve Academic Research C . Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 1: clinical trial design principles: a consensus document from the Mitral Valve Academic Research Consortium. J Am Coll Cardiol. 2015;66(3):278‐307. [DOI] [PubMed] [Google Scholar]
- 3. Enriquez‐Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet. 2009;373(9672):1382‐1394. [DOI] [PubMed] [Google Scholar]
- 4. Regueiro A, Granada JF, Dagenais F, Rodes‐Cabau J. Transcatheter mitral valve replacement: insights from early clinical experience and future challenges. J Am Coll Cardiol. 2017;69(17):2175‐2192. [DOI] [PubMed] [Google Scholar]
- 5. El‐Tallawi KC, Messika‐Zeitoun D, Zoghbi WA. Assessment of the severity of native mitral valve regurgitation. Prog Cardiovasc Dis. 2017;60(3):322‐333. [DOI] [PubMed] [Google Scholar]
- 6. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159‐e1195. [DOI] [PubMed] [Google Scholar]
- 7. Grasso C, Capodanno D, Scandura S, et al. One‐ and twelve‐month safety and efficacy outcomes of patients undergoing edge‐to‐edge percutaneous mitral valve repair (from the GRASP Registry). Am J Cardiol. 2013;111(10):1482‐1487. [DOI] [PubMed] [Google Scholar]
- 8. Feldman T, Young A. Percutaneous approaches to valve repair for mitral regurgitation. J Am Coll Cardiol. 2014;63(20):2057‐2068. [DOI] [PubMed] [Google Scholar]
- 9. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez‐Sarano M. Burden of valvular heart diseases: a population‐based study. Lancet. 2006;368(9540):1005‐1011. [DOI] [PubMed] [Google Scholar]
- 10. von Bardeleben RS, Hobohm L, Kreidel F, et al. Incidence and in‐hospital safety outcomes of patients undergoing percutaneous mitral valve edge‐to‐edge repair using MitraClip: five‐year German national patient sample including 13,575 implants. EuroIntervention. 2019;14(17):1725‐1732. [DOI] [PubMed] [Google Scholar]
- 11. Bedogni F, Testa L, Rubbio AP, et al. Real‐world safety and efficacy of transcatheter mitral valve repair with MitraClip: thirty‐day results from the Italian Society of Interventional Cardiology (GIse) Registry of transcatheter treatment of mitral valve RegurgitaTiOn (GIOTTO). Cardiovasc Revasc Med. 2020;21(9):1057‐1062. [DOI] [PubMed] [Google Scholar]
- 12. Puls M, Lubos E, Boekstegers P, et al. One‐year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: results from the German Transcatheter Mitral Valve Interventions Registry. Eur Heart J. 2016;37(8):703‐712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baumgartner H, Falk V, Bax JJ, et al. Group ESCSD 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739‐2791. [DOI] [PubMed] [Google Scholar]
- 14. Otto CM, Nishimura RA, Bonow RO, et al. ACC/AHA Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation . 2020;143(5):e35‐e71. [DOI] [PubMed]
- 15. Adamo M, Fiorelli F, Melica B, et al. COAPT‐like profile predicts long‐term outcomes in patients with secondary mitral regurgitation undergoing MitraClip implantation. JACC Cardiovasc Interv. 2021;14:15‐25. [DOI] [PubMed] [Google Scholar]
- 16. Chhatriwalla AK, Vemulapalli S, Holmes DR Jr., et al. Institutional experience with transcatheter mitral valve repair and clinical outcomes: insights from the TVT Registry. JACC Cardiovasc Interv. 2019;12(14):1342‐1352. [DOI] [PubMed] [Google Scholar]
- 17. Lavie C, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy weight and obesity prevention. J Am Coll Cardiol. 2018;72(13):1506‐1531. [DOI] [PubMed] [Google Scholar]
- 18. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53(21):1925‐1932. [DOI] [PubMed] [Google Scholar]
- 19. Lavie CJ, McAuley PA, Church TS, Milani RV, Blair SN. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol. 2014;63(14):1345‐1354. [DOI] [PubMed] [Google Scholar]
- 20. Keller K, Hobohm L, Geyer M, et al. Impact of obesity on adverse in‐hospital outcomes in patients undergoing percutaneous mitral valve edge‐to‐edge repair using MitraClip(R) procedure—results from the German nationwide inpatient sample. Nutr Metab Cardiovasc Dis. 2020;30(8):1365‐1374. [DOI] [PubMed] [Google Scholar]
- 21. Geyer M, Keller K, Sotiriou E, et al. Association of transcatheter direct mitral annuloplasty with acute anatomic, haemodynamic, and clinical outcomes in severe mitral valve regurgitation. ESC Heart Fail. 2020;7:3336‐3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30(4):303‐371. [DOI] [PubMed] [Google Scholar]
- 23. Lancellotti P, Tribouilloy C, Hagendorff A, et al. Scientific Document Committee of the European Association of Cardiovascular I. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2013;14(7):611‐644. [DOI] [PubMed] [Google Scholar]
- 24. Galie N, Humbert M, Vachiery JL, et al. Group ESCSD 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67‐119. [DOI] [PubMed] [Google Scholar]
- 25. De Palma R, Ivarsson J, Feldt K, et al. The obesity paradox: an analysis of pre‐procedure weight trajectory on survival outcomes in patients undergoing transcatheter aortic valve implantation. Obes Res Clin Pract. 2018;12(1):51‐60. [DOI] [PubMed] [Google Scholar]
- 26. Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197‐1209. [DOI] [PubMed] [Google Scholar]
- 27. Whitlock G, Lewington S, Sherliker P, et al. Body‐mass index and cause‐specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083‐1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Keller K, Hobohm L, Geyer M, et al. Obesity paradox in peripheral artery disease. Clin Nutr. 2019;38(5):2269‐2276. [DOI] [PubMed] [Google Scholar]
- 29. Smith SC Jr., Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58(23):2432‐2446. [DOI] [PubMed] [Google Scholar]
- 30. Borch KH, Braekkan SK, Mathiesen EB, et al. Abdominal obesity is essential for the risk of venous thromboembolism in the metabolic syndrome: the Tromso study. J Thromb Haemost. 2009;7(5):739‐745. [DOI] [PubMed] [Google Scholar]
- 31. Lavie CJ, De Schutter A, Patel DA, Romero‐Corral A, Artham SM, Milani RV. Body composition and survival in stable coronary heart disease: impact of lean mass index and body fat in the “obesity paradox”. J Am Coll Cardiol. 2012;60(15):1374‐1380. [DOI] [PubMed] [Google Scholar]
- 32. Keller K, Munzel T, Ostad MA. Sex‐specific differences in mortality and the obesity paradox of patients with myocardial infarction ages >70 y. Nutrition. 2018;46:124‐130. [DOI] [PubMed] [Google Scholar]
- 33. Keller K, Hobohm L, Munzel T, et al. Survival benefit of obese patients with pulmonary embolism. Mayo Clin Proc. 2019;94(10):1960‐1973. [DOI] [PubMed] [Google Scholar]
- 34. Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61(2):151‐156. [DOI] [PubMed] [Google Scholar]
- 35. Lavie CJ, Pandey A, Lau DH, Alpert MA, Sanders P. Obesity and atrial fibrillation prevalence, pathogenesis, and prognosis: effects of weight loss and exercise. J Am Coll Cardiol. 2017;70(16):2022‐2035. [DOI] [PubMed] [Google Scholar]
- 36. Keller K, Sagoschen I, Schmitt VH, et al. Obesity and its impact on adverse in‐hospital outcomes in hospitalized patients with COVID‐19. Front Endocrinol. 2022;13:876028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Movahed MR, Hepner AD. Mitral valvar prolapse is significantly associated with low body mass index in addition to mitral and tricuspid regurgitation. Cardiol Young. 2007;17(2):172‐174. [DOI] [PubMed] [Google Scholar]
- 38. van der Boon RM, Chieffo A, Dumonteil N, et al. Effect of body mass index on short‐ and long‐term outcomes after transcatheter aortic valve implantation. Am J Cardiol. 2013;111(2):231‐236. [DOI] [PubMed] [Google Scholar]
- 39. Lv W, Li S, Liao Y, et al. The ‘obesity paradox’ does exist in patients undergoing transcatheter aortic valve implantation for aortic stenosis: a systematic review and meta‐analysis. Interact Cardiovasc Thorac Surg. 2017;25(4):633‐642. [DOI] [PubMed] [Google Scholar]
- 40. Rossi A, Gaibazzi N, Bellelli G, et al. Obesity paradox in patients with aortic valve stenosis. Protective effect of body mass index independently of age, disease severity, treatment modality and non‐cardiac comorbidities. Int J Cardiol. 2014;176(3):1441‐1443. [DOI] [PubMed] [Google Scholar]
- 41. Konigstein M, Havakuk O, Arbel Y, et al. The obesity paradox in patients undergoing transcatheter aortic valve implantation. Clin Cardiol. 2015;38(2):76‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rapetto F, Bruno VD, King M, et al. Impact of body mass index on outcomes following mitral surgery: does an obesity paradox exist? Interact Cardiovasc Thorac Surg. 2018;26(4):590‐595. [DOI] [PubMed] [Google Scholar]
- 43. Galal W, van Gestel Y, Hoeks SE, et al. The obesity paradox in patients with peripheral arterial disease. Chest. 2008;134(5):925‐930. [DOI] [PubMed] [Google Scholar]
- 44. Lavie CJ, Coursin DB, Long MT. The obesity paradox in infections and implications for COVID‐19. Mayo Clin Proc. 2021;96(3):518‐520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lavie CJ From the editor's desk‐overweight and obesity and obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2021;68:106‐107. [DOI] [PubMed] [Google Scholar]
- 46. Elagizi A, Kachur S, Lavie CJ, et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61(2):142‐150. [DOI] [PubMed] [Google Scholar]
- 47. Sorajja P, Maisano F. Percutaneous treatment for native mitral regurgitation. Prog Cardiovasc Dis. 2017;60(3):405‐414. [DOI] [PubMed] [Google Scholar]
- 48. Bucholz EM, Beckman AL, Krumholz HA, Krumholz HM. Dr. Bucholz was affiliated with the Yale School of M, Yale School of Public Health during the time that the work was c. Excess weight and life expectancy after acute myocardial infarction: the obesity paradox reexamined. Am Heart J. 2016;172:173‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Angeras O, Albertsson P, Karason K, et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34(5):345‐353. [DOI] [PubMed] [Google Scholar]
- 50. Lavie CJ, De Schutter A, Parto P, et al. Obesity and prevalence of cardiovascular diseases and prognosis—the obesity paradox updated. Prog Cardiovasc Dis. 2016;58(5):537‐547. [DOI] [PubMed] [Google Scholar]
- 51. Keller K, Munzel T, Ostad MA. Gender‐specific differences in mortality and obesity paradox of patients with myocardial infarction aged 70 years and older. Nutrition. 2017;46:124‐130. [DOI] [PubMed] [Google Scholar]
- 52. Das SR, Alexander KP, Chen AY, et al. Impact of body weight and extreme obesity on the presentation, treatment, and in‐hospital outcomes of 50,149 patients with ST‐Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol. 2011;58(25):2642‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McAuley PA, Beavers KM. Contribution of cardiorespiratory fitness to the obesity paradox. Prog Cardiovasc Dis. 2014;56(4):434‐40. [DOI] [PubMed] [Google Scholar]
- 54. Keller K, Hobohm L, Schmidtmann I, Munzel T, Baldus S, von Bardeleben RS. Centre procedural volume and adverse in‐hospital outcomes in patients undergoing percutaneous transvenous edge‐to‐edge mitral valve repair using MitraClip(R) in Germany. Eur J Heart Fail. 2021;23(8):1380‐1389. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding authors upon reasonable request.


