Abstract
Introduction
Oxygen is the most common drug used in critical care patients to correct episodes of hypoxaemia. The adoption of new technologies in clinical practice, such as closed-loop systems for an automatic oxygen titration, may improve outcomes and reduce the healthcare professionals’ workload at the bedside; however, certainty of the evidence regarding the safety and benefits still remains low. We aim to evaluate the effectiveness, efficacy and safety of the closed-loop oxygen control for patients with hypoxaemia during the hospitalisation period by conducting a systematic review and meta-analysis.
Methods and analysis
MEDLINE, CENTRAL, EMBASE, LILACS, CINAHL and LOVE evidence databases will be searched. Randomised controlled trials and cross-over studies investigating the PICO (Population, Intervention, Comparator and Outcome) framework will be included. The primary outcomes will be the time in the peripheral oxygen saturation target. Secondary outcomes will include time for oxygen weaning time; length of stay; costs; adverse events; mortality; healthcare professionals’ workload, and percentage of time with hypoxia and hyperoxia. Two reviewers will independently screen and extract data and perform quality assessment of included studies. The Cochrane risk of bias tool will be used to assess risk of bias. The RevMan V.5.4 software will be used for statistical analysis. Heterogeneity will be analysed using I2 statistics. Mean difference or standardised mean difference with 95% CI and p value will be used to calculate treatment effect for outcome variables.
Ethics and dissemination
Ethical approval is not required because this systematic review and meta-analysis is based on previously published data. Final results will be published in peer-reviewed journals and presented at relevant conferences and events.
PROSPERO registration number
CRD42022306033.
Keywords: INTENSIVE & CRITICAL CARE, Adult intensive & critical care, RESPIRATORY MEDICINE (see Thoracic Medicine)
Strengths and limitations of this study
This study will be reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols guidelines.
The steps of data screening, extraction and methodological quality assessment will be performed by two reviewers independently.
Standardised methodological evaluation tools will be used to assess the risk of bias of included studies in the review.
The absence of sufficient high-quality studies, heterogeneity in the interventions, high missing or dropout and small sample size might be the limitations for this systematic review.
Introduction
Oxygen is vital for cellular metabolism and it is considered to be the most common drug used in critical care patients to correct episodes of hypoxaemia.1 2 Low levels of oxygen in the arterial blood are frequently associated with impairment of adequate gas exchange1 2, and prolonged cellular hypoxia promotes rapid and severe organ injuries triggered by natural adaptive mechanisms.2 3 Thus, supplemental oxygen administration can be considered a life-saving treatment, and may reduce the morbidity and mortality associated with hypoxaemia.1 4
Despite the benefits of oxygen therapy indication, both hypoxaemia and hyperoxia, have potential harmful side effects and complications.5–8 The literature suggests that safe and acceptable targets of peripheral oxygen saturation (SpO2) are between 92% and 98% for patients without lung diseases, and 88% and 92% for patients with previous lung diseases.9 10 However, patients’ need for oxygen varies during hospital stay, and the manual adjustment to promote adequate oxygen delivery titration has been shown to be ineffective.9 A precise delivery oxygen method for maintaining the SpO2 within the target is challenging.10–12 It is even more challenging when we look at patients requiring invasive mechanical ventilation support admitted to the intensive care unit (ICU) who often need supplemental oxygen administration during ICU and hospital stay.1 2 4
The use of artificial intelligence (AI) and machine learning (ML) is increasing in health science to make predictions, improve the interpretation of monitored data and support decision-making.10 Closed-loop systems are part of these advances, using a feedback principle to maintain a given variable around a desired set point.10–12 Delivery oxygen devices based on closed-loop technology have been developed and used in patient care in order to provide a real-time adjustment of oxygen titration, based on patients’ SpO2 preventing episodes of hypoxaemia or hyperoxia.11 12 The adoption of new technologies of AI and ML in clinical practice, may reduce the healthcare professionals’ workload at the bedside; however, there is low certainty evidence for their safety and benefits.11 12 It is still unclear whether closed-loop oxygen control devices could improve clinical outcomes, and with the technological advances, new randomised clinical trials (RCTs)13–21 have been published since the last two systematics reviews were conducted.11 12 Thus, the aim of this systematic review is to investigate the effectiveness, efficacy and safety of the closed-loop oxygen control for patients during hospitalisation.
Methods and analysis
This study is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) statement22 and followed the recommendations of the Cochrane Collaboration Handbook. The protocol is registered at the International Prospective Register of Systematic Reviews (PROSPERO).23
Patient and public involvement
No patient or public involved. Only data already existent in the literature and the aforementioned sources will be used in this study. Patients and/or the public will not be involved in the design, conduct, reporting or dissemination plans of this research.
Search strategy
A search strategy was initially designed for the Medical Literature Analysis and the Retrieval System Online—MEDLINE, via PubMed by an information specialist, responsible for assisting the authors, searching potential studies for inclusion in their reviews, and for keeping up to date with Cochrane methodological developments in information retrieval. The search strategy was independently peer-reviewed by the information specialist, and afterwards will be adapted for use into five databases, as follows: (1) Cochrane Central Register of Controlled Trials (CENTRAL)—via Wiley; (2) Excerpta Medica dataBASE (EMBASE)—via Elsevier; (3) the Latin American the Caribbean Literature in Health Sciences (LILACS)—via Virtual Health Library; (4) Cumulative Index to Nursing and Allied Health Literature (CINAHL)—via Elton Bryson Stephens Company (EBSCO); and (5) LOVE evidence databases. A handsearching will be performed to check preprints, editorials about the included studies, errata of published articles and references lists from the included studies and any relevant systematic review identified. We will track the randomised controlled trials in progress on a specific website (https://ClinicalTrials.gov) and on the WHO website. There will be no restrictions to any specific language, date or type of publication. The detailed search strategy for MEDLINE—via PubMed is shown in table 1. The study selection process will be conducted by two reviewers independently, and any disagreement between the reviewers will be resolved by consensus or by consulting a third reviewer.
Table 1.
Search strategy for MEDLINE via PubMed
| Search number | Search terms |
| #1 | “Oxygen Inhalation Therapy”(Mesh) OR “Oxygen”(Mesh) OR oxygen*(tiab) OR Dioxygen(tiab) OR O2(tiab) OR FiO2(tiab) |
| #2 | concentrat*(tiab) OR inspir*(tiab) OR inhal*(tiab) OR level*(tiab) OR tension*(tiab) OR fraction*(tiab) OR arterial*(tiab) OR saturation supply*(tiab) OR supplement*(tiab) OR supplie*(tiab) OR therap*(tiab) OR administr*(tiab) OR dosag*(tiab) OR dose*(tiab) OR dosing*(tiab) OR titrat*(tiab) OR deliver*(tiab) |
| #3 | automat*(tiab) OR algorithms(tiab) OR system*(tiab) OR closed-loop(tiab) OR closed loop(tiab) OR intelligen*(tiab) OR targeted(tiab) OR machine learning(tiab) |
| #4 | adult(All Fields) OR middle aged(sb) OR age(tw) OR (aged(tiab) OR aged(MESH) OR geriatric*(tiab) geriatrics(MESH) OR elder*(tiab) OR olding(tiab) OR ageing(tiab) OR aging(tiab) OR aging(MESH) OR “frail elderly”(MESH)) |
| #5 | SpO2(tw) OR oxygen saturation(tw) OR Blood Oxygen Level*(tw) OR Saturation of Peripheral Oxygen(tw) OR oxygen weaning(tw) OR FiO2 weaning(tw) OR Length of stay*(tw) OR Cost*(tw) OR Adverse event*(tw) OR adverse effect*(tw) OR Near Misse*(tw) OR Side Effect*(tw) OR Adverse Reaction*(tw) OR Toxicity(tw) OR Mortalit*(tw) OR Fatality Rate*(tw) OR Death(tw) OR Workload*(tw) OR Work Load*(tw) OR process optimization(tw) OR Quality Improvement*(tw) |
| #6 | ((clinical(Title/Abstract)AND trial(Title/Abstract)) OR clinical trials as topic(MeSH Terms) OR clinical trial(Publication Type) OR random*(Title/Abstract)OR random allocation(MeSH Terms) OR therapeutic use(MeSH Subheading)) |
| #7 | #1 AND #2 AND #3 AND #4 AND #5 AND #6 |
| #8 | (animals (mh) NOT humans (mh)) |
| #9 | #7 NOT #8 |
This search strategy will be modified as required for other electronic databases.
Inclusion criteria
The eligibility criteria were determined using the PICO (Population, Intervention, Comparator and Outcome) framework.24 The studies will be considered eligible based on the following inclusion criteria, as follows: (1) population: hospitalised adult patients requiring supplemental oxygen—either for patients with hypoxaemia (SpO2<92%) or with acute chronic hypoxaemia (SpO2<88%); (2) type of interventions: any devices that allow an automatic oxygen delivery, including invasive and non-invasive devices; low and high flow oxygen devices; (3) type of comparison: manual adjustments of oxygen; (4) type of outcome: time within the SpO2 target, oxygen weaning time, length of stay, costs, adverse events, mortality, healthcare professionals workload – process optimisation, and percentage of time with hypoxia and hyperoxia. Two reviewers (CGM and AGV) will independently assess the titles, abstracts and full-text published RCTs without language restriction.
Study selection
The reviewers will identify and exclude duplicates and collate multiple reports of the same study so that each study, rather than each report, is the unit of interest in the review. For the selection process we will use Rayyan—a web and mobile application for systematic reviews software.25 The selection process will be recorded in sufficient detail to complete the PRISMA flow diagram (figure 1). Two review authors (CGM and AGV) will independently screen the titles and abstracts of all the potential studies we identify as a result of the search. All the potential full-texts of the articles that fulfilled eligibility criteria will be included. If a consensus is not reached, a third reviewer (ACP) will be consulted to solve potential disagreements regarding the included articles.
Figure 1.
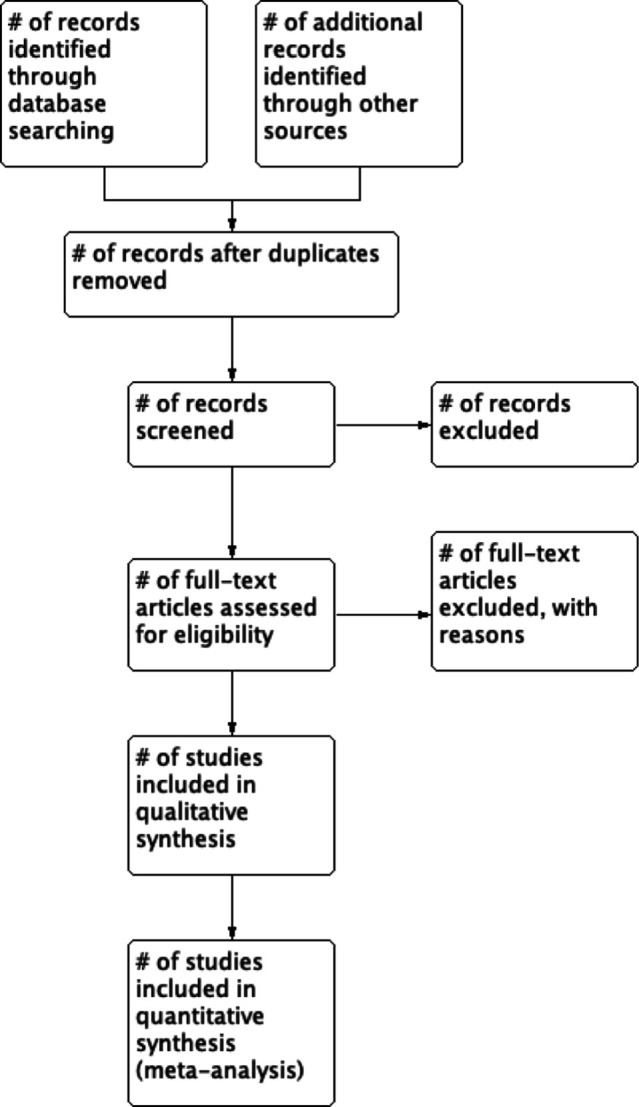
Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow diagram describing the search strategy.
Outcome measures
The primary outcome of interest will be the time spent within the SpO2 target range. Secondary outcomes of interest will be the time for oxygen weaning time, length of stay, costs, adverse events, mortality, healthcare professionals' workload, percentage of time with hypoxia and hyperoxia.
Data extraction
Two reviewers (CGM and AGV) will independently extract the data on a standard worksheet. Data will be extracted from each included study using a standardised spreadsheet developed at Microsoft Excel, as follows: authors, year, protocol number, Digital Object Identifier (DOI), study type, country of publication; the participants demographics (ie, age, gender, inclusion and exclusion criteria, number of participants, diseases, severity scores, severity of condition, comorbidity, phase of hypoxaemia), Interventions—type of device and form of delivery (ie, mechanical ventilation or conventional oxygen therapy), duration of intervention, follow-up, Comparators and Outcomes—defined in this review. We will also extract variables, as follows: time spent within the target SpO2 and other relevant variables to answer the review question (ie, oxygen weaning time, length of stay, costs, adverse events, mortality, health professionals’ workload—process optimisation). Additionally, we will extract data from the funding, sponsorship of the included studies and notable conflicts of interest of trial authors. For missing data, we will contact the corresponding authors of the studies through the email provided. In case of crossover studies inclusions, we will consider a paired analysis or if carry-over is thought to be a problem, the first period will be used to perform the analysis. If the data are homogeneous for conducting meta-analyses, one review author will transfer data into the Review Manager (RevMan) V.5.4 software. We will double-check if the data are correctly entered by comparing the data presented in the systematic review with those in the study report.
Methodological quality assessment
The risk of bias of the included trials will be assessed using the Cochrane Risk of Bias 2 (RoB2) tool for randomised trials.
Risk of bias
Assessment of the risk of bias of individual studies will be performed as recommended by the Cochrane Collaboration Handbook.26 The RoB227 will be used to evaluate the risk of bias according to five domains: (1) bias arising from the randomisation process; (2) bias due to deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in measurement of the outcome; and (5) bias in selection of the reported result. Each domain will be considered within one of the three levels, as follows: “low risk of bias”, “some concerns” or “high risk of bias”.27 We will involve a third reviewer (ACP) if a consensus cannot be reached. With the concurrence of the reviewers on the final judgement of all the included trials, the result will be displayed in a table or graph.
Assessment of bias in conducting the systematic review
The review will be conducted according to this published protocol and any deviation will be reported in the ‘differences between protocol and review’ section of the systematic review.
Assessment of certainty of evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system will be used to measure and summarise the overall current evidence of each outcome.28 The GRADE system consists of five items: (1) study limitations—risk of bias; (2) inconsistency of results (heterogeneity); (3) indirectness of evidence; (4) imprecision in effect estimates and (5) reporting bias. The quality of evidence will be classified into four categories, as follows: “high”, “moderate”, “low” and “very low”; and it will be related to the studies that contributed data to the main prespecified outcomes. All analyses will be performed using GRADEpro Guideline Development Tool (GRADEpro GDT) software.29 Two authors will rate it independently and a third author will address any discrepancy found in the study.
Data synthesis
RevMan V.5.4 (Cochrane Collaboration) software will be used to conduct the meta-analysis if appropriate—that is: statistically and clinically homogeneous. A random-effects model will be used. The mean difference or standardised mean difference will be used to analyse continuous variables with 95% CI. Dichotomous outcomes will be presented as risk ratios with 95% CI. Heterogeneity among included trials will be measured using the I2 statistic. If it is identified as substantial heterogeneity, we will report and explore it through a prespecified subgroup analysis. In addition, sensitivity analysis will be performed through separate analyses of studies judged to have a high risk of bias or a methodological weakness considered important. In cases where the combination of data does not make it possible to do the meta-analysis, we will carry out only a qualitative synthesis of each included study, of the ongoing studies identified in our search, and of the publication bias analysis.
Subgroup analysis
We plan to perform analysis of subgroups, as follows: underlying disease; hypoxaemia stage (acute vs chronic); SpO2 target (threshold <92% versus >92%), and devices (mechanical ventilation vs non-invasive devices).
Supplementary Material
Footnotes
Contributors: Conceptualisation—AGV, CGM and RKN. Protocol writing—AGV, CGM and RKN. Methodology—AGV, ACP, BMG, CGM and RKN. Project administration—AGV, ACP, CGM and RKN. Supervision—AGV, CGM and RKN. Validation—AGV, ACP, CGM and RKN. Writing—original draft—AGV, ACP, BMG, CGM and RKN. Writing—review and editing—ACP, AGV, BMG, CGM, EDSP, RAC and RKN.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Gilbert-Kawai ET, Mitchell K, Martin D, et al. Permissive hypoxaemia versus normoxaemia for mechanically ventilated critically ill patients. Cochrane Database Syst Rev 2014:CD009931.. 10.1002/14651858.CD009931.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Driscoll BR, Smith R. Oxygen use in critical illness. Respir Care 2019;64:1293–307. 10.4187/respcare.07044 [DOI] [PubMed] [Google Scholar]
- 3.Allardet-Servent J, Sicard G, Metz V, et al. Benefits and risks of oxygen therapy during acute medical illness: just a matter of dose! Rev Med Interne 2019;40:670–6. 10.1016/j.revmed.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 4.de Jonge E, Peelen L, Keijzers PJ, et al. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care 2008;12:R156. 10.1186/cc7150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barbateskovic M, Schjørring OL, Krauss SR, et al. Higher vs Lower Oxygenation Strategies in Acutely Ill Adults. Chest 2021;159:154–73. 10.1016/j.chest.2020.07.015 [DOI] [PubMed] [Google Scholar]
- 6.Valencia Gallardo JM, Solé Violán J, Rodríguez de Castro F. [Translated article] Oxygen therapy. Considerations regarding its use in acute ill patients. Arch Bronconeumol 2022;58:T102–3. 10.1016/j.arbres.2021.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chu DK, Kim LH-Y, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (iota): a systematic review and meta-analysis. Lancet 2018;391:1693–705. 10.1016/S0140-6736(18)30479-3 [DOI] [PubMed] [Google Scholar]
- 8.Li L, Zhang Y, Wang P, et al. Conservative versus liberal oxygen therapy for acutely ill medical patients: a systematic review and meta-analysis. Int J Nurs Stud 2021;118:103924. 10.1016/j.ijnurstu.2021.103924 [DOI] [PubMed] [Google Scholar]
- 9.Website. British thoracic Society emergency oxygen audit report national audit period. Available: https://www.brit-thoracic.org.uk/document-library/quality-improvement/audit-reports/emergency-oxygen-2015/
- 10.Rush B, Celi LA, Stone DJ. Applying machine learning to continuously monitored physiological data. J Clin Monit Comput 2019;33:887–93. 10.1007/s10877-018-0219-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Denault M-H, Péloquin F, Lajoie A-C, et al. Automatic versus manual oxygen titration in patients requiring supplemental oxygen in the hospital: a systematic review and meta-analysis. Respiration 2019;98:178–88. 10.1159/000499119 [DOI] [PubMed] [Google Scholar]
- 12.Sanchez-Morillo D, Olaby O, Fernandez-Granero MA, et al. Physiological closed-loop control in intelligent oxygen therapy: a review. Comput Methods Programs Biomed 2017;146:101–8. 10.1016/j.cmpb.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 13.Chelly J, Mazerand S, Jochmans S, et al. Automated vs. conventional ventilation in the ICU: a randomized controlled crossover trial comparing blood oxygen saturation during daily nursing procedures (I-NURSING). Crit Care 2020;24:453. 10.1186/s13054-020-03155-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Bie AJR, Neto AS, van Meenen DM, et al. Fully automated postoperative ventilation in cardiac surgery patients: a randomised clinical trial. Br J Anaesth 2020;125:739–49. 10.1016/j.bja.2020.06.037 [DOI] [PubMed] [Google Scholar]
- 15.Denault M-H, Ruel C, Simon M, et al. Evaluation of hyperoxia-induced hypercapnia in obese patients after cardiac surgery: a randomized crossover comparison of conservative and liberal oxygen administration. Can J Anaesth 2020;67:194–202. 10.1007/s12630-019-01500-x [DOI] [PubMed] [Google Scholar]
- 16.АА E, Komnov RD, PА T. Comparing the Intellivent-ASV® mode with conventional ventilation modes during weaning after uncomplicated cardiac surgery. Messenger of ANESTHESIOLOGY AND RESUSCITATION 2021;18:36–45. [Google Scholar]
- 17.Hansen EF, Hove JD, Bech CS, et al. Automated oxygen control with O2matic® during admission with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis 2018;13:3997–4003. 10.2147/COPD.S183762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harper JC, Kearns NA, Maijers I, et al. Closed-Loop oxygen control using a novel nasal high-flow device: a randomized crossover trial. Respir Care 2021;66:416–24. 10.4187/respcare.08087 [DOI] [PubMed] [Google Scholar]
- 19.L'Her E, Jaber S, Verzilli D, et al. Automated closed-loop versus standard manual oxygen administration after major abdominal or thoracic surgery: an international multicentre randomised controlled study. Eur Respir J 2021;57. doi: 10.1183/13993003.00182-2020. [Epub ahead of print: 05 01 2021]. [DOI] [PubMed] [Google Scholar]
- 20.Roca O, Caritg O, Santafé M, et al. Closed-Loop oxygen control improves oxygen therapy in acute hypoxemic respiratory failure patients under high flow nasal oxygen: a randomized cross-over study (the HILOOP study). Crit Care 2022;26:108. 10.1186/s13054-022-03970-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arnal J-M, Garnero A, Novotni D, et al. Closed loop ventilation mode in intensive care unit: a randomized controlled clinical trial comparing the numbers of manual ventilator setting changes. Minerva Anestesiol 2018;84:58–67. 10.23736/S0375-9393.17.11963-2 [DOI] [PubMed] [Google Scholar]
- 22.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 23.PROSPERO . Available: http://www.crd.york.ac.uk/PROSPERO [Accessed 31 Jan 2022].
- 24.InJ WT, Kneale D, Mckenzie JE. Chapter 2: determining the scope of the review and the questions it will address. 6, 2021. www.training.cochrane.org/handbook [Google Scholar]
- 25.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile APP for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JPT, Thomas J. Cochrane Handbook for systematic reviews of interventions. John Wiley & Sons 2019. [Google Scholar]
- 27.Higgins JPT, Altman DG, Gotzsche PC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials.. BMJ. 2011;343–d5928:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.GRADE handbook.. Available: http://guidelinedevelopment.org/handbook [Accessed 31 Jan 2022].
- 29.GRADEpro.. Available: http://gradepro.org [Accessed 31 Jan 2022].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


