Abstract
Background
Patients with advanced melanoma have limited treatment options after progression on immune checkpoint inhibitors (ICI). Lifileucel, a one-time autologous tumor-infiltrating lymphocyte (TIL) cell therapy, demonstrated an investigator-assessed objective response rate (ORR) of 36% in 66 patients who progressed after ICI and targeted therapy. Herein, we report independent review committee (IRC)-assessed outcomes of 153 patients treated with lifileucel in a large multicenter Phase 2 cell therapy trial in melanoma.
Methods
Eligible patients had advanced melanoma that progressed after ICI and targeted therapy, where appropriate. Melanoma lesions were resected (resected tumor diameter ≥1.5 cm) and shipped to a central good manufacturing practice facility for 22-day lifileucel manufacturing. Patients received a non-myeloablative lymphodepletion regimen, a single lifileucel infusion, and up to six doses of high-dose interleukin-2. The primary endpoint was IRC-assessed ORR (Response Evaluation Criteria in Solid Tumors V.1.1).
Results
The Full Analysis Set consisted of 153 patients treated with lifileucel, including longer-term follow-up on the 66 patients previously reported. Patients had received a median of 3.0 lines of prior therapy (81.7% received both anti-programmed cell death protein 1 and anti-cytotoxic lymphocyte-associated protein 4) and had high disease burden at baseline (median target lesion sum of diameters (SOD): 97.8 mm; lactate dehydrogenase (LDH) >upper limit of normal: 54.2%). ORR was 31.4% (95% CI: 24.1% to 39.4%), with 8 complete responses and 40 partial responses. Median duration of response was not reached at a median study follow-up of 27.6 months, with 41.7% of the responses maintained for ≥18 months. Median overall survival and progression-free survival were 13.9 and 4.1 months, respectively. Multivariable analyses adjusted for Eastern Cooperative Oncology Group performance status demonstrated that elevated LDH and target lesion SOD >median were independently correlated with ORR (p=0.008); patients with normal LDH and SOD <median had greater likelihood of response than those with either (OR=2.08) or both (OR=4.42) risk factors. The most common grade 3/4 treatment-emergent adverse events (≥30%) were thrombocytopenia (76.9%), anemia (50.0%), and febrile neutropenia (41.7%).
Conclusions
Investigational lifileucel demonstrated clinically meaningful activity in heavily pretreated patients with advanced melanoma and high tumor burden. Durable responses and a favorable safety profile support the potential benefit of one-time lifileucel TIL cell therapy in patients with limited treatment options in ICI-refractory disease.
Keywords: Immunotherapy; Melanoma; Clinical Trials, Phase II as Topic; Immunotherapy, Adoptive; Lymphocytes, Tumor-Infiltrating
WHAT IS ALREADY KNOWN ON THIS TOPIC
Adoptive cell therapy with tumor-infiltrating lymphocytes (TIL) is a promising anticancer therapy being investigated for patients with advanced solid tumors. Lifileucel, an investigational TIL cell therapy, has previously shown an investigator-assessed objective response rate (ORR) of 36% and median duration of response (DOR) not reached at a median follow-up of 33.1 months in 66 patients with advanced melanoma progressing after immune checkpoint inhibitors (ICI) and, if BRAF V600 mutation-positive, BRAF/MEK inhibitors.
WHAT THIS STUDY ADDS
This analysis reports clinically meaningful and durable activity of lifileucel, a novel one-time autologous TIL cell therapy, in the largest prospective, multicenter Phase 2 study in a population of patients with advanced melanoma in the post-ICI setting. Data from 153 lifileucel-treated patients, combining the previously reported 66 patients from Cohort 2 with the 87 previously unreported patients from Cohort 4, demonstrate a 31.4% ORR and median DOR not reached at a median study follow-up of 27.6 months.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The efficacy and safety of lifileucel, a new immunotherapy treatment option, combined with its short 22-day manufacturing duration, address an important unmet need in this patient population with traditionally difficult-to-treat disease who lack effective or approved treatment options in the post-ICI setting.
Background
An estimated 325,000 patients were diagnosed with melanoma worldwide in 2020, with approximately 57,000 deaths.1 Immune checkpoint inhibitors (ICI) and targeted therapies have revolutionized the treatment of advanced melanoma in the last decade; however, a substantial proportion of patients do not respond or eventually relapse, and treatment options are limited after progression. Many patients who receive first-line single or combination ICI progress by 12–18 months.2–4 Primary resistance to ICI is seen in 40%–65% of the patients2 5 6 and acquired resistance in 30%–40%.6–8 Moreover, occurrence of immune-related adverse events (irAEs) and subsequent discontinuation of ICI therapy is a clinical challenge.4 5 9 BRAF/MEK inhibitors are efficacious in patients with advanced melanoma,10–12 but only 35%–50% of these patients have relevant mutations that can be targeted,10 13 responses are often not durable, and disease progression may be rapid on relapse.10 11 14
Therapy after progression on ICI and BRAF/MEK inhibitor targeted treatment has shown limited benefit. Cytotoxic chemotherapy has a response rate of 4%–12%15–17 and median overall survival (OS) is ~7 months.17 Retreatment with ICI is a common practice, despite the lack of Food and Drug Administration approval in this setting and the general recommendation by the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology (NCCN Guidelines) to switch classes of agents and to consider treatments with a different mechanism of action (MOA) from previous therapies that were not efficacious.18 Reuse of ICI by treatment with anti-programmed cell death protein 1 (PD-1) and/or anti-cytotoxic lymphocyte-associated protein 4 (CTLA-4) after prior ICI failure has yielded response rates ranging from 8% to 29%,19–24 OS of 5–26 months,19–22 24 25 progression-free survival (PFS) of 3–5 months,19–22 and limited durations of response (DORs) in early-line and later-line patients20–22; similarly, the newer anti-lymphocyte activation gene 3 (LAG-3) and anti-PD-1 combination has also shown a modest response rate of 11.5% in the later setting.26 The recurrence of irAEs following rechallenge with ICI is also a concern27 28; in an analysis of patients restarting anti-PD-1 after experiencing severe irAEs on anti-PD-1 plus anti-CTLA-4 therapy, irAEs (any grade) were reported in 50% of the patients, and 30% discontinued treatment due to these AEs.28 Thus, a large unmet medical need exists for novel efficacious and safe treatment options with distinct MOA after ICI failure.
Adoptive cell therapy with tumor-infiltrating lymphocytes (TIL) has demonstrated promising antitumor activity in patients with advanced solid tumors,29–31 including melanoma refractory to ICI and BRAF/MEK inhibitors.32–36 The tumor microenvironment is replete with immunosuppressive metabolites (eg, adenosine, lactate), cytokines (eg, transforming growth factor-β), and cells (eg, regulatory T cells, tumor-associated macrophages, myeloid-derived suppressor cells) that collectively decrease cancer neoantigen-specific CD4+ and CD8+ T-cell (TIL) effector functions.37–39 Without sufficient quality and quantity of cells, endogenous TIL are thought to be ineffective in eliciting a robust antitumor immune response. Isolation, ex vivo expansion, and activation of TIL from patients with refractory disease reinvigorates the T cells by improving their phenotypic, functional, and tumor-reactive profile.40 41 Thus, the infused polyclonal TIL product is able to overcome immunosuppressive hurdles and induce robust immune-mediated tumor regression,42 43 while minimizing the selective pressure that is characteristic of single-antigen-targeting cell therapy strategies.44
Lifileucel (LN-144) is a one-time, autologous TIL cell therapy that uses TIL recovered from a patient’s tumor tissue to produce billions of polyclonal patient-specific TIL during a 22-day centralized manufacturing process.33 40 The TIL are a mix of CD8+ and CD4+ T cells45 of predominantly effector-memory phenotype, which is associated with cytotoxic function.40 45 Following a single infusion of lifileucel, TIL migrate to tumor sites throughout the body, where they recognize and target a multitude of individualized, tumor-associated neoantigens and mediate tumor cell lysis.33
In previously published analyses of the Phase 2 C-144-01 trial of patients with advanced melanoma (Cohort 2, N=66) who progressed after ICI and BRAF/MEK targeted therapies (if BRAF V600 mutation-positive), lifileucel demonstrated an investigator-assessed objective response rate (ORR) of 36%, median DOR not reached (NR) at a median follow-up of 33.1 months, and deepening responses over time.33 36 Following these positive data, we report here the results of the C-144-01 study in 153 sequentially enrolled patients, including longer-term follow-up of previously reported Cohort 2 (N=66) and the first report of Cohort 4 (N=87), which were pooled due to identical eligibility, lifileucel manufacturing process, treatment regimen, and central response assessment. Together, these data demonstrate lifileucel efficacy and safety in the largest prospectively enrolled Phase 2 study in a population of patients with advanced melanoma in the post-ICI setting.
Methods
Patients and study design
The C-144-01 trial (NCT02360579) is a prospective, Phase 2, multicohort, multicenter study in patients with advanced melanoma. Cohort 1 of the trial included patients receiving non-cryopreserved TIL generated using a manufacturing process different from that for lifileucel; patients in Cohort 2 and registrational Cohort 4 received cryopreserved lifileucel. Cohort 3 included patients from Cohorts 1, 2, and 4 who were retreated with lifileucel (online supplemental figure 1). This analysis focuses on sequentially enrolled Cohort 2 (April 2017 to January 2019) and Cohort 4 (February 2019 to December 2019).
jitc-2022-005755supp001.pdf (380.1KB, pdf)
Patients were ≥18 years of age with unresectable or metastatic melanoma (stage IIIC or stage IV) per the American Joint Committee on Cancer V.7.46 Patients had documented radiologic disease progression and must have progressed following ≥1 prior systemic therapy including a PD-1-blocking antibody, and if BRAF V600 mutation-positive, a BRAF or BRAF/MEK inhibitor (patients who were either primary or secondary refractory to prior anti-PD-1/programmed death ligand-1 (PD-L1) therapy were eligible); Eastern Cooperative Oncology Group performance status (ECOG PS) of 0 or 1; an estimated life expectancy of ≥3 months; adequate hematologic parameters and organ function; and ≥1 resectable lesion (or aggregate of lesions) providing resected tumor tissue ≥1.5 cm in diameter to generate lifileucel and ≥1 remaining measurable target lesion, as defined by Response Evaluation Criteria in Solid Tumors (RECIST) V.1.1. Patients with organ allograft or prior cell transfer therapy, uveal/ocular melanoma, hypersensitivity to lifileucel or other study drugs, symptomatic and/or untreated brain metastases, chronic systemic steroid therapy, active systemic infections, administration of live or attenuated vaccine within 28 days of non-myeloablative lymphodepletion (NMA-LD), and chronic heart or lung abnormality characterized by left ventricular ejection fraction <45% and forced expiratory volume in 1 s of ≤60% of the predicted value were excluded. Eligibility criteria were the same for Cohorts 2 and 4.33
The study was approved by the Institutional Review Board (IRB) at each site and was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines of the International Conference on Harmonization. The Strengthening the Reporting of Observational Studies in Epidemiology cohort reporting guidelines were used to ensure the quality of data reported in this study.47
Lifileucel manufacturing and infusion
Eligible patients underwent resection of a tumor(s) ≥1.5 cm to ≤4.0 cm in aggregate diameter, which was subsequently prosected (ie, trimmed and fragmented) and shipped to a centralized good manufacturing practice (GMP) facility to initiate lifileucel manufacturing. The 22-day GMP manufacturing process that results in a cryopreserved TIL infusion product has been previously described.33 The treatment regimen, consisting of NMA-LD (cyclophosphamide and fludarabine) followed by a single lifileucel infusion and an abbreviated course of high-dose interleukin-2 (IL-2), was administered as described previously.33 No bridging therapy was permitted between tumor resection and lifileucel infusion. The lifileucel manufacturing process and treatment regimen were the same for Cohorts 2 and 4.
Study endpoints and assessments
The original primary endpoint for Cohort 2 was investigator-assessed ORR.33 Cohort 4 was initiated as a single-arm registrational cohort with a prospectively defined primary endpoint of ORR by an independent review committee (IRC); accordingly, the primary endpoint of Cohort 2 was amended to IRC-assessed ORR. Pooled analysis for Cohorts 2 and 4 was not the pre-planned primary analysis; however, it was determined that this analysis would be of value given the identical eligibility, lifileucel manufacturing process, treatment regimen, and central response assessment for the two cohorts. Concordance between investigator-assessed and IRC-assessed ORR was analyzed. The secondary endpoints included DOR, OS, PFS, and safety as assessed by incidence rates, severity, seriousness, relationship to study treatment, and characteristics of treatment-emergent adverse events (TEAEs, defined as any AE with onset after lifileucel infusion through day 30 post-infusion).
Following the end-of-treatment visit, subsequent efficacy assessments occurred every 6 weeks (±3 days) until month 6 (week 24), and then every 3 months (12 weeks) for up to 5 years or until disease progression or start of new anticancer therapy. Survival assessment was conducted every 3 months via phone to obtain survival status and subsequent anticancer therapy information for up to 5 years or death, whichever occurred earlier. AE and serious AE data were graded as per the Common Terminology Criteria for Adverse Events V.4.03.
‘Primary refractory’ to anti-PD-1/PD-L1 therapy was defined as best response of progressive disease (PD) to prior anti-PD-1/PD-L1; the first anti-PD-1/PD-L1 with documented response was considered if multiple anti-PD-1/PD-L1 therapies were received. In a post hoc analysis, we also applied the Society for Immunotherapy of Cancer (SITC) Immunotherapy Resistance Taskforce criteria for ‘primary resistance.’48
Data were analyzed separately for each cohort as specified in the protocol and as a pooled analysis of the two cohorts to allow for subgroup analyses given identical eligibility, lifileucel manufacturing process, treatment regimen, and central response assessment.
Statistical analysis
Based on estimation of ORR using the maximum half width of the two-sided 95% CI of <13.2% when ORR is expected to be 20%– 50%, the planned sample size of Cohort 2 was 66 patients. The hypothesis testing for the primary endpoint of ORR in Cohort 4 as assessed by the IRC was prospectively defined as the null hypothesis of ORR ≤10% and alternative hypothesis of ORR >10%. The planned sample size for Cohort 4 was 75 patients, which would provide >90% power to demonstrate statistical significance at a two-sided overall significance level of 0.05 using the exact test and assuming that the true response rate for TIL cell therapy in this population was 25%. The IRC-assessed ORR was analyzed as a binomial proportion with two-sided confidence limits based on the Clopper-Pearson exact method at an overall alpha of 0.05. Time-to-event efficacy endpoints were estimated using Kaplan-Meier product limit method. Assessment of safety data was descriptive. Univariable logistic regression models were used to estimate odds ratios (ORs) with 95% CIs to assess the potential relationship between patient subgroups and ORR. Variables identified from the univariable analysis were examined using the best subset approach to identify independent predictors of ORR of lifileucel using a multivariable logistic regression model. All statistical analyses were conducted using the Statistical Analysis System (SAS) V.9.4.33
Results
Patients and treatment
Of 189 enrolled patients in the two cohorts, 156 received lifileucel TIL cell therapy infusion and formed the Safety Analysis Set (online supplemental figure 2); 25 patients did not receive lifileucel for patient-related reasons (PD (n=9, 4.8%), death (n=5, 2.6%), AE (n=3, 1.6%), new anticancer treatment (n=2, 1.1%), withdrawal of consent (n=1, 0.5%), withdrawal by patient (n=1, 0.5%), and other reason (n=4, 2.1%)), whereas lifileucel was not available for infusion for 8 patients (4.2%). The Full Analysis Set consisted of 153 patients (Cohort 2, N=66; Cohort 4, N=87) who were treated with 1×109–150×109 TIL cells that met the manufacturing product specification.
Baseline patient demographic and clinical characteristics are summarized in table 1. Most patients had cutaneous melanoma (n=83 (54.2%)); a minority had mucosal (n=12 (7.8%)) or acral (n=10 (6.5%)), and the remainder had either unknown primary or insufficient information (n=47 (30.7%)). At baseline, the median target lesion sum of diameters (SOD) was 97.8 mm, proportion of patients with >3 target and non-target lesions was 75.8%, and proportion of patients with lesions in ≥3 anatomic sites was 71.2%. Baseline liver and/or brain metastasis was reported for 47.1% of the patients. Elevated baseline lactate dehydrogenase (LDH) levels were observed in 54.2% of the patients, with LDH levels 1–2×upper limit of normal (ULN) in 35.3% and >2×ULN in 19.0% of the patients. Patients had received a median of 3.0 prior lines of therapy (range, 1–9). All patients had received prior anti-PD-1/PD-L1 therapy; 81.7% of the patients had also received anti-CTLA-4 therapy, and 53.6% had received combination anti-PD-1/anti-CTLA-4 therapy; 25.5% of the patients had received BRAF/MEK inhibitors. More than half of the patients (n=83 (54.2%)) were considered primary refractory to prior anti-PD-1/PD-L1 therapy. The median cumulative duration of anti-PD-1/PD-L1 therapy before lifileucel was 7 months. ICI retreatment was common; 73.9% (n=113) of patients were retreated with ICI and received a median of 2.0 lines (range, 1–7) of ICI-containing therapy (online supplemental figure 3).
Table 1.
Patient demographics and baseline characteristics of Cohorts 2, 4, and pooled Cohorts 2 and 4 (Full Analysis Set)
| Characteristic | Cohort 2 (n=66) | Cohort 4 (n=87) | Cohort 2+4 (N=153) |
| Median age, years (range) | 55.0 (20–79) | 58.0 (25–74) | 56.0 (20–79) |
| Sex, n (%) | |||
| Male | 39 (59.1) | 44 (50.6) | 83 (54.2) |
| Female | 27 (40.9) | 43 (49.4) | 70 (45.8) |
| Screening ECOG performance status, n (%) | |||
| 0 | 42 (63.6) | 62 (71.3) | 104 (68.0) |
| 1 | 24 (36.4) | 25 (28.7) | 49 (32.0) |
| Melanoma subtype,* n (%) | |||
| Cutaneous | 39 (59.1) | 44 (50.6) | 83 (54.2) |
| Mucosal | 4 (6.1) | 8 (9.2) | 12 (7.8) |
| Acral | 4 (6.1) | 6 (6.9) | 10 (6.5) |
| BRAF V600-mutated, n (%) | 17 (25.8) | 24 (27.6) | 41 (26.8) |
| PD-L1 status,† n (%) | |||
| TPS ≥1% | 37 (56.1) | 39 (44.8) | 76 (49.7) |
| TPS <1% | 12 (18.2) | 20 (23.0) | 32 (20.9) |
| Melanoma stage at study entry, n (%) | |||
| IIIC | 9 (13.6) | 1 (1.1) | 10 (6.5) |
| IV | 57 (86.4) | 86 (98.9) | 143 (93.5) |
| Liver and/or brain lesions by IRC, n (%) | 28 (42.4) | 44 (50.6) | 72 (47.1) |
| Median target lesion SOD (range), mm | 95.8 (13.5–271.3) | 99.5 (15.7–552.9) | 97.8 (13.5–552.9) |
| Baseline lesions in ≥3 anatomic sites, n (%) | 44 (66.7) | 65 (74.7) | 109 (71.2) |
| Baseline target and non-target lesions,‡ n (%) | |||
| ≤3 | 22 (33.3) | 14 (16.1) | 36 (23.5) |
| >3 | 43 (65.2) | 73 (83.9) | 116 (75.8) |
| LDH, n (%) | |||
| ≤ULN | 39 (59.1) | 31 (35.6) | 70 (45.8) |
| 1–2×ULN | 19 (28.8) | 35 (40.2) | 54 (35.3) |
| >2×ULN | 8 (12.1) | 21 (24.1) | 29 (19.0) |
| Prior systemic therapies, n (%) | |||
| Median number of therapies (range) | 3.0 (1–9) | 3.0 (1–8) | 3.0 (1–9) |
| Anti-PD-1/PD-L1 | 66 (100) | 87 (100) | 153 (100) |
| Anti-CTLA-4 | 53 (80.3) | 72 (82.8) | 125 (81.7) |
| Anti-PD-1 plus anti-CTLA-4 combination | 34 (51.5) | 48 (55.2) | 82 (53.6) |
| BRAF±MEK inhibitor | 15 (22.7) | 24 (27.6) | 39 (25.5) |
| IL-2 | 7 (10.6) | 6 (6.9) | 13 (8.5) |
| Primary refractory to anti-PD-1/PD-L1,§ n (%) | 42 (63.6) | 41 (47.1) | 83 (54.2) |
| Median cumulative duration of anti-PD-1/PD-L1 therapy before lifileucel (range), months | 5.1 (1.4–51.1) | 10.0 (0.7–75.8) | 7.0 (0.7–75.8) |
| Anatomic site of resection | |||
| Lymph node/skin/subcutaneous | 28 (42.4) | 43 (49.4) | 71 (46.4) |
| Visceral organ | 12 (18.2) | 30 (34.5) | 42 (27.5) |
| Other¶ | 26 (39.4) | 14 (16.1) | 40 (26.1) |
*Forty-seven patients (30.7%) had melanoma of other subtypes (including unknown primary subtype or insufficient information).
†Forty-five patients (29.4%) in the pooled cohorts had missing PD-L1 status.
‡One patient in Cohort 2 had missing data on the number of baseline target and non-target lesions.
§Primary refractory to anti-PD-1/PD-L1 was defined as patients who had best response of progressive disease to prior anti-PD-1/PD-L1; the first anti-PD-1/PD-L1 with documented response was considered if multiple anti-PD-1/PD-L1 therapies were received.
¶Other sites of resection included muscle, soft tissue, bone, limb/extremity, and others.
CTLA-4, cytotoxic T-lymphocyte–associated protein 4; ECOG, Eastern Cooperative Oncology Group; IL-2, interleukin 2; IRC, independent review committee; LDH, lactate dehydrogenase; PD-1, programmed cell death protein 1; PD-L1, programmed death ligand 1; SOD, sum of diameters; TPS, tumor proportion score; ULN, upper limit of normal.
The anatomic site of tumor resection for TIL manufacturing was lymph node/skin/subcutaneous (46.4%), visceral organ (27.5%), and other (26.1%; including muscle, soft tissue, bone, limb/extremity, and others). Of the 189 patients who had tumor resected, lifileucel manufacturing was terminated for two early patient withdrawals; of the remaining 187 patients, lifileucel was manufactured in 179 (95.7%; n=8, lifileucel not available) and within specification in 177 (94.7%). The median time from resection to lifileucel infusion was 33.0 days. The median number of TIL cells infused was 21.1×109 (range, 1.2×109–99.5×109). The median number of IL-2 doses administered was 6.0 (range, 0–6).
Efficacy
ORR and DOR
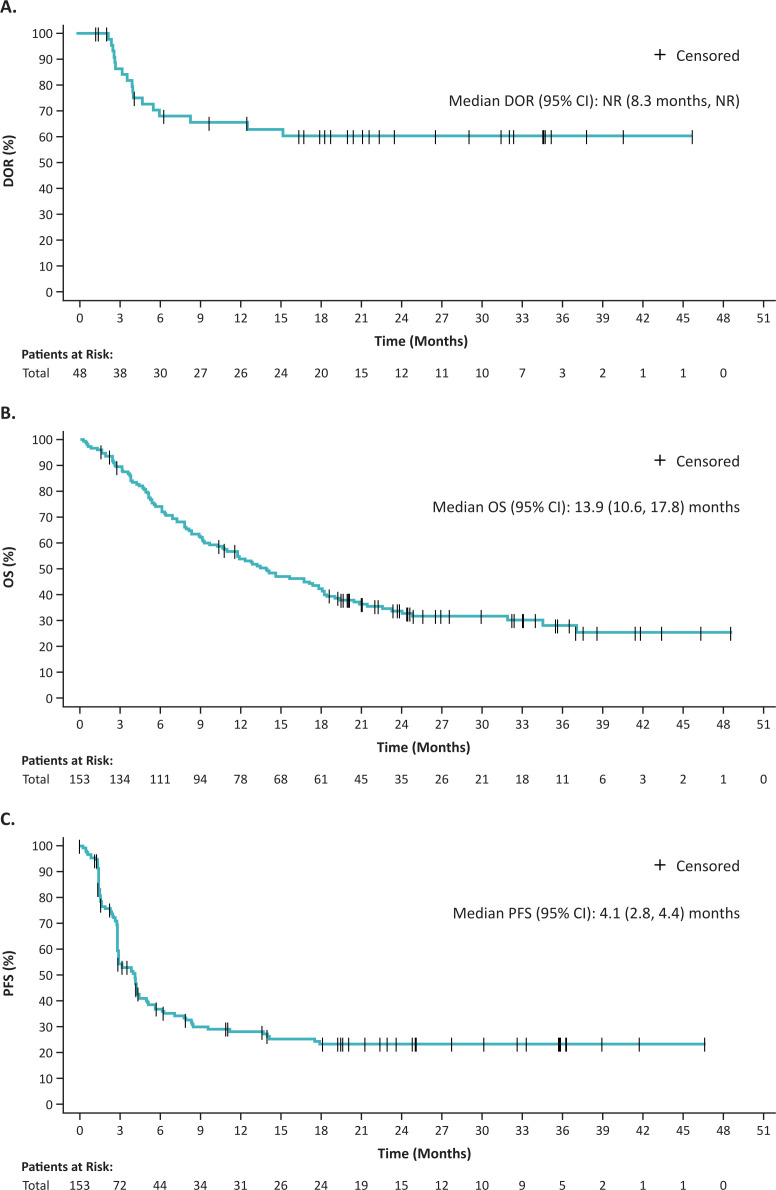
As of September 15, 2021, ORR as assessed by IRC was 31.4% (95% CI: 24.1% to 39.4%), with 8 complete responses (CRs) and 40 partial responses (PRs) (ORR for Cohort 2: 34.8% (95% CI: 23.5% to 47.6%); Cohort 4: 28.7% (95% CI: 19.5% to 39.4%); table 2). The concordance rate of IRC-assessed and investigator-assessed ORR for the pooled cohorts was 90.8% (Cohen’s Kappa coefficient 0.8 (95% CI: 0.7 to 0.9; p<0.0001). Of the 140 patients evaluable for changes of target lesion SOD, 78.6% (110/140) had SOD reduction (figure 1A). Median time from lifileucel infusion to best response was 1.5 months (range, 1.3–29.6 months; figure 1B). Thirty-nine (81.3%) responders had achieved an IRC-assessed response at the time of first response assessment. Six patients (12.5%) who were initially assessed as a PR achieved confirmed CR, and 10 patients (20.8%) improved from stable disease (SD) to PR. Response to lifileucel was observed across all subgroups analyzed (figure 1C), regardless of age, prior anti-CTLA-4 use, BRAF mutation status, PD-L1 status, and mucosal/non-mucosal subsets. In multivariable analyses adjusted for ECOG PS, elevated LDH and target lesion SOD >median were independently correlated with ORR (p=0.008); patients with normal LDH and SOD <median had greater likelihood of response than those with either (OR: 2.08) or both (OR: 4.42) of these risk factors.
Table 2.
Efficacy outcomes by IRC assessment for Cohorts 2, 4, and pooled Cohorts 2 and 4 (Full Analysis Set)
| Response (RECIST V.1.1)* | Cohort 2 (n=66) |
Cohort 4 (n=87) |
Pooled Cohorts 2+4 (N=153) |
| ORR, n (%) | 23 (34.8) | 25 (28.7) | 48 (31.4) |
| (95% CI) | (23.5 to 47.6) | (19.5 to 39.4) | (24.1 to 39.4) |
| Best overall response, n (%) | |||
| CR | 5 (7.6) | 3 (3.4) | 8 (5.2) |
| PR | 18 (27.3) | 22 (25.3) | 40 (26.1) |
| SD | 24 (36.4) | 47 (54.0) | 71 (46.4) |
| Non-CR/non-PD† | 1 (1.5) | 0 | 1 (0.7) |
| PD | 15 (22.7) | 12 (13.8) | 27 (17.6) |
| Non-evaluable‡ | 3 (4.5) | 3 (3.4) | 6 (3.9) |
| Median DOR,§ months (range) | NR (1.4+ to 45.0+)¶ | 10.4 (1.4+ to 26.3+) | NR (1.4+ to 45.0+) |
| Median study follow-up,** months | 36.6 | 23.5 | 27.6 |
*Objective response refers to patients with the best overall response of CR and PR. 95% CI for ORR was calculated using the Clopper-Pearson exact test.
†Patient did not have measurable target lesions by IRC and had best overall response of non-CR/non-PD per IRC assessment.
‡Six patients were non-evaluable for response (five due to early death; one due to new anticancer therapy).
§Based on responders and using Kaplan-Meier product-limit estimates.
¶Note: + refers to censored.
**Based on the reverse Kaplan-Meier method.
CR, complete response; DOR, duration of response; IRC, independent review committee; NR, not reached; ORR, objective response rate; PD, progressive disease; PR, partial response; RECIST, Response Evaluation Criteria in Solid Tumors; SD, stable disease.
Figure 1.
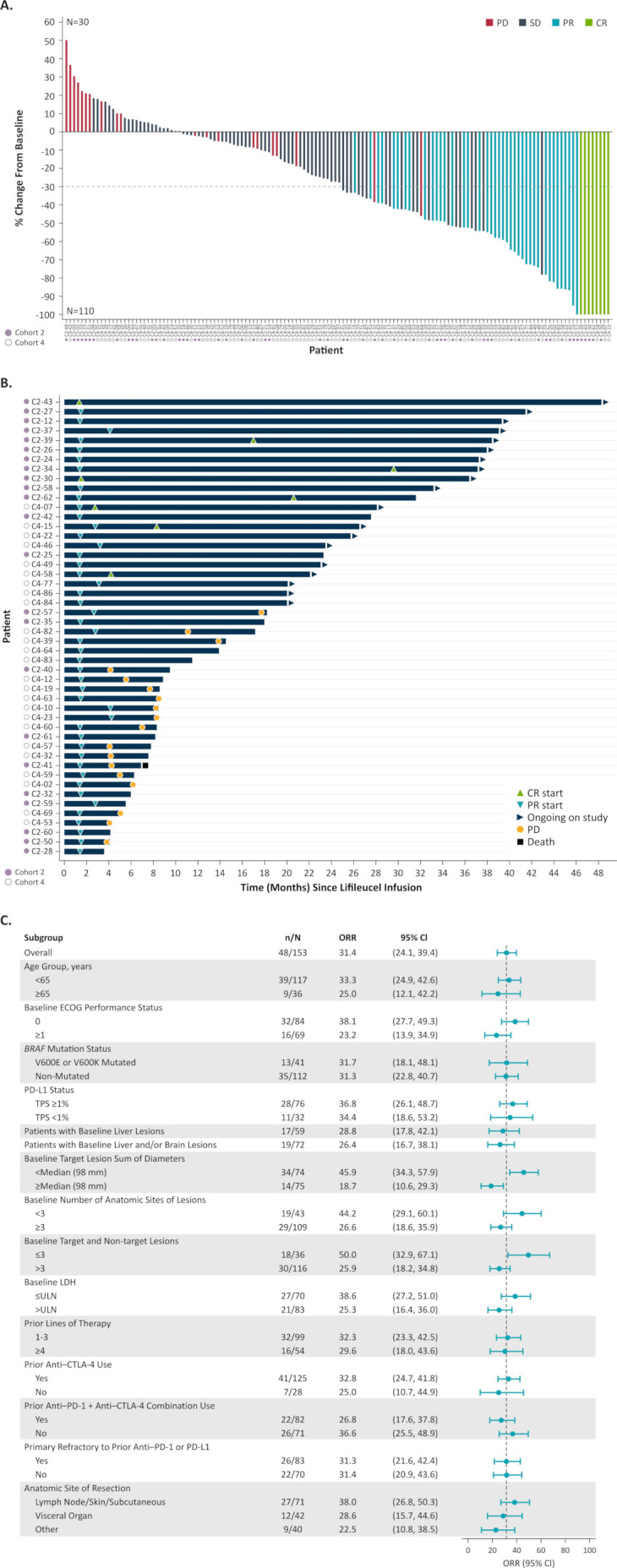
Efficacy outcomes for pooled Cohorts 2 and 4 (Full Analysis Set). (A) Best percentage change from baseline in target lesion SOD. Thirteen patients in the Full Analysis Set are not included (nine had no post lifileucel target lesion SOD measurements, and four had no acceptable target lesions by IRC). The horizontal dashed line indicates a 30% reduction in target lesion SOD. (B) Time to first response, DOR, and time on efficacy assessment for confirmed responders (PR or better). (C) ORR by subgroup per IRC assessment using the Response Evaluation Criteria in Solid Tumors V.1.1 criteria. 95% CI is calculated using the Clopper-Pearson exact test. CR, complete response; CTLA-4, cytotoxic T lymphocyte-associated protein 4; DOR, duration of response; ECOG, Eastern Cooperative Oncology Group; IRC, Independent Review Committee; LDH, lactate dehydrogenase; ORR, objective response rate; PD, progressive disease; PD-1, programmed cell death protein 1; PD-L1, programmed death-ligand 1; PR, partial response; SD, stable disease; SOD, sum of diameters; TPS, tumor proportion score; ULN, upper limit of normal.
Median DOR was NR (95% CI: 8.3 months to NR) at a median study follow-up of 27.6 months (Cohort 2: NR (95% CI: NR to NR); Cohort 4: 10.4 months (95% CI: 4.1 to NR); figure 2A); 41.7% of the patients had responses maintained for ≥18 months, and 39.6% of the responses were ongoing at the time of data cut.
Figure 2.
DOR in confirmed responders (PRor better) by IRC assessment per Response Evaluation Criteria in Solid Tumors V.1.1 (A), OS (B), and PFS (C) for pooled Cohorts 2 and 4. DOR, duration of response; IRC, independent review committee, NR, not reached; OS, overall survival; PFS, progression-free survival; PR, partial response.
Survival
The median OS was 13.9 months (95% CI: 10.6 to 17.8) (figure 2B), and 12-month OS rate was 54.0% (95% CI: 45.6% to 61.6%). In an analysis of survival by response at 1.5 months after lifileucel infusion (first planned response evaluation), the median OS in responders was NR (95% CI: 22.5 months to NR) (online supplemental figure 4). The median PFS was 4.1 months (95% CI: 2.8 to 4.4) (figure 2C); the 12-month PFS rate was 28.3% (95% CI: 20.8% to 36.3%).
Post hoc analyses
In the subset of 83 patients who were primary refractory to prior anti-PD-1/PD-L1 therapy by study criteria, lifileucel produced an ORR of 31.3% (95% CI: 21.6% to 42.4%), with 6 CRs (7.2%) and 20 PRs (24.1%). Forty (48.2%) of these patients had best response to lifileucel of SDor non-CR/non-PD, and 13 (15.7%) had PD; four patients were non-evaluable. Median DOR was NR (95% CI: 15.1 months to NR) for this subpopulation. Using SITC Immunotherapy Resistance Taskforce criteria, 109 patients (71.2%) were considered primary resistant to prior anti-PD-1/PD-L1 therapy, with an ORR of 33.0% (95% CI: 24.3% to 42.7%) and median DOR NR (95% CI: 12.5 months to NR).
In patients who received prior anti-PD-1 and anti-CTLA-4 combination, the ORR was 26.8%, and median DOR was NR (95% CI: 4.1 months to NR). In patients who received any prior anti-CTLA-4 treatment, the ORR for lifileucel was 32.8%, and in patients who received anti-CTLA-4 therapy as last treatment prior to lifileucel, ORR was 31.8%.
There was no difference in TIL dose manufactured across anatomic sites of resection (online supplemental figure 5A). Target lesion SOD reductions were seen across the range of total TIL doses (online supplemental figure 5B).
Safety
All patients in the Safety Analysis Set (N=156) experienced ≥1 TEAE (any grade) during the course of the study. Grade 3/4 TEAEs occurring in ≥30% of the patients included thrombocytopenia (76.9%), anemia (50.0%), and febrile neutropenia (41.7%) (table 3). The TEAE profile was consistent with the underlying disease and known safety profiles of NMA-LD and IL-2 regimens and was similar between cohorts. Anaphylactic and infusion-related reactions that were reported by the investigator as related to lifileucel specifically were seen in 2 (1.3%; grade 3/4) and 6 (3.8%; grade 1/2) patients, respectively. Six deaths occurred within 30 days after infusion, four of which were attributed to AEs and two to PD. Of the four grade 5 TEAEs, three were assessed by the investigator as not related to lifileucel but related to NMA-LD and/or IL-2 (ie, pneumonia, arrhythmia, acute respiratory failure) and one as related to all components of the regimen (ie, intra-abdominal hemorrhage). Tumors were resected from diverse sites with minimal surgical morbidity; grade 3/4 tumor-resection AEs related to surgery were seen in 6 (3.2%) patients (online supplemental table 1).
Table 3.
TEAEs occurring in ≥30% of the patients (Safety Analysis Set (N=156))*
| Preferred term, n (%) | Any grade | Grade 3/4 |
| Thrombocytopenia | 129 (82.7) | 120 (76.9) |
| Chills | 117 (75.0) | 8 (5.1) |
| Anemia | 97 (62.2) | 78 (50.0) |
| Fever | 81 (51.9) | 17 (10.9) |
| Neutropenia† | 66 (42.3) | 45 (28.8) |
| Febrile neutropenia | 65 (41.7) | 65 (41.7) |
| Hypophosphatemia | 58 (37.2) | 41 (26.3) |
| Leukopenia† | 54 (34.6) | 42 (26.9) |
| Hypotension | 52 (33.3) | 17 (10.9) |
| Fatigue | 51 (32.7) | 6 (3.8) |
| Lymphopenia† | 49 (31.4) | 38 (24.4) |
| Diarrhea | 48 (30.8) | 2 (1.3) |
*Other relevant events: Grade 3/4 TEAEs commonly observed with cellular therapies or IL-2 included immune effector cell-associated neurotoxicity syndrome and cytokine release syndrome (investigator-assessed, no confirmatory serum cytokine levels measured) in one patient, and capillary leak syndrome (due to IL-2) in seven patients. Grade 3/4 uveitis was reported in three patients.
†All patients had grade 4 laboratory abnormality per the Common Terminology Criteria for Adverse Events V.4.03 for leukopenia, neutropenia, and lymphopenia during the treatment-emergent period. Only clinically significant laboratory abnormalities as per investigators were reported as adverse events.
IL-2, interleukin-2; TEAE, treatment-emergent adverse event.
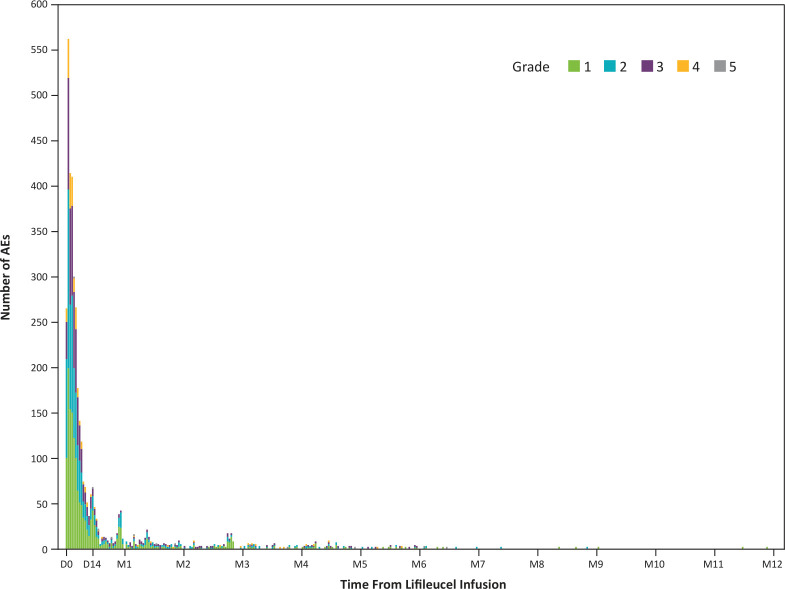
Most TEAEs were expected and manageable, and the incidence decreased rapidly over the first 2 weeks after lifileucel infusion (figure 3).
Figure 3.
Incidence of AEs over time (Safety Analysis Set).* All occurrences of AEs were counted if a patient experienced a new onset of the same AE at different time points. If multiple records were reported on the electronic case report form because of toxicity grade decrease of the same AE that had not been resolved, then the event was counted once with the highest grade reported. *Fourteen events were reported after month 12 (grade 1, n=6; grade 2, n=6; grade 3, n=1, grade 5, n=1). AE, adverse event; D, day; M, month.
Discussion
TIL cell therapy has emerged as a promising option to treat advanced ICI-refractory solid tumors due to the polyclonal nature of the infusion product targeting different tumor antigens, which is thought to attenuate the potential for immune escape via loss of target antigen expression by neoplastic cells.49 However, few prospective studies have investigated the efficacy and safety of TIL cell therapy after disease progression on ICI and targeted therapy, the current standards of care in advanced melanoma. In the current Phase 2 trial that included 153 patients enrolled in two consecutive cohorts in the ICI era, one-time lifileucel treatment using cryopreserved products demonstrated an ORR of 31.4% and median DOR was NR at a median study follow-up of 27.6 months—a marked improvement over the therapies available for patients in the post-ICI setting. Durability of responses and deepening of responses over time are consistent with ongoing antitumor activity of persisting tumor-specific TIL clones, further supporting the use of lifileucel as a novel treatment option in this patient population to address a highly unmet need.
Existing and recently approved therapies have shown limited benefit in the post-ICI setting in advanced melanoma. Studies assessing combination anti-CTLA-4 and anti-PD-1 therapy after anti-PD-1/PD-L1 therapy failure have been performed in ipilimumab-naïve patients21 or have included patients whose disease has progressed after adjuvant anti-PD-1 treatment only22 and sometimes used immune-related RECIST criteria-based responses. The patients in these studies were generally not as heavily pretreated as those in the present study, thus precluding efficacy comparisons. The recently approved combination of anti-LAG3 and anti-PD-1 antibodies (relatlimab plus nivolumab) and investigational anti-LAG3 antibody, fianlimab, in combination with cemiplimab have shown only modest response rates when administered as second-line treatment after progression on ICI therapy.26 50 Similarly modest response rates were observed in a small retrospective analysis of second-line anti-CTLA-4 therapy after progression on first-line relatlimab and nivolumab, suggesting emergence of cross-resistance to subsequent therapy after disease progression on ICI.51
In the context of these recent data and the lack of data from appropriately sized prospective, multicenter, independently reviewed RECIST-based studies in this setting, an ORR of 31.4% with lifileucel, with nearly half of the responses maintained ≥18 months in heavily pretreated patients in the post-ICI and targeted therapy (where indicated) setting, is encouraging. Further, in patients who achieved a response at 1.5 months after lifileucel infusion (time of first efficacy assessment), median OS was NR, suggesting that early response to lifileucel may be predictive of long-term outcomes and may be a good indicator of sensitivity, in contrast to ICI where imaging results at a similar time point can be misleading.52
In the present study, some notable differences were observed in the baseline characteristics of patients in the later-enrolled Cohort 4 compared with Cohort 2, which included a higher proportion of patients with >3 lesions, elevated LDH, and liver and/or brain metastasis. In addition, patients in Cohort 4 received nearly twice the cumulative duration of prior anti-PD-1/PD-L1 therapy. These indicators of greater disease burden and more difficult-to-treat disease in Cohort 4, many of which are well-known negative prognostic factors for response and survival in patients with advanced melanoma treated with ICI,53 54 may have contributed to the differences in the ORR point estimates and median DOR, although the 95% CI were overlapping.
Although the eligibility criteria (same for Cohorts 2 and 4) allowed for patients to receive lifileucel after progression on first-line ICI, the median number of prior lines of therapy was 3.0. As illustrated in online supplemental figure 3, most patients received multiple regimens of ICI-based therapy prior to receiving lifileucel. In addition, as shown in multivariable analyses, favorable clinical characteristics of lower tumor burden (ie, target lesion SOD <median, normal LDH) are associated with greater likelihood of response. The ORR of 31.4% in heavily pretreated patients in this study is encouraging compared with response rates of 29% in patients treated with anti-CTLA-4 and anti-PD-1 therapy after first-line ICI treatment failure.21 The use of lifileucel after first progression on ICI may thus represent a unique opportunity to intervene with a one-time therapy that can lead to durable responses.
Patients whose disease progresses after combination ICI therapy and BRAF/MEK inhibitors (when appropriate) have no effective therapeutic options that give clinically meaningful results. Lifileucel was efficacious in this subset of patients (ORR: 26.8%), which constituted 53.6% of the entire cohort, and thus, lifileucel could be considered as their next line of therapy.
In addition, the ORR was 31.3% in the subset of patients who were primary refractory to anti-PD-1/PD-L1 therapy per the study criteria, consistent with earlier observations.33 Notably for patients with disease defined as primary resistant per the SITC Immunotherapy Resistance Taskforce,48 the ORR was 33.0%, and median DOR was NR (95% CI: 12.5 months to NR). The efficacy of lifileucel in these patient subsets suggests that lifileucel is a viable option for patients progressing after first-line ICI monotherapy and in those progressing after combination therapy.
Recently, the Netherlands Cancer Institute reported results of a randomized Phase 3 clinical trial of autologous, in vitro expanded, non-cryopreserved TIL compared with ipilimumab in 168 patients with unresectable or metastatic melanoma who had received a maximum of one prior line of systemic therapy (86% had received prior anti-PD-1 therapy (first-line or adjuvant)). This study met its primary endpoint with a 6-month PFS rate of 53% in patients treated with TIL cell therapy compared with 21% in those treated with ipilimumab. An ORR of 49% was seen with TIL cell therapy compared with 21% with ipilimumab.55 Consistent with these earlier-line clinical findings, biological findings, particularly anti-PD-1-induced immunoediting, loss of neoantigens and neoantigen presentation, and associated relative paucity of neoantigen-reactive cells within final TIL products of patients with prior anti-PD-1 exposure,34 56 57 add weight to consideration of intervention with lifileucel early in the treatment course.
In the recent DREAMseq trial, ICI therapy (nivolumab/ipilimumab) preceding BRAF/MEK inhibitors (dabrafenib/trametinib) yielded a substantially higher 2-year OS rate (72%), longer median DOR (NR), and higher rate of ongoing responses (88%) compared with patients who received BRAF/MEK inhibitors preceding ICI therapy (2-year OS: 52%, median DOR: 12.7 months, ongoing responses: 51%).58 Adoption of ICI use before BRAF/MEK inhibitors based on this study has been a paradigm shift in the management of advanced melanoma. A long-term follow-up analysis of patients treated by the National Cancer Institute Surgery Branch going back to the pre-ICI and BRAF tyrosine kinase inhibitor era showed an inverse relationship between response to TIL and prior anti-PD-1 therapy or BRAF/MEK inhibitors.34 A higher rate of durable responses and melanoma-specific survival was demonstrated, especially in the ICI-naïve population receiving TIL, driven by firm biological rationale as recently shown by Levi et al.56 In PD-1 inhibitor-naïve patients, treatment with lifileucel in combination with pembrolizumab produced an ORR of 60% (CR rate, 30%),35 supporting the potential for improved response rates, including CR rates, with earlier TIL cell therapy. Nevertheless, lifileucel produced durable responses and a favorable safety profile across subgroups of heavily pretreated patients with high tumor burden, regardless of age, BRAF mutation status, PD-L1 status, baseline ECOG PS status, and presence of liver and/or brain lesions at baseline, which supports a potential benefit for a broad population of patients with melanoma.
In line with prior reports,32 33 TEAEs were consistent with the known safety profiles of NMA-LD and IL-2, with a majority of TEAEs occurring within the first 2 weeks post-lifileucel infusion and no new safety signals reported in the combined analysis. The transient and manageable nature of AEs support the potential benefit of one-time treatment with lifileucel.
Lifileucel was successfully manufactured for 94.7% of the eligible resected tumors, reflecting the ability to manufacture lifileucel using tumors from diverse anatomic sites and supporting the feasibility and scalability of the 22-day GMP process. The short-duration manufacturing process (compared with a historical production time of 5–7 weeks59) may benefit patients who have exhausted all approved treatment options. Rapid transition of TIL cell therapy from clinical trials into clinical practice will allow broader access, and the success of the treatment regimen will require close coordination across multidisciplinary teams, including surgeons, medical oncologists, and cell therapy physicians. Surgical best practices for tumor resection for TIL manufacturing are well established to address possible practice variations.60 Further innovation is underway to develop TIL regimens that use IL-2 analogs to enhance antitumor responses by continuous support of growth and activity of the infused TIL product, but also mitigate the toxicities associated with currently available recombinant IL-2. Moreover, efforts to reduce the doses of available cytotoxic agents or develop novel lymphodepletion regimens may allow for broader use.
This single-arm, non-randomized, uncontrolled, non-blinded study design has its inherent limitations that preclude comparative assessment of the observed PFS and OS. In addition, the post hoc pooled analyses were intended to strengthen the results and allow for more meaningful subgroup analyses, given that eligibility criteria and the clinical intervention remain unchanged across the two cohorts.
In summary, one-time treatment with lifileucel TIL cell therapy demonstrated clinically meaningful activity in heavily pretreated patients with advanced melanoma with a high tumor burden and advanced disease in a larger population and with a longer follow-up duration, consistent with data from the previously published Cohort 2. Responses were durable and AEs were transient and manageable in a population with traditionally difficult-to-treat disease that currently has no approved treatments. These findings thus support the potential of lifileucel to fulfill a large unmet medical need for novel therapeutic options distinct from ICI in patients with advanced melanoma.
jitc-2022-005755supp002.pdf (368.4KB, pdf)
Acknowledgments
The authors would like to thank the participating patients and their families. Medical writing support was provided by Jayasri Srinivasan and Swati Ghatpande of Second City Science, a Vaniam Group Company, and funded by Iovance Biotherapeutics.
Footnotes
Twitter: @melanoma_doctor, @ajsfurness
Contributors: JC, HK, EW, WS, XW, FGF, and AS contributed to conception and design of the study. KDL, MW, MC, ED-M, GQP, JCH, MO, JL, JW, AJSF, NIK, TM, and MEE were involved in the provision of study materials or patients. JC, KDL, HK, OH, EW, ST, MW, ED-M, GQP, JMK, MO, JW, NIK, TM, PH, GS, WS, XW, and AS contributed to collection and assembly of data. JC, HK, OH, EW, ST, MW, MC, ED-M, JMK, JCH, JL, AJSF, NIK, MEE, FGF, MJ, PH, GS, WS, XW, and AS contributed to data analysis and interpretation. All authors were involved in manuscript writing and have read and approved the final manuscript. FGF acts as the guarantor and takes full responsibility for the work and/or the conduct of the study, has access to the data, and controls the decision to publish.
Funding: This study is sponsored by Iovance Biotherapeutics.
Competing interests: JC reports consulting or advisory role with Amgen and research funding from Replimune, Amgen, Iovance Biotherapeutics, and Fate Therapeutics. KDL reports receiving honoraria from Array BioPharma and Iovance Biotherapeutics; consulting or advisory role with Array BioPharma, Merck, Roche, Regeneron, Sanofi, Iovance Biotherapeutics, and Nektar; research funding from Roche/Genentech, Merck, Array BioPharma, Incyte, Nektar, Iovance Biotherapeutics, Bristol-Myers Squibb, Kartos Therapeutics, OncoSec, Regeneron, Alkermes, Neon Therapeutics, Ultimovacs, Senhwa Biosciences, Replimune, Amgen, and Seagen; travel, accommodations, and expenses from Merck, Roche/Genentech, Regeneron, Neon Therapeutics, and Alkermes; and uncompensated relationships with Roche/Genentech and Regeneron. HK reports consulting or advisory role with Bristol-Myers Squibb, Clinigen, Shionogi, Chemocentryx, Calithera, Signatera, GigaGen, GI Reviewers, and Merck; and research funding from Apexigen, Bristol-Myers Squibb, and Merck. OH reports receiving honoraria and has consulting or advisory role with Aduro, Akeso, Alkermes, Amgen, BeiGene, BioAtla, Bristol-Myers Squibb, Roche Genentech, GlaxoSmithKline, Immunocore, Idera, Incyte, InstilBio, Iovance Biotherapeutics, Janssen, Merck, Nextcure, Novartis, Pfizer, Sanofi/Regeneron, Seagen, Tempus, and Zelluna; research funding from Arcus, Aduro, Akeso, Amgen, Bioatla, Bristol-Myers Squibb, CytomX, Exelixis, Roche Genentech, GSK, Immunocore, Idera, Incyte, Iovance Biotherapeutics, Merck, Moderna, Merck-Serono, NextCure, Novartis, Pfizer, Rubius, Sanofi-Regeneron, and Seagen; and is on the speaker’s bureau for Bristol-Myers Squibb, Novartis, Pfizer, and Sanofi Regeneron. EW reports consultant or advisory role with Merck; research funding received as site principal investigator for multiple studies (>30); and being on the speaker’s bureau for Bristol-Myers Squibb, Regeneron, and Castle Biosciences. ST reports honoraria, consulting or advisory role, research funding, speaker’s bureau, and travel, accommodations, expenses with Bristol-Myers Squibb, Merck, Pfizer, Ipsen, Amgen, Genentech, and Foundation One. MW reports receiving honoraria from Novartis, Pfizer, and Roche; consulting or advisory role with Bristol-Myers Squibb, Novartis, Pfizer, Cellex GmbH, Eli Lilly, Boehringer Ingelheim, ISA Pharmaceuticals, GEMoaB, Roche, MSD, AstraZeneca, Amgen, and Immatics; research funding from Roche; and travel, accommodations, and expenses from Pfizer, Bristol-Myers Squibb, AstraZeneca, Roche, Amgen, and GEMoaB. MC reports speaker’s bureau participation with Sirtex Medical. ED-M reports receiving honoraria from Castle Biosciences; consulting or advisory role and speaker’s bureau with Regeneron; and research funding from Clinigen. GQP reports honoraria from IBSA; consulting or advisory role with Acella, Amneal, and Terns; and patents, royalties, or other intellectual property with Virginia Commonwealth University. JMK reports consulting role with Amgen, Ankyra Therapeutics, Applied Clinical Intelligence, Axio Research, Becker Pharmaceutical Consulting, Bristol-Myers Squibb, Cancer Network, Checkmate Pharmaceuticals, DermTech, Fenix Group International, Harbour BioMed, Immunocore, Iovance Biotherapeutics, IQVIA, Istari Oncology, Merck, Natera, Novartis, Oncocyte, OncoSec, Pfizer, Replimune, Scopus BioPharma, SR One Capital Management LP, Takeda Development Center Americas, and Takeda Pharmaceutical Company; and research trial support to institution from Amgen, Bristol-Myers Squibb, Checkmate Pharmaceuticals, Harbour BioMed, ImmVira, Immunocore, Iovance Biotherapeutics, Novartis, Takeda, and Verastem. JCH reports honorarias for talks from Almirall, Amgen, Bristol-Myers Squibb, GSK, JSD Pharma, Novartis, Pierre Fabre, Roche, Sanofi, and Sun Pharma; advisory boards for GSK, MSD, Pierre Fabre, Sun Pharma (personal), and Bristol-Myers Squibb, Immunocore, Nektar, Novartis, and Philogen (institution); research funding from Bristol-Myers Squibb, Sun Pharma, and Sanofi; and travel, accommodations, and expenses from Sun Pharma. MO reports consulting or advisory role with TriSalus, Immunocore, Ideaya, and Delcath, and her husband is an employee of GSK. JL reports receiving honoraria from Eisai, Novartis, Incyte, Merck, touchIME, touchEXPERTS, Royal College of Physicians, Cambridge Healthcare Research, Royal College of General Practitioners, VJOncology, Agence Unik, and Bristol-Myers Squibb; consulting or advisory role with iOnctura, Apple Tree, Merck, Bristol-Myers Squibb, Eisai, Debiopharm, and Incyte; research funding from Bristol-Myers Squibb, MSD, Novartis, Pfizer, Achilles Therapeutics, Roche, Nektar, Covance, Immunocore, Pharmacyclics, and Aveo; and travel, accommodations, and expenses from Pierre Fabre, Roche, and GSK. JW reports stock or other ownership with Biond, Instil Bio, OncoV4, and Evaxion; honoraria and consulting or advisory role with Bristol-Myers Squibb, GSK, Pfizer, Sellas, Biond, OncoC4, ImCheck, Genentech, AstraZeneca, Regeneron, Instil Bio, Iovance Biotherapeutics, Evaxion, and Ultimovacs; research funding from Bristol-Myers Squibb, Moderna, Merck, Incyte, and Genentech; patents, royalties, or other intellectual property with Moffitt Cancer Center and Biodesix. AJSF reports consulting or advisory role with Immunocore and GSK; speaker’s bureau participation with Bristol-Myers Squibb, Ipsen, and Eisai; and travel, accommodations, and expenses from ESMO. NIK reports stock and other ownership interest with Bellicum Pharmaceuticals, Amarin Corporation, and Asensus Surgical; consulting or advisory role with Bristol-Myers Squibb, AstraZeneca, Regeneron, Array BioPharma, Immunocore, Merck, Incyte, Jounce Therapeutics, Iovance Biotherapeutics, NCCN/Pfizer, Genzyme, Novartis, Nektar, Castle Biosciences, and InstilBio; research funding from Bristol-Myers Squibb, Merck, Novartis, GSK, HUYA Bioscience International, Amgen, Regeneron, Celgene, and Replimune; and other relationships with Nektar, Regeneron, Bristol-Myers Squibb/Celgene, and Replimune. TM reports consulting or advisory role with Merck, Bristol-Myers Squibb, Iovance Biotherapeutics, Moderna, Nektar, Regeneron, Exicure, Checkmate Pharmaceuticals, BioAtla, Xencor, Replimune, Day One Biopharmaceuticals, Pfizer, and Taiga. MEE reports consultant or advisory role with Iovance Biotherapeutics and receiving research funding from SkylineDx. FGF, MJ, PH, GS, WS, and XW are employees of Iovance Biotherapeutics and hold stock and/or stock options. Further, FGF is in a leadership position at Iovance Biotherapeutics; owns stocks from Adverum Biotechnologies, Roche, Bristol-Myers Squibb, and Johnson & Johnson; and holds patents, royalties, or other intellectual property rights with Bristol-Myers Squibb. PH additionally reports receiving honoraria from Janssen, Amgen, Karyopharm, Bristol-Myers Squibb, and Sanofi; has been paid for a consultant or advisory role by Janssen, Amgen, Karyopharm, Bristol-Myers Squibb, and Allogen; and received travel, accommodations, and expenses from Johnson & Johnson, Bristol-Myers Squibb, and Sanofi. AS reports honoraria and consulting or advisory role with Iovance Biotherapeutics, Guidepoint, Defined Health, Huron Consulting Group, KeyQuest Health, Istari, Gerson Lehrman Group, Physicians’ Educational Resource, Medscape and MedStar Health; and holds patents, royalties, or other intellectual property rights with Moffitt Cancer Center, Iovance Biotherapeutics, and Provectus.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Providence Health & Services Institutional Review Board (IRB) (PDX15-117); Atlantic Health System IRB (763583); Advarra IRB (PRE00076076); Yale University IRB #2, 3, 4B, 5, 6—Human Investigation Committee IB Oncology, II, III, IV, 1A (1506016045); Western IRB (20160198); University of Louisville IRB (16.0817 (initial approval reference ID: 748942)); Mount Sinai Medical Center IRB (16-49-H-09 (Federalwide Assurance #FWA00000179)); NYU School of Medicine IRB (i16-00804); Sutter Health IRB—(SHIRB) (2016.124 (IRB Net # 931782)); Orlando Health IRB #1 (1092019 (reference: 17.069.060); Human Research Protection Program, University of Minnesota (STUDY00001236); UC San Diego Human Research Protections Program (171801); Thomas Jefferson University Institutional Review Board (17C.598); Fred Hutchinson Cancer Research Center IRB (9925); Roswell Park Cancer Institute IRB (STUDY00000465/P54117); Medical College of Wisconsin/ Froedtert Hospital IRB—Human Research Protection Program (PRO00031199); Office of the Human Research Protection Program (OHRPP) (IRB#19-000538); University of Miami Human Subject Research Office (HSRO)—IRB (IRB ID: 20190926); CEIm HM Hospitales (Tracked w EudraCT# - 2017-000760-15); Egészségügyi Tudományos Tanács Klinikai Farmakológiai Etikai Bizottsága (OGYEI/47943-5/2017); Comité de Protection des Personnes (CPP) Sud-Ouest et Outre Mer III (Tracked w EudraCT#- 2017-000760-15); London—West London & GTAC Research Ethics Committee (EudraCT#- 2017-000760-15; MHRA: 48580; IRAS: 229812; REC: 17/LO/1471); Ethikkommission der Medizinischen Fakultät der Technischen Universität München (Tracked w EudraCT#- 2017-000760-15); and Commission Cantonale d'Éthique de la Recherche sur l'Étre Humain (CER-VD) (2017-02031). Participants gave informed consent to participate in the study before taking part.
References
- 1.Arnold M, Singh D, Laversanne M, et al. Global burden of cutaneous melanoma in 2020 and projections to 2040. JAMA Dermatol 2022;158:495–503. 10.1001/jamadermatol.2022.0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Long GV, Robert C, Butler MO, et al. Standard-Dose pembrolizumab plus Alternate-Dose ipilimumab in advanced melanoma: KEYNOTE-029 cohort 1C, a phase 2 randomized study of two dosing schedules. Clin Cancer Res 2021;27:5280–8. 10.1158/1078-0432.CCR-21-0793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Postow MA, Goldman DA, Shoushtari AN, et al. Adaptive dosing of nivolumab + ipilimumab immunotherapy based upon early, interim radiographic assessment in advanced melanoma (the ADAPT-IT study). J Clin Oncol 2022;40:1059–67. 10.1200/JCO.21.01570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tawbi HA, Schadendorf D, Lipson EJ, et al. Relatlimab and nivolumab versus nivolumab in untreated advanced melanoma. N Engl J Med 2022;386:24–34. 10.1056/NEJMoa2109970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015;373:23–34. 10.1056/NEJMoa1504030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mooradian MJ, Sullivan RJ. What to do when anti-PD-1 therapy fails in patients with melanoma. Oncology 2019;33:141–8. [PubMed] [Google Scholar]
- 7.Hamid O, Robert C, Daud A, et al. Five-year survival outcomes for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. Ann Oncol 2019;30:582–8. 10.1093/annonc/mdz011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 2017;377:1345–56. 10.1056/NEJMoa1709684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Betof Warner A, Palmer JS, Shoushtari AN, et al. Long-term outcomes and responses to retreatment in patients with melanoma treated with PD-1 blockade. J Clin Oncol 2020;38:1655–63. 10.1200/JCO.19.01464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dummer R, Ascierto PA, Gogas HJ, et al. Encorafenib plus binimetinib versus vemurafenib or encorafenib in patients with BRAF-mutant melanoma (COLUMBUS): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2018;19:603–15. 10.1016/S1470-2045(18)30142-6 [DOI] [PubMed] [Google Scholar]
- 11.Sosman JA, Kim KB, Schuchter L, et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med 2012;366:707–14. 10.1056/NEJMoa1112302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robert C, Grob JJ, Stroyakovskiy D, et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N Engl J Med 2019;381:626–36. 10.1056/NEJMoa1904059 [DOI] [PubMed] [Google Scholar]
- 13.Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol 2011;29:1239–46. 10.1200/JCO.2010.32.4327 [DOI] [PubMed] [Google Scholar]
- 14.Mason R, Heng S, Atkinson V. Outcomes following progression on BRAF/MEK inhibition in metastatic melanoma. J Clin Oncol 2017;35:9537–37. [Google Scholar]
- 15.Keytruda . Prescribing information, 2021. [Google Scholar]
- 16.Weber JS, D'Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 2015;16:375–84. 10.1016/S1470-2045(15)70076-8 [DOI] [PubMed] [Google Scholar]
- 17.Goldinger SM, Buder-Bakhaya K, Lo SN, et al. Chemotherapy after immune checkpoint inhibitor failure in metastatic melanoma: a retrospective multicentre analysis. Eur J Cancer 2022;162:22–33. 10.1016/j.ejca.2021.11.022 [DOI] [PubMed] [Google Scholar]
- 18.© National Comprehensive Cancer Network, Inc . Referenced with permission from the NCCN clinical practice guidelines in oncology (NCCN Guidelines®) for melanoma, cutaneous V.2.2022, 2022To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. [Google Scholar]
- 19.Cybulska-Stopa B, Rogala P, Czarnecka AM, et al. Efficacy of ipilimumab after anti-PD-1 therapy in sequential treatment of metastatic melanoma patients - Real world evidence. Adv Med Sci 2020;65:316–23. 10.1016/j.advms.2020.05.005 [DOI] [PubMed] [Google Scholar]
- 20.Larkin J, Minor D, D'Angelo S, et al. Overall survival in patients with advanced melanoma who received nivolumab versus investigator's choice chemotherapy in CheckMate 037: a randomized, controlled, open-label phase III trial. J Clin Oncol 2018;36:383–90. 10.1200/JCO.2016.71.8023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olson DJ, Eroglu Z, Brockstein B, et al. Pembrolizumab plus ipilimumab following Anti-PD-1/L1 failure in melanoma. J Clin Oncol 2021;39:2647–55. 10.1200/JCO.21.00079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vanderwalde AM, Moon J, Kendra K, et al. Abstract CT013: S1616: ipilimumab plus nivolumab versus ipilimumab alone in patients with metastatic or unresectable melanoma that did not respond to anti-PD-1 therapy. Cancer Res 2022;82:CT013. 10.1158/1538-7445.AM2022-CT013 [DOI] [Google Scholar]
- 23.Zimmer L, Apuri S, Eroglu Z, et al. Ipilimumab alone or in combination with nivolumab after progression on anti-PD-1 therapy in advanced melanoma. Eur J Cancer 2017;75:47–55. 10.1016/j.ejca.2017.01.009 [DOI] [PubMed] [Google Scholar]
- 24.Chapman PB, Jayaprakasam VS, Panageas KS, et al. Risks and benefits of reinduction ipilimumab/nivolumab in melanoma patients previously treated with ipilimumab/nivolumab. J Immunother Cancer 2021;9:e003395. 10.1136/jitc-2021-003395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kirchberger MC, Hauschild A, Schuler G, et al. Combined low-dose ipilimumab and pembrolizumab after sequential ipilimumab and pembrolizumab failure in advanced melanoma. Eur J Cancer 2016;65:182–4. 10.1016/j.ejca.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 26.Ascierto PA, Bono P, Bhatia S, et al. Efficacy of BMS-986016, a monoclonal antibody that targets lymphocyte activation gene-3 (LAG-3), in combination with nivolumab in PTS with melanoma who progressed during prior anti–PD-1/PD-L1 therapy (MEL prior io) in all-comer and biomarker-enriched populations. Annals of Oncology 2017;28:v611–2. 10.1093/annonc/mdx440.011 [DOI] [Google Scholar]
- 27.Haanen J, Ernstoff M, Wang Y, et al. Rechallenge patients with immune checkpoint inhibitors following severe immune-related adverse events: review of the literature and suggested prophylactic strategy. J Immunother Cancer 2020;8:e000604. 10.1136/jitc-2020-000604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollack MH, Betof A, Dearden H, et al. Safety of resuming anti-PD-1 in patients with immune-related adverse events (irAEs) during combined anti-CTLA-4 and anti-PD1 in metastatic melanoma. Ann Oncol 2018;29:250–5. 10.1093/annonc/mdx642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jazaeri AA, Zsiros E, Amaria RN. Safety and efficacy of adoptive cell transfer using autologous tumor infiltrating lymphocytes (LN-145) for treatment of recurrent, metastatic, or persistent cervical carcinoma. J Clin Oncol 2019;37:2538–38. [Google Scholar]
- 30.Jimeno A, Papa S, Haigentz M. 353 Safety and efficacy of tumor infiltrating lymphocytes (TIL, LN-145) in combination with pembrolizumab for advanced, recurrent or metastatic HNSCC. J Immunother Cancer 2020;8:A215–6. [Google Scholar]
- 31.Schoenfeld A, Lee S, Paz-Ares L. 458 First phase 2 results of autologous tumor-infiltrating lymphocyte (TIL; LN-145) monotherapy in patients with advanced, immune checkpoint inhibitor-treated, non-small cell lung cancer (NSCLC). J Immunother Cancer 2021;9:A486–7. [Google Scholar]
- 32.Rosenberg SA, Yang JC, Sherry RM, et al. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res 2011;17:4550–7. 10.1158/1078-0432.CCR-11-0116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarnaik AA, Hamid O, Khushalani NI, et al. Lifileucel, a tumor-infiltrating lymphocyte therapy, in metastatic melanoma. J Clin Oncol 2021;39:2656–66. 10.1200/JCO.21.00612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seitter SJ, Sherry RM, Yang JC, et al. Impact of prior treatment on the efficacy of adoptive transfer of tumor-infiltrating lymphocytes in patients with metastatic melanoma. Clin Cancer Res 2021;27:5289–98. 10.1158/1078-0432.CCR-21-1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Malley D, Lee S, Psyrri A. 492 Phase 2 efficacy and safety of autologous tumor-infiltrating lymphocyte (TIL) cell therapy in combination with pembrolizumab in immune checkpoint inhibitor-naïve patients with advanced cancers. J Immunother Cancer 2021;9:A523–4. [Google Scholar]
- 36.Larkin J, Sarnaik A, Chesney JA, et al. Lifileucel (LN-144), a cryopreserved autologous tumor infiltrating lymphocyte (TIL) therapy in patients with advanced melanoma: evaluation of impact of prior anti-PD-1 therapy. JCO 2021;39:9505–05. 10.1200/JCO.2021.39.15_suppl.9505 [DOI] [Google Scholar]
- 37.Chen Y, Song Y, Du W, et al. Tumor-associated macrophages: an accomplice in solid tumor progression. J Biomed Sci 2019;26:78. 10.1186/s12929-019-0568-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Groth C, Hu X, Weber R, et al. Immunosuppression mediated by myeloid-derived suppressor cells (MDSCs) during tumour progression. Br J Cancer 2019;120:16–25. 10.1038/s41416-018-0333-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vaupel P, Multhoff G. Accomplices of the hypoxic tumor microenvironment compromising antitumor immunity: adenosine, lactate, acidosis, vascular endothelial growth factor, potassium ions, and phosphatidylserine. Front Immunol 2017;8:1887. 10.3389/fimmu.2017.01887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simpson-Abelson MR, D’Arigo K, Hilton F, et al. 1053P Iovance generation-2 tumour-infiltrating lymphocyte (TIL) product is reinvigorated during the manufacturing process. Annals of Oncology 2020;31:S720. 10.1016/j.annonc.2020.08.1173 [DOI] [Google Scholar]
- 41.Owens GL, Price MJ, Cheadle EJ, et al. Ex vivo expanded tumour-infiltrating lymphocytes from ovarian cancer patients release anti-tumour cytokines in response to autologous primary ovarian cancer cells. Cancer Immunol Immunother 2018;67:1519–31. 10.1007/s00262-018-2211-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morotti M, Albukhari A, Alsaadi A, et al. Promises and challenges of adoptive T-cell therapies for solid tumours. Br J Cancer 2021;124:1759–76. 10.1038/s41416-021-01353-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin B, Du L, Li H, et al. Tumor-infiltrating lymphocytes: warriors fight against tumors powerfully. Biomed Pharmacother 2020;132:110873. 10.1016/j.biopha.2020.110873 [DOI] [PubMed] [Google Scholar]
- 44.Sterner RC, Sterner RM. CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J 2021;11:69. 10.1038/s41408-021-00459-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ritthipichai K, Frank I, Machin M. 32Nd annual meeting and Pre-Conference programs of the Society for immunotherapy of cancer (SITC 2017): Part one. National Harbor, MD, USA 8-12 2017;5:86. November 2017. [Google Scholar]
- 46.Edge SB BD, Compton CC, Fritz AG. AJCC cancer staging manual. New York: Springer, 2010. [Google Scholar]
- 47.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 48.Kluger HM, Tawbi HA, Ascierto ML, et al. Defining tumor resistance to PD-1 pathway blockade: recommendations from the first meeting of the SITC immunotherapy resistance Taskforce. J Immunother Cancer 2020;8:e000398. 10.1136/jitc-2019-000398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maeurer MJ, Gollin SM, Martin D, et al. Tumor escape from immune recognition: lethal recurrent melanoma in a patient associated with downregulation of the peptide transporter protein TAP-1 and loss of expression of the immunodominant MART-1/Melan-A antigen. J Clin Invest 1996;98:1633–41. 10.1172/JCI118958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamid O, Wang D, Kim TM. Clinical activity of fianlimab (REGN3767), a human anti-LAG-3 monoclonal antibody, combined with cemiplimab (anti-PD-1) in patients (PTS) with advanced melanoma. J Clin Oncol 2021;39:9515–15. [Google Scholar]
- 51.Menzies AM, Pires da Silva I, Trojaniello C, et al. CTLA-4 blockade resistance after Relatlimab and nivolumab. N Engl J Med 2022;386:1668–9. 10.1056/NEJMc2119768 [DOI] [PubMed] [Google Scholar]
- 52.Hodi FS, Hwu W-J, Kefford R, et al. Evaluation of immune-related response criteria and RECIST v1.1 in patients with advanced melanoma treated with pembrolizumab. J Clin Oncol 2016;34:1510–7. 10.1200/JCO.2015.64.0391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Robert C, Ribas A, Hamid O, et al. Durable complete response after discontinuation of pembrolizumab in patients with metastatic melanoma. J Clin Oncol 2018;36:1668–74. 10.1200/JCO.2017.75.6270 [DOI] [PubMed] [Google Scholar]
- 54.Wagner NB, Lenders MM, Kühl K, et al. Pretreatment metastatic growth rate determines clinical outcome of advanced melanoma patients treated with anti-PD-1 antibodies: a multicenter cohort study. J Immunother Cancer 2021;9. 10.1136/jitc-2021-002350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.JBAG H, Rohaan MW, Borch TH. Treatment with tumor-infiltrating lymphocytes (TIL) versus ipilimumab for advanced melanoma: results from a multicenter, randomized phase trial. ESMO Congress Paris 2022. [Google Scholar]
- 56.Levi ST, Copeland AR, Nah S, et al. Neoantigen identification and response to adoptive cell transfer in anti-PD-1 naïve and experienced patients with metastatic melanoma. Clin Cancer Res 2022;28:3042–52. 10.1158/1078-0432.CCR-21-4499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kluger HM, Sarnaik A, Chesney JA. Tumor mutational burden (TMB) in immune checkpoint inhibitor (ICI)-naïve and -experienced patients with metastatic melanoma treated with lifileucel, a tumor-infiltrating lymphocyte (TIL) cell therapy. J Clin Oncol 2022;40:9524–24. [Google Scholar]
- 58.Atkins MB, Lee SJ, Chmielowski B. DREAMseq (doublet, randomized evaluation in advanced melanoma sequencing): a phase III trial—ECOG-ACRIN EA6134. J Clini Oncol 2021;39:356154–54. [Google Scholar]
- 59.Wu R, Forget M-A, Chacon J, et al. Adoptive T-cell therapy using autologous tumor-infiltrating lymphocytes for metastatic melanoma: current status and future outlook. Cancer J 2012;18:160–75. 10.1097/PPO.0b013e31824d4465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mullinax JE, Egger ME, McCarter M, et al. Surgical considerations for tumor tissue procurement to obtain tumor-infiltrating lymphocytes for adoptive cell therapy. Cancer J 2022;28:285–93. 10.1097/PPO.0000000000000608 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2022-005755supp001.pdf (380.1KB, pdf)
jitc-2022-005755supp002.pdf (368.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.