Abstract
Background:
Falls are the third highest reported safety incident in Specialist Palliative Care in-patient settings and yet specific risk factors connected with falling and associated outcomes in this setting are poorly understood.
Aim:
To understand the key individualised risk factors leading to falls in specialist in-patient palliative care settings and understand the implications and outcomes for the patients who fall.
Design:
A realist synthesis of the literature, reported following the Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) standards.
Data sources:
An iterative literature search was conducted across three recognised health collections as well as grey literature from policy, practice and other relevant areas.
Results:
Falls taking place within in-patient specialist palliative care settings can cause significant harm to patients. The risk factors for these patients are multifaceted and often interlinked with underpinning complex realist mechanisms including a history of falls, the age of the person, impact of complex medications, improving functional status and the presence of delirium.
Conclusion:
In-patients in specialist palliative care settings are at risk of falling and this is multifactorial with complex reasoning mechanisms underpinning the identified risks. There is a significant impact of a fall in this cohort of patients with many sustaining serious harm, delayed discharge and both physical and psychological impacts.
Keywords: Fall, palliative care, hospice, risk
What is already known about the topic
Falls are the third most prevalent safety incident in specialist palliative care in-patient units
Short and long-term prognosis for older patients following a serious harm fall is generally poor.
There is a wide breadth of knowledge regarding falls in older people.
What this paper adds
A realist approach identifies that there are underpinning mechanisms to the risks associated with a fall event and aims to elucidate the causes and effects of these mechanisms.
Patients are more likely to fall if they have a history of falls; if they take multiple medicines (needed for symptom control); if they are older; if their functional status is not stable and if they have delirium or cognitive impairments.
This cohort of patients have wide ranging medical and social backgrounds and will be at various stages in their disease trajectory, making the identification of those most susceptible to falls challenging.
There is no clear disease or age specific falls risk for these patients.
Implications for practice, theory or policy
People receiving care from in-patient specialist palliative care services are at high risk of a fall event occurring and sustaining significant harm either physically, psychologically, or both and the risk factors are multifactorial and complex.
Much of the current guidance relating to this cohort of people is based on policy and evidence for older people but not all the risk factors and outcomes are directly transferable due to the differences between the two specialities in regards age profiles, co-morbidities such as frailty, functional status, prognosis and disease treatment effects and trajectory.
This unique group have specific risks and needs including the combination of complex medication regimens, risk of delirium and fluctuating functional status that should be identified to allow adaptation and care planning to reduce the incidence and impact of fall events.
Background
Patient safety has gained increased prominence in palliative and end of life care in recent years1 and an analysis of reported serious incidents identified that falls are the third greatest safety incident in UK in-patient hospices after pressure ulcers and medicine errors.2 Falls have also been recognised by patients and family members as being a key concern in in-patient specialist palliative care.3 Falls prevention for this group, including combining the use of predictive falls assessment tools and clinical judgement has become a priority4 with multiple factors known to exacerbate the risk of experiencing a fall present in many of these patients.5,6 Despite this increased prominence, specific risk factors connected with falling and associated outcomes in this setting are poorly understood in specialist in-patient palliative care settings, defined as a specialist service delivered by multidisciplinary health care professionals with expertise in providing or coordinating comprehensive palliative care for patients whose complex needs cannot be met by their usual care team.7–9 This setting differs to generalist palliative care, which is delivered by healthcare providers who are not specialists in end of life care but work in other fields including primary care or other acute specialities.10
The limited literature base on the subject of fall events for people who are being cared for in specialist palliative care in-patient units has not been previously synthesised, with much of the literature base that has previously been utilised to inform palliative care policy and practice based on older people, including those in care homes, community and hospital settings. This is challenging as the two specialities of palliative care and older peoples’ medicine (or geriatric medicine) are distinct and, in many ways, different from one another in terms of the breadth of patients age, co-morbidities, prognosis and disease trajectory.11
Aims
The aim of this paper is to synthesise the literature using a realist approach to understand:
- the key risk factors that lead to people falling in specialist in-patient palliative care settings
- the implications and outcomes for people who fall whilst receiving care in specialist in-patient units.
- the theoretically and empirically most probable explanations for the patterns reported across studies.
Rationale for a realist review
Realist methodology considers practice to be occurring within complex open systems,12 where it is impossible to draw direct causal links between interventions (e.g. a falls prevention policy) and outcomes (a reduction in falls) without understanding the underpinning causal mechanisms and exploring how they work and under what conditions.13 A realist synthesis approach has multiple iterative and overlapping steps with the aim of continually developing and refining explanatory programme theories utilising existing and available evidence.14 Such explanatory theories take the shape of context-mechanism (resource, reasoning)-outcome configurations, which are the unit of analysis of a realist synthesis.15
Falls in palliative care in-patient settings is a complex and multi-faceted area of study and as such the use of a realist synthesis is appropriate to develop and refine causal links16 between the practice contexts within which patients fall, the interventions and mechanisms that lead to falls and whether those could be prevented, and the outcomes for these patients. Together, these encompass an understanding of why patients fall, which patients are susceptible to falls and the impact of falling.
Methods
The review was carried out in 2021 by a research team consisting of a PhD student and three experienced supervisors. We follow the Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) reporting standards for realist and meta-narrative evidence synthesis.16
Step 1: Developing the research question
Our professional insights and a brief initial literature review led to the formulation of the following questions: ‘Why do patients fall in in-patient palliative care settings?’, ‘Which patients are most susceptible to falls and why?’ and ‘What are the impacts of falling for the individual?’
Step 2: Exploratory literature scoping and initial programme theories
The initial scoping exercise, which included a wider breadth of papers than was included in this specific realist review including generalist falls literature, in addition to extensive clinical expertise and experience of the authors, led to the creation of nine Initial Programme Theories which were refined throughout the synthesis process, with a tenth added later in the process of analysis.
Step 3: Systematic literature search
The search was undertaken using CINAHL (Cumulative Index to Nursing and Allied Health Literature), AMED (Allied and Complementary Medicine) and Health Research Premium Collection (includes MEDLINE, Nursing and Allied Health Collections and other broad collections of relevant journals). Appropriate and defined search strings, incorporating recognised Boolean operators, were developed using key concepts from overarching broad themes reflective of the Initial Programme Theories. Searches were performed using detailed search strings that can be briefly summarised as ‘Medication as a risk factor for falls’, ‘Age and functionality as a risk factor for a fall’, ‘Medical history /diagnosis as a risk factor for a fall’ and ‘Independence or failure to seek support as a risk factor for falls’. Detailed search strings are provided in Supplemental Material 1. Grey literature was included from searches in Google Scholar and a wider internet search to elucidate any further papers, presentations and toolkits relating to falls risk and in-patient palliative care.
Step 4: Selection and appraisal
Inclusion and exclusion criteria (Table 1) were applied to ensure the synthesis was founded on evidence for specialist in-patient palliative care only. Inclusion criteria were used to identify papers where falls information such as risk factors, incidence and outcome information was included to ensure relevance to the search.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| Papers including data from specialist in-patient palliative care settings | Papers based on settings other than Specialist In-Patient Palliative Care |
| Papers which include data covering falls risk factors, falls incidence and/or the outcome of sustaining a fall. | No mention of fall related events, outcomes or risk factors. |
| Studies published from 2000 onwards | Studies published prior to the year 2000 |
| English language only | Not reported in English language |
Quality assessment of qualitative papers was performed using a Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields.17 Quality assessment in a realist synthesis does not inform decision making but supports a transparent approach to the validity and reliability of the review.18 No papers were excluded as part of the Quality Assessment. A simultaneous critical appraisal of all papers was conducted to support with weighting of shortlisted papers.
Step 5: Data extraction, analysis and synthesis
Data were extracted against the broad themes highlighted by the Initial Programme Theories, so that elements of the papers that were confirming, disconfirming, or suggesting refinement of the theory were highlighted against it. As is customary in realist synthesis, data extraction was a systematic and iterative process of documentation and refinement of theories, followed by further reading and extraction where needed. All papers were screened on several occasions to ensure that where possible, saturation of information was achieved. In realist synthesis, data extraction and analysis happen concurrently, with programme theories being refined in response to findings from the literature, until all new evidence confirms the theories as they are formulated.19 The analysis followed a retroductive approach utilising both an inductive process of creating theory from the papers reviewed and a deductive approach of starting from theory and testing the assumptions. Retroductive approaches require the researcher to not only use theory but also professional insights and hunches.20 The Initial Programme Theories are described with a summary of the evidence obtained and an analysis of their implications for the proposed theory.
Findings
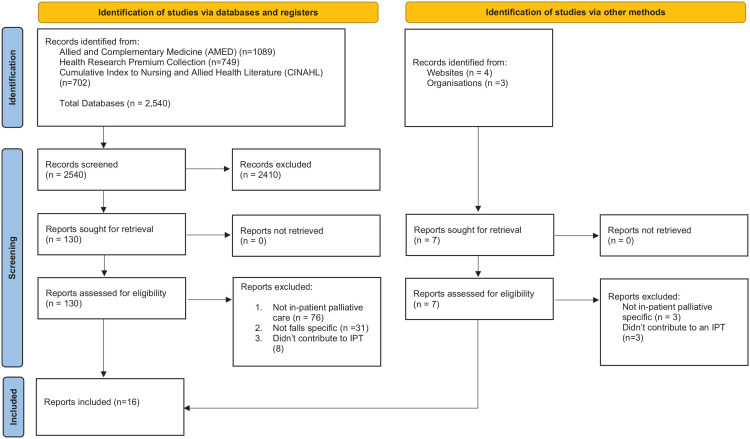
In total, 2540 records were identified from the database searches, from which 15 reports were included in the final review (Figure 1) plus one piece of grey evidence, giving a total of 16 reports. The final 16 reports consisted of retrospective data reviews (n = 4), prospective observational studies (n = 4), expert opinions (n = 3), mixed methods studies (n = 2), observational cohort study (n = 1), systematic review (n = 1), and a Toolkit (n = 1). Most reports were from UK/Europe (n = 8) and North America (n = 7). The other country was in Asia (n = 1). Table 2 presents the characteristics of included studies, and Table 3 presents the results of the search in relation to the Initial Programme Theories formulated as Context-Mechanism-Outcome (CMO) configurations. The following section presents the Initial Programme Theories, the corresponding evidence, and any subsequent changes to the Theories following data synthesis.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Table 2.
Study characteristics.
| Author | Country | Design | Sample size | Quality assessment score |
|---|---|---|---|---|
| Duncan et al.23 | USA | Retrospective data review | 186,904 patients | 22 (100%) |
| Goodridge and Marr22 | Canada | Retrospective data review | 357 patients | 21 (96%) |
| Gray5 | USA | Expert Opinion | n/a | n/a |
| Hospice UK28 | UK | Toolkit | n/a | n/a |
| Ishøy and Steptoe30 | Denmark | Prospective Observational Study | 89 Patients (135 fall incidents) | 19 (86%) |
| Jansen et al.24 | Norway | Systematic Literature Review | 12 studies | n/a |
| Krashin et al.27 | USA | Expert Opinion | n/a | n/a |
| Leland et al.32 | USA | Observational Cohort Study | 14,400 patients | 20 (91%) |
| Maeda et al.29 | Japan | Prospective Observational Study | 756 patients | 22 (100%) |
| Pautex et al.26 | Switzerland | Retrospective data review | 198 patients | 20 (91%) |
| Patrick et al.4 | USA | Retrospective data review | 3446 patients | 21 (96%) |
| Pearse et al.25 | UK | Mixed Methods | 102 patients | 22 (100%) |
| Pegram et al.31 | UK | Expert Opinion | n/a | n/a |
| Schonwetter et al.6 | USA | Prospective Observational Study | 200 patients | 22 (100%) |
| Stone et al.21 | UK | Prospective Observational Study | 185 patients | 21 (96%) |
| Yardley et al.2 | UK | Mixed Methods | 475 reports | 20 (91%) |
Table 3.
Summary of the context mechanism outcome configuration records.
| Initial Programme Theory | Context | Mechanism (Resource) | Mechanism (Reasoning) | Outcome | Evidence Summary | Evidence design and country |
|---|---|---|---|---|---|---|
| A. | Patients in a palliative care setting | who have previously fallen have a reduced functional status | as a result of the first fall (physical or psychological harm) | Are likely to fall again | Goodridge and Marr22
Gray5 Patrick et al.4 Schonwetter et al.6 Stone et al.21 |
Retrospective data review (n = 2), Expert Opinion (n = 1), Prospective observational study (n = 2) USA (n = 3), Canada (n = 1), UK (n = 1) |
| B. | Patients in a palliative care setting | Who are prescribed more than 5 medicines | Which cause impaired mobility and/or cognition | Are at increased risk of falling | Duncan et al.23
Goodridge and Marr22 Pautex et al.26 Patrick et al.4 Pearse et al.25 Schonwetter et al.6 Jansen et al.24 |
Retrospective data review (n = 4), Mixed Methods (n = 1), Prospective observational study (n = 1), Systematic Review (n = 1) USA (n = 3), Canada (n = 1), UK (n = 1), Europe (n = 2) |
| C. | Patients in a palliative care setting | Who are prescribed benzodiazepines | Have impaired cognition | Are at increased risk of falling | Krashin et al.27
Pautex et al.26 Pearse et al.25 Schonwetter et al.6 Stone et al.21 |
Retrospective data review (n = 1), Expert Opinion (n = 1), Mixed Methods (n = 1), Prospective observational study (n = 2) USA (n = 2), UK (n = 2), Europe (n = 1) |
| D. | Patients in a palliative care setting | Who experience delirium | Have cognitive impairment, inability to follow instructions or experience acute distress | Are at increased risk of falling | Goodridge and Marr22
Hospice UK28 Maeda et al.29 Pautex et al.26 Pearse et al.25 |
Retrospective data review (n = 2), Mixed Methods (n = 2), Toolkit (n = 1) UK (n = 2), Europe (n = 1), Asia (n = 1), Canada (n = 1) |
| E. | Patients in a palliative care setting | Who are over the age of 65 | Have impaired mobility and/or cognition | Are at increased risk of falling | Pearse et al.25 | Mixed Methods (n = 1) UK (n = 1), |
| F. | Patients in a palliative care setting | Who are over the age of 65 | Have impaired mobility/weakness | Are at increased risk of harm from a fall | Goodridge and Marr22
Ishoy et al.30 Patrick et al.4 Pearse et al.25 Schonwetter et al.6 |
Retrospective data review (n = 2), Mixed Methods (n = 1), Prospective observational study (n = 2) USA (n = 2), UK (n = 1), Europe (n = 1), Canada (n = 1) |
| G. | Patients in a palliative care setting | Who have elimination or continence needs | Have an urgency to use the toilet or in inability to request help and mobilise independently | Are at increased risk of falling | Goodridge and Marr22
Ishoy et al.30 |
Retrospective data review (n = 1), Prospective observational study (n = 1) Europe (n = 1), Canada (n = 1) |
| H. | Patients in a palliative care setting | Who have poor functional status | Have weakness and impaired mobility | Are more likely to fall | Goodridge and Marr22
Hospice UK28 Ishoy et al.30 Patrick et al.4 Schonwetter et al.6 Pegram et al.31 |
Retrospective data review (n = 2), Prospective observational study (n = 2), Toolkit (n = 1), Expert Opinion (n = 1) USA (n = 2), UK (n = 2), Europe (n = 1), Canada (n = 1) |
| I. | Patients in a palliative care setting | Who have a diagnosis of advanced/metastatic cancer | Have fatigue/reduced functional status /polypharmacy | Are at increased risk of falling | Pautex et al.26
Patrick et al.4 Stone et al.21 |
Retrospective data review (n = 2), Prospective observational study (n = 1), USA (n = 1), UK (n = 1), Europe (n = 1), |
| J. | In a palliative care setting | Falls prevention is a priority | Patients wish to maintain independence | Patients continue to fall | Schonwetter et al.6 | Prospective Observational study (n = 1), USA (n = 1) |
| K. | Patients in a palliative care setting | Who sustain a fall | Have complex disease processes, a fear of further deterioration in condition and functional status | Will be adversely affected and at increased risk of mortality and morbidity | Goodridge and Marr22
Gray5 Ishoy et al.30 Leland et al.32 Pautex et al.26 Patrick et al.4 Pearse et al.25 Schonwetter et al.6 Stone et al.21 Yardley et al.2 |
Retrospective data review (n = 3), Observational Cohort Study (n = 1), Expert Opinion (n = 1), Mixed Methods (n = 2), Prospective observational study (n = 3) USA (n = 4), UK (n = 3), Europe (n = 2). Canada (n = 1) |
A. Previous fall
After a fall, patients have increased pain and disability.5 A history of falls prior to admission is a significant risk factor for a fall during the admission (p = 0.022)6 and patients who have fallen frequently in the last year are more likely to fall again (p = 0.01),6 with a history of previous falls being one of the most important determinants of future falls in hospice care.4,6,21 Indeed, 63.3% of patients who fell during their admission had also fallen in another setting before admission.22 The evidence supports the notion that this Initial Programme Theory is important in determining risk of falls in an in-patient specialist palliative care population and associated outcomes, although further understanding is required of the underpinning mechanism. Taking this evidence into account, the refined programme theory reads: Patients in a specialist palliative care setting (Context) who have previously fallen are more likely to fall again (Outcome) because they have reduced functional status (Resource) as a result of the first fall (physical or physiological) (Reasoning).
B. Polypharmacy
The average specialist palliative care in-patient has 16.9 prescriptions representing 3.5 classes of medication and so if medicines do affect falls risk or incidence then this population of patients at particular risk,23 although this has been disputed in the literature.24 Two of the papers found no association between the number or type of medicines and falls risk,6,25 and that opioids had an inverse relationship to falls risk. However, it must be noted that the Schonwetter6 study reviewed cognitively intact patients only and it is unknown whether this would change if cognitively impaired patients were included. It was identified that there is no difference in number of medications being taken between patients who fell once and those who fell repeatedly.22 A further two papers found some correlation between number of medication and falls, although the significance of this varied (p ⩽ 0.0014 vs p = 0.426). In addition, it was found that people who fall were more likely to have received neuroleptics (p = 0.035).26 It has been highlighted that there are potential effects of medicines on cognition,6 which might explain the different findings described. The evidence supporting this Initial Programme Theory is therefore less clear and demonstrates a requirement for further research. While polypharmacy may be an important factor in determining risk of falls in an inpatient palliative care unit, this is not at present consistently supported by the literature. The initial programme theory has been refined as: Patients in a specialist palliative care setting (Context) who are prescribed more than five medicines (Resource) are at increased risk of falling (Outcome) because of impaired mobility and/or cognition (Reasoning).
C. Impaired cognition
The time of falling has a significant univariate association with daily benzodiazepine use, an association that persisted after adjustment for severity of anxiety and insomnia.21 Co-administration of central nervous system depressants, such as benzodiazepines or alcohol, alongside opiates may increase confusion and falls.27 Sedation, dizziness and postural disturbance are plausible explanatory mechanisms.27 A further paper found no significant difference (p = 0.614) in the mean dose of benzodiazepines between people who fall (14.4 mg (+/-9.4 mg) versus those who don’t fall (16.3 mg ± 11mg).26 In addition, benzodiazepines do not cause cognitively intact patients to fall (p = 0.477),6 however patients taking anti-depressants are more likely to fall (p = 0.045),6 and anticonvulsants are significantly linked with patients being less likely to fall (p = 0.023).6 The evidence is thus mixed, however the Initial Programme Theory has been refined in acknowledgement of the effect of medication on cognition as a potential mechanism for falls. The refined Programme Theory is formulated as: Patients in a specialist palliative care setting (Context) who are prescribed benzodiazepines and/or neuroleptic medications (Resource) are at increased risk of falling (Outcome) because of impaired cognition, sedation or other side effects (Reasoning).
D. Delirium
Cognitive impairment is an important factor in the risk of falls, p = 0.0125 and is independently significant. A diagnosis of delirium increases the risk of falling by 2.25-fold (p = 0.029).26 Patients admitted with an acute infection may be at increased risk of falls in early admission due to delirium.28 Neuroleptics/anti-psychotics are commonly used for delirium and treatment for 7 days with anti-psychotic medicines was potentially related to an occurrence of falls at 1.7%.29 No significant difference in Mini Mental State Examination (MMSE) scores between those who fell once and those who fell repeatedly was found,22 which is useful for further work however does not provide evidence for or against the proposed Initial Programme Theory, which was thus refined as: Patients in a specialist palliative care setting (Context) who experience delirium (Resource) are at increased risk of falling (Outcome) because of cognitive impairment, inability to follow commands or acute distress all of which may be related to the delirium itself, the underlying cause of the delirium and/or the medicines used to treat delirium (Reasoning).
E. Age and impaired mobility and/or cognition
The evidence for this Initial Programme Theory is linked closely with that described in Initial Programme Theory ‘F’, the difference being in the reasoning being cognition or physical weakness. The literature did not allow to distinguish between the two underpinning mechanisms and thus we decided to merge the two programme theories relating to age.
F. Age and impaired mobility/weakness
Increasing age and occurrence of falls are positively correlated (p ⩽ 0.001),22 with patients falling being on average 3.5 years older than those who do not.22 Age over 80 years is significant predictor in terms of falls risk (p = 0.01)25 and the mean age of patients who fell was 70.8 years of age.30 Older cognitively intact patients are less likely to fall than younger patients (p = 0.13) but patients who are mobile are more likely to fall than those who are immobile.6 Conversely, one paper concluded that age is not statistically significant (p = 0.3) in relation to falls risk.4 There is no clear definition of when older age becomes a factor and further work is needed on the mechanism and reasoning elements of this programme theory, which, taking the evidence into account, was formulated as: Patients in a specialist palliative care setting (Context) who are over the age of 65 (Resource) are at increased risk of falling and harm from falling (Outcome) because of impaired mobility/weakness and/or cognition (Reasoning).
G. Continence needs
We hypothesised that the need to mobilise to go to the bathroom might be a significant predictor of falls, however, whilst it was identified that 25.4% of patients who fell were getting to or from the toilet22 and that most falls occur in the patient’s room or bathroom,30 this is not specific enough evidence to contribute to the Initial Programme Theory.
Given the lack of evidence, this programme theory was invalidated.
H. Impaired mobility
Most patients who fell (82.2%) were either symptomatic and in bed >50% of the day (58.5%) or classified as bedridden (23.7%) when their performance status was reviewed.30 This is corroborated by a second paper which identified that 84.7% of patients who fell were defined as being ‘weak’ on admission.22 The majority of falls occur in patients with an Australia-modified Karnofsky Performance Status (AKPS) of 50% and who are deteriorating in phase of illness.31 When functional status was reviewed in more depth and found that impaired gait (p ⩽ 0.001), unsafe transfer technique (p = 0.002), use of a cane or walker (p ⩽ 0.001), use of furniture to aid balance (p = 0.008) and impaired mobility (p ⩽ 0.001) are all significant in terms of falls risk.4
A higher level of functional score has an associated higher risk of falls (p = 0.039) and that a greater physical dependence correlates with a lower risk of falling (p = 0.054).6 The use of ambulatory aids lowers the risk of fall, although not statistically significantly (p = 0.06).6 Cognitively intact patients who are more functional were found to be more likely to fall, whereas patients reliant on ambulatory aid were less likely (p = 0.004).6 This supports the theory of improving functional status being a factor, however, is converse to the above evidence relating to poor functional status. It must be noted that this study deals with a specific group of people – those who are cognitively intact – and so may not be representative of the whole patient cohort. Taking this evidence into account, this programme theory was formulated as: Patients in a specialist palliative care setting (Context) who have a poor functional status (Resource) are more likely to fall (Outcome) due to weakness and impaired mobility (Reasoning).
In addition, it was noted that patients fell when they were beginning to feel better and willing to increase activity levels and was hypothesised that decreasing symptom burden is a risk factor for falls.22 Patients undergoing rehabilitation present a greater risk of falls later in the admission whilst working with adjusting levels of function.28 The key risk time for specialist palliative care in-patients is as they start to become more independent due to a lower symptom burden and/or the effects of rehabilitation during their admission therefore, an additional Initial Programme Theory was added: Patients in a palliative care setting (Context) who have an improving functional status (Resource) are more likely to fall (Outcome) due to increased likelihood of independent mobility and/or adaptation to increased levels of functionality.
I. Advanced/metastatic cancer
No statistically significant correlation between diagnosis and falls risk was found.4,26 However, 52% of patients with advanced cancer under the care of a palliative care team fell within 6 months of the first point of contact but there were no data to compare this to falling rates for non-malignant disease.21 Patients with a primary brain tumour or brain metastases are more than twice as likely to fall than other patients.21 The evidence within this Initial Programme Theory was thus limited, as this review was restricted to in-patient specialist palliative care which may have missed the literature on disease-specific factors. This Initial Programme Theory was invalidated from the list of explanatory programme theories.
J. Maintaining independence
Patients who fall are more likely to have a greater ‘Fear Of Losing Independence’ (FOLI) (p = 0.023), avoid asking for help (p = 0.005), feel uneasy about asking for help (p = 0.05) and an interaction of the latter two (p = 0.001).6 The descriptor ‘patients who attempt to complete tasks by themselves’ had an insignificant impact on falls (p = 0.768).6 Utilising all aspects described previously into the analysis demonstrates that cognitively intact patients who have a FOLI and are disposed to an avoidance of asking for help have a greater likelihood of falling (p = 0.011)6 than those who did not demonstrate these behaviours. Taking this evidence into account, this programme theory was formulated as: In a specialist palliative care setting (Context) falls prevention is a priority (Resource) but patients continue to fall (Outcome) due to their wish to maintain their independence (Reasoning).
K. Impact of a fall
31.8% (n = 21) of performance status 3–4 (symptomatic and in bed more than 50% of the day (PS3) or bedridden (PS4), on the WHO Performance Status score) patients who fell died within 5 days of the incident.30 Seventy-four percent (n = 29) of falls reported to the United Kingdom national database of serious incidents resulted in an injury, most commonly a fractured neck of femur or intracranial haemorrhage.2 In 12 cases (out of 39) the fall was considered to have hastened death.2 It is important to note that the cases used within this study were all classed as serious incidents and so do not represent most falls within the hospice setting. 53.5% (n = 30) of patients who fell sustaining light injuries, 16.4% (n = 9) moderate injuries and 4.1% (n = 4) had serious injuries (fractures) requiring significant treatment.22 A further paper identified that 52% (n = 62) of participants in their study sustained a fall, following which the median survival was 73 days (95% CI = 52.9–93).21 Of those who fell, 45% sustained a soft tissue injury, 3% a fracture and 1% a dislocation.21
The outcome of a fall can result in increased pain, disability and diminished quality of life.5 Conversely, it was found that people who fell lived longer than people who did not fall (p ⩽ 0.001).4 Of patients who sustained a fractured hip within 30 days of admission to an in-patient palliative care service in the USA it was noted that 83.5% (n = 12,018) underwent surgery and of those undergoing surgery 6.2% died in hospital during the first admission.32 6-month survival rate was poor, with only 12.3% (n = 293) of those sustaining a fractured hip and have no surgery being alive at 6 months compared to 37.2% (n = 4470) of those who sustained a hip fracture and had surgery.32 There is evidence that falls within an in-patient specialist palliative care setting can increase length of stay (45.6 days vs 18.8 days, p ⩽ 0.001)22 and there is a clear trend towards longer length of stay of patients who fell (p = 0.054).26
The evidence clearly demonstrates that a fall within this patient group can have serious consequences for patients, including death. Overall, patients who fell appear to have a longer admission than those who didn’t fall which could be attributed to increased symptoms or the need for increased rehabilitation post fall. The programme theory was therefore formulated as: Patients in a specialist palliative care setting (Context) who sustain a fall (Resource) will be adversely affected and at increased risk of mortality and morbidity from the fall (Outcome) due to their complex disease processes, fear of deterioration in condition and existing reduced functional status (Reasoning).
Changes resulting from data synthesis
The 10 Initial Programme Theories were revised into 9 refined Programme Theories, with the removal of Programme Theory G and I relating to continence needs and advanced cancer being risk factors, respectively. Amendments have been made to acknowledge the side effects and interactions of medications and the effects of medications used to treat delirium. An IPT has been added reflecting that improving functional status can be seen as a risk factor for a fall event. Table 4 reports the Initial and Final Programme Theories to demonstrate where changes were made as a result of the synthesis.
Table 4.
Initial and final programme theories.
| ID | Initial programme theory | Changes | Final programme theory |
|---|---|---|---|
| A | Patients in a specialist palliative care setting (Context) who have previously fallen are more likely to fall again (Outcome) because they have reduced functional status (Resource) as a result of the first fall (physical or physiological) (Reasoning). | None | Patients in a specialist palliative care setting (Context) who have previously fallen are more likely to fall again (Outcome) because they have reduced functional status (Resource) as a result of the first fall (physical or physiological) (Reasoning). |
| B | Patients in a specialist palliative care setting (Context) who are prescribed more than 5 medicines (Resource) are at increased risk of falling (Outcome) because of impaired mobility and/or cognition (Reasoning). | None | Patients in a specialist palliative care setting (Context) who are prescribed more than 5 medicines (Resource) are at increased risk of falling (Outcome) because of impaired mobility and/or cognition (Reasoning). |
| C | Patients in a specialist palliative care setting (Context) who are prescribed benzodiazepines (Resource) are at increased risk of falling (Outcome) because of impaired cognition (Reasoning). | Effect of medication and impact of other medicines | Patients in a specialist palliative care setting (Context) who are prescribed benzodiazepines and/or neuroleptic medications (Resource) are at increased risk of falling (Outcome) because of impaired cognition, sedation or other side effects (Reasoning). |
| D | Patients in a specialist palliative care setting (Context) who experience delirium (Resource) are at increased risk of falling (Outcome) because of cognitive impairment, inability to follow instructions or acute distress (Reasoning). | Effects of medicines used to treat delirium | Patients in a specialist palliative care setting (Context) who experience delirium (Resource) are at increased risk of falling (Outcome) because of cognitive impairment, inability to follow commands or acute distress all of which may be related to the delirium itself, the underlying cause of the delirium and/or the medicines used to treat delirium (Reasoning). |
| E | Patients in a specialist palliative care setting (Context) who are over the age of 65 (Resource) are at increased risk of falling (Outcome) because of impaired mobility and/or cognition (Reasoning). | Subsumed into ‘F’ | |
| F | Patients in a specialist palliative care setting (Context) who are over the age of 65 (Resource) are at increased risk of harm from a fall (Outcome) because of impaired mobility/weakness (Reasoning) | E and F combined | Patients in a specialist palliative care setting (Context) who are over the age of 65 (Resource) are at increased risk of falling and harm from falling (Outcome) because of impaired mobility/weakness and/or cognition (Reasoning). |
| G | Falls (Outcome) in a specialist palliative care setting (Context) can often be related to elimination or continence needs (Resource) because of urgency or inability to request help and therefore the patient independently mobilises to the bathroom (Reasoning). | Invalidated | |
| H | Patients in a specialist palliative care setting (Context) who have a poor functional status (Resource) are more likely to fall (Outcome) due to weakness and impaired mobility (Reasoning). | None | Patients in a specialist palliative care setting (Context) who have a poor functional status (Resource) are more likely to fall (Outcome) due to weakness and impaired mobility (Reasoning). |
| Additional PT added | Patients in a specialist palliative care setting (Context) who have an improving functional status (Resource) are more likely to fall (Outcome) due to increased likelihood of independent mobility and/or adaptation to increased levels of functionality. | ||
| I | Patients in a specialist palliative care setting (Context) who have a diagnosis of advanced/metastatic cancer (Resource) are at increased risk of falling (Outcome) because of fatigue/reduced functional status/polypharmacy (Reasoning). | Invalidated | |
| J | In a specialist palliative care setting (Context) falls prevention is a priority (Resource) but patients continue to fall (Outcome) due to their wish to maintain their independence (Reasoning). | None | In a specialist palliative care setting (Context) falls prevention is a priority (Resource) but patients continue to fall (Outcome) due to their wish to maintain their independence (Reasoning). |
| K | Patients in a specialist palliative care setting (Context) who sustain a fall (Resource) will be adversely affected and at increased risk of mortality and morbidity from a the fall (Outcome) due to their complex disease processes, fear of deterioration in condition and existing reduced functional status (Reasoning) | None | Patients in a specialist palliative care setting (Context) who sustain a fall (Resource) will be adversely affected and at increased risk of mortality and morbidity from a the fall (Outcome) due to their complex disease processes, fear of deterioration in condition and existing reduced functional status (Reasoning) |
Discussion
Summary of findings
A history of a previous fall is a significant risk factor for a further incident of a similar nature, however the reasoning behind this is less clear and could be due to a multitude of factors. People who have previously sustained a fall may have reduced mobility in turn causing further risk of falls; they may have sustained psychological harm as a result of the fall causing them increased anxiety and a fear of further falling which affects their confidence and results in deconditioning; a fall could be precipitated by a change in condition, disease progression or infection for example. The reasoning requires the inclusion of qualitative data from people experiencing falls in this setting, which should be the focus of future research.
People being cared for in specialist palliative care settings take multiple medicines of varying pharmacological families, all of which have the potential for interaction. Due to the nature of disease and symptom burden for patients requiring specialist palliative care, there is a common use of opioid and non-opioid analgesics, anxiolytics, antiemetics, corticosteroids, laxatives and antipsychotics33 all of which can have significant side effect profiles. The evidence for multiple medications causing an increased risk of falls is not clear and at times is contradictory, however there is a case for further analysis and investigation when reviewing the outcomes of included studies.4,26
The literature indicates a possible link between benzodiazepine usage and an increased risk of falling. Benzodiazepines are commonly used in palliative care settings for a variety of symptoms including insomnia, anxiety, terminal agitation, breathlessness associated with anxiety, seizure management, spasm pain and nausea and vomiting.34 Common side effects are sedation, impaired psychomotor skills, cognitive impairment and hypotonia which manifests as unsteadiness and therefore can have a direct impact on the risk of falling.
Delirium and cognitive impairment have been clearly identified as significant risk factors for falls in in-patient palliative care settings.26 The reasoning behind this is potentially multifaceted and requires further investigation. Likely mechanisms are that patients with delirium may have an inability to follow instruction aimed at maintaining safety; they may be scared and agitated causing additional and potentially uncoordinated movement; they are often treated with medicines causing sedation which may affect safe mobility and decision making; they may not recognise the environment and fall as a result of unfamiliarity. Delirium is present in up to 42% of patients admitted to palliative care units35 and can be present in up to 85%–90% of patients who are terminally ill36 and therefore warrants further review in relation to falls risk factors.
There is a general agreement in the literature that advancing age is a risk factor for falls.22,25 The reasoning behind this risk factor is complex, as older age brings with it a multitude of physiological and psychological changes. For instance, older people may have less muscle condition making mobility harder; they may have confusion or dementia affecting the ability to maintain a safe environment; they are more likely to receive multiple medications with potential side effects and interactions.37,38 From an impact of a fall perspective, older people are more likely to have osteoporosis or other bone disease which makes a fracture or significant harm more likely.39 Age is important as the average age of people being cared for in these settings is 69.9 years (standard deviation 12.4 years), with 12.2% of people over 85 years.40
Functional performance is important in determining risk for these patients. The literature included in this review indicates the key factors in relation to performance status is when people start to improve in condition and mobilise more or when they remain mobile but are functionally compromised.22,28 The mechanism is likely to be related to a reduction in muscle condition and overall strength from their illness or recent decline in condition. Patients who are weak but remain mobile are more likely to fall than those who are bedbound and the likely mechanism is that they will be mobilising and trying to rehabilitate but with reduced strength or balance.
Strengths and limitations
Utilising a realist approach enabled this review to explore why patients fall in specialist palliative care settings and which patients are most susceptible to falls and why. The explanatory nature of realist theory and the iterative nature of the review provides a strong framework for a focussed search strategy with a reduced risk of missing key concepts during the process.
The literature was wide ranging with most being data driven by prospective or retrospective analysis of incidents, risk factors and other patient related information. There was little qualitative data identified and this can be seen as a potential weakness as the opinion and understanding of the people involved is key.
There is a broad knowledge base of falls-related literature relating to care homes and older people available and this was included in the wider exploratory scoping exercise, but due to the highly specialist nature of in-patient care has not been utilised as part of the realist review.
Excluding this data allowed the review to separate the distinct specialisms of palliative care and older peoples’ medicine,11 though this may have affected the breadth of the synthesis as there will undoubtedly be some level of overlap, the extent to which is unknown. Similarly, many of the papers for screening were based on ‘cancer’ and cancer wards and a key challenge was to differentiate cancer care from palliative care as in several papers they are used interchangeably. The definition of ‘palliative’ in oncology is different to the World Health Organisation definition41 which describes the approach of supportive care rather than those who are not for curative treatment as per the oncological definition.42 Whilst this enabled the search to be focussed and highly specific, it may have reduced the overall impact of the synthesis.
What this study adds
This realist review brings together, for the first time, evidence and theory regarding falls for people in an in-patient specialist palliative care unit and by utilising a realist approach presents the evidence using a causal approach to the creation and testing of theories. The evidence presented is valuable as the impact of falling is so significant in this population and therefore any additional support for clinicians in identifying and working alongside those at greater risk is beneficial in terms of patient and organisational outcomes.
The review identifies a clear risk of falling for patients in a specialist palliative care in-patient unit and that it is multifactorial and complex in nature. The risks of falling includes a history of previous falls events, medicine side effects and interactions, the increasing age of the patient and functional status and the presence of a delirium or cognitive impairment. This cohort of patients have wide ranging medical and social backgrounds and will be at various stages in their disease trajectory, making the identification of those most susceptible to falls challenging. We have not identified any clear disease specific falls risk for these patients.
A number of the programme theories require additional testing and refinement and therefore there is an opportunity to develop a specific knowledge base using existing and future research to meet the complex and specific needs of these patients.
Recommendations for research, practice and policy
Policy for palliative care patients and falls is based on a generalised approach to falls reduction and prevention for older people outside of specialist palliative care settings. This review demonstrates that specific policy is required for palliative care patients due to the complexity of their diagnosis, treatments, physical and psychological abilities. The utilisation of realist methodology allows us to explore the underlying mechanisms of the identified risk factors, supporting clinicians and policy makers to adapt and refine tools specifically for use in this group.
Key to understanding the most effective way to work with people and to understand what risk factors are most important will be to engage with clinicians providing care on a regular basis. Qualitative approaches to understanding their experiences of falls and what they feel are key risks will add to our understanding and provide continued development of the Initial Programme Theories.
Conclusion
By utilising a realist approach, we can conclude that in-patients in specialist palliative care settings are at risk of falling and that this is multifactorial with complex reasoning mechanisms underpinning the identified risks. There is also a significant impact of sustaining a fall in this cohort of patients with many sustaining serious harm, delayed discharge from to home, and both physical and psychological impacts. This cohort of patients have wide ranging medical and social backgrounds and will be at various stages in their disease trajectory, making the identification of those most susceptible to falls challenging. Individualised assessment and care planning is required due to the complex nature of persons disease, history and presentation. A history of falls prior to or during admission is a significant risk factor for further incidents but requires a patient-centred review of the reasoning behind this. Medication side effects and interactions are also likely to be important in this complex process and this area warrants further review and research. The age of the patient and the presence of delirium are also critical factors in predicting falls risk. Functional status is key to reducing falls and those patients who are improving and regaining independence are at potentially greater risk as they adapt and regain strength as are those who are mobile but lacking in strength.
Further work is warranted to explore the reasoning element of many of the programme theories developed in this review and to incorporate the opinions and understanding of the people receiving the care and those clinicians involved in care delivery.
Supplemental Material
Supplemental material, sj-pdf-1-pmj-10.1177_02692163221127808 for Why patients in specialist palliative care in-patient settings are at high risk of falls and falls-related harm: A realist synthesis by Helen Louise Forrow, Monique Lhussier, Jason Scott and Joanne Atkinson in Palliative Medicine
Footnotes
Authorship: Helen Forrow
• Associate Director of Strategic Partnerships and Services, Marie Curie North East and Yorkshire, Marie Curie Hospice, Newcastle NE4 6SS
• Doctoral Student, Northumbria University
• Registered Nurse
Dr Monique Lhussier
• Professor in Public Health and Wellbeing
• Director of Research and Knowledge Exchange, Department of Social Work, Education and Community Wellbeing, Northumbria University
Dr Jason Scott
• Associate Professor, Department of Social Work, Education and Community Wellbeing Northumbria University
Dr Joanne Atkinson
• Head of Department and Associate Professor, Department of Social Work, Education and Community Wellbeing, Northumbria University
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Marie Curie who fund the doctoral degree of HF.
ORCID iD: Helen Louise Forrow  https://orcid.org/0000-0002-0275-1364
https://orcid.org/0000-0002-0275-1364
Supplemental material: Supplemental material for this article is available online.
References
- 1. Carrasco AJP, Volberg C, Pedrosa DJ, et al. Patient Safety in palliative and end-of-life care: a text mining approach and systematic review of definitions. Am J Hospice Palliat Med 2021; 38: 1004–1012. [DOI] [PubMed] [Google Scholar]
- 2. Yardley I, Yardley S, Williams H, et al. Patient safety in palliative care: A mixed-methods study of reports to a national database of serious incidents. Palliat Med 2018; 32: 1353–1362. [DOI] [PubMed] [Google Scholar]
- 3. Oliver DP, Washington K, Kruse RL, et al. Hospice family members’ perceptions of and experiences with End-of-Life care in the Nursing Home. J Am Med Dir Assoc 2014; 15: 744–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patrick RJ, Slobodian D, Debanne S, et al. The predictive value of fall assessment tools for patients admitted to hospice care. BMJ Support Palliat Care 2017; 7: 341–346. [DOI] [PubMed] [Google Scholar]
- 5. Gray J. Protecting hospice patients: a new look at falls prevention. Am J Hosp Palliat Med 2007; 24: 242–247. [DOI] [PubMed] [Google Scholar]
- 6. Schonwetter RS, Kim S, Kirby J, et al. Etiology of falls among cognitively intact hospice patients. J Palliat Med 2010; 13: 1353–1363. [DOI] [PubMed] [Google Scholar]
- 7. Zimmermann C, Riechelmann R, Krzyzanowska M, et al. Effectiveness of specialized palliative care: A systematic review. JAMA 2008; 299: 1698–1709. [DOI] [PubMed] [Google Scholar]
- 8. Gaertner J, Frechen S, Sladek M, et al. Palliative care consultation service and palliative care unit: why do we need both? Oncologist 2012; 17: 428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. NHS England. NHS England Specialist Level Palliative Care: Information for commissioners April 2016, https://www.england.nhs.uk/wp-content/uploads/2016/04/speclst-palliatv-care-comms-guid.pdf (2016, accessed May 17, 2022).
- 10. Shipman C, Gysels M, White P, et al. Improving generalist end of life care: national consultation with practitioners, commissioners, academics, and service user groups. BMJ 2008; 337: a1720–a1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Voumard R, Rubli Truchard E, Benaroyo L, et al. Geriatric palliative care: A view of its concept, challenges and strategies. BMC Geriatr 2018; 18: 220. DOI: 10.1186/s12877-018-0914-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pawson R, Tilley N. Realistic Evaluation. 1997.
- 13. McEvoy P, Richards D. Critical realism: a way forward for evaluation research in nursing? Method Issues Nurs Res 2003; 43: 411–420. [DOI] [PubMed] [Google Scholar]
- 14. Pawson R, Greenhalgh T, Harvey G, et al. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005; 10: 21–34. [DOI] [PubMed] [Google Scholar]
- 15. Pawson R, Greenhalgh T, Harvey G, et al. Realist synthesis: an introduction. 2004. ESRC Research Methods Programme, University of Manchester. RMP Methods Paper 2.
- 16. Greenhalgh T, Wong G, Westhorp G, et al. Protocol-realist and meta-narrative evidence synthesis: Evolving Standards (RAMESES), http://www.biomedcentral.com/1471-2288/11/115 (2011). [DOI] [PMC free article] [PubMed]
- 17. Kmet L, Lee R, Cook L. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta, www.ahfmr.ab.ca/hta (2004). Alberta Heritage Foundation for Medical Research. [Google Scholar]
- 18. Guerrero-Torrelles M, Monforte-Royo C, Rodríguez-Prat A, et al. Understanding meaning in life interventions in patients with advanced disease: a systematic review and realist synthesis. Palliat Med 2017; 31: 798–813. [DOI] [PubMed] [Google Scholar]
- 19. Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: Realist syntheses. BMC Med 2013; 11: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cooper C, Lhussier M, Carr S. Blurring the boundaries between synthesis and evaluation. A customized realist evaluative synthesis into adolescent risk behavior prevention. Res Synth Methods 2020; 11: 457–470. [DOI] [PubMed] [Google Scholar]
- 21. Stone CA, Lawlor PG, Savva GM, et al. Prospective study of falls and risk factors for falls in adults with advanced cancer. J Clin Oncol 2012; 30: 2128–2133. [DOI] [PubMed] [Google Scholar]
- 22. Goodridge D, Marr H. Factors associated with falls in an inpatient palliative care unit: an exploratory study. Intl J Pall Nurs 2002; 8: 548–556. [DOI] [PubMed] [Google Scholar]
- 23. Duncan I, Maxwell TL, Huynh N, et al. Polypharmacy, medication possession, and deprescribing of potentially Non-Beneficial drugs in Hospice Patients. Am J Hosp Palliat Care 2020; 37: 1076–1085. [DOI] [PubMed] [Google Scholar]
- 24. Jansen K, Haugen DF, Pont L, et al. Safety and effectiveness of palliative drug treatment in the last days of life-a systematic literature review. J Pain Symptom Manag 2018; 55: 508–521.e3. [DOI] [PubMed] [Google Scholar]
- 25. Pearse H, Nicholson L, Bennett M. Falls in hospices: A cancer network observational study of fall rates and risk factors. Palliat Med 2004; 18: 478–481. [DOI] [PubMed] [Google Scholar]
- 26. Pautex S, Herrmann FR, Zulian GB. Factors associated with falls in patients with cancer hospitalized for palliative care. J Palliat Med 2008; 11: 878–884. [DOI] [PubMed] [Google Scholar]
- 27. Krashin D, Murinova N, Jumelle P, et al. Opioid risk assessment in palliative medicine. Expert Opin Drug Saf 2015; 14: 1023–1033. [DOI] [PubMed] [Google Scholar]
- 28. Hospice UK. Falls toolkit for prevention and management 2016, https://professionals.hospiceuk.org/docs/default-source/What-We-Offer/Care-Support-Programmes/falls-toolkit (2016, accessed December 13, 2021).
- 29. Maeda I, Ogawa A, Yoshiuchi K, et al. Safety and effectiveness of antipsychotic medication for delirium in patients with advanced cancer: A large-scale multicenter prospective observational study in real-world palliative care settings. Gen Hosp Psychiatry 2020; 67: 35–41. [DOI] [PubMed] [Google Scholar]
- 30. Ishøy T, Steptoe P. A multicentre survey of falls among Danish hospice patients. Int J Palliat Nurs 2011; 17: 75–79. [DOI] [PubMed] [Google Scholar]
- 31. Pegram D, Osborne T, Naismith J. P-145 Rising up – falls improvement. BMJ Support Palliat Care 2019; 9: A63. [Google Scholar]
- 32. Leland NE, Teno JM, Gozalo P, et al. Decision making and outcomes of a hospice patient hospitalized with a hip fracture. J Pain Symptom Manag 2012; 44: 458–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sera L, McPherson ML, Holmes HM. Commonly prescribed medications in a population of hospice patients. Am J Hosp Palliat Med 2014; 31: 126–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Howard P, Twycross R, Shuster J, et al. Benzodiazepines. J Pain Symptom Manag 2014; 47: 955–964. [DOI] [PubMed] [Google Scholar]
- 35. Bush SH, Tierney S, Lawlor PG. Clinical Assessment and management of delirium in the palliative care setting. Drugs 2017; 77: 1623–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Morita T, Chinone Y, Ikenaga M, et al. Efficacy and safety of palliative sedation therapy: a multicenter, prospective, observational study conducted on specialized palliative care units in Japan. J Pain Symptom Manag 2005; 30: 320–328. [DOI] [PubMed] [Google Scholar]
- 37. Park H, Satoh H, Miki A, et al. Medications associated with falls in older people: Systematic review of publications from a recent 5-year period. Eur J Clin Pharmacol 2015; 71: 1429–1440. [DOI] [PubMed] [Google Scholar]
- 38. NHS Scotland. Preventing Falls. NHS Inform.
- 39. Anderson KA. J Royal Coll Phys Edinburgh 2008; 38: 138–143. [Google Scholar]
- 40. Sleeman KE, Davies JM, Verne J, et al. The changing demographics of inpatient hospice death: Population-based cross-sectional study in England, 1993-2012. Palliat Med 2016; 30: 45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sepúlveda C, Marlin A, Yoshida T, et al. Palliative Care: The World Health Organization’s Global Perspective. J Pain Symptom Manag 2002; 24. [DOI] [PubMed] [Google Scholar]
- 42. van Kleffens T, Van Baarsen B, Hoekman K, et al. Clarifying the term “palliative” in clinical oncology. Eur J Cancer Care 2004; 13: 263–271. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-pmj-10.1177_02692163221127808 for Why patients in specialist palliative care in-patient settings are at high risk of falls and falls-related harm: A realist synthesis by Helen Louise Forrow, Monique Lhussier, Jason Scott and Joanne Atkinson in Palliative Medicine