Abstract
Background:
Ambulation devices may differ in their utility, muscle activation patterns, and how they affect regional blood flow. This study aimed to evaluate popliteal blood flow and vessel dimensions in response to ambulation with a hands-free crutch (HFC), axillary crutches (AC), a medical kneeling scooter (MKS), and regular walking in healthy adults.
Methods:
HFC, AC, MKS, and regular walking were completed in a random order by 40 adults aged 18-45 years. Participants ambulated at a comfortable pace for 10 minutes with each device. At baseline and immediately following each trial, a trained operator used diagnostic ultrasonography to capture popliteal vein and artery dimensional and flow characteristics.
Results:
Significant increases were observed from baseline (0.65 ± 0.23 cm) in venous diameter following walking (0.71 ± 0.21 cm, P = .012) and MKS (0.73 ± 0.21 cm, P = .003). Venous blood flow was also significantly different between conditions (P = .009) but was only greater following walking (124 ± 79 mL/min) compared to MKS (90 ± 64 mL/min, P = .021). No differences were observed in arterial dimensions between ambulation conditions. Significant increases were found in arterial blood flow from baseline (107 ± 69 mL/min) following walking (184 ± 97 mL/min, P < .001) and HFC (163 ± 86 mL/min, P < .001). Arterial blood flow following walking was greater than AC (132 ± 72 mL/min, P = .016) and MKS (128 ± 74 mL/min, P = .003).
Conclusion:
We found an average decrease in venous time-averaged mean velocity between walking and use of the MKS, but no such decrease with either HFCs or use of ACs in this healthy experimental cohort.
Level of Evidence:
Level III, diagnostic comparative study.
Keywords: neuromuscular disuse, flow-mediated dilation, acute hemodynamics
Introduction
Millions of Americans report to emergency departments for lower extremity injuries each year, many of which require a period of mechanical unloading and rehabilitation.15 Two negative consequences of unloading include skeletal muscle atrophy and strength loss.1,4 Several options for mobility assistance are available to lower-limb injury patients during the recovery period.22 Axillary crutches (AC) are the most common form of device, although they have drawbacks regarding pain and upper extremity function.20 A medical kneeling scooter (MKS) can be used as an alternative, but is limited in the surfaces it can maneuver and requires some upper extremity contribution to steer the device.22 A new type of hands-free crutching device (HFC) is also available, and recent research suggests it closely simulates a regular gait while still mechanically unloading the lower leg musculature.19 HFC use elevates muscle activation in the rectus femoris, vastus lateralis, and lateral gastrocnemius compared with AC and MKS.7,8 Although not directly shown, these data may provide indirect evidence of the potential to mitigate atrophy and strength loss in specific muscle groups over the duration of an unloading period.
Alternatively, ambulation devices and unloading conditions may also influence local blood flow.6,14,21,28 Venous thromboembolism, which may present as deep vein thrombosis (DVT), is a consequence of prolonged immobilization and is a concern for patients and clinicians. Incidence of DVT following foot and ankle surgery has been elusive to determine but may range from 0.22% up to 32%.24,26 Associated factors are also difficult to predict and include (but are not limited to) inherited thrombophilia, postoperative infection, prolonged surgical tourniquet time, immobility within 30 days, and absence of full weightbearing.11
A fixed knee angle has also previously been attributed to increased stasis and higher incidents (2.7%) of DVT in unilateral lower limbs suspension (eg, spaceflight model of disuse).3 The influence of knee angle has also been examined in blood flow simulations with various mobility devices. For example, Ciufo et al5 showed reduced popliteal venous volumetric flow rates in healthy adults in the flexed knee position on an MKS (106 mL/min) compared to standing (227.8 mL/min). The authors concluded that the duration of scooter use and the flexed knee position may have an effect on the degree of stasis.6 However, this study was limited in that it did not account of the potential effects of skeletal muscle pump activity on venous flow during muscular contractions.11 Reb et al21 recently showed simulated muscle pump activity (ie, plantar and dorsal flexion at 1 motion per second) increased all venous blood flow parameters and countered the negative effect of gravity and knee flexion. A limitation of both previous investigations was that blood flow characteristics could not be evaluated during a full ambulation simulation given current technologies (Doppler ultrasonography and probe) require minimal movement.2 Given HFC simulates regular gait and requires weightbearing through the gait cycle, we hypothesized this would enhance muscle pump activity and affect local blood flow and vessel dimensions.7,8 Thus, the aim of this research was to investigate blood flow and vessel dimensions at rest (baseline) and immediately following an ambulation simulation involving regular walking, MKS, AC, and HFC.
Methods
Study Design
A randomized, within-subject, crossover experimental design was used to compare popliteal blood flow and vessel dimension effects between 4 different ambulation conditions. The study consisted of 3 sessions: (1) informed consent/fitting, (2) ambulation device practice, and (3) testing. Appropriate precautions were taken to minimize COVID-19 exposure risk including screening, the use of masks when able, and sanitization of all contact surfaces. The 4 different ambulation conditions were as follows: (1) walking, (2) medical kneeling scooter (MKS) (Elenker, Chino, CA), (3) hands-free crutch (HFC) (iWalkFree Inc, Long Beach, CA), and (4) axillary crutches (AC) (Personal Care Products, Larchmont, NY). Following the completion of written informed consent, participants were fit according to manufacturer instructions. Fitting for the HFC involved matching portions of the device to participants’ limb lengths and adjusting for varus and/or valgus present in participants’ normal gait. A picture of the HFC device is available elsewhere.16
Participants returned on a different day for a familiarization session to ensure competency in each ambulation condition. In this session, the 3 ambulation conditions (not including regular walking) were continuously practiced on a similar course to the one utilized during data collection. The familiarization session ended when participants met the following criteria with all 3 devices: completion of 5 minutes of ambulation without stopping; able to navigate turns without losing balance; subject looks comfortable and expresses confidence in ambulation. No additional practice followed this session. The testing session occurred within 1 week after the familiarization session. All participants completed testing within a single session.
Participants arrived at the laboratory the day of data collection after refraining from exercise for 24 hours and caffeine for 12 hours. Ambulation condition order was randomized to mitigate any crossover effects of trial order. First, height and body mass (shoes removed) were recorded by researchers using a stadiometer (Seca 213; Chino, CA) and digital scale (Denver Instrument DA-150; Arvada, CO). Baseline ultrasonography measures (as described later) were then collected prior to the first condition. Following baseline ultrasonography measures, participants were prepared for the first condition. Participants then completed a 10-minute trial of the first ambulation condition around a 30.5-m (100-ft) rectangular walkway. At the conclusion of the 10 minutes, participants ambulated directly back to the training table for immediate right lower limb (disuse leg) popliteal ultrasonography. A 5-minute rest period occurred between each trial. The procedures were repeated until all 4 ambulation conditions were completed with respective ultrasonography.
Subjects
Persons aged 18-45 years were recruited via email listservs and word of mouth. After providing written informed consent to engage in study protocols, participants completed a DVT screening questionnaire, a Physical Activity Readiness Questionnaire, and additional study-specific questions.12,27 Exclusion criteria included cardiac condition, pregnancy, lower limb pain, recent injury, inability to self-ambulate unassisted, body mass over 124.7 kg (275 pounds), or height outside the range of 152.4 to 193 cm (5 ft to 6 ft 4 in.). The descriptive characteristics of the 40 participants are shown in Table 1. Sample size for the study was estimated above previous studies on blood flow in ambulatory conditions.6,21 A retrospective power analysis for our main dependent effects of popliteal venous and arterial flow determined that the sample size of 40 participants was above 85% power at an alpha level of 0.05.
Table 1.
Participant Characteristics.
| Characteristic | Mean ± SD |
|---|---|
| Age, y | 24.3 ± 5.1 |
| Height, cm | 173.6 ± 7.7 |
| Body mass, kg | 77.7 ± 13.8 |
| BMI | 25.7 ± 3.6 |
Abbreviation: BMI, body mass index.
Ultrasonography
Baseline and post-mobility device popliteal hemodynamics were collected on the right lower limb (disuse limb) via duplex ultrasonography (Terason uSmart 3300, Terason, Burlington MA, USA) of the popliteal fossa while prone on a training table with the ankle propped to set the knee angle between 15 and 20 degrees of flexion.21 Vessels were imaged longitudinally with a 15L4 linear transducer. Doppler was superimposed over 2D imaging to measure velocity (cm/s). Utilizing software calipers, vessel diameter was measured at the widest portion of each still longitudinal image. Each ultrasonographic measure was collected in duplicate to ensure reliability.
All measurements were collected by an investigator trained in ultrasonographic techniques. Baseline reliability data are shown in Table 2. Cross-sectional area (cm2) was calculated as π*D2/4 under the assumption that vessel cross-sections were circular.6 Venous and arterial flow (mL/min) were calculated by multiplying the product of time-averaged mean velocity (TAMV) and cross-sectional area by 60 s/min.6 The probe was posited with an angle of insonation no greater than 60 degrees. Ultrasonographic data collection times were measured using a stopwatch starting at the completion of the 10-minute trial and ending at the freezing of the final image. Average ultrasonography collection time (mean ± SD) was 90.8 ± 25.5 seconds postambulation.
Table 2.
Baseline Popliteal Blood Flow and Vessel Dimension Reliability.
| Characteristic | Venous ICC | Arterial ICC |
|---|---|---|
| Diameter | .983 | .957 |
| TAMV | .863 | .947 |
| Flow | .914 | .934 |
Abbreviations: ICC, intraclass correlation coefficient (Cronbach’s alpha); TAMV, time-averaged mean velocity.
Statistics
Statistical analyses were completed using SPSS version 28.0 (IBM, Armonk, NY). The descriptive characteristics were presented as mean ± SD. Intraclass correlation coefficients (type 6) were calculated between all duplicate baseline ultrasonographic values to determine reliability.25 Parametric analysis of variance (ANOVA) with repeated measures were used to determine hemodynamic differences. An alpha level of 0.05 was used for all analyses. When significance was identified, Sidak post hoc tests were used to evaluate differences between the 4 ambulation conditions.
Results
There were significant differences in venous dimensions between baseline and ambulation conditions (Table 3). There were significant differences in venous flow (F4,36 = 3.5, P = .009) and TAMV (F4,36 = 3.0, P = .032). Post hoc analyses for venous flow are shown in Figure 1. There were no significant differences in arterial dimensions between baseline and any conditions (Table 4). However, there were significant differences in arterial flow (F4,35 = 10.7, P < .001) and time-averaged mean velocity (TAMV) (F4,35 = 10.0, P < .001). Post hoc analyses for arterial flow are shown in Figure 2.
Table 3.
Popliteal Vein Flow and Dimensions.
| Characteristic | Baseline, Mean ± SD |
Walk, Mean ± SD |
HFC, Mean ± SD |
AC, Mean ± SD |
MKS, Mean ± SD |
|---|---|---|---|---|---|
| Diameter (cm) | 0.65 ± 0.23 | 0.71 ± 0.21a | 0.70 ± 0.22 | 0.68 ± 0.20 | 0.73 ± 0.21ab |
| Cross-sectional area (cm2) | 0.37 ± 0.23 | 0.43 ± 0.24a | 0.42 ± 0.25 | 0.39 ± 0.21 | 0.45 ± 0.24ab |
| TAMV (cm/s) | 4.54 ± 2.47 | 5.19 ± 3.07 | 4.55 ± 2.52 | 4.67 ± 2.94 | 3.80 ± 2.34c |
Abbreviations: AC, axillary crutches; HFC, hands-free crutch; MKS, medical kneeling scooter; TAMV, time-averaged mean velocity.
Different from baseline, P < .05.
Different from AC, P < .05.
Different from walk, P < .05.
Figure 1.
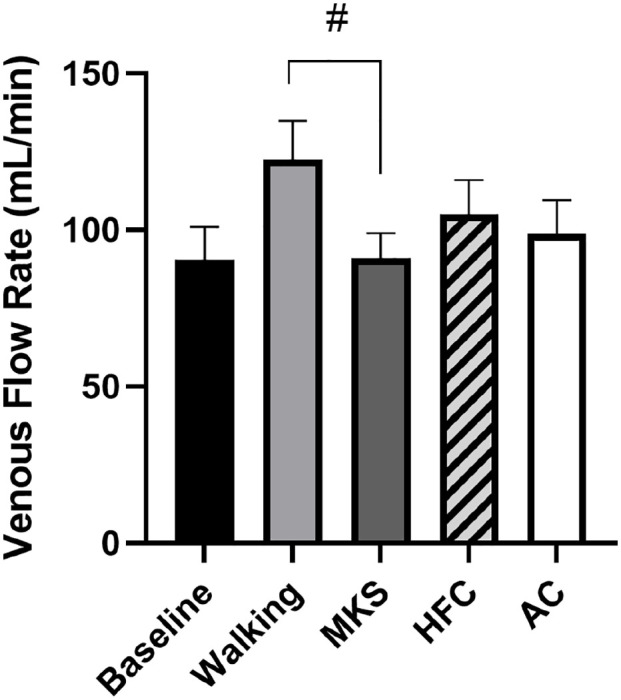
Popliteal vein blood flow immediately following each ambulation condition.
All values shown as mean ± SD. Abbreviations: HFC, hands-free crutch; AC, axillary crutches; MKS, medical kneeling scooter. #Significant decline from walking P < .05.
Table 4.
Popliteal Artery Flow and Dimensions.
| Characteristic | Baseline, Mean ± SD |
Walking, Mean ± SD |
HFC, Mean ± SD |
AC, Mean ± SD |
MKS, Mean ± SD |
|---|---|---|---|---|---|
| Diameter (cm) | 0.62 ± 0.08 | 0.63 ± 0.07 | 0.63 ± 0.08 | 0.62 ± 0.08 | 0.62 ± 0.08 |
| Cross-sectional area (cm2) | 0.30 ± 0.08 | 0.32 ± 0.08 | 0.32 ± 0.08 | 0.31 ± 0.09 | 0.31 ± 0.08 |
| TAMV (cm/s) | 5.89 ± 3.67 | 9.61 ± 4.91a | 8.64 ± 4.24a | 7.30 ± 3.73b | 7.16 ± 4.03ab |
Abbreviations: AC, axillary crutches; HFC, hands-free crutch; MKS, medical kneeling scooter; TAMV, time-averaged mean velocity.
Significantly greater than baseline, P < .05.
Significantly different from walking, P < .05.
Figure 2.

Popliteal artery blood flow immediately following each ambulation condition.
All values shown as mean ± SD. Abbreviations: HFC, hands-free crutch; AC, axillary crutches; MKS, medical kneeling scooter. *Significant increase from baseline, P < .05. #Significant decline from walking, P < .05.
Discussion
The principal findings of this investigation revealed venous blood flow differences between ambulation conditions, which may have implications pertaining to the prevention of DVT. We found significant decrease in venous time-averaged mean velocity between walking and use of the knee scooter.
DVT is a concern with prolonged knee flexion and is associated with decreased popliteal venous flow and stasis.11 Previous investigations highlight a negative effect of knee flexion on venous flow when standing still, but neither HFC nor MKS affected venous flow compared to baseline in this study despite a flexed knee position.21 Venous dimensions are not influenced by knee flexion in other reports, perhaps because of lack of ambulation.6 However, in the current study, use of the MKS elicited a larger venous diameter than baseline and AC but lower venous flow than walking, supporting previous evidence that weightbearing with a straight knee stimulates venous flow more than weightbearing on a flexed knee.21 This combination of dilation without comparable flow increase is likely indicative of venous pooling. However, despite having a flexed knee, venous flow following HFC was not different than walking. The effect of knee flexion in HFC was likely mitigated by its unique ambulation similar to walking gait, given that muscular activity is a major determinant of popliteal venous flow, and previously mentioned evidence demonstrates elevated surface electromyography when using HFC.7,19 The use of HFC may be a better option than MKS in populations requiring foot/ankle unloading where venous pooling is of concern, such as those at risk for DVT.
Participants experienced an increase in popliteal arterial flow from baseline following both walking and HFC, whereas MKS and AC likewise both resulted in a decrease in flow compared to walking. Acute popliteal arterial flow is a concern in many disuse conditions and can be reduced by up to 61% from 8 hours of constant sitting.14 We speculate that blood flow and vessel dimensions are influential in disuse outcomes via nutrient delivery and waste clearance, though the logistics of longitudinal blood flow research makes such data collection highly implausible.5,9,13,17,23
Several additional factors are at play when selecting an ambulatory aid. HFC has a much smaller base and is less stable than the 4-wheeled MKS, which may be relevant to high-risk DVT populations with poor balance.10,16 Although this may be disadvantageous on a level, unobstructed surface, the small base of the HFC allows for better maneuverability around corners and can be used to climb stairs. Maintaining independence is critical for this population, as low independence in daily life is associated with DVT onset.18 The hands-free nature of HFC allows for full upper body use while ambulating during daily tasks, whereas the MKS requires the user to be stationary. Clinicians must balance potential DVT risk advantages, balance concerns, and utility when recommending an ambulatory aid to patients.
Our investigation is not without limitations. Unlike actual injured patients, the population studied was healthy and passed a DVT risk screening.12 Rest time was standardized between all devices’ simulation, and a return to baseline was not verified by collecting heart rate data or conducting additional ultrasonography. However, given the conditions were randomized, the effect of ambulation condition order should be minimal. Although popliteal blood flow and vessel dimensions were directly measured using ultrasonography, data were collected immediately following each condition and may not represent live values during ambulation. Subjects were positioned prone with knee flexed to 15-20 degrees for ultrasonography, different from the unique positioning of each ambulatory condition. This study design decision was influenced by the popliteal strap of HFC that obstructed probe access during ultrasonographic measurement. Therefore, blood flow measures were standardized to the prone position for all devices immediately following physical activity.
Conclusion
Unlike MKS and AC, HFC did not differ significantly from walking in any popliteal blood flow or vessel dimension measure. Ambulation conditions affect popliteal venous dimensions and blood flow. Popliteal arterial blood flow but not vessel dimensions are affected by ambulation conditions. The negative effects of knee flexion on venous blood flow are mitigated by ambulation. Clinicians aiming to prevent stasis may consider HFC as a promising ambulation device option during periods of unloading.
Footnotes
Ethical Approval: The study was approved by the Institutional Review Board at North Dakota State University (IRB0003736). All participants were provided with an explanation of the risks and benefits of the study and written informed consent was obtained before any study procedures were initiated.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Adam P. Bradley, MS, Alexis S. Roehl, and Kyle J. Hackney, PhD, report research grant from IwalkFree, Inc, grant to institution (North Dakota State University [NDSU]); medical knee scooter, axillary crutches, and IwalkFree devices were provided for study via grant (1), and devices provided to institution (NDSU). ICMJE forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was completed from a research grant provided by iWalkFree, Inc. The sponsor role was to provide resources for the investigational team to conduct and publish the study, as well as proper training on Hands-Free Crutch use. The sponsor made no contribution to collection or publication of data. The sponsor was allowed a prepublication draft prior to submission to ensure no proprietary information on product was released.
ORCID iD: Kyle J. Hackney, PhD,  https://orcid.org/0000-0003-1586-5392
https://orcid.org/0000-0003-1586-5392
References
- 1. Berg HE, Dudley GA, Häggmark T, Ohlsén H, Tesch PA. Effects of lower limb unloading on skeletal muscle mass and function in humans. J Appl Physiol. 1991;70(4):1882-1885. doi: 10.1152/jappl.1991.70.4.1882 [DOI] [PubMed] [Google Scholar]
- 2. Blanco P. Volumetric blood flow measurement using Doppler ultrasound: concerns about the technique. J Ultrasound. 2015;18(2):201-204. doi: 10.1007/s40477-015-0164-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bleeker MWP, Hopman MTE, Rongen GA, Smits P. Unilateral lower limb suspension can cause deep venous thrombosis. Am J Physiol Regul Integr Comp Physiol. 2004;286(6):R1176-R1177. doi: 10.1152/ajpregu.00718.2003 [DOI] [PubMed] [Google Scholar]
- 4. Casaburi R, Barstow TJ, Robinson T, Wasserman K. Dynamic and steady-state ventilatory and gas exchange responses to arm exercise. Med Sci Sports Exerc. 1992;24(12):1365-1374. [PubMed] [Google Scholar]
- 5. Ciufo DJ, Anderson MR, Baumhauer JF. Impact of knee scooter flexion position on venous flow rate. Foot Ankle Int. 2019;40(1):80-84. doi: 10.1177/1071100718794966 [DOI] [PubMed] [Google Scholar]
- 6. de Boer MD, Maganaris CN, Seynnes OR, Rennie MJ, Narici MV. Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young men. J Physiol. 2007;583(3):1079-1091. doi: 10.1113/jphysiol.2007.135392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dewar C, Grindstaff TL, Farmer B, et al. EMG activity with use of a hands-free single crutch vs a knee scooter. Foot Ankle Orthop. 2021;6(4):24730114211060054. doi: 10.1177/24730114211060054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dewar C, Martin KD. Comparison of lower extremity EMG muscle testing with hands-free single crutch vs standard axillary crutches. Foot Ankle Orthop. 2020;5(3):247301142093987. doi: 10.1177/2473011420939875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Exton JH. Gluconeogenesis. Metabolism. 1972;21(10):945-990. doi: 10.1016/0026-0495(72)90028-5 [DOI] [PubMed] [Google Scholar]
- 10. Heit JA, Silverstein MD, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ. Risk factors for deep vein thrombosis and pulmonary embolism. Arch Intern Med. 2000;160(6):809. doi: 10.1001/archinte.160.6.809 [DOI] [PubMed] [Google Scholar]
- 11. Hitos K, Cannon M, Cannon S, Garth S, Fletcher JP. Effect of leg exercises on popliteal venous blood flow during prolonged immobility of seated subjects: implications for prevention of travel-related deep vein thrombosis. J Thromb Haemost. 2007;5(9):1890-1895. doi: 10.1111/j.1538-7836.2007.02664.x [DOI] [PubMed] [Google Scholar]
- 12. Illinois State Medical Society. Are you at risk for DVT? 2013. https://pdf4pro.com/amp/view/are-you-at-risk-for-dvt-venous-resource-center-1f5305.html
- 13. Johnson PC, Wayland H. Regulation of blood flow in single capillaries. Am J Physiol. 1967;212(6):1405-1415. doi: 10.1152/ajplegacy.1967.212.6.1405 [DOI] [PubMed] [Google Scholar]
- 14. Kurosawa Y, Nirengi S, Tabata I, Isaka T, Clark JF, Hamaoka T. Effects of prolonged sitting with or without elastic garments on limb volume, arterial blood flow, and muscle oxygenation. Med Sci Sports Exerc. 2022;54(3):399-407. doi: 10.1249/MSS.0000000000002822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lambers K, Ootes D, Ring D. Incidence of patients with lower extremity injuries presenting to US emergency departments by anatomic region, disease category, and age. Clin Orthop Relat Res. 2012;470(1):284-290. doi: 10.1007/s11999-011-1982-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Martin KD, Unangst AM, Huh J, Chisholm J. Patient preference and physical demand for hands-free single crutch vs standard axillary crutches in foot and ankle patients. Foot Ankle Int. 2019;40(10):1203-1208. doi: 10.1177/1071100719862743 [DOI] [PubMed] [Google Scholar]
- 17. McArdle W, Katch F, Katch V. Essentials of Exercise Physiology. Wolters Kluwer; 2015. [Google Scholar]
- 18. Nakanishi K, Kanda T, Kobata T, Mori M, Yamada S, Kasamaki Y. New score including daily life independence levels with dementia is associated with the onset of deep vein thrombosis in frail older adults. Geriatr Gerontol Int. 2020;20(5):414-421. doi: 10.1111/ggi.13873 [DOI] [PubMed] [Google Scholar]
- 19. Rambani R, Shahid MS, Goyal S. The use of a hands-free crutch in patients with musculoskeletal injuries: randomized control trial. Int J Rehabil Res. 2007;30(4):357-359. doi: 10.1097/MRR.0b013e3282f1fecf [DOI] [PubMed] [Google Scholar]
- 20. Rasouli F, Reed KB. Walking assistance using crutches: a state of the art review. J Biomech. 2020;98:109489. doi: 10.1016/J.JBIOMECH.2019.109489 [DOI] [PubMed] [Google Scholar]
- 21. Reb CW, Haupt ET, Vander Griend RA, Berlet GC. Pedal musculovenous pump activation effectively counteracts negative impact of knee flexion on human popliteal venous flow. Foot Ankle Spec. Published online March 3, 2021. doi: 10.1177/1938640021997275 [DOI] [PubMed] [Google Scholar]
- 22. Salminen AL, Brandt Å, Samuelsson K, Töytäri O, Malmivaara A. Mobility devices to promote activity and participation: a systematic review. J Rehabil Med. 2009;41(9):697-706. doi: 10.2340/16501977-0427 [DOI] [PubMed] [Google Scholar]
- 23. Sands JM, Timmer RT, Gunn RB. Urea transporters in kidney and erythrocytes. Am J Physiol Ren Physiol. 1997;273(3 pt 2):F321-F339. doi: 10.1152/ajprenal.1997.273.3.f321 [DOI] [PubMed] [Google Scholar]
- 24. Saragas NP, Ferrao PNF, Saragas E, Jacobson BF. The impact of risk assessment on the implementation of venous thromboembolism prophylaxis in foot and ankle surgery. Foot Ankle Surg. 2014;20(2):85-89. doi: 10.1016/j.fas.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 25. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420-428. doi: 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- 26. Sullivan M, Eusebio ID, Haigh K, Panti JP, Omari A, Hang JR. Prevalence of deep vein thrombosis in low-risk patients after elective foot and ankle surgery. Foot Ankle Int. 2019;40(3):330-335. doi: 10.1177/1071100718807889 [DOI] [PubMed] [Google Scholar]
- 27. Warburton DER, Jamnik V, Bredin SSD, Shephard RJ, Gledhill N. The 2018 Physical Activity Readiness Questionnaire for Everyone (PAR-Q+) and electronic Physical Activity Readiness Medical Examination (ePARmed-X+). Heal Fit J Canada. 2018;11(1):31-34. doi: 10.14288/HFJC.V11I1.260 [DOI] [Google Scholar]
- 28. Watenpaugh DE, Buckey JC, Lane LD, et al. Effects of spaceflight on human calf hemodynamics. J Appl Physiol. 2001;90(4):1552-1558. doi: 10.1152/jappl.2001.90.4.1552 [DOI] [PubMed] [Google Scholar]


