Abstract
Background:
Compare the recurrence rate of paresthesias in patients undergoing primary cubital tunnel surgery in those with and without wrapping of the ulnar nerve with the human amniotic membrane (HAM).
Methods:
A retrospective investigation of patients undergoing primary cubital tunnel surgery with a minimum 90-day follow-up was performed. Patients were excluded if the nerve was wrapped using another material, associated traumatic injury, simultaneous Guyon’s canal release, or revision procedures. Failure was defined as those patients who experienced initial complete resolution of symptoms (paresthesias) but then developed recurrence of paresthesias.
Results:
A total of 57 controls (CON) and 21 treated with HAM met our inclusion criteria. There was a difference in the mean age of CON (48.4 ± 13.5 years) and HAM (30.6 ± 15) (P< 0.0001). There was no difference in gender mix (P=0.4), the severity of symptoms (P=0.13), and length of follow-up (P=0.084). None of 21 (0%) treated with HAM developed recurrence of symptoms compared to 11 of 57 (19.3%) (P=0.03) (CON). Using a multivariate regression model adjusted for age and procedure type, CON was 24.4 (95% CI=1.26-500, P=0.0348) times higher risk than HAM of developing a recurrence of symptoms.
Conclusion:
The HAM wrapping used in primary cubital tunnel surgery significantly reduced recurrence rates of paresthesias. Further prospective studies with randomization should be carried out to better understand the role HAM can play in cubital tunnel surgery.
Key Words: Amnion, Cubital tunnel, Human amniotic membrane, Nerve wrap, Ulnar nerve
Introduction
Cubital tunnel syndrome is the second most common compressive neuropathy of the upper extremity.1-3 There are approximately 75,000 new cases each year in the United States.4-6 Surgical treatment is performed when nonoperative methods fail. Several procedures have been described including anterior transposition (subcutaneous or submuscular), in-situ decompression, endoscopic release,and partial medial epicondylectomy.7-13
Four possible outcomes can be achieved following an ulnar nerve procedure. The first is when the patient gets complete relief from symptoms after surgery and symptoms do not recur. In the second scenario, symptoms worsen after surgery and can be attributed to iatrogenic injury to the nerve. The third one, patients get no or partial relief from the surgery. This can be attributed to persistent compression from incomplete release of the nerve or due to failure of the nerve to recover in the setting of a complete release. In the fourth scenario, the patient gets complete relief, but symptoms recur after some time. This recurrence has been attributed to perineural fibrosis and scarring those forms around the nerve thus causing compression of the nerve.14-16 The recurrence rate following cubital tunnel surgery has been reported between 3.2%-35%.2,7
Amnion has been used for over a century for medical procedures. It has been used for corneal injuries and for burn wound coverage.17 It has been used in several orthopedic applications.18 One of the many properties of amnion is its ability to prevent scar tissue formation.19,20 In a rabbit model, Kim et al demonstrated that human amniotic membrane (HAM) wrapping of the ulnar nerve following an ulnar neuropathy resulted in a significant reduction in perineural fibrosis and scarring. 21 One study has reported on 8 patients where HAM was used in revision cubital tunnel surgery with significant improvements in VAS, DASH, and grip strength.22
The purpose of our study was to compare the recurrence of ulnar nerve paresthesias in patients who underwent cubital tunnel procedures with and without HAM.
Materials and Methods
Patient Information
After obtaining Institutional Review Board approval, patients who underwent an ulnar nerve procedure between January 1, 2012, and June 30, 2018, at a single facility were identified. Our integrated health care system does not use CPT codes, but rather procedure codes. All procedures with the following codes were identified and reviewed: 1. “Cubital tunnel release”; 2. “Ulnar nerve transposition”, 3. “Ulnar nerve at elbow decompression.” Procedures were performed by three fellowship-trained hand surgeons with Certificates of Added Qualification in orthopedic hand surgery and one fellowship-trained shoulder and elbow surgeon with a Certificate of Added Qualification in orthopedic sports medicine. Each surgeon had a minimum of 10 years of experience in practice. Our inclusion criteria included patients who underwent primary procedures for cubital tunnel syndrome with a minimum of 90 days follow-up. The exclusion criteria included: the wrong diagnosis, wrapped with another product, trauma cases where the nerve was transposed as a routine part of the procedure, planned revision surgery for ease of ulnar nerve exploration, simultaneous cubital and Guyon’s canal tunnel releases, and revision ulnar nerve procedures. Patient demographic information, prior surgery, concomitant procedures, smoking status, the severity of nerve involvement (based on McGowan classification), tourniquet time, and re-operations were recorded. 23 We defined failure as those patients who had initial resolution of symptoms following surgery but then developed a recurrence of symptoms after the procedure.5 We defined clinical follow-up as the time from surgery to the last clinic visit with an orthopedic provider. We defined chart review as the time from surgery to when the patient’s chart was reviewed for data collection. Patient enrollment status in our health plan was also confirmed at that time. If the patient was no longer a member, the chart review was documented from surgery to the last encounter with any healthcare provider in our system. Patients in our integrated health care system are captured and are very unlikely to seek medical outside of our system (due to health insurance plans). Therefore, any medical care rendered to patients would be recorded in the electronic medical record and reviewed for analysis. Each surgeon assessed their patient postoperatively and documented it in the chart. Our only endpoint was the recurrence of symptoms. Patient-reported outcome scores were not recorded.
Surgical Technique
An in situ decompression consisted of a 3-4 cm incision midway between the olecranon and medial epicondyle. The Osborne ligament and the superficial and deep fascia of the flexor carpi ulnaris (FCU) were released distally, while the fascia between the medial triceps and medial intermuscular septum was released proximally. The medial intermuscular septum was left intact. Circumferential dissection of the nerve was performed to release scar tissue and allow the wrapping of HAM. In our series, all the anterior transpositions were subcutaneous. The nerve was initially decompressed with circumferential dissection to allow for mobilization and transposition. The longitudinal vessels with the nerve were not cauterized. The medial intermuscular septum was excised, the Arcade of Struthers was released, and the nerve was transposed anteriorly and secured with subcutaneous tissue only. A fascial sling was not created. The choice of the procedure and use of HAM was left to the discretion of each surgeon. The choice of amnion use was by one physician (Raffy Mirzayan, MD) who used it on all consecutive patients without any selection criteria.
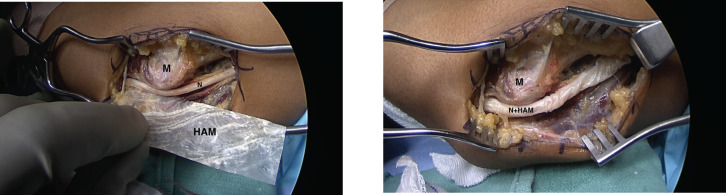
A DryFlex amnion matrix (BioD, LLC, Memphis, TN) was used in the first 16 patients who underwent HAM wrapping, and Amnion Matrix (Arthrex, Naples, FL) was used in five patients. [Figure 1 A; B] The HAM was dehydrated and had undergone aseptic processing. It was stored at room temperature and did not require to be frozen. The size used was 8 cm x 3 cm. The HAM was wrapped from just proximal to the first motor branch of the ulnar nerve and as proximally as it would extend (8cm). The HAM did not require any special handling. It was stiff when initially opened from the packaging but became elastic and pliable with minimal saline or blood contact. It was not secured with sutures.
Figure 1.
A. Human amniotic membrane (HAM) is held next to a decompressed ulnar nerve (N), B. Ulnar nerve wrapped in HAM (N+HAM). M- medial epicondyle
The patients were immobilized in a long arm posterior molded plaster splint, which was removed at the first post-operative visit between 7 and 14 days. The patients were referred to occupational therapy for rehabilitation.
Statistical analysis
Sample characteristics were described as mean ± standard deviation for continuous variables and N (%) for categorical variables. The Wilcoxon rank-sum test was used for continuous variables and the chi-square test for the categorical variable to detect the difference between HAM and control groups. Logistic regression was applied to evaluate the risk ratio of having a recurrence. Logistic regression with penalized likelihood method was used to control for significant variables to determine odds ratios. All analyses were analyzed using SAS version 9.4 (SAS Institute Inc, Cary, NC) and the statistical significance level was set as P < 0.05.
Results
Our search identified 165 cases. Of those, 58 were excluded for inadequate follow-up, 6 for wrong diagnosis/procedure, 2 were wrapped with another material, 12 trauma cases requiring transposition, and 9 planned revision surgery, leaving 78 patients who met our inclusion criteria. Of those, 21 patients (26.9%) underwent HAM wrapping at the time of the index procedure while 57 (73.1%) did not. The chart review was carried out on an average of 46 + 19 months (range 10 to 82 months) in the HAM group and 61 + 27 months (range: 9 to 101 months) in the CON group (P=0.0112).
There was a significant difference in the mean age of the HAM group 30.6 ± 15 years (range, 16-63 years) compared to 48.4 ± 13.5 years (range, 14-70 years) in the CON group (P<0.0001). There was no difference noted in the ratio of women to men within the respective groups, with 14 of 21 (66.7%) being men in the HAM group, and 46 of 57 (59%) being men in CON (P=0.4). The average length of follow-up for all patients was 447.4 days (range, 91-1926 days). No significant difference in the length of follow-up between the two groups, with a mean of 346+243 days (range, 91-876 days) in the HAM group versus 485+445 days (range, 91-1926 days) in CON (P=0.084).
Based on the McGowan Classification, 23 47 of 58 (82.5%) in the HAM group had moderate to severe disease, as compared to 14 of 21 (66.7%) in the CON group (P=0.13). The average tourniquet time for all patients was 56.6+22 minutes (range, 24-121 minutes). No difference was found with respect to tourniquet time between the HAM group, with 66.7+3 minutes (range, 32-121 minutes), compared to 52.3+2 minutes (range, 24-115 minutes) in the CON group (P=0.076).
Patients underwent one of two procedures, in situ ulnar nerve decompression (UND) or subcutaneous ulnar nerve transposition (UNT). There was a difference in procedure types between the two groups. In the CON group, 49 of 57 (86%) underwent UND compared to 13 of 21 (62%) in the HAM group (P=0.02).
A total of 11 of 57 (19.3%) patients in the CON group experienced a recurrence of symptoms following the index procedure compared to none of 21 (0%) in the HAM group (P=0.03). Using a multivariate regression model adjusted for age and procedure type, CON was 24.4 (95% CI=1.26-500, P=0.0348) times higher risk than HAM of developing a recurrence of symptoms. The mean time of recurrence was 10.4 + 4 months (range: 4 - 18.4 months)
Discussion
Our findings show that wrapping of the ulnar nerve with HAM following cubital tunnel surgery significantly reduces the recurrence of paresthesias. None of the patients treated with HAM developed recurrent symptoms and when controlled for age and procedure type, those not wrapped with HAM had a 24 times higher likelihood for recurrence.
Cubital tunnel syndrome is the second most common compressive neuropathy of the upper extremity.1-3 The annual incidence has been reported to be 25 cases per 100,000 person-years in men and 19 cases in 100,000 person-years in women, translating to approximately 75,000 new cases each year in the United States.4-6, 24 Surgical treatment is performed when nonoperative methods fail. The rate of surgical treatment for cubital tunnel syndrome has increased over the last decade.8 Several procedures have been described including anterior transposition (subcutaneous or submuscular), in-situ decompression, endoscopic release,and partial medial epicondylectomy.7-13 Each of these procedures has advantages and disadvantages. Soltani et al. 8 reported that over the course of 11 years, the rate of in situ decompression has increased while that of transposition has decreased. This is in part due to several prospective studies and meta-analyses that have shown no difference in clinical outcomes between the two procedures. 6,25-31 However, revision rates between 3.2% to 25% have been reported with in situ decompression and as high as 12% in transposition.7,32
Failure of cubital tunnel surgery can be divided into three categories.22 The first is that the patient’s symptoms worsen after surgery, which can be attributed to iatrogenic injury.33,34 The second scenario is one where the patient gets no or partial relief from the surgery. This can be attributed to incomplete decompression of the nerve.33,35,36 The third scenario is that the patient gets complete relief, but symptoms recur after some time. This recurrence has been attributed to perineural fibrosis and scarring those forms around the nerve, thus causing recurrent compression of the nerve.14-16,37 Therefore, various materials have been used to wrap the ulnar nerve to prevent scarring including saphenous nerve autograft, pedicled adipose autograft, substitutes dural flaps, decellularized human dermal tissue, porcine extracellular matrices, and collagen matrix wrap.38-43
Amnion has been used for over a century for medical procedures. It has been used for corneal injuries and for burn wound coverage.17,44,45 Amnion has anti-inflammatory properties, including downregulation of TGF-β, which can reduce perineural fibrosis and scarring and recurrence of symptoms following cubital tunnel surgery. 19,21,46-49 Several animal models have used amniotic tissue to prevent scar formation. In a rabbit model, Kim et al.21 demonstrated that human amniotic membrane (HAM) wrapping of the ulnar nerve following a neuropathy resulted in a significant reduction in perineural fibrosis and scarring. This has also been demonstrated in human patients.20 Meng et al.50 using a rat model, transected and repaired sciatic nerves and found that those wrapped with processed HAM had significantly fewer adhesions and less scar formation than controls. In another rat model, Ozgenel et al.51 investigated the extent of adhesions and perineurial scar thickness macroscopically and histologically at 4 and 12 weeks following circumferential epineurectomies of sciatic nerves and found that nerves treated with HAM wrapping and hyaluronic acid injection had the least amount of adhesion and perineurial scar tissue.
Application of HAM in human patients has been performed mostly to reduce postoperative scarring and adhesion formation prostate, spine, lung, vaginal reconstructions, and ocular surgery. 46, 52-57 HAM has been used in several orthopedic applications.18 Vines et al.58 performed a six patient feasibility study using amnion injections to treat symptomatic knee osteoarthritis. Zelen et al.59 injected micronized dehydrated human amniotic/chorionic membrane (mDHACM) as an alternative to surgical intervention in the treatment of refractory plantar fasciitis. Hanselman et al. 60 compared cryopreserved human amniotic membrane (c-hAM) injections to corticosteroid injections in plantar fasciitis patients. It has also been used for tendon wrapping in foot and ankle surgery.61, 62
One other study has investigated the use of HAM in revision cubital tunnel surgery.22 The researchers reported on eight patients, with two failed prior ulnar nerve operations, who underwent revision neurolysis with HAM wrapping. At a mean of 30 months follow-up, the patients had significant improvement in VAS, DASH, and grip strength. We began using human amniotic membranes in 2011 at our institution. Initially, it was used in trauma and arthroplasty cases where the likelihood of revision surgery was high and ulnar nerve identification and dissection would be made easier during revision surgery. On several occasions of revision surgery, it was noted that dissection of the ulnar nerve was simplified due to the lack of scar formation around the nerve. Therefore, one of the authors (Raffy Mirzayan, MD) began using HAM routinely on all the cubital tunnel procedures to prevent the recurrence of symptoms of paresthesias.
Our study is not without limitations. It is retrospective with its inherent shortcomings. There were no standardized indications to perform the type of procedure, and occupational therapy protocols were carried out by various therapists. There were no patient-reported outcomes or pain scores, nor the grip and pinch strength measurements. While these measurements are important to collect and report, several prospective studies and meta-analyses have shown no difference in clinical outcomes of cubital tunnel release and anterior transposition surgery with the only difference being in recurrence rates. 6, 25-31 Therefore, our study was specifically aimed to address recurrence rates and not functional outcomes. In addition, although a minimum of 90 days may not be long enough, our patients are captured in our healthcare system, and if they did have a recurrence of symptoms, they would have sought medical intervention, which would have appeared in their chart at the time of review. Another limitation is that there was only one surgeon who used HAM which could have led to selection bias, other factors, and confounders, besides HAM that might explain the difference in recurrence such as patient selection, surgical technique, post-op protocol.
While our findings are promising, larger prospective, randomized controlled studies should be performed to better control for variables and better refine indications for use of HAM in cubital tunnel surgery.
References
- 1.Palmer BA, Hughes TB. Cubital tunnel syndrome. J Hand Surg Am. 2010;35(1):153–63. doi: 10.1016/j.jhsa.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Camp CL, Ryan CB, Degen RM, Dines JS, Altchek DW, Werner BC. Risk factors for revision surgery following isolated ulnar nerve release at the cubital tunnel: a study of 25,977 cases. J Shoulder Elbow Surg. 2017;26(4):710–5. doi: 10.1016/j.jse.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 3.Staples JR, Calfee R. Cubital Tunnel Syndrome: Current Concepts. J Am Acad Orthop Surg. 2017;25(10):e215–e24. doi: 10.5435/JAAOS-D-15-00261. [DOI] [PubMed] [Google Scholar]
- 4.Shi Q, MacDermid JC, Santaguida PL, Kyu HH. Predictors of surgical outcomes following anterior transposition of ulnar nerve for cubital tunnel syndrome: a systematic review. J Hand Surg Am. 2011;36(12):1996–2001 e1-6. doi: 10.1016/j.jhsa.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Nellans K, Tang P. Evaluation and treatment of failed ulnar nerve release at the elbow. Orthop Clin North Am. 2012;43(4):487–94. doi: 10.1016/j.ocl.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89(12):2591–8. doi: 10.2106/JBJS.G.00183. [DOI] [PubMed] [Google Scholar]
- 7.Gaspar MP, Kane PM, Putthiwara D, Jacoby SM, Osterman AL. Predicting Revision Following In Situ Ulnar Nerve Decompression for Patients With Idiopathic Cubital Tunnel Syndrome. J Hand Surg Am. 2016;41(3):427–35. doi: 10.1016/j.jhsa.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Soltani AM, Best MJ, Francis CS, Allan BJ, Panthaki ZJ. Trends in the surgical treatment of cubital tunnel syndrome: an analysis of the national survey of ambulatory surgery database. J Hand Surg Am. 2013;38(8):1551–6. doi: 10.1016/j.jhsa.2013.04.044. [DOI] [PubMed] [Google Scholar]
- 9.Aleem AW, Krogue JD, Calfee RP. Outcomes of revision surgery for cubital tunnel syndrome. J Hand Surg Am. 2014;39(11):2141–9. doi: 10.1016/j.jhsa.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Krogue JD, Aleem AW, Osei DA, Goldfarb CA, Calfee RP. Predictors of surgical revision after in situ decompression of the ulnar nerve. J Shoulder Elbow Surg. 2015;24(4):634–9. doi: 10.1016/j.jse.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Tsai TM, Bonczar M, Tsuruta T, Syed SA. A new operative technique: cubital tunnel decompression with endoscopic assistance. Hand Clin. 1995;11(1):71–80. [PubMed] [Google Scholar]
- 12.Tsai TM, Tsuruta T, Syed SA, Kimura H. A new technique for endoscopic carpal tunnel decompression. J Hand Surg Br. 1995;20(4):465–9. doi: 10.1016/s0266-7681(05)80154-8. [DOI] [PubMed] [Google Scholar]
- 13.King T, Morgan FP. Late results of removing the medial humeral epicondyle for traumatic ulnar neuritis. J Bone Joint Surg Br. 1959;41-B(1):51–5. doi: 10.1302/0301-620X.41B1.51. [DOI] [PubMed] [Google Scholar]
- 14.Filippi R, Charalampaki P, Reisch R, Koch D, Grunert P. Recurrent cubital tunnel syndrome Etiology and treatment. Minim Invasive Neurosurg. 2001;44(4):197–201. doi: 10.1055/s-2001-19937. [DOI] [PubMed] [Google Scholar]
- 15.Gabel GT, Amadio PC. Reoperation for failed decompression of the ulnar nerve in the region of the elbow. J Bone Joint Surg Am. 1990;72(2):213–9. [PubMed] [Google Scholar]
- 16.Rogers MR, Bergfield TG, Aulicino PL. The failed ulnar nerve transposition Etiology and treatment. Clin Orthop Relat Res. 1991(269):193–200. [PubMed] [Google Scholar]
- 17.Fairbairn NG, Randolph MA, Redmond RW. The clinical applications of human amnion in plastic surgery. J Plast Reconstr Aesthet Surg. 2014;67(5):662–75. doi: 10.1016/j.bjps.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 18.Heckmann N, Auran R, Mirzayan R. Application of Amniotic Tissue in Orthopedic Surgery. Am J Orthop (Belle Mead NJ) 2016;45(7):E421–e5. [PubMed] [Google Scholar]
- 19.Ferguson MW, O’Kane S. Scar-free healing: from embryonic mechanisms to adult therapeutic intervention. Philos Trans R Soc Lond B Biol Sci. 2004;359(1445):839–50. doi: 10.1098/rstb.2004.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mirzayan R, Syed SP, Shean CJ. Dissection of an Ulnar Nerve Previously Transposed and Wrapped with Human Amniotic Membrane: A Report of 3 Cases. JBJS Case Connect. 2021;11:3. doi: 10.2106/JBJS.CC.21.00066. [DOI] [PubMed] [Google Scholar]
- 21.Kim SS, Sohn SK, Lee KY, Lee MJ, Roh MS, Kim CH. Use of human amniotic membrane wrap in reducing perineural adhesions in a rabbit model of ulnar nerve neurorrhaphy. J Hand Surg Eur Vol. 2010;35(3):214–9. doi: 10.1177/1753193409352410. [DOI] [PubMed] [Google Scholar]
- 22.Gaspar MP, Abdelfattah HM, Welch IW, Vosbikian MM, Kane PM, Rekant MS. Recurrent cubital tunnel syndrome treated with revision neurolysis and amniotic membrane nerve wrapping. J Shoulder Elbow Surg. 2016;25(12):2057–65. doi: 10.1016/j.jse.2016.09.013. [DOI] [PubMed] [Google Scholar]
- 23.McGowan A. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32-B(3):293–301. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 24.Latinovic R, Gulliford MC, Hughes RA. Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psychiatry. 2006;77(2):263–5. doi: 10.1136/jnnp.2005.066696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bartels RH, Verhagen WI, van der Wilt GJ, Meulstee J, van Rossum LG, Grotenhuis JA. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery. 2005;56(3):522–30; discussion -30. doi: 10.1227/01.neu.0000154131.01167.03. [DOI] [PubMed] [Google Scholar]
- 26.Biggs M, Curtis JA. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58(2):296–304; discussion 296-304. doi: 10.1227/01.NEU.0000194847.04143.A1. [DOI] [PubMed] [Google Scholar]
- 27.Gervasio O, Gambardella G, Zaccone C, Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56(1):108–17; discussion 17. doi: 10.1227/01.neu.0000145854.38234.81. [DOI] [PubMed] [Google Scholar]
- 28.Nabhan A, Ahlhelm F, Kelm J, Reith W, Schwerdtfeger K, Steudel WI. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 2005;30(5):521–4. doi: 10.1016/j.jhsb.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 29.Catalano LW, 3rd , Barron OA. Anterior subcu-taneous transposition of the ulnar nerve. Hand Clin. 2007;23(3):339–44, vi. doi: 10.1016/j.hcl.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 30.Macadam SA, Gandhi R, Bezuhly M, Lefaivre KA. Simple decompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surg Am. 2008;33(8):1314 e1–12. doi: 10.1016/j.jhsa.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 31.Zhang D, Earp BE, Blazar P. Rates of Complications and Secondary Surgeries After In Situ Cubital Tunnel Release Compared With Ulnar Nerve Transposition: A Retrospective Review. J Hand Surg Am. 2017;42(4):294 e1–e5. doi: 10.1016/j.jhsa.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Hutchinson DT, Sullivan R, Sinclair MK. Long-term Reoperation Rate for Cubital Tunnel Syndrome: Subcutaneous Transposition Versus In Situ Decompression. Hand (N Y) 2021;16(4):447–452. doi: 10.1177/1558944719873153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mackinnon SE, Novak CB. Operative findings in reoperation of patients with cubital tunnel syndrome. Hand (N Y) 2007;2(3):137–43. doi: 10.1007/s11552-007-9037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tanaka SK, Lourie GM. Anatomic course of the medial antebrachial cutaneous nerve: a cadaveric study with proposed clinical application in failed cubital tunnel release. J Hand Surg Eur Vol. 2015;40(2):210–2. doi: 10.1177/1753193413515826. [DOI] [PubMed] [Google Scholar]
- 35.Mackinnon SE. Pathophysiology of nerve compression. Hand Clin. 2002;18(2):231–41. doi: 10.1016/s0749-0712(01)00012-9. [DOI] [PubMed] [Google Scholar]
- 36.Tang DT, Barbour JR, Davidge KM, Yee A, Mackinnon SE. Nerve entrapment: update. Plast Reconstr Surg. 2015;135(1):199e–215e. doi: 10.1097/PRS.0000000000000828. [DOI] [PubMed] [Google Scholar]
- 37.Abe Y, Doi K, Kawai S. An experimental model of peripheral nerve adhesion in rabbits. Br J Plast Surg. 2005;58(4):533–40. doi: 10.1016/j.bjps.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 38.Kokkalis ZT, Jain S, Sotereanos DG. Vein wrapping at cubital tunnel for ulnar nerve problems. J Shoulder Elbow Surg. 2010;19(2 Suppl):91–7. doi: 10.1016/j.jse.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 39.Danoff JR, Lombardi JM, Rosenwasser MP. Use of a pedicled adipose flap as a sling for anterior subcutaneous transposition of the ulnar nerve. J Hand Surg Am. 2014;39(3):552–5. doi: 10.1016/j.jhsa.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 40.Ulivieri S, Pluchino MG, Petrini C, Giorgio A, Oliveri G. Protective wrapping of the ulnar nerve in severe cubital tunnel syndrome: treatment and long-term results. G Chir. 2010;31(10):459–61. [PubMed] [Google Scholar]
- 41.Puckett BN, Gaston RG, Lourie GM. A novel technique for the treatment of recurrent cubital tunnel syndrome: ulnar nerve wrapping with a tissue engineered bioscaffold. J Hand Surg Eur Vol. 2011;36(2):130–4. doi: 10.1177/1753193410384690. [DOI] [PubMed] [Google Scholar]
- 42.Papatheodorou LK, Williams BG, Sotereanos DG. Preliminary results of recurrent cubital tunnel syndrome treated with neurolysis and porcine extracellular matrix nerve wrap. J Hand Surg Am. 2015;40(5):987–92. doi: 10.1016/j.jhsa.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 43.Soltani AM, Allan BJ, Best MJ, Mir HS, Panthaki ZJ. Revision decompression and collagen nerve wrap for recurrent and persistent compression neuropathies of the upper extremity. Ann Plast Surg. 2014;72(5):572–8. doi: 10.1097/SAP.0b013e3182956475. [DOI] [PubMed] [Google Scholar]
- 44.Tosi GM, Massaro-Giordano M, Caporossi A, Toti P. Amniotic membrane transplantation in ocular surface disorders. J Cell Physiol. 2005;202(3):849–51. doi: 10.1002/jcp.20181. [DOI] [PubMed] [Google Scholar]
- 45.Sippel KC, Ma JJ, Foster CS. Amniotic membrane surgery. Curr Opin Ophthalmol. 2001;12(4):269–81. doi: 10.1097/00055735-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Tao H, Fan H. Implantation of amniotic membrane to reduce postlaminectomy epidural adhesions. Eur Spine J. 2009;18(8):1202–12. doi: 10.1007/s00586-009-1013-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Niknejad H, Peirovi H, Jorjani M, Ahmadiani A, Ghanavi J, Seifalian AM. Properties of the amniotic membrane for potential use in tissue engineering. Eur Cell Mater. 2008;15:88–99. doi: 10.22203/ecm.v015a07. [DOI] [PubMed] [Google Scholar]
- 48.Lee SB, Li DQ, Tan DT, Meller DC, Tseng SC. Suppression of TGF-beta signaling in both normal conjunctival fibroblasts and pterygial body fibroblasts by amniotic membrane. Curr Eye Res. 2000;20(4):325–34. [PubMed] [Google Scholar]
- 49.Tseng SC, Li DQ, Ma X. Suppression of transforming growth factor-beta isoforms, TGF-beta receptor type II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrix. J Cell Physiol. 1999;179(3):325–35. doi: 10.1002/(SICI)1097-4652(199906)179:3<325::AID-JCP10>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 50.Meng H, Li M, You F, Du J, Luo Z. Assessment of processed human amniotic membrane as a protective barrier in rat model of sciatic nerve injury. Neurosci Lett. 2011;496(1):48–53. doi: 10.1016/j.neulet.2011.03.090. [DOI] [PubMed] [Google Scholar]
- 51.Ozgenel GY, Filiz G. Combined application of human amniotic membrane wrapping and hyaluronic acid injection in epineurectomized rat sciatic nerve. J Reconstr Microsurg. 2004;20(2):153–7. doi: 10.1055/s-2004-820772. [DOI] [PubMed] [Google Scholar]
- 52.Patel VR, Samavedi S, Bates AS, et al. Dehydrated Human Amnion/Chorion Membrane Allograft Nerve Wrap Around the Prostatic Neurovascular Bundle Accelerates Early Return to Continence and Potency Following Robot-assisted Radical Prostatectomy: Propensity Score-matched Analysis. Eur Urol. 2015;67(6):977–80. doi: 10.1016/j.eururo.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 53.Subach BR, Copay AG. The use of a dehydrated amnion/chorion membrane allograft in patients who subsequently undergo reexploration after posterior lumbar instrumentation. Adv Orthop. 2015;2015:501202. doi: 10.1155/2015/501202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cargnoni A, Ressel L, Rossi D, et al. Conditioned medium from amniotic mesenchymal tissue cells reduces progression of bleomycin-induced lung fibrosis. Cytotherapy. 2012;14(2):153–61. doi: 10.3109/14653249.2011.613930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ashworth MF, Morton KE, Dewhurst J, Lilford RJ, Bates RG. Vaginoplasty using amnion. Obstet Gynecol. 1986;67(3):443–6. [PubMed] [Google Scholar]
- 56.Tancer ML, Katz M, Veridiano NP. Vaginal epithelialization with human amnion. Obstet Gynecol. 1979;54(3):345–9. [PubMed] [Google Scholar]
- 57.Kamiya K, Wang M, Uchida S, et al. Topical application of culture supernatant from human amniotic epithelial cells suppresses inflammatory reactions in cornea. Exp Eye Res. 2005;80(5):671–9. doi: 10.1016/j.exer.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 58.Vines JB, Aliprantis AO, Gomoll AH, Farr J. Cryopreserved Amniotic Suspension for the Treatment of Knee Osteoarthritis. J Knee Surg. 2016;29(6):443–50. doi: 10.1055/s-0035-1569481. [DOI] [PubMed] [Google Scholar]
- 59.Zelen CM, Poka A, Andrews J. Prospective, randomized, blinded, comparative study of injectable micronized dehydrated amniotic/chorionic membrane allograft for plantar fasciitis--a feasibility study. Foot Ankle Int. 2013;34(10):1332–9. doi: 10.1177/1071100713502179. [DOI] [PubMed] [Google Scholar]
- 60.Hanselman AE, Tidwell JE, Santrock RD. Cryopreserved human amniotic membrane injection for plantar fasciitis: a randomized, controlled, double-blind pilot study. Foot Ankle Int. 2015;36(2):151–8. doi: 10.1177/1071100714552824. [DOI] [PubMed] [Google Scholar]
- 61.DeMill SL, Granata JD, McAlister JE, Berlet GC, Hyer CF. Safety analysis of cryopreserved amniotic membrane/umbilical cord tissue in foot and ankle surgery: a consecutive case series of 124 patients. Surg Technol Int. 2014;25:257–61. [PubMed] [Google Scholar]
- 62.Warner M, Lasyone L. An Open-label, Single-center, Retrospective Study of Cryopreserved Amniotic Membrane and Umbilical Cord Tissue as an Adjunct for Foot and Ankle Surgery. Surg Technol Int. 2014;25:251–5. [PubMed] [Google Scholar]