Abstract
Colorectal cancer (CRC) is the third most revalent type of cancer in the world and the second most common cause of cancer death (about 1 million per year). Historically, natural compounds and their structural analogues have contributed to the development of new drugs useful in the treatment of various diseases, including cancer. Essential oils are natural odorous products made up of a complex mixture of low molecular weight compounds with recognized biological and pharmacological properties investigated also for the prevention and treatment of cancer. The aim of this paper is to highlight the possible role of essential oils in CRC, their composition and the preclinical studies involving them. It has been reviewed the preclinical pharmacological studies to determine the experimental models used and the anticancer potential mechanisms of action of natural essential oils in CRC. Searches were performed in the following databases PubMed/Medline, Web of science, TRIP database, Scopus, Google Scholar using appropriate MeSH terms. The results of analyzed studies showed that EOs exhibited a wide range of bioactive effects like cytotoxicity, antiproliferative, and antimetastatic effects on cancer cells through various mechanisms of action. This updated review provides a better quality of scientific evidence for the efficacy of EOs as chemotherapeutic/chemopreventive agents in CRC. Future translational clinical studies are needed to establish the effective dose in humans as well as the most suitable route of administration for maximum bioavailability and efficacy. Given the positive anticancer results obtained from preclinical pharmacological studies, EOs can be considered efficient complementary therapies in chemotherapy in CRC.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12935-022-02806-5.
Keywords: Colorectal cancer, Natural essential oils, Anticancer properties, Cytotoxicity, Apoptosis, Anticancer therapy
Introduction
Colorectal cancer (CRC) is a devastating disease with a high incidence and mortality rate, accounting for more than 10% of all cancer death in 2020, being the third most common cancer in men and the second in women [1, 2]. According to the International Agency for Research on Cancer, in 2018, the global cancer burden is estimated to have risen to 18.1 million new cases and 9.6 million deaths. CRC is the second largest cancer worldwide with 881,000 deaths in 2018 [3–5]. Studies show that approximately 90% of colorectal cancer cases occur in people over the age of 50 and the number of patients diagnosed with CRC exceeds that of patients diagnosed with lung cancer. CRC has a high rate of treatment success when it is detected in its early stages [6]. Thus the 5-year survival rate is over 90% in early-diagnosed colorectal cancer, but only 40% of tumors are found at a localized stage and approximately 56% of colorectal cancer patients die from the tumor. In stage IV, survival is low, only 14–16% at 5 years [7]. CRC is a type of cancer that affects colon or rectum cells and normally starts on the inner lining of these tissues, where the pathologist can find the so-called polyps [8]. Even if polyps are not strictly malignant, with time they can sometimes enlarge, grow and spread originating cancer. The most common form of CRC is adenocarcinoma and this review analyzed only this kind of tumor, not considering less frequent forms of cancer affecting the colon and rectal tissues, such as carcinoid tumors, gastrointestinal stromal tumors (GISTs), lymphomas, and sarcomas [9, 10]. In general, CRC does not cause symptoms at the initial stages, even if small blood loss, fatigue, lack of appetite, anemia, weight loss, stubborn constipation, alternating with diarrhea can be present [11]. The diagnosis of CRC is based on an accurate anamnesis, followed by blood tests with the research of carcinoembryonic tumor marker (CEA), digital rectal examination and colonoscopy with biopsies. In addition, ultrasound, computed tomography (CT) and magnetic resonance imaging can be used to assess the extent of the tumor itself and the presence or absence of distant metastases [12]. More recently, clinicians are beginning to use the results of the molecular profile of CRC from biopsy, as it can serve to better define the prognosis and therapy of this neoplasia [13]. The therapeutic strategy is essentially based on surgery, which can be assisted by chemotherapy and radiotherapy, alone or combined, adjuvant or neoadjuvant. Moreover, targeted therapy and immunotherapy are two recent therapeutic tools for the management of aggressive, advanced or metastatic CRC [14, 15]. Nonetheless, these strategies have numerous adverse side effects, and as a result, new adjuvant therapies in the treatment of cancer have been sought, the naturally bioactive compounds being known as potential anticancer adjuvant and complementary agents [16–19]. The study of natural products has always guided the field of applied pharmacology [20]. They have played a key role in drug discovery, especially for cancer and infectious diseases [21, 22]. In the area of cancer, since the 1940s, more than 50% of the active molecules are unaltered or derivative natural products of different origins (plant, animal and microbial) [16, 23]. Among these, some examples are paclitaxel (Taxol®), vincristine (Oncovin®), vinorelbine (Navelbine®), teniposide (Vumon®) and various water-soluble analogues of camptothecin (e.g. Hycamtin®) [24–26]. After a decline in the pharmaceutical industry's search for natural products from the 1990s onwards due to technical barriers to screening, isolation, characterization and optimization, in recent years, technological and scientific development has revitalized the interest in them [27, 28]. According to Newman & Cragg [26], natural products still offer the best potential for discovering new compounds that can lead to effective agents in a variety of human diseases. Essential oils, complex mixtures of volatile organic compounds extracted from plants by steam distillation, dry distillation or a suitable mechanical process without heating, possess biological and pharmaceutical properties including anticancer activity [29]. Various types of malignancies are reported to be lowered after treatment with essential oils [30]. The current status of knowledge regarding their potential in the treatment strategies of CRC, the second deadliest (about 1 million per year) and third most commonly diagnosed cancer in the world (about 2 million cases in 2020) [1], is covered in this review.
Essential oils: a brief overview
Traditional uses
Humans use medicinal plants for disease treatment for a long time [27, 31–33]. Such a traditional method possesses more than thousands of years of history, as noted by ancient Persian, Indian, Chinese, Arabic, and Greek manuscripts [20, 34]. Among natural phytochemicals, EOs have attracted human attention due to their pleasant aroma [35]. They have been ethnotraditionally used for the treatment and prevention of various diseases by different human cultures [36]. The application of EOs against neoplasia is a very promising field [37]. In 2005, Warnke and coauthors reported that the application of tea tree and eucalyptus oils has reduced tumor smell and inflammation in cancer patients [38]. Rosa x damascena has a long history of use in traditional medicine: its EO could increase cell proliferation on SW742 when higher concentrations were used, i.e. 10 μg/mL with 48 h of incubation time [39]. Moreover, the same work showed that similar effects were perceived in human normal fibroblasts, thus inducing the authors to suggest that the EO of Rosa x damascene could stimulate cell growth. EOs extracted from 6 sand-dune plants of Portugal region (Seseli tortuosum L., Otanthus maritimus (L.) Hoffmanns. & Link, Eryngium maritimum L., Crithmum maritimum L., Artemisia campestris subsp. maritima (DC.) Arcang., Juniperus phoenicea var. turbinate (Guss.) Parl.,) reported promising cytotoxic properties [40]. In 1997, Gould has postulated that the naturally occurring monoterpenes are a potential new class of potential anticancer agents [41]. For example, D-limonene showed anticancer activity against many rodent solid tumor types by carcinogen detoxification and inhibition of the posttranslational isoprenylation of growth-controlling small G proteins (p21ras) [42].
Chemical composition
Many plants produce volatile terpene substances in their vital processes. In addition to terpene hydrocarbons, some volatile molecules have various oxygen or sulphur-containing functional group such as hydroxyl, carbonyl, carboxyl, thiol and others [43, 44]. The mixture of these compounds commonly called EOs contains more than twenty constituents at varying concentrations with two–three major components [45]. EOs are characterized by complex chemistry due to a set of aromatic substances known as secondary low molecular weight metabolites [46]. These molecules belong to several classes of compounds predominantly represented by monoterpenes [47], sesquiterpenes [48] and their derivatives. EOs are obtained by hydro- or steam distillation starting from different parts of the plant such as leaves, flowers, and stems[35]. Precisely because of their rich and varied chemical composition, accurate characterization by gas chromatography and mass spectrometry is essential.
Anticancer mechanisms of EOs: molecular evidence from preclinical studies
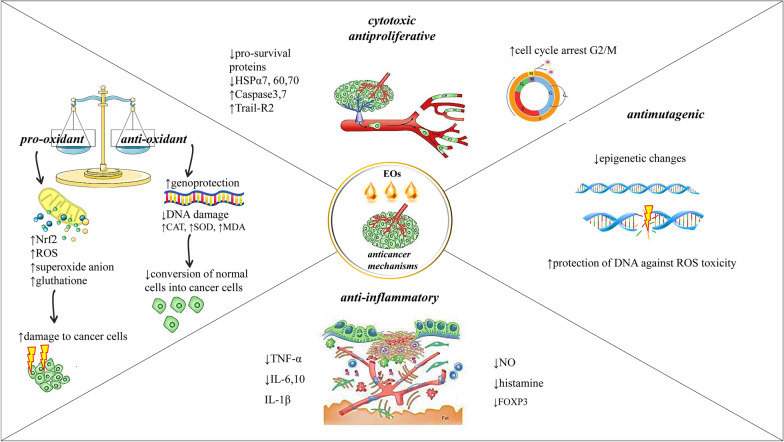
Various EOs have been studied in many types of experimental models in the search for new treatments for colon cancer with very promising results [16, 20] (Additional file 1). EOs exhibit a wide range of bioactive effects like cytotoxicity, antiproliferative, and antimetastatic effects on cancer cells through various mechanisms of action [49]. It has been demonstrated that EOs possessed, for the most part, a prodigious activity directed against cancer cells [45]. In the case of CRC, the effect of EOs has been analyzed in vitro studies on human colon cancer cell lines such as HT-29, Caco-2, SW480, and HCT-116, among others. HCT-116 cells have been the most studied since they are classified as a cell line model to study the molecular mechanisms involved in tumor metastasis [50]. The EOs' bioactive compounds against colorectal cancer models are summarized in Table 1 and Fig. 1.
Table 1.
Chemical composition of EOs and the correlation with different CRC experimental models
| Plant species | Family of plants | Tested CRC cell lines |
Concentration | Potential mechanism | Main chemical compounds | Refs. |
|---|---|---|---|---|---|---|
|
Lavandula stoechas ssp. stoechas |
Lamiaceae Labiatae | COL-2 | IC50 = 9.8 μg/mL | Not available | pulegone, hexahydrothymol, menthone | [51] |
|
Annona Cheirmola Annon squamosa Annona Abdel Razik |
Annonaceae | HCT116 |
IC50 = 2.1 μg/mL IC50 = 0.7 μg/mL IC50 = 0.7 μg/mL |
Not available |
α-pinene, β-pinene, α-copaene, 2-carene isocaryophyllene, caryophyllene |
[52] |
| Cymbopogon flexuosus | Poaceae |
HT-29 HCT-15 SW-620 502,713 |
IC50 = 42.4 μg/mL IC50 = 60.2 μg/mL IC50 = 28.1 μg/mL IC50 = 4.2 μg/mL |
Not available | not available | [53] |
| Illicium verum | Asteraceae Compositae |
HCT-116 HT-29 CCD-18co |
IC50 = 50.34 μg/mL IC50 = 100 μg/mL IC50 = 200 μg/mL |
↑Apoptosis ↓ Metastasis |
tans-anethole elaidic acid palmitic acid |
[54] |
| Commiphora molmol | Burseraceae | HCT-116 | IC50 = 19.71 μg/mL | Not available |
2-acetoxy-furano-diene furanoeudesma-1,3-diene furanoeudesma-1,4-dien-6-one isofuranogermacrene |
[55] |
| Capparis spinosa L | Burseraceae | HT-29 | Not available |
↓Proliferation, ↓NF-kB no apoptosis in HT-29 cells ↑Cell cycle arrest G2/M phase |
methyl isothiocyanate | [56] |
|
L. hybrid Re L. latifolia Medikus L. vera D.C |
Lamiaceae Labiatae | Caco-2 |
IC50 = 0.9132 mg/mL IC50 = 0.7798 mg/mL IC50 = 1.224 mg/mL IC50 = 1.631 mg/mL |
↑ROS/RNS, ↓Akt ↓mTOR ↓MAPK, ↓NF-κB |
linalool linalyl acetate 1,8-cineole |
[57] |
| Cinnamomum glanduliferum Bark | Lamiaceae | HCT-116 | IC50 = 9.1 μg/mL | Not available |
eucalyptol, terpinen-4-ol α -terpineol |
[58] |
|
Achillea fragrantissima |
Asteraceae |
SW48 HCT116 |
IC50 = 110.1 μg/mL IC50 = 134.6 μg/mL |
Not available |
Artemisia ketone camphor, α-bisabolol |
[59] |
| Grapefruit | Rutaceae | HCT116 | Not available | Dose-dependent antiproliferative activity |
nerylisovalerate, 1,8-cineole neryl-2-methyl-butanoate chamazulene, linalool, camphor germacrene D, nerol linalyl propionate |
[60] |
| Artemisia dubia Wall | Asteraceae | IC50 = 31.25 μg/mL | Not available |
limonene, linalyl acetate γ-terpinene, linalool β-pinene, bergapten |
[61] | |
| Ocimum viride | Lamiaceae Labiatae |
HT-29 502,713 SW-620 |
IC50 = 0.034 μL/mL |
↑DNA damage ↑Cells death ↑Apoptotis |
thymol, γ -terpinene p-cymene |
[62] |
| Cinnamomum stenophyllum (Meisn.) Vattimo-Gil | Lauraceae | HCT116 | IC50 = 9.95 μg/mL | Not available |
eugenol, safrol, benzyl benzoate, 1,8-cineole, camphor |
[63] |
|
Citrus aurantifolia (Christm.) Swingle |
Rutaceae |
NIH3T3 SW-480 |
IC50 = 6.25 μg/mL |
↑DNA fragmentation ↑caspase-3 ↑Bax/Bcl2 |
D-Limonene, D-Dihydrocarvone α -Terpineol |
[64] |
| Citrus limettioides | Rutaceae | SW480 | IC50 = 50 μg/mL | ↑Apoptosis |
d-Limonene triacontane α-Bisabolene α-Farnesene (R)-( +)-Citronellol |
[65] |
|
Heracleum pastinacifoliu Heracleum persicum Heracleum rechingeri Heracleum transcaucasicum |
Apiaceae | LS180 | IC50 = 1.4 mg/mL | Not available |
myristicin (E)-anethole hexyl butanoate elemicin |
[66] |
| Comptonia peregrina L | Myricaceae | DLD-1 | IC50 = 47 μg/mL | Not available |
β -caryophyllene, α-humulene, β -myrcene |
[67] |
| Cotula cinerea (Delile) | Asteraceae | HCT116 |
IC50 = 86.7 μg/mL IC90 = 122.3 µg/mL |
Not available |
trans-thujone santolina triene, α- pinene, sabinene, 1,8-cineole |
[68] |
| Leonotis nepetifolia | Lamiaceae Labiatae | IC50 = 16.78 mg/mL | Not available |
germacrene D, α-humulene, 3-octanone, (E)-ocimene, (Z)-ocimene, linalool, β -caryophyllene, 1-octen-3-ol |
[69] | |
| Eryngium campestre Eryngium amethystinum | Apiaceae |
IC50 = 1.65 μg/mL IC50 = 1.64 μg/mL |
Not available |
germacrene D, spathulenol, alloaromadendrene, ledol, γ-cadinene, β -Elemene |
[70] | |
| Tagetes erecta L | Asteraceae | HT29 | IC50 = 6.94 μg/mL | Not available |
limonene (10.4%), dihydrotagetone (11.8%), terpinolene (18.1%), (E)-ocimenone (13.0%) |
[71] |
| Tetradenia riparia (Hochst.) | Lamiaceae Labiatae | IC50 = 77.47 μg/mL |
fenchone (6.1%), dronabinol (11.0%), aromadendrene oxide (14.7%) (E,E)–farnesol (15.0%) |
|||
| Bidens sulphurea (Cav.) | Asteraceae | IC50 = 268.8 μg/mL |
(E)-caryophyllene(10.5%) germacrene D (35.0%) 2,6-di-tert-butyl-4-methylphenol (43.0%) |
|||
| Foeniculum vulgare Mill., | Apiaceae | Not available |
limonene (21.3%) (E)-anethole (70.2%) |
|||
| Piper betel L | Piperaceae | RCM-1 | IC50 = 500 μg/mL | Duct formation after treated with EO | chavicol, chavibetol, cineol, eugenol | [72] |
| Cymbopogon nadus L | Poaceae |
octyl acetate (54.9–60.2%) octyl butyrate (10.1–13.4%) |
||||
| Syzygium aromaticum L | Myrtaceae |
eugenol, eugenyl acetate, β-caryophyllene, α-humulene |
||||
| Alpinia galanga L | Zingiberaceae |
1,8-cineol, alpha-pinene, eugenol, camphor, methyl cinnamate |
||||
| Psidium guajava L | Myrtaceae |
β-caryophyllene, cineol |
||||
| Ocimum americanum L | Lamiaceae Labiatae |
limonene, 1,8-cineol, δ-cadinene, α-pinene α-terpineol |
||||
| Ocimum tenuiflorum L |
camphor, cineol, eugenol, limonene, rosmarinic acid |
|||||
| Citrus hystrix DC | Rutaceae | β-pinene, limonene, caryophyllene, sabinene, citronellol, 1,8-cineol | ||||
|
Cymbopogon citratus (DC) Stapf |
Poaceae |
citral, myrcene, geraniol, nerol, farnesol, citronellol |
||||
|
Boesenbergia rotunda (L.) Mansf |
Zingiberaceae |
camphene, eucalyptol, ocimen, camphor, geraniol |
||||
|
Citrus aurantifolia (Christm. et Panz.) Swings |
Rutaceae |
D-limonene, pinene, camphene, bergapten |
||||
| Ocimum basilicum L | Lamiaceae Labiatae |
estragole, linalool, 1,8-cineole |
||||
|
Curcuma longa L |
Zingiberaceae |
turmerone, aromatic (ar-) turmerone |
||||
| Rosa damascena | Rosaceae | SW742 | IC50 = 10 μg/mL | ↓Cell proliferation | not available | [39] |
| Pistacia atlantica | Anacardiaceae | Caco-2 HCT116 |
IC50 = 62.85 μg/mL IC50 = 34.97 μg/mL |
Not available | α-pinene, sabinene, limonene, terpinene-4-ol, β-pinene | [73] |
| Phoebe bournei (Hemsl.) | Laureaceae | SW480 | IC50 = 41.3 l μg/mL | Not available |
α-copaene, α-muurolene, δ-cadinene, 1 s-calamenene |
[74] |
|
Ammodaucus leucotrichus Cosson & Durieu |
Apiaceae | HCT116 | IC50 = 41.3 l μg/mL | Not available |
perillaldehyde, D- limonene α-pinene |
[75] |
| Inula graveolens (Linnaeus) Desf | Linnaeus | HT29 | IC50 = 24.6 μg/mL | Not available |
bornyl acetate, corneol caryophyllene oxide δ-cadinol, camphene |
[76] |
| Ocimum viride | Lamiaceae Labiatae | COLO 205 |
IC50 = 0.070, 0.058, 0.033 μg/mL at 24, 48, and 72 h, respectively |
↑DNA damage ↑mitochondrial membrane permeability ↑apoptosis |
thymol, α-pinene geranyl acetate β-caryophyllene oxide |
[77] |
| Artemisia indica Wild | Asteraceae | Caco-2 | IC50 = 19.5 μg/mL | Not available | Artemisia ketone, germacrene B borneol cis-chrysanthenyl acetate | [78] |
| Pogostemon cablin | Lamiaceae Labiatae |
HCT116 SW480 |
Not available |
↑p21 ↓Cyclin D1 ↓CDK4 |
not available | [79] |
| Eugenia uniflora | Myrtaceae | HCT-116 |
IC50 = 16.26 μg/mL IC50 = 9.28 μg/mL |
Not available |
curzerene, selina-1,3,7(11)-trien-2- one, selina-1,3,7(11)-trien-2-one epoxide, germacrene B, caryophyllene oxide, (E)-caryophyllene |
[80] |
| Origanum onites L | Origanum | HT-29 | IC50 = 0.35 μg/mL | Not available |
terp-1-in-4-ol, sabinene hydrate, γ-terpinene, p-cymene α-terpineol |
[81] |
| Stachys viticina Boiss | Lamiaceae Labiatae | Colo-205 | Not available | Not available |
endo-borneol, eucalyptol epizonarene |
[82] |
| Moringa oleifera | Moringaceae | Caco-2 | ↑Cytotoxicity |
↑Morphological alterations ↑Cell blebbing and vacuolation ↑Autophagy ↑Cancer cell death |
not available | [83] |
| Citrus bergamia Risso et Poiteau | Rutaceae | Human and rat isolated CRC cells | Not available | EOs inhibited neuronally-mediated contractions in the rat and human CRC |
(R)-( +)-limonene linalyl acetate linalool |
[84] |
| Melissa officinalis | Lamiaceae Labiatae |
HT-29 T84 |
IC50 = 346 μg/mL IC50 = 120 μg/mL |
↑Cell cycle arrest ↑Apoptosis |
not available | [85] |
| Mesua ferrea | Calophyllaceae |
HCT 116 IM1215 |
IC50 = 17.38 μg/mL IC50 = 18.86 μg/mL |
↑Morphological and biochemical changes in HCT 116 | isoledene, elemene | [86] |
| Origanum majorana | Lamiaceae Labiatae | HT-29 | Not available |
↑Autophagy ↑Apoptotis ↑p38, ↑MAPK |
terpinen-4-ol, alpha-terpinol α-pinene, camphene, p-cymol β-caryophyllene, bicyclogermacrene, neophytadiene |
[87] |
| Thymus alternans |
HCT-15 HCT116 |
IC50 = 5–8 l μg/mL | Not available |
(E)-nerolidol, (E)-β-Ocimene geranial |
[88] | |
| Mentha citrata | HCT116 |
IC50 = 80.6 μg/mL IC90 = 119.1 μg/mL |
Not available |
linalool. linalyl acetate 1,8-cineole, a-terpineol |
[89] | |
|
Teucrium alopecurus |
Not available |
↑Apoptosis ↓Cells survival ↓Proliferation ↓Invasion ↓Angiogenesis ↓Metastasis |
( +)-epi-bicyclo sesquiphellandrene α-bisabolol, Ƭ-muurolol α-cadinol, β-phellandrene d-limonene |
[90] | ||
|
Ocimum basilicum, Mentha spicata, Pimpinella anisum, Fortunella margarita |
Lamiaceae Apiaceae Rutaceae |
Caco2 |
Sweet basil IC50 = 0.071 mg/mL Kumquat IC50 = 0.1 mg/mL Spearmint IC50 = 0.162 mg/mL Anise IC50 = 0.25 mg/mL |
Not available |
carvone in spearmint methyl chavicol in sweet basil trans-anethole in anise limonene in kumquat |
[91] |
| Pinus roxburghii | Pinaceae | HCT116 | IC50 = 25.0 μg/mL | ↑Apoptosis |
α-pinene caryophyllene oxide 3-carene β-pinene |
[92] |
| Artemisia santonicum | Asteraceae | HCT116 | Not available |
↓Pro-inflammatory factors ↓Cell growth ↓Cancer cells survival |
camphor, 1,8-cineole α-thujone borneol, β-thujone |
[93] |
| Smyrnium olusatrum L | Apiaceae | HCT116 | IC50 = 10.71 μg/mL |
↑DNA fragmentation ↑Phosphatidylserine ↑Caspase-3 |
isofuranodiene germacrone furano-4(15)-eudesmen-1-one furanoeremophil-1-one 1β-acetoxyfuranoeudesm-4(15)-ene |
[94] |
| Zataria multiflora Boiss | Lamiaceae Labiatae |
HCT116 SW48 |
Not available |
↓Cell proliferation ↑Apoptosis |
not available | [95] |
| Zedoary Turmeric | Zingiberaceae | HCT116 | IC50 = 101 μg/mL |
↓Growth of cancer cells ↑Senescence ↑Apoptosis |
not available | [96] |
| Artemisia campestri | Asteraceae | HT-29 | Not available | Not available |
A.Campestris: β-pinene, limonene,, germacrene-D, γ-terpinene, β-myrcene, α-pinene, (Z)-β-ocimene (E)-β-ocimene |
[97] |
| Croton lechleri | Cynomoriaceae | LoVo | IC50 = 74.95 μg/mL | ↑Change in fatty acid composition | sesquicineole, α-calacorene, 1,10-di-epi-cubenol,, β-calacorene, epicedrol | [98] |
| Allium Roseum L | Alliaceae |
HT-29 Caco-2 |
IC50 = 4.64 μg/mL IC50 = 8.22 μg/mL |
Not available |
methyl methanethiosulfinate, 3-vinyl.1,2-dithiacyclohex-5-ene diallyl trisulfide |
[99] |
| Chrysanthemum coronarium L | Asteraceae | Caco-2 | IC50 = 43.0 μg/mL | Not available | not available | [100] |
| Beilschmiedia erythrophloia | Lauraceae | HT-29 | IC50 = 18.9 μg/mL | Not available |
β-caryophyllene, α-humulene terpinen-4-ol, cis-β-ocimene, sabinene, limonene |
[101] |
| Machilus mushaensis | Lauraceae | IC50 = 3.8 μg/mL | Not available | n-decanal, α-cadinol | [102] | |
| Porcelia macrocarpa | Annonaceae | IC50 = 50.8 μg/mL | Not available | germacrene D, bicyclogermacrene | [103] | |
| Neolitsea variabillima | Lauraceae | IC50 = 16.8 μg/mL | Not available |
β-ocimene, α-cadinol, terpinen-4-ol, τ-cadinol, β-caryophyllene, sabinene |
[104] | |
| Diospyros discolor | Ebonaceae | IC50 = 10.6 μg/mL | Not available |
(2Z,6E)-farnesol, α-cadinol, (E)-nerolidol, Ƭ-cadinol, Ƭ-muurolol, α-humulene, β-caryophyllene |
[105] | |
| Machilus thunbergii | Lauraceae | IC50 = 3.8 μg/mL | Not available |
n-decana, β-caryophyllene α-humulene, β-eudesmol |
[106] | |
| Salvia libanotica | Lamiaceae Labiatae |
HCT116 p53 + / + HCT116 p53-/- |
Not available |
↑Apoptosis ↑Caspase-3 in p53 + / + cancer cells but not p53-/- cells |
not available | [107] |
| Origanum vulgare | Lamiaceae Labiatae | HT-29 | Not available | Not available | 4-terpineol, thymol, γ-terpinene, carvacrol | [108] |
| Athanasia brownii | Asteraceae | HCT116 | IC50 = 29.5 μg/mL | Not available |
selin-11-en-4a-ol, caryophyllene oxide humulene epoxide II (E)-nerolidol |
[109] |
|
Afrostyrax lepidophyllus, Scorodophloeus zenkeri |
Huaceae, Fabaceae |
IC50 = 12.4 μg/mL IC50 = 8.5 μg/mL |
Not available | 2,4,5,7-tetrathiaoctane | [110] | |
|
Salvia officinalis |
Lamiaceae Labiatae |
HT-29 Caco-2 HCT116 |
Not available | ↑Morphological changes |
α-thujone 1,8-cineole, camphor |
[111] |
| Hedychium spicatum | Zingiberaceae |
LD-1 SW620 |
IC50 = 26.75–94.35 mg/mL | Not available | 1,8-cineol, hedycaryol, β-eudesmol, Ƭ-eudesmol, cubenol, α-cadinol | [112] |
| Allium sativum | Allium | HT-29 c | Not available | ↑Apoptotis | not available | [113] |
| Moringa oleifera | Moringaceae | Caco-2 | Toxicity% = 49.7% | ↓Cell viability | not available | [83] |
| Myristica fragrans | Myristicaceae | Caco-2 | Not available | Not available |
myristicin, sabinene, α-pinene β-pinene, β-Phellandrene safrole, terpinen-4-ol |
[114] |
| Callistemon citrinus | Myrtaceae | Colo-205 | Not available | Not remarkable activity |
α-pinene, limonene α-terpineol in leaf oil, 1,8-cineole α-pinene in flower oil |
[115] |
|
Eugenia egensis Eugenia flavescens Eugenia polystachya Eugenia patrisii |
Myrtaceae | HCT-116 | IC50 = 10.5–216.3 mg/mL | ↑Cell membrane disruption |
5-hydroxy-cis-calemene (2E,6E)-farnesol, (2E,6Z)-farnesol caryophylla-4(12),8(13)-dien-5-ol-5 -ol E–bisabolene, germacrene D, and ishwarane |
[116] |
| Aquilaria crassna | Thymelaeaceae | IC50 = 28.0 μg/mL |
↑Apoptotis ↑DNA fragmentation ↑mitochondrial damage |
β-caryophyllene 1-Phenanthrenecarboxylic acid 2-naphthalene-methanol α-caryophyllene benzenedicarboxylic acid Azulene, naphthalene, cyclodecene |
[117] | |
| Nectandra leucantha | Lauraceae | HCT | IC50 = 194.8 μg/mL | Not available |
bicyclogermacrene germacrene A spathulenol, globulol |
[118] |
| Semenovia suffruticosa | Apiaceae | HT-29 | IC50 = 341 μg/mL | Morphological changes |
Z-β-ocimene linalool, β-bisabolol |
[119] |
| Piper aequale | Piperaceae | HCT-116 | IC50 = 8.68 μg/mL | Not available |
δ-elemene, β-pinene, α-pinene, cubebol, β-atlantol bicyclogermacrene |
[120] |
| Pistacia lentiscus var. chia | Anacardiaceae |
HT-29 Caco-2 CT26 |
IC50 = 0.1752 mg/mL IC50 = 0.0368 mg/mL IC50 = 0.1335 mg/mL |
↓Proliferation of colon cancer cells |
α-pinene myrcene |
[121] |
|
Faeniculum vulgare |
Apiaceae | HCT-116 | Not available |
↓DNA damages ↓mitochondrial membrane potential loss |
not available | [122] |
Symbols: ↑increase, ↓decrease
Fig. 1.
Diagram with the most representative anticancer molecular mechanism of natural EOs. Legend: ↑increase, ↓decrease, Nuclear factor erythroid 2-related factor 2 (Nrf2), Reactive oxygen species (ROS), Deoxyribonucleic Acid (DNA), Heat shock proteins (Hsps), Interleukin (IL), Tumor necrosis factor (TNF), Forkhead box P3 (FOXP3)
Cytotoxic and antiproliferative effects of EOs
The EO from rhizome of Curcuma purpurascens BI. demonstrated cytotoxic effects against HT-29 cells (IC50 value 4.9 ± 0.4 μg/mL) [123]. In 2009, Sharma and coworkers reported that the lemongrass EO (Cymbopogon flexuosus (Nees ex Steud.) W.Watson) showed promising anticancer activity and caused a loss in tumor cell viability by activating the apoptotic process. The IC50 values were 4.2 and 4.7 μg/ml for 502,713 (colon) and IMR-32 (neuroblastoma) cell lines, respectively [53].
Blood oranges EO, a variety of orange (Citrus × sinensis), showed pro-apoptotic and anti-angiogenesis potential on colon cancer cells [124]. Volatile EO isolated from Artemisia campestris L. exhibited significant antitumor activity against the HT-29 cells and it is recommended for further research into the chemoprevention and treatment [97, 125].
Thymoquinone (TQ) is a volatile secondary metabolite found in many species including Nigella sativa L. (black cumin) and Monarda fistulosa L. This monoterpene exhibited anti-proliferative activity against Caco-2, HCT-116, LoVo, DLD-1 and HT-29 cell lines, but not against human intestinal FHs74Int cells [126]. More recently two interesting reviews extensively explored TQ effects in preclinical settings. The first one suggested as TQ could increase the efficacy of chemotherapeutic agents in CRC, in addition to other common cancers (i.e. lung, liver, breast, prostate, etc.), inducing the authors to recommend this combination strategy to fight cancer [127]. Similarly, the other work investigated the combination regimen of TQ and chemotherapy, but also examined the use of nanotechnologies incorporating TQ, encouraging clinicians to test this molecule in clinical trials [128].
Carvacrol-rich EO of Origanum onites L. was evaluated in twenty female BALB/c mice xenograft of colon cancer cells (CT26). Origanum onites EO was administered orally at a daily dose of 0.370 g/kg of animal body weight for 13 days [81]. The authors reported that colon cancer cells were the most sensitive to Origanum onites EO [55, 81]. On the same line, another work obtained an IC50 of carvacrol corresponding to 92 µM and 42 µM for HCT-116 and HT-29 cells, respectively [129].
EOs obtained from Rosa x damascena were studied in 2D cell models of the RKO cell line (colorectal cancer) and HEK293-T cell line (human embryonic kidney), while for 3D cell models were used only MCF7 cell line (breast cancer). Indeed, in the RKO 2D cell line, the most active EOs were those extracted by S. tortuosum and O. maritimus, which possessed an IC50 of 0.034 and 0.34 μl/mL, respectively. Moreover, Murata and collaborators showed that 1,8-cineole exerted antitumor activity on HCT-116 and RKO cell lines [130]. The authors explored the antiproliferative effect of 1,8-cineole, with an IC50 > 10 mM for both cell lines and found induction of apoptosis via activation of the caspase-dependent pathway starting as 25 mM for RKO cell lines.
The EO of Cinnamomum stenophyllum (Meisn.) Vattimo leaf has been shown potent cytotoxic effect on HCT-116 cells [131]. This effect on HCT-116 cells has been demonstrated by exposing cells to: a) extracts of 3 Annona species (A. squamosa L., A. cherimola Mill., and the hybrid between them—Abdel Razek), b) oil and extracts of Eugenia uniflora L., and EO of Commiphora myrrha (Nees) Engl., c) EO from Piper aequale Vahl, d) EO from Thymus roegneri K. Koch, e) EO isolated from the bark of Cinnamomum glanduliferum (Wall.) Meisn., f) light phase obtained by molecular distillation of grapefruit [55, 58, 60, 80, 88, 120, 132]. The same cytotoxic effect has been achieved in HT-29 cells by exposing them to Dittrichia graveolens (L.) Greuter EO, Machilus thunbergii Siebold & Zucc. EO and Diospyros discolor Willd. flower. The latter two also exhibited antineoplastic properties on a panel of cancer cells, suggesting a wider effect in different cancer types [105, 106, 133]. On the other hand, the EO of bulbs Allium roseum L. presented an antiproliferative dose-dependent effect against two human colon adenocarcinoma cell lines, HT-29 and Caco-2 [99]. Besides, the EO of Achillea fragrantissima (Forssk.) Sch.Bip. revealed an IC50 of 110.1 and 134.6 µg/mL on human colorectal cancer cells (SW480 and HCT-116) [59].
In a recent study, anticancer effects of Eryngium campestre L. and Eryngium amethystinum L. were studied, showing IC50 values (1.65–5.32 and 1.5–2.99 µg/mL for E. amethystinum and E. campestre, respectively) comparable or close to those of the chemotherapeutic drug cisplatin [70]. A more selective effect was observed with Brocchia cinerea (Delile) Vis. EO, in two human cancer cell lines HCT-116 and liver cancer cell line (HePG2): the results indicated that such EO possessed a significant (66.9%) cell growth inhibition capacity in colon cancer cells [134].
Eucalyptol from the EO of Cinnamomum glanduliferum (the main compound) showed great antitumoral potential in HCT-116 cells with IC50 of 9.1 μg/ml [58]. Moreover, the molecular mechanisms of Mesua ferrea L. oil-gum resin extract on colon cancer cells HCT-116 and LIM1215 were studied. The extract could negatively regulate the expression of multiple pro-survival proteins, such as survivin, xIAP, HSP27, HSP60, and HSP70, and increase the expression of reactive oxygen species (ROS), caspase-3,7 and TRAIL-R2 in HCT-116 [86].
It has been demonstrated that the EO of Salvia officinalis L., showed antiproliferative effect based on cell cycle arrest. Through MTT test, at 72 h Caco-2, HT-29, and HCT-116 cells were treated with different concentrations of EOs, exhibiting a dose-dependent cell growth inhibition. Moreover, when analyzing all the possible combinations of the 3 main compounds of the EO, i.e. α-tujona, eucalyptol, and camphor, the same effect was observed. In addition, S. officinalis EOs induced cell cycle arrest at the G2/M phase in Caco-2 and HCT-116 cells and the S phase in HT-29 cells. Concomitantly, the treatment with a combination of the three main components increased the percentage of Caco-2 and HCT-116 cells in G0/G1 and HT-29 cells in G2/M. It is worth highlighting that normal colon epithelial cell line FHC was not affected by the same treatment [111]. It also analyzed the effect on cell proliferation of Melissa officinalis L. extract on HT-29 and T84 human colon adenocarcinoma cells. The results showed that after 3 and 4 days of treatments there was a growth inhibition of HT-29 and T84 cells with an IC50 of 346 and 120 μg/mL, respectively. This antiproliferative effect was associated with a cell cycle arrest in the G2/M phase [85].
Another study suggested that certain EOs might have a chemopreventive and antimetastatic effect. For example, EOs obtained from the fruits of Illicium verum Hook. f. decreased cell migration ability of HCT-116 cells in a dose-dependent manner (25, 50, and 90 μg/mL), already at 24 h of treatment [50]. Differently from previous findings, other EOs showed lesser anticancer effects. The EO of Leonotis nepetifolia (L.) R.Br. and several isolated compounds (hentriacontane, phyllo palmitate, stigmasteryl glycoside, 6,7-dimethoxy-5,3',4'trihydroxyflavone, apigenin-7-O-glucoside, and luteolin-7-O-glucoside) showed a low cytotoxic effect on HCT-116 cells [69]. In addition, EOs from different Eugenia species (E. egensis DC., E. flavescens DC., E. polystachya Rich., and E. patrisii Vahl) revealed that the most active EO was extracted from E. polystachya, at least in HCT-116 cell model. The E. flavescens and E. patrisii EOs, on the other hand, showed greater toxicity on normal MRC5 cells (human fibroblasts) [116]. Overall, these results do not limit the possibility of improving and innovating the cancer therapy by EOs, rather they should be considered as a stimulus to search for a more successful and reliable therapy against CRC.
Pro-oxidant and antioxidant effects of EOs
Oxidative stress is one of the causes of cell and DNA damage that can trigger the development of many diseases. [21, 135–137]. The use of a pro-oxidant strategy has been proposed to damage the modified tissues selectively [138]. Therefore, the search for bioactive compounds with antioxidant capacity is a strategy to prevent this problem [139–141]. Numerous studies are showing antioxidant properties using in vitro tests such as DPPH or FRAP, but few exist in cell lines of human colon cancer (i.e. Caco-2, HCT-116, LoVo, DLD-1 and HT-29).
EOs from the bulb of Allium roseum L., rich in sulphur compounds as methyl methanethiosulfinate, showed an interesting antiproliferative activity against HT-29 and Caco-2 cells in a dose-dependent manner. It also showed antioxidant activity in FRAP and DPPH assays, and the ability to inhibit the production of superoxide anion in the above-mentioned cell lines [99]. In another study, the treatment of HCT-116 and HT-29 cells and primary fetal colon cells (FHC) with cinnamaldehyde and an ethanolic extract of cinnamon bark (Cinnamomum cassia (L.) J.Presl), upregulated cellular protein levels of Nrf2, increased cellular levels of glutathione and protected HCT-116 cells against hydrogen peroxide-induced genotoxicity and arsenic-induced oxidative damage [142].
The antioxidant activity of EOs could protect DNA and tissues from damage caused by oxidative stress and ROS (reactive oxygen species) [143, 144]. A recent study in HT-29 cells showed that certain chemical compounds in EOs such as nerolidol, thymol, geraniol, methyl isoeugenol, eugenol, linalool and a commercial mixture (Agolin) showed antioxidant as well as cytotoxic activity against this cell line [145]. Genoprotection against oxidative DNA damage was also observed for all studied compounds, being thymol (at 12.5 ppm) the most protective compound against oxidative DNA damage. Geraniol (at 125 ppm) also protected cells against DNA damage by methylation. Another study investigated the cytotoxic, genotoxic, and DNA protective effects of carvacrol and thymol in HepG2 and Caco-2 cell lines. Both compounds did not induce DNA chain breaks in any cell line, and in the presence of hydrogen peroxide, they offered significant protection against DNA strand breaks [146].
The effects of fennel EO, Foeniculum vulgare Mill., were evaluated against the toxicity induced by an insecticide-triflumuron in HCT116 cells [5]. When cells were pretreated with this EO, rich in estragole, cell viability was augmented while ROS generation was modulated by increasing CAT and SOD activities; MDA levels were also reduced compared to cells which were treated only with insecticide [122]. Although these results show that fennel EO has antioxidant activity and reduces DNA damage, it could increase the viability of a cancerous cell line, even if not reported by the authors.
The essential oil from Myrica rubra Siebold & Zucc. leaves has been showed mild antioxidant activity in a non-cancerous cell line from a primary culture of rat hepatocytes, however, it demonstrated a strong pro-oxidative effect on Caco-2 cancer cells due to increased production of ROS [147]. Furthermore, this EO combined with doxorubicin improved its antiproliferative and pro-oxidant properties in cancer cells. The chemical composition of M. rubra EO presents β-caryophyllene (43%), α-humulene (22%), humulene epoxide I (8%), valencene (6%), epi-α-selinene (6%), γ-muurolene (3%), β-caryphyllene-oxide (3%) and transnerolidol (2%) [148]. As a side result, it is noteworthy that this EO showed a significant antiproliferative effect in several intestinal cancer cell lines [149]. Another study investigated the antioxidant capacity of carvacrol, thymol and their mixture (10:1) in Caco-2 cells by measuring ROS production. It was observed that carvacrol and the mixture at high concentrations induced oxidative stress, while at low concentrations showed protection against lipid peroxidation and protein oxidation induced by hydrogen peroxide [150].
EOs have shown different properties to redox conditions. On one hand, the antioxidant properties could reduce the damage associated with ROS production preventing the conversion of benign cells into cancer cells, as well as DNA damage, but on the other hand, a pro-oxidant condition could also be a strategy to attack cancerous tissues (Table 2). This antioxidant-prooxidant activity of sesquiterpenes has been already reported [151].
Table 2.
In vitro Antioxidant activities of EOs and isolated compounds
| Type of EO | Tested cell lines | Results | Refs. |
|---|---|---|---|
| Allium roseum bulb EO |
HT-29 CaCo-2 |
↓Production of superoxide anion | [99] |
|
Cinnamaldehyde Cinnamon bark extract |
HCT-116 HT-29 FHC |
↑Nrf2, ↑cellular glutathione ↓Oxidative stress |
[142] |
| Thymol | HT-29 | ↑ Protection of the colonic epithelium against oxidative DNA damage | [145] |
| Geraniol | HT-29 | ↑Protection from DNA methylation damage | [145] |
|
Carvacrol Thymol |
Caco-2 | ↑Antioxidant properties against DNA strand breaks | [146] |
| Fennel (Foeniculum vulgare) EO | HCT-116 |
↑Cell viability, ↑Antioxidant properties ↑DNA protection |
[122] |
| EO from Myrica rubra leaves | Caco-2 | ↑Selective pro-oxidative effect on cancer cells | [147] |
| Thymoquinone | DLD-1 |
↑Pro-oxidative effects ↑Apoptosis |
[126] |
| Carvacrol | Caco-2 |
↑Pro-oxidative effects at high doses ↑Antioxidant effects at low concentrations |
[150] |
Antimutagenic effects of EOs
As described in the previous section, some components of EOs can be considered potential antimutagenic compounds since they are capable of protecting DNA against ROS-induced toxicity. Thymol, geraniol and fennel EOs have demonstrated this potential antimutagenic effect due to their antioxidant properties [122, 145]. The essential oil from Croton lechleri Müll. Arg. stem bark showed a protective efficacy in Ames test against mutagenic heterocyclic amines such as 2-amino-3-methylimidazo-[4,5-f]quinoline and 2-amino-3,4- dimethylimidazo-[4,5-f]quinolone [98]. It might be due to the inhibition of the metabolic activation via P450 and the blocking of mutagen access to DNA. It also showed antiproliferative properties in the LoVo and HepG2 cell lines. This EO contains 76.93% of sesquiterpenes, being sesquicineole the major compound, and 18.89% of monoterpenes, being the limonene the major representative.
Anti-inflammatory effects of EOs
Inflammation is initiated/mediated by oxidative stress, which induces cytokines (mainly TNF-α, IL-6 or IL-10) production in response to an external or pathophysiological agent [152]. Both ROS and cytokines may activate different lymphocytes to encounter inflammation [153, 154]. During the inflammatory process, other mediators, such as nitric oxide (NO), interleukin 1 beta (IL-1β), histamine or PAF may have a role in the harmful mechanism [23, 155, 156]. Chronic exposure to all these mediators may lead to increased cell proliferation, mutagenesis, oncogene activation, and angiogenesis [157, 158]. Usually, plant extracts have been proved as anti-inflammatory agents due to the presence of polyphenols, such as phenolic acids; however, EOs and monoterpenes have been scarcely tested as anti-inflammatory compounds in cancer conditions [159]. Chronic inflammation and its associated infections account for approximately 20% of cancer-related deaths [160–162]. Turmeric has been used as a medicinal herb for thousands of years for the treatment of various disorders. Although curcumin is the most studied active constituent of turmeric, accumulating evidence suggests that other components of turmeric have additional anti-inflammatory and anti-tumorigenic properties [163]. Some studies have shown that curcumin preparations containing turmerone and turmeric EOs revealed that anti-inflammatory cytokines including IL-10 and IL-11 as well as FOXP3 were upregulated in the colon. The combined treatment of curcumin and turmerone provides superior protection from dextran sodium sulfate-induced colitis than curcumin alone, highlighting the anti-inflammatory potential of turmeric [164].
Myrcene and α-pinene are monoterpenes found in the aerial parts (leaves, twigs and berries) of Pistacia lentiscus L. They have been well characterized for their antibacterial and anti-inflammatory properties. Nonetheless, poor information exists on their potential anticancer activity. An increasing number of studies has revealed that EOs from P. lentiscus L. trunk resin (namely mastic gum) which contains α-pipene, β-pipene, β-myrcine, linalool, trans-caryophyllene and camphene, may exert anticancer activity in several types of human neoplasia, including prostate and colon carcinomas as well as haematological malignancies [165–167]. Particularly, hexane and ethanolic extracts of mastic gum were shown to induce p53- and p21-independent G1-phase arrest followed by apoptosis in human colon cancer HCT-116 cells in vitro [168, 169].
Another research revealed a dose-dependent reduction of tumour cell viability induced by myrcene and α-pinene in Caco-2 cells. Intracellular ROS production slightly increased according to P. lentiscus EOs exposure, but it was one of the lowest ROS levels compared to other cell lines. Probably the reason was that the concentrations tested in this assay were too high (640 µg/mL) [170]. Previously, anti-inflammatory properties were reported for limonene, β-pinene and γ-terpinene, which reduced leukocyte migration to the damaged tissue and exhibited anti-inflammatory activity [171, 172].
Thymus alternans K. EO has also demonstrated anti-inflammatory properties and antiproliferative activity in HCT-15 and HCT-116 cells. Such effect was specifically due to nerolidol, the main volatile component of T. alternans [88]. This sesquiterpene was also responsible for the cytotoxic activity of Comptonia peregrina L. Coulter, a native plant from Canada used in traditional medicine against cancer, in the human colon adenocarcinoma cell line DLD-1 [88].
Table 3 summarizes the anti-inflammatory properties of the EOs tested on different colon cancer cell lines. Generally, monoterpenes and sesquiterpenes seem to be the most active compounds. These terpenes have not only demonstrated an anti-inflammatory effect, but also concomitant antiproliferative and antibacterial ones. As inflammation is related to oxidative stress, these results are well linked to those exposed in “Anti-inflammatory effects of EOs” section.
Table 3.
Anti-inflammatory effects of EOs and isolated compounds
| EO | Tissue or cells | Results | References |
|---|---|---|---|
| Turmerone | Mouse colon cells |
Anti-inflammatory ↓IL-10,↓ IL-11, ↑FOXP3 |
[164] |
|
EO from leaves, twigs and berries of Pistacia lentiscus |
HCT-116 |
Antibacterial ↓Pro-inflammatory markers ↓NO, ↓PGE2, ↓TNF-α |
[165–167] |
|
Turmerone Tocotrienol |
HT-29 HCT-116 |
↓Growth of colon cancer cells | [173] |
| Thymoquinone |
COLO-205 HCT-116 |
↓Phosphorylation of p65 protein ↓NF-κB, ↑Apoptosis |
[174] |
| Nerolidol |
HCT-15 HCT-116 DLD-1 |
↓Pro-inflammatory cytokines ↓TNF-α, ↓IL-1β Antiproliferative |
[88] |
↑increase, ↓decrease
TNF-α Tumor necrosis factor alpha, FOXP3 Forkhead box P3, PGE2 Prostaglandin E2, IL Interleukin, NO Nitric oxide
The synergistic anticancer effect of EOS associated with other bioactive compounds or conventional chemotherapy
The synergy between different compounds is a sought-after effect in the fight against cancer. Such effect of the essential polyphenolic compounds of curcumin, the EO of turmeric (ETO-Cur), and the tocotrienol-rich fraction (TRF) of the vitamin E isomers has been evaluated in HT-29 and HCT-116 cells. Indeed, the combined treatment, especially for ETO-Cur and TRF, showed synergistic potential in the 2 cell models. Similarly, in in vivo studies, HCT-116 cells xenograft in SCID mice were treated by ETO-Cur and TRF, which synergically acted to inhibit tumor volume. Moreover, even changes in microbial diversity were observed in xenograft mice treated with such EOs combination [173].
Various studies have reported that TQ could enhance anti-cancer potential when co-administered with several chemotherapeutic agents while reducing their toxic side effects [175]. Different compounds (menthol, trans-anethole) were investigated for the preparation of oil/water microemulsions for the delivery of methotrexate, and the ability of methotrexate-loaded microemulsions to inhibit cancer cell growth. Menthol and trans-anethole EOs led to cytotoxic microemulsions decreasing HeLa cells proliferation by MTT assay concluding that the oily component could play a role in the efficacy and safety of the microemulsions (for comparison α-tocopherol based-formulations showed opposite effects with increased cell proliferation) [176]. EO from the leaves of M. rubra also demonstrated an antiproliferative effect on Caco2 cells, with strong prooxidative effect. In addition, this EO was able to improve the antiproliferative and prooxidative activity of doxorubicin enhancing intracellular and nuclei accumulation, as previous described [147].
Limitations, clinical challenges and future perspectives
A limitative aspect of using the EOs in CRC management is represented by variable concentrations of bioactive compounds. Many factors, including ecological and geographical conditions influence to the quality and quantity of EOs. The chemical composition and biological activities of EOs depend on various factors such as habitat, climatic conditions, seasonality, cultivation and harvesting and conservation practices, the type of soil, the different extraction procedures [177–180] as well as a substantial variability based on the part of the plant used for the extraction of EO. Altitude is an important factor affecting yield, composition, and biology of plant extracts. Satureja thymbra L. EO showed increased cytotoxic activity at an altitude of 661 m if compared to the same EO collected at 156 m above sea level. This result was obtained using the sulforhodamine B assay on HCT-116 colon cancer cells with an IC50 of 2.45 ± 0.21 μg/mL. In this case, the EO composition was prevailed by carvacrol (14.30%) [181]. Another important therapeutic limitation derives from the fact that it is not known exactly and completely the pharmacokinetic profiles of the essential oils, and due to their hydrophobic nature EOs can lead to poor bioavailability and pharmacodynamics issues.
Clinical challenges derived from the search for a natural therapy that includes EOs has led to attempts to find methods for administering the extracts. To overcome these issues, researchers explored the possibility to load nano-carriers with EOs, individually or combined with conventional chemotherapeutic agents. For example, A Carum carvi L. oil nanoemulsion system was tested on HT-29 cells, whereas it demonstrated a cytotoxic effect and apoptosis induction by increased gene expression of caspase-3. Besides, the authors suggested that the use of dietary supplements with nanoemulsions could potentially decrease the risk of cancer and that more research was needed to confirm this hypothesis [182]. This approach of drug delivery however has been poorly studied in CRC and EOs thus leaving the possibility to go down this route, at least in preclinical models. In order to improve the anticancer therapeutic potential and reduce the toxicity of bioactives compounds, new nanopharmaceutical forms for target transport such as nanoparticles, liposomes, nanocapsules, niosomes should be developed and researched [21, 22, 163, 183]. Alternatively, EOs can be combined with other more bioavailable compounds in order to harness their impact on human organism. For example, EOs can be used together with other plant natural derived products to search for an additive or a synergistic effect. Nonetheless, this combination scheme should be carefully evaluated, as sometime novel compounds put inside in a complex organism can lead also to antagonistic effects, an activity that need to be avoided. Despite remarkable anticancer activity of EOs in CRC and cancer in general, clinical trials that face the challenge of using such preparations in humans are still lacking. It is hoped that this gap will be rapidly filled in and that new works will explore the superb effects of EOs in CRC.
Conclusion
Essential oils have been used in alternative medicine for a very long time, due to the healing properties that have been studied and demonstrated. Numerous experimental pharmacological studies have shown that they can inhibit the development of cancer and deserve to be used in prevention and even as adjuncts to classical chemotherapy. Therapeutic strategies to fight against CRC relay on surgery, radiotherapy, immunotherapy, and chemotherapeutic agents. EOs, defined as volatile chemical molecules from plants, can be potentially inserted in the last category of curative tools for the treatment of cancer. Though numerous advancements have been reported in surgery and chemotherapy in the last decades leading to progression of patient time survival and even in the increase of clinical conditions of affected patients, the death rate of CRC is still worrying healthcare system worldwide. This updated review showed scientific evidence on the potential anticancer effect of EOs in CRC. EOs can exhibit cytotoxic effects on living cells depending on type and concentration. In eukaryotic cells, EOs can act as prooxidants affecting inner cell membranes and organelles such as mitochondria. In some cases, changes in intracellular redox potential and mitochondrial dysfunction induced by EO can be associated with their capacity to exert antigenotoxic effects. EOs can interfere with several molecular targets in a pleiotropic fashion, but undeniably the cytotoxic activity of EOs is based on their individual components. In general, EOs (due to their lipophilic properties and low molecular weights) can cross cell membranes altering the phospholipid layers, increasing membrane fluidity, and leading to leakage of ions and/or other cytoplasmic content, thus inducing ATP reduction, alteration of pH gradient and loss of mitochondrial potential. In the light of these results, EOs can be a new therapeutic window and a potential adjuvant chemotherapy of CRC.
Supplementary Information
Additional file 1. CRC preclinical models.
Acknowledgements
This work was supported by the Ministry of Science and Higher Education of the Republic of Kazakhstan [Grant number AP08052551].
Author contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas. That is, revising or critically reviewing the article; giving final approval of the version to be published; agreeing on the journal to which the article has been submitted; and, confirming to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Funding
Not Applicable.
Availability of data and materials
Not Applicable.
Declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
Authors wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Raffaele Pezzani and Sara Vitalini authors should be regarded as co-last authors
Contributor Information
Stefania Garzoli, Email: stefania.garzoli@uniroma1.it.
Pedro Alarcón-Zapata, Email: pedroalarcon.z@gmail.com.
Gulnaz Seitimova, Email: sitigulnaz@mail.ru.
Barbara Alarcón-Zapata, Email: b.alarcon.zapata@gmail.com.
Miquel Martorell, Email: mmartorell@udec.cl.
Farukh Sharopov, Email: shfarukh@mail.ru.
Patrick Valere Tsouh Fokou, Email: ptsouh@gmail.com.
Darline Dize, Email: darline.dize@yahoo.fr.
Lauve Rachel Tchokouaha Yamthe, Email: yamthe_lauve@yahoo.fr.
Marcello Iriti, Email: marcello.iriti@unimi.it.
Javad Sharifi Rad, Email: javad.sharifirad@gmail.com.
Eda Sönmez Gürer, Email: edagurer@cumhuriyet.edu.tr.
Daniela Calina, Email: calinadaniela@gmail.com.
Raffaele Pezzani, Email: raffaele.pezzani@unipd.it.
Sara Vitalini, Email: sara.vitalini@unimi.it.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Collaborators GCRF. The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 2022;400(10352):563–591. doi: 10.1016/S0140-6736(22)01438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cancer TIAfRo: Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018. In: PRESS RELEASE N° 263. GLOBOCAN 2018: WHO; 2018. https://www.iarc.who.int/featured-news/latest-global-cancer-data-cancer-burden-rises-to-18-1-million-new-casesand-9-6-million-cancer-deaths-in-2018/. Accessed 11 Mar 2022.
- 4.Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14(10):101174. doi: 10.1016/j.tranon.2021.101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2016 Neurology Collaborators Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–480. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Venugopal A, Carethers JM. Epidemiology and biology of early onset colorectal cancer. Excli j. 2022;21:162–182. doi: 10.17179/excli2021-4456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA. 2021;325(7):669–685. doi: 10.1001/jama.2021.0106. [DOI] [PubMed] [Google Scholar]
- 8.Mitrut P, Docea AO, Kamal AM, Mitrut R, Calina D, Gofita E, Padureanu V, Gruia C, Streba L. Colorectal cancer and inflammatory bowel disease. In: Rodrigo L, editor. Colorectal cancer - from pathogenesis to treatment. London: IntechOpen; 2016. [Google Scholar]
- 9.NICE NIfHaCEG-: Colorectal cancer In: Colorectal cancer. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE 2021. 2021. https://www.nice.org.uk/guidance/ng151. Accessed 18 May 2022.
- 10.Zlatian OM, Comanescu MV, Rosu AF, Rosu L, Cruce M, Gaman AE, Calina CD, Sfredel V. Histochemical and immunohistochemical evidence of tumor heterogeneity in colorectal cancer. Rom J Morphol Embryol. 2015;56(1):175–181. [PubMed] [Google Scholar]
- 11.de Assis JV, Coutinho LA, Oyeyemi IT, Oyeyemi OT, Grenfell R. Diagnostic and therapeutic biomarkers in colorectal cancer: a review. Am J Cancer Res. 2022;12(2):661–680. [PMC free article] [PubMed] [Google Scholar]
- 12.Liu W, Zeng AR, Tang HZ, Qiang JW. Radiologic imaging modalities for colorectal cancer. Dig Dis Sci. 2021 doi: 10.1007/s10620-021-07166-0. [DOI] [PubMed] [Google Scholar]
- 13.Ros J, Baraibar I, Martini G, Salvà F, Saoudi N, Cuadra-Urteaga JL, Dienstmann R, Tabernero J, Élez E. The evolving role of consensus molecular subtypes: a step beyond inpatient selection for treatment of colorectal cancer. Curr Treat Options Oncol. 2021;22(12):113. doi: 10.1007/s11864-021-00913-5. [DOI] [PubMed] [Google Scholar]
- 14.Sakata S, Larson DW. Targeted therapy for colorectal cancer. Surg Oncol Clin N Am. 2022;31(2):255–264. doi: 10.1016/j.soc.2021.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Carlsen L, Huntington KE. Immunotherapy for colorectal cancer: mechanisms and predictive biomarkers. Cancers. 2022 doi: 10.3390/cancers14041028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kitic D, Miladinovic B, Randjelovic M, Szopa A, Sharifi-Rad J, Calina D, Seidel V. Anticancer potential and other pharmacological properties of Prunus armeniaca L.: an updated overview. Plants. 2022;11(14):1885. doi: 10.3390/plants11141885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konovalov DA, Cáceres EA, Shcherbakova EA, Herrera-Bravo J, Chandran D, Martorell M, Hasan M, Kumar M, Bakrim S, Bouyahya A, et al. Eryngium caeruleum: an update on ethnobotany, phytochemistry and biomedical applications. Chinese Med. 2022;17(1):114. doi: 10.1186/s13020-022-00672-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salehi B, Prakash Mishra A, Nigam M, Karazhan N, Shukla I, Kiełtyka-Dadasiewicz A, Sawicka B, Głowacka A, Abu-Darwish MS, Hussein Tarawneh A, et al. Ficus plants: State of the art from a phytochemical, pharmacological, and toxicological perspective. Phytother Res. 2021;35(3):1187–1217. doi: 10.1002/ptr.6884. [DOI] [PubMed] [Google Scholar]
- 19.Sharifi-Rad J, Quispe C, Turgumbayeva A, Mertdinç Z, Tütüncü S, Aydar EF, Özçelik B, Anna S-W, Mariola S, Koziróg A, et al. Santalum Genus: phytochemical constituents, biological activities and health promoting-effects. Zeitschrift für Naturforschung C. 2022 doi: 10.1515/znc-2022-0076. [DOI] [PubMed] [Google Scholar]
- 20.Sharifi-Rad J, Herrera-Bravo J, Kamiloglu S, Petroni K, Mishra AP, Monserrat-Mesquida M, Sureda A, Martorell M, Aidarbekovna DS, Yessimsiitova Z, et al. Recent advances in the therapeutic potential of emodin for human health. Biomed Pharmacother. 2022;154:113555. doi: 10.1016/j.biopha.2022.113555. [DOI] [PubMed] [Google Scholar]
- 21.Dhyani P, Quispe C, Sharma E, Bahukhandi A, Sati P, Attri DC, Szopa A, Sharifi-Rad J, Docea AO, Mardare I, et al. Anticancer potential of alkaloids: a key emphasis to colchicine, vinblastine, vincristine, vindesine, vinorelbine and vincamine. Cancer Cell Int. 2022;22(1):206. doi: 10.1186/s12935-022-02624-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharifi-Rad J, Quispe C, Patra JK, Singh YD, Panda MK, Das G, Adetunji CO, Michael OS, Sytar O, Polito L, et al. Paclitaxel: application in modern oncology and nanomedicine-based cancer therapy. Oxid Med Cell Longev. 2021;2021:3687700. doi: 10.1155/2021/3687700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Javed Z, Khan K, Herrera-Bravo J, Naeem S, Iqbal MJ, Raza Q, Sadia H, Raza S, Bhinder M, Calina D, et al. Myricetin: targeting signaling networks in cancer and its implication in chemotherapy. Cancer Cell Int. 2022;22(1):239. doi: 10.1186/s12935-022-02663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pezzuto JM. Plant-derived anticancer agents. Biochem Pharmacol. 1997;53(2):121–133. doi: 10.1016/S0006-2952(96)00654-5. [DOI] [PubMed] [Google Scholar]
- 25.Nobili S, Lippi D, Witort E, Donnini M, Bausi L, Mini E, Capaccioli S. Natural compounds for cancer treatment and prevention. Pharmacol Res. 2009;59(6):365–378. doi: 10.1016/j.phrs.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 26.Newman DJ, Cragg GM. Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. J Nat Prod. 2020;83(3):770–803. doi: 10.1021/acs.jnatprod.9b01285. [DOI] [PubMed] [Google Scholar]
- 27.Popović-Djordjević J, Quispe C, Giordo R, Kostić A, Katanić Stanković JS, Tsouh Fokou PV, Carbone K, Martorell M, Kumar M, Pintus G, et al. Natural products and synthetic analogues against HIV: a perspective to develop new potential anti-HIV drugs. Eur J Med Chem. 2022;233:114217. doi: 10.1016/j.ejmech.2022.114217. [DOI] [PubMed] [Google Scholar]
- 28.Sharifi-Rad J, Bahukhandi A, Dhyani P, Sati P, Capanoglu E, Docea AO, Al-Harrasi A, Dey A, Calina D. Therapeutic potential of Neoechinulins and their derivatives: an overview of the molecular mechanisms behind pharmacological activities. Front Nutr. 2021;8:664197. doi: 10.3389/fnut.2021.664197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sousa C, Duarte D, Silva-Lima B, Videira M. Repurposing natural dietary flavonoids in the modulation of cancer tumorigenesis: decrypting the molecular targets of Naringenin Hesperetin and Myricetin. Nutr cancer. 2022;74(4):1188–1202. doi: 10.1080/01635581.2021.1955285. [DOI] [PubMed] [Google Scholar]
- 30.Raut JS, Karuppayil SM. A status review on the medicinal properties of essential oils. Ind Crops Prod. 2014;62:250–264. doi: 10.1016/j.indcrop.2014.05.055. [DOI] [Google Scholar]
- 31.Sharifi-Rad J, Quispe C, Herrera-Bravo J, Martorell M, Sharopov F, Tumer TB, Kurt B, Lankatillake C, Docea AO, Moreira AC, et al. A pharmacological perspective on plant-derived bioactive molecules for epilepsy. Neurochem Res. 2021;46(9):2205–2225. doi: 10.1007/s11064-021-03376-0. [DOI] [PubMed] [Google Scholar]
- 32.Dhyani P, Sati P, Sharma E, Attri DC, Bahukhandi A, Tynybekov B, Szopa A, Sharifi-Rad J, Calina D, Suleria HAR, et al. Sesquiterpenoid lactones as potential anti-cancer agents: an update on molecular mechanisms and recent studies. Cancer Cell Int. 2022;22(1):305. doi: 10.1186/s12935-022-02721-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baba Y, Kato Y. Deguelin, a novel anti-tumorigenic agent in human Esophageal squamous cell carcinoma. EBioMedicine. 2017;26:10. doi: 10.1016/j.ebiom.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharma E, Attri DC, Sati P, Dhyani P, Szopa A, Sharifi-Rad J, Hano C, Calina D, Cho WC. Recent updates on anticancer mechanisms of polyphenols. Front Cell Dev Biol. 2022 doi: 10.3389/fcell.2022.1005910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharifi-Rad J, Quispe C, Kumar M, Akram M, Amin M, Iqbal M, Koirala N, Sytar O, Kregiel D, Nicola S, et al. Hyssopus essential oil: an update of its phytochemistry, biological activities, and safety profile. Oxid Med Cell Longev. 2022;2022:8442734. doi: 10.1155/2022/8442734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharifi-Rad J, Quispe C, Rahavian A, Pereira Carneiro JN, Rocha JE, Alves Borges Leal AL, Bezerra Morais Braga MF, Melo Coutinho HD, Ansari Djafari A, Alarcón-Zapata P, et al. Bioactive compounds as potential agents for sexually transmitted diseases management: a review to explore molecular mechanisms of action. Front Pharmacol. 2021 doi: 10.3389/fphar.2021.674682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adlard ER. K. Hüsnü Can Başer and Gerhard Buchbauer (Eds.): handbook of essential oils science, technology and applications 2nd Edn. Chromatographia. 2016;79(11):791–791. doi: 10.1007/s10337-016-3055-7. [DOI] [Google Scholar]
- 38.Warnke PH, Sherry E, Russo PAJ, Sprengel M, Açil Y, Bredee JP, Schubert S, Wiltfang J, Springer IN. Antibacterial essential oils reduce tumor smell and inflammation in cancer patients. J Clin Oncol. 2005;23(7):1588–1589. doi: 10.1200/JCO.2005.05.380. [DOI] [PubMed] [Google Scholar]
- 39.Rezaie-Tavirani M, Fayazfar S, Heydari-Keshel S, Rezaee MB, Zamanian-Azodi M, Rezaei-Tavirani M, Khodarahmi R. Effect of essential oil of Rosa Damascena on human colon cancer cell line SW742. Gastroenterol Hepatol Bed Bench. 2013;6(1):25–31. [PMC free article] [PubMed] [Google Scholar]
- 40.Beeby E, Magalhães M, Poças J, Collins T, Lemos MFL, Barros L, Ferreira I, Cabral C, Pires IM. Secondary metabolites (essential oils) from sand-dune plants induce cytotoxic effects in cancer cells. J Ethnopharmacol. 2020;258:112803. doi: 10.1016/j.jep.2020.112803. [DOI] [PubMed] [Google Scholar]
- 41.Gould MN. Cancer chemoprevention and therapy by monoterpenes. Environ Health Perspect. 1997;105(Suppl 4):977–979. doi: 10.1289/ehp.97105s4977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crowell PL, Gould MN. Chemoprevention and therapy of cancer by d-limonene. Crit Rev Oncog. 1994;5(1):1–22. doi: 10.1615/CritRevOncog.v5.i1.10. [DOI] [PubMed] [Google Scholar]
- 43.Sharifi-Rad J, Dey A, Koirala N, Shaheen S, El Omari N, Salehi B, Goloshvili T, Cirone Silva NC, Bouyahya A, Vitalini S, et al. Cinnamomum species: bridging phytochemistry knowledge, pharmacological properties and toxicological safety for health benefits. Front Pharmacol. 2021;12:600139–600139. doi: 10.3389/fphar.2021.600139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scheau C, Caruntu C, Badarau IA, Scheau AE, Docea AO, Calina D, Caruntu A. Cannabinoids and Inflammations of the gut-lung-skin barrier. J Pers Med. 2021 doi: 10.3390/jpm11060494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Blowman K, Magalhães M, Lemos MFL, Cabral C, Pires IM. Anticancer properties of essential oils and other natural products. Evid Based Complement Alternat Med. 2018;2018:3149362. doi: 10.1155/2018/3149362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hossain R, Quispe C, Saikat ASM, Jain D, Habib A, Janmeda P, Islam MT, Daştan SD, Radha, Kumar M, et al. Biosynthesis of secondary metabolites based on the Regulation of MicroRNAs. Biomed Res Int. 2022;2022:9349897. doi: 10.1155/2022/9349897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tong Y, Yang W, Koeffler HP. Mouse models of colorectal cancer. Chin J Cancer. 2011;30(7):450–462. doi: 10.5732/cjc.011.10041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.De CássiaSilveira e Sá R DA, De Andrade LN, Sousa DP. Sesquiterpenes from essential oils and anti-inflammatory activity. Nat Product Commun. 2015;10(10):1934578. [PubMed] [Google Scholar]
- 49.Sharifi-Rad J, Quispe C, Herrera-Bravo J, Akram M, Abbaass W, Semwal P, Painuli S, Konovalov DA, Alfred MA, Kumar NVA, et al. Phytochemical constituents, biological activities, and health-promoting effects of the Melissa officinalis. Oxid Med Cell Longev. 2021;2021:6584693. doi: 10.1155/2021/6584693. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 50.Muhammad Asif AHS, Al-Mansoub MA, Revadigar V, Ezzat MO, Khadeer MB, Ahamed CE, Oon VM, Majid ASA, Majid AMSA. Anticancer attributes of Illicium verum essential oils against colon cancer. South African J Botany. 2016;103:156–161. doi: 10.1016/j.sajb.2015.08.017. [DOI] [Google Scholar]
- 51.Gören AC, Topçu G, Bilsel G, Bilsel M, Aydoğmusç Z, Pezzuto JM. The chemical constituents and biological activity of essential oil of Lavandula stoechas ssp. stoechas. Zeitschrift für Naturforschung C. 2002;57(9–10):797–800. doi: 10.1515/znc-2002-9-1007. [DOI] [PubMed] [Google Scholar]
- 52.Tu PT, Tawata S. Anti-oxidant, anti-aging, and anti-melanogenic properties of the essential oils from two varieties of Alpinia zerumbet. Molecules. 2015;20(9):16723–16740. doi: 10.3390/molecules200916723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sharma PR, Mondhe DM, Muthiah S, Pal HC, Shahi AK, Saxena AK, Qazi GN. Anticancer activity of an essential oil from Cymbopogon flexuosus. Chem Biol Interact. 2009;179(2–3):160–168. doi: 10.1016/j.cbi.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 54.Asif M, Yehya AHS, Al-Mansoub MA, Revadigar V, Ezzat MO, Ahamed MBK, Oon CE, Murugaiyah V, Majid ASA, Majid AMA. Anticancer attributes of Illicium verum essential oils against colon cancer. S Afr J Bot. 2016;103:156–161. doi: 10.1016/j.sajb.2015.08.017. [DOI] [Google Scholar]
- 55.Khalil N, Fikry S, Salama O. Bactericidal activity of Myrrh extracts and two dosage forms against standard bacterial strains and multidrug-resistant clinical isolates with GC/MS profiling. AMB Express. 2020;10(1):21. doi: 10.1186/s13568-020-0958-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kulisic-Bilusic T, Schmöller I, Schnäbele K, Siracusa L, Ruberto G. The anticarcinogenic potential of essential oil and aqueous infusion from caper (Capparis spinosa L.) Food Chem. 2012;132(1):261–267. doi: 10.1016/j.foodchem.2011.10.074. [DOI] [PubMed] [Google Scholar]
- 57.Donadu MG, Usai D, Mazzarello V, Molicotti P, Cannas S, Bellardi MG, Zanetti S. Change in Caco-2 cells following treatment with various lavender essential oils. Nat Prod Res. 2017;31(18):2203–2206. doi: 10.1080/14786419.2017.1280489. [DOI] [PubMed] [Google Scholar]
- 58.Taha AM, Eldahshan OA. Chemical characteristics, antimicrobial, and cytotoxic activities of the essential oil of Egyptian Cinnamomum glanduliferum bark. Chem Biodivers. 2017 doi: 10.1002/cbdv.201600443. [DOI] [PubMed] [Google Scholar]
- 59.Mansi IA, Awadh Ali NA, Mhaidat NM, Hussain K, Al-Kaf AG, Anwar S, Setzer WN. Chemical composition and biological activity of the essential oil isolated from the leaves of Achillea fragrantissima growing wild in Yemen. Pharmacognosy J. 2019 doi: 10.5530/pj.2019.11.168. [DOI] [Google Scholar]
- 60.Deng W, Liu K, Cao S, Sun J, Zhong B, Chun J. Chemical composition, antimicrobial, antioxidant, and antiproliferative properties of grapefruit essential oil prepared by molecular distillation. Molecules. 2020 doi: 10.3390/molecules25010217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shameem SA, Khan KZ, Waza AA, Banday AH, Ramzan A, Shah AH, Ganai BA. Chemical profile and biological activities of essential oil from flowers of Artemisia dubia wall. ex Bess. Growing Wild in Western Himalaya India. Asian J Chem. 2019;31(8):1762–1766. doi: 10.14233/ajchem.2019.21970. [DOI] [Google Scholar]
- 62.Bhagat M, Sangral M, Kumar A, Rather RA, Arya K. Chemical, biological and in silico assessment of Ocimum viride essential oil. Heliyon. 2020;6(6):e04209. doi: 10.1016/j.heliyon.2020.e04209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Silva FL, Silva RVS, Branco PC, Costa-Lotufo LV, Murakami C, Young MCM, Azevedo DA, Moreno PRH. Chemical composition of the Brazilian native Cinnamomum stenophyllum (Meisn.) Vattimo-Gil essential oil by GC-qMS and GC× GC-TOFMS, and its cytotoxic activity. Arab J Chem. 2020;13(4):4926–4935. doi: 10.1016/j.arabjc.2020.01.012. [DOI] [Google Scholar]
- 64.Patil JR, Jayaprakasha GK, Murthy KNC, Tichy SE, Chetti MB, Patil BS. Apoptosis-mediated proliferation inhibition of human colon cancer cells by volatile principles of Citrus aurantifolia. Food Chem. 2009;114(4):1351–1358. doi: 10.1016/j.foodchem.2008.11.033. [DOI] [Google Scholar]
- 65.Jayaprakasha GK, Murthy KNC, Uckoo RM, Patil BS. Chemical composition of volatile oil from Citrus limettioides and their inhibition of colon cancer cell proliferation. Ind Crops Prod. 2013;45:200–207. doi: 10.1016/j.indcrop.2012.12.020. [DOI] [Google Scholar]
- 66.Firuzi O, Asadollahi M, Gholami M, Javidnia K. Composition and biological activities of essential oils from four Heracleum species. Food Chem. 2010;122(1):117–122. doi: 10.1016/j.foodchem.2010.02.026. [DOI] [Google Scholar]
- 67.Zhou W, He Y, Lei X, Liao L, Fu T, Yuan Y, Huang X, Zou L, Liu Y, Ruan R, et al. Chemical composition and evaluation of antioxidant activities, antimicrobial, and anti-melanogenesis effect of the essential oils extracted from Dalbergia pinnata (Lour.) Prain. J Ethnopharmacol. 2020;254:112731. doi: 10.1016/j.jep.2020.112731. [DOI] [PubMed] [Google Scholar]
- 68.Larbi BAM, Naima B, Elsharkawy ER, Salah N. Phytochemical characterization, in-vitro cytotoxic and antibacterial activity of Cotula cinerea (Delile) Vis essential oil. J Nat Remedies. 2018;18(3):107–112. doi: 10.18311/jnr/2018/22380. [DOI] [Google Scholar]
- 69.Damasceno LMO, Silva ALN, Santos RFD, Feitosa TA, Viana LGFC, Oliveira-Júnior RG, Silva MG, Rolim LA, Araújo CdS, Araújo ECdC et al. Cytotoxic activity of chemical constituents and essential oil from the leaves of Leonotis nepetifolia (Lamiaceae). In: 2019.
- 70.Cianfaglione K, Blomme EE, Quassinti L, Bramucci M, Lupidi G, Dall'Acqua S, Maggi F. Cytotoxic essential oils from Eryngium campestre and Eryngium amethystinum (Apiaceae) growing in Central Italy. Chem Biodivers. 2017 doi: 10.1002/cbdv.201700096. [DOI] [PubMed] [Google Scholar]
- 71.Oliveira PFD, Alves JM, Damasceno JL, Oliveira RAM, Dias Júnior H, Crotti AEM, Tavares DC. Cytotoxicity screening of essential oils in cancer cell lines. Revista Brasileira de Farmacognosia. 2015;25:183–188. doi: 10.1016/j.bjp.2015.02.009. [DOI] [Google Scholar]
- 72.Rattanamaneerusmee A, Thirapanmethee K, Nakamura Y, Chomnawang MT. Differentiation-inducing effect in human colon cancer cells of essential oils. Pharm Sci Asia. 2018;45(3):154–160. doi: 10.29090/psa.2018.03.154. [DOI] [Google Scholar]
- 73.Awwad O, Abu-Dahab R, Abaza IF, Alabbassi R, Majdalawi L, Afifi FU. Effect of the galling aphid of Baizongia pistaciae L. on composition and biological activities of essential oils of Pistacia atlantica Desf growing wild in Jordan. J Essential Oil Bearing Plants. 2017;20(3):791–800. doi: 10.1080/0972060X.2017.1341343. [DOI] [Google Scholar]
- 74.Ding W, Liping N, Xing H, Wei Z, Zhoua Q, Nong R, Chen J. Essential oil extracted from leaf of Phoebe bournei (Hemsl.) yang: chemical constituents, antitumor, antibacterial, hypoglycemic activities. Nat Prod Res. 2020;34(17):2524–2527. doi: 10.1080/14786419.2018.1542393. [DOI] [PubMed] [Google Scholar]
- 75.Naima B, Abdelkrim R, Ouarda B, Salah NN, Larbi BAM. Chemical composition, antimicrobial, antioxidant and anticancer activities of essential oil from Ammodaucus leucotrichus cosson & durieu (Apiaceae) growing in South Algeria. Bull Chem Soc Ethiop. 2019;33(3):541–549. doi: 10.4314/bcse.v33i3.14. [DOI] [Google Scholar]
- 76.Karan T, Yildiz I, Aydin A, Erenler R. Inhibition of various cancer cells proliferation of bornyl acetate and essential oil from Inula graveolens (Linnaeus) Desf. Rec Nat Prod. 2018 doi: 10.25135/rnp.30.17.09.057. [DOI] [Google Scholar]
- 77.Sharma M, Agrawal SK, Sharma PR, Chadha BS, Khosla MK, Saxena AK. Cytotoxic and apoptotic activity of essential oil from Ocimum viride towards COLO 205 cells. Food Chem Toxicol. 2010;48(1):336–344. doi: 10.1016/j.fct.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 78.Rashid S, Rather MA, Shah WA, Bhat BA. Chemical composition, antimicrobial, cytotoxic and antioxidant activities of the essential oil of Artemisia indica Willd. Food Chem. 2013;138(1):693–700. doi: 10.1016/j.foodchem.2012.10.102. [DOI] [PubMed] [Google Scholar]
- 79.Jeong JB, Choi J, Lou Z, Jiang X, Lee SH. Patchouli alcohol, an essential oil of Pogostemon cablin, exhibits anti-tumorigenic activity in human colorectal cancer cells. Int Immunopharmacol. 2013;16(2):184–190. doi: 10.1016/j.intimp.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 80.Figueiredo PLB, Pinto LC, da Costa JS, da Silva ARC, Mourão RHV, Montenegro RC, da Silva JKR, Maia JGS. Composition, antioxidant capacity and cytotoxic activity of Eugenia uniflora L. chemotype-oils from the Amazon. J Ethnopharmacol. 2019;232:30–38. doi: 10.1016/j.jep.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 81.Spyridopoulou K, Fitsiou E, Bouloukosta E, Tiptiri-Kourpeti A, Vamvakias M, Oreopoulou A, Papavassilopoulou E, Pappa A, Chlichlia K. Extraction, chemical composition, and anticancer potential of Origanum onites L. essential oil. Molecules. 2019 doi: 10.3390/molecules24142612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jaradat N, Al-Maharik N. Fingerprinting, antimicrobial, antioxidant, anticancer, cyclooxygenase and metabolic enzymes inhibitory characteristic evaluations of Stachys viticina Boiss. essential oil. Molecules. 2019 doi: 10.3390/molecules24213880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Elsayed EA, Sharaf-Eldin MA, Wadaan M. In vitro evaluation of cytotoxic activities of essential oil from Moringa oleifera seeds on HeLa, HepG2, MCF-7, CACO-2 and L929 cell lines. Asian Pacific J Cancer Prevention: APJCP. 2015;16(11):4671–4675. doi: 10.7314/APJCP.2015.16.11.4671. [DOI] [PubMed] [Google Scholar]
- 84.Straface M, Makwana R, Palmer A, Rombolà L, Aleong JC, Morrone LA, Sanger GJ. Inhibition of neuromuscular contractions of human and rat colon by bergamot essential oil and linalool: evidence to support a therapeutic action. Nutrients. 2020 doi: 10.3390/nu12051381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Weidner C, Rousseau M, Plauth A, Wowro SJ, Fischer C, Abdel-Aziz H, Sauer S. Melissa officinalis extract induces apoptosis and inhibits proliferation in colon cancer cells through formation of reactive oxygen species. Phytomedicine. 2015;22(2):262–270. doi: 10.1016/j.phymed.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 86.Asif M, Yehya AHS, Dahham SS, Mohamed SK, Shafaei A, Ezzat MO, Abdul Majid AS, Oon CE, Abdul Majid AMS. Establishment of in vitro and in vivo anti-colon cancer efficacy of essential oils containing oleo-gum resin extract of Mesua ferrea. Biomed pharmacother. 2019;109:1620–1629. doi: 10.1016/j.biopha.2018.10.127. [DOI] [PubMed] [Google Scholar]
- 87.Athamneh K, Alneyadi A, Alsamri H, Alrashedi A, Palakott A, El-Tarabily KA, Eid AH, Al Dhaheri Y, Iratni R. Origanum majorana essential oil triggers p38 MAPK-mediated protective autophagy, apoptosis, and caspase-dependent cleavage of P70S6K in colorectal cancer cells. Biomolecules. 2020 doi: 10.3390/biom10030412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dall'Acqua S, Peron G, Ferrari S, Gandin V, Bramucci M, Quassinti L, Mártonfi P, Maggi F. Phytochemical investigations and antiproliferative secondary metabolites from Thymus alternans growing in Slovakia. Pharm Biol. 2017;55(1):1162–1170. doi: 10.1080/13880209.2017.1291689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ouakouak H, Benchikha N, Hassani A, Ashour ML. Chemical composition and biological activity of Mentha citrata Ehrh, essential oils growing in southern Algeria. J Food Sci Technol. 2019;56(12):5346–5353. doi: 10.1007/s13197-019-04005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Guesmi F, Tyagi AK, Prasad S, Landoulsi A. Terpenes from essential oils and hydrolate of Teucrium alopecurus triggered apoptotic events dependent on caspases activation and PARP cleavage in human colon cancer cells through decreased protein expressions. Oncotarget. 2018;9(64):32305–32320. doi: 10.18632/oncotarget.25955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fitsiou E, Mitropoulou G, Spyridopoulou K, Tiptiri-Kourpeti A, Vamvakias M, Bardouki H, Panayiotidis M, Galanis A, Kourkoutas Y, Chlichlia K, et al. Phytochemical profile and evaluation of the biological activities of essential oils derived from the Greek aromatic plant species Ocimum basilicum, Mentha spicata, Pimpinella anisum and Fortunella margarita. Molecules. 2016 doi: 10.3390/molecules21081069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sajid A, Manzoor Q, Iqbal M, Tyagi AK, Sarfraz RA, Sajid A. Pinus Roxburghii essential oil anticancer activity and chemical composition evaluation. EXCLI J. 2018;17:233. doi: 10.17179/excli2016-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ferrante C, Zengin G, Menghini L, Diuzheva A, Jekő J, Cziáky Z, Recinella L, Chiavaroli A, Leone S, Brunetti L. Qualitative fingerprint analysis and multidirectional assessment of different crude extracts and essential oil from Wild Artemisia santonicum L. Processes. 2019;7(8):522. doi: 10.3390/pr7080522. [DOI] [Google Scholar]
- 94.Quassinti L, Maggi F, Barboni L, Ricciutelli M, Cortese M, Papa F, Garulli C, Kalogris C, Vittori S, Bramucci M. Wild celery (Smyrnium olusatrum L.) oil and isofuranodiene induce apoptosis in human colon carcinoma cells. Fitoterapia. 2014;97:133–141. doi: 10.1016/j.fitote.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 95.Ahani N, Sangtarash MH, Alipour Eskandani M, Houshmand M. Zataria multiflora Boiss. essential oil induce apoptosis in two human colon cancer cell lines (HCT116 & SW48) Iran J Public health. 2020;49(4):753–762. [PMC free article] [PubMed] [Google Scholar]
- 96.Su M-Q, Zhou Y-R, Li C-Q, Wang Z, Wang Y-L, Shen B-Y, Dou J. Zedoary turmeric oil induces senescence and apoptosis in human colon cancer HCT116 cells. Nat Prod Commun. 2018;13(7):1934578X1801300731. [Google Scholar]
- 97.Akrout A, Gonzalez LA, El Jani H, Madrid PC. Antioxidant and antitumor activities of Artemisia campestris and Thymelaea hirsuta from southern Tunisia. Food chem Toxicol. 2011;49(2):342–347. doi: 10.1016/j.fct.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 98.Rossi D, Guerrini A, Paganetto G, Bernacchia G, Conforti F, Statti G, Maietti S, Poppi I, Tacchini M, Sacchetti G. Croton lechleri Müll Arg (Euphorbiaceae) stem bark essential oil as possible mutagen-protective food ingredient against heterocyclic amines from cooked food. Food chem. 2013;139(1–4):439–447. doi: 10.1016/j.foodchem.2013.01.076. [DOI] [PubMed] [Google Scholar]
- 99.Touihri I, Boukhris M, Marrakchi N, Luis J, Hanchi B, Kallech-Ziri O. Chemical composition and biological activities of Allium roseum L. var. grandiflorum Briq. essential oil. J oleo Sci. 2015;64(8):869–879. doi: 10.5650/jos.ess15055. [DOI] [PubMed] [Google Scholar]
- 100.Bardaweel SK, Hudaib MM, Tawaha KA, Bashatwah RM. Studies on the in vitro antiproliferative, antimicrobial, antioxidant, and acetylcholinesterase inhibition activities associated with chrysanthemum coronarium essential oil. Evid-Based Complementary Alternat Med: eCAM. 2015;2015:790838. doi: 10.1155/2015/790838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Su Y-C, Ho C-L. Composition and in-vitro cytotoxicactivities of the leaf essential oil of Beilschmiedia erythrophloia from Taiwan. Nat Prod Commun. 2013;8(1):1934578X1300800135. [PubMed] [Google Scholar]
- 102.Su YC, Ho CL. Composition, in-vitro anticancer, and antimicrobial activities of the leaf essential oil of Machilus mushaensis from Taiwan. Nat Prod Commun. 2013;8(2):273–275. [PubMed] [Google Scholar]
- 103.da Silva EB, Matsuo AL, Figueiredo CR, Chaves MH, Sartorelli P, Lago JH. Chemical constituents and cytotoxic evaluation of essential oils from leaves of Porcelia macrocarpa (Annonaceae) Nat Prod Commun. 2013;8(2):277–279. [PubMed] [Google Scholar]
- 104.Su YC, Hsu KP, Wang EI, Ho CL. Composition and in vitro anticancer activities of the leaf essential oil of Neolitsea variabillima from Taiwan. Nat Prod Commun. 2013;8(4):531–532. [PubMed] [Google Scholar]
- 105.Su YC, Hsu KP, Wang EI, Ho CL. Composition, in vitro cytotoxic, and antimicrobial activities of the flower essential oil of Diospyros discolor from Taiwan. Nat Prod Commun. 2015;10(7):1311–1314. [PubMed] [Google Scholar]
- 106.Su YC, Hsu KP, Li SC, Ho CL. Composition, in vitro cytotoxicity, and anti-mildew activities of the leaf essential oil of Machilus thunbergii from Taiwan. Nat Prod Commun. 2015;10(11):2013–2016. [PubMed] [Google Scholar]
- 107.Itani WS, El-Banna SH, Hassan SB, Larsson RL, Bazarbachi A, Gali-Muhtasib HU. Anti colon cancer components from lebanese sage (Salvia libanotica) essential oil: mechanistic basis. Cancer Biol Ther. 2008;7(11):1765–1773. doi: 10.4161/cbt.7.11.6740. [DOI] [PubMed] [Google Scholar]
- 108.Begnini KR, Nedel F, Lund RG, Carvalho PH, Rodrigues MR, Beira FT, Del-Pino FA. Composition and antiproliferative effect of essential oil of Origanum vulgare against tumor cell lines. J Med Food. 2014;17(10):1129–1133. doi: 10.1089/jmf.2013.0063. [DOI] [PubMed] [Google Scholar]
- 109.Rasoanaivo P, Fortuné Randriana R, Maggi F, Nicoletti M, Quassinti L, Bramucci M, Lupidi G, Petrelli D, Vitali LA, Papa F, et al. Chemical composition and biological activities of the essential oil of Athanasia brownii Hochr. (Asteraceae) endemic to Madagascar. Chem Biodivers. 2013;10(10):1876–1886. doi: 10.1002/cbdv.201300147. [DOI] [PubMed] [Google Scholar]
- 110.Fogang HP, Maggi F, Tapondjou LA, Womeni HM, Papa F, Quassinti L, Bramucci M, Vitali LA, Petrelli D, Lupidi G, et al. In vitro biological activities of seed essential oils from the Cameroonian spices Afrostyrax lepidophyllus MILDBR. and Scorodophloeus zenkeri HARMS rich in sulfur-containing compounds. Chem Biodivers. 2014;11(1):161–169. doi: 10.1002/cbdv.201300237. [DOI] [PubMed] [Google Scholar]
- 111.Luca T, Napoli E, Privitera G, Musso N, Ruberto G, Castorina S. Antiproliferative effect and cell cycle alterations induced by Salvia officinalis essential oil and its three main components in human colon cancer cell lines. Chem Biodivers. 2020;17(8):e2000309. doi: 10.1002/cbdv.202000309. [DOI] [PubMed] [Google Scholar]
- 112.Mishra T, Pal M, Meena S, Datta D, Dixit P, Kumar A, Meena B, Rana TS, Upreti DK. Composition and in vitro cytotoxic activities of essential oil of Hedychium spicatum from different geographical regions of western Himalaya by principal components analysis. Nat Prod Res. 2016;30(10):1224–1227. doi: 10.1080/14786419.2015.1049176. [DOI] [PubMed] [Google Scholar]
- 113.Altonsy MO, Andrews SC. Diallyl disulphide, a beneficial component of garlic oil, causes a redistribution of cell-cycle growth phases, induces apoptosis, and enhances butyrate-induced apoptosis in colorectal adenocarcinoma cells (HT-29) Nutr Cancer. 2011;63(7):1104–1113. doi: 10.1080/01635581.2011.601846. [DOI] [PubMed] [Google Scholar]
- 114.Piras A, Rosa A, Marongiu B, Atzeri A, Dessì MA, Falconieri D, Porcedda S. Extraction and separation of volatile and fixed oils from seeds of Myristica fragrans by supercritical CO2: chemical composition and cytotoxic activity on Caco-2 cancer cells. J Food Sci. 2012;77(4):C448–453. doi: 10.1111/j.1750-3841.2012.02618.x. [DOI] [PubMed] [Google Scholar]
- 115.Kumar D, Sukapaka M, Babu GD, Padwad Y. Chemical composition and in vitro cytotoxicity of essential oils from leaves and flowers of Callistemon citrinus from Western Himalayas. PLoS ONE. 2015;10(8):e0133823. doi: 10.1371/journal.pone.0133823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.da Silva JKR, Andrade EHA, Barreto LH, da Silva NCF, Ribeiro AF, Montenegro RC, Maia JGS. Chemical composition of four essential oils of Eugenia from the Brazilian Amazon and their cytotoxic and antioxidant activity. Medicines. 2017 doi: 10.3390/medicines4030051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dahham SS, Tabana YM, Iqbal MA, Ahamed MB, Ezzat MO, Majid AS, Majid AM. The anticancer, antioxidant and antimicrobial properties of the sesquiterpene β-caryophyllene from the essential oil of Aquilaria crassna. Molecules (Basel, Switzerland) 2015;20(7):11808–11829. doi: 10.3390/molecules200711808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Grecco SS, Martins EGA, Figueiredo CR, Girola N, Matsuo AL, Sartorelli P, Lago JHG. Cytotoxic potential of new phenylpropanoid derivatives isolated from Nectandra leucantha Nees & Mart (Lauraceae) Planta Medica. 2014;80(16):P1L67. doi: 10.1055/s-0034-1394724. [DOI] [Google Scholar]
- 119.Soltanian S, Mohamadi N, Rajaei P, Khodami M, Mohammadi M. Phytochemical composition, and cytotoxic, antioxidant, and antibacterial activity of the essential oil and methanol extract of Semenovia suffruticosa. Avicenna J Phytomed. 2019;9(2):143. [PMC free article] [PubMed] [Google Scholar]
- 120.da Silva JK, Pinto LC, Burbano RM, Montenegro RC, Andrade EH, Maia JG. Composition and cytotoxic and antioxidant activities of the oil of Piper aequale Vahl. Lipids Health Dis. 2016;15(1):174. doi: 10.1186/s12944-016-0347-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Spyridopoulou K, Tiptiri-Kourpeti A, Lampri E, Fitsiou E, Vasileiadis S, Vamvakias M, Bardouki H, Goussia A, Malamou-Mitsi V, Panayiotidis MI, et al. Dietary mastic oil extracted from Pistacia lentiscus var chia suppresses tumor growth in experimental colon cancer models. Sci Rep. 2017;7(1):3782. doi: 10.1038/s41598-017-03971-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Timoumi R, Salem IB, Amara I, Annabi E, Abid-Essefi S. Protective effects of fennel essential oil against oxidative stress and genotoxicity induced by the insecticide triflumuron in human colon carcinoma cells. Environ Sci Pollut Res Int. 2020;27(8):7957–7966. doi: 10.1007/s11356-019-07395-x. [DOI] [PubMed] [Google Scholar]
- 123.Hong S-L, Lee G-S, Syed Abdul Rahman SN, Ahmed Hamdi OA, Awang K, Aznam Nugroho N, Abd Malek SN. Essential oil content of the rhizome of Curcuma purpurascens Bl (Temu Tis) and its antiproliferative effect on selected human carcinoma cell lines. ScientificWorldJournal. 2014;2014:397430–397430. doi: 10.1155/2014/397430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chidambara Murthy KN, Jayaprakasha GK, Patil BS. D-limonene rich volatile oil from blood oranges inhibits angiogenesis, metastasis and cell death in human colon cancer cells. Life Sci. 2012;91(11–12):429–439. doi: 10.1016/j.lfs.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 125.Bayala B, Bassole IH, Scifo R, Gnoula C, Morel L, Lobaccaro J-MA, Simpore J. Anticancer activity of essential oils and their chemical components - a review. Am J Cancer Res. 2014;4(6):591–607. [PMC free article] [PubMed] [Google Scholar]
- 126.El-Najjar N, Chatila M, Moukadem H, Vuorela H, Ocker M, Gandesiri M, Schneider-Stock R, Gali-Muhtasib H. Reactive oxygen species mediate thymoquinone-induced apoptosis and activate ERK and JNK signaling. Apoptosis. 2010;15(2):183–195. doi: 10.1007/s10495-009-0421-z. [DOI] [PubMed] [Google Scholar]
- 127.Jehan S, Huang J, Farooq U, Basheer I, Zhou W. Combinatorial effect of thymoquinone with chemo agents for tumor therapy. Phytomedicine. 2022;98:153936. doi: 10.1016/j.phymed.2022.153936. [DOI] [PubMed] [Google Scholar]
- 128.Malik S, Singh A, Negi P, Kapoor VK. Thymoquinone: a small molecule from nature with high therapeutic potential. Drug Discovery Today. 2021;26(11):2716–2725. doi: 10.1016/j.drudis.2021.07.013. [DOI] [PubMed] [Google Scholar]
- 129.Pakdemirli A, Karaca C, Sever T, Daşkin E, Leblebici A, Yiğitbaşi T, Başbinar Y. Carvacrol alters soluble factors in HCT-116 and HT-29 cell lines. Turk J Med Sci. 2020;50(1):271–276. doi: 10.3906/sag-1907-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Murata S, Shiragami R, Kosugi C, Tezuka T, Yamazaki M, Hirano A, Yoshimura Y, Suzuki M, Shuto K, Ohkohchi N, et al. Antitumor effect of 1, 8-cineole against colon cancer. Oncol Rep. 2013;30(6):2647–2652. doi: 10.3892/or.2013.2763. [DOI] [PubMed] [Google Scholar]
- 131.De Souza Schmidt Gonçalves AE, Lajolo FM, Genovese MI. Chemical composition and antioxidant/antidiabetic potential of Brazilian native fruits and commercial frozen pulps. J Agric Food Chem. 2010;58(8):4666–4674. doi: 10.1021/jf903875u. [DOI] [PubMed] [Google Scholar]
- 132.Hassan EM, El-Gengaihi SE, Aboul-Enein AM, Mohammed MA. Antiproliferative effect and chemical constituents of Annona species. Plant Archives. 2020;20:2650–2657. [Google Scholar]
- 133.Karan T, yıldız I, Aydin A, Erenler R. Inhibition of various cancer cells proliferation of Bornyl Acetate and essential oil from Inula graveolens (Linnaeus) Desf. Rec Nat Prod. 2018 doi: 10.25135/rnp.30.17.09.057. [DOI] [Google Scholar]
- 134.Ben AM, Larbi BN, Elsharkawy ER, Salah Neghmouche N. Phytochemical characterization in-vitro cytotoxic and antibacterial activity of Cotula cinerea (Delile) Vis essential oil. J Nat Rem. 2019 doi: 10.18311/jnr/2018/22380. [DOI] [Google Scholar]
- 135.Quetglas-Llabrés MM, Quispe C, Herrera-Bravo J, Catarino MD, Pereira OR, Cardoso SM, Dua K, Chellappan DK, Pabreja K, Satija S, et al. Pharmacological properties of Bergapten: mechanistic and therapeutic aspects. Oxid Med Cell Longev. 2022;2022:8615242. doi: 10.1155/2022/8615242. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 136.Islam MT, Nasiruddin M, Khan IN, Mishra SK, Kudrat-E-Zahan M, Riaz TA, Ali ES, Rahman MS, Mubarak MS, Martorell M, et al. A Perspective on emerging therapeutic interventions for COVID-19. Front Public Health. 2020 doi: 10.3389/fpubh.2020.00281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Calina D, Rosu L, Rosu AF, Ianosi G, Ianosi S, Zlatian O, Mitrut R, Docea AO, Rogoveanu O, Mitrut P, et al. Etiological diagnosis and pharmacotherapeutic management of parapneumonic pleurisy. Farmacia. 2016;64(6):946–952. [Google Scholar]
- 138.Sharifi-Rad J, Rapposelli S, Sestito S, Herrera-Bravo J, Arancibia-Diaz A, Salazar LA, Yeskaliyeva B, Beyatli A, Leyva-Gómez G, González-Contreras C, et al. Multi-target mechanisms of phytochemicals in Alzheimer's disease: effects on oxidative stress neuroinflammation and protein aggregation. J Pers Med. 2022 doi: 10.3390/jpm12091515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Semwal P, Painuli S, Abu-Izneid T, Rauf A, Sharma A, Daştan SD, Kumar M, Alshehri MM, Taheri Y, Das R, et al. Diosgenin: an updated pharmacological review and therapeutic perspectives. Oxid Med Cell Longev. 2022;2022:1035441. doi: 10.1155/2022/1035441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Alshehri MM, Quispe C, Herrera-Bravo J, Sharifi-Rad J, Tutuncu S, Aydar EF, Topkaya C, Mertdinc Z, Ozcelik B, Aital M, et al. A review of recent studies on the antioxidant and anti-infectious properties of Senna plants. Oxid Med Cell Longev. 2022;2022:6025900. doi: 10.1155/2022/6025900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Amin R, Thalluri C, Docea AO, Sharifi-Rad J, Calina D. Therapeutic potential of cranberry for kidney health and diseases. Food. 2022;3(5):e33. [Google Scholar]
- 142.Wondrak GT, Villeneuve NF, Lamore SD, Bause AS, Jiang T, Zhang DD. The cinnamon-derived dietary factor cinnamic aldehyde activates the Nrf2-dependent antioxidant response in human epithelial colon cells. Molecules (Basel, Switzerland) 2010;15(5):3338–3355. doi: 10.3390/molecules15053338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sharifi-Rad J, Quispe C, Durazzo A, Lucarini M, Souto EB, Santini A, Imran M, Moussa AY, Mostafa NM, El-Shazly M, et al. Resveratrol’ biotechnological applications: enlightening its antimicrobial and antioxidant properties. J Herb Med. 2022;32:100550. doi: 10.1016/j.hermed.2022.100550. [DOI] [Google Scholar]
- 144.Mititelu RR, Padureanu R, Bacanoiu M, Padureanu V, Docea AO, Calina D, Barbulescu AL, Buga AM. Inflammatory and oxidative stress markers-mirror tools in rheumatoid arthritis. Biomedicines. 2020 doi: 10.3390/biomedicines8050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Thapa D, Richardson AJ, Zweifel B, Wallace RJ, Gratz SW. Genoprotective effects of essential oil compounds against oxidative and methylated DNA damage in human colon cancer cells. J Food Sci. 2019;84(7):1979–1985. doi: 10.1111/1750-3841.14665. [DOI] [PubMed] [Google Scholar]
- 146.Undeğer U, Başaran A, Degen GH, Başaran N. Antioxidant activities of major thyme ingredients and lack of (oxidative) DNA damage in V79 Chinese hamster lung fibroblast cells at low levels of carvacrol and thymol. Food Chem Toxicol. 2009;47(8):2037–2043. doi: 10.1016/j.fct.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 147.Ambrož M, Hanušová V, Skarka A, Boušová I, Králová V, Langhasová L, Skálová L. Essential oil from Myrica rubra leaves potentiated antiproliferative and prooxidative effect of doxorubicin and its accumulation in intestinal cancer cells. Planta Med. 2016;82(1–2):89–96. doi: 10.1055/s-0035-1558083. [DOI] [PubMed] [Google Scholar]
- 148.Langhasova L, Hanusova V, Rezek J, Stohanslova B, Ambroz M, Kralova V, Vanek T, Lou JD, Yun ZL, Yang J. Essential oil from Myrica rubra leaves inhibits cancer cell proliferation and induces apoptosis in several human intestinal lines. Ind Crops Prod. 2014;59:20–26. doi: 10.1016/j.indcrop.2014.04.018. [DOI] [Google Scholar]
- 149.Sun C, Huang H, Xu C, Li X, Chen K. Biological activities of extracts from Chinese bayberry (Myrica rubra Sieb. et Zucc.): a review. Plant foods Hum Nutr (Dordrecht, Netherlands) 2013;68(2):97–106. doi: 10.1007/s11130-013-0349-x. [DOI] [PubMed] [Google Scholar]
- 150.Llana-Ruiz-Cabello M, Gutiérrez-Praena D, Puerto M, Pichardo S, Jos Á, Cameán AM. In vitro pro-oxidant/antioxidant role of carvacrol, thymol and their mixture in the intestinal Caco-2 cell line. Toxicol in vitro. 2015;29(4):647–656. doi: 10.1016/j.tiv.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 151.Bartikova H, Hanusova V, Skalova L, Ambroz M, Bousova I. Antioxidant, pro-oxidant and other biological activities of sesquiterpenes. Curr Top Med Chem. 2014;14(22):2478–2494. doi: 10.2174/1568026614666141203120833. [DOI] [PubMed] [Google Scholar]
- 152.Kato Y, Ozawa S, Miyamoto C, Maehata Y, Suzuki A, Maeda T, Baba Y. Acidic extracellular microenvironment and cancer. Cancer Cell Int. 2013;13(1):89. doi: 10.1186/1475-2867-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Islam MT, Hossen M, Kamaz Z, Zali A, Kumar M, Docea AO, Arsene AL, Calina D, Sharifi-Rad J. The role of HMGB1 in the immune response to SARS-COV-2 infection: from pathogenesis towards a new potential therapeutic target. Farmacia. 2021;69(4):621–634. doi: 10.31925/farmacia.2021.4.1. [DOI] [Google Scholar]
- 154.Asgharian P, Tazekand AP, Hosseini K, Forouhandeh H, Ghasemnejad T, Ranjbar M, Hasan M, Kumar M, Beirami SM, Tarhriz V, et al. Potential mechanisms of quercetin in cancer prevention: focus on cellular and molecular targets. Cancer Cell Int. 2022;22(1):257. doi: 10.1186/s12935-022-02677-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ali ES, Akter S, Ramproshad S, Mondal B, Riaz TA, Islam MT, Khan IN, Docea AO, Calina D, Sharifi-Rad J, et al. Targeting Ras-ERK cascade by bioactive natural products for potential treatment of cancer: an updated overview. Cancer Cell Int. 2022;22(1):246. doi: 10.1186/s12935-022-02666-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Amin R, Quispe C, Docea AO, Ydyrys A, Kulbayeva M, Durna Daştan S, Calina D, Sharifi-Rad J. The role of tumour necrosis factor in neuroinflammation associated with Parkinson's disease and targeted therapies. Neurochem Int. 2022;158:105376. doi: 10.1016/j.neuint.2022.105376. [DOI] [PubMed] [Google Scholar]
- 157.Iqbal MJ, Javed Z, Herrera-Bravo J, Sadia H, Anum F, Raza S, Tahir A, Shahwani MN, Sharifi-Rad J, Calina D, et al. Biosensing chips for cancer diagnosis and treatment: a new wave towards clinical innovation. Cancer Cell Int. 2022;22(1):354. doi: 10.1186/s12935-022-02777-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Sutoo S, Maeda T, Suzuki A, Kato Y. Adaptation to chronic acidic extracellular pH elicits a sustained increase in lung cancer cell invasion and metastasis. Clin Exp Metastasis. 2020;37(1):133–144. doi: 10.1007/s10585-019-09990-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Taheri Y, Quispe C, Herrera-Bravo J, Sharifi-Rad J, Ezzat SM, Merghany RM, Shaheen S, Azmi L, Prakash Mishra A, Sener B, et al. Urtica dioica-derived phytochemicals for pharmacological and therapeutic applications. Evid Based Complement Alternat Med. 2022;2022:4024331. doi: 10.1155/2022/4024331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sethi G, Shanmugam MK, Ramachandran L, Kumar AP, Tergaonkar V. Multifaceted link between cancer and inflammation. Biosci Rep. 2012;32(1):1–15. doi: 10.1042/BSR20100136. [DOI] [PubMed] [Google Scholar]
- 161.Chai EZ, Siveen KS, Shanmugam MK, Arfuso F, Sethi G. Analysis of the intricate relationship between chronic inflammation and cancer. Biochem J. 2015;468(1):1–15. doi: 10.1042/BJ20141337. [DOI] [PubMed] [Google Scholar]
- 162.Kato Y, Maeda T, Suzuki A, Baba Y. Cancer metabolism: new insights into classic characteristics. Jpn Dent Sci Rev. 2018;54(1):8–21. doi: 10.1016/j.jdsr.2017.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Quispe C, Herrera-Bravo J, Khan K, Javed Z, Semwal P, Painuli S, Kamiloglu S, Martorell M, Calina D, Sharifi-Rad J. Therapeutic applications of curcumin nanomedicine formulations in cystic fibrosis. Prog Biomater. 2022 doi: 10.1007/s40204-022-00198-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Toden S, Theiss AL, Wang X, Goel A. Essential turmeric oils enhance anti-inflammatory efficacy of curcumin in dextran sulfate sodium-induced colitis. Sci Rep. 2017;7(1):814. doi: 10.1038/s41598-017-00812-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Dimas KS, Pantazis P, Ramanujam R. Review: Chios mastic gum: a plant-produced resin exhibiting numerous diverse pharmaceutical and biomedical properties. In vivo (Athens, Greece) 2012;26(5):777–785. [PubMed] [Google Scholar]
- 166.Giaginis C, Theocharis S. Current evidence on the anticancer potential of Chios mastic gum. Nutr Cancer. 2011;63(8):1174–1184. doi: 10.1080/01635581.2011.607546. [DOI] [PubMed] [Google Scholar]
- 167.Paraschos S, Mitakou S, Skaltsounis AL. Chios gum mastic: a review of its biological activities. Curr Med Chem. 2012;19(14):2292–2302. doi: 10.2174/092986712800229014. [DOI] [PubMed] [Google Scholar]
- 168.Balan KV, Demetzos C, Prince J, Dimas K, Cladaras M, Han Z, Wyche JH, Pantazis P. Induction of apoptosis in human colon cancer HCT116 cells treated with an extract of the plant product, Chios mastic gum. In vivo (Athens, Greece) 2005;19(1):93–102. [PubMed] [Google Scholar]
- 169.Balan KV, Prince J, Han Z, Dimas K, Cladaras M, Wyche JH, Sitaras NM, Pantazis P. Antiproliferative activity and induction of apoptosis in human colon cancer cells treated in vitro with constituents of a product derived from Pistacia lentiscus L. var.chia. Phytomedicine. 2007;14(4):263–272. doi: 10.1016/j.phymed.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 170.Catalani S, Palma F, Battistelli S, Benedetti S. Oxidative stress and apoptosis induction in human thyroid carcinoma cells exposed to the essential oil from Pistacia lentiscus aerial parts. PLoS ONE. 2017;12(2):e0172138. doi: 10.1371/journal.pone.0172138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Amorim JL, Simas DL, Pinheiro MM, Moreno DS, Alviano CS, da Silva AJ, Fernandes PD. Anti-inflammatory properties and chemical characterization of the essential oils of four citrus species. PLoS ONE. 2016;11(4):e0153643. doi: 10.1371/journal.pone.0153643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Maxia A, Sanna C, Frau MA, Piras A, Karchuli MS, Kasture V. Anti-inflammatory activity of Pistacia lentiscus essential oil: involvement of IL-6 and TNF-alpha. Nat Prod Commun. 2011;6(10):1543–1544. [PubMed] [Google Scholar]
- 173.Farhana L, Sarkar S, Nangia-Makker P, Yu Y, Khosla P, Levi E, Azmi A, Majumdar APN. Natural agents inhibit colon cancer cell proliferation and alter microbial diversity in mice. PLoS ONE. 2020;15(3):e0229823. doi: 10.1371/journal.pone.0229823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhang L, Bai Y, Yang Y. Thymoquinone chemosensitizes colon cancer cells through inhibition of NF-κB. Oncol Lett. 2016;12(4):2840–2845. doi: 10.3892/ol.2016.4971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Shanmugam MK, Arfuso F, Kumar AP, Wang L, Goh BC, Ahn KS, Bishayee A, Sethi G. Modulation of diverse oncogenic transcription factors by thymoquinone, an essential oil compound isolated from the seeds of Nigella sativa Linn. Pharmacol Res. 2018;129:357–364. doi: 10.1016/j.phrs.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 176.Flores SE, Rial-Hermida MI, Ramirez JC, Pazos A, Concheiro A, Alvarez-Lorenzo C, Peralta RD. Microemulsions for colorectal cancer treatments. General considerations and formulation of methotrexate. Mini Rev Med Chem. 2016;16(6):498–508. doi: 10.2174/1389557515666150909142920. [DOI] [PubMed] [Google Scholar]
- 177.Sefidkon F, Abbasi K, Khaniki GB. Influence of drying and extraction methods on yield and chemical composition of the essential oil of Satureja hortensis. Food Chem. 2006;99(1):19–23. doi: 10.1016/j.foodchem.2005.07.026. [DOI] [Google Scholar]
- 178.Russo A, Formisano C, Rigano D, Senatore F, Delfine S, Cardile V, Rosselli S, Bruno M. Chemical composition and anticancer activity of essential oils of Mediterranean sage (Salvia officinalis L) grown in different environmental conditions. Food Chem Toxicol. 2013;55:42–47. doi: 10.1016/j.fct.2012.12.036. [DOI] [PubMed] [Google Scholar]
- 179.Garzoli S, Pirolli A, Vavala E, Di Sotto A, Sartorelli G, Božović M, Angiolella L, Mazzanti G, Pepi F, Ragno R. Multidisciplinary approach to determine the optimal time and period for extracting the essential oil from Mentha suaveolens Ehrh. Molecules (Basel, Switzerland) 2015;20(6):9640–9655. doi: 10.3390/molecules20069640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Mehdizadeh L, Moghaddam M. Essential oils: biological activity and therapeutic potential. In: therapeutic, probiotic, and unconventional foods. Amsterdam: Elsevier; 2018. pp. 167–179. [Google Scholar]
- 181.Khalil N, El-Jalel L, Yousif M, Gonaid M. Altitude impact on the chemical profile and biological activities of Satureja thymbra L. essential oil. BMC Complement Med Ther. 2020;20(1):186. doi: 10.1186/s12906-020-02982-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Khatamian N, Homayouni Tabrizi M, Ardalan P, Yadamani S, Darchini Maragheh A. Synthesis of Carum Carvi essential oil nanoemulsion, the cytotoxic effect, and expression of caspase 3 gene. J Food Biochem. 2019;43(8):e12956. doi: 10.1111/jfbc.12956. [DOI] [PubMed] [Google Scholar]
- 183.Quispe C, Herrera-Bravo J, Javed Z, Khan K, Raza S, Gulsunoglu-Konuskan Z, Daştan SD, Sytar O, Martorell M, Sharifi-Rad J, et al. Therapeutic applications of curcumin in diabetes: a review and perspective. Biomed Res Int. 2022;2022:1375892. doi: 10.1155/2022/1375892. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. CRC preclinical models.
Data Availability Statement
Not Applicable.