Abstract
BACKGROUND
Telemedicine provides a gateway to specialty care that, otherwise, patients with multiple sclerosis (MS) could have difficulty accessing. Studies have shown that telemedicine provides a valid alternative to in-person visits. There are limited data on the strengths and limitations of telemedicine from the perspective of MS providers.
METHODS
After reviewing the literature and pilot testing questions about telemedicine in provider focus groups, a 34-question survey was created on the Qualtrics web platform. A stratified sample of MS providers throughout the United States was recruited to participate. The survey initiated in November 2019 and closed in November 2020.
RESULTS
Survey participants (N = 94) included neurologists (43.0%), advanced practice providers (28.0%), nurses (14.0%), mental health providers (7.0%), social workers (3.0%), rehabilitation providers (4.0%), and pharmacists (1.0%). Clinical video telemedicine (CVT) was the most commonly used platform, and 76.6% of respondents indicated that they used telemedicine to care for patients with MS. As a result of the COVID-19 pandemic, the rate of telemedicine use increased from 44.4% to 84.2%. Most health care providers (93.0%) were “very satisfied” or “somewhat satisfied” with their most recent telemedicine visit, and 94.4% of providers reported a desire to continue using telemedicine, although 84.6% found it difficult to perform a full examination.
CONCLUSIONS
There was a large uptick in the use of telemedicine when the COVID-19 pandemic forced clinics to cease in-person visits. Providers predominantly used CVT; store-and-forward telemedicine and remote patient monitoring have fewer technical issues than CVT and seem to be underused.
Keywords: telemedicine, COVID-19, survey, multiple sclerosis
It is often difficult for patients with multiple sclerosis (MS) to access specialty care; major barriers include geographic distance from providers, traveling restrictions due to neurologic disability, and limited or partial health insurance coverage.1 Access is further impaired by inclement weather and health-related concerns (eg, COVID-19, MS flare). One study showed that 30% of patients with MS do not see a neurologic specialist for their care.2 Patients who are seen by a neurologist are more likely to be prescribed a disease-modifying treatment and receive multidisciplinary services,2 improving their quality of life.
Telemedicine, the use of technology to provide access to clinical care when distance separates patients and providers,3 could allow for broader and more convenient access to MS specialty care. There are several types of telemedicine: (1) clinical video telemedicine (CVT), in which a provider and patient communicate through an audiovisual platform (eg, Zoom [Zoom Video Communications, Inc]); (2) pure audio real-time interface (eg, performing telephone surveys); (3) store-and-forward telemedicine, in which patient test results (eg, cognitive tests, optical coherence tomography) are stored and then reviewed by a remote clinician; and (4) remote monitoring, which includes wearing a device or using an app that sends real-time data to a remote provider.3
The COVID-19 pandemic forced a shift in how practitioners provided care due to the need for social distancing to decrease potential exposures for a patient population that is at higher risk4 than the general population. Providers and the National Multiple Sclerosis Society issued guidance for using telemedicine to help reduce this risk.5 This was made possible by health insurance providers relaxing restrictions on reimbursement for telemedicine services, which had resulted in limited use.4 Centers for MS quickly made plans to transition to telemedicine platforms.6 As a result, there was a massive rise in the use of teleneurology, with virtual visits skyrocketing and in-person visits plummeting.4
Most studies looking at the use of telemedicine in MS care have been single-center studies with small sample sizes. There are limited data on the strengths and limitations of telemedicine from the perspective of MS providers. Designed and begun before the rise of COVID-19, this study aimed to examine the views of a large, diverse group of MS care providers on telemedicine. We were fortunate to capture the pre–COVID-19 pandemic period as well as the pandemic period in the survey.
METHODS
The survey questions were developed by evaluating the current telemedicine literature3 and previous surveys of telemedicine in MS care.7 Questions were pilot tested for readability, relevance, and completion time with a group of 10 MS care providers in the Washington, DC, region. Once finalized, the questions were uploaded to the Qualtrics web platform (Qualtrics). The survey consent, platform, and distribution were approved by the Washington, DC, Veterans Affairs Medical Center institutional review board.
The study team sampled providers from the 4 US Census regions by targeting major MS programs in these regions along with MS provider groups (eg, the International Organization of Multiple Sclerosis Nurses). Major MS programs were tertiary referral centers and part of the Consortium of Multiple Sclerosis Centers. The MS provider groups were composed of the core subspecialists that care for patients with MS. We sampled several different types of MS programs (eg, academic, private practice, government) in different geographic areas of the United States. The MS health care provider sample included (1) specialty and general neurologists, (2) rehabilitation specialists (eg, physiatrists, physical and occupational therapists), (3) advanced practice providers (APPs), (4) nurse specialists, and (5) other specialty providers (eg, psychologists, psychiatrists, social workers). The goal was to assess a broad national sample of MS health care providers to determine use patterns and views of telehealth.
The survey was composed of 34 questions and was distributed using a secure Qualtrics platform weblink to individual email addresses (FIGURE S1, which is published in the online version of this article at IJMSC.org). Original emails were sent to the practice as a whole, and then follow-up emails targeted individual providers; 2 or 3 reminder emails were sent, which increased participation 25% on average. The actual response rate is unclear because the number of people who received the initial group email is unknown; depending on the practice, it seems to have ranged from approximately 50% to 100%. The MS health care providers completed the web-based survey between November 20, 2019, and November 15, 2020. Responses were then stratified based on those who completed the survey before March 2020 (pre–COVID-19 pandemic) and during and after March 2020 (peri–COVID-19 pandemic).
The web-based survey data contained no unique identifiers. Survey responses were analyzed using Qualtrics software and SAS version 15.2 (SAS Institute Inc). Participants were not offered compensation or incentives to participate in the survey.
RESULTS
Overview of Respondents
The survey was opened by 105 people; 94 completed the full survey, representing a diverse group of provider types (TABLE S1). The respondents’ specialty areas were as follows: neurologist (n = 40; 42.6%); APPs (n = 26; 27.7%); nurse (n = 13;13.8%); psychologist, neuropsychologist, or psychiatrist (n = 7; 7.4%); social worker (n = 3; 3.2%); physiatrist (n = 2; 2.1%); physical therapist or occupational therapist (n = 2; 2.1%); and pharmacist (n = 1; 1.1%). The breakdown by US Census region was balanced. The providers had been in practice for a mean ± SD of 17.5 ± 12.1 years (range, 1–49 years).
In terms of use, 72 (76.6%) of the 94 respondents indicated that they had used telemedicine to evaluate patients with MS. Of those who had used telemedicine, a mean of 65.5% of their practice was dedicated to telemedicine. The most common platform for telemedicine was CVT (87.5%); 70.8% had used pure audio (ie, telephone counseling or surveys), 9.7% had used store-and-forward telemedicine, and 1.4% had used remote patient monitoring. Most providers used CVT in nonclinical settings (ie, from home) (82%) vs in clinical settings (ie, remote clinic room) (7.9%), with 11.1% of providers seeing patients in both settings. All providers had telehealth encounters in their same state, with a large portion also seeing patients across state lines (75.0%). A small proportion of MS providers even saw patients internationally (4.2%).
Overall, 93.0% of respondents were “very satisfied” or “somewhat satisfied” with their most recent telemedicine visit, 4.2% were “neither satisfied nor dissatisfied,” and 2.8% were “somewhat dissatisfied.” Respondents stated that they would “definitely” (73.2%) or “probably” (21.1%) like to continue using telemedicine, with 1.4% “not being sure” and 4.2% “probably not wanting” to use telemedicine again (FIGURE S2).
Providers reported that the benefits of telemedicine were improved access to services or specialists for patients (88.2%), greater convenience for providers (57.0%), lower costs for providers (29.0%), and better interactions with patients (28.0%) (FIGURE 1). Among the write-in advantages for telemedicine, the most common answer was greater convenience for patients (28.0%). Alternatively, 3.2% of providers responded, “Telemedicine would not provide any advantages for me,” and 2.1% were not sure what advantages there were.
FIGURE 1.
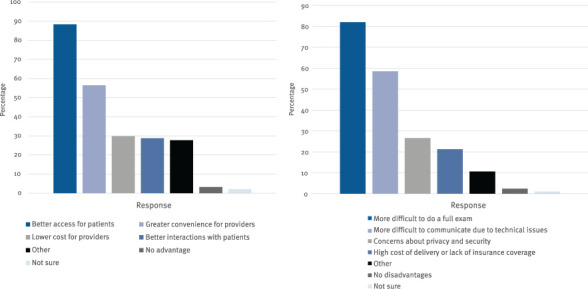
Respondents' Agreement With Advantages and Disadvantages of Telemedicine.
Among the challenges with telemedicine, 84.6% of providers felt that it was difficult to perform a full examination using a remote platform (Figure 1). Other disadvantages reported were difficulties communicating with patients due to technological issues (60.4%), concerns about privacy and security (26.4%), the high cost of telemedicine equipment and support or lack of health insurance coverage (22.0%), and the inability to view laboratory test results (8.8%). A small group of providers felt that telemedicine would not provide any disadvantages for their practice (2.2%).
Pre–COVID-19 and Peri–COVID-19 Pandemic Differences in Telemedicine
No surveys were completed between December 24, 2019, and March 17, 2020, providing a clear divide between respondents before the COVID-19 pandemic in the United States and those during the COVID-19 pandemic. The first case of COVID-19 was diagnosed in the United States in February 2020, but the response to the pandemic did not begin until March 2020.8 The last survey response was completed in November 2020. There were 18 survey responses before the start of the pandemic and 77 during the pandemic.
Looking at the data collected before vs during the COVID-19 pandemic, there was a dramatic rise in provider use of telemedicine, from 44.4% to 84.2% (Figure S3). During the peripandemic period, providers also dedicated more of their practice to telemedicine: 72.4% vs 14.4% before the pandemic (FIGURE 2). During the peripandemic period, providers were more likely to be unsatisfied with their most recent telemedicine visit (3.1% vs 0%) and to experience technical difficulties (89.3% vs 57.1%) and were less likely to be confident in their findings via telemedicine (21.9% vs 62.5%), to have telemedicine training (78.1% vs 87.5%), and to want to continue using telemedicine (93.8% vs 100%).
FIGURE 2.
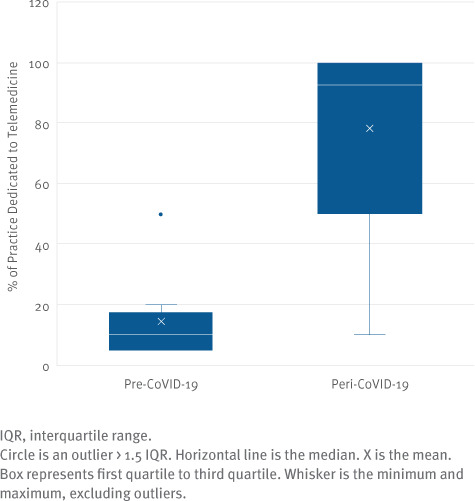
Percentage of Practice Dedicated to Telemedicine by Respondents Before vs During the COVID-19 Pandemic
Provider Similarities and Differences in Telemedicine
There do not seem to be differences in satisfaction with the most recent telemedicine visit or desire to continue using telemedicine in the future among different provider types. There are differences in use of telemedicine and percentage of practice dedicated to telemedicine: neurologists, APPs, and nurses had similar use (75%–80%) and practice dedication (65%–70%); psychiatrists/psychologists had notably lower telemedicine use (57.1%) and practice dedication (43.8%). Neurologists were less confident in their evaluations via CVT compared with their in-person evaluations, with 24.2% reporting that they are not as confident; 9.5% of APPs were less confident as well, but no other provider type cited less confidence.
Regional Differences
Practitioners who did not use telemedicine were more likely to be from the South. The low rate of telemedicine use persisted during the pandemic: in the South, telemedicine use was 70.8%, compared with 89.5% in the Northeast and the West and 92.9% in the Midwest. When prepandemic numbers are included, the south’s telemedicine use drops to 59.5%. The South also had the lowest percentage of practice dedicated to telemedicine, 42.7%, compared with the Northeast’s 70.9%, the Midwest’s 84.3%, and the West’s 82.4%.
Years in Practice Differences
There did not seem to be a strong correlation between the number of years in practice and the use of telemedicine or percentage of practice dedicated to telemedicine. In fact, the highest percentage of telemedicine use was among those with more than 30 years practicing medicine (90.9%), slightly above those who had been in practice 5 years or less (89.5%). The lowest use of telemedicine was among providers who had been in practice 6 to 10 years (61.5%); those practicing 21 to 30 years (70%) and 11 to 20 years (74.2%) were closer to the average.
DISCUSSION
This survey of 94 MS providers from around the United States gives a glimpse into their telemedicine use and their opinions regarding its benefits and limitations. Overall, most MS providers are comfortable using CVT and other types of telemedicine to evaluate patients. Telemedicine’s strengths included improved access and convenience and lower costs. Challenges were interpreting remote examinations, communicating with patients, and technical difficulties. This survey assessed MS providers before and during the COVID-19 pandemic; given the exponential growth in the use of telemedicine, provider views on its benefits and disadvantages are even more important.
Previous surveys of all physician types showed that telemedicine was vastly underused, with a 2016 study showing that only 15.4% of providers had used this option. Neurologists showed slightly better than average use compared with other physicians at 17.4%.9 Similar to the present study, CVT was the preferred mode of telemedicine, with store-and-forward telehealth and remote patient monitoring rarely used.
A recent article showed most MS providers (95.1%) using telemedicine in mid-2020, with almost half dedicating more than 50% of their practice to remote encounters.10 The overall higher percentage of telemedicine use but lower percentage of time dedicated to telemedicine compared with the present study may be accounted for by our longer period of data collection, which included earlier parts of the pandemic. This report did not capture data on prepandemic use of telemedicine.
Patients have expressed enthusiasm about using mobile and wearable devices to track clinical outcomes,11 and, as this study shows, this type of telemedicine tends to have fewer technical difficulties than CVT. Despite these advantages, there is limited clinical use of these types of telemedicine.
Among practitioners who said they were not sure whether they would like to continue using telemedicine or would probably not want to continue using telemedicine, 3 were neurologists and 1 was an APP. They had been in practice for a mean ± SD of 25.3 ± 13.9 years (range, 14.0–49.0 years). All 4 practitioners indicated that they had received training in telemedicine and felt very comfortable with computers, and 3 stated they that were not as confident in their evaluations. They were either “somewhat satisfied” or “neither satisfied nor dissatisfied” with their most recent telemedicine visit. Two were from the South, 1 was from the Midwest, and 1 was from the West.
Of interest, satisfaction with the most recent telemedicine visit did not seem to correlate with the desire to continue using telemedicine. Of the 6 providers who said that they were “somewhat disappointed” or “neither disappointed nor satisfied” with their most recent visit, 2 said that they would definitely want to continue using telemedicine, 2 said that they would probably want to continue, and 2 said that they would probably not want to continue.
Regional differences may be explained by differing loca government levels of pandemic restriction on travel and social distancing. Although other regions imposed strict lockdowns, the South did not completely restrict movement between states and within businesses. This may account for the reduced use of telemedicine in the South. In addition, telehealth policies vary between states. Many states in the south did not pass as many comprehensive laws to expand telemedicine coverage.12 This is consistent with the idea that the increase in telemedicine was due to necessity during the COVID-19 pandemic.
There are several differences in the pre–COVID-19 pandemic and the peripandemic responders. First, the peripandemic responders spent much more of their practice performing telemedicine, reported a higher percentage of technical difficulties, were less confident in their ability to assess and treat patients compared with in-person interactions, and had less telemedicine resources/support. The most likely explanation for these differences between the prepandemic group and the peripandemic group is that those already using telemedicine before the onset of the pandemic had chosen to make this a part of their practice and were comfortable with the technology. These clinics had the support, contingency plans, and tools necessary to run their operations smoothly, whereas the peri–COVID-19 pandemic group included providers who were forced into telemedicine by default. In addition, the surge of telemedicine use likely taxed the information technology infrastructure, and peripandemic providers were spending a far greater proportion of their practice using telemedicine. Teleconferencing fatigue is an often-experienced phenomenon that could explain some practitioners’ negative attitudes toward telemedicine.13 Finally, the pre–COVID-19 pandemic group skewed younger with less years of experience in practice compared with the peripandemic group. This age gap may have played a part in why those in the prepandemic group were earlier adopters of telemedicine and felt more comfortable with its implementation.
There are several recent studies demonstrating how telehealth has been successfully used in various aspects of MS care, including fatigue management14 and rehabilitation.15 The use of CVT has been shown to be feasible and cost-effective, and it had high satisfaction ratings from both patients and providers.3 Studies have shown little to no difference between telemedicine and in-person interventions3 and have demonstrated that the Expanded Disability Status Scale evaluation can be successfully and reliably completed via telemedicine.16 In addition, telemedicine has been shown to reduce patient travel burden, lower the indirect costs of missed work, and lower caregiver burden.17
The strengths of this study include reaching a diverse pool of providers, not only in scope of practice, but also in geography. We acquired responses from all corners of the United States, representing 24 states and the District of Columbia. We also received input from a multidisciplinary range of MS care providers. Finally, the timing of the start of the study allowed us to collect data before and after the pandemic.
A limitation of this study is the limited scope of health care providers. Although the study sampled a wide range of providers, most were neurologists, APPs, or nurses, with only a few responders from other provider types. As a result, it is hard to compare these other provider types and may account for some of the intergroup differences noted. Moreover, the sample size of the pre–COVID-19 pandemic group is significantly smaller than that of the peripandemic group; a larger sample may have yielded more representative results. The study was designed before the COVID-19 pandemic, but the start date resulted in a limited recruitment period and a small sample before the pandemic onset. Ideally, a larger prepandemic sample coupled with the opportunity to retake the survey after the near universal adoption of telemedicine during the pandemic would have illustrated how provider views on telemedicine changed after increased exposure.
CONCLUSION
Overall, telemedicine provides a pathway to improve access to high-quality, cost-effective care for patients with MS and their providers. Most providers using CVT were satisfied, and the less technically challenging options of store-and-forward telemedicine and remote patient monitoring can be better used. Except for select clinical situations (eg, neurologic procedures), technological and reimbursement problems can be resolved if the practices and policies instituted during the pandemic are preserved. There is federal and state legislation to continue the current insurance reimbursements and policy allowances for telemedicine.18 Further studies are needed to see how the levels of training and support for telemedicine change as the use of telemedicine increases. To improve patient care and outcomes, the MS community, patients and providers of all types, should work toward nationwide telemedicine funding and interoperability.
PRACTICE POINTS
» Use of telemedicine skyrocketed when the COVID-19 pandemic forced many multiple sclerosis health care providers to engage with telemedicine platforms for the first time.
» Despite initial concerns about their ability to perform a comprehensive physical examination and to overcome technical difficulties, multiple sclerosis health care providers were overall satisfied using telemedicine.
» Two underused forms of telemedicine with low technical error rates and, thus, the potential for growth, are store-and-forward and remote monitoring.
Supplementary Material
ACKNOWLEDGMENTS:
Thanks to the health care providers who participated in the surveys and responded to the promises and challenges of telemedicine.
Funding Statement
FUNDING/SUPPORT: This study was supported by the National Multiple Sclerosis Society (HC-1610-25978) and the US Department of Veterans Affairs Multiple Sclerosis Center of Excellence.
Footnotes
FINANCIAL DISCLOSURES: The authors declare no conflicts of interest.
PRIOR PRESENTATION: Preliminary data from this study were presented as part of an abstract poster at the Americas Committee on Treatment and Research in MS Forum 2021 Virtual Conference; February 25-27, 2021.
REFERENCES
- 1.D’Haeseleer M, Eelen P, Sadeghi N, D’Hooghe MB, Van Schependom J, Nagels G. Feasibility of real time internet-based teleconsultation in patients with multiple sclerosis: interventional pilot study. J Med Internet Res . 2020;22(8):e18178. doi: 10.2196/18178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robb JF, Hyland MH, Goodman AD. Comparison of telemedicine versus in-person visits for persons with multiple sclerosis: a randomized crossover study of feasibility, cost, and satisfaction. Mult Scler Relat Disord . 2019;36:101258. doi: 10.1016/j.msard.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Yeroushalmi S, Maloni H, Costello K, Wallin MT. Telemedicine and multiple sclerosis: a comprehensive literature review. J Telemed Telecare . 2019;26(7–8):400. doi: 10.1177/1357633x19840097. [DOI] [PubMed] [Google Scholar]
- 4.McGinley MP, Ontaneda D, Wang Z et al. Teleneurology as a solution for outpatient care during the COVID-19 pandemic. Telemed J E Health . 2020;26(12):1537–1539. doi: 10.1089/tmj.2020.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brownlee W, Bourdette D, Broadley S, Killestein J, Ciccarelli O. Treating multiple sclerosis and neuromyelitis optica spectrum disorder during the COVID-19 pandemic. Neurology . 2020;94(22):949–952. doi: 10.1212/WNL.0000000000009507. [DOI] [PubMed] [Google Scholar]
- 6.Grossman S, Han S, Balcer L et al. Rapid implementation of virtual neurology in response to the COVID-19 pandemic. Neurology . 2020;94(24):1077–1087. doi: 10.1212/WNL.0000000000009677. [DOI] [PubMed] [Google Scholar]
- 7.Marziniak M, Brichetto G, Feys P, Meyding-Lamadé U, Vernon K, Meuth SG. The use of digital and remote communication technologies as a tool for multiple sclerosis management: narrative review. JMIR Rehabil Assist Technol . 2018;5(1):e5. doi: 10.2196/rehab.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jorden MA, Rudman SL, Villarino E, et al. ; CDC COVID-19 Response Team Evidence for limited early spread of COVID-19 within the United States, January–February 2020. MMWR Morb Mortal Wkly Rep . 2020;69(22):680–684. doi: 10.15585/mmwr.mm6922e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood) . 2018;37(12):1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 10.Morrison EH, Michtich K, Hersh CM. How the COVID-19 pandemic has changed multiple sclerosis clinical practice: results of a nationwide provider survey. Mult Scler Relat Disord . 2021;51:102913. doi: 10.1016/j.msard.2021.102913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marrie RA, Leung S, Tyry T, Cutter GR, Fox R, Salter A. Use of eHealth and mHealth technology by persons with multiple sclerosis. Mult Scler Relat Disord . 2019;27:13–19. doi: 10.1016/j.msard.2018.09.036. [DOI] [PubMed] [Google Scholar]
- 12.States’ actions to expand telemedicine access during COVID-19 and future policy considerations. The Commonwealth Fund. June 23, 2021. Accessed July 13, 2021. https://www.commonwealthfund.org/publications/issue-briefs/2021/jun/states-actions-expand-telemedicine-access-covid-19.
- 13.Bailenson JN. Nonverbal overload: a theoretical argument for the causes of Zoom fatigue. Technol Mind Behav . 2021;2(1) doi: 10.1037/TMB0000030. [DOI] [Google Scholar]
- 14.Plow M, Packer T, Mathiowetz VG et al. REFRESH protocol: a non-inferiority randomised clinical trial comparing internet and teleconference to in-person ‘Managing Fatigue’ interventions on the impact of fatigue among persons with multiple sclerosis. BMJ Open . 2020;10(8):e035470. doi: 10.1136/bmjopen-2019-035470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw MT, Best P, Frontario A, Charvet LE. Telerehabilitation benefits patients with multiple sclerosis in an urban setting. J Telemed Telecare . 2021;27(1):39–45. doi: 10.1177/1357633X19861830. [DOI] [PubMed] [Google Scholar]
- 16.Bove R, Bevan C, Crabtree E et al. Toward a low-cost, in-home, telemedicine-enabled assessment of disability in multiple sclerosis. Mult Scler J . 2019;25(11):1526–1534. doi: 10.1177/1352458518793527. [DOI] [PubMed] [Google Scholar]
- 17.Bove R, Garcha P, Bevan C, Crabtree-Hartman E, Green A, Gelfand J. Clinic to in-home telemedicine reduces barriers to care for patients with MS or other neuroimmunologic conditions. Neurol Neuroimmunol Neuroinflamm . 2018;5(6):e505. doi: 10.1212/NXI.0000000000000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wicklund E. The CONNECT Act is back, giving telehealth policy a 4th shot at passage. mHealth Intelligence. Accessed July 13, 2021. https://mhealthintelligence.com/news/the-connect-act-is-back-giving-telehealth-policy-a-4th-shot-at-passage.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


