Abstract
Morbidity and mortality are on the rise among Baby Boomers and younger cohorts. This study investigates whether this unfavorable health trend across birth cohorts 1925–1999 is related to rising income inequality Americans face during childhood. We use two nationally representative datasets: National Health and Nutrition Examination Surveys (NHANES) 1988–2018 and Panel Studies of Income Dynamics (PSID) 1968–2013, and two health outcomes: biomarkers of physiological dysregulation, and a chronic disease index. Childhood income inequality is measured by the average of the Gini index at the national level each birth cohort is exposed to between birth and age 18, where the Gini index from 1925 to 2016 is computed based on Internal Revenue Service income data. By merging childhood income inequality to individual level data from NHANES or PSID based on birth cohort, we find childhood income inequality is positively associated with the risk of physiological dysregulation in adulthood for all gender and racial groups in the NHANES data. It is also significantly related to the risk of chronic disease in the PSID data. This association is robust to controls for individual level childhood health and family background, adulthood socioeconomic and marital status, and contemporary macro socioeconomic factors. More importantly, childhood income inequality exposure explains a substantial amount of variation in these two health outcomes across cohorts, a pattern not observed for other early life exposures that display negative temporal trends similar to those for childhood income inequality. This study provides important evidence that income inequality experienced during childhood may have a long-lasting negative consequence for adult health, which partially explains the adverse health trends experienced by Baby Boomers and younger cohorts in the United States.
Keywords: Childhood income inequality, Early-life conditions, Adult health, Physiological dysregulation, Chronic diseases, Health trend, Health decline
Introduction
Stagnating and declining life expectancy since 2015 has become an alarming population health crisis in the United States. This declining life expectancy has been attributed to rising drug-, alcohol-, and suicide-related mortality combined with slowing progress in combating heart disease (Barbieri, 2019; Case and Deaton, 2017) although their relative contributions may differ by demographic groups (i.e., race and gender) (National Academies of Sciences, Engineering, and Medicine (NASEM), 2021). Much attention has been focused on Baby Boomers who reached middle age and early old age in the past two decades, while recent studies report the declining health trend has extended to younger age groups or recent birth cohorts (NASEM, 2021; Zang et al., 2019). For example, physiological dysregulation (PD), the early stage of the morbidity process (Crimmins et al., 2010) and indicated by several biological risk factors, such as inflammation, metabolic syndrome, and deterioration of lung and renal function (Seeman et al. 2001), has continuously increased for Baby Boomers and members of the Generation X and Generation Y cohorts (Zheng and Echave, 2021).
At the same time, income inequality has been dramatically increasing since the mid-1940s when Baby Boomers were born (Frank, 2014). In fact, the deteriorating trend in PD across cohorts very closely mirrors the trend of income inequality (indicated by the Gini coefficient) experienced during childhood (ages 0–18) across cohorts as shown in Figure 1. Both PD and childhood income inequality declined from Early Children of the Depression (1925–1930) until War Babies (1943–1945) and increased since early Baby Boomers (1946–1955). May the declining health across cohorts partially result from rising income inequality Americans faced during their childhoods?
Figure 1. Cohort trend in physiological dysregulation and childhood Gini coefficient.
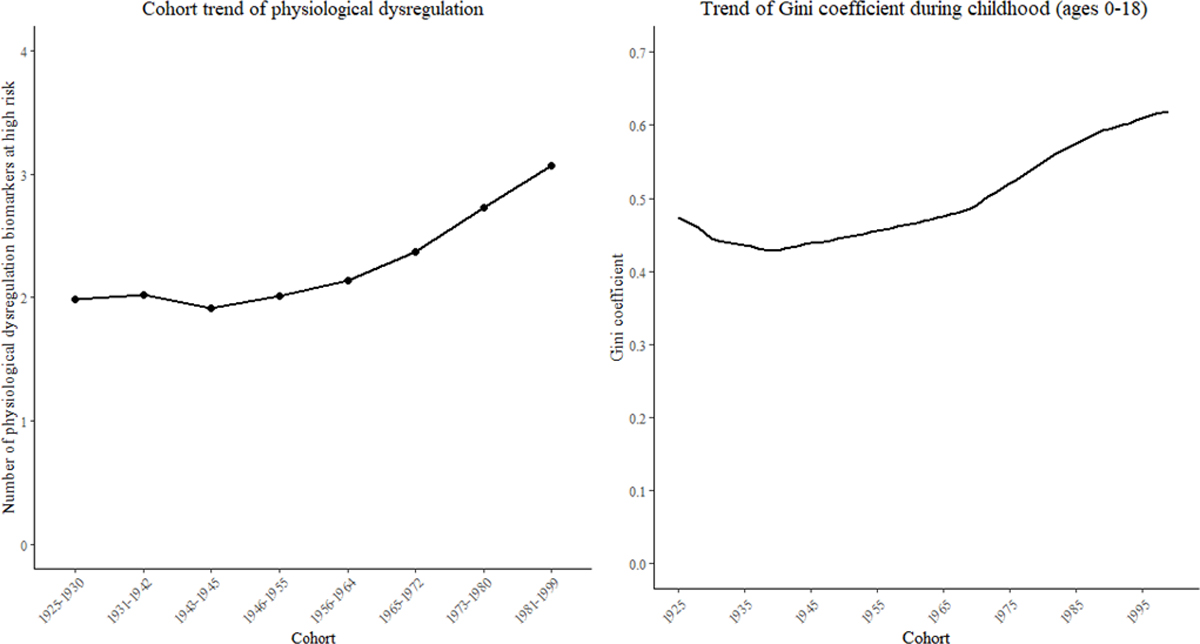
Notes: Date source for physiological dysregulation is National Health and Nutrition Examination Survey (NHANES) 1988–2018. Physiological dysregulation is summary index of nine biomarkers including seven markers of metabolic functions, one marker of chronic inflammation (i.e., low serum albumin), and one additional marker (i.e., urinary function-creatinine clearance). The cohort trend is obtained from the random effect coefficients of cohort based on Poisson mixed effects models with fixed effect coefficient of age and random effect coefficients of cohort and period. Gini coefficient during childhood (ages 0–18) is computed based on Internal Revenue Service income data (Frank, 2014). The childhood Gini coefficient is the average of Gini coefficients each cohort is exposed to between ages of 0 and 18.
Exposure to income inequality in early life may impact later life health through material and psychosocial pathways. First, income inequality may lead to the reduction of socioeconomic resources people need to produce health. In societies with rising inequalities, the interests of economic elites begin to diverge from those of average citizens (Kawachi and Kennedy, 1999). The economic elites demand specialized services or policies that help maintain their wealth such as tax breaks and are less likely to support income redistribution or public expenditure policies (e.g., public education and health care) that do not directly benefit them (Bartels, 2008; Osberg et al., 2004; Ponzetto and Troiano, 2018). Studies show politicians are more likely to support policies that match the interests of the affluent because they have a vested interest in maintaining a strong economy and are reliant on the economic resources of the affluent to advance their political agendas (e.g., campaign contributions) (Gilens, 2012; Gilens and Page, 2014). That is a major reason why countries with greater income inequality tend to devote fewer resources to public expenditure policies (Osberg et al., 2004). Therefore, children growing up in a period of rising income inequality may face reduced social spending, which can lead to a reduction of life opportunities and deterioration of life circumstances throughout their life course (Bradley and Taylor, 2013; Davey, 1996; Kaplan et al., 1996).
Second, rising income inequality can also intensify relative deprivation, which emphasizes the gap between one’s own income and incomes of those richer than oneself. Relative deprivation is associated with risky behaviors (e.g., smoking, obesity) and heightened mortality (Eiber et al., 2004; Eibner and Evans, 2005). That is because relative deprivation induces psychological stress (e.g., negative self-assessment, frustration, and depression), which can harm health in the long run (Kawachi and Kennedy, 1999; Kondo et al., 2008). Third, income inequality leads to loss of social cohesion and the erosion of social capital (Wilkinson, 1992, 1996), suggesting that inequality acts as a social stressor (Pickett and Wilkinson, 2015). In more unequal societies, people show less solidarity, less concern for social harmony, and less willingness to help others (de Vries et al., 2011; Paskov and Dewilde, 2012; Putnam and Garrett, 2020). Lack of social cohesion has been found to be harmful for cognitive, emotional, and behavioral outcomes (DeWall et al., 2011) and mediate the association between income inequality and health (Delhey and Dragolov, 2014; Kawachi et al., 1997; Zimmerman and Bell, 2006). These psychosocial pathways suggest that children growing up in a period of rising income inequality are exposed to exacerbated relative deprivation and social isolation, which can have long-lasting negative consequences for their mental and physical well-being (Kawachi and Kennedy, 1999).
Based on these discussions, we hypothesize that childhood income inequality has long-lasting consequences for adult health. Exposure to rising childhood inequality contributes to declining adult health across cohorts. We use two independent datasets -- the National Health and Nutrition Examination Surveys (NHANES) and Panel Studies of Income Dynamics (PSID)) -- to test this hypothesis and account for various confounders across the life course. This study provides the first investigation on how childhood income inequality since the second half of the last century may have a lingering impact on U.S. population health.
Background Literature on Income Inequality and Health
The relationship between income inequality and health has been extensively studied, but current literature has provided mixed findings. Many scholars now are skeptical of the adverse impact of income inequality on health (e.g., Leigh and Jencks, 2007; Mellor and Milyo, 2003) while others believe the initial theoretical arguments and maintain that the effects may still exist in certain situations (e.g., Lillard et al., 2015; Tibber et al., 2022; Zheng, 2012). This uncertainty has high stakes as most developed and developing countries have experienced dramatic increases in income inequality in the past several decades. If income inequality adversely affects health, then even a small effect may have considerable consequences for the population as a whole (Kondo et al., 2009).
These mixed findings have been attributed to differences in countries, time periods, units of analysis, levels of income inequality, inclusion of mediating variables as controls, and timing of effects (Subramanian and Kawachi, 2004; Wilkinson and Pickett, 2006; Zheng, 2012). Timing concerns the lags between income inequality and health outcomes. Emerging studies have estimated the lagged effect of income inequality on health. Some test the aggregate association between income inequality and the population mortality rate, while others examine the relationship between income inequality and individual health or mortality risk using multilevel designs. Among the aggregate-level studies, Kim and colleagues (2008) report significant 10-year lag effects, while other studies report either non-significant or mixed results (e.g., Leigh and Jencks, 2007; Mellor and Milyo, 2003; Shi et al., 2003, 2004). Multilevel studies have reported a lag effect up to 6 years (Dahl et al., 2006), 8 years (Lochner et al., 2001), 12 years (Zheng, 2012), and 15 years (Blakely et al., 2000; Subramanian and Kawachi, 2004), while other studies do not find such long-term effects (e.g., Blakely et al., 2003; Osler et al., 2003). One study also links early life income inequality exposure to adult health (Lillard et al., 2015), which, however, has not been corroborated in other studies. Research has yet to investigate whether income inequality experienced in childhood may contribute to health decline across cohorts in the United States.
It is reasonable to assume that early life income inequality exposure may have long-term health consequences. The fetal origins hypothesis, proposed by Barker and his colleagues (1990), holds that the risk of developing coronary heart disease in adulthood may originate from in utero biological programing associated with maternal and fetal undernutrition. Many later studies further develop the fetal origins hypothesis into a broader developmental origins of health and disease theory. This theory posits that adult health, disease, morbidity, and mortality originate in part from environmental exposures in early life (e.g., postnatal infection, early life health status, mother’s education, parental income, childhood poverty) (Ben-Shlomo and Kuh, 2002; Elo and Preston, 1992; Hayward and Gorman, 2004; Lynch and Davey Smith, 2005). It usually takes years before exposures to risk factors are observed to predict chronic illness, e.g., cardiovascular diseases, cancer, stroke, diabetes (Yusuf et al., 2001). Chronic conditions have long latency periods, accounting for the lags between the accumulation of risk factors and the onset of diseases and subsequent morbidity and mortality (Lynch and Davey Smith, 2005). The conjecture of long-lasting health consequences of early life income inequality exposure is consistent with the developmental origins of health and disease theory.
Built on this developmental theory and prior studies on the lagged effect of income inequality on health, we use a cohort perspective to investigate whether income inequality experienced during childhood may have long-lasting consequences for adult health, how this may shape the cohort trend in health, and whether this consequence may vary by demographic groups (gender and race). Therefore, our study not only contributes to the evidence regarding the lagged impact of income inequality on health, but also sheds light on the underlying mechanisms shaping the health decline across U.S. cohorts.
Methods
Data
We use two large nationally representative datasets: NHANES 1988–2018 and PSID 1968–2013. NHANES is a pooled cross-sectional dataset, each wave of which collects different samples. Nonetheless, we can create synthetic cohorts and obtain cohort trends in health. NHANES data were collected from household interviews as well as physical examinations and laboratory tests performed in a mobile examination center. We combined NHANES III data, collected between 1988 and 1994, with the data collected in ten continuous waves from 1999 to 2018. Detailed descriptions of the survey designs, procedures, and methodologies are available on the NCHS website. We constrained the sample to those born in 1925–1999 to exclude very old and very young cohorts with small sample sizes. Of the 44,804 respondents born in this period and with valid PD information, we excluded respondents with missing data on education (n=535), marital status (n=1,478), poverty income ratio (n=1,656), those in “other” racial groups (n=3,248), or any without valid sampling weight (n=2,378), reaching a sample size of 35,509 individuals aged 17 years and older.
PSID is multi-cohort longitudinal dataset, which tracks individuals over time and yields a life course history of real cohorts. This survey began in 1968 with a nationally representative sample of families. The survey was administered annually until 1997 and biennially thereafter. We use information from the Family and Individual Files 1968–2013. Children from the original 1968 families were added to the Family Files after they became heads of households or the spouses of one. Our analysis period consists of the 1999 to 2013 waves when the health outcome (chronic disease index (CDI)) is measured, with information on early life conditions (early life diseases, mother’s education, parental smoking) obtained from prior waves. We restricted our sample to heads of households and spouses born in 1925–1995 with valid information on CDI, which includes 17,010 individuals with 88,249 observations. After excluding respondents with missing data on age, race, and gender (n=479), early life factors (early life disease index, parental smoking before age 17, and mother’s education, n=3,449), and adulthood factors (education, income, and marital status, n=158), we reached a sample size of 12,924 individuals and 68,271 observations.
Both datasets have advantages and disadvantages. NHANES data are relatively large so we can break down analysis by race and gender and examine whether childhood income inequality may explain cohort health decline for all demographic subgroups. But NHANES data do not have measures of childhood health and family background. That is why we use PSID data to test the robustness of findings produced from the NHANES data by taking into account the possible correlation between childhood income inequality and childhood health and family background. By adding these controls, however, we risk over-controlling for the full association between childhood income inequality and adult health if these controls are actually mediators. The disadvantage of the PSID data is that it has a relatively smaller sample size so we cannot disaggregate the analysis by race and gender. We provide results from both datasets and examine consistency across different measures and research designs.
Income inequality is measured by the Gini Index computed using Internal Revenue Service (IRS) data by Frank (2014). There are advantages and disadvantages to using IRS data compared to Census or Current Population Survey (CPS) data to compute inequality indexes (Atkinson et al., 2011). IRS data are better at capturing higher income brackets and income from capital gains, while CPS data are better at capturing lower income brackets (Frank 2009). The Frank (2014) data utilizes pre-tax income based on individual income tax returns and includes capital gains in addition to wages and salaries. A benefit of these data is they provide consistent measurements of inequality dating back to 1917. We use this historical data from 1925 to 2016 to construct a measure of childhood inequality. This measure is based on the average Gini Index at the national level for individuals when they were between 0 to 18 years old. For example, someone born in 1925 would have their childhood Gini Index consist of the average of the Gini Index from 1925 to 1943. This allows us to construct childhood Gini Index scores for respondents based on their birth year. Childhood Gini Index is linked to NHANES and PSID data based on birth year. We construct the childhood Gini index at the national level for both theoretical and technical reasons. Theoretically, income inequality at the national level reflects the scale of social stratification or how hierarchical a society is (Wilkinson and Pickett, 2006), and is more consequential for individual health than income inequality measured in the local context (Kondo et al., 2011; Pickett and Wilkinson, 2015). Technically, individuals often move during childhood. It is infeasible to track local income inequality individuals may be exposed to because no such data exist.
We also collected several contemporary macro measures that were merged with NHANES (1988–2018) or PSID (1999–2013) based on survey year. Gini Index and percentage with a college degree were obtained from Frank (2014) data. GDP growth rate and unemployment rate were obtained from Federal Reserve Economic Data. Union coverage is measured as the percentage of employed workers in unions using data from Mayer (2004) and Hirsch and Macpherson (2003) that rely on the Handbook of Labor Statistics (Bureau of Labor Statistics) and Current Population Survey data.
Measures
Supplemental Information 1 and 2 display the descriptive statistics of measures from the NHANES data. Supplemental Information 3 displays the descriptive statistics of measures from PSID data. All the measures are at the individual level except childhood income inequality and contemporary period macro measures which are at the national level.
Outcome variables
Dependent variables are the biomarker measures of PD from NHANES data and CDI from PSID data. PD is operationalized as a count of high-risk physiological parameters across multiple systems, including markers of inflammation, metabolic functions, lung function, and renal function. It is based on nine markers of physiological functions listed in Supplemental Information 1, including seven markers of metabolic functions, one marker of chronic inflammation (i.e., low serum albumin), and one additional marker (i.e., urinary function-creatinine clearance). The cutoff points for high-risk levels of these markers are based on previous studies (Crimmins et al., 2003; Yang and Kozloski, 2011). PD is the summary index of positive indicators of all nine markers and indicates the number of biomarkers at high risk. It ranges from 0 to 9. We did not include additional markers of inflammation (e.g., fibrinogen, C-reactive protein) and metabolic function (e.g., fasting glucose) in this measure because these markers were not collected in more recent surveys. Specifically, fibrinogen was not collected after 2001–2002, C-reactive protein was not collected after 2009–2010, and fasting glucose was not collected for 2017–2018. We also created an alternative measure of PD based on the proportion of positive indicators among all the available markers and the overall cohort pattern was similar. The CDI consists of 10 health problems: stroke, diabetes, chronic lung disease, high blood pressure, cancer, heart attack, heart disease, emotional problems, arthritis, and asthma. A respondent’s disease index score consists of the sum of all conditions he or she reported, and it ranges from 0 to 10. CDI is time varying as it comes from longitudinal PSID data.
Explanatory variables
The main explanatory variables are cohort and childhood income inequality. We categorize all single birth-year cohorts into eight historical groups: Early Children of Depression (born 1925–30), Late Children of Depression (born 1931–42), War Babies (born 1943–45), Early-Baby Boomers (born 1946–55), Late-Baby Boomers (born 1956–64), Early-Generation X (born 1965–72), Late-Generation X (born 1973–80), and Generation Y (born 1981–99). This categorization of birth cohorts is well established in the literature (e.g., O’Rand and Hamil-Luker, 2020; Zang et al., 2019) and data collection (e.g., Health and Retirement Study). We also group them by 10-year birth cohorts (1925–1934, 1935–1944, ……, 1985–1999) and overall findings are very similar. As explained in the Data section, the childhood Gini Index was obtained by computing the average of the Gini index at the national level for respondents between the ages of 0 to 18. Gini coefficient ranges in value from 0 to 1, with higher values indicating higher levels of income inequality. Figure 1 displays the trend in childhood Gini index for cohorts born from 1925 to 1999.
Control variables
Covariates include age, age squared, gender, race, survey year, educational attainment, marital status, family poverty income ratio (NHANES) or family income-to-needs ratio (PSID), and contemporary period macro socioeconomic measures. Age and survey year are controlled to obtain the net trend of cohort. The individual level socioeconomic and demographic statuses and period macro socioeconomic characteristics are controlled to account for possible confounding factors that may contribute to the cohort trend in health. Age is grand mean centered. Race consists of three groups: non-Hispanic White (White hereafter), non-Hispanic Black (Black hereafter), and Hispanic. Educational attainment is categorized as less than high school (reference), high school diploma, and college educated or higher. Marital status is categorized as married or cohabitating (reference), divorced or separated, widowed, and never married. Poverty income ratio is the ratio of total household income to a year-specific federal poverty threshold. It is categorized into three groups: below poverty line (less than 1) as a reference, middle (1–2.99), and high (3 or more). Family income-to-needs ratio is a continuous variable and measured as a respondent’s family income divided by the U.S. Census Bureau’s defined needs of the family (PSID, 2013). Contemporary period macro measures include the Gini Index, GDP growth rate, unemployment rate, percentage of union workers, and percentage with a college education. The Gini Index ranges from 0 to 1 with higher values indicating greater income inequality. The unit of the other four period macro measures is percentage. GDP growth rate represents the percentage increase in real annual GDP between two adjacent years with negative percentages indicating negative growth. Unemployment rate represents the percentage of people in the labor force who are unemployed. Union coverage is measured as the percentage of employed workers in unions. Percentage of college education is the percentage of the population with a college degree.
Additional control variables in PSID
Additional early-life factors from the PSID data include early life disease index, parental smoking before age 17, and mother’s education. The early-life disease index consists of the number of 12 health problems a respondent reported before age 17, and scores for this index range from 0 to 12. These health problems are asthma, diabetes, respiratory disease, allergies, heart trouble, epilepsy, severe headaches/migraines, stomach issues, high blood pressure, depression, drug/alcohol abuse, and emotional/psychiatric problems. Parental smoking before age 17 is a dummy variable with 1 indicating that at least one parent/guardian smoked when the respondent was 0 to 17 years old. Mother’s education consists of five categories: 1 (did not graduate from high school), 2 (high school graduate), 3 (some college), 4 (college graduate), and 5 (graduate degree). It is possible that these early life factors are mediators rather than confounders in the relationships between childhood income inequality and adult health. Thus, we may be at risk of over-controlling by including them in the model (Pickett and Wilkinson, 2015).
Statistical procedures
Because the dependent variables (i.e., PD, CDI) are count variables, we estimated Poisson mixed effects models to obtain the net effects of birth cohort after controlling for age, period, and basic sociodemographic characteristics (Yang and Land, 2006). Specifically, these models estimated the fixed effects of age and sociodemographic variables and random effects of cohort and period. Supplemental Information 4 provides a detailed explanation of model specification. Poisson regression models the log of the expected count as a function of the predictor variables, so the regression coefficient can be interpreted as follows: for a one unit change in the predictor variable, the expected count of the dependent variable will change by [exp(regression coefficient)−1]*100 percent. Model1 only includes cohort, period, and age. Model2 additionally adjusts for childhood income inequality. Sociodemographic characteristics such as educational attainment, marital status, and poverty income ratio (NHANES) or income-to-needs ratio (PSID) are added in the Model3. Period macro factors are added in Model4. Analysis based on PSID data additionally accounts for early life factors before adding adult characteristics and period factors. We accounted for both surveys’ complex designs by adjusting for sampling weights. All statistical analyses were performed using SAS PROC GLIMMIX. Analyses based on NHANES data were conducted for the whole sample and separately for six gender-race-ethnicity groups: White males, White females, Black males, Black females, Hispanic males, and Hispanic females. PSID data were conducted for the whole sample due to the sample size concern.
Results
Table 1 shows the results from Poisson mixed effect models of PD based on the NHANES data. Model 1 controls for age, age squared, birth cohort and survey year. Cohort random effect coefficients indicate an increasing risk of PD from Early Baby Boomers to Generation Y. Variance components indicate a strong cohort pattern of PD. Model 2 adds the childhood Gini index, which has a significant positive association with PD. Each 0.01 unit increase in childhood Gini index is associated with a 3% (= [exp(2.989*0.01)−1]*100) increase in the level of PD. More importantly, childhood Gini index explains a substantial amount of variation in PD across cohorts. After controlling for childhood Gini index, birth cohort variance substantially reduces from 0.025 to 0.001. Additional analyses by gender and racial groups presented in Supplemental Information 5–10 show that the impact of childhood Gini index on PD is especially large among White males and Black females. Each 0.01 unit increase in childhood Gini index is associated with 3.7% and 3.2% increase in the level of PD among White males and Black females, respectively, while it is associated with 2.6% increase among White females and Hispanic females, 2.4% increase among Black males, and 2.2% increase among Hispanic males.
Table 1.
Fixed and Random Effect Estimates from Poisson Mixed Models of Physiological Dysregulation, NHANES, 1988–2018
| Model1 | Model2 | Model3 | Model4 | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Coef. | S.E | Coef. | S.E | Coef. | S.E | Coef. | S.E | |
|
| ||||||||
| Fixed effects | ||||||||
| Intercept | 0.765** | 0.059 | 0.774** | 0.018 | 0.998** | 0.015 | 0.142 | 0.100 |
| Age | 0.028** | 0.000 | 0.028** | 0.000 | 0.028** | 0.000 | 0.027** | 0.000 |
| Age squared | 0.000** | 0.000 | 0.000** | 0.000 | 0.000** | 0.000 | 0.000** | 0.000 |
| Female | 0.040** | 0.000 | 0.040** | 0.000 | 0.035** | 0.000 | 0.035** | 0.000 |
| Race (ref: Whites) | ||||||||
| Blacks | 0.118** | 0.000 | 0.118** | 0.000 | 0.073** | 0.000 | 0.073** | 0.000 |
| Hispanics | 0.149** | 0.000 | 0.149** | 0.000 | 0.067** | 0.000 | 0.068** | 0.000 |
| Gini index [0–18] | 2.989** | 0.219 | 3.028** | 0.175 | 2.467** | 0.167 | ||
| Education (ref: Less than high school) | ||||||||
| High school diploma | 0.003** | 0.000 | 0.003** | 0.000 | ||||
| More than high school | −0.127** | 0.000 | −0.129** | 0.000 | ||||
| Marital status (ref: Married) | ||||||||
| Widowed | −0.011** | 0.000 | −0.008** | 0.000 | ||||
| Divorced/Separated | −0.071** | 0.000 | −0.070** | 0.000 | ||||
| Never married | −0.046** | 0.000 | −0.044** | 0.000 | ||||
| Poverty income ratio (ref: Low (<1)) | ||||||||
| Middle (≥1, <3) | −0.067** | 0.000 | −0.066** | 0.000 | ||||
| High (≥3) | −0.175** | 0.000 | −0.173** | 0.000 | ||||
| Period macro measures | ||||||||
| Gini index | 0.721** | 0.123 | ||||||
| Percent of college | 0.012** | 0.002 | ||||||
| Percent of union | 0.040** | 0.003 | ||||||
| GDP growth rate | −0.026** | 0.001 | ||||||
| Unemployment rate | −0.040** | 0.001 | ||||||
| Random Effects | ||||||||
| Birth cohorts | ||||||||
| Early children of depression (1925–1930) | −0.107 | 0.056 | −0.043** | 0.012 | −0.063** | 0.009 | −0.047** | 0.010 |
| Late children of depression (1931–1942) | −0.092 | 0.056 | 0.045** | 0.015 | 0.035** | 0.012 | 0.027* | 0.012 |
| War babies (1943–1945) | −0.149** | 0.056 | −0.017 | 0.014 | −0.013 | 0.011 | −0.029* | 0.012 |
| Early-baby Boomers (1946–1955) | −0.108 | 0.056 | −0.011 | 0.013 | 0.006 | 0.010 | −0.014 | 0.011 |
| Late-baby Boomers (1956–1964) | −0.060 | 0.056 | −0.015 | 0.011 | −0.010 | 0.009 | −0.034** | 0.010 |
| Early-gen Xers (1965–1972) | 0.051 | 0.056 | 0.030 | 0.011 | 0.034** | 0.009 | 0.010 | 0.009 |
| Late-gen Xers (1973–1980) | 0.173** | 0.056 | 0.029** | 0.015 | 0.030* | 0.012 | 0.017 | 0.012 |
| Gen Yers (1981–1999) | 0.292** | 0.056 | −0.018 | 0.025 | −0.019 | 0.020 | −0.016 | 0.019 |
| Survey years | ||||||||
| Wave3 (1988–1994) | 0.081** | 0.018 | 0.081** | 0.015 | 0.059** | 0.012 | 0.012** | 0.003 |
| 1999–2000 | 0.010 | 0.018 | 0.010 | 0.015 | 0.002 | 0.012 | −0.042** | 0.002 |
| 2001–2002 | 0.015 | 0.018 | 0.015 | 0.015 | 0.018 | 0.012 | −0.012** | 0.002 |
| 2003–2004 | 0.017 | 0.018 | 0.017 | 0.015 | 0.012 | 0.012 | 0.036** | 0.002 |
| 2005–2006 | 0.021 | 0.018 | 0.021 | 0.015 | 0.026* | 0.012 | 0.009** | 0.002 |
| 2007–2008 | 0.053** | 0.018 | 0.052** | 0.015 | 0.053** | 0.012 | 0.022** | 0.002 |
| 2009–2010 | −0.070** | 0.018 | −0.070** | 0.015 | −0.067** | 0.012 | 0.022** | 0.002 |
| 2011–2012 | −0.078** | 0.018 | −0.078** | 0.015 | −0.075** | 0.012 | 0.016** | 0.002 |
| 2013–2014 | −0.066** | 0.018 | −0.066** | 0.015 | −0.063** | 0.012 | −0.045** | 0.002 |
| 2015–2016 | −0.063** | 0.018 | −0.063** | 0.015 | −0.055** | 0.012 | −0.069** | 0.002 |
| 2017–2018 | 0.080** | 0.018 | 0.080** | 0.015 | 0.090** | 0.012 | 0.050** | 0.002 |
| Variance components | ||||||||
| Birth cohorts | 0.025* | 0.013 | 0.001* | 0.000 | 0.001** | 0.000 | 0.001* | 0.000 |
| Survey years | 0.004* | 0.002 | 0.002** | 0.001 | 0.002** | 0.000 | 0.000 | 0.000 |
|
| ||||||||
| Pseudo-BIC | 290,040,000 | 290,040,000 | 285,620,000 | 285,620,000 | ||||
| Sample size | 35,509 | 35,509 | 35,509 | 35,509 | ||||
Notes:
<0.05
<0.01
Abbreviations: Coef., regression coefficients or variance estimates for random effect; S.E, standard error.
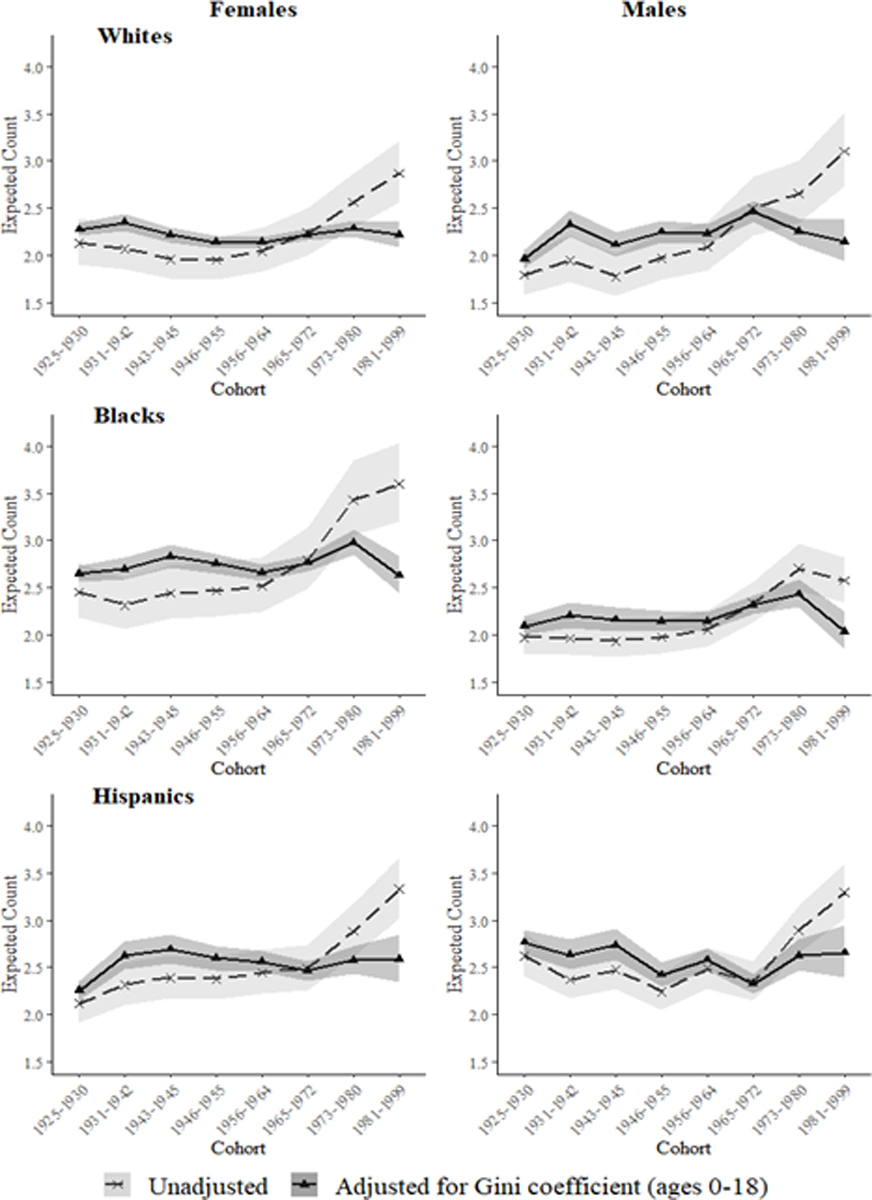
Figure 2 displays the cohort trend in PD for each group based on the random effect coefficients of cohort in Model 1 and Model 2 of Supplemental Information 5–10. Predicted levels of PD for each cohort were calculated and plotted for the six groups, holding age at mean value. A general pattern is that PD has substantially increased across cohorts since Baby Boomers even though the exact timing and slope of increase vary across groups. For example, PD increased since Early Baby Boomers (born 1946–1955) for White males, one historical cohort earlier than for White females. White males also experience the steepest increase in PD among males, while Black females observe a steeper increase than the other two female groups. White males and Black females happen to be most impacted by childhood income inequality exposure. After controlling for childhood Gini index, the cohort trend in PD becomes much flatter for each gender and racial group. This visually displays the substantial reduction in birth cohort variance component from Model 1 to Model 2 in these supplemental tables.
Figure 2. Trend in number of physiological dysregulation biomarkers at high risk across birth cohorts with/without adjusting for childhood Gini coefficient (ages 0–18).
Model 3 and Model 4 of Table 1 additionally control for individual level socioeconomic statuses (educational attainment, marital status, and poverty income ratio), and five period macro socioeconomic factors (Gini index, GDP growth rate, unemployment rate, percentage of union, and percentage of college education) to ensure the patterns observed in Model 2 are not due to individual adulthood factors and contemporary period determinants. These factors, however, generally do not explain the cohort trend in PD as shown in little change in birth cohort variance components once they are controlled. More importantly, after including these variables in the models, the association between childhood Gini index and PD remains strong and significant.
Table 2 shows the results on CDI based on PSID data. Variance components suggest CDI clearly follows a cohort pattern. Model 2 controls for childhood Gini index. Each 0.01 unit increase in childhood Gini index is associated with 7% (= [exp(6.769*0.01)−1]*100) increase in the level of CDI. After controlling for childhood Gini index, birth cohort variance substantially reduces from 0.134 to 0.024. Model 3 additionally adjusts for early childhood factors, including early life disease index, parental smoking status before age 17, and mother’s education, which slightly decrease the coefficient estimates of childhood Gini index and birth cohort variance. Further analysis finds that the reduction in birth cohort variance is completely due to early life disease index. In fact, it is offset by parental smoking status before age 17 and mother’s education because early life disease index worsens across cohorts while the latter two improve across cohorts. Model 4 and Model 5 add individual adulthood factors and macro contemporary period determinants, which explain neither the association between childhood Gini index and CDI nor the cohort trend of CDI (cohort variance component becomes bigger). These findings corroborate those based on NHANES data.
Table 2.
Fixed and Random Effect Estimates from Poisson Mixed Models of Adult Chronic Disease Index, PSID, 1999–2013
| Model1 | Model2 | Model3 | Model4 | Model5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Coef. | S.E | Coef. | S.E | Coef. | S.E | Coef. | S.E | Coef. | S.E | |
|
| ||||||||||
| Fixed effects | ||||||||||
| Intercept | −0.564** | 0.131 | −3.811** | 0.566 | −3.829** | 0.511 | −3.260** | 0.554 | 2.406 | 2.687 |
| Age | 0.056** | 0.000 | 0.056** | 0.000 | 0.058** | 0.000 | 0.062** | 0.000 | 0.062** | 0.000 |
| Age squared | 0.000** | 0.000 | 0.000** | 0.000 | 0.000** | 0.000 | 0.000** | 0.000 | 0.000** | 0.000 |
| Female | 0.129** | 0.002 | 0.129** | 0.002 | 0.087** | 0.002 | 0.037** | 0.002 | 0.037** | 0.002 |
| Blacks | 0.279** | 0.002 | 0.279** | 0.002 | 0.282** | 0.002 | 0.184** | 0.002 | 0.184** | 0.002 |
| Hispanics | −0.056** | 0.004 | −0.056** | 0.004 | −0.060** | 0.004 | −0.115** | 0.004 | −0.115** | 0.004 |
| Gini index [0–18] | 6.769** | 1.173 | 6.508** | 1.059 | 6.712** | 1.147 | 6.702** | 1.146 | ||
| Disease index before 17 | 0.291** | 0.001 | 0.281** | 0.001 | 0.281** | 0.001 | ||||
| Parental smoking before 17 | 0.158** | 0.002 | 0.135** | 0.002 | 0.135** | 0.002 | ||||
| Mother’s education (ref: less than high school) | ||||||||||
| High school graduate | −0.144** | 0.002 | −0.094** | 0.002 | −0.094** | 0.002 | ||||
| Some college | −0.183** | 0.003 | −0.092** | 0.003 | −0.092** | 0.003 | ||||
| College graduate | −0.184** | 0.003 | −0.068** | 0.003 | −0.068** | 0.003 | ||||
| Graduate degree | −0.176** | 0.005 | −0.023** | 0.005 | −0.023** | 0.005 | ||||
| Highest grade attained | −0.036** | 0.000 | −0.036** | 0.000 | ||||||
| Family income to needs ratio | −0.019** | 0.000 | −0.019** | 0.000 | ||||||
| Marital/cohabitating status | −0.121** | 0.002 | −0.121** | 0.002 | ||||||
| Period macro measures | ||||||||||
| Gini index | 0.144 | 1.924 | ||||||||
| Percent of college | −0.133 | 0.069 | ||||||||
| Percent of union | −0.268* | 0.114 | ||||||||
| GDP growth rate | 0.001 | 0.017 | ||||||||
| Unemployment rate | 0.020 | 0.025 | ||||||||
| Random Effects | ||||||||||
| Birth cohorts | ||||||||||
| Early children of depression (1925–1930) | −0.446** | 0.130 | −0.314** | 0.059 | −0.284** | 0.054 | −0.307** | 0.058 | −0.307** | 0.058 |
| Late children of depression (1931–1942) | −0.310* | 0.129 | −0.001 | 0.076 | −0.017 | 0.069 | −0.021 | 0.074 | −0.021 | 0.074 |
| War babies (1943–1945) | −0.158 | 0.129 | 0.134 | 0.074 | 0.124 | 0.067 | 0.122 | 0.073 | 0.122 | 0.072 |
| Early-baby Boomers (1946–1955) | −0.082 | 0.129 | 0.132* | 0.066 | 0.124* | 0.059 | 0.141* | 0.064 | 0.141* | 0.064 |
| Late-baby Boomers (1956–1964) | −0.118 | 0.129 | −0.019 | 0.057 | −0.002 | 0.051 | −0.001 | 0.056 | −0.001 | 0.056 |
| Early-gen Xers (1965–1972) | 0.046 | 0.129 | −0.007 | 0.055 | −0.002 | 0.050 | 0.005 | 0.054 | 0.005 | 0.054 |
| Late-gen Xers (1973–1980) | 0.436** | 0.130 | 0.083 | 0.082 | 0.059 | 0.074 | 0.072 | 0.080 | 0.072 | 0.080 |
| Gen Yers (1981–1995) | 0.633** | 0.130 | −0.008 | 0.123 | −0.002 | 0.111 | −0.011 | 0.121 | −0.011 | 0.120 |
| Survey years | ||||||||||
| 1999 | −0.111** | 0.021 | −0.111** | 0.021 | −0.104** | 0.020 | −0.103** | 0.020 | 0.006 | 0.044 |
| 2001 | −0.059 | 0.020 | −0.059** | 0.020 | −0.055** | 0.020 | −0.053** | 0.020 | −0.040 | 0.033 |
| 2003 | 0.019 | 0.020 | 0.019 | 0.020 | 0.025 | 0.020 | 0.025 | 0.020 | 0.023 | 0.038 |
| 2005 | 0.059** | 0.020 | 0.059** | 0.020 | 0.062** | 0.020 | 0.063** | 0.020 | 0.018 | 0.031 |
| 2007 | 0.050* | 0.020 | 0.050* | 0.020 | 0.051** | 0.020 | 0.051** | 0.020 | 0.003 | 0.038 |
| 2009 | 0.023 | 0.020 | 0.023 | 0.020 | 0.020 | 0.020 | 0.022 | 0.020 | 0.026 | 0.040 |
| 2011 | 0.009 | 0.020 | 0.009 | 0.020 | 0.002 | 0.020 | −0.001 | 0.020 | −0.027 | 0.039 |
| 2013 | 0.010 | 0.020 | 0.010 | 0.020 | −0.002 | 0.020 | −0.003 | 0.020 | −0.008 | 0.043 |
| Variance components | ||||||||||
| Birth cohorts | 0.134* | 0.072 | 0.024* | 0.014 | 0.019* | 0.011 | 0.023* | 0.013 | 0.022* | 0.013 |
| Survey years | 0.003* | 0.002 | 0.003* | 0.002 | 0.003* | 0.002 | 0.003* | 0.002 | 0.002 | 0.002 |
|
| ||||||||||
| Pseudo-BIC | 2,205,878 | 2,205,889 | 1,990,867 | 1,930,704 | 1,930,770 | |||||
| Sample size | 12,924 | 12,924 | 12,924 | 12,924 | 12,924 | |||||
| Observations | 68,271 | 68,271 | 68,271 | 68,271 | 68,271 | |||||
Notes:
<0.05
<0.01
Abbreviations: Coef., regression coefficients or variance estimates for random effect; S.E, standard error.
Auxiliary analyses
Table 1 and Table 2 clearly show that childhood income inequality has long-term health consequences, and helps explain the cohort trend in deteriorating PD and CDI. The findings are also robust to control of early life disease and family socioeconomic and health behavioral factors, adulthood sociodemographic factors, and contemporary period determinants. These findings are also not influenced by different categorizations of birth cohorts as shown in Supplemental Information 11 and 12. But are these patterns unique to income inequality people experience in childhood? In order to answer this question, we replace childhood Gini index with the other four childhood exposures (childhood percentage of union workers, childhood GDP growth rate, childhood unemployment rate, and childhood percentage with a college education). These four childhood exposures are constructed in the same way as childhood Gini index, that is as the average of these exposures between the ages of 0 and 18 for each cohort. Supplemental Information 13 displays the cohort trends in these four indicators, which show a similar negative trend except childhood percentage with a college education.
Table 3 shows the percentage change in birth cohort variance component across models for each early life exposure measure by race and gender from NHANES data 1988–2018. It consists of 96 models (4 models for each demographic group and early-life factor × 6 demographic groups × 4 early-life factors). The detailed results for childhood Gini index are presented in Supplemental Information 5–10, while those for childhood percentage of union workers, childhood GDP growth rate and childhood unemployment rate are available in Supplemental Information 14, 15 and 16. The results for childhood percentage of college education are not presented because either the model could not converge or it had a positive association with PD, which basically just picks up the cohort trend. The “% change” column shows the percentage change in birth cohort variance component from Model 1 to subsequent models. The setup of Model 1 to Model 4 is the same as that in Table 1. The “coef” column shows the coefficient estimate of each early life exposure factor in Model 2, Model 3, and Model 4.
Table 3.
Comparison of the Percentage Change in Birth Cohort Variance Components from Model1 to Model4 by Each Early Life Exposure Measure, NHANES, 1988–2018
| Gini Index [0–18] | Percentage of Union [0–18] | GDP Growth Rate [0–18] | Unemployment Rate [0–18] | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Models | % change | coef. | % change | coef. | % change | coef. | % change | coef. |
|
| ||||||||
| White Females | ||||||||
| Model 1-Model 2 | 94.39% | 2.573** | 75.10% | −0.018** | 53.79% | −0.064 | 14.52% | 0.002 |
| Model 1-Model 3 | 97.36% | 2.974** | 42.83% | −0.018* | 52.12% | −0.096* | 5.50% | −0.007 |
| Model 1-Model 4 | N.C. | . | 50.97% | −0.018* | 34.88% | −0.096 | N.C. | . |
|
| ||||||||
| White Males | ||||||||
| Model 1-Model 2 | 87.29% | 3.681** | −21.46% | −0.019 | −8.63% | −0.123 | −43.14% | −0.017 |
| Model 1-Model 3 | 58.32% | 3.814** | −7.30% | −0.019 | −3.09% | −0.134 | 12.21% | −0.020 |
| Model 1-Model 4 | N.C. | . | −61.81% | −0.019 | 22.33% | −0.134* | N.C. | |
|
| ||||||||
| Black Females | ||||||||
| Model 1-Model 2 | 92.62% | 3.128** | 38.54% | −0.018* | 30.02% | −0.119* | −14.83% | −0.009 |
| Model 1-Model 3 | 93.26% | 2.770** | 50.43% | −0.016* | 47.62% | −0.107* | 11.07% | −0.008 |
| Model 1-Model 4 | 93.26% | 2.771** | 50.28% | −0.016* | 46.84% | −0.107* | 9.62% | −0.008 |
|
| ||||||||
| Black Males | ||||||||
| Model 1-Model 2 | 78.75% | 2.351** | 26.88% | −0.014* | 23.57% | −0.089 | −19.70% | −0.006 |
| Model 1-Model 3 | 79.18% | 2.464** | 19.25% | −0.014 | 19.98% | −0.094 | −23.12% | −0.007 |
| Model 1-Model 4 | 79.53% | 2.465** | 22.05% | −0.014 | 22.39% | −0.094 | −18.35% | −0.007 |
|
| ||||||||
| Hispanic Females | ||||||||
| Model 1-Model 2 | 81.89% | 2.522** | 9.85% | −0.011 | 26.12% | −0.095 | −0.87% | −0.021 |
| Model 1-Model 3 | 83.43% | 2.362** | 19.23% | −0.010 | 29.74% | −0.086 | 15.00% | −0.020 |
| Model 1-Model 4 | 83.45% | 2.362** | 18.67% | −0.010 | 29.74% | −0.086 | 12.09% | −0.020 |
|
| ||||||||
| Hispanic Males | ||||||||
| Model 1-Model 2 | 74.65% | 2.161** | 60.73% | −0.017** | −0.06% | −0.053 | −12.38% | 0.005 |
| Model 1-Model 3 | 72.45% | 1.995** | 67.47% | −0.016** | 9.07% | −0.046 | 1.19% | 0.006 |
| Model 1-Model 4 | 72.88% | 1.995** | 67.35% | −0.016** | 12.26% | −0.046 | −12.38% | 0.006 |
Notes:
<0.05
<0.01
Abbreviations: Coef., regression coefficient of each early life exposure measure; % change, percentage change in birth cohort variance component from Model1 to each model; N.C, not converged
Model1: includes age, cohort, period.
Model2: additionally adjusts for each early life exposure measure.
Model3: additionally adjusts for educational attainment, marital status, and poverty income ratio.
Model4: additionally adjusts for five period macro measures including Gini index, GDP growth rate, unemployment rate, percentage of union, and percentage of college education.
For example, according to Model 2 among White females, each 0.01 unit increase in childhood Gini index is associated with 2.6% (= [exp(2.573*0.01)−1]*100) increase in the level of PD; each 1 percentage point increase in childhood union coverage is associated with 1.8% (= [exp(−0.018)−1]*100) decrease in the level of PD; each 1 percentage point increase in childhood GDP growth rate is associated with 6% (= [exp(−0.064) −1]*100) decrease in the level of PD; and each 1 percentage point increase in childhood unemployment rate is associated with 0.2% (= [exp(0.002)−1]*100) increase in the level of PD. The “% change” column from Model 1 to Model 2 shows that childhood Gini index explains over 70% of variation in PD across cohorts, while the contributions of the other three early life factors to the cohort variation in PD are substantially smaller. Supplemental Information 17–19 visually display that accounting for these three early life factors does not change the cohort trend as much as childhood Gini (Figure 2). Additional controls of individual adulthood factors (Model 3) and contemporary period macro factors (Model 4) generally do not explain the birth cohort variance component.
Discussion and Conclusion
Around the turn of the century, Americans’ health began to decline. After decades of improvement in functioning and a decline in disability among the U.S. population ages 65 and older (Crimmins et al., 1997; Cutler, 2001; Freedman et al., 2004; Manton et al., 2006; Schoeni et al., 2001); starting in the late 1990s, however, newer cohorts approaching middle age (40–59) and early old age (60–69) began to experience increasing functional limitations and disability (Freedman et al., 2013; Fuller-Thomson et al., 2009; Martin et al., 2009, 2010; Seeman et al., 2010). In the early 2000s, the worsening disability trend was accompanied by increasing mortality rates among the middle-aged (Case and Deaton, 2015; Montez and Zajacova, 2013). A more alarming picture is that this elevated morbidity and mortality is not constrained to Baby Boomers who reached middle age and early old age in the past two decades but extends to younger cohorts (Zang et al., 2019; Zheng and Echave, 2021).
Against this backdrop, this study corroborates that Americans’ health has been continuously declining since the Early Baby Boomer cohort, no matter whether it is measured by physiological status based on a list of biomarkers or a disease index based on several chronic illnesses. It is consistently observed in two large nationally representative data sets. Scientific research is urgently needed to understand the cause of this health crisis. We find the cohort trend in physiological dysregulation very closely mirrors the cohort trend in early life income inequality exposure (Figure 1). By linking NHANES and PSID data to historical income inequality data, we find that early life income inequality exposure is significantly associated with poorer adulthood health, especially for White males and Black females (Table 1–2, Supplemental Information 5–10). But more importantly, we find early life income inequality exposure explains over 70% of cohort variation in PD and CDI. These findings are very robust to a wide range of controls, including early life health and family background, adulthood sociodemographic and economic factors, and contemporary macro socioeconomic determinants (e.g., contemporary income inequality). These findings are not simply due to a temporal correlation, as other similar negative temporal trends in early life exposures (i.e., childhood percentage of union membership, childhood GDP growth rate, and childhood unemployment rate) do not exhibit equivalent contributions to declining health across cohorts (Table 3, Supplemental Information 14–19).
Our study not only sheds light on the socioeconomic mechanisms that may shape the health decline in the United States, but also contributes to the substantial debate on the health consequences of income inequality. Our study suggests that income inequality experienced during childhood has a long-term impact on adult health, consistent with some prior studies (e.g., Lillard et al., 2015). Thus, childhood may be a sensitive period in which income inequality is strongly associated with poor health in adulthood. This is probably because children growing up in a period with rising income inequality may be particularly influenced by its negative socioeconomic and psychosocial consequences. Prior literature has demonstrated that income inequality can lead to decreasing public expenditures (e.g., public education and health care) (Gilens, 2012; Osberg et al., 2004), intensified relative deprivation (Kawachi and Kennedy, 1999; Kondo et al., 2008), and erosion of social capital (Kawachi et al., 1997; Wilkinson, 1992, 1996). These then reduce the socioeconomic, psychological, and healthcare resources families and children need to produce and protect health, the negative impact of which may contribute throughout the life course. The time lag between income inequality and health also may be due to both the time requirement from income inequality to the health pathways (Kondo et al., 2011) and the latency period between exposure to risk factors and diseases initiation, deterioration, and subsequent mortality (Lynch and Davey Smith, 2005).
Due to the nature of our research design, we are not able to infer causality in the link between income inequality and health from the econometrics standard. But temporality, an important criterion in the epidemiological causal framework (Pickett and Wilkinson, 2015), and robustness to control of a wide range of confounders do yield a certain degree of confidence about the validity of this link. Researchers who doubt that income inequality has an effect on health tend to argue that income inequality is a consequence of policies and social processes, therefore we should focus on the processes that generate income inequality rather than income inequality itself (Case and Deaton, 2020: 134). We, however, view income inequality as a meaningful antecedent of health in and of itself. Income inequality may be a proxy for broader institutional and systematic problems, but the health consequences of these processes and institutions work directly through inequality. Income inequality not only may have an impact on population health and mortality, but also may reinforce the processes that generate income inequality.
This study has several limitations. First, it only examines the contextual effect of income inequality at the national level. Several scholars have demonstrated that national income inequality and social hierarchies matter more to people than local social inequality structures (e.g., Kondo et al., 2011; Wilkinson and Pickett, 2006). Further research can investigate the long-term impact of childhood income inequality at the state level on adulthood morbidity and mortality risk, which, however, requires researchers to have complete data on respondents’ residential histories during their childhoods. Empirically, we think the findings will be similar as (1) we examine the association between cohort trend in childhood income inequality and cohort trend in adult health and (2) the overall temporal trend in income inequality is remarkably similar across states even though levels differ (Zheng and George, 2012). Second, even though we controlled a long list of possible confounders including childhood and adulthood socioeconomic and demographic factors and contemporary period determinants, other confounders may still influence both childhood income inequality and adult health.
There are several priority issues for future research. First, we rely on prior literature that has both conceptualized and empirically tested mechanisms linking income inequality to health (e.g., Davey, 1996; Delhey and Dragolov, 2014; Kaplan et al., 1996; Kawachi et al., 1997; Kawachi and Kennedy, 1999; Kondo et al., 2008; Pickett and Wilkinson, 2015; Zimmerman and Bell, 2006), and hypothesize that both material mechanisms (reductions in social spending) and psychosocial mechanisms (erosion of social capital and aggravation of relative deprivation) may have long-lasting consequences and contribute to the link between childhood income inequality exposure and adult health. Nonetheless, we are not able to test these and other potential mechanisms (e.g., reduced economic mobility and opportunities, increased geographic segregation, see Bor et al., 2017) due to both data limitations and the scope of this study. Future studies should directly test these and other potential mechanisms.
Second, results from the NHANES data indicate that the impact of childhood income inequality was especially strong for White males and Black females. These relationships are robust to controls for individual level childhood health and family background, adulthood socioeconomic and marital status, and contemporary macro socioeconomic factors. Given the broad array of variables controlled, it is difficult to understand why childhood income inequality was more important for White men and Black women than for the other four sex by race/ethnicity groups. These patterns are observed across cohorts, suggesting that the increased health risks experienced by White men and Black women reflect long-term, structural sources of vulnerability. Future research should both confirm these results in other data sets and examine possible explanations for them.
In conclusion, this study portrays a robust link between early life income inequality exposure and adult health and proposes a mechanism that may account for cohort differences in health. Although there are likely other contributing factors, our results suggest that the declining health across cohorts since the Early Baby Boomers may be partially due to increasing inequalities Americans face in early life. This may imply that reducing income inequality has a promising prospect of reversing this unfavorable trend and improving the health of current and future cohorts. Childhood income inequality exposure is linked to adult health probably through both material and psychosocial pathways. If these untested pathways are true, narrowing the income gap may require not only redistributive tax policies and a reduction in income differences before taxes from the top down (Pickett and Wilkinson, 2015) but also a strengthening of social cohesion and communities from the bottom up (Rajan, 2019).
Supplementary Material
Acknowledgements
Support for this project was provided by the Ohio State University Institute for Population Research through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development of the National Institutes of Health, P2CHD058484.
References:
- Atkinson AB, Piketty T, & Saez E (2011). Top Incomes in the Long Run of History. Journal of Economic Literature, 49, 3–71. [Google Scholar]
- Barbieri M (2019). The contribution of drug-related deaths to the US disadvantage in mortality. International Journal of Epidemiology, 48(3), 945–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJP (1990). The fetal and infant origins of adult disease. British Medical Journal, 301(6761), 1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels L (2008). Unequal Democracy: The Political Economy of the New Gilded Age. New York: Russell Sage Foundation. [Google Scholar]
- Ben-Shlomo Y, & Kuh D (2002). A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31(2), 285–293. [PubMed] [Google Scholar]
- Blakely TA, Atkinson J, & O’Dea D (2003). No Association of Income Inequality with Adult Mortality within New Zealand. Journal of Epidemiology and Community Health, 57(4), 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakely TA, Kennedy BP, Glass R, & Kawachi I (2000). What Is The Lag Time between Income Inequality and Health Status? Journal of Epidemiology and Community Health, 54(4), 318–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J, Cohen GH, & Galea S (2017). Population health in an era of rising income inequality: USA, 1980–2015. The Lancet, 389(10077), 1475–1490. [DOI] [PubMed] [Google Scholar]
- Bradley EH, & Taylor LA (2013). The American health care paradox: why spending more is getting us less. New York, NY: Public Affairs. [Google Scholar]
- Case A, & Deaton A (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences of the United States of America, 112(49), 15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, & Deaton A (2017). Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity, 2017, 397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, & Deaton A (2020). Deaths of despair and the future of capitalism. Princeton University Press. [Google Scholar]
- Crimmins EM, Johnston M, Hayward M, & Seeman T (2003). Age differences in allostatic load: An index of physiological dysregulation. Experimental Gerontology, 38(7), 731–734. [DOI] [PubMed] [Google Scholar]
- Crimmins E, Kim JK, & Vasunilashorn S (2010). Biodemography: New approaches to understanding trends and differences in population health and mortality. Demography, 47(SUPPL.1), S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y, & Reynolds SL (1997). Further evidence on recent trends in the prevalence and incidence of disability among older americans from two sources: The LSOA and the NHIS. Journals of Gerontology - Series B Psychological Sciences and Social Sciences, 52(2), S59–S71. [DOI] [PubMed] [Google Scholar]
- Cutler DM (2001). Declining disability among the elderly. Health Affairs, 20(6), 11–27. [DOI] [PubMed] [Google Scholar]
- Dahl E, Elstad JI, Hofoss D, & Martin-Mollard M (2006). For Whom is Income Inequality Most Harmful? A Multi-Level Analysis of Income Inequality and Mortality in Norway. Social Science and Medicine,63, 2562–2574. [DOI] [PubMed] [Google Scholar]
- Davey SG (1996). Income inequality and mortality: why are they related? British Medical Journal, 312, 987–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delhey J, & Dragolov G (2014). Why Inequality Makes Europeans Less Happy: The Role of Distrust, Status Anxiety, and Perceived Conflict. European Sociological Review, 30(2), 151–165. [Google Scholar]
- de Vries R, Gosling S, & Potter J (2011). Income inequality and personality: Are less equal U.S. states less agreeable? Social Science and Medicine, 72(12), 1978–1985. [DOI] [PubMed] [Google Scholar]
- DeWall CN, Deckman T, Pond RS, & Bonser I (2011). Belongingness as a Core Personality Trait: How Social Exclusion Influences Social Functioning and Personality Expression. Journal of Personality, 79(6), 1281–1314. [DOI] [PubMed] [Google Scholar]
- Elo IT, & Preston SH (1992). Effects of early-life conditions on adult mortality: a review. Population index, 58(2), 186–212. [PubMed] [Google Scholar]
- Frank M (2009). Inequality and Growth in the United States: Evidence from a New State-Level Panel of Income Inequality Measure. Economic Inquiry, 47(1), 55–68. [Google Scholar]
- Frank M (2014). A New State-Level Panel of Annual Income Inequality. Journal of Business Strategies, 31(1), 241–263. [Google Scholar]
- Freedman VA, Crimmins EM, Schoeni RF, Spillman BC, Aykan H, Kramarow E, et al. (2004). Resolving inconsistencies in trends in old-age disability: Report from a technical working group. Demography, 41(3), 417–441. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Spillman BC, Andreski PM, Cornman JC, Crimmins EM, Kramarow E, et al. (2013). Trends in late-life activity limitations in the United States: An update from five national surveys. Demography, 50(2), 661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Thomson E, Yu B, Nuru-Jeter A, Guralnik JM, & Minkler M (2009). Basic ADL disability and functional limitation rates among older americans from 2000–2005: The end of the decline? Journals of Gerontology - Series A Biological Sciences and Medical Sciences, 64(12), 1333–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilens M (2012). Affluence and influence: Economic inequality and political power in America. Princeton University Press. [Google Scholar]
- Gilens M, & Page BI (2014). Testing theories of American politics: Elites, interest groups, and average citizens. Perspectives on Politics, 12(3), 564–581. [Google Scholar]
- Hayward MD, & Gorman BK (2004). The long arm of childhood: The influence of early-life social conditions of men’s mortality. Demography, 41(1), 87–107. [DOI] [PubMed] [Google Scholar]
- Hirsch T & Macpherson DA (2003). Union Membership and Coverage Database from the Current Population Survey: Note. Industrial and Labor Relations Review, 56(2), 349–354. [Google Scholar]
- Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, & Balfour JL (1996). Inequality in Income and Mortality in the United States: Analysis of Mortality and Potential Pathways. British Medical Journal, 312(7037), 999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, & Kennedy BP (1999). Income Inequality and Health: Pathways and Mechanisms. Health Services Research, 34, 215–227. [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP, Lochner K, & Prothrow-Stith D (1997). Social Capital, Income Inequality, and Mortality. American Journal of Public Health, 87(9), 1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Kawachi I, Hoorn SV, & Ezzati M (2008). Is Inequality at the Heart of It? Cross-Country Associations of Income Inequality with Cardiovascular Diseases and Risk Factors. Social Science and Medicine,66, 1719–32. [DOI] [PubMed] [Google Scholar]
- Kondo N, Kawachi I, Subramanian SV, Takeda Y, & Yamagata Z (2008). Do social comparisons explain the association between income inequality and health?: Relative deprivation and perceived health among male and female Japanese individuals. Social Science and Medicine, 67(6), 982–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, & Yamagata Z (2009). Income Inequality, Mortality, and Self-Rated Health: Meta-Analysis of Multilevel Studies. British Medical Journal, 339, b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo N, van Dam RM, Sembajwe G, Subramanian SV, Kawachi I, & Yamagata Z (2011). Income Inequality and Health: The Role of Population Size, Inequality Threshold, Period Effects and Lag Effects. Journal of Epidemiology and Community Health, doi: 10.1136/jech-2011-200321. [DOI] [PubMed] [Google Scholar]
- Leigh A, & Jencks C (2007). Inequality and Mortality: Long-Run Evidence from A Panel of Countries. Journal of Health Economics, 26, 1–24. [DOI] [PubMed] [Google Scholar]
- Lillard DR, Burkhauser RV, Hahn MH, & Wilkins R (2015). Does early-life income inequality predict self-reported health in later life? Evidence from the United States. Social Science and Medicine, 128, 347–355. 10.1016/j.socscimed.2014.12.026 [DOI] [PubMed] [Google Scholar]
- Lochner K, Pamuk E, Makuc D, Kennedy BP, & Kawachi I (2001). State-Level Income Inequality and Individual Mortality Risk. American Journal of Public Health, 91(3), 385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch J, & Davey Smith G (2005). A Life Course Approach to Chronic Disease Epidemiology. Annual Review of Public Health, 26, 1–35. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu XL, & Lamb VL (2006). Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proceedings of the National Academy of Sciences of the United States of America, 103(48), 18374–18379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, Freedman VA, Schoeni RF, & Andreski PM (2009). Health and functioning among baby boomers approaching 60. Journals of Gerontology - Series B Psychological Sciences and Social Sciences, 64(3), 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, Freedman VA, Schoeni RF, & Andreski PM (2010). Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Affairs, 29(4), 725–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer G (2004). Union Membership Trends in the United States. Congressional Research Service Report for Congress. Received through the CRS Web. [Google Scholar]
- Mellor JM, & Milyo J (2003). Is Exposure to Income Inequality a Public Health Concern? Lagged Effects of Income Inequality on Individual and Population Health. Health Services Research, 38(1 Pt. 1), 137–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, & Zajacova A (2013). Trends in mortality risk by education level and cause of death among US White Women from 1986 to 2006. American Journal of Public Health, 103(3), 473–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2021). High and rising mortality rates among working-age adults. High and Rising Mortality Rates Among Working-Age Adults. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- O’Rand AM, & Hamil-Luker J (2020). Landfall After the Perfect Storm: Cohort Differences in the Relationship Between Debt and Risk of Heart Attack. Demography, 57(6), 2199–2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osler M, Christensen U, Due P, Lund R, Andersen I, Diderichsen F, & Prescott E (2003). Income Inequality and Ischaemic Heart Disease in Danish Men and Women. International Journal of Epidemiology, 32(3), 375–380. [DOI] [PubMed] [Google Scholar]
- Osberg L, Smeeding TM, & Schwabish J (2004). Income distribution and public social expenditure: Theories, effects, and evidence. Pp. 821–59 in Social Inequality, edited by Neckerman Kathryn. New York: Russell Sage Foundation. [Google Scholar]
- Paskov M, & Dewilde C (2012). Income inequality and solidarity in Europe. Research in Social Stratification and Mobility, 30(4), 415–432. [Google Scholar]
- Pickett KE, & Wilkinson RG (2015). Income inequality and health: A causal review. Social Science and Medicine, 128, 316–326. [DOI] [PubMed] [Google Scholar]
- Ponzetto GAM, & Troiano U (2018). Social Capital, Government Expenditures, and Growth. National Bureau of Economic Research Working Paper 24533. [Google Scholar]
- PSID Main Interview User Manual: Release 2013. Institute for Social Research, University of Michigan, July 2013. [Google Scholar]
- Rajan R (2019). The third pillar: How markets and the state leave the community behind. Penguin Press. [Google Scholar]
- Putnam RD, & Garrett SR (2020). The Upswing: How American Came Together a Century Ago and How We Can Do It Again. New York, NY: Simon & Schuster. [Google Scholar]
- Schoeni RF, Freedman VA, & Wallace RB (2001). Persistent, consistent, widespread, and robust? Another look at recent trends in old-age disability. Journals of Gerontology - Series B Psychological Sciences and Social Sciences, 56(4), S206–S218. [DOI] [PubMed] [Google Scholar]
- Seeman TE, McEwen BS, Rowe JW, & Singer BH (2001). Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences of the United States of America, 98(8), 4770–4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Merkin SS, Crimmins EM, & Karlamangla AS (2010). Disability trends among older Americans: National Health and Nutrition Examination surveys, 1988–1994 and 1999–2004. American Journal of Public Health, 100(1), 100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Macinko J, Starfield B, Xu J, & Politzer R (2003). Primary Care, Income Inequality, and Stroke Mortality in the United States: A Longitudinal Analysis, 1985–1995. Stroke, 34(8), 1958–1964. [DOI] [PubMed] [Google Scholar]
- Shi L, Macinko J, Starfield B, Xu J, Regan J, Politzer R, & Wulu J (2004). Primary Care, Infant Mortality, and Low Birth Weight in the States of the USA. Journal of Epidemiology and Community Health, 58(5), 374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, & Kawachi I (2004). Income Inequality and Health: What Have We Learned So Far? Epidemiologic Reviews, 26, 78–91. [DOI] [PubMed] [Google Scholar]
- Tibber MS, Walji F, Kirkbride JB, & Huddy V (2022). The association between income inequality and adult mental health at the subnational level—a systematic review. Social Psychiatry and Psychiatric Epidemiology, 57(1), 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG (1992). Income distribution and life expectancy. British Medical Journal, 304(6820), 165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG (1996). Unhealthy Societies: The Afflictions of Inequality. New York: Routledge. [Google Scholar]
- Wilkinson RG, & Pickett KE (2006). Income Inequality and Population Health: A Review and Explanation of The Evidence. Social Science and Medicine, 62, 1768–1784. [DOI] [PubMed] [Google Scholar]
- Yang Y, & Kozloski M (2011). Sex differences in age trajectories of physiological dysregulation: Inflammation, metabolic syndrome, and allostatic load. Journals of Gerontology - Series A Biological Sciences and Medical Sciences, 66 A(5), 493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, & Land KC (2006). A mixed models approach to the age-period-cohort analysis of repeated cross-section surveys, with an application to data on trends in verbal test scores. In Sociological Methodology (Vol. 36, Issue 1, pp. 75–97). John Wiley & Sons, Ltd. [Google Scholar]
- Yusuf S, Reddy S, Ounpuu S, & Anand S (2001). Global Burden of Cardiovascular Diseases: Part I: General Considerations, the Epidemiologic Transition, Risk Factors, and Impact of Urbanization. Circulation, 104, 2746–2753. [DOI] [PubMed] [Google Scholar]
- Zang E, Zheng H, Yang YC, & Land KC (2019). Recent trends in US mortality in early and middle adulthood: Racial/ethnic disparities in inter-cohort patterns. International Journal of Epidemiology, 48(3), 934–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H (2012). Do people die from income inequality of a decade ago? Social Science and Medicine, 75(1), 36–45. [DOI] [PubMed] [Google Scholar]
- Zheng H, & Echave P (2021). Are Recent Cohorts Getting Worse? Trends in U.S. Adult Physiological Status, Mental Health, and Health Behaviors across a Century of Birth Cohorts. American Journal of Epidemiology, 190(11), 2242–2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, & George LK (2012). Rising U.S. income inequality and the changing gradient of socioeconomic status on physical functioning and activity limitations, 1984–2007. Social Science and Medicine, 75(12), 2170–2182. [DOI] [PubMed] [Google Scholar]
- Zimmerman FJ, & Bell JF (2006). Income inequality and physical and mental health: Testing associations consistent with proposed causal pathways. Journal of Epidemiology and Community Health, 60(6), 513–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


