1. Introduction
Beyond the immediate health implications, the COVID-19 pandemic has also led to mounting financial losses with little immediate prospects for recovery. Lockdowns and other extreme restrictions have also added additional mental health and economic stresses that may generate considerable uncertainty. This has been exacerbated by conflicting messages from governments and public health authorities. Intolerance of uncertainty (UI) refers to an individual's negative emotions, cognitions, and behaviors when uncertainty is experienced and is defined as: "an individual's dispositional incapacity to endure the aversive response triggered by the perceived absence of salient, key, or sufficient information, and sustained by the associated perception of uncertainty."(Carleton et al., 2012; p. 31). Research suggests that intolerance of uncertainty may play a central role in the etiology and maintenance of worry and rumination, which may explain its transdiagnostic associations with variety of psychological disorders (Yook et al., 2010). Indeed, intolerance of uncertainty has been associated with poor mental health during the COVID-19 pandemic (Rettie and Daniels, 1037), while intolerance of uncertainty was found to explain the positive connection between anxiety symptoms and anger (Fracalanza et al., 2014). The array of losses accompanying COVID-19 (e.g. health of self or loved ones, finances, routines and opportunities to see friends and family) might be expected to arouse anger and civil unrest (Galea and Abdalla, 2020). This anger in itself is associated with depression (Busch, 2009) and can include greater symptom severity and worse treatment response (Cassiello‐Robbins and Barlow, 2016). Both expressed and suppressed anger can be a source of conflict and become self-directed which may lead to coronary heart diseases, diabetes, bulimic behaviors and road accidents (Staicu and Cuţov, 2010). In accordance with the above, we explore the role of anger as a moderator between intolerance of uncertainty and depression in the light of the ongoing coronavirus pandemic.
2. Methods
We deployed the Israeli Ipanel company to deploy the COVID-19 Mental Health Survey. The panel is a probability-based panel with 100,000 members designed to be representative of the adult Jewish population in Israel. Data were collected from August 3 to August 30, 2020. The sample was administered online, and all participants signed an electronic informed consent. The study was approved by Ariel University Institutional Review Board (AU-SOC-YHR-20200616). Out of 1350 invitations sent, 1030 responded (response rate = 76.2%). We conducted a priori sensitivity analyses and found no statistically significant differences between those who answered the survey and those who did not for each of the demographic variables in the study. The sample mean age was 40.75 (SD = 14.75; range 18–75) with 521 (50.6%) women, 645 (62.6%) who are in intimate relationship, 465 (45.1%) who have an academic degree. We employed the Intolerance of Uncertainty Scale (IUS-12) (Carleton et al., 2007), a 12-item self-report measure of negative beliefs about and reactions to uncertainty (e.g., “Uncertainty makes life intolerable”). Items on the IUS-12 are rated on a five-point, Likert-type scale ranging from 1 (Not at all characteristic of me) to 5 (Entirely characteristic of me) (IUS-12 scale, α = 0.91). The IUS-12 skewness was 0.425 (Skewness SD = .076) and Kurtosis was -.189 (Kurtosis SD = .152). Anger was measured by the Short Anger Measure (SAM) (Gerace and Day, 2014), a 12-item self-report measure of angry feelings and aggressive impulses (SAM scale, α = 0.90). Items on the SAM are rated on a five-point, Likert scale ranging from 1(never) to 5 (almost always). The SAM skewness was 0.813 (Skewness SD = .076) and Kurtosis was 0.401 (Kurtosis SD = .152). Depression was measured using the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001). This 9-item self-report measure asks participants indicate how often they have been bothered by each symptom over the last two weeks using a four-point Likert scale ranging from 0 (Not at all) to 3 (Nearly every day). Possible scores range from 0 to 27, with higher scores indicative of higher levels of depression. A cut-off score of ≥10 is used to identify those who are likely to meet the criteria for depressive disorder. This cut-off produces good sensitivity (0.88) and specificity (0.88) (PHQ-9; α =.88). The PHQ-9 skewness was 1.222 (Skewness SD = .076) and Kurtosis was 1.303 (Kurtosis SD = .152). The analytic plan used moderation analysis to examine the potential moderating effect of anger on the association between intolerance of uncertainty and depressive symptoms. No multicollinearity was found in the study. For IUS and SAM the VIF was 1.208 and the tolerance was 0.828. In addition, we have added Cohen's d for measuring effect size. Cohen suggested that d = 0.2 be considered a ‘small’ effect size, 0.5 a ‘medium’ effect size, and 0.8 a ‘large’ effect size (Cohen, 2013).
3. Results
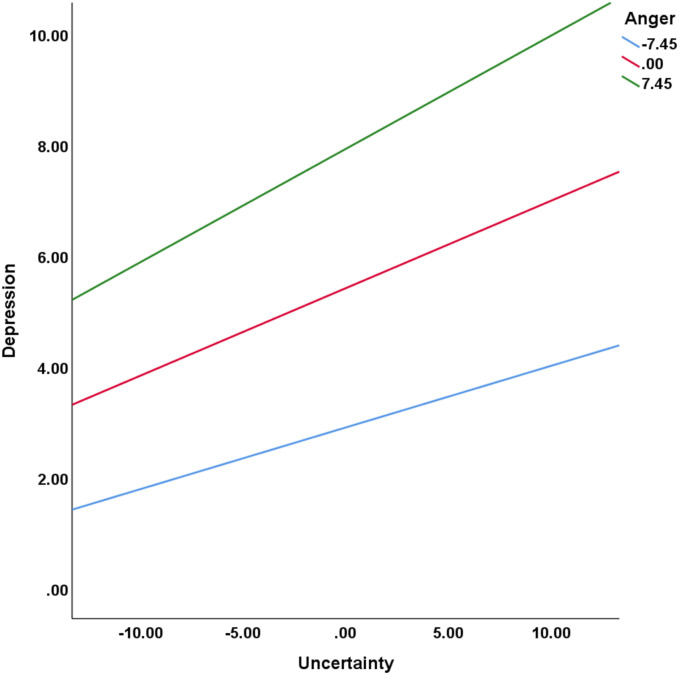
The prevalence rate of probable depression in August 2020 showed that 20.5% (95% CI, 18.1%–23.1%) of respondents had met reached the cut-off point and above for depression. This compares to a 2007 Israel National Health Survey which reports a prevalence of 9.8% (95% CI, 9.0%–10.6%) for major depression (Levinson et al., 2007). Anger was examined as a moderator of the association between intolerance of uncertainty and depression. Using SPSS process module Model 1(Hayes, 2017), intolerance of uncertainty and anger were entered in the first step of the regression analysis, in the second step the interaction term between intolerance of uncertainty and anger explained a significant increase in variance in depression, ΔR2 = .01, F (1, 1030) = 16.51, p < .001. Thus, anger was a significant moderator of the relationship between intolerance of uncertainty and depression. The unstandardized simple slope for depression 1 SD below the mean of anger was 0.11 (t = 6.93; p < .001), for depression with a mean level of anger was 0.16 (t = 11.28; p < .001), and for depression 1 SD above the mean of anger was 0.20 (t = 10.26; p < .001) (Fig. 1 ). Finally, Cohen's d measuring effect size in the regression for the association between intolerance of uncertainty and depression was 0.75 (r = 0.35) and 1.21 (r = 0.52) for the association between anger and depression.
Fig. 1.
The moderation of Anger on the relationship between Uncertainty and depression.
4. Discussion
The current findings demonstrated a direct link between intolerance of uncertainty and depression during COVID-19. This result highlights the need to provide structured and targeted psychological support and guidance to reduce intolerance of uncertainty during COVID (Busch, 2009). As uncertainty continues, governments should strive to provide clearer information regarding COVID-19 management, including the use of lockdowns and other restrictions, in order to provide relief and reduce uncertainty. Anger had an indirect effect on the association between intolerance of uncertainty and depression, stressing the importance of targeting ways to reduce anger to increase wellbeing. Anger management through cognitive behavior therapy techniques have been shown to be very effective for anger reduction (Bradbury and Clarke, 2007). By integrating assessment of anger into COVID-19 care settings depression may be identified at an early stage, ensuring the capacity for timely consultation with mental health specialists.
The current study was limited by its cross-sectional design and possible response bias introduced by participation through an online application. In addition, the sample consist of a high percentage of subjects with an academic degree. Comparison with 2007 data might be difficult as there could be an underestimation of depression due to more stigmatization or lesser awareness. Findings demonstrate the increased mental health burden associated with uncertainty during a pandemic. In doing so they highlight the importance of identifying and targeting mediator variables such as anger in order to facilitate the management of psychological health during uncertain times.
Ethics approval
The study was approved by Ariel University Institutional Review Board (AU-SOC-YHR-20200616).
Funding/support
The study was supported via internal research grant from Ariel University Research Authority (RA2000000302).
Role of the funder/sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration of competing interest
The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
References
- Bradbury K.E., Clarke I. Cognitive behavioural therapy for anger management: effectiveness in adult mental health services. Behav. Cognit. Psychother. 2007;35(2):201–208. [Google Scholar]
- Busch F.N. Anger and depression. Adv. Psychiatr. Treat. 2009;15:271–278. [Google Scholar]
- Carleton R.N., Norton M.P.J., Asmundson G.J. Fearing the unknown: a short version of the intolerance of uncertainty scale. J. Anxiety Disord. 2007;21(1):105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Mulvogue M.K., Thibodeau M.A., McCabe R.E., Antony M.M., Asmundson G.J. Increasingly certain about uncertainty: intolerance of uncertainty across anxiety and depression. J. Anxiety Disord. 2012;26(3):468–479. doi: 10.1016/j.janxdis.2012.01.011. [DOI] [PubMed] [Google Scholar]
- Cassiello-Robbins C., Barlow D.H. Anger: the unrecognized emotion in emotional disorders. Clin. Psychol. Sci. Pract. 2016;23(1):66–85. [Google Scholar]
- Cohen J. Academic press; 2013. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Fracalanza K., Koerner N., Deschênes S.S., Dugas M.J. Intolerance of uncertainty mediates the relation between generalized anxiety disorder symptoms and anger. Cognit. Behav. Ther. 2014;43(2):122–132. doi: 10.1080/16506073.2014.888754. [DOI] [PubMed] [Google Scholar]
- Galea S., Abdalla S.M. COVID-19 pandemic, unemployment, and civil unrest: underlying deep racial and socioeconomic divides. JAMA. 2020;324(3):227–228. doi: 10.1001/jama.2020.11132. [DOI] [PubMed] [Google Scholar]
- Gerace A., Day A. The Short Anger Measure: development of a measure to assess anger in forensic populations. J. Forensic Nurs. 2014;10:44–49. doi: 10.1097/JFN.0000000000000010. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford publications; 2017. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ‐9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson D., Zilber N., Lerner Y., Grinshpoon A., Levav I. Prevalence of mood and anxiety disorders in the community: results from the Israel National Health Survey. Isr. J. Psychiatry Relat. Sci. 2007;44(2):94–103. [PubMed] [Google Scholar]
- Rettie H, Daniels J. Coping and Tolerance of Uncertainty: Predictors and Mediators of Mental Health during the COVID-19 Pandemic. American Psychologist Advance online publication. 10.1037/amp0000710. [DOI] [PubMed]
- Staicu M.L., Cuţov M. Anger and health risk behaviors. J. Med.life. 2010;3(4):372–375. [PMC free article] [PubMed] [Google Scholar]
- Yook K., Kim K.H., Suh S.Y., Lee K.S. Intolerance of uncertainty worry, and rumination in major depressive disorder and generalized anxiety disorder. J. Anxiety Disord. 2010;24(6):623–628. doi: 10.1016/j.janxdis.2010.04.003. [DOI] [PubMed] [Google Scholar]