Abstract
The COVID-19 pandemic has upended the lives of everyone in the United States, negatively impacting social interactions, work, and living situations, and potentially exacerbating mental health issues in vulnerable individuals. Within the Department of Veterans Affairs (VA) healthcare system, two vulnerable groups include those with a psychotic disorder (PSY) and those who have recently experienced homelessness (recently housed Veterans, RHV). We conducted phone interviews with PSY (n = 81), RHV (n = 76) and control Veterans (CTL, n = 74) between mid-May – mid-August 2020 (“initial”) and between mid-August – mid-October 2020 (“follow-up”). At the initial period, we also collected retrospective ratings relative to January 2020 (“pre-COVID-19”). We assessed clinical factors (e.g., depression, anxiety, loneliness) and community integration (e.g., social and role functioning). All groups reported worse clinical outcomes after the onset of the COVID-19 pandemic. However, PSY and RHV exhibited improvements in depression and anxiety from initial to follow up, whereas CTL continued to exhibit elevated levels. There was little change in community integration measures. Our results indicate that all groups reported increased mental health problems after the onset of the pandemic, but vulnerable Veterans were not disproportionately affected and had better mental health resilience (i.e., for depression and anxiety) as the pandemic progressed compared to CTL. This effect could be due to the availability and utilization of VA services for PSY and RHV (e.g., housing and financial support, medical and mental health services), which may have helped to mitigate the impact of the pandemic.
Keywords: COVID pandemic, Veterans, Homeless, Psychosis, Mental health, Community integration
1. Introduction
The global coronavirus disease (COVID-19) pandemic has upended the daily lives of most people throughout the world and raised widespread mental health concerns. The stay-at-home orders and social distancing recommendations that have been put in place by public health authorities in response to COVID-19 have dramatically impacted people's daily social interactions, work, and living situations. These impacts are likely to have affected a range of mental health issues.
In terms of psychological consequences, the current pandemic and resulting public health measures have increased levels of anxiety, depression, suicidal ideation, and loneliness across a wide swath of the world population (Bauerle et al., 2020; Jewell et al., 2020; Killgore et al., 2020; Newby et al., 2020; Salari et al., 2020; Shah et al., 2020), similar to prior pandemics (Peng et al., 2010; Wheaton et al., 2012; Zortea et al., 2020). Other aspects of mental health may also be impacted. For example, concerns about contamination and obsessive behaviors (such as hand washing) are likely to have increased for obvious reasons (Abba-Aji et al., 2020). In addition, safer-at-home and social distancing mandates have severely disrupted aspects of community functioning, including a reduction in social and family contacts, substantial job loss and reduction in pay, and potential loss of housing (Tsai and Wilson, 2020).
Two populations of special concern during the pandemic within the U.S. Department of Veterans Affairs (VA) system are those who have a psychotic disorder (PSY) and those who have recently experienced homelessness (recently housed Veterans, RHV). These groups generally do not have strong social contacts to begin with and might be particularly vulnerable to mental health and social impacts of the pandemic (Kozloff et al., 2020). Therefore, in the current, ongoing longitudinal study we aimed to determine the impact of social distancing and COVID-19 restrictions on clinical factors (e.g., anxiety, depression) and community integration factors (e.g., social networks, family networks, work) in these two vulnerable Veteran groups, in addition to control Veterans (CTL) who have never experienced psychosis or homelessness. We also examined whether any of the negative impacts on clinical and community integration factors would be moderated by age. Some studies have found that older adults are relatively resilient to the effects of the pandemic and not show negative impacts on community integration or mental health (Vahia et al., 2020). We hypothesized that all three groups would experience negative impacts on clinical and community integration factors due to the pandemic. We further hypothesized that the two vulnerable groups of Veterans (PSY, RHV) would experience disproportionate negative impacts of the pandemic on these factors compared to controls.
2. Methods
Data collection occurred between mid-May – mid-August 2020 for the initial period (“initial”) and mid-August – mid-October 2020 for the follow up period (“follow-up”). Potential participants were recruited through two main sources: 1) two VA administrative datasets (the Corporate Data Warehouse and Homeless Veteran Registry) from the VA Informatics and Computing Infrastructure (VINCI) platform; and 2) Veterans who have participated in prior studies in our lab and agreed to be contacted for future studies. For RHV, we utilized the VA Computerized Patient Record Systems (CPRS) and VINCI to determine if the participant had a current housing voucher administered by the Housing and Urban Development – VA Supportive Housing (HUD-VASH) initiative. For PSY, we examined CPRS to determine if a psychotic disorder was listed in their medical record to verify eligibility. All procedures were approved by the VA Greater Los Angeles Institutional Review Board.
Selection criteria for the groups were intentionally broad and relied on the chart diagnoses from VA medical records. For PSY, participants required a psychotic disorder diagnosis (other than substance-induced psychosis), such as schizophrenia (n = 42), schizoaffective disorder (n = 22), depressive disorder with psychotic features (n = 1), bipolar disorder with psychotic features (n = 9), or psychotic disorder not otherwise specified (n = 7). For RHV, participants required a history of homelessness and attainment of housing within the past 12 months with a HUD-VASH voucher. Of the RHV, eight received a diagnosis for a psychotic disorder, which was permissible for this group. For the control group (CTL), participants required no history of a psychotic disorder or evidence of homelessness based on codes in VINCI and review of medical records. Once enrolled in the study, we examined CPRS for all participants for current mental health and alcohol/substance use disorder diagnoses. Based on this review, we report the percentage of participants in each group with a mood disorder, posttraumatic stress disorder (PTSD), and a current alcohol or substance use disorder in addition to providing demographic information. PTSD and mood disorders were present in all three groups, though to a lesser degree in PSY. Alcohol and substance use were comparatively high in PSY and RHV compared to CTL.
We identified 956 potentially eligible participants who were contacted by phone by a lab research assistant. After a brief description of the project, participants who agreed to participate provided verbal informed consent. The participant's contact information was then provided to one of ten clinically trained interviewers. Interviewers typically conducted the initial assessment in two parts on separate days. In the first part, interviewers obtained information on demographics (e.g., age, gender, race/ethnicity, personal education, etc.), finances (e.g., monthly income, work hours/pay reductions, furloughs, etc.) and COVID-specific questions (e.g., COVID-19 positive test, self-quarantine, etc.). In the second part, interviewers administered several questionnaires assessing clinical, risk/protective, and community integration factors (details below). Most questionnaires for the clinical and community integration factors were assessed for three rating periods: initial, follow-up, and a retrospective evaluation collected at initial, in which participants were asked to give ratings for January 2020 (“pre-COVID”).
The schedule of assessments along with scales and questionnaires used are detailed in Table 2 . For clinical factors, we assessed depression, anxiety, obsessive-compulsive traits, paranoid thoughts, self-report motivation, suicidal ideation, substance and alcohol use, and loneliness. We also administered the Fear of Illness and Virus Evaluation (FIVE) questionnaire (Ehrenreich-May 2020) which assessed people's fears and behaviors about contamination and illness, social distancing, and the impact of COVID-19 on their lives. For the assessment of alcohol and substance use, we administered the Addiction Severity Index (ASI) (McLellan et al., 1980), which assessed the number of days in the past 30 days that participants endorsed using alcohol or a substance (e.g., cannabis, methamphetamine). As few participants endorsed using any substance other than cannabis, only alcohol and cannabis use are reported in the Results.
Table 2.
List of questionnaires and interviews to assess clinical factors, vulnerability and protective factors, and community integration.
| Measure (Reference) | Scoring | Pre-COVID | Initial | Follow Up |
|---|---|---|---|---|
| Clinical Factors | ||||
| Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001) | Higher score = greater depression | X | X | X |
| General Anxiety Disorder (GAD-7) (Spitzer et al., 2006) | Higher score = greater anxiety | X | X | X |
| Dimensional Obsessive-Compulsive Scale (DOCS) (Abramowitz et al., 2010) | Higher score = greater endorsement of obsessive-compulsive behaviors | X | X | X |
| Revised Paranoid Thoughts Scale (RGPTS) (Freeman et al., 2019) | Higher score = greater level of paranoid thoughts | X | X | X |
| Motivation and Pleasure Scale – Self-Report (MAP-SR) (Llerena et al., 2013) | Higher score = diminished motivation and pleasure | X | X | |
| Montgomery-Åsberg Depression Rating Scale (MADRS) (Montgomery and Asberg, 1979) | Ratings≥4 indicate moderate to severe suicidal ideation | X | X | |
| Fear of Illness and Virus Evaluation (FIVE) – Adult Report Form (Ehrenreich-May 2020) | Higher score = greater fear and distress related to COVID and quarantine orders | X | X | |
| Revised UCLA Loneliness Scale (ULS) (Russell et al., 1980) | Higher score = greater loneliness | X | X | X |
| Community Integration | ||||
| Lubben Social Network Scale (LSNS) (Lubben et al., 2002) | Higher score = better family and social functioning | X | X | X |
| Role Functioning Scale (RFS) – Family and Social Subscales (Goodman et al., 1993) | Higher score = better family and social functioning | X | X | X |
| Role Functioning Scale (RFS) – Work and Ind. Living Subscales (Goodman et al., 1993) | Higher score = better work and better independent living outcomes | X | X | X |
2.1. Analytical approach
For demographics and the risk and protective factors, we used either Chi-square or analysis of variance (ANOVA) tests to examine group differences at the initial assessment. Group (CTL, PSY, RHV) by Time (pre-COVID, initial, follow-up) effects for the clinical and community integration factors were analyzed with linear mixed-effects models using R version 4.0.2 and the lme4 package version 1.1–23 (Bates et al., 2015). Separate models for each measure were fit using restricted maximum likelihood (REML), and no missing value imputation was utilized. We entered time and group as fixed effects, with participant as a random effect. The formula for each analysis was thus DV ~ Group*Time + (1|Participant). P-values were calculated using the Satterthwaite method using the afex package version 0.28–0 (Singmann et al., 2020). If a significant main effect or interaction was identified, we performed post-hoc comparisons using false-discovery rate (FDR) correction with the emmeans package version 1.5.1 (Lenth et al., 2020). For these analyses, we present in tables the F-value, degrees of freedom, and estimated p-value for main effects and interactions; we present the full summary statistics, including parameter estimates, confidence intervals, p-values, and degrees of freedom, in the supplementary files. For the ASI, we conducted a repeated measures ordinal logistic regression using the GENLIN function in SPSS version 26 (IBM SPSS Statistics, Armonk, NY, USA). Finally, we conducted exploratory analyses using age as a covariate to determine if age moderated any of the negative effects of the pandemic on the clinical or community integration factors. For these analyses, we included age as a covariate in the model with the resulting formula, DV ~ Group*Time + Age + (1|Participant). Because some participants did not answer all questions, there are minor differences in degrees of freedom from measure to measure.
3. Results
3.1. Demographics
Demographic information and the statistical results and p-values are presented in Table 1. We collected data on 81 PSY, 76 RHV, and 74 CTL for both the pre-COVID and initial periods. Retention for the follow-up period was relatively high (>82% in each group), with 74 PSY, 63 RHV, and 66 CTL assessed during this period. As is typical of studies consisting solely of Veterans, the samples included a relatively high proportion of Black participants and the majority (87.1%) were male. Groups did not differ significantly on ethnicity, race, or gender. There were significant group differences in age and in personal education. The control group was significantly older than the RHV group; there were no other significant age differences. Controls also had significantly higher personal education levels compared to the other two groups; there were no significant differences between RHV and PSY. However, there were no significant differences in parental education, which serves as a proxy measure of familial socioeconomic status, across the three groups. Regarding direct COVID-related impacts, fewer than 2.7% of participants in each group reported being diagnosed with COVID-19 at initial and none reported a new diagnosis at follow-up; fewer than 20% of participants in each group reported having to self-quarantine due to potential COVID-19 exposure at initial, and fewer than 9% in each group reported subsequent need to self-quarantine at follow-up.
Table 1.
Demographics and clinical diagnoses.
| Control (n = 74) | Recently Housed (n = 76) | Psychosis (n = 81) | Statistic (F or χ2) | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 56.5 (9.5) | 51.6 (12.5) | 54.4 (9.8) | F2,228 = 4.03, p = 0.019 C > RH |
| Gender (M:F) | 63:11 | 66:10 | 72:9 | χ2(2) = 0.485, p = 0.785 |
| Personal Education (years) | 14.6 (2.0) | 13.4 (1.5) | 13.4 (1.6) | F2,228 = 12.94, p < 0.001 C > RH, P |
| Parental Education | 13.0 (3.1) | 13.5 (3.1) | 12.9 (3.9) | F2,228 = 0.74, p = 0.477 |
| Ethnicity (H:NH) | 19:55 | 21:55 | 16:63 | χ2(2) = 1.23, p = 0.541 |
| Race (B:W:O) | 28:38:8 | 34:31:9 | 40:29:10 | χ2(4) = 3.47, p = 0.482 |
| Clinical Diagnoses from Medical Records | ||||
| Mood Disorder | 47.3% | 60.5% | 23.5% | −−− |
| PTSD | 39.2% | 42.1% | 22.2% | −−− |
| Alcohol Use Disorder | 4.1% | 22.4% | 23.5% | −−− |
| Substance Use Disorder | 9.5% | 38.2% | 33.3% | −−− |
Note: M = male, F = Female, H = Hispanic, NH = Non-Hispanic, B = Black, W = White, O = Other, PTSD = posttraumatic stress disorder.
3.2. Clinical factors
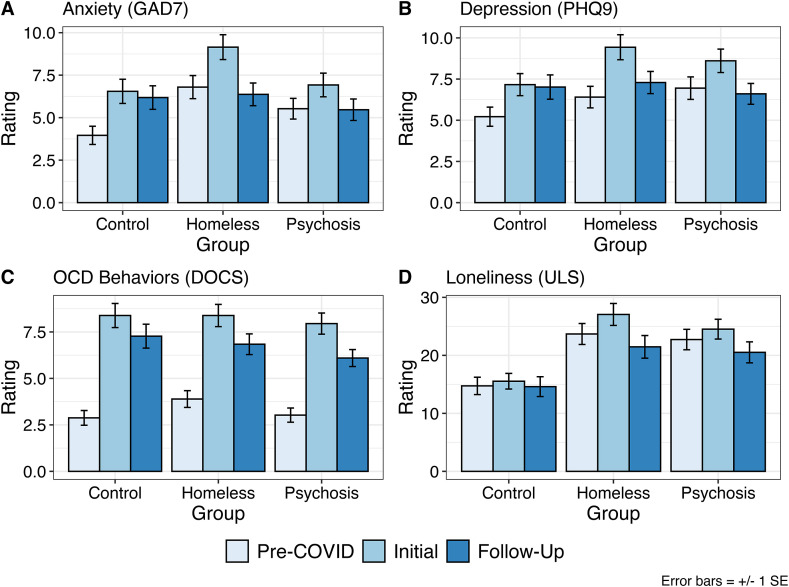
For clinical measures, descriptive statistics as well as inferential statistics and p-values are reported in Table 3 . For depression, there was a significant main effect of Time (Fig. 1 A) and a significant Time × Group interaction; the main effect of Group was not significant. The interaction was driven by CTL showing significantly increased depression at initial and follow-up relative to pre-COVID ratings, with no change between initial and follow-up. Both RHV and PSY showed a significant increase in depression from pre-COVID to initial, followed by a significant decrease from initial to follow-up. For anxiety (Fig. 1B), there were significant main effects of Group and Time, and a significant Group × Time interaction. The interaction was driven by CTL reporting increased anxiety at initial and follow-up relative to pre-COVID, with no change between initial and follow-up. Both RHV and PSY showed a significant increase in anxiety from pre-COVID to initial, followed by a significant decrease from initial to follow-up.
Table 3.
Descriptive statistics and statistical test results for clinical factors, including depression (PHQ-9), anxiety (GAD-7), obsessive-compulsive traits (DOCS), suspiciousness (RGPTS), alcohol and cannabis use, motivation and pleasure (MAPS-SR), suicidal ideation (MADRS), and Fear of Illness and Virus Evaluation (FIVE). Values are raw means and standard deviations.
| Control |
Recently Housed |
Psychosis |
Statistics |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Initial | Follow Up | Pre | Initial | Follow Up | Pre | Initial | Follow Up | ||
| Depression (PHQ9) | 5.22 (5.00) | 7.16 (5.76) | 7.02 (6.00) | 6.41 (5.64) | 9.43 (6.53) | 7.29 (5.30) | 6.95 (6.07) | 8.61 (6.32) | 6.60 (5.40) | Time: F2,424.09 = 28.6, p = 2.2 x 10−12 Group: F2,225.11 = 1.48, p = 0.230 T x G: F4,424.08 = 2.65, p = 0.033 |
| Anxiety (GAD7) | 3.96 (4.58) | 6.55 (6.08) | 6.18 (5.62) | 6.80 (5.85) | 9.15 (6.28) | 6.37 (5.25) | 5.53 (5.38) | 6.92 (6.15) | 5.47 (5.40) | Time: F2,423.55 = 22.5, p = 5.01 x 10−10 Group: F2,223.85 = 3.36, p = 0.037 T x G: F4,423.53 = 2.75, p = 0.028 |
| OCD – Contamination (DOCS) | 2.88 (3.38) | 8.38 (5.54) | 7.27 (5.22) | 3.89 (3.86) | 8.38 (5.11) | 6.84 (4.39) | 3.03 (3.38) | 7.95 (5.03) | 6.10 (3.90) | Time: F2,424.62 = 137.3, p < 2.0 x 10−16 Group: F2,222.84 = 0.69, p = 0.505 T x G: F4,424.60 = 1.013, p = 0.400 |
| Suspiciousness (RGPTS) | 10.29 (11.09) | 10.89 (10.58) | 10.71 (13.26) | 15.64 (16.20) | 15.62 (16.76) | 14.34 (16.23) | 17.83 (17.21) | 17.16 (16.23) | 17.81 (18.08) | Time: F2,415.67 = 0.08, p = 0.920 Group: F2,217.37 = 5.53, p = 0.005 T x G: F4,415.66 = 0.58, p = 0.676 |
| ASI Alcohol+ | Time: Wald χ2(2) = 5.21, p = 0.074 Group: Wald χ2(2) = 4.73, p = 0.094 T X G: Wald χ2(4) = 5.52, p = 0.24 |
|||||||||
| None | 69.4 | 61.1 | 65.2 | 50.7 | 46.4 | 58.3 | 64.9 | 64.9 | 65.8 | |
| Occasional | 26.4 | 31.9 | 25.8 | 33.3 | 37.7 | 25.0 | 22.1 | 24.7 | 24.7 | |
| Frequent | 4.2 | 7.0 | 9.1 | 16.0 | 15.9 | 16.7 | 13.0 | 10.4 | 9.6 | |
| ASI Cannabis+ | Time: Wald χ2(2) = 8.50, p = 0.014 Group: Wald χ2(2) = 17.88, p < 0.001 T X G: Wald χ2(4) = 14.85, p = 0.005 |
|||||||||
| None | 91.7 | 93.1 | 95.5 | 65.2 | 59.4 | 76.7 | 74.0 | 81.8 | 80.8 | |
| Occasional | 4.2 | 2.8 | 0.0 | 8.7 | 11.6 | 1.7 | 10.4 | 7.8 | 9.6 | |
| Frequent | 4.1 | 4.1 | 4.5 | 26.1 | 29.0 | 21.7 | 15.6 | 10.4 | 9.6 | |
| Motivation (MAPS-SR) | – | 39.64 (12.52) | 38.89 (13.77) | – | 32.48 (14.13) | 35.90 (12.66) | – | 34.83 (14.51) | 36.48 (13.31) | Time: F1,200.25 = 2.65, p = 0.105 Group: F2,214.72 = 3.68, p = 0.027 T x G: F2,200.23 = 1.61, p = 0.202 |
| Loneliness (ULS) | 14.74 (12.71) | 15.54 (11.43) | 14.61 (13.87) | 23.68 (15.45) | 27.05 (16.18) | 21.47 (15.39) | 22.73 (15.46) | 24.52 (14.99) | 20.52 (15.48) | Time: F2,418.03 = 11.39, p = 1.53 x 10−5 Group: F2,219.81 = 10.7, p = 3.74 x 10−5 T x G: F4,418.02 = 0.98, p = 0.419 |
| Fear of Illness (FIVE) | – | 77.68 (19.96) | 74.56 (19.14) | – | 73.39 (17.85) | 72.16 (20.00) | – | 72.66 (17.19) | 68.84 (15.64) | Time: F1,200.30 = 6.11, p = 0.014 Group: F2,215.351 = 1.58, p = 0.207 T x G: F2,200.27 = 0.43, p = 0.654 |
ASI = Addiction Severity Index; + Percent participants reporting use in past 30 days for the categories of None, Moderate (1–8 days), and Severe (9+ days).
Fig. 1.
Raw means and ± 1 standard error bars for clinical factors assessed pre-COVID (light purple), initial (aqua), and follow up (blue) for control Veterans (CTL), Veterans with psychosis (PSY), and recently-housed Veterans (RHV). A) Anxiety symptoms (GAD7); B) Depression symptoms (PHQ9); C) loneliness (ULS); and D) obsessive-compulsive behaviors (DOCS). For all ratings a higher score indicates increased pathology. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
For suspiciousness, there was a significant main effect of Group in that both RHV and PSY had higher levels of suspiciousness compared to CTL, though this effect did not survive FDR correction. The main effect of Time and the Group × Time interaction were not significant. For OCD-like features, there was a significant main effect of Time (Fig. 1C). The Group main effect and the Group × Time interaction were not significant. Follow-up tests for the Time main effect revealed significant differences between each pair of timepoints (p's < 0.001), with OCD-like features highest at the initial assessment. For Motivation and Pleasure, the Group main effect was significant, in that CTL reported significantly greater levels compared to RHV but not PSY; the main effect of Time and the Group × Time interaction were not significant. For Fear of Illness, the Time main effect was significant, with a small but significant decrease from initial to follow up; the main effect of Group and the Group × Time interaction were not significant.
For loneliness, there were significant main effects of Time and Group (Fig. 1D). The Group × Time interaction was not significant. Follow-up tests for the Time main effect revealed significant differences between each pair of timepoints (p's < 0.05), with loneliness highest at the initial assessment. Follow-up tests for the Group main effect revealed significantly higher loneliness in RHV and PSY compared to CTL (p's < 0.0005), with no significant difference between RHV and PSY. Regarding the MADRS, most participants endorsed no or mild thoughts of suicidal ideation at initial or follow up (>85% in all three groups had ratings of 0 or 1). Only five participants at initial (1 CTL, 1 RHV, 3 PSY) and one participant at follow up (1 PSY) had a score of 4 indicating moderate levels of suicidal ideation. No participant in any group had a rating higher than 4.
For the ASI we assigned participants to one of three severity categories based on inspection of the distribution of reported days used: None (0 days), Occasional (1–8 days), and Frequent (9 or more days). For alcohol use, there were no significant main effects of Time or Group, and the Group × Time interaction was not significant. For cannabis use, there was a significant main effect of Group, Wald χ2 (2) = 17.88, p < 0.001, and a significant main effect of Time, Wald χ2 (2) = 8.50, p = 0.014. However, there was a significant Group × Time interaction, Wald χ2 (4) = 14.85, p = 0.005. The significant interaction was driven by the RHV reporting a significant increase in cannabis use at Initial relative to pre-COVID; there were no significant changes in the PSY or CTL groups.
Age was a significant covariate for only two measures: anxiety and motivation. Adding age as a covariate only changed the significance of one result, compared to the models that did not include an age covariate: for anxiety, the Group main effect changed from significant (p = 0.037) to a trend (p = 0.095). Adding age as a covariate did not change the significance of any other main effects or interactions. All results of the models including age covariates can be found in the Supplement.
3.3. Community integration
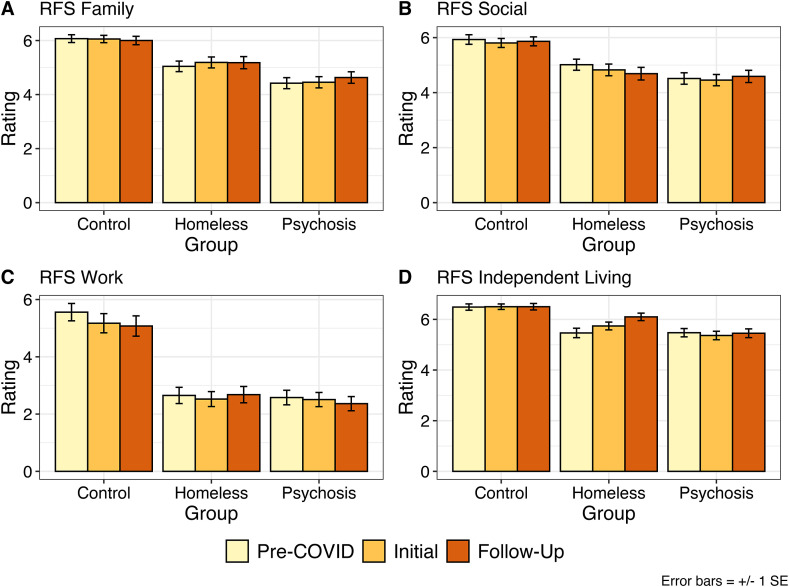
For community integration measures, descriptive statistics as well as inferential statistics and p-values are reported in Table 4 . The Lubben Social Network Scale showed a significant main effect of Group; CTL reported significantly higher levels of social networks compared to either the RHV or PSY (p's < 0.02), with no significant differences between the latter two groups. The main effect of Time and the Time × Group interaction were not significant. For Social Network functioning from the RFS, there was a significant main effect of Group; CTL reported significantly higher social network scores compared to both the RHV and PSY groups (p's < 0.0005), with no significant differences between the latter two groups (Fig. 2 A). The Time main effect and Group × Time interaction were not significant. For Family functioning from the RFS, there was a significant main effect of Group (Fig. 2B); all three groups differed from each other significantly (p's < 0.02), with functioning highest in CTL, lowest in PSY, and intermediate in RHV. The main effect of Time and Group × Time interaction were not significant.
Table 4.
Descriptive statistics and statistical test results for Community Integration factors. Values are raw means and standard deviations.
| Control |
Recently Housed |
Psychosis |
Statistics |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Initial | Follow Up | Pre | Initial | Follow Up | Pre | Initial | Follow Up | ||
| Social Networks (Lubben) | 31.25 (10.29) | 31.07 (10.17) | 31.11 (9.90) | 26.52 (11.34) | 26.28 (11.65) | 27.34 (10.66) | 26.19 (13.04) | 25.91 (13.06) | 25.15 (13.46) | Time: F2,411.86 = 0.23, p = 0.795 Group: F2,215.76 = 5.82, p = 0.003 T x G: F4,411.86 = 1.61, p = 0.172 |
| Role Functioning | ||||||||||
| Work | 5.56 (2.33) | 5.17 (2.56) | 5.08 (2.58) | 2.65 (2.24) | 2.52 (2.07) | 2.68 (2.13) | 2.58 (2.14) | 2.51 (2.08) | 2.36 (2.01) | Time: F2,358.73 = 1.75, p = 0.175 Group: F2,195.99 = 36.00, p = 4.65 x 10−7 T x G: F4,358.71 = 1.27, p = 0.281 |
| Independent Living | 6.49 (1.06) | 6.50 (0.92) | 6.50 (1.04) | 5.43 (1.54) | 5.72 (1.28) | 6.10 (1.15) | 5.49 (1.42) | 5.37 (1.47) | 5.45 (1.47) | Time: F2,412.25 = 7.26, p = 7.98 x 10−4 Group: F2,216.49 = 15.61, p = 4.65 x 10−7 T x G: F4,412.25 = 6.35, p = 5.77 x 10−5 |
| Family | 6.07 (1.23) | 6.06 (1.15) | 6.00 (1.26) | 5.04 (1.62) | 5.19 (1.68) | 5.18 (1.76) | 4.42 (1.78) | 4.45 (1.82) | 4.63 (1.82) | Time: F2,412.16 = 0.88, p = 0.417 Group: F2,216.34 = 20.58, p = 6.56 x 10−9 T x G: F4,412.16 = 1.00, p = 0.407 |
| Social | 5.93 (1.48) | 5.81 (1.39) | 5.86 (1.32) | 5.01 (1.68) | 4.82 (1.77) | 4.69 (1.79) | 4.51 (1.81) | 4.45 (1.80) | 4.59 (1.90) | Time: F2,411.07 = 1.85, p = 0.159 Group: F2,215.54 = 15.51, p = 5.09 x 10−7 T x G: F4,411.07 = 0.46, p = 0.767 |
Fig. 2.
Raw means and ± 1 standard error bars for community integration factors assessed with the Role Functioning Scale (RFS) pre-COVID (light yellow), initial (light orange), and follow up (dark orange) for control Veterans (CTL), Veterans with psychosis (PSY), and recently-housed Veterans (RHV). A) Family network functioning (RFS Family); B) Social network functioning (RFS Social); C) Work functioning (RFS Work); and D) Independent living (RFS Independent Living). For all ratings a higher score indicates better functioning. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Work functioning showed a significant main effect of Group (Fig. 2C); CTL had significantly greater work functioning than both RHV and PSY (p's < 0.001), but there was no significant difference between RHV or PSY. There was no significant effect of Time nor a Group × Time interaction. For independent living, there were significant main effects of Time and Group, and a significant Group × Time interaction (Fig. 2D). The interaction was due to a small but significant increase in independent living ratings in RHV from pre-COVID to initial to follow-up (p's < 0.015), with no significant changes in CTL or PSY.
Exploratory models that included age as a covariate showed broadly consistent results to the primary models. Age was a significant covariate for only one measure, social functioning from the RFS, but the age covariate did not change the significance of any main effects or interactions found using the primary model that did not include age. The results of all models including age covariates are described in the Supplement.
4. Discussion
In the current study, we found evidence of negative mental health impacts related to the COVID-19 pandemic on Veterans from two vulnerable groups (i.e., Veterans with psychosis, recently housed Veterans), as well as Veterans from a control group. Consistent with our hypotheses, all three groups reported increased levels of depression, anxiety, loneliness, and concerns about contamination relative to the retrospective report of their pre-COVID state. However, contrary to our hypotheses, we did not observe a disproportionate worsening of clinical symptoms in the two vulnerable Veteran groups compared to the Veteran controls. On the contrary, we found that for depression and anxiety both the PSY and RHV groups showed significant decreases from initial to follow up, whereas CTL maintained higher levels at both time periods relative to pre-COVID. The mental health effects in the current study are consistent with published reports in non-Veteran populations (e.g., Jewell et al., 2020). While this finding was unexpected it is consistent with previous research showing that humans are quite resilient and often do not show increased psychopathology after natural disasters, including pandemics (Pfefferbaum and North, 2020). Further, there is evidence that adversity in vulnerable Veteran groups might actually result in improvements in mental health outcomes and general health (Tsai et al., 2015). In addition, we found no increased use of alcohol in any groups, and only the RHV showed an increase in cannabis use. As expected, community integration (strength of family and social networks, work, independent living) was lower overall in the two vulnerable groups, however, the pandemic did not have a noticeable effect in these areas in any group. Moreover, we did not find that age influenced any of the findings in any substantial way. Finally, we did not detect any signs of imminent suicide risk.
There are some potential reasons for the lack of disproportionate effect on vulnerable Veterans. First, our sample was older and consisted of more males than most published reports to date. Some studies have found a disproportionate mental health impacts in the domains assessed in the current study among younger or female participants relative to older or male participants (Barros et al., 2020; Groarke et al., 2020; Jia et al., 2020). Second, it is likely that many of the vulnerable Veterans in the current study were engaged with mental health and case management services available to them through the VA. The VA very rapidly adapted telehealth service in homeless, mental health, and medical services when in-person visits became difficult due to the pandemic (Connolly et al., 2020; Heyworth et al., 2020). As we collect additional follow-up data, we will examine the role of specific types of VA mental health services and their role in mitigating negative effects of the pandemic. Finally, population-specific factors may have led to improvements in functioning and symptoms in the two vulnerable groups relative to the control group. For example, it is possible that those with psychosis may already prefer to spend more time indoors or avoid social situations due to social impairments in this population. Thus, they may have been less impacted over time by social distancing measures. For the recently housed group, their levels of symptoms may have been mitigated by the fact that they have less anxiety and depression over time that are associated with being housed after a period of homelessness. While these are intriguing possibilities, we unfortunately did not directly assess for these possibilities.
The study had several limitations. First, the study relied on retrospective self-reports of functioning prior to the onset of the pandemic for some measures. While the participants might not have been able to estimate a particular point in time from a few months prior, their responses are an indication of their impression of their own functioning pre-COVID, and thus could serve as a comparison to the follow-up assessment. However, as with other self-report measures there are biases that may affect the validity of the data, including poor recall and any cognitive impairments that can influence the participant's reporting. Thus, it is possible that the vulnerable participants, many of whom have cognitive impairments and past or present substance use issues, provided somewhat biased estimates of their pre-COVID mental health. However, if this were the case, we would expect to see similar biases on both the clinical and community integration measures. Instead, we found that the community integration measures were relatively unchanged for the current vs. pre-COVID assessment period. Second, all of the participants were Veterans so we cannot make comparisons to the general population. Third, as mentioned earlier, nearly all participants were male, making it impossible to examine for any possible gender effects. Finally, Veterans with a history of homelessness may be at greater risk of testing positive for COVID-19 (Tsai et al., in press), but we were not able to examine this possibility in our data because very few participants reported having been diagnosed with COVID-19 (<3% at initial, none at follow-up) and few reported that they needed to self-quarantine (<20% at initial and <9% at follow up). Given that we had too few participants directly impacted by COVID-19 (diagnosed or needing to self-quarantine) to examine for these possibilities, we are unable to determine the direct impact of COVID-19 on the clinical factors we examined.
Despite these limitations, the current results suggest a negative impact of the pandemic on mental health and daily functioning in all three groups of Veterans we examined. However, the “vulnerable” groups (PSY and RHV) actually showed more resilience in their mental health than non-vulnerable control Veterans in the follow-up period. Nevertheless, the COVID-19 pandemic continues, and infection rates across much of the United States have worsened in late 2020 and early 2021. Going forward, it will be important to understand how mental health and community integration in these groups may continue to change as the pandemic wears on over an extended period of time. We are continuing to conduct follow-up interviews with the same participants and can examine in future papers how measures of vulnerability and protective factors (e.g., resilience, perceived stress, coping skills, etc.) we assessed moderated the effects of the pandemic on mental health and community functioning we found in the vulnerable groups in the current study.
CRediT authorship contribution statement
Jonathan K. Wynn: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Supervision. Amanda McCleery: Conceptualization, Methodology, Writing – review & editing, Supervision, Project administration. Derek Novacek: Methodology, Writing – review & editing, Investigation. Eric A. Reavis: Conceptualization, Methodology, Writing – review & editing. Jack Tsai: Conceptualization, Methodology, Writing – review & editing. Michael F. Green: Conceptualization, Methodology, Writing – review & editing, Funding acquisition.
Declaration of competing interest
None of the authors report any conflicts of interest for this publication.
Acknowledgments
We extend our gratitude to our recruiters and interviewers without whom this work would not have been possible: Lauren Catalano, PhD, Gerard De Vera, Arpi Hasratian, Julio Iglesias, Brian Ilagan, Mark McGee, Jessica McGovern, PhD, Ana Ceci Myers, Megan Olsen, and Michelle Torreliza. We would like to thank Catherine Sugar, Ph.D. for statistical consultation. Finally, we thank our Veteran volunteers for taking the time to participate in this research.
The contents of this article do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.03.051.
Funding statement
This study was funded by the Research Enhancement Award Program to Enhance Community Integration in Homeless Veterans Rehabilitation Research and Development grant D1875-F from the Department of Veterans Affairs to Dr. Green and by the VA National Center on Homelessness Among Veterans. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abba-Aji A., Li D., Hrabok M., Shalaby R., Gusnowski A., Vuong W., Surood S., Nkire N., Li X.M., Greenshaw A.J., Agyapong V.I.O. COVID-19 pandemic and mental health: prevalence and correlates of new-onset obsessive-compulsive symptoms in a Canadian province. Int. J. Environ. Res. Publ. Health. 2020;17(19) doi: 10.3390/ijerph17196986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramowitz J.S., Deacon B.J., Olatunji B.O., Wheaton M.G., Berman N.C., Losardo D., Timpano K.R., McGrath P.B., Riemann B.C., Adams T., Bjorgvinsson T., Storch E.A., Hale L.R. Assessment of obsessive-compulsive symptom dimensions: development and evaluation of the Dimensional Obsessive-Compulsive Scale. Psychol. Assess. 2010;22(1):180–198. doi: 10.1037/a0018260. [DOI] [PubMed] [Google Scholar]
- Barros M.B.A., Lima M.G., Malta D.C., Szwarcwald C.L., Azevedo R.C.S., Romero D., Souza Júnior P.R.B., Azevedo L.O., Machado Í E., Damacena G.N., Gomes C.S., Werneck A.O., Silva D., Pina M.F., Gracie R. Report on sadness/depression, nervousness/anxiety and sleep problems in the Brazilian adult population during the COVID-19 pandemic. Epidemiol. Serv. Saude. 2020;29(4) doi: 10.1590/s1679-49742020000400018. [DOI] [PubMed] [Google Scholar]
- Bates D., Mächler M., Bolker B., Walker S. Fitting linear mixed-effects models using lme4. J. Stat. Software. 2015;67(1):1–48. [Google Scholar]
- Bauerle A., Teufel M., Musche V., Weismuller B., Kohler H., Hetkamp M., Dorrie N., Schweda A., Skoda E.M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health. 2020;42(4):672–678. doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly S.L., Stolzmann K.L., Heyworth L., Weaver K.R., Bauer M.S., Miller C.J. Rapid increase in telemental health within the department of veterans Affairs during the COVID-19 pandemic. Telemed. e-Health. 2020 doi: 10.1089/tmj.2020.0233. In press. [DOI] [PubMed] [Google Scholar]
- Ehrenreich-May J. 2020. Fear of Illness and Evaluation Scales. [Google Scholar]
- Freeman D., Loe B.S., Kingdon D., Startup H., Molodynski A., Rosebrock L., Brown P., Sheaves B., Waite F., Bird J.C. The revised Green et al., Paranoid Thoughts Scale (R-GPTS): psychometric properties, severity ranges, and clinical cut-offs. Psychol. Med. 2019:1–10. doi: 10.1017/S0033291719003155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S.H., Sewell D.R., Cooley E.L., Leavitt N. Assessing levels of adaptive functioning: the role functioning scale. Community Ment. Health J. 1993;29:119–131. doi: 10.1007/BF00756338. [DOI] [PubMed] [Google Scholar]
- Groarke J.M., Berry E., Graham-Wisener L., McKenna-Plumley P.E., McGlinchey E., Armour C. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 psychological wellbeing study. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyworth L., Kirsh S., Zulman D., Ferguson J.M., Kizer K.W. 2020. Expanding Access through Virtual Care: the VA's Early Experience with COVID-19. NEHM Catalyst: Innovations in Care Delivery. [Google Scholar]
- Jewell J.S., Farewell C.V., Welton-Mitchell C., Lee-Winn A., Walls J., Leiferman J.A. Mental health during the COVID-19 pandemic in the United States: online survey. JMIR Form. Res. 2020;4(10) doi: 10.2196/22043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia R., Ayling K., Chalder T., Massey A., Broadbent E., Coupland C., Vedhara K. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open. 2020;10(9) doi: 10.1136/bmjopen-2020-040620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatr. Res. 2020;290:113117. doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozloff N., Mulsant B.H., Stergiopoulos V., Voineskos A.N. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr. Bull. 2020;46(4):752–757. doi: 10.1093/schbul/sbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenth R., Buerkner P., Herve M., Love J., Riebl H., Singmann H. Emmeans: estimated marginal means. 2020. https://CRAN.R-project.org/package=emmeans
- Llerena K., Park S.G., McCarthy J.M., Couture S.M., Bennett M.E., Blanchard J.J. The Motivation and Pleasure Scale-Self-Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr. Psychiatr. 2013;54(5):568–574. doi: 10.1016/j.comppsych.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubben J., Gironda M., Lee A. The Behavioral Measurement Letter; 2002. Refinements to the Lubben Social Network Scale: the LSNS-R; pp. 2–11. [Google Scholar]
- McLellan A.T., Luborsky L., Woody G.E., O'Brien C.P. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J. Nerv. Ment. Dis. 1980;168(1):26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Montgomery S.A., Asberg M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Newby J.M., O'Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng E.Y., Lee M.B., Tsai S.T., Yang C.C., Morisky D.E., Tsai L.T., Weng Y.L., Lyu S.Y. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J. Formos. Med. Assoc. 2010;109(7):524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Russell D., Peplau L.A., Cutrona C.E. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J. Pers. Soc. Psychol. 1980;39(3):472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S.M.A., Mohammad D., Qureshi M.F.H., Abbas M.Z., Aleem S. Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community Ment. Health J. 2020;57(1):101–110. doi: 10.1007/s10597-020-00728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singmann H., Bolker B., Westfall J., Aust F., Ben-Shachar M.S. Afex: analysis of factorial experiments. 2020. https://CRAN.R-project.org/package=afex
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tsai J., El-Gabalawy R., Sledge W.H., Southwick S.M., Pietrzak R.H. Post-traumatic growth among veterans in the USA: results from the national health and resilience in Veterans study. Psychol. Med. 2015;45:165–179. doi: 10.1017/S0033291714001202. [DOI] [PubMed] [Google Scholar]
- Tsai, J., Huang, M., Elbogen, E., (in press). Mental Health and Psychosocial Characteristics Associated with COVID19 in US Adults. Psychiatric Services. [DOI] [PubMed]
- Tsai J., Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5(4):e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahia I.V., Jeste D.V., Reynolds C.F., 3rd Older adults and the mental health effects of COVID-19. J. Am. Med. Assoc. 2020;324(22):2253–2254. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response tot he H1N1 (Swine Flu) pandemic. Cognit. Ther. Res. 2012;36:210–218. [Google Scholar]
- Zortea T.C., Brenna C.T.A., Joyce M., McClelland H., Tippett M., Tran M.M., Arensman E., Corcoran P., Hatcher S., Heise M.J., Links P., O'Connor R.C., Edgar N.E., Cha Y., Guaiana G., Williamson E., Sinyor M., Platt S. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis. 2020:1–14. doi: 10.1027/0227-5910/a000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.