Abstract
Background
Performing elective orthopaedic surgery on patients with high BMI, poorly controlled hyperglycemia, and who use tobacco can lead to serious complications. Some surgeons use cutoffs for BMI, hemoglobin A1c, and cigarette smoking to limit surgery to patients with lower risk profiles rather than engaging in shared decision-making with patients about those factors. Other studies have suggested this practice may discriminate against people of lower income levels and women. However, the extent to which this practice approach is used by orthopaedic surgeons at leading hospitals is unknown.
Questions/purposes
(1) How often are preoperative cutoffs for hemoglobin A1c and BMI used at the top US orthopaedic institutions? (2) What services are available at the top orthopaedic institutions for weight loss, smoking cessation, and dental care? (3) What proportion of hospital-provided weight loss clinics, smoking cessation programs, and dental care clinics accept Medicaid insurance?
Methods
To investigate preoperative cutoffs for hemoglobin A1c and BMI and patient access to nonorthopaedic specialists at the top orthopaedic hospitals in the United States, we collected data on the top 50 orthopaedic hospitals in the United States as ranked by the 2020 US News and World Report’s “Best Hospitals for Orthopedics” list. We used a surgeon-targeted email survey to ascertain information regarding the use of preoperative cutoffs for hemoglobin A1c and BMI and availability and insurance acceptance policies of weight loss and dental clinics. Surgeons were informed that the survey was designed to assess how their institution manages preoperative risk management. The survey was sent to one practicing arthroplasty surgeon, the chair of the arthroplasty service, or department chair, whenever possible, at the top 50 orthopaedic institutions. Reminder emails were sent periodically to encourage participation from nonresponding institutions. We received survey responses from 70% (35 of 50) of hospitals regarding the use of preoperative hemoglobin A1c and BMI cutoffs. There was no difference in the response rate based on hospital ranking or hospital region. Fewer responses were received regarding the availability and Medicaid acceptance of weight loss and dental clinics. We used a “secret shopper” methodology (defined as when a researcher calls a facility pretending to be a patient seeking care) to gather information from hospitals directly. The use of deception in this study was approved by our institution’s institutional review board. We called the main telephone line at each institution and spoke with the telephone operator at each hospital asking standardized questions regarding the availability of medical or surgical weight loss clinics, smoking cessation programs, and dental clinics. When possible, researchers were referred directly to the relevant departments and asked phone receptionists if the clinic accepted Medicaid. We were able to contact every hospital using the main telephone number. Our first research question was answered using solely the surgeon survey responses. Our second and third research questions were addressed using a combination of the responses to the surgeon surveys and specific hospital telephone calls.
Results
Preoperative hemoglobin A1c cutoffs were used at 77% (27 of 35) of responding institutions and preoperative BMI cutoffs were used at 54% (19 of 35) of responding institutions. In the secret shopper portion of our study, we found that almost all the institutions (98% [49 of 50]) had a medical weight loss clinic, surgical weight loss clinic, or combined program. Regarding smoking cessation, 52% (26 of 50) referred patients to a specific department in their institution and 18% (9 of 50) referred to a state-run smoking cessation hotline. Thirty percent (15 of 50) did not offer any internal resource or external referral for smoking cessation. Regarding dental care, 48% (24 of 50) of institutions had a dental clinic that performed presurgical check-ups and 46% (23 of 50) did not offer any internal resource or external referral for dental care. In the secret shopper portion of our study, for institutions that had internal resources, we found that 86% (42 of 49) of weight loss clinics, 88% (23 of 26) of smoking cessation programs, and 58% (14 of 24) of dental clinics accepted Medicaid insurance.
Conclusion
Proceeding with TJA may not be the best option for all patients; however, surgeons and patients should come to this consensus together after a thoughtful discussion of the risks and benefits for that particular patient. Future research should focus on how shared decision-making may influence patient satisfaction and a patient’s ability to meet preoperative goals related to weight loss, glycemic control, smoking cessation, and dental care. Decision analyses or time trade-off analyses could be implemented in these studies to assess patients’ tolerance for risk.
Clinical Relevance
Orthopaedic surgeons should engage in shared decision-making with patients to develop realistic goals for weight loss, glycemic control, smoking cessation, and dental care that consider patient access to these services as well as the difficulties patients experience in losing weight, controlling blood glucose, and stopping smoking.
Introduction
Given that performing elective orthopaedic surgery on patients with high BMI, poorly controlled hyperglycemia, and tobacco use can lead to serious complications [2, 15, 20, 23], some surgeons use cutoffs for BMI, hemoglobin A1c, and cigarette smoking to limit surgery to patients with lower risk profiles rather than engaging in shared decision-making with patients about those factors [1, 4, 5, 7, 8, 11, 18, 19, 21, 22, 24]. Many of these cutoffs are applied in the context of preoperative risk management programs that are implemented by orthopaedic surgeons before total joint arthroplasty (TJA). Multiple studies have demonstrated that the utilization of preoperative risk management programs is associated with reduced readmissions, emergency department visits, and costs [1, 5, 11]. However, the use of cutoffs may contribute to disparities in care for Black and Hispanic patients, patients with lower incomes, and patients with Medicaid insurance [13, 29]. Enforcing strict preoperative cutoffs is especially concerning if orthopaedic programs do not provide patients with the necessary resources to achieve changes in weight, diabetes management, or smoking cessation. Additionally, these programs often recommend referrals to other specialists such as nutritionists, bariatric surgeons, cardiologists, dentists, and endocrinologists [4, 5, 11, 21, 24], but only one of these studies [21] reported information regarding the success of their referrals to these specialists.
Strict preoperative cutoffs and limited access to nonorthopaedic specialty care are two potential barriers for patients seeking TJA. However, little is known about the extent of preoperative cutoff use in orthopaedic practice and patient access to nonorthopaedic specialty care.
To investigate the use of preoperative cutoffs in TJA practice and patient access to nonorthopaedic specialty care, we performed a three-part study to answer the following questions: (1) How often are preoperative cutoffs for hemoglobin A1c and BMI used at the top US orthopaedic institutions? (2) What services are available at the top orthopaedic institutions for weight loss, smoking cessation, and dental care? (3) What proportion of hospital-provided weight loss clinics, smoking cessation programs, and dental care clinics accept Medicaid insurance?
Materials and Methods
Study Design
To investigate preoperative cutoffs for hemoglobin A1c and BMI and patient access to nonorthopaedic specialists for the top orthopaedic hospitals, we focused on the top 50 orthopaedic hospitals in the United States as ranked by the 2020 US News and World Report’s “Best Hospitals for Orthopedics” list [27]. We used a surgeon-targeted email survey to ascertain information regarding the use of preoperative cutoffs for hemoglobin A1c and BMI and the availability and insurance acceptance policies of weight loss and dental clinics (Supplementary Fig. 1; http://links.lww.com/CORR/A869). The survey directly asked questions regarding the use of preoperative cutoffs for hemoglobin A1c and BMI and the value of these cutoffs. Further questions were asked regarding the availability and Medicaid acceptance policies of nutrition clinics, bariatric surgery clinics, metabolic weight loss clinics, and dental clinics at the surgeon’s institution. Weight loss and dental care were chosen as these both have differential insurance coverage policies that may limit patient access to these services. We believe that our survey was designed to adequately assess our primary and secondary research questions given that it directly posed these questions to the surgeon. Surgeons were informed that the survey was designed to assess how their institution addresses preoperative risk management and were able to answer with “unsure” if they were unsure of the answer to a specific question. There was no time limit for the survey response, and surgeons could choose which questions they wanted to answer because no questions required a response. The survey was sent to one practicing arthroplasty surgeon, the chair of the arthroplasty service, or department chair, whenever possible, at the top 50 orthopaedic institutions. Reminder emails were sent periodically to encourage participation from nonresponding institutions.
Because individual surgeons may not have complete knowledge regarding the nonorthopaedic services provided at their institution, we also implemented a second arm of the study to reflect the patient experience more closely. We used a “secret shopper” methodology (defined as when a researcher calls a facility pretending to be a patient seeking care) to gather information from hospitals directly. The use of deception in this study was approved by our institution’s institutional review board (IRB). We called the main telephone line at each institution and spoke with the telephone operator at each asking standardized questions regarding the availability of medical or surgical weight loss clinics, smoking cessation programs, and dental clinics (Supplementary Fig. 2; http://links.lww.com/CORR/A868). When possible, researchers were referred directly to the relevant departments and asked phone receptionists if the clinic accepted Medicaid.
Our first research question was answered using solely the surgeon survey responses. Our second and third research questions were addressed using a combination of the responses to the surgeon surveys and specific hospital telephone calls. The surgeon survey data were collected between October and December 2021, and the secret shopper data were collected between June and November 2021.
Participants
We emailed the chiefs of the joint reconstruction service at each institution using their contact information in the American Association of Hip and Knee Surgeons membership directory. If this individual did not respond, we randomly contacted another arthroplasty surgeon at the institution. We received survey responses from 70% (35 of 50) of the hospitals regarding the use of preoperative hemoglobin A1c and BMI cutoffs. We received fewer responses regarding the availability and Medicaid acceptance of weight loss and dental clinics. We received fewer responses to the questions regarding availability of nutrition clinics (66% [33 of 50]), bariatric surgery clinics (66% [33 of 50]), metabolic weight loss clinics (64% [32 of 50]), and dental clinics (64% [32 of 50]). We received responses from 56% (28 of 50) of surgeons regarding Medicaid acceptance at nutrition clinics, 54% (27 of 50) for bariatric surgery clinics, and 46% (23 of 50) for metabolic weight loss clinics. We received responses from 28% (14 of 50) of surgeons regarding Medicaid acceptance and the provision of free care at dental clinics.
For the institution-specific telephone calls, we called the main telephone line of each hospital, and we used a standardized script to ask questions regarding access to nonorthopaedic specialists using a secret shopper format (Supplementary Fig. 2; http://links.lww.com/CORR/A868) [30]. Researchers were observed by the study principal investigator when making the initial calls to ensure that the script was followed. If additional information regarding a specific department was provided by the telephone operator, the caller attempted to contact the department directly to ask standardized questions regarding insurance acceptance policies. We were able to contact every hospital using the main telephone number and directly ask the telephone operator if the institution had weight loss clinics, smoking cessation services, and dental clinics.
Nonresponder Analysis
For the surgeon-targeted email survey, there was no difference in response frequency when considering hospital rank (top half of institutions versus bottom half of institutions) or region (Northeast, Midwest, South, West) for all survey questions (Supplementary Table 1; http://links.lww.com/CORR/A867). We used chi-square analyses in Stata Version 16.1 (StataCorp) to assess for differences in response frequency. A p value greater than 0.05 was considered nonsignificant.
We obtained responses from all 50 institutions for the secret shopper portion of the study.
Primary and Secondary Study Outcomes
Our primary study goal was to determine how frequently preoperative cutoffs for hemoglobin A1c and BMI were used at the top orthopaedic institutions. To achieve this, we utilized a surgeon-targeted email survey that directly asked about the use of these cutoffs and their values.
Our secondary study goals were to characterize the availability of nutrition, bariatric surgery, metabolic weight loss, and dental clinics and the Medicaid acceptance policies of these clinics. We utilized both the surgeon-targeted email survey and secret shopper methodology to ask either the surgeon directly or the telephone operator directly about the availability of nutrition, bariatric surgery, metabolic weight loss, and dental clinics. To obtain information about the Medicaid acceptance policies of these clinics, we either asked the surgeon directly or asked the telephone operator to transfer the researcher to the appropriate clinic to ask the receptionist at the clinic. Another secondary study goal was to determine the availability of smoking cessation resources and the Medicaid acceptance policies for these resources. Smoking cessation resource availability and Medicaid acceptance was solely assessed using a secret shopper methodology where a researcher asked the telephone operator about the availability of smoking cessation resources and then asked to be transferred to the appropriate department to ask the receptionist if the clinic accepted Medicaid.
Ethical Approval
Our IRB granted an exemption for the survey and secret shopper portions of our study. Surgeons were informed regarding the purpose of the survey and were provided an information sheet with additional details describing the study. The IRB granted an exemption for the secret shopper portion of the study because they agreed that deception was necessary to obtain information from each institution. If telephone operators and clinic receptionists were aware that they were providing information for a research study, their responses might be different than those they would normally provide to a patient. To best replicate the patient experience, deception was explicitly permitted in this study by our institution’s IRB.
Results
Preoperative Cutoffs for Hemoglobin A1c and BMI
Preoperative hemoglobin A1c cutoffs were used at 77% (27 of 35) of responding institutions, and the most common cutoff among institutions with cutoffs was a hemoglobin A1c level of less than 8% (74% [20 of 27]). Nine percent (3 of 35) of responding institutions indicated they had soft cutoffs for hemoglobin A1c, with a recommended value of less than 8%. Fourteen percent (5 of 35) of responding institutions did not have a preoperative hemoglobin A1c cutoff. Most responding institutions also used preoperative BMI cutoffs (54% [19 of 35]) ranging from BMI < 35 kg/m2 to BMI < 50 kg/m2. The most common BMI cutoff among institutions with cutoffs was BMI < 40 kg/m2 (at 79% [15 of 19] of institutions). Fourteen percent (5 of 35) of responding institutions had soft cutoffs for BMI, with four recommending a BMI < 40 kg/m2 and one recommending a BMI less than 40 to 45 kg/m2. Thirty-one percent (11 of 35) of responding institutions did not endorse preoperative BMI cutoffs.
Services Available for Weight Loss, Smoking Cessation, and Dental Care
Weight Loss
In our survey, 91% (30 of 33) of responding surgeons reported their institutions had nutrition clinics, 91% (30 of 33) reported their institutions had bariatric surgery clinics, and 75% (24 of 32) indicated their institutions had metabolic weight loss clinics.
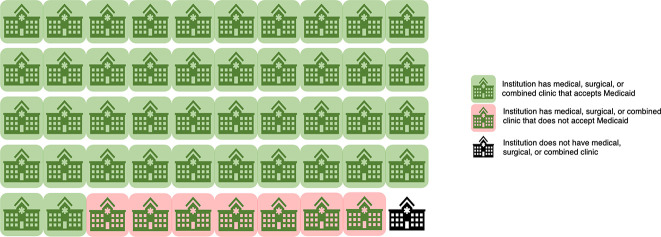
Through the secret shopper calls, we found that almost all institutions (98% [49 of 50]) had either a medical weight loss clinic, surgical weight loss clinic, or combined program (Fig. 1). Some institutions had separate medical and surgical weight loss clinics. One hospital did not have a weight loss clinic nor an affiliated center to refer patients to for care.
Fig. 1.
This figure shows medical, surgical, and combined medical and surgical weight loss clinic availability and Medicaid acceptance at the top orthopaedic institutions in the United States.
Smoking Cessation
After calling each hospital to inquire about smoking cessation resources, we found that 52% (26 of 50) of institutions referred patients to a specific department in their institution, and 18% (9 of 50) of institutions referred to a resource outside their hospital such as a state-run smoking cessation hotline. Thirty percent (15 of 50) did not have a specific department or an outside resource (Fig. 2).
Fig. 2.
This figure shows smoking cessation resource availability and Medicaid acceptance at the top orthopaedic institutions in the United States.
Dental Care
Of the surgeons who provided information about dental care through our survey, 41% (13 of 32) of institutions had a dental clinic, 56% (18 of 32) did not have a dental clinic, and 3% (1 of 32) were unsure about the presence of a dental clinic.
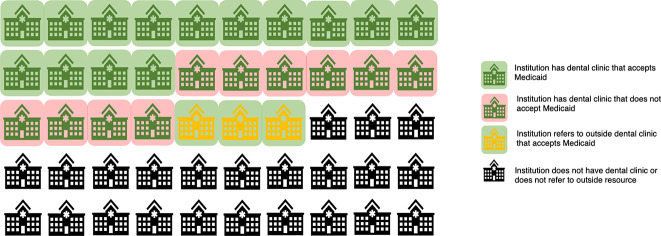
After calling each hospital and inquiring about dental care, we found that 48% (24 of 50) had a dental clinic that could perform presurgical check-ups for adults, and 6% (3 of 50) provided referral information about outside resources. Forty-six percent (23 of 50) were not able to provide a referral to an outside resource or a specific department (Fig. 3).
Fig. 3.
This figure shows dental clinic availability and Medicaid acceptance at the top orthopaedic institutions in the United States.
Medicaid Acceptance Policies for Weight Loss, Smoking Cessation, and Dental Clinics
Weight Loss
For institutions with nutrition clinics and surgeons who provided information about Medicaid acceptance through our survey, 4% (1 of 28) did not accept Medicaid, 54% (15 of 28) accepted Medicaid, and 43% (12 of 28) were unsure about Medicaid acceptance. Of institutions that had bariatric surgery clinics and provided information about Medicaid acceptance, 7% (2 of 27) did not accept Medicaid, 63% (17 of 27) accepted Medicaid, and 30% (8 of 27) were unsure about Medicaid acceptance. Of those that had metabolic medical management clinics and provided information about Medicaid acceptance for these clinics, 4% (1 of 23) did not accept Medicaid, 48% (11 of 23) accepted Medicaid, and 40% (11 of 23) were unsure about Medicaid acceptance.
From the secret shopper portion of our study, we found that 86% (42 of 49) of institutions with weight loss clinics had at least one type of weight loss clinic that accepted Medicaid (Fig. 1). When considering individual clinic types, 76% (16 of 21) of institutions with metabolic weight loss clinics accepted Medicaid and 100% (21 of 21) accepted private insurance; 95% (18 of 19) of institutions with surgical weight loss clinics accepted Medicaid and 100% (19 of 19) accepted private insurance. At institutions with combined medical and surgical clinics, 75% (12 of 16) accepted Medicaid and 100% (16 of 16) accepted private insurance.
Smoking Cessation
Our calls to the telephone operator found that 88% (23 of 26) of institutions with internal smoking cessation clinics accepted Medicaid and 100% (26 of 26) accepted private insurance (Fig. 2). Thirty-six percent (18 of 50) of institutions either did not provide patients with any smoking cessation resources or did not provide patients with Medicaid access to their internal smoking cessation clinics.
Dental Care
For the 13 institutions at which surgeons indicated they had dental clinics and who provided information about Medicaid acceptance through our survey, 11 accepted Medicaid, seven offered free care, two were unsure about Medicaid acceptance, and five were unsure about the provision of free care. One surgeon stated that the dental clinic at their institution did not provide free care for patients.
In the secret shopper portion of our study, we found that 58% (14 of 24) of institutions which had dental clinics that performed presurgical check-ups for adults accepted Medicaid. The three institutions that provided outside referrals all referred patients to clinics that accepted Medicaid (Fig. 3). Combining the institutions that did not provide patients with any dental clinic resources and internal dental clinics that did not accept Medicaid, 66% (33 of 50) of institutions did not provide patients with Medicaid resources for dental care before proceeding with TJA.
Discussion
Serious complications can result from performing elective orthopaedic surgery on patients with comorbidities such as poorly controlled diabetes or morbid obesity. Rather than engage in shared decision-making with patients regarding these risk factors, some surgeons may utilize cutoffs for BMI, hemoglobin A1c, and cigarette smoking to limit surgery for patients. Our study sought to understand the use of preoperative cutoffs as well as access to weight loss, smoking cessation, and dental care services for patients considering TJA. We found that most of the responding top orthopaedic institutions use preoperative cutoffs for hemoglobin A1c (77% [27 of 35]) and BMI (54% [19 of 35]). Although many institutions have services for assistance with weight loss, services that assist with smoking cessation and dental care were less available. Orthopaedic surgeons should engage in shared decision-making with patients to develop realistic and attainable goals for weight loss, glycemic control, smoking cessation, and dental care that consider patient access to these services as well as the inherent challenges patients face when attempting to lose weight, control blood glucose, or stop smoking.
Limitations
This study has limitations. First, in our surgeon survey, 30% (15 of 50) of those surveyed did not respond. There was no difference between the responders and nonresponders based on hospital ranking or hospital region, thus we believe that our findings are applicable to the top orthopaedic institutions overall. Second, for the secret shopper portion of our study, it is possible that on any given day, a specific operator would provide different information than another operator at the same institution. However, we were able to compare the results of the secret shopper portion of our study with the survey portion, and we found that the telephone operators provided similar information when compared with the surgeons at each institution. Although there were some differences between the surgeon responses and telephone operator responses, we believe that this reveals some of the uncertainty patients may face when attempting to access these services and that by including the data from both the survey and secret shopper portions of the study, we provide a more complete picture of the available services and their accessibility for patients with Medicaid. In addition, we believe that the format of our study best reflects a patient’s experience by replicating how they would seek information, and as such, possible differences in the information provided would be acceptable as they are a realistic representation of what a patient might experience when attempting to access services at a specific institution.
Preoperative Cutoffs for Hemoglobin A1c and BMI
We found that preoperative cutoffs for hemoglobin A1c and BMI were widely used at the top orthopaedic institutions. Many preoperative risk management programs include the use of preoperative goals for hemoglobin A1c and BMI [10]; however, as was shown in a modeling study, the use of strict preoperative cutoffs may lead to reduced access for patients from racial and ethnic minority backgrounds, women, and patients with lower incomes [29]. Although few would question whether patients with lower BMIs or improved glycemic control are at a lower risk of a prosthetic joint infection after TJA, substantial, sustained weight loss is possible only in a small minority of patients, and large improvements in glycemic control are not easy to achieve for many patients [13]. Orthopaedic surgeons should engage in shared decision-making discussions with patients, and they should set goals for realistic improvements in BMI and glycemic control. Surgeons should acknowledge the progress patients make with regard to weight loss and blood glucose levels and when goals are met, proceed with surgery even if patients do not meet preconceived cutoffs. If the surgeon and patient come to a shared decision that TJA would not be feasible due to elevated risk, then the surgeon should support the patient in pursuing other treatment options such as steroid injections, physical therapy, and NSAIDs, as indicated. Follow-up studies that assess postoperative readmissions, emergency department visits, and complication frequency as well as patient satisfaction when patients engage in shared decision-making regarding proceeding with elective surgery should be performed to evaluate the impact of more modest improvements in weight loss and glycemic control. Research studies that include decision analyses or time trade-off analyses may be useful to assess patient risk tolerance and may assist with future shared decision-making discussions.
Services Available for Weight Loss, Smoking Cessation, and Dental Care
Preoperative risk management programs often make recommendations that patients lose weight, stop smoking, or receive preoperative dental care [4, 5, 11, 21, 24]. However, limited research has been done on how often patients are referred to weight loss, smoking cessation, and dental care specialists. One study [21] found that only 34% of patients for whom specialist care was recommended received that care. Patient access to services for nonoperative weight loss and weight loss surgery can be limited by insurance coverage and access to a regular healthcare provider [16, 25]. Smoking cessation efforts have improved over time, but fewer than one-third of current smokers older than 18 years use counseling or medication to aid in smoking cessation efforts [28]. Consistent access to and use of dental care is limited, especially given the narrow scope of care reimbursed by Medicare and Medicaid [9, 17]. Our study found that although many of the top orthopaedic institutions provide services for weight loss, only half also provide services for smoking cessation and dental care. Given these barriers to access, understanding the resources available to patients receiving orthopaedic care and needing access to weight loss services, smoking cessation programs, or dental clinics is essential to ensure that patients are receiving equitable care so they are considered eligible for surgery. Orthopaedic surgeons should advocate within their institutions to create pathways for patients to access weight loss, smoking cessation, and dental care services. Although patients may seek care outside of a surgeon’s institution, services provided within the same hospital system may allow for improved care coordination and facilitate patient access to these services. In addition, surgeons should discuss potential barriers to care directly with patients when engaging in shared decision-making discussions so that reasonable goals can be developed that incorporate these barriers. When considering solutions at the insurance-provider level, we believe similar incentives should be presented for preoperative risk management strategies like those offered for improvements in readmissions, emergency department visits, and length of stay.
Medicaid Acceptance Policies for Weight Loss, Smoking Cessation, and Dental Clinics
Weight Loss
Regarding weight management, we found that most of the institutions had at least one weight loss clinic that accepted Medicaid insurance. However, the availability of weight loss services alone is insufficient to ensure that patients can meet preoperative BMI cutoffs. Many patients have difficulty maintaining weight loss even when engaging in treatment modalities [6, 12]. Orthopaedic surgeons must collaborate with their colleagues in weight management specialties to either ensure that patients can meet the preoperative BMI cutoffs they enforce or support patients in their efforts to meet more realistic goals. Surgeons should engage in shared decision-making to discuss what resources are available for weight loss and what would be an attainable weight loss goal that allows the surgeon to operate safely. In addition, surgeons must have frank discussions with patients regarding the risks of proceeding with surgery and what would be necessary if the patient develops an infection or requires a revision procedure as well as the risks of limb loss or loss of independent movement. If the surgeon does not feel that a patient can safely proceed with the surgery, then the surgeon should discuss other treatment options with the patient or refer to a colleague who may have different thresholds when considering TJA.
Smoking Cessation
Regarding smoking cessation, we found that 36% (18 of 50) of institutions either had smoking cessation clinics that did not accept Medicaid or did not provide any smoking cessation resources to patients. Smoking cessation is challenging for any patient; however, patients with lower incomes may experience additional difficulties [14]. Medicaid insurance compared with non-Medicaid insurance has been associated with a decreased likelihood of using medication to aid in smoking cessation and reduced social support to quit smoking [3]. Access to smoking cessation services does not guarantee that patients will access these services or be successful in reducing smoking. Given this, surgeons must acknowledge that smoking cessation may not be feasible for every patient. If the patient and surgeon come to a consensus that complete cessation will not be possible, the surgeon must consider if they are comfortable proceeding with surgery if the patient is only able to reduce instead of completely stop smoking. Alternatively, through a shared decision-making process, the patient and surgeon may decide that even reduction in smoking is not possible, and the patient may benefit more from nonoperative treatment modalities for osteoarthritis.
Dental Care
Dental care is a less common component of preoperative risk management programs. However, it can still be a barrier for patients seeking TJA care. Our study found that a high proportion of institutions (66% [33 of 50]) do not provide patients with Medicaid with resources to receive dental care. Even at dental clinics that accept Medicaid, cost may be a challenge because many state Medicaid programs do not cover dental services for adults [17]. Additionally, even with expanded Medicaid access to dental services, use of dental care is still limited for patients with lower incomes [26]. Again, shared decision-making is needed so that the patient and surgeon can discuss the risks of proceeding with an elective arthroplasty if the patient has an active dental infection or is at a high risk for a dental infection. If a patient is unable to access dental care, we believe the surgeon should collaborate with colleagues to determine whether there are locations that would provide free or sliding-scale services.
Conclusion
Preoperative cutoffs are widely used at the top orthopaedic institutions, and most implemented preoperative cutoffs for hemoglobin A1c and BMI. Additionally, although medical and surgical weight loss clinics are widely available, the availability of smoking cessation programs and dental clinics is more limited at these institutions, as are the Medicaid acceptance policies for smoking cessation and dental services. Orthopaedic surgeons should engage in shared decision-making with patients to develop realistic goals for weight loss, glycemic control, smoking cessation, and dental care that consider patient access to these services as well as the difficulties patients experience in losing weight, controlling blood glucose, and stopping smoking. Proceeding with TJA may not be the best option for all patients; however, surgeons and patients should come to this consensus together after a thoughtful discussion of the risks and benefits for that particular patient. Future research should focus on how shared decision-making may influence patient satisfaction and a patient’s ability to meet preoperative goals related to weight loss, glycemic control, smoking cessation, and dental care. Decision analyses or time trade-off analyses could be implemented in these studies to assess patients’ tolerance for risk. In addition, research studies that investigate how orthopaedic surgeons can implement preoperative risk management programs that are sensitive to potential barriers to care such as access and insurance acceptance policies for patients who have comorbid conditions should be pursued.
Acknowledgement
We thank Annie Chen BS for her assistance with data collection.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
This study was deemed exempt from institutional review board approval by Yale University, New Haven, CT, USA (numbers 2000025429 and 2000031322).
Contributor Information
Tanner Metcalfe, Email: tanner.metcalfe@yale.edu.
Sanjana Jain, Email: sanjanajainct@gmail.com.
Anchal Bahel, Email: bahelan23@amityschools.org.
Claire A. Donnelley, Email: claire.donnelley@yale.edu.
Daniel H. Wiznia, Email: daniel.wiznia@yale.edu.
References
- 1.Bernstein DN, Liu TC, Winegar AL, et al. Evaluation of a preoperative optimization protocol for primary hip and knee arthroplasty patients. J Arthroplasty. 2018;33:3642-3648. [DOI] [PubMed] [Google Scholar]
- 2.Boyce L, Prasad A, Barrett M, et al. The outcomes of total knee arthroplasty in morbidly obese patients: a systematic review of the literature. Arch Orthop Trauma Surg. 2019;139:553-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brady BR, O'Connor PA, Martz MP, Grogg T, Nair US. Medicaid-insured client characteristics and quit outcomes at the Arizona smokers' helpline. J Behav Health Serv Res. 2022;49:61-75. [DOI] [PubMed] [Google Scholar]
- 4.Bullock MW, Brown ML, Bracey DN, Langfitt MK, Shields JS, Lang JE. A bundle protocol to reduce the incidence of periprosthetic joint infections after total joint arthroplasty: a single-center experience. J Arthroplasty. 2017;32:1067-1073. [DOI] [PubMed] [Google Scholar]
- 5.Dlott CC, Moore A, Nelson C, et al. Preoperative risk factor optimization lowers hospital length of stay and postoperative emergency department visits in primary total hip and knee arthroplasty patients. J Arthroplasty. 2020;35:1508-1515.e1502. [DOI] [PubMed] [Google Scholar]
- 6.Evans EH, Sainsbury K, Marques MM, et al. Prevalence and predictors of weight loss maintenance: a retrospective population-based survey of european adults with overweight and obesity. J Hum Nutr Diet. 2019;32:745-753. [DOI] [PubMed] [Google Scholar]
- 7.Featherall J, Brigati DP, Arney AN, et al. Effects of a total knee arthroplasty care pathway on cost, quality, and patient experience: toward measuring the triple aim. J Arthroplasty. 2019;34:2561-2568. [DOI] [PubMed] [Google Scholar]
- 8.Featherall J, Brigati DP, Faour M, Messner W, Higuera CA. Implementation of a total hip arthroplasty care pathway at a high-volume health system: effect on length of stay, discharge disposition, and 90-day complications. J Arthroplasty. 2018;33:1675-1680. [DOI] [PubMed] [Google Scholar]
- 9.Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102:411-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johns WL, Layon D, Golladay GJ, Kates SL, Scott M, Patel NK. Preoperative risk factor screening protocols in total joint arthroplasty: a systematic review. J Arthroplasty. 2020;35:3353-3363. [DOI] [PubMed] [Google Scholar]
- 11.Kim KY, Anoushiravani AA, Chen KK, et al. Perioperative orthopedic surgical home: optimizing total joint arthroplasty candidates and preventing readmission. J Arthroplasty. 2019;34:S91-S96. [DOI] [PubMed] [Google Scholar]
- 12.Kraschnewski JL, Boan J, Esposito J, et al. Long-term weight loss maintenance in the United States. Int J Obes (Lond). 2010;34:1644-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leopold SS. Editorial: The shortcomings and harms of using hard cutoffs for BMI, hemoglobin a1c, and smoking cessation as conditions for elective orthopaedic surgery. Clin Orthop Relat Res. 2019;477:2391-2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leventhal AM, Bello MS, Galstyan E, Higgins ST, Barrington-Trimis JL. Association of cumulative socioeconomic and health-related disadvantage with disparities in smoking prevalence in the United States, 2008 to 2017. JAMA Intern Med. 2019;179:777-785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marchant MH, Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am. 2009;91:1621-1629. [DOI] [PubMed] [Google Scholar]
- 16.Nelson HD, Cantor A, Wagner J, et al. AHRQ Comparative Effectiveness Reviews. Achieving Health Equity in Preventive Services. Agency for Healthcare Research and Quality; 2019. [PubMed] [Google Scholar]
- 17.Northridge ME, Kumar A, Kaur R. Disparities in access to oral health care. Annu Rev Public Health. 2020;41:513-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nussenbaum FD, Rodriguez-Quintana D, Fish SM, Green DM, Cahill CW. Implementation of preoperative screening criteria lowers infection and complication rates following elective total hip arthroplasty and total knee arthroplasty in a veteran population. J Arthroplasty. 2018;33:10-13. [DOI] [PubMed] [Google Scholar]
- 19.Plate JF, Ryan SP, Black CS, et al. No changes in patient selection and value-based metrics for total hip arthroplasty after comprehensive care for joint replacement bundle implementation at a single center. J Arthroplasty. 2019;34:1581-1584. [DOI] [PubMed] [Google Scholar]
- 20.Podmore B, Hutchings A, van der Meulen J, Aggarwal A, Konan S. Impact of comorbid conditions on outcomes of hip and knee replacement surgery: a systematic review and meta-analysis. BMJ Open. 2018;8:e021784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryan SP, Howell CB, Wellman SS, et al. Preoperative optimization checklists within the comprehensive care for joint replacement bundle have not decreased hospital returns for total knee arthroplasty. J Arthroplasty. 2019;34:S108-S113. [DOI] [PubMed] [Google Scholar]
- 22.Ryan SP, Plate JF, Black CS, et al. Value-based care has not resulted in biased patient selection: analysis of a single center's experience in the care for joint replacement bundle. J Arthroplasty. 2019;34:1872-1875. [DOI] [PubMed] [Google Scholar]
- 23.Sahota S, Lovecchio F, Harold RE, Beal MD, Manning DW. The effect of smoking on thirty-day postoperative complications after total joint arthroplasty: a propensity score-matched analysis. J Arthroplasty. 2018;33:30-35. [DOI] [PubMed] [Google Scholar]
- 24.Schultz BJ, Segovia N, Castillo TN. Successful implementation of an accelerated recovery and outpatient total joint arthroplasty program at a county hospital. J Am Acad Orthop Surg Glob Res Rev. 2019;3:e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shikora SA, Kruger RS, Jr, Blackburn GL, et al. Best practices in policy and access (coding and reimbursement) for weight loss surgery. Obesity (Silver Spring). 2009;17:918-923. [DOI] [PubMed] [Google Scholar]
- 26.Singhal A, Damiano P, Sabik L. Medicaid adult dental benefits increase use of dental care, but impact of expansion on dental services use was mixed. Health Affairs. 2017;36:723-732. [DOI] [PubMed] [Google Scholar]
- 27.U.S. News & World Report. Best hospitals for orthopedics. Available at: https://health.usnews.com/best-hospitals/rankings/orthopedics. Accessed June 22, 2021.
- 28.United States Public Health Service Office of the Surgeon G, National Center for Chronic Disease P, Health Promotion Office on S, Health. Publications and reports of the surgeon general. Smoking Cessation: A Report of the Surgeon General. US Department of Health and Human Services; 2020. [Google Scholar]
- 29.Wang AY, Wong MS, Humbyrd CJ. Eligibility criteria for lower extremity joint replacement may worsen racial and socioeconomic disparities. Clin Orthop Relat Res. 2018;476:2301-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yousman LC, Hsiang WR, Jin G, et al. Musculoskeletal urgent care centers restrict access for patients with medicaid insurance based on policy and location. Clin Orthop Relat Res. 2021;479:2447-2453. [DOI] [PMC free article] [PubMed] [Google Scholar]