Since John Tebbets described the dual-plane technique,1 the use of a submuscular pocket for breast implants has become increasingly popular among plastic surgeons. Over the years, the vast number of publications has revealed the continuous pursuit of reliable implant stability. Particularly in times where the use of textured surface implants is controversial, this theme is of utmost importance.
We currently use an approach that creates a modified submuscular pocket where the implant is supported by an inferolateral muscular sling.2 When using smooth implants, we currently prefer a double sling (inferolateral + inferomedial) pocket.
When dealing with nonprimary surgery and subglandular to submuscular pocket change, we follow a sequence that combines the pectoralis major and the existing implant capsule to create a new submuscular pocket.3 In cases where the pectoralis major is atrophic due to previous subglandular implant pressure and/or the posterior capsule is poorly expandable, the volume of the new implant may be severely limited and the risk of muscle rupture increased. However, in such cases, a solution that we refer to as “pocket expansion” creates adequate room for the new implant and helps to prevent pectoralis rupture.
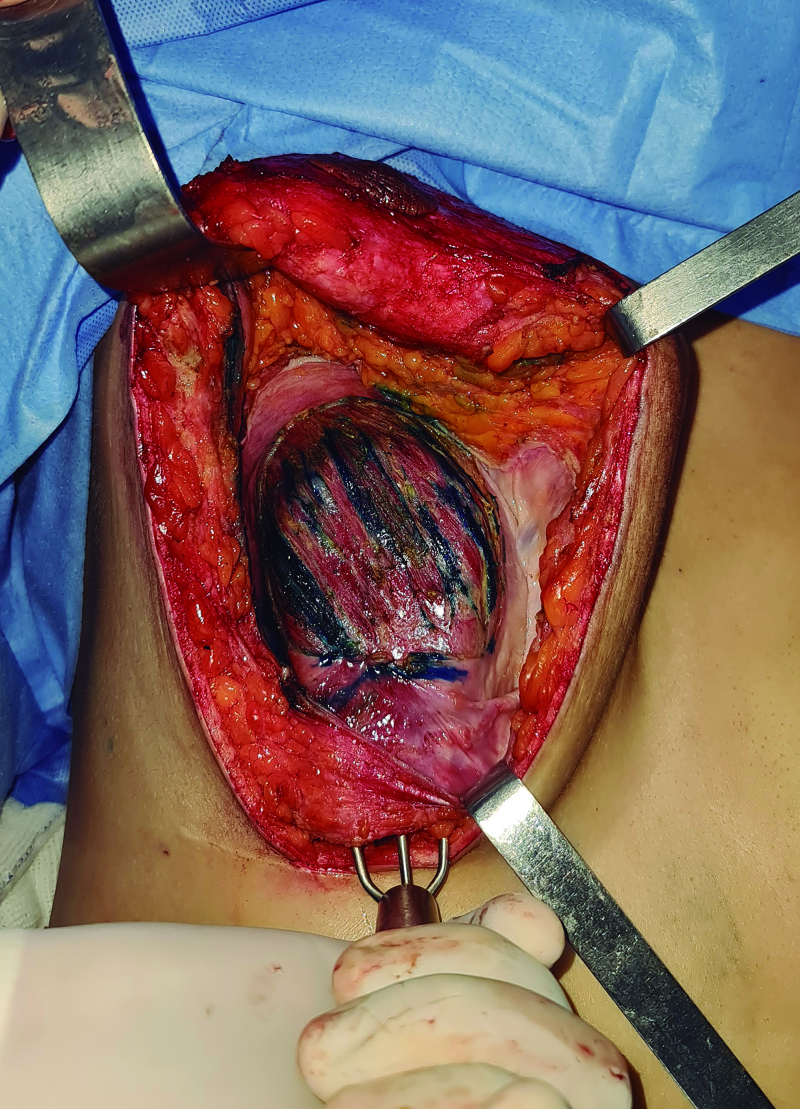
The procedure begins with resection of the posterior capsule in the area where expansion is desired. Split-thickness myotomies are then performed, respecting the orientation of the pectoralis major fibers. A retractor pulled up in the submuscular pocket verifies adequate expansion (Fig. 1). A part of the resected anterior capsule is sutured as a patch overlying the pectoralis muscle beyond the area of the myotomies; the outer surface of the capsule faces the muscle, preventing the previous luminal surface from being in contact with the new implants in case the muscle tears. The maximum amount of expansion is limited according to the size of the anterior capsule patch.
Fig. 1.
A retractor pulled up in the submuscular pocket verifies adequate expansion.
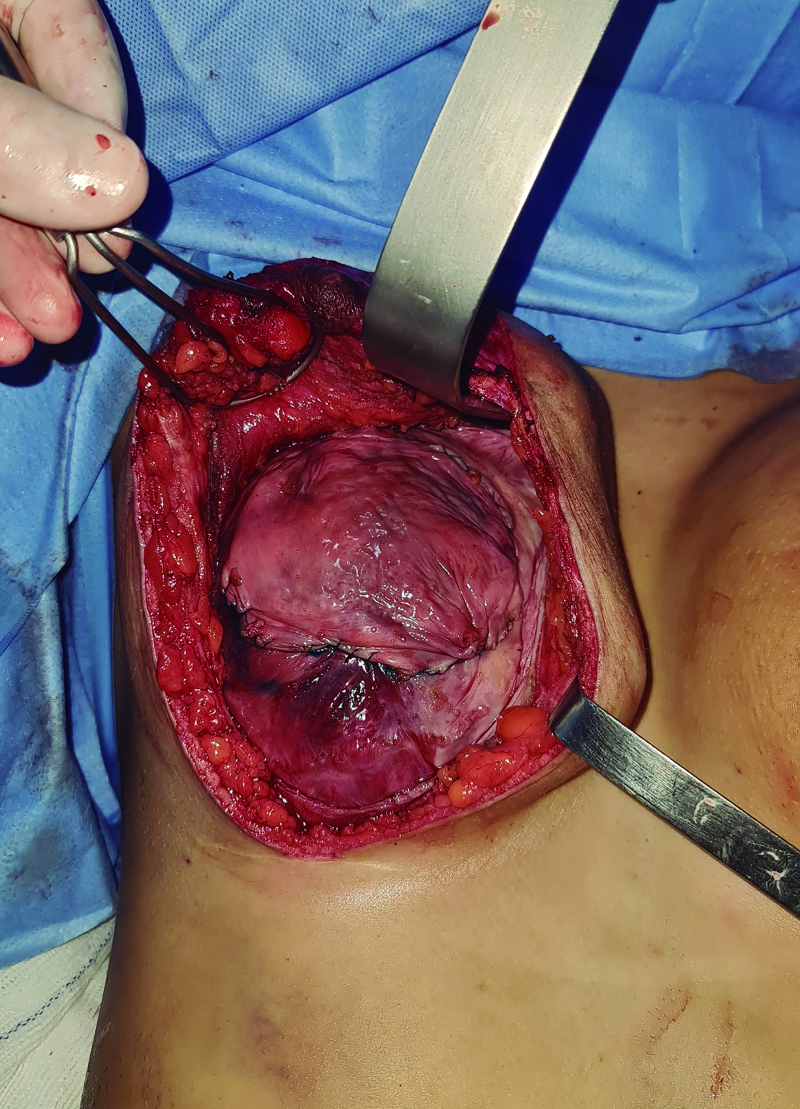
Thus, the submuscular pocket can be expanded up to the desired volume. Also, in the event of a muscular full-thickness tear, the patch will keep the submuscular pocket sealed (safety pocket) (Fig. 2). This strategy helps prevent uncontrolled muscular rupture at regions difficult to repair. (See Video 1 [online], which displays the main steps of the pocket expansion technique.)
Fig. 2.
Implants in the submuscular pocket; capsular patch placed.
Video. This video displays the main steps of pocket expansion technique.
Considering that the capsules are either acellular or have a low cell density4 and that dermal matrix grafts are high-priced, this may be a viable alternative. Regarding the pre-existing capsule, the literature shows no consensus on the outcomes of capsulectomy versus capsulotomy in the prevention or recurrence of diseases related to breast implants.5 Obviously, any indication for total capsulectomy precludes the technique.
We have carried out 32 cases, using smooth implants between 220 and 430 ml (average of 350 ml), with the most recent follow-up being 4 months and the later being 14 months (average of 10 months). The pocket expansion is a useful tool in subglandular to submuscular pocket change, especially when medium-to-large-sized and more projected implants are desired. Although no complications have been reported so far, a longer follow-up period is needed to assess stability and potential long-term complications.
Footnotes
Published online 13 December 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107:1255–1272. [DOI] [PubMed] [Google Scholar]
- 2.Ono MT, Karner BM. Four-step augmentation mastopexy: lift and augmentation at single time (LAST). Plast Reconstr Surg Glob Open. 2019;7:e2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ono MT, Karner BM. Subglandular-to-subpectoral conversion with mastopexy: the four-step approach. Plast Reconstr Surg. 2022;149:209e–215e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bui JM, Perry T, Ren CD, et al. Histological characterization of human breast implant capsules. Aesthetic Plast Surg. 2015;39:306–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calobrace MB. Elective implant removal and replacement in asymptomatic aesthetic patients with textured devices. Plast Reconstr Surg. 2021;147(5S):14S–23S. [DOI] [PubMed] [Google Scholar]