Background:
Generalized anxiety disorder (GAD) tightly traps modern people. Its incidence shows an increased peak during the 2019 novel coronavirus (COVID-19) epidemic. Acupuncture is regarded as an effective way to relieve anxiety symptoms. However, there are still controversies. This study aimed to systematically evaluate the clinical efficacy of acupuncture in patients with GAD.
Methods:
Four English and 3 Chinese databases were searched from their inception to January 2022. Only randomized controlled trials (RCTs) in which acupuncture was the main intervention were included. The literature was independently screened and extracted by two investigators. The Cochrane Bias Risk Assessment Tool was used for quality evaluation. Analyses were conducted by RevMan 5.3.0 and STATA 15.0 software. The primary outcome was the Hamilton Anxiety Scale (HAMA). The secondary indicators were the total effective rate, the Self-Rating Anxiety Scale (SAS), and the Treatment Emergent Symptom Scale (TESS).
Results:
Twenty-seven studies were included with a total of 1782 participants. The risk of performance bias or reporting bias for most of the included trials was unclear. Combined results showed the acupuncture group had better outcomes in the HAMA score [MD = −0.78, 95%CI (−1.09, −0.46)], the total effective rate [RR = 1.14, 95%CI (1.09, 1.19)], the SAS score [MD = −2.55, 95%CI (−3.31, −1.80)] compared with the control group. Regarding the number of adverse events, the acupuncture group was safer than the control group and scored less grade in the TESS score [MD = −1.54, 95%CI (−1.92, −1.17)].
Conclusions:
Acupuncture can effectively relieve the anxiety symptoms of generalized anxiety disorder patients with fewer side effects, but randomized controlled trials with large sample size and high quality are also required to support the result.
Keywords: acupuncture, generalized anxiety disorder, meta-analysis, randomized controlled trial, systematic review
1. Introduction
Generalized Anxiety Disorder (GAD) is a major subtype of common chronic anxiety disorder, with a total incidence of 5–7% among the population.[1,2] It occurs especially frequently in women.[3] During menopause, the occurrence is as high as 63.3%.[4] Besides, the incidence shows an increased peak during the 2019 novel coronavirus (COVID-19) epidemic.[5–7] GAD mainly manifests as persistent, uncontrollable, and excessive anxiety. Physical symptoms trouble patients seriously, such as sleep disturbance and muscle tension.[8–10] The discomfort is especially acute during the outbreak, which is easily combined with other mental disorders and develops into bipolar disorder.[11]
Modern medical research believes that the serotonin system (5-HT) is of great importance to fear and anxiety.[12] Selective serotonin reuptake inhibitors are focused on solving the problem of GAD,[13] such as benzodiazepines. However, the use of these neurological drugs has been questioned due to their adverse effects on the public and physical dependence.[14] It is increasingly urgent to find effective treatments for GAD.
At present, patients are gradually opting to combine medications with complementary and alternative medicine (CAM) treatments to reduce anxiety symptoms.[15,16] Acupuncture therapy is targeted, flexible, effective and safe, which has been practiced as an adjuvant treatment for GAD in plenty of clinical trials.[17,18] However, most of them are randomized controlled trials (RCTs) with small sample sizes and single centers. There are still controversies about the scientific basis and safety assurance. Therefore, this study aims to collect clinical RCTs of acupuncture in the treatment of GAD and conduct a meta-analysis of the included literature, to provide an evidence-based basis for clinicians.
2. Materials and methods
2.1. Study registering and reporting
This is a systematic review, and ethical approval was not necessary. The protocol of this review was registered on PROSPERO (https://www.crd.york. ac. uk/PROSPERO/; trial ID CRD42020205834). The following list was provided based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (available at http://dx.doi.org/10.21037/apm-21-499).[19]
2.2. Literature inclusion and exclusion criteria
Literature was included if the following criteria were met: (a) Research type and design: clinical RCTs of acupuncture treatment (AT) for GAD published at home and abroad; (b) Research objects: met the GAD diagnostic criteria; (c) Intervention measures: the experimental group adopts only AT (needle materials, acupoint selection, needle implementation, needle retention time and course were not limited) or combined with the conventional treatments (psychotherapy or western medicine). The intervention measures of the control group were western medicine (the type of medicine was not limited), psychotherapy (CBT), or western medicine plus CBT; (d) Clinical efficacy outcome indicators: primary indicators: the Hamilton Anxiety Scale (HAMA); secondary indicators: the Self-Rating Anxiety Scale (SAS), the Total Effective Rate (TER) and the Treatment Emergent Symptom Scale (TESS). Literature was excluded if one of the following criteria were met: (I) Non-RCT test or self-control RCTs; (II) Comparison of curative effects of different acupuncture techniques, acupoint selection and treatment time, etc; (III) The control group did not belong to western medicine or CBT; (IV) There were obvious quality problems in the literature, such as statistical errors; (V) Documents with incomplete research data or original data could not be obtained; (VI) Literature review, evaluation literature, theoretical research, case report, clinical experience, academic theoretical discussion, repetitive literature, etc.
2.3. Methods of obtaining literature
A comprehensive search of the electronic databases was conducted including the Chinese Biomedical Literature (CBM http://www.sinomed.ac.cn/), China Knowledge Network (CNKI https://www.cnki.net/), China Science and Technology Journal (VIP http://www.cqvip.com/), Wanfang (WF http://www.wanfangdata.com.cn), PubMed, Embase and Cochrane Library databases. Relevant references. Master’s and doctoral degrees papers were also selected. In addition, we searched the National Institutes of Health Clinical Trials Database (http://clinicaltrials.gov) and the Chinese Clinical Trials Registry (www.chictr.org.cn/searchproj.asp), to screen the completed but unpublished clinical studies to find as many relevant studies as possible. Subject and free words were combined for document retrieval. The search term of the disease was “generalized anxiety disorder”; the intervention measures were “acupuncture treatment” or “acupuncture” or “acupuncture therapy”. The retrieval date was up to 2022-01. The search strategy of PubMed is as follows:
-
#1
Search ((“Generalized Anxiety Disorder” or “Disorder, Anxiety” or “Anxiety Disorders”)).
-
#2
Search (“Acupuncture” [Mesh]) OR ((“Acupuncture treatment” or “Electroacupuncture” or “Acupuncture, Ear” or “Acupuncture Points”)).
-
#3
#1 AND #2.
2.4. Data extraction and management
After the literature was downloaded, the search results were imported into the Note- Express3.60 document management software to filter out the duplicate documents. Then, the title and abstract were read to conduct a preliminary screening. The articles that passed the first checkpoint were further sieved in full text. Finally, an excel table was developed according to the relevant information items to extract data and analyze the results. All documents were independently screened by two people (M Li and X Ye) and cross-checked with each other. In case of disagreement, they would discuss and resolve it with the third researcher (X Liu).
2.5. Literature quality evaluation
According to Cochrane Handbook 5.1.0,[20] the included RCTs were evaluated by the quality and risk of bias, rated as low-risk, unclear, or high-risk level. The evaluation basis is mainly as follows: (I) Whether the random method is appropriate; (II) Whether there is allocation concealment; (III) Whether the blind method is implemented; (IV)Whether the result data is complete; (V)Whether there is selective reporting of results; (VI) Whether there are other biases. The quality evaluation process of the included studies was cross-checked by two evaluators (M Li and X Ye). For included articles that were divergent and difficult to determine, the two parties would negotiate or the third evaluator (X Liu) would help to decide a solution.
2.6. Statistical methods
Revman 5.3.0 (Cochrane Collaboration, Copenhagen, Denmark) and STATA 15.0 software (StataCorp, College Station, TX) were used for meta-analysis. The HAMA score, the SAS score, and the TESS score were both continuous variables, and the mean difference (MD) was estimated. TER was a categorical variable and the relative risk (RR) was selected. The effect sizes were expressed in 95% confidence intervals (95% CI). The heterogeneity between studies was tested by I² or Q. If I2 < 50%, P > .05, it means that there was no statistical heterogeneity among the studies, and the fixed effects model was used to combine the effect values; If I2 > 50%, P < .05, it meant that the heterogeneity between the studies could not be ignored. For that one-by-one elimination was conducted to find the possible sources of the heterogeneity (clinical heterogeneity or methodological heterogeneity), and sensitivity analysis was applicated to test the robustness of the results. If the heterogeneity could not be eliminated, the random-effects model would finally analyze the effect value. Besides, Revman 5.3.0 was used for inverted funnel chart qualitative analysis, and STATA 15.0 software was applied for Egger test quantitative analysis for publication bias detection.
3. Results
3.1. Literature search results
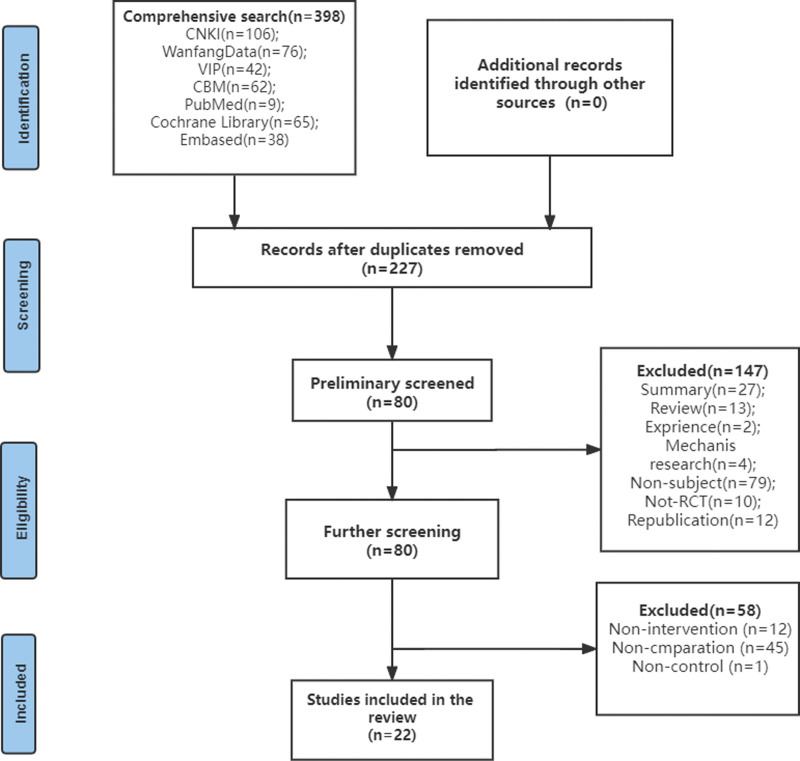
398 literatures were initially excavated through seven major databases, containing 270 in Chinese and 128 in English. 22 articles were finally included in the study, involving 900 cases in the treatment group and 882 cases in the control group. The literature retrieval process was shown in Fig. 1 and the basic characteristics of the included studies were on record in Table 1.
Figure 1.
Search Flowchart.
Table 1.
Basic characteristics of the included literature.
| Included literature | Sample size | Treatment measures | Outcome | Course | |
|---|---|---|---|---|---|
| Therapy | Control | ||||
| WANG 2003(10) | 30/32 | EA | WM (Trazodone Hydrochloride) | ①②③ | 6 weeks |
| WANG 2005(11) | 35/30 | AT | WM (lorazepam & oryzanol/ propranolol) | ②③ | A month |
| LIU 2007(1)(12) | 29/29 | AT | WM (Paroxetine) | ①②③④ | 6 weeks |
| LIU 2007(2)(12) | 28/29 | AT + WM | WM (Paroxetine) | ①②③④ | 6 weeks |
| WANG 2007(13) | 21/20 | AT | WM (Flupentixol and Melitracen) | ①③ | A month |
| FU 2008(1)(14) | 20/20 | AT | WM (Paroxetine) | ①②③④ | 6 weeks |
| FU 2008(2)(14) | 20/20 | AT + WM | WM (Paroxetine) | ①②③④ | 6 weeks |
| DENG 2009(15) | 28/27 | AT + WM | WM (Flupentixol and Melitracen) | ①③④ | A month |
| TAI 2010(1)(16) | 23/21 | AT + CBT | CBT | ②③ | 4–8weeks |
| TAI 2010(2)(16) | 29/21 | AT + CBT | CBT | ②③ | 4–8 weeks |
| SHI 2010(17) | 30/30 | AT | WM (Flupentixol and Melitracen) | ①②③④ | 4 weeks |
| GONG 2012(18) | 56/57 | AT + CBT | WM (Duloxetine) | ①③④ | 6 weeks |
| XIONG 2013(19) | 36/35 | AT | WM (Flupentixol and Melitracen) | ②③ | A month |
| ZHOU 2013(20) | 40/40 | AT | WM (clonazepam) | ① | 6 weeks |
| ZHAO 2014(21) | 30/30 | AT | WM (Paroxetine) | ①②③④ | 6 weeks |
| FANG 2014(22) | 50/50 | AT + CBT | CBT | ① | 4 weeks |
| FAN 2014(23) | 40/41 | EA + AT | WM (Paroxetine) | ① | 6 weeks |
| CHE 2015(24) | 40/40 | AT | WM (Paroxetine) | ①②④ | 6 weeks |
| SHENG2015(1)(25) | 30/30 | AT | WM (Paroxetine) | ③ | 6 weeks |
| SHENG 2015(2)(25) | 30/30 | AT | WM (Paroxetine) | ③ | 6 weeks |
| LI 2015(26) | 21/24 | AT | WM (Paroxetine) | ① | 6 weeks |
| ZHOU 2015(27) | 30/30 | AT + WM | WM (Paroxetine) | ① | 8 weeks |
| XU 2016(28) | 30/30 | AT + WM | WM (Buspirone hydrochloride) | ①③ | 15 days |
| ZHANG 2018(29) | 48/42 | AT + CBT | CBT | ① | 28 days |
| ZHAO 2018(30) | 60/60 | EA | WM (Buspirone hydrochloride) | ①③ | 6 weeks |
| LIANG 2020(1)(31) | 38/38 | AT | WM (Paroxetine) | ①②③④ | 4 weeks |
| LIANG 2020(2)(31) | 38/38 | AT | WM (Paroxetine) | ①②③④ | 4 weeks |
Note: ①HAMA: the Hamilton Depression Rating Scale ②SAS: the Self-Rating Anxiety Scale ③TEF: the Total Effective Rate ④TESS: Treatment Emergent Symptom Scale.
AT = Acupuncture treatment, EA = Electro-acupuncture, WM = Western Medicine.
3.2. Features of included studies
3.2.1. Research type.
A Parallel randomized control design was adopted. Five included articles are academic papers,[21–25] and 17 pieces are journaled papers. Five 3-arm experiments[21,25–28] were divided into double-arm experiments for statistics. Finally, a total of 27 databases were reviewed. And all studies reported baseline similarity of patients before treatment.
3.2.2. Intervention measures.
In the intervention group, 17 trials used acupuncture alone, 7 trials used the combination of acupuncture and western medicine, and 3 trials used the combination of acupuncture and CBT. In the control group, 23 articles compared acupuncture with western medicine (paroxetine, Flupentixol and Melitracen, Trazodone Hydrochloride, buspirone hydrochloride, lorazepam & oryzanol/ propranolol, lorazepam, duloxetine, clonazepam). Four studies compared acupuncture with CBT.
3.2.3. Measurement indicators.
The primary outcome was the HAMA score. The secondary indicators were the TER, SAS score, and TESS score. The HAMA score reduction rate was recorded in 21 documents. The TER was selected in 25 articles. The SAS score was scored in 14 articles. The TESS score was recorded in 11 documents.
3.3. Evaluation of the quality of included studies
15 literatures clarified the specific random method (55.56%); 6 documents adopted the envelope method for distribution hiding (22.22%); 4 articles blinded the assessors (14.81%); 11 (40.74%) mentioned withdrawal; Loss to follow-up bias and reporting bias was well controlled in the all of the included research. The details are exhibited in Table 2.
Table 2.
Bias evaluation results of included literature.
| Included literature | Random sequence generation | Allocation hiding | Blind researchers or subjects | Blind Evaluator | Completeness of outcome | Selective report | Other biases |
|---|---|---|---|---|---|---|---|
| WANG 2003[9] | L | U | U | U | L | U | U |
| WANG 2005[10] | U | U | U | U | L | U | U |
| LIU 2007(1)[11] | L | L | U | U | L | U | U |
| LIU 2007(2)[11] | L | L | U | U | L | U | U |
| WANG 2007[12] | H | U | U | U | L | U | U |
| FU 2008(1)[13] | L | L | U | U | L | U | U |
| FU 2008(2)[13] | L | L | U | U | L | U | U |
| DENG 2009[14] | L | U | U | U | L | U | U |
| TAI 2010(1)[15] | U | U | U | U | L | U | U |
| TAI 2010(2)[15] | U | U | U | U | L | U | U |
| SHI 2010[16] | H | U | U | U | L | U | U |
| GONG 2012[17] | U | U | U | U | L | U | U |
| XIONG 2013[18] | U | U | U | U | L | U | U |
| ZHOU 2013[19] | H | U | U | U | L | U | U |
| ZHAO 2014[20] | L | U | U | U | L | U | U |
| FANG 2014[21] | L | U | U | L | L | U | U |
| FAN 2014[22] | L | U | U | L | L | U | U |
| CHE 2015[23] | U | U | U | U | L | U | U |
| SHENG 2015(1)[24] | L | U | U | U | L | U | U |
| SHENG 2015(2)[24] | L | U | U | U | L | U | U |
| LI 2015[25] | U | U | U | U | L | U | U |
| ZHOU 2015[26] | U | U | U | U | L | U | U |
| XU 2016[27] | L | U | U | U | L | U | U |
| ZHANG 2018[28] | H | U | U | U | L | U | U |
| ZHAO 2018[29] | L | U | U | U | L | U | U |
| LIANG 2020(1)[30] | L | L | U | L | L | U | U |
| LIANG 2020 (2)[30] | L | L | U | L | L | U | U |
Note: L = low risk, U = unclear risk, H = high risk.
3.4. Meta-analysis
3.4.1. The HAMA score.
A total of 21 articles[21–26,29–40] were included to evaluate the remission of the HAMA score. The heterogeneity among the studies was statistically significant (I2 = 71%, P < .00001), and a random-effects model was selected. The results showed that the HAMA score of AT group was lower than the control group, and the difference was statistically significant [MD = –1.26, 95%CI (–1.96, –0.56)].
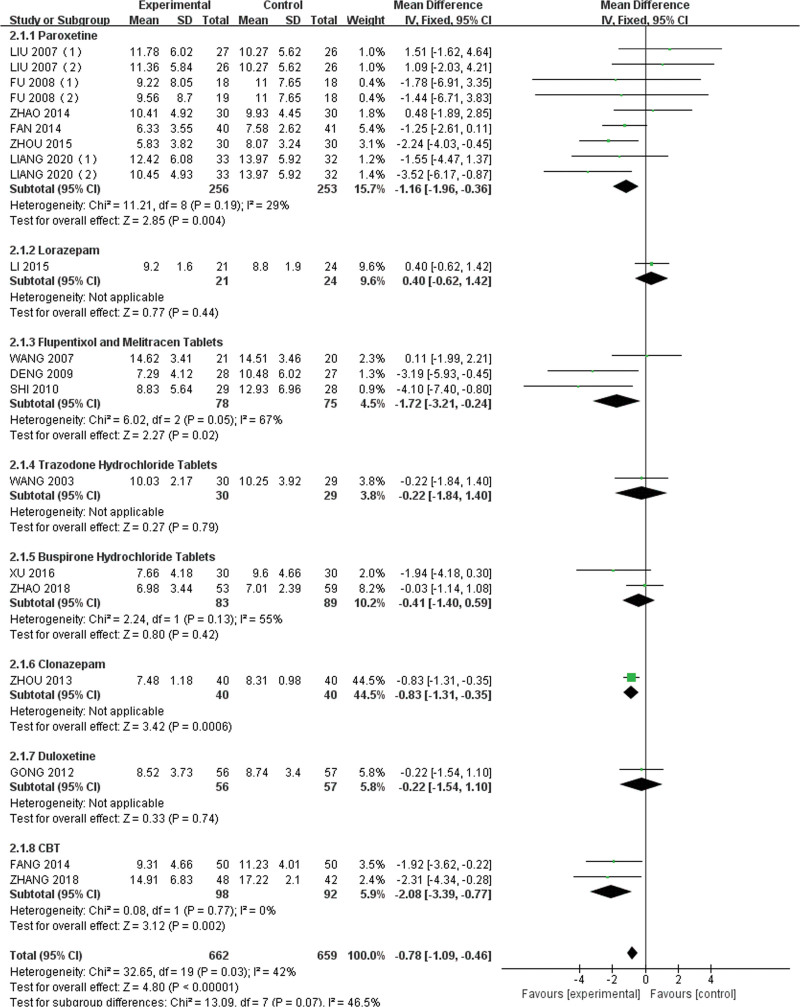
One-by-one elimination and sensitivity analysis were performed to consider the large heterogeneity, and Che Lina was found as a suspicious influencing factor. After the article of Che Lina was removed, the heterogeneity decreased (I2 < 50%), and the fixed effects model was finally applied to analyze the final results. Results of subgroup analyses indicated that acupuncture appeared an anxiety improvement compared with paroxetine [MD = –1.16, 95%CI (–1.96, –0.36)] and Flupentixol and Melitracen [MD = –1.72, 95%CI (–3.21, –0.24)]. The results were shown in Fig. 2. The funnel chart and Egger test were performed by STATA 15.0 software. The results suggest that there was no publication bias [t = –0.82, 95% CI (–2.11), –0.92), P > .05], and the credibility of the included literature was high.
Figure 2.
HAMA Forest plot.
3.4.2. The Total effective rate.
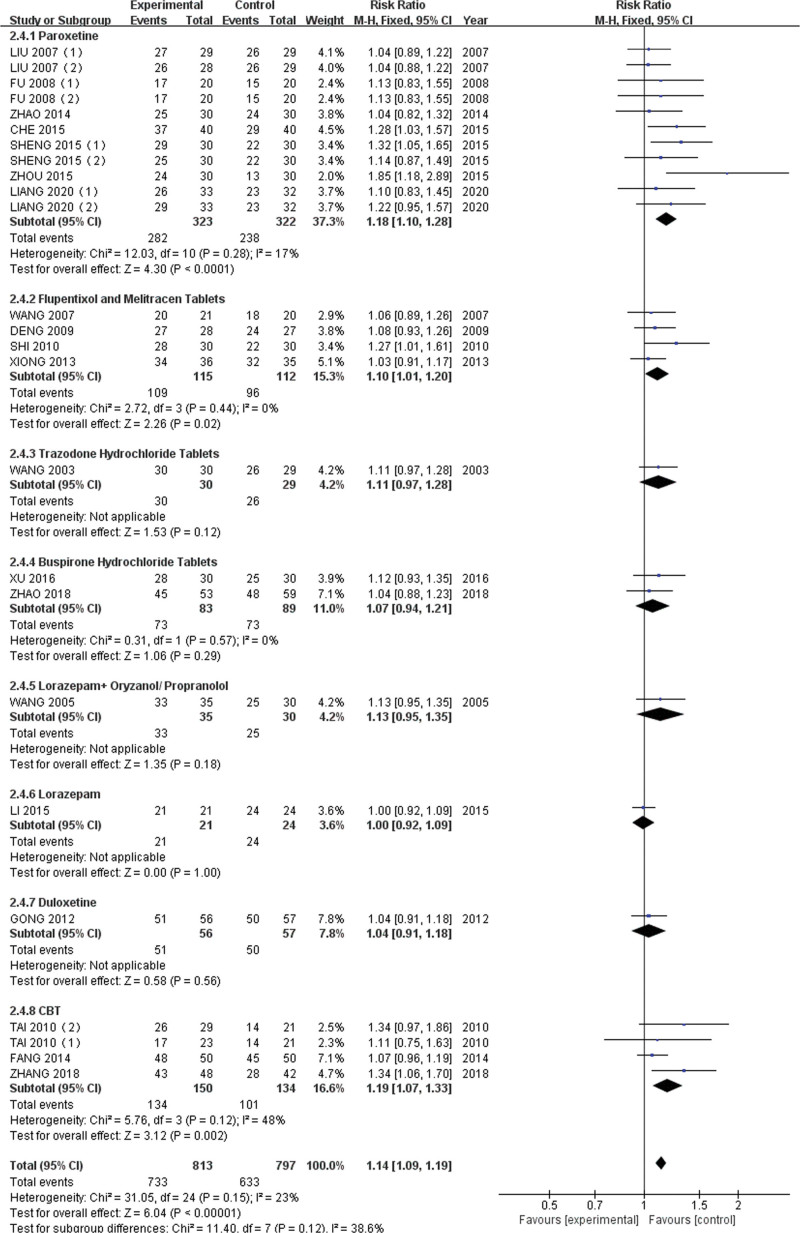
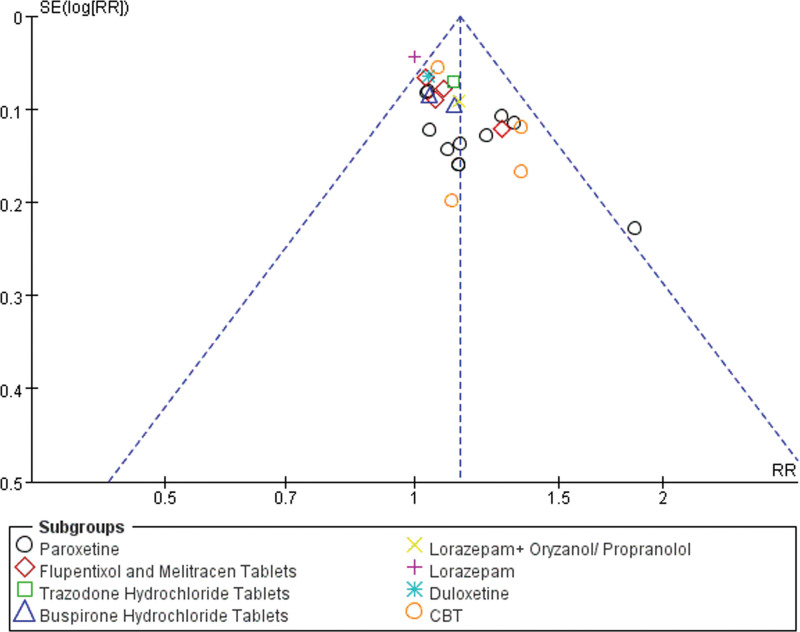
A total of 25 articles[21–31,33,34,36–42] were included to estimate the remission rate of the HAMA score. The heterogeneity among the studies was not statistically significant (I2 = 27%, P > .05), and the fixed effects model was conducted. Results of subgroup analyses indicated that acupuncture appeared an active effect on the anxiety symptom compared with paroxetine [RR = 1.18, 95%CI (1.10, 1.28)] and Flupentixol and Melitracen [RR = 1.10, 95%CI (1.01, 1.20)]. The result was shown in Fig. 3. The funnel chart (Fig. 4) and Egger test suggest no publication bias [t = 4.12, 95 % CI (0.90, 2.71), P = .00].
Figure 3.
The Total Effect Rate Forest plot.
Figure 4.
The total Effect Rate Funnel plot.
3.4.3. The SAS Score.
A total of 14 articles[21,23,25–27,29,33,36,41,42] reported SAS score. The heterogeneity among the studies was statistically significant (I2 = 72%, P < .0001), So the random-effects model was selected. The results showed the difference in clinical efficacy between the AT group with the control group was statistically significant [MD = –3.19, 95%CI (–4.78, –1.61)].
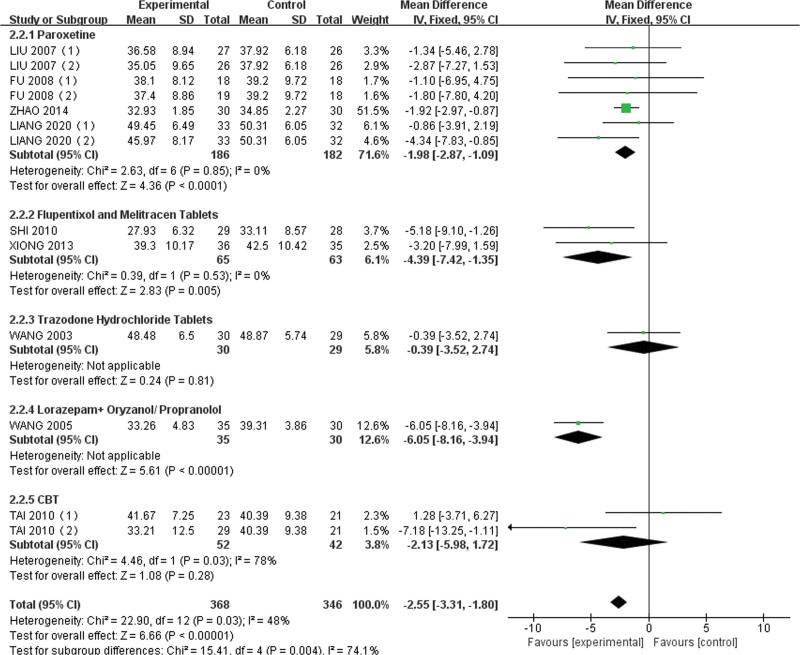
By excluding the literature one by one and sensitivity analysis to find the source of heterogeneity, Che Lina was thought of as a suspicious influencing factor. After the article exclusion, the heterogeneity decreased (I2 < 50%), and the final analysis of the data results adopted the fixed-effects model. Results of subgroup analyses indicated a statistically significant difference that acupuncture performs a positive effect on the anxiety symptom compared with paroxetine [MD = –1.98, 95%CI (–2.87, –1.09)] and Flupentixol and Melitracen [MD = –4.39, 95%CI (–7.42, –1.35)]. The result was shown in Fig. 5. The funnel chart and Egger test suggested no publication bias, and the credibility of the included literature was high [t = 0.07, 95% CI (–2.07, 2.20), P = .95].
Figure 5.
SAS Forest plot.
3.4.4. The TESS score.
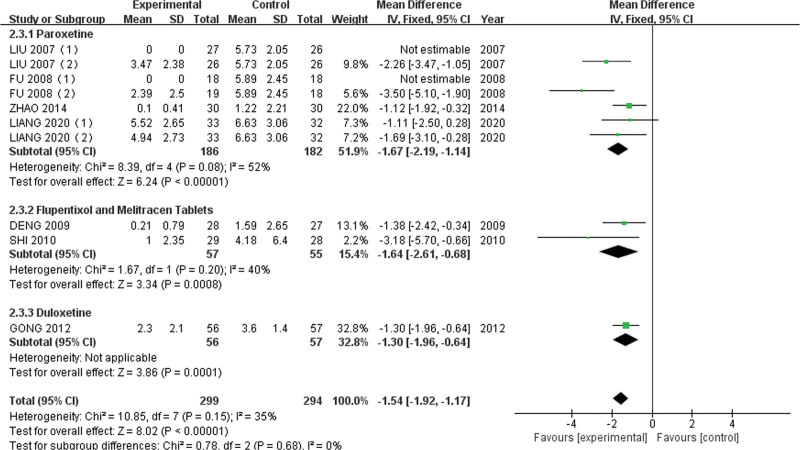
A total of 11 articles[21–23,25,26,31,33,36] applied TESS score. The heterogeneity among the studies was statistically significant (I2 = 78%, P < .0001), so a randomized effect model was conducted. The results revealed that few adverse events occurred in the acupuncture group compared with the control group and the difference was statistically significant [MD = –1.99, 95%CI (–2.72, –1.27)].
Then one-by-one elimination and sensitivity analysis were carried out to find the heterogeneous sources, Che Lina seemed like a suspicious influencing factor. After the article was removed, the heterogeneity decreased (I2 < 50%), and the analysis was finally analyzed by the fixed-effects model. The results delineated that AT group reported fewer adverse reactions. The final result was shown in Fig. 6. Funnel chart and Egger test confirmed the reliability of the included literature [t = 0.71, 95% CI (–2.90, 5.39), P > .05].
Figure 6.
TESS Forest plot.
4. Discussion
Over the past 2 years, COVID-19 has spread around the world and infected millions of people.[43] The pandemic has changed our way of life and threatened our health. In addition to causing physical health problems globally, the outbreak has also made a major impact on our mental health. Wearing masks, isolation, and protection has greatly reduced the way we relieve stress.[44] On the contrary, pressure sources such as online check-in, online classes, grabbing shopping resources, unemployment, car loans, and mortgages have skyrocketed,[45] which leads to unending anxiety, depressive symptoms, insomnia, panic, and denial. It belongs to one of the important reasons for the rapid increase in the prevalence of GAD during the epidemic. Huang Y et al conducted a cross-sectional online survey among Chinese citizens aged ≥18 years from January 31 to February 2, 2020. The study surveyed 4827 participants across 31 provinces and autonomous regions in mainland China. The online survey showed the prevalence of GAD was up to 22.6% across the 31 areas, and the highest prevalence was up to 35.4% in the Hubei province.[46] It may be beneficial to promote public mental health by enhancing stress resistance during the COVID-19 outbreak, and it is helpful to buffer the negative psychological impact of fears about the novel coronavirus.[47]
Acupuncture treatment for GAD is still controversial. To obtain reliable clinical evidence, this study design a reasonable retrieval strategy to fully obtain associated literature for meta-analysis. Based on the specification of clinical guidelines,[13] the HAMA scores from 14 to 28 are regarded as mild to moderate degrees of anxiety, and CBT is recommended. The HAMA scores from 28 to 56 belong to the scope of severe anxiety, and anti-anxiety medicine is the main treatment means. Therefore, we define the interventions of the control group to be Western medicine or CBT.
A total of 1782 patients, originating from the clinic or inpatient department of the hospital, were included. Among the included articles, few of them mentioned anxiety levels. 24 pieces employed western medicine as a positive control and only 4 chose CBT instead. The results seemed to indicate the bottleneck of GAD treatment. Due to the professionalism and specificity of CBT,[9] western pills were irregularly used instead. It reminded us that GAD needs to be further strengthened in the guideline diagnosis of grading to better standard treatment.
The literature was classified by different western medicine and the CBT for subgroup analysis, and we incorporated multiple ending indicators to ensure the accuracy and reliability of the research. In the HAMA scores and TER, acupuncture showed better efficacy for GAD compared with Paroxetine, CBT, Flupentixol and Melitracen. Besides, acupuncture reported fewer side effects. However, high integrated heterogeneity was found. After one-by-one elimination and sensitivity analysis, the article of Che Lina was found to affect heterogeneity. The possible reasons for the production of heterogeneity are as follows: (1) Methodology of the literature is incorporated, which makes it unable to follow the whole trial principles during clinical treatment. (2) The process of generating a random sequence is not explicitly reported and without hidden and blinding. (3) The amount of test samples is too small and the data quality is uneven.
Given that this study only observes the efficacy, without exploring the effects of different intervention methods, such as acupuncture (acupuncture course, duration, etc.) or changes in parameters of western medicine (western medicine Dosage, etc.), a large number of high-quality RCTs are still needed to further verify the effectiveness and safety of acupuncture for GAD.[48]
GAD patients still lack understanding and acceptance of CBT,[49] which may be related to the current lack of psychological counselors in China[50] and the chaos of the psychological counseling clinics.[51] Besides, given the long-term side effects, patients often refuse to insist on taking western medicine. Acupuncture is gradually becoming an alternative to relieve anxiety disorders during the epidemic. However, due to the small sample size of the included literature, it is not clear that there is a significant association between acupuncture and GAD. Researchers are encouraged to design future experiments, including larger sample sizes and more rigorous experimental designs.
5. Conclusion
In summary, the results of this study suggest that acupuncture has clear superiority in relieving anxiety symptoms compared with western medications or psychotherapy, so acupuncture is recommended for improving the quality of health for patients with generalized anxiety disorder during COVID-19. It is hoped that this research can play a certain role in replenishing the deficiencies of psychotherapy and improving the standard use of anti-anxiety drugs. It also provides references for clinicians to make superior decisions. However, high-quality clinical trials will be needed in the future.
Author contributions
(I) Conception and design: M Li; (II) Administrative support: L Zhuang; (III) Provision of study materials or patients: X Liu; (IV) Collection and assembly of data: M Li, X Ye; (V) Data analysis and interpretation: M Li, X Liu; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Abbreviations:
- 5-HT =
- the serotonin system
- AT =
- acupuncture treatment
- CAM =
- complementary and alternative medicine
- CBM =
- Chinese Biomedical Literature
- CBT =
- psychotherapy
- CI =
- confidence intervals
- CNKI =
- China Knowledge Network
- COVID-19 =
- 2019 novel coronavirus
- GAD =
- Generalized anxiety disorder
- HAMA =
- Hamilton Anxiety Scale
- MD =
- mean difference
- PRISMA =
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCTs =
- randomized controlled trials
- RR =
- relative risk
- SAS =
- the Self-Rating Anxiety Scale
- TER =
- Total effective rate
- TESS =
- Treatment-Emergent Symptom Scale
- VIP =
- China Science and Technology Journal
- WF =
- Wanfang
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Li M, Liu X, Ye X, Zhuang L. Efficacy of acupuncture for generalized anxiety disorder: A PRISMA-compliant systematic review and meta-analysis. Medicine 2022;101:49(e30076).
This work was supported by the National Natural Science Foundation of China (81903971), and the Natural Science Foundation of Guangdong Province (2021A1515011470). Innovative Clinical Research Project of the First Affiliated Hospital of Guangzhou University of Chinese Medicine (2019ZWB07).
All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-499). The authors have no conflicts of interest to declare.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethical approval: Since our research did not have close or direct contact with every patient, no ethical clearance was required for this manuscript.
Contributor Information
Meichen Li, Email: 2386471273@qq.com.
Xin Liu, Email: 20198103034@stu.gzucm.edu.cn.
Xinyi Ye, Email: yexinyigzu@163.com.
References
- [1].Stein DJ, Kazdin AE, Ruscio AM, et al. Perceived helpfulness of treatment for generalized anxiety disorder: a world mental health surveys report. BMC Psychiatry. 2021;21:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Robin MCBA, Hans-Ulrich WPD, Inf HPD, et al. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depress Anxiety. 2010;13:78–88. [DOI] [PubMed] [Google Scholar]
- [3].Witlox M, Garnefski N, Kraaij V, et al. Prevalence of anxiety disorders and subthreshold anxiety throughout later life: systematic review and meta-analysis. Psychol Aging. 2021;36:268–87. [DOI] [PubMed] [Google Scholar]
- [4].Qu L, Ye R. Epidemiological survey of depression/anxiety disorders in outpatient clinics of general hospitals in Guangzhou area. Chin J Clin Psychol. 2009;17:61–3. [Google Scholar]
- [5].Stocker R, Tran T, Hammarberg K, et al. Patient Health Questionnaire 9 (PHQ-9) and General Anxiety Disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 2021;298:113792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) Epidemic among the general population in China. Int J Environ Res Public Health. 2020;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the covid-19 pandemic and compliance with precautionary measures: age and sex matter. Int J Environ Res Public Health. 2020;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wathelet M, Duhem S, Vaiva G, et al. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591e2025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fisher JR, Tran TD, Hammarberg K, et al. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust. 2020;213:458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].McGuire A. Diagnosing the diagnostic and statistical manual of mental disorders. Disabil Soc. 2015;30:1582–5. [Google Scholar]
- [11].Lin J, Su Y, Lu X. A multicenter cross-sectional survey of potential risk factors in depression patients with Comorbid generalized anxiety disorder. 2020;53:287–94. [Google Scholar]
- [12].Carpenter JK, Andrews LA, Witcraft SM, et al. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hoge EA, Ivkovic A, Fricchione GL. Generalized anxiety disorder: diagnosis and treatment. BMJ. 2012;345:e7500. [DOI] [PubMed] [Google Scholar]
- [14].Buszewicz M, Cape J, Serfaty M, et al. Pilot of a randomised controlled trial of the selective serotonin reuptake inhibitor sertraline versus cognitive behavioural therapy for anxiety symptoms in people with generalised anxiety disorder who have failed to respond to low-intensity psychological treatments as defined by the national institute for health and care excellence guidelines. Health Technol Assess. 2017;21:1–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Trkulja V, Barić H. Current research on Complementary and Alternative Medicine (CAM) in the treatment of anxiety disorders: an evidence-based review. Adv Exp Med Biol. 2020;1191:415–49. [DOI] [PubMed] [Google Scholar]
- [16].Barić H, Đorđević V, Cerovečki I, et al. Complementary and alternative medicine treatments for generalized anxiety disorder: systematic review and meta-analysis of randomized controlled trials. Adv Ther. 2018;35:261–88. [DOI] [PubMed] [Google Scholar]
- [17].Goyatá SL, Avelino CC, Santos SV, et al. Effects from acupuncture in treating anxiety: integrative review. Rev Bras Enferm. 2016;69:602–9. [DOI] [PubMed] [Google Scholar]
- [18].Amorim D, Amado J, Brito I, et al. Acupuncture and electroacupuncture for anxiety disorders: a systematic review of the clinical research. Complement Ther Clin Pract. 2018;31:31–7. [DOI] [PubMed] [Google Scholar]
- [19].Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JPT. Cochrane handbook for systematic reviews of interventions. Cochrane Collaboration. Cochrane database of systematic reviews (Online). 2011;2011. [Google Scholar]
- [21].Fu A. Clinical study on treatment of generalized anxiety disorder mainly by acupuncture at backshu point. Heilongjiang University of Traditional Chinese Medicine. 2008. [Google Scholar]
- [22].Deng X. Observation on the clinical efficacy of acupuncture combined with low-dose deanxit in the treatment of generalized anxiety disorder [硕士]. Shandong Univ Tradit Chin Med. 2009. [Google Scholar]
- [23].Shi C. Clinical study on treatment of generalized anxiety disorder by acupuncture at rendu vessel points [硕士]. Heilongjiang Univ Tradit Chin Med. 2010. [Google Scholar]
- [24].Xu M, Zhou J, Liu Y, et al. Observations on the efficacy of long retention of needles in scalp emotional zone plus medication for generalized anxiety disorder. Shanghai J Acupunct. 2016;35:1281–3. [Google Scholar]
- [25].Liang H. Clinical study on acupuncture treatment of generalized anxiety disorder based on simultaneous treatment of heart and brain, Gansu UnivTradit Chin Med. 2020. [Google Scholar]
- [26].Liu H. Clinical observation on acupuncture for generalized anxiety disorder. J Guangzhou Univ Tradit Chin Med. 2007;24:119–22. [Google Scholar]
- [27].Tai X. Clinical observation on acupuncture and psychotherapy treating generalized anxiety disorder. Tradit Chin Med Info. 2010;27:72–3. [Google Scholar]
- [28].Sheng G, Li H, Tang Y. Clinical observation on the treatment of electroacupuncture jiaji acupoint therapy combined with scalp acupuncture for generalized anxiety disorder. J Clin Acupunct Moxibustion. 2015:42–3. [Google Scholar]
- [29].Wang C, Liang J, Luo H, et al. Comparative observation on clinical effects of treatment of comprehensive anxiety neurosis with electric acupuncture and trazodone. J Beijing Univ Tradit Chin Med. 2003;10:37–9. [Google Scholar]
- [30].Wang G. Acupuncture treatment of 21 cases of generalized anxiety disorder. Henan Tradit Chin Med. 2007;27:55–6. [Google Scholar]
- [31].Gong Y, He N, Liu R. Observation on the curative effect of electroacupuncture combined with duloxetine in the treatment of generalized anxiety. China Minkang Med. 2012;24:2877–99. [Google Scholar]
- [32].Zhou X, Li Y, Zhu H, et al. Impacts of acupuncture at twelve meridians acupoints on brain waves of patients with general anxiety disorder. Chin Acupunct. 2013;33:395–8. [PubMed] [Google Scholar]
- [33].Zhao Y, Zou W, Teng W, et al. Clinical study of tongdu tiaoshen acupuncture for the treatment of generalized anxiety disorder. J Clin Acupunct Moxibustion. 2014:24–6. [Google Scholar]
- [34].Fang Y, Zhou W, Yuan Y, et al. Clinical study of electroacupuncture combined with drug in treatment of patients with generalized anxiety disorder. Chin Minkang Med. 2014;26:13–5. [Google Scholar]
- [35].Fan Z, Liang Z, Huang Y, et al. Effect of electroacupuncture combined with paroxetine in the treatment of generalized anxiety disorder. Guangdong Med. 2014;35. [Google Scholar]
- [36].Che L. Discussion on the curative effect of acupuncture on patients with generalized anxiety disorder. Chin Minkang Med. 2015;27:86–7. [Google Scholar]
- [37].Li T, Zhao A, Zhang W, et al. Clinical analysis of “qingxinchufan” acupuncture treatment of 21 cases of senile general anxiety. Chin Emerg Med. 2015;35:417–8. [Google Scholar]
- [38].Zhou B. Clinical observation on the treatment of generalized anxiety disorder by tiaoshen needling method combined with paroxetine [博士]. Guangzhou Univ Chin Med. 2015. [Google Scholar]
- [39].Zhang H, Guo L, Peng J, et al. Clinical observation on acupuncture and moxibustion combined with psychological intervention on patients with generalized anxiety disorder. Bright Chin Med. 2018;33:1005–7. [Google Scholar]
- [40].Zhao R, Qin L, Zhao S. Observation on therapeutic effect of acupuncture with “soothe the mind and relieve” in the treatment of generalized anxiety disorder. Beijing Tradit Chin Med. 2018;37:122–4. [Google Scholar]
- [41].Wang Z, Li Y, Lin H. Clinical observation on acupuncture treatment of generalized anxiety (GAS). Tianjin Tradit Chin Med. 2005:44. [Google Scholar]
- [42].Xiong Y. Clinical observation on the treatment of generalized anxiety disorder by acupuncture, reinforcing and regulating duty. Bright Chin Med. 2013;28:2589–90. [Google Scholar]
- [43].Yasmin F, Dapke K, Khalid MR, et al. Generalized anxiety disorder and depressive symptoms among pakistani population during the second wave of the COVID-19 pandemic: a regression analysis. Am J Trop Med Hyg. 2021;105:915–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Huang Y, Zhao N. Corrigendum to generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey [Psychiatry Research, 288 (2020) 112954]. Psychiat Res. 2021;299:113803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Zakeri MA, Hossini Rafsanjanipoor SM, Kahnooji M, et al. Generalized anxiety disorder during the COVID-19 outbreak in Iran: the role of social dysfunction. J Nerv Ment Dis. 2021;209:491–6. [DOI] [PubMed] [Google Scholar]
- [46].Chen H, Gao J, Dai J, et al. Generalized anxiety disorder and resilience during the COVID-19 pandemic: evidence from China during the early rapid outbreak. BMC Public Health. 2021;21:1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Cordaro M, Grigsby TJ, Howard JT, et al. Pandemic-specific factors related to generalized anxiety disorder during the initial COVID-19 protocols in the United States. Issues Ment Health N. 2021;42:747–57. [DOI] [PubMed] [Google Scholar]
- [48].Mochcovitch MD, Da Rocha Freire RC, Garcia RF, et al. Can long-term pharmacotherapy prevent relapses in generalized anxiety disorder? A systematic review. Clin Drug Invest. 2017;37:737–43. [DOI] [PubMed] [Google Scholar]
- [49].Wang K. A meta-analysis of the efficacy of domestic cognitive behavioral therapy combined with drugs in the treatment of generalized anxiety. Chin J Health Psychol. 2017;25:481–5. [Google Scholar]
- [50].Chen Z, Liu Z, Zhu Z, et al. Development status, problems and countermeasures of psychological consultation and psychotherapy in China. Bull Chin Acad Sci. 2016;31:1198–207. [Google Scholar]
- [51].Li G. Talking about the development status and countermeasures of psychological counselors. Hum Resour Dev. 2014:41–2. [Google Scholar]