Abstract
Background
In mental health services, the past several decades has seen a slow but steady trend towards employment of past or present consumers of the service to work alongside mental health professionals in providing services. However the effects of this employment on clients (service recipients) and services has remained unclear.
We conducted a systematic review of randomised trials assessing the effects of employing consumers of mental health services as providers of statutory mental health services to clients. In this review this role is called 'consumer‐provider' and the term 'statutory mental health services' refers to public services, those required by statute or law, or public services involving statutory duties. The consumer‐provider's role can encompass peer support, coaching, advocacy, case management or outreach, crisis worker or assertive community treatment worker, or providing social support programmes.
Objectives
To assess the effects of employing current or past adult consumers of mental health services as providers of statutory mental health services.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library 2012, Issue 3), MEDLINE (OvidSP) (1950 to March 2012), EMBASE (OvidSP) (1988 to March 2012), PsycINFO (OvidSP) (1806 to March 2012), CINAHL (EBSCOhost) (1981 to March 2009), Current Contents (OvidSP) (1993 to March 2012), and reference lists of relevant articles.
Selection criteria
Randomised controlled trials of current or past consumers of mental health services employed as providers ('consumer‐providers') in statutory mental health services, comparing either: 1) consumers versus professionals employed to do the same role within a mental health service, or 2) mental health services with and without consumer‐providers as an adjunct to the service.
Data collection and analysis
Two review authors independently selected studies and extracted data. We contacted trialists for additional information. We conducted analyses using a random‐effects model, pooling studies that measured the same outcome to provide a summary estimate of the effect across studies. We describe findings for each outcome in the text of the review with considerations of the potential impact of bias and the clinical importance of results, with input from a clinical expert.
Main results
We included 11 randomised controlled trials involving 2796 people. The quality of these studies was moderate to low, with most of the studies at unclear risk of bias in terms of random sequence generation and allocation concealment, and high risk of bias for blinded outcome assessment and selective outcome reporting.
Five trials involving 581 people compared consumer‐providers to professionals in similar roles within mental health services (case management roles (4 trials), facilitating group therapy (1 trial)). There were no significant differences in client quality of life (mean difference (MD) ‐0.30, 95% confidence interval (CI) ‐0.80 to 0.20); depression (data not pooled), general mental health symptoms (standardised mean difference (SMD) ‐0.24, 95% CI ‐0.52 to 0.05); client satisfaction with treatment (SMD ‐0.22, 95% CI ‐0.69 to 0.25), client or professional ratings of client‐manager relationship; use of mental health services, hospital admissions and length of stay; or attrition (risk ratio 0.80, 95% CI 0.58 to 1.09) between mental health teams involving consumer‐providers or professional staff in similar roles.
There was a small reduction in crisis and emergency service use for clients receiving care involving consumer‐providers (SMD ‐0.34 (95%CI ‐0.60 to ‐0.07). Past or present consumers who provided mental health services did so differently than professionals; they spent more time face‐to‐face with clients, and less time in the office, on the telephone, with clients' friends and family, or at provider agencies.
Six trials involving 2215 people compared mental health services with or without the addition of consumer‐providers. There were no significant differences in psychosocial outcomes (quality of life, empowerment, function, social relations), client satisfaction with service provision (SMD 0.76, 95% CI ‐0.59 to 2.10) and with staff (SMD 0.18, 95% CI ‐0.43 to 0.79), attendance rates (SMD 0.52 (95% CI ‐0.07 to 1.11), hospital admissions and length of stay, or attrition (risk ratio 1.29, 95% CI 0.72 to 2.31) between groups with consumer‐providers as an adjunct to professional‐led care and those receiving usual care from health professionals alone. One study found a small difference favouring the intervention group for both client and staff ratings of clients' needs having been met, although detection bias may have affected the latter. None of the six studies in this comparison reported client mental health outcomes.
No studies in either comparison group reported data on adverse outcomes for clients, or the financial costs of service provision.
Authors' conclusions
Involving consumer‐providers in mental health teams results in psychosocial, mental health symptom and service use outcomes for clients that were no better or worse than those achieved by professionals employed in similar roles, particularly for case management services.
There is low quality evidence that involving consumer‐providers in mental health teams results in a small reduction in clients' use of crisis or emergency services. The nature of the consumer‐providers' involvement differs compared to professionals, as do the resources required to support their involvement. The overall quality of the evidence is moderate to low. There is no evidence of harm associated with involving consumer‐providers in mental health teams.
Future randomised controlled trials of consumer‐providers in mental health services should minimise bias through the use of adequate randomisation and concealment of allocation, blinding of outcome assessment where possible, the comprehensive reporting of outcome data, and the avoidance of contamination between treatment groups. Researchers should adhere to SPIRIT and CONSORT reporting standards for clinical trials.
Future trials should further evaluate standardised measures of clients' mental health, adverse outcomes for clients, the potential benefits and harms to the consumer‐providers themselves (including need to return to treatment), and the financial costs of the intervention. They should utilise consistent, validated measurement tools and include a clear description of the consumer‐provider role (eg specific tasks, responsibilities and expected deliverables of the role) and relevant training for the role so that it can be readily implemented. The weight of evidence being strongly based in the United States, future research should be located in diverse settings including in low‐ and middle‐income countries.
Keywords: Adult, Humans, Peer Group, Case Management, Counseling, Counseling/methods, Counseling/organization & administration, Employment, Mental Disorders, Mental Disorders/therapy, Mental Health Services, Mental Health Services/legislation & jurisprudence, Mental Health Services/organization & administration, Patient Advocacy, Patient Participation, Patient Participation/methods, Patient Participation/trends, Quality of Life, Randomized Controlled Trials as Topic, Social Support
Plain language summary
Involving adults who use mental health services as providers of mental health services to others
Past or present consumers of mental health services can work in partnership with mental health professionals in 'consumer‐provider' roles, when providing mental health services to others. Their roles may include peer support, coaching, advocacy, specialists or peer interviewers, case management or outreach, crisis worker or assertive community treatment worker, or providing social support programmes. Until now, the effects of employing past or present consumers of mental health services, in providing services to adult clients of these services, have not been assessed rigorously.
We conducted a systematic review, comprehensively searching databases and other materials to identify randomised controlled trials which involved past or present consumers of mental health services employed as providers of mental healthcare services for adult clients. To be included, studies had to make one of two comparisons: 1) consumer‐providers versus professionals employed to do the same role within a mental health service, or 2) mental health services with and without consumer‐providers as an adjunct to the service.
We found 11 randomised controlled trials involving approximately 2796 people. The quality of the evidence is moderate to low; it was unclear in many cases whether steps were taken to minimise bias, both in the way that participants were allocated to groups, and in how the outcomes were assessed and reported.
Five of the 11 trials involving 581 people compared consumer‐providers to professionals who occupied similar roles within mental health services (case management roles (4 trials), and facilitating group therapy (1 trial)). There were no significant differences between the two groups, in terms of client (care recipient) quality of life, mental health symptoms, satisfaction, use of mental health services, or on the numbers of people withdrawing from the study. People receiving care from past or present users of mental health services used crisis and emergency services slightly less than those receiving care from professional staff. Past or present consumers who provided mental health services did so differently than professionals; they spent more time face‐to‐face with clients, and less time in the office, on the telephone, with clients' friends and family, or at provider agencies.
Six of the 11 trials, involving 2215 people, compared mental health services with or without the addition of consumer‐providers. There were no significant differences in quality of life, empowerment, function and social relations, in client satisfaction, attendance rates, hospital use, or in the numbers of people withdrawing from the study, between groups with consumer‐providers as an adjunct to professional care and those receiving usual care by health professionals alone. None of these six studies reported on clients' mental health symptoms. None of the studies reported on adverse outcomes (harms) for clients, or on the costs of providing the services.
Overall, we concluded that employing past or present consumers of mental health services as providers of mental health services achieves psychosocial, mental health symptom and service use outcomes that are no better or worse than those achieved by professional staff in providing care.
There is no evidence that the involvement of consumer‐providers is harmful. More high‐quality and well‐reported randomised trials are needed, particularly to evaluate mental health outcomes, adverse outcomes for clients, the potential benefits and harms to the consumer‐providers themselves (including a need to return to treatment), and whether it is cost‐effective to employ them. Future researchers should include a clear description of the consumer‐provider role and relevant training for the role so that it can be readily implemented, and should investigate consumer‐providers in settings outside the United States.
Background
Terms used in this review
In mental health services, the last 30 to 40 years has seen a slow but steady trend towards employment of past or present consumers of the service to work alongside mental health professionals. In this review, we call this role 'consumer‐provider', and use the term 'statutory mental health services' to refer to public services, those required by statute or law, or public services which involve statutory duties (i.e. specific duties required by law). In Appendix 1 we define key terms for this review, and describe our rationale for the choice of the term 'consumer‐provider'. We also explain the issues associated with the use of other terms (eg service users, survivors, peers).
The role of consumer‐providers can encompass peer support (Davidson 2012), coaching, advocacy, case management or outreach roles, crisis worker or assertive community treatment team, or providing clinical or social support programmes (Mowbray 1998). Past or present clients of mental health services can play other roles, such as providing a wholly consumer‐run or operated service (Segal 2011), including self‐help groups (Segal 1995) (sometimes known as consumer‐operated service providers (COSPs)) but our review does not assess this form of intervention. Nor does this review examine the role of consumers as trainers for professionals providing mental health services, or as researchers designing or conducting service evaluations (Coulter 2011); both of these interventions are important, however, and are the subject of companion reviews (Simpson 2003a; Simpson 2003b).
The protocol for this review was written by Emma Simpson and colleagues (Simpson 2003c) but they were unable to complete the review. The current authors completed the review using the scope of the original protocol because this is the standard expected of Cochrane reviews (see Acknowledgements). Referees of the review identified the need for a review of the evidence of user‐controlled consumer services, as well as an evaluation of the impact of service provision on consumer‐providers themselves, but these topics could not be assessed by this current review.
User involvement in mental health services
The consumer participation and self‐help movements have driven an increase in user involvement in mental health services, since at least the 1970s (Doughty 2011; Wright‐Berryman 2011). Providers of mental health services, like other health service providers, increasingly involve service users. Health policies often recommend the involvement of users in services, for example the United Kingdom (UK) Department of Health has an emphasis on patient and public involvement (Department 1999; Department 2001). Legislation also now may require such involvement (Campbell 2008a); an example is the UK Health and Social Care Act 2001. User involvement is often seen as intrinsically worthwhile (van Vugt 2012), but it can also have measurable effects (positive or negative) on client and service outcomes.
Despite encouragement of user involvement in service planning in Western Europe and North America, there are few rigorous assessments of its effects (Crawford 2002). Users have been involved as consumer‐providers internationally, including in the UK, Australia, the United States of America (USA) and Canada (Church 1989; Mowbray 1988; O'Donnell 1998; Perkins 1997; Salzer 2010). Data are limited on how widespread this practice is (Crawford 2003; Geller 1998), but there are indications that the consumer‐provider workforce is growing (Salzer 2010), spurred, for instance, by government funding and advocacy organisation support for service provision by peers (Segal 2011). The 2003 USA report of the President's New Freedom Commission on Mental Health (President 2003) helped to stimulate powerfully the "transformation of mental health services to a recovery orientation", in which consumer involvement is considered to be central.
How the intervention might work
This review assesses partnership approaches to service provision in the context of mental health, where service users work in partnership with mental health professionals in consumer‐provider roles integrated within statutory mental health services. Users can be involved as consumer‐providers within adult mental health services in a variety of ways. They can be employed in roles specifically designated for them, such as peer support specialists or peer interviewers (Lecomte 1999; Mowbray 1996; Salzer 2010; Pfeiffer 2011). Users can also be appointed to roles that apply to both users or non‐users, such as case management or outreach roles (Fisk 2000; Sherman 1991). Alternatively, user‐run programmes may be integrated into the mental health system that are closely linked with professional services, for example user‐run drop‐in centres (Brown 2010), or social support programmes for service users discharged from hospital (Chinman 2001; Kaufmann 1993).
Potential benefits and harms
van Vugt 2012 describes a fundamental belief that "involving consumers improves the health and quality of life of clients". However clients of mental health services can have divergent perceptions of the involvement of consumer‐providers. Some clients may prefer to receive services from consumer‐providers because they believe it will provide hope, or lead to more patient‐centred care, better understanding, or empathy with their condition (Chinman 2010; van Vugt 2012). However other clients may prefer to receive care from mental health professionals because they believe they have a greater capacity to meet their health needs (described by Campbell 2008a as a "credibility gap"). Consumer‐providers and mental health professionals may also differ in the outcomes they consider important for clients. While health professionals may be interested in therapeutic outcomes such as mental health symptoms, consumer‐providers and clients may have a greater interest in their overall quality of life.
Differences in the nature of consumer‐provider involvement compared to health professionals may also be important regarding how and where they spend their time and the potential impact this may have on relationships between clients and staff, use of available resources, or job satisfaction for staff (Salzer 2010). Services involving consumer‐providers may be seen as more engaging and accessible to clients (President 2003; van Vugt 2012), and may also be seen as empowering local communities (Greenfield 2008).
Why it is important to do this review
Involving consumers in mental health services has the potential to produce a number of benefits but there is also potential for harm. Mechanisms of involving consumer‐providers need to be carefully considered, and practice needs to be guided by evidence on effectiveness. Such evidence can be found from comparisons of services provided by consumers with services provided by mental health professionals. We aimed to assess current evidence from randomised controlled trials regarding the benefits and harms for clients of consumer‐providers in mental health services. We also aimed to look at service provision patterns when consumers are involved in service delivery.
The current review overlaps with an earlier review (Simpson 2002) of involving consumers as providers of mental health services. The earlier review identified eight trials for inclusion, of which three met our inclusion criteria. The current review updates the section in Simpson 2002 on employing users as providers, and additionally uses Cochrane systematic review methods.
A number of related Cochrane reviews exist. The most relevant is the planned review Van Ginneken 2011, which will examine the effects of non‐specialist health workers (NSHWs) such as doctors, nurses and lay providers, and professionals with other health roles (such as teachers and community workers) for providing mental health care in low and middle income countries. The main distinctions between Van Ginneken 2011 and the present review are the intervention provider and setting; we focus only on current or past clients of mental health services, as providers, and van Ginneken focuses only on low and middle income country settings. Nilsen 2006 examines the involvement of consumers in health policy and research, guideline development and patient information materials, but not in service provision. Dale 2008 assessed care provided by peers via telephone and found that it can be effective for certain health‐related concerns; some of the included studies assessed peer supporters versus healthcare professionals as callers, whilst others assessed peer support callers versus usual care (no telephone call). Lewin 2010 examines lay health workers in primary and community health care for improving maternal and child health and the management of infectious diseases.
This review is one of a suite of three reviews designed to assess different aspects of consumer involvement in mental health services, namely service provision, research (Simpson 2003a) and training (Simpson 2003b).
Objectives
To assess the effects of employing adults who are current or past consumers of mental health services, as providers of statutory mental health services.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Clients of statutory mental health services (ie. care recipients) who were 18 years and older and diagnosed with a mental health condition.
Types of interventions
Adults with current or past use of mental health services, involved as consumer‐providers, working in statutory services or in services that are integrated within statutory mental health services. Services needed to be specifically targeted for mental health purposes. (See Appendix 1 for definitions of key terms).
We considered that there was evidence of 'integration' in mental health services when:
mental health professionals and consumers worked together in a team; or
there was formal consultation between consumer‐providers and mental health professionals as part of the mental health service; or
there was recruitment, training, supervision or payment of consumer‐providers by statutory organisations.
Studies involving unpaid users as volunteers were also considered eligible if user roles were within, or integrated with, statutory mental health services.
Comparisons
We included:
studies comparing the effect of having a consumer‐provider in a role that would otherwise be occupied by a professional in a mental health service (consumer‐provider versus professional staff); and
studies comparing the effect of involving a consumer‐provider in addition to the usual mental health service (usual care plus a consumer‐provider as adjunct versus usual care) (see Figure 1).
1.
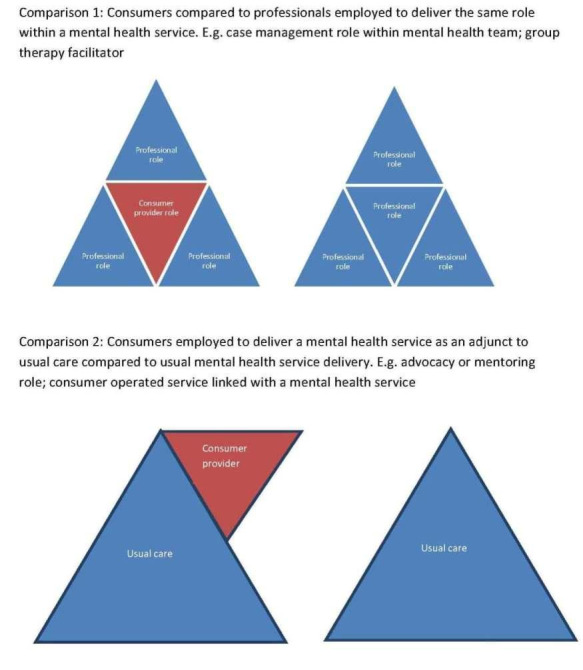
Graphical representation of comparisons 1 and 2
Exclusions
We excluded social services (such as employment or housing), befriending services, and forensic services for people with mental health conditions.
We excluded studies in which consumer involvement was limited to service planning or policy committees, or if consumers were involved in self‐help services that were run independently of statutory mental health services, or provided services that were not specifically mental health services.
Types of outcome measures
We present a detailed description of standard tools used to measure outcomes in the included studies in Table 1.
1. Outcome measurement tools.
| Tool | Abbreviation | Reference/s | Description | Outcome | Assessor | Studies |
| Lehman Quality of Life (also in Brief Version) | QOLI (and QOLI‐Brief) |
Lehman 1988 Lehman 1994 |
Subjective subscales: Life satisfaction, Daily activities, Family contact, Social relations, Finances, Health, Safety (score 1‐7). Objective subscales: Family contacts, Social relations (score 1‐5), Daily activities, Finances (score 0‐1). Higher scores better. |
Quality of life | Client self‐report (interview) | Sells 2006, Rivera 2007, Solomon 1995 |
| Quality of Life Index for Mental Health | QOLIMH | Becker 1993 | A brief 25‐item questionnaire modified from the Quality of Life Index for Mental Health. | Quality of life | Client self‐report | O'Donnell 1999 |
| Making Decisions Empowerment | MDE | Rogers 1997 | 28 items (score 1‐4). Responses are summed. Higher scores better (individual scale values reversed). | Empowerment | Client self‐report | Rogers 2007 |
| Personal Empowerment | PE | Segal 1995 | 20 items with two sub‐scales; 1) choice and 2) reduction in chance. Choice sub‐scale employs four point Likert scale . Reduction in Chance sub‐scale employs five‐point scale. Responses are summed. Higher scores better (individual scale values reversed). | Empowerment | Client self‐report | Rogers 2007 |
| Life Skills Profile | LSP | Rosen 1989 | A 39‐item measure of function and disability. Higher scores better. | Function | Case managers and families | Craig 2004 |
| Significant Others Scale | SOS | Power 1988 | Interview assesses size of social network and ratings of qualitative aspects of support provided by individuals in the network. | Social | Client self‐report (interview) | Craig 2004 |
| Hopkins Symptoms Checklist‐58 | HSCL‐58 | Derogatis 1974 | 58‐items on a four‐point scale. Higher scores worse. | Symptoms | Client self‐report | Bright 1999 |
| Brief Symptom Inventory | BSI | Derogatis 1983 | Measures clinically relevant symptoms (score 1‐5). Higher scores better. | Symptoms | Client self‐report | Rivera 2007 |
| Brief Psychiatric Rating Scale (also expanded version) | BPRS |
Overall 1962 Velligan 2005 |
18 items (expanded version has 24 items) rated on seven point scale. Higher scores worse. | Symptoms | Trained interviewer | Kaufmann 1995, Solomon 1995, |
| Symptom Check List‐90 | SCL‐90 | Derogardis 1977 | Self‐administered check list of 90 items rated on a five point scale (0 = not at all; 4 = extremely), eight sub scale scores were computed and three global indices, global severity index, positive symptoms distress index, and positive symptom total. | Symptoms | Client self‐report | Kaufmann 1995 |
| Beck Depression Inventory | BDI | Beck 1979 | 21‐item scale. Each item consists of four statements of depressive symptoms (score 0‐3) and assesses respondents mood in the past week. Maximum score 63 (≥19 indicates significant depressive symptoms). Higher scores worse. | Depression | Client self‐report | Bright 1999 |
| Hamilton Rating Scale for Depression (revised) | HRSD | Rehm 1985 | Observer‐rated scale for depressive symptomatology following clinical interview taking into account patient behaviour in the immediate preceding week (score 0‐52; 30 = severe illness). Higher scores worse. | Depression | Clinician | Bright 1999 |
| Behavioral Health Care Rating of Satisfaction | BHCRS | Dow 1995 | Client satisfaction with clinical staff and services (score 1‐6). Higher scores better. | Satisfaction | Client | Rivera 2007 |
| Verona Service Satisfaction Scale | VSSS | Cozza 1997 | 54 questions that cover seven dimensions: overall satisfaction, professionals’ skills and behaviour, information access, efficacy, types of intervention and relative’s involvement. Higher scores better. | Satisfaction | Client | Craig 2004 |
| Client Service Satisfaction Questionnaire | CSQ |
Larsen 1979 Greenfield 1989 |
Modified nine‐item scale. Higher scores better. | Satisfaction | Client | O'Donnell 1999 |
| Satisfaction with treatment | Hoult 1983, modifying Stein 1980 | Interview based 16 item scale to measure client satisfaction with all MH treatment (not case management services alone) on a 4‐point scale. Higher scores associated with greater satisfaction, authors note that they used a modified version of the instrument for assessing community treatment team approach | Satisfaction | Trained interviewer | Solomon 1995 | |
| Camberwell Assessment of Needs | CAN | Phelan 1995 | Sum score (possible score 0‐22). Higher scores worse. | Satisfaction | Can be rated independently by staff and clients | Craig 2004 |
| Barrett‐Lennard Relationship Inventory | BLRI | Barrett‐Lennard 1962 | 64 items, six point scale (1=definitely false, 6=definitely true). Higher score better. | client‐counselor relationship | client self‐report | Sells 2006 |
| Working Alliance Inventory | WAI |
Ralph 1992 Hovarth 1989 |
36 items (score 1‐7) equally divided across 3 subscales: Goals, Tasks, and Bonds. Higher scores better. | Client‐manager relationship | Client and case managers | Solomon 1995 |
Primary outcomes
Outcomes for clients (those receiving services)
1) Standardised measures of psychosocial outcomes (eg quality of life, function, social relations, empowerment) 2) Standardised measures of mental health (eg general symptoms, depression) 3) Adverse outcomes for clients, not captured in other primary outcomes We intended to include client subjective descriptions where these were treated as data in the study, for example with a set proportion of participants from both groups given the opportunity to comment.
Outcomes for service provision
4) Client satisfaction with service provision (or client‐manager relationship) 5) Use of services (eg uptake or drop‐out rates, crisis or emergency services use) 6) Service provision patterns (such as time spent by employees on various tasks, or times and locations of meetings with clients)
Secondary outcomes
7) Professionals' attitudes 8) Financial costs of service provision
Search methods for identification of studies
Electronic searches
We searched the following bibliographic databases using the terms and strategies listed in Appendices 2 to 7.
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, 2009, Issue 1)
MEDLINE (OvidSP): 1950 to March week 3, 2009
EMBASE (OvidSP): 1988 to week 11, 2009
PsycINFO (OvidSP): 1806 to March week 3, 2009
CINAHL (EBSCO): 1981 to March week 3, 2009
Current Contents (OvidSP): 1993 week 27 to week 12, 2009
For unpublished and ongoing trials, we contacted authors and other researchers in the field.
We updated searches in March 2012, as follows, using the abovementioned strategies unchanged with the exception of the PsycINFO strategy, the updated version of which is reported in Appendix 8:
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, 2012, Issue 3)
MEDLINE (OvidSP): 2009 to March 2012
EMBASE (OvidSP): 2009 to March 2012
PsycINFO (OvidSP): 2009 to March 2012 (Appendix 8).
Current Contents (OvidSP): 2009 to March 2012.
We were unable to update the search of CINAHL (EbscoHOST) in 2012, as the database was not working reliably.
Searching other resources
We searched the reference lists of potentially‐relevant articles that we obtained in full text.
Data collection and analysis
Selection of studies
The citations returned by the electronic searches were transferred into an Endnote library and the titles and abstracts were screened for inclusion independently by three review authors (RR, VP, DL) using the pre‐specified criteria. Review authors were not blinded to author names during the screening process. We obtained all potentially relevant articles in full text to assess their eligibility for inclusion (see Criteria for considering studies for this review). Disagreements regarding study eligibility were discussed between VP and DL (2009) or MP and DL (2012) until consensus was reached, or a third review author was consulted for a final decision. We provide reasons for the exclusion of potentially‐relevant studies in the Characteristics of excluded studies.
Data extraction and management
Data were collected from each of the included studies by one review author (DL, RR or VP) using a data extraction form specifically designed for this review. We extracted data on study design, settings, methods, participant characteristics, provider characteristics, interventions and outcomes. All data were checked by a second review author (DL, VP, RR or LB) and any discrepancies were discussed and corrected upon agreement. If there had been any unresolved disagreements, a third review author (MP) would have been involved through discussion until consensus was reached.
The data extraction sheet recorded:
study design;
numbers of participants in each treatment group;
characteristics of trial participants (including diagnoses and demographics of clients);
description of the service or setting of consumer‐provider involvement;
characteristics of consumer‐providers (number involved, diagnoses, demographics);
the mechanism of involving consumer‐providers (role description, training provided, support available);
details of mental health service provided to the intervention and comparison groups; and
outcomes (list of outcomes assessed, tools used, information regarding validity of tools, time points assessed, outcome data).
Outcomes were separated independently by two review authors (VP, DL) into those prespecified as primary and secondary outcomes for this review and those which did not appear to fit within our prespecified categories of outcomes. One of the review authors (SEH) provided clinical expertise to assess whether any of the additional outcomes identified should be included in the review. This rigorous process of data extraction and selection was necessary due to the large number of outcomes measured in multiple ways in the included trials.
Where data were not available in published reports of studies, we contacted study authors for further information.
Assessment of risk of bias in included studies
For each of the included studies, we assessed the following items to identify risk of bias in study outcomes and presented the findings in Risk of bias tables (see Characteristics of included studies), in accordance with Cochrane Handbook guidance (Higgins 2011):
adequate sequence generation
allocation concealment
blinding (blinding of participants for self‐reported outcomes, blinding of all other outcomes)
incomplete outcome data (reported separately for outcomes measured up to six months and outcomes measured after six months)
selective outcome reporting
comparability of groups at baseline
contamination between treatment groups
We contacted trial authors where information required to assess risk of bias was not reported. Any disagreements in assessment were resolved by discussion between VP and DL or by consulting a third author (MP) for a final decision.
Although blinding of participants was assessed for each study, it is important to acknowledge that the declared consumer status of the consumer‐provider is part of the intervention, therefore any impact on the results due to unblinded participants is attributed to the effects of the intervention rather than bias.
Measures of treatment effect
Based on the Criteria for considering studies for this review, we identified two possible pairwise comparisons for this review:
Comparison 1: Studies comparing the effect of having a consumer‐provider in a role that would otherwise be occupied by a professional in a mental health service (consumer‐provider versus professional staff); and
Comparison 2: Studies comparing the effect of involving a consumer‐provider in addition to the usual mental health service (usual care plus a consumer‐provider as adjunct versus usual care).
Figure 1 depicts these comparisons graphically.
We did not anticipate in advance there would be sufficient homogeneity of interventions and outcome measures to warrant meta‐analysis. However we found that several studies did report similar outcome measures, and we have presented pooled analyses wherever appropriate, as well as presenting individual study results using forest plots wherever sufficient data were available to do so.
For dichotomous outcomes, we analysed data based on the number of events and the number of people assessed in the intervention and comparison groups. We used the Mantel‐Haenszel method (random‐effects model) to calculate the risk ratio (RR) and 95% confidence interval (CI).
For continuous measures, we analysed data based on the mean, standard deviation (SD) and number of people assessed for both the intervention and comparison groups to calculate mean difference (MD) and 95% CI. If more than one study measured the same outcome using different tools, we calculated the standardised mean difference (SMD) and 95% CI using the inverse variance method in Review Manager 5 (random‐effects model). As SMD is not easily interpreted, pooled effect estimates expressed as SMD were back transformed by multiplying the SMD with an SD of a standard instrument used to measure the outcome (ie points on the Hopkins Symptoms Checklist (HSCL)‐58 scale). We imputed SD values using the average baseline SD values from the intervention and comparison arms of a trial that used the standard instrument of interest.
Where the same outcome was reported as dichotomous or continuous measures in separate studies (eg crisis/emergency service use), we pooled these outcomes using the generic inverse variance method in Review Manager 5. We calculated the SMD and standard error (SE) for each study (dichotomous outcomes were expressed as an odds ratio (OR) and converted to SMD) using standard formulae described in sections 7.7.7 and 9.4.6 of the Cochrane Handbook (Higgins 2011).
Dealing with missing data
We attempted to contact study authors for any information we were unable to collect from the published articles we had identified in our search. This included clarification of the involvement of consumer‐providers within studies, descriptions of how studies were conducted (eg method of random sequence generation, method of allocating participants to treatment groups), and requesting unpublished data for measured outcomes.
For outcomes assessed using measurement scales (eg quality of life scales, Brief Psychiatric Rating Scale) we presented overall scores wherever possible. If no overall score was provided, we reported results of sub‐scales considered to be most relevant to the outcome of interest, as recorded in the Notes section of the Characteristics of included studies.
If the number of people assessed for each outcome was not specified, this was imputed based on the number of people originally randomised to the treatment groups. For continuous measures, we imputed missing SD values based on reported values for standard error multiplied by the square root of the number of people assessed for the outcome. For dichotomous outcomes, percentages were used to impute missing raw data for the number of events or the number of people assessed. We recorded all data imputations in the Notes section of the Characteristics of included studies.
Assessment of heterogeneity
We assessed statistical heterogeneity visually using forest plots. Where more than one study measured the same outcome, the consistency of results across studies was assessed based on the degree of overlapping confidence intervals. We intended to explore any heterogeneity by referring to the characteristics of individual studies such as the population and type of intervention to try to account for any observed differences in outcomes. We chose not to consider the Chi2 statistic to measure statistical heterogeneity, given that this test has low power in meta‐analyses involving small sample size or few studies (Higgins 2011, section 9.5.2)
Assessment of reporting biases
We attempted to identify potential outcome reporting bias using a matrix listing the outcomes measured in each of the studies (based on outcome assessments described in the published articles). We compared whether sufficient data were available for meta‐analysis or whether data were incompletely reported or not available in the published articles. We present this information in Table 2.
2. Missing data and outcome reporting bias.
| Outcome | Studies assessed outcome |
n studies with outcome data (total N included in analysis) |
n studies with incomplete data (total N randomised) |
| COMPARISON 1 (n = 5) | |||
| Primary outcomes | |||
| QOL | 3 | 1 (130) | 2 (233) |
| Function | 3 | 1 (130) | 2 (233) |
| Social | 3 | 1 (130) | 2 (233) |
| Symptoms | 3 | 2 (197) | 1(96) |
| Depression | 2 | 1(67) | 1(96) |
| Satisfaction | 2 | 2 (213) | 0 |
| Client manager relationship | 2 | 2 (160) | 0 |
| Use of mental health services | 3 | 2 (227) | 1 (137) |
| Client attrition | 5 | 3 (333) | 2 (250) |
| Hospital admissions | 2 | 1 (114) | 1 (96) |
| Crisis/Emergency services | 3 | 2 (250) | 1 (96) |
| Length of stay | 2 | 1 (136) | 1 (96) |
| Secondary outcomes | |||
| Providers' attitudes | 1 | 1 (96) | 0 |
| COMPARISON 2 (n = 6) | |||
| Primary outcomes | |||
| QOL | 1 | 0 | 1 (84) |
| Function | 3 | 1 (45) | 2 (208) |
| Social | 2 | 1 (45) | 1 (89) |
| Symptoms | 1 | 0 | 1 (90) |
| Sense of community | 1 | 0 | 1 (89) |
| Motivation for change | 1 | 0 | 1 (89) |
| Self‐determination | 1 | 0 | 1 (89) |
| Hope | 1 | 0 | 1 (89) |
| Satisfaction | 2 | 2 (125) | 0 |
| Client manager relationship | 1 | 0 | 1 (89) |
| Use of mental health services | 1 | 1 (45) | 0 |
| Client attrition | 3 (218) | 3 (199) | |
| Hospital admissions | 3 (199) | 1 (84) | |
| Crisis/emergency services | 1 | 0 | 1 (84) |
| Length of stay | 4 | 3(199) | 1 (84) |
| Secondary outcomes | |||
| Providers' attitudes | 3 | 1 (45) | 2 (173) |
Data synthesis
We calculated estimated effects of the intervention and CIs for all primary and secondary outcomes wherever possible. We anticipated that interventions were likely to be heterogeneous across studies, and therefore we planned to conduct analyses using a random‐effects model. If more than one study measured the same outcome, we pooled the results to provide a summary estimate of the effect across studies. We planned to report findings for the different comparison groups separately. For each comparison, we planned to report measures of treatment effect as point estimates with 95% CIs wherever possible, and acknowledge instances where outcomes may have been measured but we were unable to calculate a summary estimate. Where outcomes were measured at multiple time points within individual studies, we have presented outcome data collected at the longest follow up point. We describe findings for each outcome in the text of the review with consideration of the potential impact of bias on the size or direction of the effect. We interpreted results that reached statistical significance with respect to clinical importance based on input from a clinical expert (SEH).
Consumer participation
This draft review was sent to two mental health consumers (one consumer‐researcher and one consumer‐employee) in the UK and Australia as part of the Cochrane Consumers and Communication Review Group's refereeing process. Their feedback was particularly helpful in prompting clarification of terminology and concepts described in this review.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies.
Results of the search
Searches run in March 2009 generated 9815 records. We removed duplicate records and screened the titles and abstracts of all citations to identify 196 articles that were potentially eligible for inclusion. We reviewed these in full text against the selection criteria, and identified ten studies that met the inclusion criteria. Seven of these ten studies were reported in multiple publications (see Additional Table 3).
3. Included studies reported in multiple publications.
| Study | Other papers reporting study |
| Clarke 2000 | Herinckx 1997; Paulson 1996; Paulson 1999 |
| Craig 2004 | Doherty 2004 |
| Gordon 1979 | Edmunson 1982; Edmunson 1984; Gordon 1979b |
| O'Donnell 1999 | O'Donnell 1998 |
| Rogers 2007 | Johnsen 2005 |
| Sells 2006 | Jewell 2006; Sells 2008 |
| Solomon 1995 | Solomon 1994a; Solomon 1994b; Solomon 1995b; Solomon 1995c; Solomon 1995d; Solomon 1996a; Solomon 1996b |
We attempted to contact authors of each of the included studies to obtain additional information, but we were only able to clarify details for three studies (Bright 1999; Craig 2004; Sells 2006).
One author (MP) updated the searches in March 2012, resulting in 3776 records. After duplicates were removed, 2691 records remained. These were initially screened by one author (MP) and 1902 records were excluded as clearly not meeting the inclusion criteria. Two authors (DL, MP) assessed the remaining 789 records and rejected 755 as clearly not meeting the inclusion criteria. The authors obtained the remaining 34 papers in full text. These 34 papers reported on 26 studies. Five were reviews and 2 were book chapters not reporting particular trials; 2 studies were already included in the review (Rogers 2007; Sells 2006); 11 studies were excluded as not meeting the inclusion criteria; 2 studies had already been excluded; 2 studies are ongoing (Chinman 2012; Tondora 2010); 1 newly‐identified study awaits further information in order to be classified (Kroon 2011); 1 study was included (Sledge 2011). A further study identified through the reference list in Gordon 1979 is awaiting further information in order to be classified (Stone 1979) .
Included studies
Eleven trials met the selection criteria for this review. Of these, five trials compared an intervention where the only difference was the involvement of a consumer‐provider in the intervention group in a role that was fulfilled by a professional in the comparison group (Comparison 1: Bright 1999; Clarke 2000; Rivera 2007; Sells 2006; Solomon 1995). Six studies compared groups receiving usual care with groups receiving services from consumer‐providers in addition to usual care (Comparison 2: Craig 2004; Gordon 1979; Kaufmann 1995; O'Donnell 1999; Rogers 2007; Sledge 2011).
Three of the 11 included studies had three‐armed comparisons (Clarke 2000; O'Donnell 1999; Rivera 2007). We included for analysis only the arms that met the inclusion criteria. For more information see Characteristics of included studies.
Sample sizes
Sample sizes ranged from 45 to 1827 participants, with a total of 2796 participants in the 11 studies addressing the 2 main comparisons in this review.
Setting
Trials were conducted in state‐ or community‐based outpatient clinics within statutory mental health services. Two studies involved statutory services linked with consumer‐operated service providers (COSPs) (Rogers 2007; Sells 2006). Nine studies were conducted in the USA (Bright 1999; Clarke 2000; Gordon 1979; Kaufmann 1995; Rivera 2007; Rogers 2007; Sells 2006; Sledge 2011; Solomon 1995); two of these were multi‐site trials (Rogers 2007; Sells 2006). One study was conducted in the United Kingdom (Craig 2004) and one in Australia (O'Donnell 1999).
Participants
Participants (clients receiving services) in the 11 included studies were adult clients of statutory mental health services, who had severe mental health diagnoses including psychotic illnesses and major mood disorders. Bright 1999 included participants with a score of ten or higher on the Hamilton Rating Scale for Depression, and meeting the Structured Clinical Interview DSM‐III‐R criteria for current episode of definite major depressive disorder, dysthymia, or depression not otherwise specified. The remaining ten trials all involved participants with severe mental illnesses. Of these, three studies did not specify the type of illness (Craig 2004; Gordon 1979; Solomon 1995) and seven studies included people with both psychotic and mood disorders (Clarke 2000; Kaufmann 1995; O'Donnell 1999; Rivera 2007; Rogers 2007; Sells 2006; Sledge 2011).
Four studies did not describe any participant exclusion criteria (Gordon 1979; Rivera 2007; Sells 2006; Solomon 1995). The other seven studies (Bright 1999; Clarke 2000; Craig 2004; Kaufmann 1995; O'Donnell 1999; Rogers 2007; Sledge 2011) had varying exclusion criteria for potential participants (see Characteristics of included studies.)
Interventions
In all 11 trials, the interventions were delivered by consumer‐providers within statutory mental health settings, or as an adjunct to statutory mental health services. We provide a detailed description of interventions in the Characteristics of included studies.
Of the five studies comparing consumer‐providers and professional staff in the same role (Comparison 1), four of the studies involved consumer‐providers in a case management role within a mental health team (Clarke 2000; Rivera 2007; Sells 2006; Solomon 1995). The remaining study trained consumer‐providers as facilitators of mutual support group therapy or cognitive behavioural therapy sessions that were otherwise facilitated by professional staff (Bright 1999).
Of the six studies assessing consumer‐providers as an adjunct to usual care (Comparison 2), four studies involved consumer‐providers in mentoring or advocacy roles (Craig 2004; Gordon 1979; O'Donnell 1999; Sledge 2011) and two studies referred clients to consumer‐operated services that were integrated with traditional mental health services in addition to usual care (Kaufmann 1995; Rogers 2007).
Consumer‐providers
Consumer‐providers were recruited through formal advertising (Sledge 2011), mental health services (Gordon 1979; O'Donnell 1999) or from existing self‐help groups (Bright 1999), consumer‐operated drop in centres (Clarke 2000), peer advocacy programs (Rivera 2007) and peer engagement projects (Sells 2006). Four studies did not describe how consumer‐providers were recruited (Craig 2004; Kaufmann 1995; Rogers 2007; Solomon 1995). The number of consumer‐providers in the included studies ranged from two to nine, with no studies providing a rationale for the number recruited.
The employment history and other relevant experience of consumer‐providers was reported only in Bright 1999 (with half having previously led self‐help groups and most holding a bachelor degree) and Craig 2004 (with consumer‐providers having been unemployed for some years at the time of employment) (see Characteristics of included studies). Their diagnoses were reported in Clarke 2000 (self‐identified mental health consumers with a DSM‐III‐R axis I diagnosis); Rivera 2007 (history of multiple hospitalisations for mood or psychotic disorders, eligible for disability benefits, reliant on medication and having three to eight years of stability in the community); and Sells 2006 (some had a history of co‐occurring drug use disorder).
In O'Donnell 1999, those delivering the intervention initially comprised present or past consumers of mental health services, 'secondary' consumers (carers or siblings of primary consumers), or lay individuals. After a brief period, as a result of employee turnover, only primary consumers were employed.
Consumer‐provider training and support
Studies varied in the degree of training and ongoing support given to consumer‐providers. Most studies described an initial intensive training period lasting for between two days and six weeks, followed by ongoing supervision (weekly or monthly sessions) and support (eg telephone debriefing).
Excluded studies
We list the 48 studies excluded from this review, with reasons, at Characteristics of excluded studies. Eleven of these studies appeared to meet the review's selection criteria, but were later excluded. These studies investigated mental health services involving consumer‐providers that were compared to a different mental health service that did not involve consumer‐providers (Cook 2012a; Forchuk 2005; Greenfield 2008; Jonikas 2011; Lafave 1996; Lehman 1997; Liberman 1998; Quinlivan 1995; Reynolds 2004; Salyers 2010; Sytema 2007). We excluded these studies as we were unable to disentangle the effects of consumer‐providers in studies comparing two different complex interventions (see 11 studies listed as "comparison group differed on more factors than consumer‐provider alone" in Characteristics of excluded studies).
The main reasons for excluding studies were:
the intervention was not integrated within statutory mental health services (17 studies);
the comparison group differed by more factors than the consumer‐provider role (11 studies);
allocation to treatment groups was not randomised (or not adequately randomised) (9 studies).
Risk of bias in included studies
We present 'Risk of bias' Information in Characteristics of included studies and Figure 2 and Figure 3.
2.
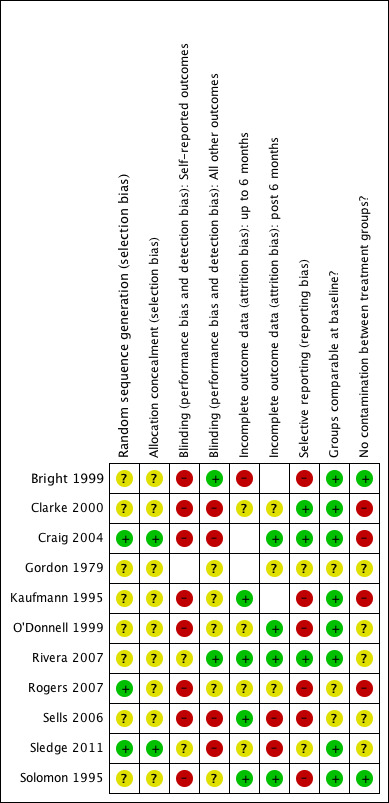
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
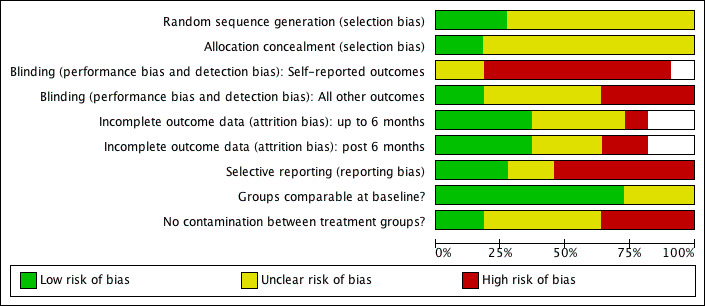
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
All of the five studies comparing consumer‐providers to professionals in the same role (Comparison 1) describe random assignment of participants to treatment groups but do not provide enough information about whether participants were truly randomised or whether group allocations were concealed.
Three of the six studies assessing consumer‐providers as an adjunct to usual care (Comparison 2) describe adequate randomisation methods (Craig 2004; Rogers 2007; Sledge 2011). Two of these describe concealment of allocation (Craig 2004; Sledge 2011).
Overall, there is an unclear risk of selection bias in the trials' results.
Blinding
Participants and providers
None of the clients or care providers in any of the studies was considered blind to treatment assignment, because disclosure of consumer‐provider status was an important part of the intervention. Because the primary outcomes of the review rely largely on self‐reported assessments (eg quality of life, function, social interaction, mental health symptoms, and service satisfaction) the clients' beliefs about consumer‐providers' effectiveness were likely to have affected their assessment of these outcomes.
Outcome assessors
Only two (Bright 1999; Rivera 2007) of the five studies in Comparison 1 stated that outcome assessors were blind to group assignment. Data reported for service use outcomes (eg hospital admissions, crisis/emergency service) may be subject to detection bias where outcome assessors were not blinded. Clarke 2000 and Rivera 2007 both reported data for these outcomes, however Clarke 2000 did not blind outcome assessors.
Only one study (Kaufmann 1995) in Comparison 2 stated that outcome assessors were unaware of group assignment, but we were unable to obtain data from this study for inclusion in this review. Craig 2004; Gordon 1979 and Sledge 2011 reported service use data; outcome assessors were not blind to group assignment and had a vested interest in seeing the intervention succeed in these studies.
Overall, the lack of blinding of participants, care providers and outcome assessors creates an unclear to high risk of bias in the trials' results.
Incomplete outcome data
The five studies in Comparison 1 reported losses to follow up ranging from 6% to 30% of the total participants. Losses were balanced across treatment groups in Bright 1999 and Solomon 1995. It was unclear whether losses were balanced across groups in Clarke 2000 or Rivera 2007. Sells 2006 reported greater loss of participants in the assertive community treatment (ACT) group without consumer‐providers. The reasons for losses were poorly reported; it is unclear whether the losses may have biased these studies' results and, if so, in which direction.
Four of the six studies in Comparison 2 reported minimal losses (ie less than 10%) that were balanced across groups and unlikely to bias outcomes. However, Rogers 2007 reported 20.5% of participants were lost to follow up without describing whether losses were balanced across groups; disproportionate losses in either group may have biased outcomes in either direction. In Sledge 2011, 17% of participants withdrew consent post‐randomisation (balanced between groups), and while it appears that service use data are reported for all of the remaining participants, the authors note that they did not have verifiable data on whether patients were hospitalised at other facilities during the follow‐up period.
Overall, the studies are at low to unclear risk of attrition bias.
Selective reporting
In order to indicate potential outcome reporting bias in this review, we compared the number of studies (and total participants) contributing data for each of the outcomes, to the number of studies (and total participants) that were likely to have measured outcomes but reported limited data (insufficient to include in a meta‐analysis) or did not report all outcomes that were measured (see Table 2).
Three of the five studies in Comparison 1 selectively reported only some of the outcomes that were measured (Bright 1999; Sells 2006; Solomon 1995).
Only one of the six studies in Comparison 2 reported data for all outcomes measured (Craig 2004). Selective outcome reporting was indicated in four of these studies (O'Donnell 1999; Kaufmann 1995; Rogers 2007; Sledge 2011); however, correspondence with the authors of Sledge 2011 indicates that a manuscript is under preparation for the secondary outcomes assessed in the trial. Further, data for Gordon 1979 were poorly reported and it was not possible to determine how many of the 80 people randomised were allocated to each group.
Overall, 6 of the 11 included studies are at high risk of bias in terms of selective outcome reporting.
Other potential sources of bias
All of the five studies with direct comparisons of consumer‐providers to professionals in the same role (Comparison 1) reported comparability of groups at baseline and none of these studies was considered at risk of confounding through contamination of treatment groups (eg participants in the comparison group receiving services from a consumer‐provider instead of a professional).
Four of six studies in Comparison 2 involved treatment groups that were comparable at baseline. For the remaining two studies this could not be determined (Gordon 1979; Rogers 2007). Most of these studies were at high risk of contamination between treatment groups due to comparison groups having partial or complete access to the consumer‐provider intervention that could lead to an underestimate of the effects of the intervention (Craig 2004; Kaufmann 1995; Rogers 2007). Two studies indicated participants were able to continue receiving standard mental health services and access the consumer‐provider intervention regardless of randomised assignments (Kaufmann 1995; Rogers 2007). This resulted in equal numbers of participants from both groups accessing the intervention in Kaufmann 1995, cancelling out the effect of randomisation. It is unclear how this may have affected study outcomes for Rogers 2007.
Most of the included studies declared their funding sources which included National or Commonwealth mental health department or health institute grants (Clarke 2000; Kaufmann 1995; O'Donnell 1999; Rogers 2007; Sells 2006; Sledge 2011; Solomon 1995) and other sources ( Rivera 2007; see also Characteristics of included studies). Sledge 2011 received some funding from a pharmaceutical company. Bright 1999; Gordon 1979 and Craig 2004 did not report their funding source. No study discussed the funders' role and degree of input to the study.
Effects of interventions
We analyse and present separately the effects of interventions for each of the two comparisons in this review (see Figure 1):
Consumer‐providers versus professionals employed to do the same role within a mental health service;
Mental health services with and without consumer‐providers as an adjunct to the service.
For each of these comparisons, we assessed the effect of interventions on clients receiving services (psychosocial, mental health, adverse outcomes) as well as outcomes for service provision (client satisfaction with service provision, use of services, service provision patterns) (see Types of outcome measures). We assessed secondary outcomes of professionals' attitudes and financial costs associated with service provision. We analysed outcomes measured at the longest follow‐up time (typically 12 months). We provide further information and references for outcome measurement tools in Table 1.
We present qualitative effects of interventions on consumer‐providers across all studies separately (see Discussion: Qualitative outcomes).
Comparison 1: Consumer‐provider versus professional
Five low to moderate quality studies compared consumer‐providers in the intervention group and professionals employed in the same role in the comparison group (Bright 1999; Clarke 2000; Rivera 2007; Sells 2006; Solomon 1995).
Summary
Overall, the five studies found no difference in psychosocial, mental health and client satisfaction outcomes. They found a small reduction in use of crisis and emergency service use in clients receiving services from consumer‐providers, but no other difference in service use. There were different service provision patterns in the intervention and comparison group, including a lower caseload for consumer‐providers. One study found no difference in provider perspectives of the client‐manager relationship in either group. The five studies did not report adverse outcomes for clients or financial costs.
Primary outcomes for clients receiving services
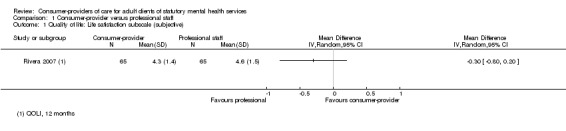
1) Standardised measures of psychosocial outcomes (quality of life, function, social relations)
Three studies (Rivera 2007; Sells 2006; Solomon 1995) used the Lehman Quality of Life Interview (QOLI), but data were not available from two of the studies (N = 233) (Sells 2006; Solomon 1995). The third study, Rivera 2007 (130 participants), assessed the effect of consumer‐providers within a strengths‐based intensive case management team compared to using licensed clinical social workers in the same role. There was no significant difference between groups after 12 months regarding life satisfaction (mean difference (MD) ‐0.30 (95% CI ‐0.80 to 0.20) Analysis 1.1), daily activities (MD 0.00 (95% CI ‐0.07 to 0.07) Analysis 1.2), or social relations (MD ‐0.10 (95% CI ‐0.48 to 0.28) Analysis 1.3). The results are consistent with Sells 2006 and Solomon 1995 that both found no difference in these QOLI subscales for participants receiving case management services with and without consumer‐providers.
1.1. Analysis.
Comparison 1 Consumer‐provider versus professional staff, Outcome 1 Quality of life: Life satisfaction subscale (subjective).
1.2. Analysis.
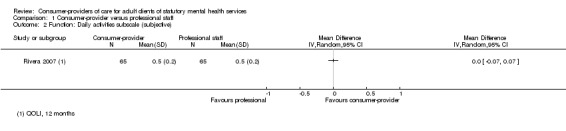
Comparison 1 Consumer‐provider versus professional staff, Outcome 2 Function: Daily activities subscale (subjective).
1.3. Analysis.
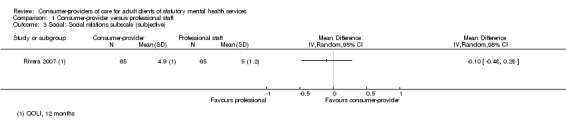
Comparison 1 Consumer‐provider versus professional staff, Outcome 3 Social: Social relations subscale (subjective).
Although we could not determine whether adequate randomisation and allocation concealment had occurred in these studies, it is unlikely that selection bias has significantly impacted these results. Inclusion of missing data from Sells 2006 and Solomon 1995 is likely to strengthen the evidence of no difference between clients managed by consumer‐providers or professional staff.
2) Standardised measures of mental health (general symptoms, depression)
General symptoms
Three studies used different tools to measure mental health symptoms (Bright 1999; Rivera 2007; Solomon 1995. See Table 1). We were unable to calculate a summary estimate for Solomon 1995 (N = 96). Bright 1999 conducted two parallel studies involving 98 participants comparing the effect of consumer‐providers and health professionals leading a 10‐week course in either mutual support group therapy or cognitive behaviour therapy. There was no difference in symptoms between groups immediately post‐intervention (N = 67) using the Hopkins Symptoms Checklist‐58. This is consistent with Rivera 2007 (N = 130) that showed no difference in Brief Symptom Inventory scores after 12 months of case management services. The pooled estimate of effect is ‐0.24 SMD (95%CI ‐0.52 to 0.05, P = 0.10) (Analysis 1.4) indicating there was no difference in symptoms between the groups. These results are consistent with Solomon 1995 which reported no difference between groups in symptoms measured by the Brief Psychiatric Rating Scale (BPRS). Inclusion of the missing data from Solomon 1995 in the pooled analysis would probably increase the precision of the results indicating no difference between the groups. It is unlikely that the potential selection bias identified in these studies would have significantly influenced these results.
1.4. Analysis.
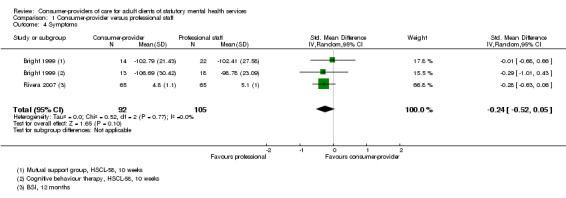
Comparison 1 Consumer‐provider versus professional staff, Outcome 4 Symptoms.
Depression
One study (Bright 1999) measured depression using the Beck Depression Inventory. There was no significant difference in self‐reported depression for participants in mutual support group (MSG) therapy led by consumer‐providers compared to professional employees (MD 3.61 (95% CI ‐1.37 to 8.59) Analysis 1.5.1) however the wide confidence interval means we cannot rule out that some clients of consumer‐providers will have higher (worse) scores. For cognitive behavioural therapy (CBT), clients of consumer‐providers had lower (better) scores for depression, however this difference did not reach statistical significance (MD ‐5.57 (95% CI ‐12.90 to 1.76) Analysis 1.5.1). When providers assessed depression using the Hamilton Rating Scale for Depression (MSG therapy: MD 2.43 (95%CI ‐0.58 to 5.44), CBT: MD 1.32 (95%CI ‐2.26 to 4.90) Analysis 1.5.2) there was no strong evidence of a clinical difference between the groups. Solomon 1995 measured depression as a separate subscale of the BPRS and reported no differences between groups, but did not provide sufficient data to include in a meta‐analysis.
1.5. Analysis.
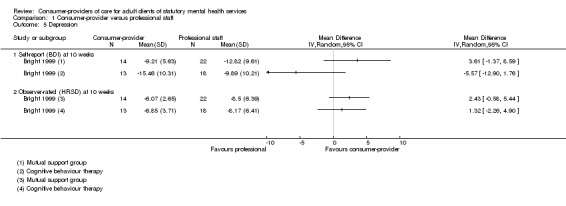
Comparison 1 Consumer‐provider versus professional staff, Outcome 5 Depression.
Although outcome data for Bright 1999 were incomplete, the attrition was balanced across the groups and hence is unlikely to have biased these outcomes.
3) Adverse outcomes for clients
There were no adverse outcomes reported for clients in the five studies comparing consumer‐providers to professionals in the same role within mental health services.
Primary outcomes for service provision
4) Client satisfaction with service provision
Two studies assessed participant satisfaction; one study used the Behavioural Health Care Rating of Satisfaction (Rivera 2007) and one study used the trialists' own trial‐specific tool to assess satisfaction with treatment (16 items assessed using a four‐point scale, Solomon 1995). A pooled estimate (2 studies, total N = 213) indicates there is no significant difference in satisfaction between groups (SMD ‐0.22 (95%CI ‐0.69 to 0.25), P = 0.35) (Analysis 1.6).
1.6. Analysis.
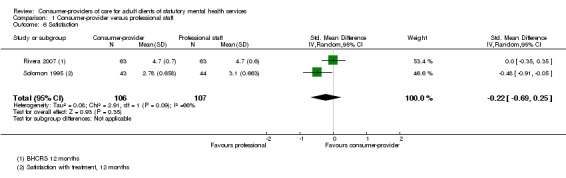
Comparison 1 Consumer‐provider versus professional staff, Outcome 6 Satisfaction.
Client‐manager relationship
Two studies reported participant assessment of the client‐manager relationship (Sells 2006; Solomon 1995). Sells 2006 used the Barrett‐Lennard relationship inventory at 12 months and Solomon 1995 used the Working Alliance Inventory at 2 years. The pooled estimate shows no significant difference between groups (total N = 160; SMD 0.22 (95%CI ‐0.10 to 0.53), P = 0.18) (Analysis 1.7).
1.7. Analysis.
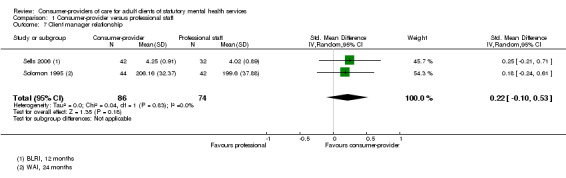
Comparison 1 Consumer‐provider versus professional staff, Outcome 7 Client manager relationship.
5) Use of services (mental health services, crisis/emergency services, hospital use, client attrition)
Use of mental health services
Three studies (Rivera 2007; Solomon 1995; Sells 2006) assessed the uptake of mental health services provided to participants. We were unable to calculate summary estimates for Sells 2006. Rivera 2007 used hospital records to assess how many additional individual or group rehabilitation therapy sessions participants accessed in 12 months. There was no significant difference between groups (individual therapy: MD 0.00 (95%CI ‐0.08 to 0.08); group therapy: MD 1.90 (95%CI ‐1.18 to 4.98)) (Analysis 1.8.1). In Solomon 1995, the number of hours of rehabilitation services used in 12 months appeared skewed for each treatment group, and the summary estimate is imprecise, as indicated by the wide confidence interval (MD ‐70.89 (95%CI ‐248.84 to 107.06)).
1.8. Analysis.
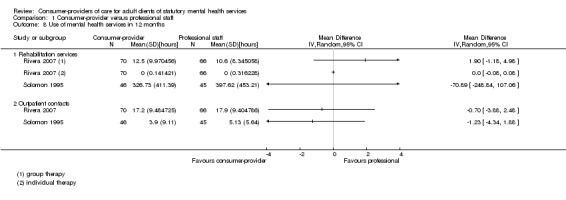
Comparison 1 Consumer‐provider versus professional staff, Outcome 8 Use of mental health services in 12 months.
Rivera 2007 and Solomon 1995 also assessed use of outpatient services (Analysis 1.8.2). Solomon 1995 reported outpatient service use for 91 participants with no significant difference in favour of either group at 12 months (MD ‐1.23 (95%CI ‐4.34 to 1.88)), consistent with Rivera 2007 (MD ‐0.70 (95% CI ‐3.88 to 2.48). Sells 2006 reported no difference between groups in service use over 12 months, but did not provide sufficient data to include in a meta‐analysis.
Potential selection bias from inadequate randomisation or concealment of allocation has not resulted in outcomes that strongly favour either treatment group in these studies.
Crisis/emergency service use
Three studies compared client use of crisis or emergency services in each of the treatment groups (Clarke 2000; Rivera 2007; Solomon 1995). Pooled summary estimates of 2‐year data from Clarke 2000 and 12‐month data from Rivera 2007 show a small but significant reduction in crisis or emergency service use in clients within the consumer‐provider group (SMD ‐0.34 (95% CI ‐0.60 to ‐0.07) P = 0.01) (Analysis 1.14). These findings are based on self‐reported use of services collected at 6‐monthly (Clarke 2000) or monthly interviews (Rivera 2007). It is unlikely that potential selection bias may have significantly influenced results of these studies, however the accuracy of the results are likely to be affected by the participants' ability to recall their use of services. It is unclear whether participant awareness of treatment allocation in Clarke 2000 may have biased this self‐reported outcome measure and what direction the bias would be (this could depend on the participant's belief in the capability of the different providers as to whether they are likely to under‐report or exaggerate their need for these services).
1.14. Analysis.
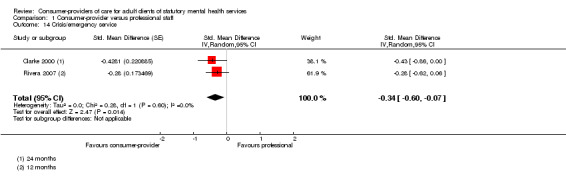
Comparison 1 Consumer‐provider versus professional staff, Outcome 14 Crisis/emergency service.
Solomon 1995 reported no difference in service use between groups, but did not provide sufficient data to include in a meta‐analysis. Inclusion of missing data from Solomon 1995 may render the pooled effect non‐significant.
Hospital use
Two studies collected data regarding hospital admission (Clarke 2000; Solomon 1995). Although fewer people were admitted to hospital in the consumer‐provider group in Clarke 2000, this difference did not reach statistical significance and the confidence interval incorporates both increased and decreased risk of admission in the consumer‐provider group (RR 0.68 (95% CI 0.45 to 1.03), Analysis 1.15). This finding is based on self‐reported recall of hospitalisation at interviews conducted every 6 months for 114 participants who were aware of treatment allocation. Potential selection bias or performance bias did not result in an effect estimate that significantly favours either group.
1.15. Analysis.
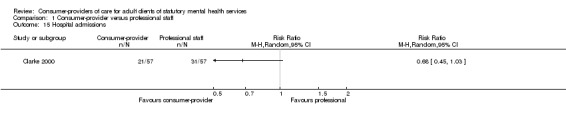
Comparison 1 Consumer‐provider versus professional staff, Outcome 15 Hospital admissions.
We were unable to calculate a summary estimate for Solomon 1995 which reported no difference between groups. As Clarke 2000 and Solomon 1995 both involve similar numbers of participants, incorporating missing data from Solomon 1995 in a pooled analysis with Clarke 2000 is unlikely to show a significant difference between groups.
Two studies collected information on length of hospital stay. Rivera 2007 compared the length of stay for 136 participants and found no significant difference between groups (MD 1.10 (95% CI ‐0.72 to 2.92), Analysis 1.16). We were unable to calculate a summary estimate for Solomon 1995 which reported no significant difference between groups. Depending on the measure of variance in the outcome data of Solomon 1995, it is unclear whether inclusion of this missing data for 96 participants in a pooled analysis would result in an overall significant difference in hospital stays between the groups.
1.16. Analysis.
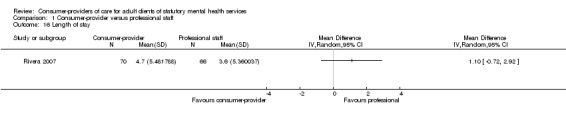
Comparison 1 Consumer‐provider versus professional staff, Outcome 16 Length of stay.
Client attrition
All five studies in Comparison 1 (consumer‐provider versus professional staff) experienced dropouts or described reasons why participants were unable to be assessed at follow up. We were unable to determine whether losses were balanced across treatment groups in Clarke 2000 (20/178 across all three arms; 11% attrition overall) or Rivera 2007 (52/255 across all three arms; 20% attrition overall). Most of the lost participants in Clarke 2000 failed to commence treatment with the assigned provider, and it is unclear whether this related to group assignment. Most of the losses in Rivera 2007 were due to participants being discharged to long‐term residential care that precluded enrolment in the clinic‐based arm of the trial, although the trialists state there were no differences in the characteristics of participants who were excluded and those who remained in the study. The other three studies ranged in overall attrition from 5% (Solomon 1995) to 46% (Sells 2006) and losses were balanced across groups (RR 0.80 (95%CI 0.58 to 1.09), P = 0.16) (Analysis 1.9).
1.9. Analysis.
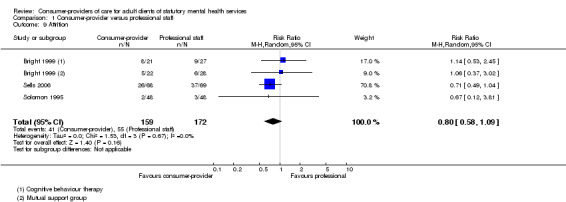
Comparison 1 Consumer‐provider versus professional staff, Outcome 9 Attrition.
6) Service provision patterns (caseload, time allocated to tasks, location of services, case manager tasks)
Caseload
Of the five studies in Comparison 1, only two studies appeared to have balanced caseloads between the consumer‐provider and professional staff groups (Bright 1999; Solomon 1995). In Analysis 1.10 we present a comparison of caseload, number of personnel, or number of clients assigned to each treatment group. Clarke 2000 had lower numbers of clients in the consumer‐provider groups compared to the professionals. The workload of individual personnel also differed between treatment groups in Rivera 2007, in which four consumer‐providers were employed at half‐time compared to two professionals that were employed full‐time. It is unlikely these small differences would significantly bias performance in favour of consumer‐providers, however this is not the case for Sells 2006 in which consumer‐providers had approximately half the caseload compared to professional staff. Significant differences in caseload or the time spent with clients may have biased outcomes in favour of the service delivered by consumer‐providers in this study.
1.10. Analysis.
Comparison 1 Consumer‐provider versus professional staff, Outcome 10 Service provision: Caseload/personnel.
| Service provision: Caseload/personnel | |||
|---|---|---|---|
| Study | Description | Consumer‐provider | Professional staff |
| Bright 1999 | Caseload (Mutual support groups) | n = 22 | n = 27 |
| Bright 1999 | Caseload (Cognitive behavioural therapy groups) | n = 21 | n = 27 |
| Clarke 2000 | Average caseload | 4.6 clients/case manager | 5.4 clients/case manager |
| Rivera 2007 | Personnel | 4 x 0.5 EFT personnel (n = 70) | 2 x 1.0 EFT personnel (n = 66) |
| Sells 2006 | Average caseload | 10 to 12 clients/case manager | 20 to 24 clients/case manager |
| Solomon 1995 | Personnel | 4 personnel (n = 48) |
4 personnel (n = 48) |
Time allocated to tasks
Two studies compared the time that consumer‐providers and professionals spent on different tasks within a case manager's role (Clarke 2000; Solomon 1995). We were unable to calculate summary estimates for Clarke 2000 which reported the percentage of overall time spent with the team, clients, alone, or with family members, staff and other agencies or operators. Clarke 2000 reported no differences between consumer‐providers and professionals in how much time was spent across each of the different categories (Analysis 1.11). In Solomon 1995 each case manager in the two treatment groups recorded time spent on different activities. Overall, consumer‐providers spent at least 18 hours more time face‐to‐face with clients (MD 28.25 hours (95%CI 18.06 to 38.45)) and at least 13 hours less time on the telephone with clients (MD ‐15.90 hours (95% CI ‐18.55 to ‐13.25) compared to professional staff. Consumer‐providers also spent at least 8 hours less time in contact with client family and friends (MD ‐13.16 hours (95% CI ‐18.54 to ‐7.78)) and at least 16 hours less time with provider agencies and staff (MD ‐23.58 hours (95% CI ‐30.84 to ‐16.32)). However the mean difference in number of hours spent by consumer‐providers on all case management services was not significantly different (MD 19.28 hours (95% CI ‐5.09 to 42.63) compared to professional staff.
1.11. Analysis.
Comparison 1 Consumer‐provider versus professional staff, Outcome 11 Service provision: Time allocation.
| Service provision: Time allocation | ||||
|---|---|---|---|---|
| Study | Time spent with | Consumer‐provider | Professional staff | Effect measure |
| Clarke 2000 | Team | 40% | 40% | not estimable |
| Clarke 2000 | Clients | 33% | 33% | not estimable |
| Clarke 2000 | Alone | 25% | 25% | not estimable |
| Clarke 2000 | Family/staff and other agencies/operators |
6% | 6% | not estimable |
| Clarke 2000 | ||||
| Solomon 1995 | Face‐to‐face with client | mean 38.2 (SD 33.63), n=46 | mean 9.95 (SD 10.54), n = 45 | MD 28.25 hours [95% CI 18.06 to 38.45] |
| Solomon 1995 | Telephone with client | mean 5.90 (SD 6.44), n = 46 | mean 21.8 (SD 6.44), n = 45 | MD ‐15.90 hours [95% CI ‐18.55 to ‐13.25] |
| Solomon 1995 | Contact with client family/friends | mean 0.46 (SD 1.22), n = 46 | mean 13.62 (SD 18.38), n = 45 | MD ‐13.16 hours [95% CI ‐18.54 to ‐7.78] |
| Solomon 1995 | Contact with provider agency or staff | mean 1.98 (SD 7.03), n = 46 | mean 25.56 (SD 23.87), n = 45 | MD ‐23.58 hours [95% CI ‐30.84 to ‐16.32] |
| Solomon 1995 | All case management services | mean 83.79 (SD 63.71), n = 46 | mean 64.51 (SD 54.62), n = 45 | MD 19.28 hours [95% CI ‐5.08 to 43.63] |
Location of services
Two studies reported the locations at which case managers provided service to clients (Clarke 2000; Solomon 1995). We were unable to calculate summary estimates for Clarke 2000 which reported similar percentages of time for both groups providing service to clients at the study institution (consumer‐provider 15% versus professional 13%) but a difference in the proportion of time spent with clients outside the office (consumer‐provider 61% versus professional 73%) (Analysis 1.12) without reporting any measures of variance. Solomon 1995 found that consumer‐providers spent more time providing services in the client's home (MD 4.02 hours (95% CI 0.30 to 7.74)), on the street (MD 3.39 hours (95% CI 0.77 to 6.01)), or at the provider agency (MD 26.49 hours (95% CI 15.68 to 37.30)) and less time in the office (MD ‐50.29 hours (95% CI ‐63.51 to ‐37.07)) or hospital (MD ‐3.97 hours (95% CI ‐6.50, ‐1.44)) compared to professional staff.
1.12. Analysis.
Comparison 1 Consumer‐provider versus professional staff, Outcome 12 Service provision: Location of services.
| Service provision: Location of services | ||||
|---|---|---|---|---|
| Study | Location | Consumer‐provider | Professional staff | Effect measure |
| Clarke 2000 | Out of office (eg client home or public place) | 61% | 73% | not estimable |
| Clarke 2000 | Institution | 15% | 13% | not estimable |
| Clarke 2000 | ||||
| Clarke 2000 | ||||
| Clarke 2000 | ||||
| Solomon 1995 | Office | mean 13.01 (SD 13.77), n = 46 | mean 63.30 (SD 43.15), n = 45 | MD ‐50.29 hours [95% CI ‐63.51 to ‐37.07] |
| Solomon 1995 | Client's home | mean 9.23 (SD 9.71), n = 46 | mean 5.21 (SD 8.34), n = 45 | MD 4.02 hours [95% CI 0.30 to 7.74] |
| Solomon 1995 | On the street | mean 4.89 (SD 8.32), n = 46 | mean 1.50 (SD 3.52), n = 45 | MD 3.39 hours [95% CI 0.77 to 6.01] |
| Solomon 1995 | Provider agency | mean 28.44 (SD 37.29), n = 46 | mean 1.95 (SD 3.01), n = 45 | MD 26.49 hours [95% CI 15.68 to 37.30] |
| Solomon 1995 | Hospital (no difference in days hospitalised between groups) | mean 1.08 (SD 2.55), n = 46 | mean 5.05 (SD 8.30), n = 45 | MD ‐3.97 hours [95% CI ‐6.50 to ‐1.44] |
Case manager tasks
Only Clarke 2000 provided a detailed account of the types of tasks undertaken within the case manager role; categorised as either tasks related to service provision or administrative tasks. We were unable to calculate summary estimates to determine whether there were any significant differences in the tasks undertaken by each group (Analysis 1.13).
1.13. Analysis.
Comparison 1 Consumer‐provider versus professional staff, Outcome 13 Service provision: Case manager tasks.
| Service provision: Case manager tasks | |||
|---|---|---|---|
| Study | Category | Consumer‐provider | Professional staff |
| Service categories | |||
| Clarke 2000 | Support/structure | 14% | 15% |
| Clarke 2000 | Treatment Plan | 3% | 6% |
| Clarke 2000 | Service Coordination | 8% | 8% |
| Clarke 2000 | Crisis | 1% | 1% |
| Clarke 2000 | Assess/monitor | 6% | 7% |
| Clarke 2000 | Training (skill/job) | 1% | 3% |
| Clarke 2000 | Transporting | 3% | 5% |
| Clarke 2000 | Counselling | 3% | 3% |
| Clarke 2000 | Other | 3% | 2% |
| Administrative | |||
| Clarke 2000 | Travel | 11% | 11% |
| Clarke 2000 | Paperwork | 13% | 14% |
| Clarke 2000 | Administration/Supervision | 15% | 8% |
| Clarke 2000 | Team meetings | 19% | 17% |
| Clarke 2000 | |||
| Clarke 2000 | |||
| Clarke 2000 | |||
| Clarke 2000 | |||
| Clarke 2000 | |||
Secondary outcomes
7) Professional's attitudes
Solomon 1995 assessed the client‐manager relationship from the provider's perspective using the Working Alliance Inventory. The effect estimate for this outcome at two years is imprecise and the confidence interval incorporates differences in favour of both groups (MD 2.56 (95% CI ‐9.51 to 14.63) (Analysis 1.17)).
1.17. Analysis.
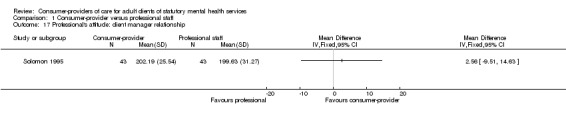
Comparison 1 Consumer‐provider versus professional staff, Outcome 17 Professional's attitude: client manager relationship.
8) Financial costs of service provision
There were no studies reporting information about the costs of service provision.
Comparison 2: Consumer‐provider as adjunct versus usual care
Six studies compared groups receiving usual care with groups receiving services from consumer‐providers in addition to usual care (Craig 2004; Gordon 1979; Kaufmann 1995; O'Donnell 1999; Sledge 2011; Rogers 2007).
Summary
Overall, the six low to moderate quality studies found no difference in psychosocial, client satisfaction or service use outcomes. One study found a small difference favouring the intervention group for both staff and client ratings of clients' needs having been met; however the staff rating may have been affected by detection bias. The six studies did not report mental health measures, adverse outcomes for clients or financial costs.
Primary outcomes for clients receiving services
1) Standardised measures of psychosocial outcomes (quality of life, empowerment, function, social relations)
Quality of life
O'Donnell 1999 (N = 84) assessed the effects of client quality of life, of client‐focused case management services provided for 12 months with or without the addition of a consumer (consumer‐provider) advocate. The study used a modified version of the Quality Of Life Index for Mental Health (QOLIMH) and reported no significant difference between groups, although insufficient data were reported to calculate a summary estimate.
Empowerment
One study assessed empowerment (Rogers 2007) and a second study of 80 participants measured motivation for change, self‐determination and hope (Sledge 2011), however these data are yet to be published. Rogers 2007 is a multi‐site study involving 1827 participants. It investigated the effects of attending a consumer operated service provider (COSP) in addition to traditional mental health services. The study used a Making Decisions Empowerment (MDE) questionnaire and reported no significant difference in clients' subjective feelings of empowerment after 12 months between groups (time x group interaction F(1.4059) = 2.30, P = 0.13). It also found no significant difference between groups on the Personal Empowerment (PE) questionnaire in how much choice clients felt they had in their lives (time x group interaction F(1.4062) = 3.53, P = 0.06). Nor was there a significant difference between groups in how they rated the amount of certainty in their social, residential, and financial lives (time x group interaction F(1.4025) = 0.05, P = 0.82). It is important to consider the moderate attendance at COSPs by the intervention group (57%) and potential confounding by those attending COSPs in the control group (15%) for this study, which largely compromises the reliability of these findings.
Function
One small study (Craig 2004) assessed function and disability using the Life Skills Profile (LSP). Data from a second study that also measured function status are not yet published (Sledge 2011). Craig 2004 investigated the impact of adding consumer‐providers as healthcare assistants to assertive outreach teams. Although the overall results for the LSP at 12 months did not reach statistical significance, the wide confidence interval of the summary estimate incorporates important differences in both directions for participants receiving additional support from consumer‐providers (MD 3.00 (95% CI ‐5.75 to 11.75), Analysis 2.1). It is important to note that some of the control group also attended social functions hosted by the consumer‐providers, which may have confounded the results. Participants were aware of treatment allocation in this study and variation in the results could have been biased based on individual participant beliefs about the capability of consumer‐providers to help with their condition.
2.1. Analysis.
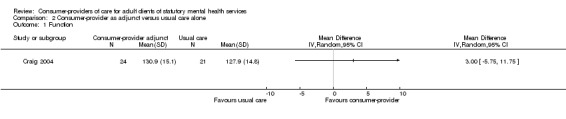
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 1 Function.
Social relations
Craig 2004 and Sledge 2011 assessed participant satisfaction with their own social network. Craig 2004 used the Significant Others Scale (SOS) and found no significant difference after 12 months between groups (MD ‐0.10 (95% CI ‐0.53 to 0.33), Analysis 2.2). Data are not yet available for Sledge 2011.
2.2. Analysis.
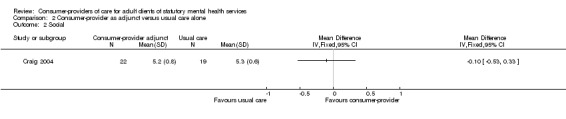
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 2 Social.
2) Standardised measures of mental health (general symptoms, depression)
Kaufmann 1995 planned to assess mental health symptoms. This study planned to involve 90 participants to investigate the effect of self‐help groups run by consumer‐providers in addition to care provided by community health centres. The trialists planned to collect data using the BPRS and Symptom Check List‐90 (SCL‐90) at six‐monthly intervals, however follow‐up data collection was stopped early because there was a low level of attendance at the self‐help groups for the intervention group (9 out of 54, 17%) as well as the control group (6 out of 36, 17%). No usable data were available from this study.
3) Adverse outcomes for clients
There were no adverse outcomes reported for clients in the six studies in Comparison 2.
Primary outcomes for service provision
4) Client satisfaction with service provision
Three studies assessed participant satisfaction with treatment (Craig 2004; O'Donnell 1999; Analysis 2.3), however Sledge 2011 has not yet published these data. Craig 2004 used the Verona Service Satisfaction Scale to assess participant satisfaction with both the service (SMD 0.24 (95% CI ‐0.37 to 0.85)) and staff (SMD 0.18 (95% CI ‐0.43 to 0.79)). O'Donnell 1999 assessed participant satisfaction with the service using a modified version of the Client Service Satisfaction Questionnaire (SMD 1.67 (95% CI 0.08 to 3.25)). The pooled effect estimate for satisfaction with service from Craig 2004 and O'Donnell 1999 (total N = 125) was SMD 0.76 (95% CI ‐0.59 to 2.10), P = 0.27, indicating no significant difference between groups.
2.3. Analysis.
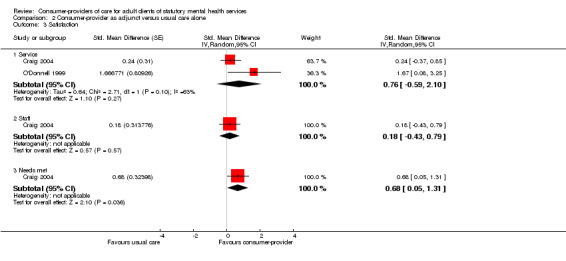
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 3 Satisfaction.
Craig 2004 also used the client version of the Camberwell Assessment of Need to assess participants' satisfaction that their needs had been met, and described the result as demonstrating no important difference between groups even though the difference just reached statistical significance (SMD 0.68 (95% CI 0.05 to 1.31), P = 0.04).
5) Use of services (mental health services, hospital use, client attrition)
Use of mental health services
Craig 2004 (N = 45) compared participant attendance rates for clinic appointments (Analysis 2.4), and found no difference between groups (SMD 0.52 (95% CI ‐0.07 to 1.11), P = 0.09).
2.4. Analysis.
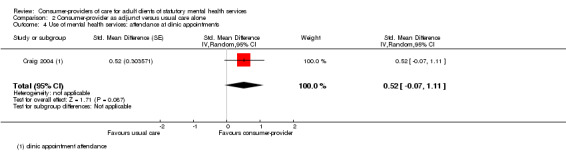
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 4 Use of mental health services: attendance at clinic appointments.
Hospital use
Craig 2004 compared the proportion of people in each group hospitalised during the 12‐month follow up period (Analysis 2.6). The addition of consumer‐providers as assistants in the intervention group did not result in any difference in this outcome (N = 45, RR 1.07 (95% CI 0.55 to 2.07), P = 0.84). Sledge 2011 measured the number of hospitalisations in each group during the 9‐month follow up period. The addition of consumer‐providers did not result in a difference in the number of hospitalisations between the two groups (MD ‐0.64; 95% CI ‐1.3 to 0.02; Analysis 2.7).
2.6. Analysis.
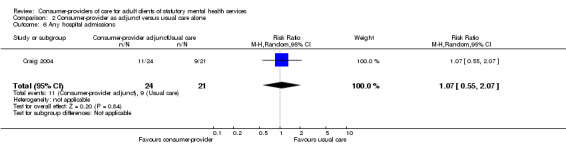
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 6 Any hospital admissions.
2.7. Analysis.
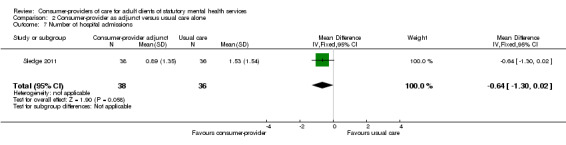
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 7 Number of hospital admissions.
Comparison of the length of hospital stay across the two groups in Craig 2004 and Sledge 2011 was less precise, with wide confidence intervals (MD ‐13.41 (95% CI ‐32.09 to 5.27), P = 0.16). The overall difference between groups did not reach statistical significance (Analysis 2.8). Gordon 1979 also measured rehospitalisation (17.5% in intervention, 35% in control group), length of stay (7 days in intervention; 24.6 days in control group) and use of community mental health services (47.5% in intervention and 74% in control group) at ten months. While there were 80 people in the study, the number randomised to each arm was not provided.
2.8. Analysis.
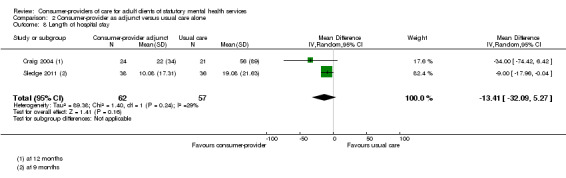
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 8 Length of hospital stay.
Client attrition
Four of the six studies in Comparison 2 reported dropouts or described reasons why participants were unable to be assessed at follow up (Craig 2004; O'Donnell 1999; Rogers 2007; Sledge 2011). Kaufmann 1995 was stopped early due to low rates of participation in the intervention group, and cross‐over between the intervention and control groups (17% of subjects in both groups attended self‐help groups). We were unable to determine whether losses were balanced across treatment groups in Gordon 1979 and Rogers 2007. The remaining studies ranged in overall attrition from 9% (Craig 2004) to 30% (O'Donnell 1999). More participants were lost from the intervention group in O'Donnell 1999 but this difference did not appear to have been related to the intervention itself. Pooling results from Craig 2004, Sledge 2011 and O'Donnell 1999 showed no overall difference in attrition between intervention and usual care groups (RR 1.29 (95% CI 0.72 to 2.31), P = 0.39) (Analysis 2.5).
2.5. Analysis.
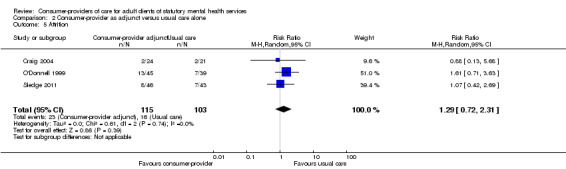
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 5 Attrition.
Secondary outcomes
7) Professionals' attitudes
One study included staff assessment of whether they felt the clients' needs had been met (Analysis 2.9). Craig 2004 reported a small but significant difference in favour of those receiving additional support from consumer‐providers (MD 1.56 (95% 0.50 to 2.62), P = 0.004). The statistical significance of this result is probably a result of detection bias as it is based on interviews with staff who were not blind to the intervention and had a vested interest in seeing it succeed.
2.9. Analysis.
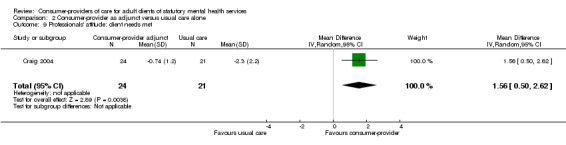
Comparison 2 Consumer‐provider as adjunct versus usual care alone, Outcome 9 Professionals' attitude: client needs met.
8) Financial costs of service provision
No studies reported information about the costs of service provision.
Discussion
Summary of main results
Comparison 1
There is a small amount of low to moderate quality evidence based on three studies (total N = 363) that consumer‐providers have no significant effect on quality of life, function, or social relations after 12 months of case management services, compared to professional staff providing the same service (Rivera 2007; Sells 2006; Solomon 1995). Similarly, three studies of low to moderate quality (total N = 293) showed no significant differences in general mental health symptoms (Bright 1999; Rivera 2007; Solomon 1995). One small study at high risk of bias (N = 67) involving a 10‐week program of either mutual support group therapy or cognitive behavioural therapy showed no difference in depression symptoms between groups led by a consumer‐provider or professional (Bright 1999), consistent with the only other study to measure this outcome (Solomon 1995). The studies did not report any adverse outcomes for clients.
Two studies of low to moderate quality (total N = 213) demonstrated no difference in satisfaction with treatment between groups involving a consumer‐provider or professional staff (Rivera 2007; Solomon 1995). Two studies (N = 160) showed no difference in assessment of the client‐manager relationship between groups using case management services (Sells 2006; Solomon 1995).
Two low to moderate quality studies (Clarke 2000; Rivera 2007; total N = 150) demonstrated a small but significant decrease in crisis and emergency service use favouring consumer‐providers, although a third study without usable data reported no difference in this outcome. There was no difference between groups in terms of hospital admissions (Clarke 2000; Solomon 1995; N = 210) or length of stay (Rivera 2007; Solomon 1995; N = 232).
There did not appear to be a significant difference in uptake of mental health services (Rivera 2007; Solomon 1995; total N = 213) or attrition (3 studies, Bright 1999; Sells 2006; Solomon 1995; total N = 293). There were differences in caseloads, with consumer‐providers tending to have fewer clients (Bright 1999; Clarke 2000; Rivera 2007; Sells 2006; Solomon 1995). Results for time allocation, tasks, and location of service provision, were mixed (Clarke 2000; Solomon 1995).
Comparison 2
There is limited evidence from two low to moderate quality studies (N = 164) that the addition of consumer‐providers to existing mental health services has no significant impact on psychosocial outcomes including quality of life, function and social relations after 12 months (Craig 2004; O'Donnell 1999). The studies did not report any adverse outcomes for clients. Limited evidence (the same 2 studies involving up to 125 participants) suggests the addition of consumer‐providers has no significant impact on client satisfaction with services or staff, although in one study it did improve clients' satisfaction with having their needs met, but this result did not reach clinical importance. Limited evidence from two studies (Craig 2004; Sledge 2011; N = 119), indicates that the addition of consumer‐providers had no effect on clients' use of mental health services (including hospital use). Evidence from one small, moderate quality trial (Craig 2004, N = 45) suggests care providers may perceive the addition of consumer‐providers as leading to improvements in meeting clients' needs, although this is likely to have been affected by detection bias.
Overall completeness and applicability of evidence
Comparison 1
The main comparison for this review involved studies with a consumer‐provider in a role that was occupied by professional staff in the comparison group. Five studies were identified involving a total of 581 trial participants, however we were only able to collect outcome data for up to three studies (up to 331 participants) for each of the outcomes assessed in this review. Although we attempted to obtain missing data from trialists, we were unable to determine effect estimates for a number of outcomes in individual studies (particularly in Solomon 1995 and Sells 2006). In most cases, it is likely that outcomes were selectively reported based on the lack of statistically significant findings, as outcomes with missing data were often described as having no significant difference between groups. Table 2 provides a summary of missing data and reporting bias for the outcomes addressed in this review. As there was no strong evidence of effect across any of the outcomes we assessed, and outcomes with missing data were reported as 'non significant', the potential inclusion of missing data in meta‐analyses is unlikely to change the results of this review.
Current evidence indicates there is no clinically important benefit or harm when consumer‐providers are involved in the delivery of statutory mental health services. This evidence largely applies to consumer‐providers as case managers within community‐based mental health teams in the USA (Clarke 2000; Rivera 2007; Sells 2006; Solomon 1995). Interestingly, consumer‐providers and professionals in some studies interacted on the same treatment teams, attended the same meetings and were able to share practice activities, which may explain the lack of differences between groups if the consumer‐providers and professionals consequently adopted similar behaviours to each other.
Comparison 2
For the second comparison group (six studies, up to 2215 participants), the three USA studies involved consumer‐operated service providers as an adjunct to mental health services (Gordon 1979; Kaufmann 1995; Rogers 2007), and studies in the USA, UK and Australia involved consumer‐providers in advocacy roles (Craig 2004; O'Donnell 1999; Sledge 2011). Selective outcome reporting and missing data were also limitations for this comparison group. Summary estimates for most outcomes rely on data from one small study (N = 45) conducted by Craig 2004. Several outcomes from O'Donnell 1999 (N = 84) had insufficient data for inclusion in a pooled analysis with Craig 2004 but results are unlikely to show any significant difference in outcomes between groups (O'Donnell 1999 reported no significant difference for outcomes where data were missing).
Both Kaufmann 1995 and Rogers 2007 involved referral to consumer‐operated services in addition to usual care, and both studies indicated uptake of these services across comparison groups as a confounder of the outcomes evaluated. These studies suggest spontaneous uptake of consumer‐operated services may be between 15% to 17% when clients are not actively encouraged to attend (ie in usual care), with a potential participation rate of 57% when clients are encouraged to attend the services. These findings have implications for future studies (ie designing an intervention that takes into account potential non‐adherence) and indicates there may be limited uptake of these interventions outside a research context, where uptake of services would be expected to be less.
Interestingly, Rogers 2007 was the largest study (N = 1827) included in this review (Comparison 2) and the outcomes reported in this study (empowerment) were not assessed in any other studies. The applicability of these findings and the contribution of this large study to the overall body of evidence is therefore very limited.
Consideration of resources and costs
Given there is no strong evidence of significant clinical benefits or harms when employing consumer providers, there may be other factors such as resources and cost that should be considered for this type of intervention. Consumer‐providers may be considered a lower cost alternative to degree‐qualified health professionals (Salzer 2010), but others may argue the cost implications are the same if life experience is considered acceptable preparation for case management (Solomon 1995).
Importantly, our review identifies potential differences in working capacity (Sells 2006) and professional expertise, and potential increases in staff turnover (Craig 2004; O'Donnell 1999) for consumer‐providers that must be taken into account in any cost‐benefit analysis. Some studies noted absenteeism, and challenges in retaining consumer‐providers. Several consumer‐providers resigned due to the work being too stressful, training too lengthy, travel distance, and the negative effect of employment on welfare benefits (Clarke 2000; Craig 2004; O'Donnell 1999; Sells 2006). Almost all of the studies showed that consumer‐providers had reduced caseloads or working hours compared to professional staff in the same role (Analysis 1.10; Bright 1999; Clarke 2000; Rivera 2007; Sells 2006). There may also be differences in expected deliverables between consumer‐providers and professional staff, as indicated in qualitative data collected by Sells 2006: "Peers were not required to fulfil traditional case manager responsibilities, giving them time and attention to devote to their clients". It is unclear what the potential impact would be for clients if traditional case manager responsibilities were reduced for professional staff as well and they too had added time to devote attention to their clients.
Qualitative data reported in trials
Six included studies (Clarke 2000; Craig 2004; Gordon 1979; O'Donnell 1999; Sells 2006; Solomon 1995) also examined qualitative experiences of consumer‐providers as providers of statutory mental health services and the impacts on both the consumer‐providers themselves as well as the health professional providers, participants and/or carers.
The main recurring themes were:
Consumer‐providers were expected to develop their role over time. They tended to feel this severely hampered their service delivery and created a perception that employing a consumer‐provider was a token gesture.
Consumer‐provider absenteeism due to illness or relapse of their mental health condition increased caseload for remaining staff.
Some consumer‐providers experienced the role as highly rewarding and important to their lives (Gordon 1979).
Traditional staff felt there were added expectations to support, train and supervise consumer‐providers within mental health teams, increasing their workload or adding burden.
Some professional staff found it challenging to manage having different ‘providers' in the team.
Clients felt there were limited outcome measures relevant to assessing the impact of consumer‐providers in mental health services.
Clients' beliefs about the capability of past or current service users to improve the client's condition may impact on these interventions' effects. Awareness of the care‐provider's history may be an important factor for clients' behaviour modification, and subsequent receptiveness and adherence to treatment. This is reflected in qualitative data exploring how the involvement of consumer‐providers is perceived by professional staff and consumer‐providers themselves, and their clients and carers. These data suggest that:
a clearer description of the consumer‐provider tasks, responsibilities and expected deliverables is required;
employing more consumer‐providers and providing a support network for them may address relapse and absenteeism;
addressing preconceptions and impacts on traditional staff by better outlining consumer‐provider roles, and the required training and support would be beneficial; and
the effects on consumer‐providers themselves, including impact on skill levels, employment outcomes, social functioning, quality of life and the need to return to treatment, require further consideration.
The consumer‐provider role
It is important to consider the role given to consumer‐providers within statutory mental health services in the included studies, and the degree of training and support required. At least two of the studies indicated the role of consumer‐providers was unclear, and developed throughout the duration of the trial (O'Donnell 1999; Sells 2006). Training and ongoing supervision of consumer‐providers were described in most studies and, whilst lengthy training was considered one of the barriers to retaining staff, some consumer‐providers felt they had received insufficient training for their role (Craig 2004). Future studies would benefit from having a clear description of the consumer‐provider role (eg specific tasks, responsibilities and expected deliverables of the role) and relevant training for the role so that it can be readily implemented. The ongoing supervision provided by professional staff should also be considered as an additional resource that is needed to support consumer‐providers in their role.
Outcomes
During the lengthy gestation of this review, the research and practice context relating to user involvement in mental health service provision has changed. A new focus on individual recovery pathways (rather than cure, per se) should be reflected in the explicit consideration of different client outcomes, as well as community outcomes, in future updates of the review. These may include hope and optimism, life satisfaction, wellness, confidence, connectedness, community empowerment and social support (Greenfield 2008; Simon 2011; Sledge 2011; van Gestel 2012).
Quality of the evidence
The overall evidence of the effects of employing past or current users of mental health services is of moderate to low quality (Figure 3), and is largely based on findings from three relatively small studies (total N = 363). It is unclear whether studies took appropriate measures to allocate clients of mental health services to groups with either a consumer‐provider or professional staff member independent of any potential bias the trialists, care providers, or clients had about their expected outcomes for each group. A lack of standard outcome measures across trials means it is difficult to pool outcomes across separate studies. Selective or incomplete reporting of study outcomes is a key limitation of the included studies with some studies failing to report on all of the outcomes that were assessed, others not providing comparison data across treatment groups, and one study using outcome measures specifically designed for their own study that are not assessed in any other studies. While most studies declared their funding sources, none discussed the role or level of input the funder had.
Potential biases in the review process
This review was conducted according to methods specified in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This advice is based on empirical evidence and current international consensus for methods that minimise bias in the conduct of systematic reviews. We attempted to contact all authors of included studies for missing data and, whilst receiving some responses, were unable to obtain any further unpublished data for inclusion in the review. Nevertheless we have considered the potential impact of including missing data for outcomes presented in the review.
A variety of terms is used to describe consumer‐providers (eg users, survivors, peers) in the literature and it is possible that potentially relevant studies using alternative terms to those listed in the search strategy may not have been identified in our searches. Moreover, whilst no language restrictions were applied in our searches, we did not search non‐English language databases, which may have resulted in a bias towards English‐language papers in this review. We welcome suggestions of any potentially eligible trials that were not assessed for inclusion in this review.
Agreements and disagreements with other studies or reviews
A previous review (Simpson 2002) identified eight studies involving users as employees of mental health services. Five of these studies were non‐randomised trials or observational studies and were ineligible for inclusion in this review. The remaining three studies (Solomon 1995; Clarke 2000; O'Donnell 1999) are included in both reviews. Simpson and colleagues identified key differences in service delivery between consumer‐providers and non consumer‐providers that are consistent with the findings of this review. Overall, consumer‐providers spent longer in supervision, in face‐to‐face contact with clients, or doing outreach work, and they spent less time on the telephone or in the office. Simpson 2002 also reported the higher turnover rate of consumer‐providers and the observation that consumer‐providers had less distinct professional boundaries. They concluded that consumer‐providers did not have any detrimental effect on clients in terms of symptoms, functioning, or quality of life which is also reflected in our review's findings. However, our review also found no significant difference in client satisfaction with their personal circumstances or hospitalisation, whilst Simpson 2002 reported improvement in these outcomes for clients of consumer‐providers.
Wright‐Berryman 2011 reviewed the literature on consumer‐provided services on assertive community treatment and intensive case management teams, and concluded that there was some evidence to support consumer‐provided services for improving engagement and reducing hospitalisation. Evidence of the intervention's impact on reducing symptoms and improving quality of life was, however, lacking. The authors' findings of limited evidence on the impact of consumer‐provided services accords with our review. Likewise, Cook 2011 briefly reviewed the evidence for peer‐provided, recovery‐oriented mental health services and found results similar to those of our review, namely that randomised trials show comparable outcomes for peer and non‐peer provided services.
We look forward to the completion of the Van Ginneken 2011 review of non‐specialist health workers providing mental health care in low and middle income countries, to assess the extent to which our review's findings are consistent with it. The review of lay health workers for improving maternal and child health and the management of infectious diseases (Lewin 2010) identified improvements in maternal and child health (specifically breastfeeding, immunisation, and childhood morbidity and mortality), and limited improvements in tuberculosis management, through the use of lay health workers. Lewin's review included substantially more studies (N = 82), in a wider range of settings than this review. Its promising findings are not inconsistent with those of our review, indicating that non‐professional staff can effect positive health outcomes for clients.
Authors' conclusions
Implications for practice.
There is low to moderate quality evidence from 11 randomised controlled trials indicating that involving consumer‐providers in mental health teams results in psychosocial, mental health symptom and service use outcomes for clients that are no better or worse than those achieved by professionals employed in similar roles, particularly for case management services. There is no difference in client satisfaction with services. There is no evidence of harm associated with involving consumer‐providers in mental health teams.
Future decisions regarding consumer‐provider involvement should consider how their involvement differs compared to trained professionals and the potential impact this will have. Job descriptions, wages and benefits, training and supervision, and strategies to successfully integrate consumer‐providers into multi‐disciplinary teams are important issues to consider when implementing this type of intervention.
Implications for research.
Future randomised controlled trials of consumer‐providers in mental health service provision should minimise bias through the use of adequate randomisation and concealment of allocation, blinding of outcomes where possible, the comprehensive reporting of outcome data, and the avoidance of contamination between treatment groups. Researchers should adhere to the SPIRIT (SPIRIT 2013) and CONSORT (CONSORT 2010) reporting standards for clinical trials, and use consistent, validated measurement tools.
Current evidence from controlled trials indicates there is no harm to clients associated with involving consumer‐providers in mental health teams. Future studies should ensure that standardised mental health measures and adverse client outcomes are assessed. Potential benefits and harms to consumer‐providers themselves have been less rigorously evaluated. Outcomes such as increased skills and improvements in employment outcomes, social functioning and quality of life for consumer‐providers have been described in qualitative studies, but rigorous evaluation using appropriate measures for consumer‐providers (eg income, living situation, need to return to treatment) in controlled studies is lacking. Economic analyses will help to inform whether potential benefits and harms for consumer‐providers, and the resources required to support their role, is a cost effective investment for mental health services and clients.
Future studies should include a clear description of the consumer‐provider role (eg specific tasks, responsibilities and expected deliverables of the role) and relevant training for the role so that it can be readily implemented.
The weight of evidence being strongly based in the United States, future research should be located in diverse settings including in low‐ and middle‐income countries.
Acknowledgements
We thank the staff and editors of the Cochrane Consumers and Communication Review Group, particularly contact editor Dr. Sandy Oliver and Trials Search Co‐ordinator Mr. John Kis‐Rigo. We also thank the referees (including mental health consumers) who provided feedback on the draft protocol and review.
We also acknowledge the contribution of the authors of the protocol for this review (Simpson 2003c): Emma Simpson, Michael Barkham, Simon Gilbody and Allan House.
Appendices
Appendix 1. Glossary of key terms
The term 'consumer' describes any adult who is currently using mental health services. Some publications have employed the terms '(service) user', 'customer', 'client', or 'patient' to describe consumers. The term 'consumer' is intended to be seen as a neutral definition. The term 'user' is sometimes avoided because of connotations of substance abuse (Chamberlain 1993). In this review, 'user' does not imply drug use. For this review, the term 'consumer' excludes carers, potential service users and user representatives.
'Ex‐user' denotes any former user of mental health services. Some ex‐users prefer the term 'survivor' (Graley 1994), however this can have connotations of abuse survival, and some professionals have found this inappropriate (Everett 1998).
In this review, we use the term 'consumer‐provider' (Cook 1995) to describe consumers acting as mental health service employees, for example consumers working as case managers (Solomon 1995), or as staff in a crisis assessment programme (Lyons 1996). This may be either paid or unpaid employment with the service. We use the term 'consumer‐provider' to indicate the role played in the service, as a service provider with declared consumer (user or ex‐user) status. It does not imply any differences in demographics or mental health status between consumer‐providers and other consumers (users or ex‐users). Alternatively, consumer‐providers have been referred to as consumer‐survivors, peer educators, peer specialists (Repper 2011), consumer‐employees (Mowbray 1996), user‐employees, or prosumers (Solomon 1998).
Consumer‐provided services are different from consumer‐operated service providers (COSPs). COSPs are independent, rather than statutory, organisations (ViaHope 2013), providing peer run and delivered services in the 'self‐help' model, not in partnership with professionals (Segal 2011). They are "administratively and financially controlled by mental health consumers who plan, deliver, and evaluate their services" (Campbell 2008b). COSPs are outside the scope of this review.
The term 'mental health professionals' refers to staff of statutory mental health services. Although some professionals will have experience of using mental health services, they are not included as consumer‐providers, as the latter are in roles designated only for declared service users.
The term 'client' refers to recipients of the mental health services in the studies. They may be receiving services from consumer‐providers. We use the term 'client' to avoid confusion between those consumers receiving the service (clients) and those providing the service (consumer‐providers). Distinguishing between roles that consumers take in a service (eg provider or recipient) by referring to them in different terms is common practice in the literature of involving consumers as service providers (Solomon 1998).
For this review, the terms 'user involvement' or 'consumer involvement' refer to involvement in services (not in own care), and are understood to mean active involvement in the provision of mental health services.
Appendix 2. CENTRAL search strategy
| #1 | MeSH descriptor Mental Health Services explode all trees |
| #2 | MeSH descriptor Psychotherapy explode all trees |
| #3 | MeSH descriptor Psychiatry explode all trees |
| #4 | MeSH descriptor Substance Abuse Treatment Centers, this term only |
| #5 | MeSH descriptor Mental Disorders explode all trees |
| #6 | MeSH descriptor Behavioral Symptoms explode all trees |
| #7 | (mental* next (ill* or disorder or disease or health* or patient or treatment or hospital)) or ((chronic* or serious* or severe* or persistent) next mental*) |
| #8 | (personality or mood or dysthymic or cognit* or anxiety or stress or eating or adjustment or reactive or somatoform or conversion or substance‐related or alcohol‐related or behavior or perception or psycho* or impulse‐control) next disorder* |
| #9 | schizo* or psychos*s or psychotic* or paranoi* or neuros*s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or addiction or substance‐abuse or drug‐abuse or drug‐dependen* or suicid* or self‐injur* or self‐harm |
| #10 | *psychiatr* or psychotherap* or "psychosocial care" or ((cognitive or behavio*) next therap*) |
| #11 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10) |
| #12 | consumer:kw |
| #13 | "patient advocacy":kw |
| #14 | "peer group":kw |
| #15 | "assertive community treatment" |
| #16 | (involv* or inclusion or participati* or collaborati*) near/2 (patient or client or user or (service next user) or consumer or (mental next health next consumer) or survivor or people*) |
| #17 | (#12 OR #13 OR #14 OR #15 OR #16) |
| #18 | provide* or staff* or employ* or (case next manag*) or (service* near/4 deliver*) or collaborator* or aide or specialist* or consultant* or personnel |
| #19 | (#17 AND #18) |
| #20 | ((patient* or client* or user* or (service next user*) or consumer* or (mental next health next consumer*) or survivor* or people*) near/2 (provide* or (service next provider*) or staff* or team* or personnel or employ* or (case next manag*) or "service delivery" or collaborat* or aide or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run)):ti,ab |
| #21 | peer next (provider or (service next provider*) or staff or specialist or support or companion or organized or based or run or delivered or led or managed or conducted or directed) |
| #22 | ((involv* or inclusion or includ* or participati* or collaborati* or advoca*) and (patient or client or user or (service next user) or consumer or (mental next health next consumer) or survivor or people*)):ti |
| #23 | (#19 OR #20 OR #21 OR #22) |
| #24 | (#11 AND #23) |
Appendix 3. MEDLINE search strategy
| 1 | mental health/ |
| 2 | exp mental health services/ |
| 3 | exp psychotherapy/ |
| 4 | exp psychiatry/ |
| 5 | psychiatric nursing/ |
| 6 | community mental health centers/ |
| 7 | hospitals psychiatric/ |
| 8 | substance abuse treatment centers/ |
| 9 | exp mental disorders/ |
| 10 | exp behavioral symptoms/ |
| 11 | mentally ill persons/ |
| 12 | ((mental* or psychiatric) adj (ill* or disorder* or disease* or health* or patient* or treatment or hospital*)).tw. |
| 13 | ((chronic* or severe*) adj (mental* or psychiatric)).tw. |
| 14 | or/1‐13 |
| 15 | exp consumer organizations/ |
| 16 | consumer advocacy/ |
| 17 | patient advocacy/ |
| 18 | peer group/ |
| 19 | ((involv* or inclusion or participati* or collaborati*) adj2 (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness)).tw. |
| 20 | assertive community treatment.tw. |
| 21 | or/15‐20 |
| 22 | (provide* or staff* or employ* or case manag* or (service* adj4 deliver*) or collaborator* or aide or aides or specialist* or consultant* or personnel).tw. |
| 23 | employment/ |
| 24 | health personnel/ or "personnel staffing and scheduling"/ |
| 25 | or/22‐24 |
| 26 | 21 and 25 |
| 27 | ((patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness) adj2 (provide* or service provider* or staff* or team* or personnel or employ* or case manag* or service delivery or collaborat* or aide or aides or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run)).tw. |
| 28 | (peer adj (provider* or service* or staff or specialist* or support or companion* or organi#ed or based or run or delivered or led or managed or conducted or directed)).tw. |
| 29 | or/26‐28 |
| 30 | 14 and 29 |
| 31 | randomized controlled trial.pt. |
| 32 | controlled clinical trial.pt. |
| 33 | randomized.ab. |
| 34 | placebo.ab. |
| 35 | drug therapy.fs. |
| 36 | randomly.ab. |
| 37 | trial.ab. |
| 38 | groups.ab. |
| 39 | or/31‐38 |
| 40 | (animals not (humans and animals)).sh. |
| 41 | 39 not 40 |
| 42 | 30 and 41 |
Appendix 4. EMBASE search strategy
| 1 | exp mental health/ |
| 2 | exp mental health care/ |
| 3 | exp psychiatry/ |
| 4 | exp psychiatric treatment/ |
| 5 | exp drug dependence treatment/ |
| 6 | mental health center/ or community mental health center/ |
| 7 | exp mental disease/ |
| 8 | mental patient/ |
| 9 | ((mental* or psychiatric) adj (ill* or disorder* or disease* or health* or patient* or treatment or hospital*)).tw. |
| 10 | ((chronic* or severe*) adj (mental* or psychiatric)).tw. |
| 11 | or/1‐10 |
| 12 | consumer/ |
| 13 | consumer advocacy/ |
| 14 | patient advocacy/ |
| 15 | peer group/ |
| 16 | ((involv* or inclusion or participati* or collaborati*) adj2 (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness)).tw. |
| 17 | assertive community treatment.tw. |
| 18 | or/12‐17 |
| 19 | (provide* or staff* or employ* or personnel or case manag* or (service* adj4 deliver*) or collaborator* or aide or aides or specialist* or consultant*).tw. |
| 20 | exp employment/ |
| 21 | health care personnel/ or mental health care personnel/ |
| 22 | or/19‐21 |
| 23 | 18 and 22 |
| 24 | ((patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness) adj2 (provide* or service provider* or staff* or employ* or personnel or team* or case manag* or service delivery or collaborat* or aide or aides or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run)).tw. |
| 25 | (peer adj (provider* or service* or staff or specialist* or support or companion* or organi#ed or based or run or delivered or led or managed or conducted or directed)).tw. |
| 26 | or/23‐25 |
| 27 | 11 and 26 |
| 28 | randomized controlled trial/ |
| 29 | random*.tw. |
| 30 | placebo*.tw. |
| 31 | ((singl* or doubl* or tripl* or trebl*) and (blind* or mask*)).tw. |
| 32 | single blind procedure/ or double blind procedure/ |
| 33 | (crossover* or cross over*).tw. |
| 34 | crossover procedure/ |
| 35 | factorial*.tw. |
| 36 | (assign* or allocat* or volunteer*).tw. |
| 37 | or/28‐36 |
| 38 | nonhuman/ |
| 39 | 37 not 38 |
| 40 | 27 and 39 |
Appendix 5. PsycINFO search strategy (to 2009)
| # | Search: 1806 to March Week 3 2009 (19/03/2009) |
| 1 | exp mental health/ |
| 2 | exp mental health services/ |
| 3 | exp mental health programs/ |
| 4 | exp psychotherapy/ |
| 5 | exp psychiatry/ |
| 6 | psychiatric clinics/ or psychiatric units/ |
| 7 | community mental health centers/ |
| 8 | psychiatric hospitals/ |
| 9 | psychiatric hospital programs/ |
| 10 | exp mental disorders/ or exp behavior disorders/ |
| 11 | exp psychopathology/ |
| 12 | psychiatric symptoms/ |
| 13 | psychiatric patients/ |
| 14 | ((mental* or psychiatric) adj (ill* or disorder* or disease* or health* or patient* or treatment or hospital*)).ti,ab,hw,id. |
| 15 | ((chronic* or severe*) adj (mental* or psychiatric)).ti,ab,hw,id. |
| 16 | or/1‐15 |
| 17 | participation/ or client participation/ or involvement/ |
| 18 | advocacy/ |
| 19 | empowerment/ |
| 20 | cooperation/ or collaboration/ |
| 21 | peers/ or peer counseling/ or peer relations/ |
| 22 | ((involv* or inclusion or participati* or collaborati*) adj2 (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness)).ti,ab,hw,id. |
| 23 | assertive community treatment.ti,ab,hw,id. |
| 24 | or/17‐23 |
| 25 | (provide* or staff* or employ* or personnel or case manag* or (service* adj4 deliver*) or collaborator* or aide or aides or specialist* or consultant*).ti,ab,hw,id. |
| 26 | 24 and 25 |
| 27 | ((patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness) adj2 (provide* or service provider* or staff* or employ* or personnel or team* or case manag* or service delivery or collaborat* or aide or aides or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run)).ti,ab,hw,id. |
| 28 | (peer adj (provider* or service* or staff or specialist* or support or companion* or organi#ed or based or run or delivered or led or managed or conducted or directed)).ti,ab,hw,id. |
| 29 | or/26‐28 |
| 30 | 16 and 29 |
| 31 | random*.ti,ab,id. |
| 32 | trial?.ti,ab,hw,id. |
| 33 | placebo*.ti,ab,hw,id. |
| 34 | ((singl* or doubl* or triple* or trebl*) and (blind* or mask*)).ti,ab,id. |
| 35 | (crossover or cross over).ti,ab,id. |
| 36 | factorial*.ti,ab,id. |
| 37 | latin square.ti,ab,id. |
| 38 | (assign* or allocat* or volunteer*).ti,ab,id. |
| 39 | mental health program evaluation/ |
| 40 | treatment effectiveness evaluation/ |
| 41 | exp experimental design/ |
| 42 | "2000".md. |
| 43 | or/31‐42 |
| 44 | limit 43 to human |
| 45 | 30 and 44 |
Appendix 6. CINAHL search strategy
| S1 | MH mental health services+ |
| S2 | MH psychotherapy+ |
| S3 | MH psychiatry+ |
| S4 | MH psychiatric service+ |
| S5 | MH psychiatric units |
| S6 | MH psychiatric nursing+ |
| S7 | MH hospitals, psychiatric |
| S8 | MH substance use rehabilitation programs+ |
| S9 | MH mental disorders+ |
| S10 | MH psychiatric patients+ |
| S11 | mental* ill* or mental disorder* or mental disease* or mental health* or mental patient* or mental hospital* |
| S12 | psychiatric ill* or psychiatric disorder* or psychiatric disease* or psychiatric health* or psychiatric patient* or psychiatric hospital* or psychiatric treatment |
| S13 | chronic* mental* or chronic* psychiatric* or severe* mental* or severe* psychiatric* or serious* mental* or serious* psychiatric* |
| S14 | s1 or s2 or s3 or s4 or s5 or s6 or s7 or s8 or s9 or s10 or s11 or s12 or s13 |
| S15 | consumer advoca* or patient advoca* |
| S16 | MH consumer organizations+ |
| S17 | MH mental health organizations+ |
| S18 | (involv* or inclusion or participati* or collaborati*) and (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people*) |
| S19 | MH peer group |
| S20 | assertive community treatment |
| S21 | s15 or s16 or s17 or s18 or s19 or s20 |
| S22 | provide* or staff* or employ* or case manag* or (service* N4 deliver*) or collaborator* or aide or aides or specialist* or consultant* or personnel |
| S23 | s21 and s22 |
| S24 | TI (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness) and TI (provide* or service provider* or staff* or team* or personnel or employ* or case manag* or service delivery or collaborat* or aide or aides or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run) |
| S25 | AB (user* N2 provide*) or AB (user* N2 service provide*) or AB (user* N2 staff*) or AB (user* N2 team*) or AB (user* N2 personnel) or AB (user* N2 employ*) or AB (user* N2 case manag*) or AB (user* N2 sevice delivery) or AB (user* N2 collaborat*) or AB (user* N2 aide) or AB (user* N2 aides) or AB (user* N2 specialist*) or AB (user* N2 consultant*) or AB (user* N2 delivered) or AB (user* N2 operated) or AB (user* N2 assisted) or AB (user* N2 led) or AB (user* N2 managed) or AB (user* N2 conducted) or AB (user* N2 directed) or AB (user* N2 run) |
| S26 | AB (consumer* N2 provide*) or AB (consumer* N2 service provide*) or AB (consumer* N2 staff*) or AB (consumer* N2 team*) or AB (consumer* N2 personnel) or AB (consumer* N2 employ*) or AB (consumer* N2 case manag*) or AB (consumer* N2 sevice delivery) or AB (consumer* N2 collaborat*) or AB (consumer* N2 aide) or AB (consumer* N2 aides) or AB (consumer* N2 specialist*) or AB (consumer* N2 consultant*) or AB (consumer* N2 delivered) or AB (consumer* N2 operated) or AB (consumer* N2 assisted) or AB (consumer* N2 led) or AB (consumer* N2 managed) or AB (consumer* N2 conducted) or AB (consumer* N2 directed) or AB (consumer* N2 run) |
| S27 | s23 or s24 or s25 or s26 |
| S28 | s14 and s27 |
| S29 | randomi?ed controlled trial* |
| S30 | PT Clinical Trial |
| S31 | MH Clinical Trials+ |
| S32 | MH Random Assignment |
| S33 | MH Placebos |
| S34 | MH Quantitative Studies |
| S35 | AB (random* or trial or groups or placebo*) or TI (random* or trial or groups or placebo*) |
| S36 | AB (singl* or doubl* or tripl* or trebl*) and AB (blind* or mask*) |
| S37 | TI (singl* or doubl* or tripl* or trebl*) and TI (blind* or mask*) |
| S38 | S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 |
| S39 | s28 and s38 |
| S40 | s39 |
Appendix 7. Current Contents search strategy
| 1 | (mental* adj (ill* or disorder* or disease* or health* or patient* or treatment or hospital*)).mp. |
| 2 | ((chronic* or severe* or serious* or persistent) adj mental*).mp. |
| 3 | (psychiatr* or psychotherap* or ((cognitive or behavio*) adj therap*)).mp. |
| 4 | ((personality or mood or dysthymic or cognit* or anxiety or stress or eating or adjustment or reactive or somatoform or conversion or substance related or alcohol related or behavior or perception or psycho* or impulse control) adj disorder*).mp. |
| 5 | (schizo* or psychos#s or psychotic* or paranoi* or neuros#s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or addiction or substance abuse or drug abuse or drug dependen* or suicid* or self injur* or self harm).mp. |
| 6 | or/1‐5 |
| 7 | ((involv* or inclusion or participati* or collaborati*) adj2 (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness)).mp. |
| 8 | assertive community treatment.mp. |
| 9 | peer group.mp. |
| 10 | or/7‐9 |
| 11 | (provide* or staff* or employ* or case manag* or (service* adj4 deliver*) or collaborator* or aide or aides or specialist* or consultant* or personnel).mp. |
| 12 | 10 and 11 |
| 13 | ((patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness) adj2 (provide* or service provider* or staff* or team* or personnel or employ* or case manag* or service delivery or collaborat* or aide or aides or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run)).tw. |
| 14 | (peer adj (provider* or service* or staff or specialist* or support or companion* or organi#ed or based or run or delivered or led or managed or conducted or directed)).mp. |
| 15 | or/12‐14 |
| 16 | 6 and 15 |
| 17 | (random* or trial* or placebo* or assign* or allocat* or volunteer* or ((singl* or doubl* or tripl* or trebl*) and (blind* or mask*)) or crossover or cross over or factorial* or latin square).mp. |
| 18 | 16 and 17 |
| 19 | (beha or clin).sb. |
| 20 | 18 and 19 |
Appendix 8. Updated PsycINFO (OvidSP) search strategy, March 2012
1. exp mental health/
2. exp mental health services/
3. exp mental health programs/
4. exp psychotherapy/
5. exp psychiatry/
6. psychiatric clinics/ or psychiatric units/
7. community mental health centers/
8. psychiatric hospitals/
9. psychiatric hospital programs/
10. exp mental disorders/ or exp behavior disorders/
11. exp psychopathology/
12. psychiatric symptoms/
13. psychiatric patients/
14. ((mental* or psychiatric) adj (ill* or disorder* or disease* or health* or patient* or treatment or hospital*)).ti,ab,hw,id.
15. ((chronic* or severe*) adj (mental* or psychiatric)).ti,ab,hw,id.
16. or/1‐15
17. participation/ or client participation/ or involvement/
18. advocacy/
19. empowerment/
20. cooperation/ or collaboration/
21. peers/ or peer counseling/ or peer relations/
22. ((involv* or inclusion or participati* or collaborati*) adj2 (patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness)).ti,ab,hw,id.
23. assertive community treatment.ti,ab,hw,id.
24. or/17‐23
25. (provide* or staff* or employ* or personnel or case manag* or (service* adj4 deliver*) or collaborator* or aide or aides or specialist* or consultant*).ti,ab,hw,id.
26. 24 and 25
27. ((patient* or inpatient* or outpatient* or client* or user* or service user* or consumer* or mental health consumer* or survivor* or people* or people with mental illness) adj2 (provide* or service provider* or staff* or employ* or personnel or team* or case manag* or service delivery or collaborat* or aide or aides or specialist* or consultant* or delivered or operated or assisted or led or managed or conducted or directed or run)).ti,ab,hw,id.
28. (peer adj (provider* or service* or staff or specialist* or support or companion* or organi#ed or based or run or delivered or led or managed or conducted or directed)).ti,ab,hw,id.
29. or/26‐28
30. 16 and 29
31. random*.ti,ab,id.
32. trial?.ti,ab,hw,id.
33. placebo*.ti,ab,hw,id.
34. ((singl* or doubl* or triple* or trebl*) and (blind* or mask*)).ti,ab,id.
35. (crossover or cross over).ti,ab,id.
36. factorial*.ti,ab,id.
37. latin square.ti,ab,id.
38. (assign* or allocat* or volunteer*).ti,ab,id.
39. mental health program evaluation/
40. treatment effectiveness evaluation/
41. exp experimental design/
42. "2000".md.
43. or/31‐42
44. 30 and 43
Data and analyses
Comparison 1. Consumer‐provider versus professional staff.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quality of life: Life satisfaction subscale (subjective) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Function: Daily activities subscale (subjective) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Social: Social relations subscale (subjective) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Symptoms | 2 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.52, 0.05] |
| 5 Depression | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Self‐report (BDI) at 10 weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Observer‐rated (HRSD) at 10 weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Satisfaction | 2 | 213 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.69, 0.25] |
| 7 Client manager relationship | 2 | 160 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.10, 0.53] |
| 8 Use of mental health services in 12 months | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Rehabilitation services | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Outpatient contacts | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Attrition | 3 | 331 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.58, 1.09] |
| 10 Service provision: Caseload/personnel | Other data | No numeric data | ||
| 11 Service provision: Time allocation | Other data | No numeric data | ||
| 12 Service provision: Location of services | Other data | No numeric data | ||
| 13 Service provision: Case manager tasks | Other data | No numeric data | ||
| 13.1 Service categories | Other data | No numeric data | ||
| 13.2 Administrative | Other data | No numeric data | ||
| 14 Crisis/emergency service | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.34 [‐0.60, ‐0.07] | |
| 15 Hospital admissions | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 16 Length of stay | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 17 Professional's attitude: client manager relationship | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 2. Consumer‐provider as adjunct versus usual care alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Function | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Social | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Satisfaction | 2 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 3.1 Service | 2 | Std. Mean Difference (Random, 95% CI) | 0.76 [‐0.59, 2.10] | |
| 3.2 Staff | 1 | Std. Mean Difference (Random, 95% CI) | 0.18 [‐0.43, 0.79] | |
| 3.3 Needs met | 1 | Std. Mean Difference (Random, 95% CI) | 0.68 [0.05, 1.31] | |
| 4 Use of mental health services: attendance at clinic appointments | 1 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.07, 1.11] | |
| 5 Attrition | 3 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.72, 2.31] |
| 6 Any hospital admissions | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.55, 2.07] |
| 7 Number of hospital admissions | 1 | 74 | Mean Difference (IV, Fixed, 95% CI) | ‐0.64 [‐1.30, 0.02] |
| 8 Length of hospital stay | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐13.41 [‐32.09, 5.27] |
| 9 Professionals' attitude: client needs met | 1 | 45 | Mean Difference (IV, Random, 95% CI) | 1.56 [0.50, 2.62] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bright 1999.
| Methods | RCT Setting: Fee for service outpatient clinic, University of Memphis Department of Psychology, Memphis (TN), USA. Funding: Not reported. Recruitment (Clients): media advertisements, those eligible were added to clinic caseload as regular fee for service outpatients, with partial fee reimbursement for those who attended weekly sessions. Met inclusions: 146/400; of these 23 were excluded and 25 refused to take part (no reasons reported). Recruitment (consumer‐providers): Recruited from self‐help groups in which they had participated or led. Training/support: Both consumer‐providers and professionals received 2‐day training, using protocol and treatment manuals for cognitive behavioural therapy (CBT) and mutual support group therapy (MSG). Modules were: common interventions, cognitive behavioural techniques, and mutual support group methods. Therapists were paired with an opposite gender co‐therapist with similar availability. Professionals were paired together as were consumer‐providers. Further training/supervision was provided if therapists failed to adhere to the protocol (see 'fidelity' in Interventions section below). Inclusion criteria (Clients): Age between 18‐60 years, not currently in therapy, not currently on medication for mood disorders, no current drug or alcohol problems, minimum eighth‐grade education, ability to read and complete pretreatment assessment questionnaire, score ten or higher on Hamilton Rating Scale for Depression, Structured Clinical Interview DSM‐III‐R Non‐Patient Edition (SCID‐NP) criteria for current episode of definite major depressive disorder, dysthymia, or depression not otherwise specified. Exclusions (Clients): Diagnosis of bipolar disorder, alcoholism, drug abuse or dependence, organic brain syndrome, history of schizophrenia, depression with psychotic features, or mental retardation, receiving concurrent treatment, experiencing current active suicidal potential, or experiencing other need for immediate treatment. |
|
| Participants |
Clients: 98 participants (28.6% male). Mean age 45.8 (SD not reported). Range 21‐72 years. Principal mental health problem/diagnosis: Moderate to severe depressive symptoms. Treatment currently receiving: None (participants were excluded if they were receiving concurrent treatment). Description consumer‐providers: Half of the consumer‐providers (3 of 6) had led community‐based self‐help groups; and half of the professionals (4 of 8) had led self‐help groups. All of the consumer‐providers had participated in community‐based self‐help groups. Consumer‐providers' average age was 36 years (28 years for the professional therapists). Diagnosis of consumer‐providers: not reported. |
|
| Interventions |
Study aim: To assess the relative efficacy of professional and consumer‐provider therapists in providing group CBT and MSG. Intervention aim: To reduce clients' symptoms of depression and improve mood. Trialists hypothesised that clients in the professionally‐led CBT group would demonstrate better skill acquisition in monitoring and modifying dysfunctional thoughts compared with clients in the consumer‐led CBT group; and that clients in the consumer‐provider MSG group would show greater self‐disclosure than those in the professionally‐led MSG group. Role of consumer‐providers: Involvement as therapists delivering CBT or MSG interventions. Intervention (MSG): (n = 22) MSG therapy led by two paraprofessional consumer‐providers (male and female) . Sessions involved informal exchanges of information between individuals faced with the same difficulties. Intervention (CBT): (n = 21) CBT led by two paraprofessional consumer‐providers (male and female). Sessions were based on Feeling Good Seminar Series 1 with accompanying participant workbook, The Feeling Good Handbook. Control (CBT): (n = 27) CBT provided by two professional therapists (male and female). Control (MSG): (n = 29) MSG led by two professional therapists (male and female). Delivery: Ten weekly 90‐minute sessions. Each pair of co‐therapists (consumer‐providers and professionals) conducted an MSG and CBT group concurrently. Fidelity: Therapist sessions were supervised once weekly, and all therapy sessions were audio‐taped and observed by trained raters. If the therapist failed to accomplish any of the four general objectives for the intended condition or if they included any of the four general objectives from the other treatment conditions, further training/supervision was provided. Consumer involvement outside of the intervention: None. Changes in trial protocol: Unclear. |
|
| Outcomes | Assessments were conducted at baseline (pretreatment), weekly during the treatment phase, posttreatment (10 weeks), and 6 months follow up. Hamilton Rating Score for Depression (HRSD) Beck Depression Inventory (BDI) Automatic Thoughts Questionnaire (ATQ) Hopkins Symptoms Checklist‐58 (HSCL‐58) Out‐of‐session practice: average time spent working on personal issues (MSG) or homework assignments (CBT) between sessions. Therapy Compliance Checklist: observers rated therapy teams on four general objectives specific to CBT and four objectives specific to MSG. Each was rated as not present (0), subthreshold (+/‐1), or present (+/‐2), with positive indicating a match and negative indicating a mismatch between treatment intended and treatment delivered. Possible scores ‐8 to 8, higher scores better. |
|
| Notes | Four‐arm trial involved two relevant comparisons; 1) consumer‐provider led CBT vs professional led CBT and 2) consumer‐provider led MSG vs professional led MSG. Each comparison has been analysed separately. Direction of benefit was reversed for analysis of HSCL‐58 and HRSD outcome data. Power Calculation: Trialists estimated that N = 96 on the basis of an assumed attrition rate of 20%, a significance level of 0.05, power of 0.80 and an estimated moderate effect size of 0.30. Thirty clients terminated therapy before completing 7 sessions and the analysed outcome data for BDI, HSRD, HSCL‐58, and ATQ included only the 68 participants who attended at least 7 sessions and returned for the "posttest assessment". In some cases it may have been possible to collect and include posttest data from clients who attended less than 7 sessions and this may have been inappropriately excluded from the primary analysis. It is unclear what effect omission of data pertaining to these individuals would have on the outcomes. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "patients were blocked for gender and BDI score and were randomly assigned either to CBT or MSG" "Therapists negotiated among themselves on their practical availability to conduct a group at a given time...With these leaders then in place, group members were randomised to condition." (author communication) |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | "...clients were informed that they would be randomly assigned to the professional/paraprofessional and CBT/MSG conditions" (author communication) All outcomes involved participant responses who were not blinded to group assignments. |
| Blinding (performance bias and detection bias) All other outcomes | Low risk | "...outcome assessment was conducted by clinicians not involved in the trial who were blind to treatment assignment" (author communication) [However all outcomes were by self‐report]. |
| Incomplete outcome data (attrition bias) up to 6 months | High risk | "Thirty clients terminated therapy before completing seven sessions...We analysed outcome data from the BDI, the HSRD, the HSCL‐58, and the ATQ for the 68 participants who attended at least seven therapy sessions and returned for the posttest assessment" It is likely that in some cases it could have been possible to collect and include posttest data from clients that attended less than seven sessions and this may have been inappropriately excluded from the primary analysis. |
| Selective reporting (reporting bias) | High risk | Six month follow up data not reported. |
| Groups comparable at baseline? | Low risk | "...there were no pre‐treatment differences in the professional/paraprofessional groups" (author communication) |
| No contamination between treatment groups? | Low risk | Therapy compliance was assessed to ensure the integrity of the intervention was maintained by the different group leaders across the separate treatment groups and it is unlikely there was any crossover of group leaders or participants attending a different session than the one they were assigned to. |
Clarke 2000.
| Methods | RCT Setting: Community‐based mental health services in Portland (OR), USA in conjunction with consumer run drop in centre and subsequently case management services Mind Empowered Inc. (MEI), an assertive case management/supported housing program. MEI was entirely consumer operated and over 80% of the Board of Directors were consumers. MEI was the site for both the consumer‐provider and non‐consumer teams. Funding: Center for Mental Health Services. Recruitment (Clients): Clients being discharged from state and local hospitals or transferring to new service providers in the community were recruited by county mental health workers. Direct referrals from mental health agencies were also accepted. Research staff screened clients for eligibility. 180/189 met the inclusion criteria, two participants declined (no reasons reported). Recruitment (Consumer‐provider): Recruitment details not provided. Training/support: Intensive training on the assertive community treatment (ACT) model provided to staff from both teams at the beginning of the study, and throughout the next several years. Inclusion criteria: Adults in the Portland metropolitan area who met the Oregon definition of chronically mentally ill and priority 1 criteria. All had to be 18 years with a severe mental disorder as identified by a psychiatrist, a licensed clinical psychologist or a certified non medical examiner, and having a documented history of persistent psychotic symptoms (not caused by substance abuse), as well as impaired role functioning in two of three areas (social role, daily living skills, and social acceptability). Exclusions: Mental retardation. |
|
| Participants |
Clients: 178 participants (60.7% male). Mean age 36.5 (SD 10.3). Principal mental health problem/diagnosis: Schizophrenia (59.5%). Other characteristics: Substance abuse (33,1%), homeless in past six months (30.7%), hospitalised in the last six months (60.7%), and at least one prior arrest (63.2%). Treatment receiving: Not described. Description consumer‐providers: Self‐identified mental health consumers with a DSM‐III‐R axis I diagnosis. Main diagnosis was bipolar disorder (n = 4, 50%), other diagnoses included major depression, schizoaffective disorder, or cyclothymia. Most held a Bachelor's degree. |
|
| Interventions |
Study aim: To examine time to first episode, and number of clients experiencing hospital use, incarceration, emergency room visits and homelessness in people randomised to ACT involving consumer‐providers compared to ACT with professional staff or usual care. Intervention aim: To decrease adverse outcomes such as episodes of hospital use, incarceration, ER visits and homelessness. Trial duration: 3 years. Role of consumer‐provider: Case managers in ACT teams. Both ACT teams shared a psychiatrist, nurse practitioner, and clinical director. Each team consisted of four full‐time and one part‐time case manager, including a team leader. Intervention:(n = 57) Consumer‐provider case managers in an ACT team. Average caseload was 4.6 clients per case manager. Non‐consumer ACT team: (n = 57) Professional case managers with no diagnosable mental illness. Most held a Masters degree. Average caseload was 5.4 clients per case manager. Usual care: (n = 49) Participants received mental health services from agencies in the Portland metropolitan area. Delivery: Clients in ACT groups frequently had three to five weekly contacts with their mental health providers. Fidelity: Assessed with the Dartmouth ACT Fidelity Scale. Both ACT groups scored lower on all three scales compared with other states (Illinois and East Coast). Poor effectiveness may have been due to poor implementation based on lower fidelity. Consumer involvement outside of the intervention: None. Changes in trial protocol: None stated. |
|
| Outcomes | Interviews conducted every 6 months up to 24 months post randomisation. Case manager activity logs Case manager time allocation Location of services provided Emergency room visits Psychiatric hospitalisation |
|
| Notes | Data analysis involved comparison of the two ACT teams (Comparison 1) and did not include the usual care group. Power calculation: Authors calculated sample sizes needed to detect significant effects for each major outcome. Sample size used was far too small to detect an effect for each outcome. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly assigned to one of three conditions" Insufficient information provided to determine whether adequate sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Participants had to provide consent and were most likely aware of purpose of study. |
| Blinding (performance bias and detection bias) All other outcomes | High risk | Providers were aware of the different treatment being provided to participants. |
| Incomplete outcome data (attrition bias) up to 6 months | Unclear risk | Fifteen participants were excluded from the analysis (11 never began assigned treatment, 3 engaged with non‐study providers, and one subject had a developmental disability and was unable to complete the baseline interview). It is unclear whether missing data were balanced across treatment groups. |
| Incomplete outcome data (attrition bias) post 6 months | Unclear risk | Fifteen participants were excluded from the analysis (11 never began assigned treatment, 3 engaged with non‐study providers, and one subject had a developmental disability and was unable to complete the baseline interview). It is unclear whether missing data were balanced across treatment groups. |
| Selective reporting (reporting bias) | Low risk | Data reported for all quantitative outcomes. |
| Groups comparable at baseline? | Low risk | "No significant baseline differences were found between study conditions on demographic or clinical characteristics" |
| No contamination between treatment groups? | High risk | "While none of the usual care CMHC's initially operated assertive outreach case management teams, over the study period some agencies adopted aspects of the ACT program" Although located at separate locations, ACT teams involving consumer‐providers or professionals only shared staff that participated in treatment planning and consultation across both groups. |
Craig 2004.
| Methods | RCT Setting: Assertive outreach team in inner London Borough (UK) that targets the most alienated and least engaged users across the sector providing outpatient services. Funding: Not reported. Recruitment (clients): Clients currently registered with assertive outreach teams were screened for eligibility. Ninety clients met inclusion criteria however the case management team prioritised 45 clients for initial allocation because of case load limits. Recruitment (consumer‐providers): No details provided. Training/support: Originally 6 weeks training was provided to 3 part‐time consumer‐providers, however this was reduced substantially after unsuccessful retention of these consumer‐providers. The revised training focused on the client's social care needs, and the consumer‐provider role as client befrienders and advocates. Inclusion criteria: Clients of assertive outreach team with severe mental illness and a history of poor engagement. Exclusions: Clients of assertive outreach team that are well engaged with regular outpatient or depot clinic attendance, currently in prison, in the process of transfer to another team, or in long term hospital placements. |
|
| Participants |
Clients: 45 participants (66.7% male). Mean age 37.6 (SD 8.9), single (82%), live alone (56%). Principal mental health diagnosis/problem: All participants were moderately symptomatic, with an average total BPRS score of 39.4 (range 25‐64, higher scores worse) and suffered from chronic psychotic illnesses with paranoid schizophrenia the main diagnosis (87%). Other diagnoses/problems: Significant drug or alcohol abuse (29%), history of violence (40%), or criminal record (9/45). Fourteen participants were hospitalised at least once in previous year for average 67 days, 11 of these admissions were involuntary. Treatment currently receiving: Outpatient services. Description consumer‐providers: Two consumer‐provider roles, both suffered severe mental illness and were unemployed for a number of years, but had previously held down jobs. |
|
| Interventions |
Study aim: To investigate the feasibility and impact of employing mental health services users as health care assistants (HCAs) within an assertive outreach team. Intervention aim: To improve uptake and engagement with services, to decrease the number of unmet care needs, increase the size of the social network, and increase satisfaction with care. Role of consumer‐provider: Employed as full time HCAs (two positions), no other involvement in control of providing care, or development of program. Consumer‐providers engaged with clients from the outset in a befriending social care and client advocate role. Intervention: (n = 24) Assertive outreach team incorporating consumer‐providers as HCAs. Consumer‐providers reviewed welfare benefits and benefit uptake, encouraged attendance at clinic and vocational/social activities, led a recreational group at a church hall and helped clients with practical daily activities. Control: (n = 21) Case management and assertive outreach team involving psychiatrists and case managers from a nursing background. Duration: 12 months. Fidelity: Not reported. Intervention content and delivery likely to be highly variable between clients (ie individualised care was one of the aims of the intervention). Training was provided to providers but it is not clear whether this aimed to standardise the delivery or content of the intervention. Consumer involvement outside of the intervention: None. Changes in trial protocol: Yes, original protocol recruited and trained three consumer‐providers. None stayed with the program and two new consumer‐providers were recruited and trained with a different emphasis on training and role. |
|
| Outcomes | Outcomes assessed at baseline and 12 months follow up. Life Skills Profile (LSP) Significant Others Scale (SOS) Camberwell Assessment of Need (CANSAS ‐ staff version and client version) Verona Service Satisfaction Scale (VSSS) Service use |
|
| Notes | Percentage values were used to estimate the number of people with events for dichotomous outcomes. Client assessment of unmet needs (CAN) was used as an outcome measure for client satisfaction (direction of benefit reversed so that higher scores are favourable). CAN staff assessment of unmet needs was used as an outcome measure for professional attitudes (ie staff assessment of client needs; direction of benefit reversed so that higher scores are favourable). Did not attend rates for clinic appointments are presented in analyses as use of mental health services (direction of benefit reversed so that higher scores indicate benefit). Power calculation: Power calculation performed but not reported. Authors indicate that the study (pilot) was based on a sample size that was approximately half that suggested by the power calculation therefore the study was underpowered to detect significant differences between groups if they existed. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...random number tables" |
| Allocation concealment (selection bias) | Low risk | "The case management team identified 45 clients for initial allocation and these were sequentially numbered and random number tables were used to allocate them" "Participant allocation was carried out according to sequence allocation through a telephone call to an administrator who was independent of the clinical team and the research staff" (author communication) |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | "All clients were told of the project, that allocation to meeting one of the HCAs was by randomisation" |
| Blinding (performance bias and detection bias) All other outcomes | High risk | "With the exception of attendance records, therefore, the major findings from the secondary outcome analysis are reliant on interviews with staff who were not blind to the intervention and had a vested interest in seeing it succeed" |
| Incomplete outcome data (attrition bias) post 6 months | Low risk | "12 participants either refused or provided incomplete baseline interviews and four of these also refused follow‐up interview" Attrition losses were balanced across treatment groups. |
| Selective reporting (reporting bias) | Low risk | Protocol not available. Data reported for all quantitative outcomes. |
| Groups comparable at baseline? | Low risk | "...intervention and comparison groups were well balanced with no substantial differences on any demographic variable at baseline" |
| No contamination between treatment groups? | High risk | "some of the clients in the standard care arm also attended the social occasions that the HCAs led" |
Gordon 1979.
| Methods | RCT Setting: Residential hospital in Florida, USA Funding: Not reported. Recruitment (clients): Recruited during last two weeks of nine‐week residence at Florida Mental Health Institute; patients were involved in a previous study of a peer management peer‐support program during their stay. Recruitment (consumer‐providers): Previous residential clients of Florida Mental Health Institute could apply to be Community Area Managers or a Network Director. The consumer providers receive training and a Peer Counselling manual. The manuals provide instructions on solutions for such issues as employment, housing, recreation, patient crises and instability, and medical problems. Staff from the Community Network Development projects supervise and provide clinical back‐up. Inclusion criteria: Clients experiencing their first hospital admission or who had had less than four months' hospitalisation before the current hospitalisation for mental illness. No further details provided. Exclusions: Not described. |
|
| Participants |
Clients: 80 clients (aged 18‐45) recruited two weeks before discharge from a nine‐week mental health early intervention program. No baseline data provided. Principal mental health diagnosis/problem: Not provided. Other diagnoses/problems: Not described. Treatment currently receiving: Outpatient services. Description consumer‐providers: Former hospital inpatients, selected on the basis of overall emotional adjustment and motivation, and possession of a current driver's license, car and telephone. No further details provided. |
|
| Interventions |
Study aim: To assess the effectiveness of a Community Network Development (CND) program involving consumer‐providers in reducing patient recidivism. Intervention aim: To reduce rehospitalisation and community mental health service use. Role of consumer‐provider: to maintain contact with 20 to 50 local CND members; organise and lead weekly meetings; provide peer counseling' organise business or fund raising activities; assist group members in times of crisis; maintain positive attitude among group members. Intervention: (n = not described) Prior to discharge, clients received support on transition to community life, including training on pre‐employment skills, peer counseling, group leadership, and community living. After discharge, in addition to treatment as usual, clients were followed up by Community Area Managers staff who live locally (within 30 mins drive). Clients were encouraged to attend meetings which included a social activity (eg picnic, shopping etc). Support for transportation and social contact was encouraged between group members. Control: (n = not described) Treatment as usual; traditional aftercare services with referring therapists or a local Community Mental Health Centre. Duration: 10 months. Fidelity: Not reported. Consumer involvement outside of the intervention: None. Changes in trial protocol: None described. |
|
| Outcomes | Outcomes assessed at 10 months. Rehospitalization. Length of stay Use of community mental health services |
|
| Notes | Numbers randomised to each group were not specified. Therefore outcome data reported are unusable. Paper published in Self‐Help Reporter in March‐April 1979 was not able to be obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) All other outcomes | Unclear risk | No information provided on blinding of outcomes. |
| Incomplete outcome data (attrition bias) post 6 months | Unclear risk | Data not provided in a usable format. |
| Selective reporting (reporting bias) | Unclear risk | Authors provide data for outcomes, however, data are unusable as there is not information on numbers randomised to each group. It is also unclear if other outcomes were measured and not reported. |
| Groups comparable at baseline? | Unclear risk | No baseline data provided. |
| No contamination between treatment groups? | Unclear risk | No information provided. |
Kaufmann 1995.
| Methods | RCT Setting: Community mental health centre (CHMC), Pittsburgh (PA), USA. Funding: National Institute of Mental Health Recruitment clients: Clients of urban community mental health centre who received treatment during a period of 27 months and met eligibility criteria were recruited to the study. Subjects were paid for completing research interviews. 823 participants met inclusion criteria, however 582 were excluded (they were either inpatients, enrolled in a partial hospital program that met at the same time as the self‐help groups, or were already members of the self‐help groups) and 151 refused to take part (2 after informed consent, 1 had incomplete data, and no reasons given for the remaining 148). Recruitment consumer‐providers: Not described. Training/support: Investigators and staff at the self‐help group and CMHCs collaborated together. All research contacts with self‐help group members were made with the agreement of the membership of the self‐help group and individual members could veto over researcher participation in the project. Vetoes involved excluding the recording of any activity at the drop‐in centres, and limiting access to pre‐arranged times. Biannual community Advisory Board meetings at the drop‐in centres were conducted and researchers updated the Board on research project progress and members presented demonstrations and personal accounts of activities at self‐help group meetings. Inclusion criteria: Psychiatric diagnosis of schizophrenia, schizoaffective disorder or major mood disorder, normal intelligence, recent inpatient or outpatient psychiatric treatment. Exclusions: Personality disorders. |
|
| Participants |
Clients: 90 participants (38.9% male). Mean age 42 (SD not reported), unemployed (87%), never married (51%). Principal diagnosis: Schizophrenia (54.4%), schizoaffective disorder (13.3%), or major affective disorder (32.2%). Treatment receiving: Inpatient or outpatient treatment at community mental health centres. Description consumer‐providers: Current and former psychiatric patients working at drop in centers operated under sponsorship of the community mental health centre. |
|
| Interventions |
Study aim: To test the effectiveness of self‐help group on outcomes for people with severe and long‐standing mental illness. Intervention aim: To reduce symptoms in people with severe and long‐standing mental illness. Intervention: (n = 54) Participants referred to 1 of 3 self‐help groups run by current and former psychiatric patients with a psychosocial rehabilitation clubhouse approach, in addition to usual care at the CMHC. A consumer outreach worker from the self‐help groups also contacted experimental subjects, and offered to accompany them to their first group meeting. Group meetings occurred once a week at three community mental health sponsored and operated drop‐in centres. The centres were not solely run by consumers, however they had at least one self‐help group member in a paid staff position. Attendance at the drop in centre was voluntary. Control: (n = 36) Participants not told about the self‐help groups; encouraged to continue with their usual care at the community mental health centre. Duration: Unclear, records at the self‐help group were kept for 6 months. Fidelity: Attendance at the drop in centre was voluntary. There was cross‐over between groups (17% of both the treatment and control groups participated in self‐help groups). Consumer involvement outside of the intervention: Data collection. The research team provided a cash honorarium to those members who collected data for the research project. Changes in trial protocol: Yes, post hoc design aimed at uncovering reasons for low participation in self‐help activities in the study sample. Due to the overall low rates of participation, and the number of subjects who were cross‐overs, the researchers decided to stop collecting follow‐up outcome data and searched for factors in the sample's composition and the self‐help group membership which might account for low participation. |
|
| Outcomes | Outcomes assessed at baseline and six months. Brief Psychiatric Rating Scale (BPRS) Symptom Check List‐90 (SCL‐90) Attendance |
|
| Notes | 9/54 experimental subjects (17%) participated in self‐help group activities. 6/36 (17%) control subjects participated; hence there was no significant difference in participation rates between groups. Data were only reported comparing participators vs non‐participators and did not compare the original randomised groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...randomly assigned" Insufficient information provided to determine whether adequate sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | "Subjects were told that they were volunteers in a study of self‐help" Participants not blind however, data assessors were not aware of group assignments. |
| Blinding (performance bias and detection bias) All other outcomes | Unclear risk | Unclear whether health professionals were blind to group assignments. |
| Incomplete outcome data (attrition bias) up to 6 months | Low risk | "Two subjects withdrew after initial consent, and one had incomplete data" |
| Selective reporting (reporting bias) | High risk | "...we stopped collecting follow up outcome data and searched for factors in the sample's composition and the self‐help group membership which might account for low participation" Data analysis compared participators to non‐participators regardless of the groups they were assigned to by randomisation. |
| Groups comparable at baseline? | Low risk | "Analysis of baseline assessment data showed no statistically significant differences between experimental and control subjects" |
| No contamination between treatment groups? | High risk | "...there was no significant difference in rate of self‐help group participation between experimental and control subjects" Nine (17%) experimental subjects and six (17%) control subjects participated in self‐help group activities. |
O'Donnell 1999.
| Methods | RCT Setting: Outpatient mental health services, Eastern Sydney Area Health Service (Australia). Funding: Commonwealth Innovative Grants Program of the National Mental Health Strategy. Recruitment clients: Inpatients or community health centre clients referred for case management were invited to participate. 530 clients met the inclusion criteria, 359 were excluded from participation, and 52 refused to take part (no reasons provided). Recruitment consumer‐‐providers: Recruited over a 14 month period through Eastern Area Mental Health. No other details reported. Training/support: Consumer Consultants trained the consumer‐providers and other advocates over a 3‐day period on subjects including the Mental Health Act, patient rights, communication and listening skills, assertiveness, conflict resolution, and stress management. Mental Health staff provided training on the diagnosis and treatment of schizophrenia and bipolar disorder, psychosocial and family interventions, case management, rehabilitation, supportive accommodation services and other community resources. Advocates met individually with a Project Director monthly, and advocates met as a group once a month. After some time this was considered inadequate support, so phone debriefing was established with an experienced advocate. Inclusion criteria: People aged 18‐65 years, English‐speaking, met DSM‐IV criteria for schizophrenia, schizoaffective disorder, schizophreniform disorder or bipolar affective disorder, referred for case management by community health services within old Eastern Sydney Area Health Service. Exclusions: Co‐diagnosis of substance dependence disorder, current Community Treatment Order or Community Counselling Order, history of violence (unless associated with acute psychosis). |
|
| Participants |
Clients: 119 participants (57.1% male). Mean age 36 years (SD 9.8). Mean education 11.6 years. Predominately lived alone (39%), or with family (30%), and were supported by pension (72%), mean duration 80 months. Principal mental health diagnosis/problem: Schizophrenia (66%); schizoaffective disorder (16%); schizophreniform disorder (6%); and bipolar (12%). Stage of illness: Mean duration of illness was 117 months (SD 98.9, range 1‐432), mean number of hospital admissions 6 (SD 6.4, range 1‐30), and mean number of admissions per year 1 (SD 0.93, range 0‐6). Description consumer‐providers: Six advocates and three reserve advocates were included that were either: 1) recovered individuals who had experienced mental illness themselves (consumer‐providers); 2) siblings or carers of people who had experienced mental illness (secondary consumers); or 3) non‐consumers who were interested in working with people with mental illness. During the project the focus changed to studying the effects of only primary consumers so advocates were replaced as positions opened with consumer‐providers only. |
|
| Interventions |
Study aim: To redress the perceived hierarchical delivery of mental health services, in which the "service" has the authority and the client has little or none, with the services being imposed. The project aimed to empower the client by establishing parity between client and staff without legal imposition and involve clients in their rehabilitative process in a consensual manner that promoted respect, dignity and self‐determination. Intervention aim: To test if the delivery of client focused case management services compared with standard community practice would improve functioning, disability, quality of life, and service satisfaction for clients, as well as family burden of care outcomes. To test if consumer advocacy services in addition to client focused case management service delivery would improve outcomes, and whether clients who were more empowered by the use of client‐focused approaches would be more satisfied and compliant with services received. Role of consumer‐provider: Employed as consumer advocates in case management teams, initially recruited to each work 3 hrs/week (based on Rozelle Hospital advocate program). Advocates were assigned 3‐6 clients each for 12‐month period. Intervention: Client‐focused case management (n = 45) plus consumer advocates (some consumer‐providers). Consumer advocates provided self‐advocacy for clients, encouraged client's self confidence, and were role models for clients during their recovery. They also communicated with case managers and participated in the development of recovery agreement meetings where requested by clients. Control 1: Client‐focused case management (n = 39). Case managers trained in the use of Rose's Advocacy Empowerment Model in clinical practice and familiar with solution‐focused and narrative approaches to therapy. Involved customised recovery plans, with emphasis on client recovery goals. Recovery agreement meetings held between client, case manager, treating psychiatrist, family member or significant other, and sometimes consumer advocate to reinforce support for client achieving recovery goals. Control 2: Standard case management (n = 35). Usual case management practices provided by existing community case managers. Duration: 12 months. Fidelity: Consumer advocacy and client participation was seemingly compromised as it was not possible to widely advertise or promote consumer advocacy or its potential benefits because the study was only open to clients in particular diagnostic categories. This meant consumer advocates had to explain their role and promote themselves to clients, and this reportedly had a disempowering effect on the advocates. Client‐related illness (eg paranoid symptoms) also led to clients rejecting advocates before they could develop rapport. Consumer involvement outside of the intervention: None. Changes in trial protocol: Changed eligibility criteria from 55 to 65 years to increase potential participants. Siblings, carers or interested non‐consumers, in addition to consumer‐providers, were originally recruited as advocates but a post hoc decision meant that only consumer‐providers were recruited to replace advocates that left during the project. |
|
| Outcomes | Outcomes were assessed at baseline 6 months and 12 months. Quality of Life Index for Mental Health (QOLIMH) Health of the Nation Outcomes Scales (HoNOS) Life Skills Profile (LSP) Client Service Satisfaction Questionnaire (CSQ) Service use |
|
| Notes | Data analysis involved comparison of the two client focused case management teams and did not include the usual care group (note that reported data in the article appears to be the client focused case management groups combined and compared to standard case management). Power calculation: Not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly assigned to one of three groups". Insufficient information to determine whether adequate sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Participants required to provide informed consent therefore unlikely to be blinded. |
| Blinding (performance bias and detection bias) All other outcomes | Unclear risk | Unclear whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) up to 6 months | Unclear risk | Six month data not reported. |
| Incomplete outcome data (attrition bias) post 6 months | Low risk | Losses were unbalanced across treatment groups however reasons provided indicate this is an unlikely source of bias. |
| Selective reporting (reporting bias) | High risk | "Although subjects were also followed up at 6 months, the results for this stage will not be presented here as they add little to the study results" |
| Groups comparable at baseline? | Low risk | "...there were no significant differences between the three groups at baseline with respect to sociodemographic variables, illness factors or medication factors" |
| No contamination between treatment groups? | Unclear risk | It is unclear whether any community peer support services were available to participants in the control groups. |
Rivera 2007.
| Methods | RCT Setting: Elmhurst Hospital Center, New York City (NYC), USA. Funding: NYC Department of Health and Mental Hygiene, New York State Office of Mental Health, and the NYC Health and Hospitals Corporation. Recruitment (clients): Research assistants recruited discharged inpatients with persistent and severe mental illness from inpatient units at a city hospital Jul 1997 ‐ Dec 2000. Recruitment (consumer‐provider): Recruited from vocational training and peer advocacy programs, 369 /585 clients who met inclusion criteria consented to take part, 114 clients were excluded (mostly because they were discharged to alternative treatment settings), and 216 refused to take part (no reasons reported). Training/support: Professional and consumer‐provider intensive case management staff received similar orientation and training with additional elements to address their specific roles. Before working with clients, staff had 40 hours of training with competency testing. Staff also received 1 hr individual supervision and 1 hr group supervision, and 1.5 hours of training weekly for the duration of the project. Consumer‐providers were supervised by a full‐time and half‐time social worker who met with them individually and in groups to solve problems and plan activities. Inclusion criteria: Aged 18+ years, diagnosed psychotic or mood disorder on axis I, and two or more psychiatric hospitalizations in the previous 2 years. Exclusions: None stated. |
|
| Participants |
Clients: 255 participants. Mean age 38.3 (SD 12.8). Never married (60%). Education 12.0 years (SD 3.0). Principal mental health diagnosis/problem: Schizophrenia (29%), schizoaffective disorder (20%), bipolar (26%), depression (22%) or other psychotic disorder (3%). Treatment receiving: Intensive case management or clinic care. Description consumer‐provider: Consumer‐providers had history of multiple hospitalizations for mood or psychotic disorders, were eligible for disability benefits, relied on medication for stability and had between three to eight years of sobriety and stability in the community. |
|
| Interventions |
Study aim: To compare intensive case management involving consumer‐providers or professionals with standard clinic‐based care. Intervention aim: To evaluate whether consumer‐providers enhance case management outcomes through the provision of social support. Consumer‐providers were expected to improve social networks for clients leading to positive changes in social function and quality of life. Role of consumer‐provider: Part of intensive case management team, responsible for developing social support and contribute to treatment planning case management meetings. Intervention: (n = 70) Consumer‐provider assisted strengths‐based intensive case management which focused on client autonomy. Consumer‐providers engaged clients in social activities and helped develop supportive social networks. They were guided by preferences of clients in planning activities which included home or community based one‐on‐one group social activities to help facilitate independent relationship building using natural community resources. They were instructed not to provide peer routine case management services. Consumer‐providers also contributed to treatment planning and provided information about participants during weekly team meetings. Standard care: (n = 66) Strengths‐based intensive case management provided by 2 licensed clinical social workers. Individual care provided using natural community resources and backup from a team member. Caseloads limited to 20 participants. 24 hour telephone coverage. Participants encouraged to participate in cognitive‐behavioural group therapy. Clinic‐based care: (n = 67) Doctoral‐level psychologist and clinical social worker provided clinic‐based services using a strengths‐based approach. No 24‐hour telephone coverage available. Duration: 30 months. Fidelity: No details reported. Consumer involvement outside of the intervention: None. Changes in trial protocol: None described. |
|
| Outcomes | Assessments conducted at 6 and 12 months. Lehman Quality of Life Inventory (QOLI) Brief Symptom Inventory (BSI) Pattison Network Inventory (PNI) Behavioural Health Care Rating of Satisfaction (BHCRS) Hours of activity with care providers Hours of individual therapy Hours of group therapy Contacts with mobile crisis unit/case management Days of hospitalisation Outpatient clinic visits Days of hospital treatment |
|
| Notes | Data collected from 1 to 6 months and 7 to 12 months were added together to give overall data for 12 months for health service use outcomes and hospital service use. The subjective social relations subscale of QOLI was used as the social outcome measure. Data analysis involved comparisons of the strengths based intensive case management teams involving consumer‐providers and professionals and did not include the clinic based care group. Power calculation: Trialists reported that approximately 150 participants divided among three groups would be needed to detect a moderate group effect with 80% power at the 0.05 alpha level. To detect treatment by time interactions of moderate size the same number of participants would yield 90% power at the 0.05 alpha level. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomly assigned to one of the three treatment groups". No other information provided. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Unclear risk | Unclear whether participants were aware of purpose of study. |
| Blinding (performance bias and detection bias) All other outcomes | Low risk | "Research assistants who were blind to the treatment assignments collected all interview data...Data were entered into a secure database by using unique identification numbers for participants" Other outcomes probably blinded. |
| Incomplete outcome data (attrition bias) up to 6 months | Low risk | "...sample size was reduced from 255 to 203, mostly because some clients were discharged to long‐term residential programs that would not allow enrolment in our clinic...Missing data contributed to small variations in sample sizes for the analyses" |
| Incomplete outcome data (attrition bias) post 6 months | Low risk | Same as above. |
| Selective reporting (reporting bias) | Low risk | All outcome data reported. |
| Groups comparable at baseline? | Low risk | "There were no significant differences between treatment groups at baseline on the following variables: sex, race or ethnicity, age, education, marital status, and diagnosis" |
| No contamination between treatment groups? | Unclear risk | No information provided. |
Rogers 2007.
| Methods | RCT Setting: 8 study sites in various states across the USA (3 in northeast, 1 on west coast, 2 in the south, and 2 in the Midwest). Experimental and control groups located at each site. Funding: USA Department of Health and Human Services (DHHS), Substance Abuse and Mental Health Services Administration (SAM‐HSA). Recruitment (clients): Participants recruited from traditional mental health providers who partnered with consumer operated service programs (COSP). No details were provided on numbers eligible, excluded, or refused participation. Recruitment (consumer‐provider): Not described. Inclusion criteria: Diagnosed serious and persistent mental illness (DSM Mental Disorder Axis I or II), 18 years or older, able to provide full and informed consent, actively attending traditional mental health provider within previous 12 months (at least 4 mental health services in past year and at least 1 in the past 4 months). Exclusions: Unable to participate in research interviews, more than 3 visits to the COSPs under study in the past 6 months. |
|
| Participants |
Clients: 1827 participants (39.9% male). Mean age 42.7. College/Vocational Training (38.7%), married (12.6%), have children (52.8%), currently employed for pay or volunteer (29.3%), currently in own residence (57.9%), currently homeless (10.2%), social security income past 30 days (83.6%). Principal diagnoses: Schizophrenia or psychotic disorder (50.4%), mood disorders (44.4%), anxiety disorders (3.7%), other (1.5%). Stage of illness/problem: Mean age first psychiatric contact 23.0. Recent psychiatric hospitalisation (16.0%). Other health problem: Physical disability (51.7%). Description consumer‐provider: Eight COSPs categorised as drop‐in (n = 4), peer support and mentoring (n = 2), and education and advocacy (n = 2). Common ingredients across all COSPs included a focus on peer support, recovery education, empowerment, and tangible assistance for independent community living. |
|
| Interventions |
Study aim: To examine the effectiveness of COSPs on improving psychological, social, and objective and subjective functioning outcomes in individuals who receive traditional mental health services. Intervention aim: To provide peer support, recovery education, empowerment, and tangible assistance for independent community living. Role of consumer‐provider: Services included drop‐in (n = 4 sites), peer support and mentoring (n = 2 sites), and education and advocacy (n = 2 sites). Intervention: Attendance at a COSP in addition to traditional mental health service. COSPs varied in the type of service provided such as drop‐in, peer support and mentoring, and education and advocacy. Common ingredients across all COSPs included a focus on peer support, recovery education, empowerment, and tangible assistance for independent community living. Control: Traditional mental health services provided by professionals or paraprofessionals including psychiatrists, social workers, psychologists, and residential providers. Duration: 1998 to 2004. Fidelity: Fidelity Assessment Common Ingredients Tool (FACIT). Program Structure (possible score 10‐48); drop‐in 39.13, peer support 35.00, education and advocacy 42.00. Environment (possible score 11‐50); drop‐in 42.38, peer support 34.00, education and advocacy 36.75. Belief Systems (possible score 9‐40); drop‐in 34.75, peer support 35.50, education and advocacy 34.50. Peer Support (possible score 8‐35); drop‐in 29.25, peer support 29.50, education and advocacy 23.25. Education (possible score 5‐25); drop‐in 13.25, peer support 16.50, education and advocacy 23.75]. Advocacy (possible score 3‐15); drop‐in 8.00, peer support 12.00, education and advocacy 13.50. Authors note that they conducted two rounds of pilot testing of the assessment protocol and the standardised interviewer training to ensure accurate data collection. Consumer involvement outside of the intervention: Consumer/survivors who represented the COSPs joined with other consumers on research teams to form a Consumer Advisory Panel as part of their participation in the federal study. Changes in trial protocol: None described. |
|
| Outcomes | Assessments conducted at baseline, 4, 8, and 12 months. Making Decisions Empowerment (MDE) Personal Empowerment (PE) Organisationally Mediated Empowerment (OME) Attendance: Dichotomous (any contact vs no contact) as well as categories based on frequency of utilisation (0 = no contact, 1 = > 0 and < 8.5 visits, 2 = > 8.5 visits). |
|
| Notes | Percentage values were used to estimate number of people with events for dichotomous outcomes. Number of people assessed in each group was assumed to be the number of people randomised. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Each site developed randomisation procedures that prevented "gaming", largely through the use of computer‐generated random number tables" |
| Allocation concealment (selection bias) | Unclear risk | (see quote above) "...these procedures remained under the control of the researchers and not the interviewers or program staff" It is unclear whether researchers had the opportunity to manipulate group assignments. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Participants had to provide informed consent and were likely to be aware of purpose of study. |
| Blinding (performance bias and detection bias) All other outcomes | Unclear risk | Unclear whether mental health service providers, clinicians or research staff were blinded to group assignments. |
| Incomplete outcome data (attrition bias) up to 6 months | Unclear risk | Data not provided. |
| Incomplete outcome data (attrition bias) post 6 months | Unclear risk | "The attrition rate from baseline to the end point of the study (12 months) was approximately 20.5 percent" Insufficient information to determine whether an imbalance of losses across treatment groups or the potential impact of incomplete data on results. |
| Selective reporting (reporting bias) | High risk | Complete data set provided for baseline assessments of all outcomes however follow‐up data are less comprehensive and appears to be selectively reported for a subset of participants or results that are based on the trialists' 'as treated' approach. |
| Groups comparable at baseline? | Unclear risk | "We found no significant differences in baseline scores for the MDE, PE Choice, PE Reduction in Chance, or OME for the entire sample by experimental condition" However, baseline participant characteristics were not reported separately for each experimental condition therefore unable to judge whether there were any potential confounders between groups. |
| No contamination between treatment groups? | High risk | "..participants were able to continue to receive traditional mental health services and use COSPs regardless of their randomisation assignment...We found that 57 percent of those assigned to the intervention condition and 15 percent of those assigned to the control condition used the COSPs" |
Sells 2006.
| Methods | RCT Setting: 4 study sites across Connecticut, USA. 3 sites were state‐operated mental health agencies; two urban and one rural. Fourth site was a nonprofit agency serving a rural population. Funding: Yale Institution for Social and Policy Studies. Peer‐based treatment sponsored by Connecticut Department of Mental Health and Addiction Services. Recruitment (client): Prospective participants identified through mental health authorities were invited to a project interview. Consenting participants were paid $20 for completion of baseline interview. Recruitment (consumer‐providers): All peer staff worked as providers within the Connecticut Peer Engagement Specialists project, a four‐site statewide investigation at public mental health centres in three Connecticut towns and through contract with a nonprofit agency in a fourth town. No details were provided on numbers eligible, excluded, or refused participation. Training/support: Consumer‐providers received 2 weeks training by professional and peer healthcare staff. Topics included outreach and engagement; ethical guidelines; local community resources; and record keeping. Consumer‐providers received supervision from clinical supervisors. Regular providers worked on the same treatment teams as consumer‐providers. Inclusion criteria: Diagnosed serious mental illness (schizophrenia spectrum disorder, major mood disorder, or both) with a history of being difficult to engage in treatment (provider‐assessed using Level of Care Utilization System) and inflicted or threatened to inflict serious physical injury upon another person within the last 5 years. Exclusions: None stated. |
|
| Participants |
Clients: 137 participants (61.3% male). Mean age 41 (SD 9), range 20‐63. Principal diagnoses: Main diagnoses were psychotic disorder (61%) or major mood disorders (63%). Co‐occurring disorders (70%). Description consumer‐providers: All 8 consumer‐provider staff had publicly disclosed histories of severe mental illness and some had disclosed histories of co‐occurring drug use disorders. |
|
| Interventions |
Study aim: To study the effects of consumer‐provider case management services on treatment relationship dimensions and engagement for clients with severe mental illness early in the treatment process. Intervention aim: Consumer‐provider communications were expected to be more validating than invalidating compared to regular providers. It was hypothesised that invalidating communication from consumer‐providers, but not from traditional providers, would be significantly associated with favourable client outcomes including significantly higher rates of enrolment and participation, lower rates of hospitalisation and incarceration, more days in stable housing and higher scores on quality of life and community integration measures compared to those in usual care. Role of consumer‐provider: Consumer‐providers partnered with assertive community treatment teams. Consumer‐providers delivered non clinical activities determined by the clients' interests. Consumer‐provider caseload average was 10‐12 clients (approximately half the case load of the control group). Intervention: Mental health agency sites (n = 3) provided ACT with consumer‐providers as case managers. Non‐profit agency (n = 1) provided three integrated teams for case management, clinical, and psychosocial rehabilitation. Consumer‐providers were assigned to psychosocial rehabilitation team. However consumer‐provider peer specialists were not integrated within the teams and worked almost exclusively with their clients. They were not required to fulfil traditional case manager responsibilities and focused their time on clients. Control: Regular community‐based treatment provided at each study site without involvement of consumer‐providers. Ideally, ACT staff worked as a team, sharing responsibility for meeting all of their clients’ basic needs while focusing primarily on medication and case management. Duration: July 2001 to June 2003 (participants received 12 months of intervention). Fidelity: 3 agency sites delivered ACT while the non‐profit agency site used 3 different integrated teams: case management, clinical, and psychosocial rehabilitation. Consumer involvement outside of the intervention: None. Changes in trial protocol: None described. |
|
| Outcomes | Outcomes assessed at baseline, 6 and 12 months. Quality of Life (QOLI‐B) Barrett‐Lennard Relationship Inventory (BLRI) Attendance: Number of contacts in past 30 days Service use |
|
| Notes | Calculated the treatment effect of each BLRI subscale (positive regard, empathy, unconditionality) and presented the median treatment effect in the analysis for the client manager relationship outcome. Power calculation: Not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided. |
| Allocation concealment (selection bias) | Unclear risk | "After the client left the room, the researcher would randomly assign the individual to one of two groups." Insufficient information to determine whether adequate concealment of allocation. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Participants were aware of the purpose of the study. |
| Blinding (performance bias and detection bias) All other outcomes | High risk | Providers were not blinded. |
| Incomplete outcome data (attrition bias) up to 6 months | Low risk | "The discovery by researchers that ineligible clients had been enrolled resulted in an overhaul of the referral process and exclusion of several enrolled clients." BLRI data: 54/68 participants assessed in consumer‐provider group and 51/69 in control group. Losses balanced across groups. |
| Incomplete outcome data (attrition bias) post 6 months | High risk | BLRI data: 42/68 participants assessed in consumer‐provider group and 32/69 in control group. Reasons for losses not provided. Losses not balanced across groups could bias results in either direction. |
| Selective reporting (reporting bias) | High risk | Only reported on a subsample of 25 clients for attendance (those rated by clinicians as least engaged in treatment). Limited information provided for QOLI‐B or service use. |
| Groups comparable at baseline? | Unclear risk | Conditions of serious mental illness balanced across groups however, no further information provided about the characteristics of participants across treatment groups. |
| No contamination between treatment groups? | Unclear risk | "...all providers attended the same meetings and could freely interact and share practice activities." Peer and regular providers were on the same treatment teams. |
Sledge 2011.
| Methods | RCT Setting: Yale‐New Haven Psychiatric Hospital, acute care hospital, New Haven, Connecticut, USA. Funding: Grant M123828 Eli Lilly; Connecticut Department of Mental Health and Addiction Services; George D and Esther S Gross Professor of Psychiatry endowment. Recruitment (client): Prospective participants identified people admitted to the Yale‐New Haven Psychiatric Hospital between 1 Nov 2006 and 1 Nov 2008. Recruitment (consumer‐provider): Recruited from formal job postings. No details were provided on numbers applied, eligible, excluded, or refused participation. Training/support: Consumer‐providers received training on fundamentals of recovery philosophy and promotion practices, local resources available, boundaries, safety, cultural competence, gender factors, trauma‐informed care, motivational interviewing techniques. Training occurred over 16 days during four weeks, with homework. Received a salary from the state Department of Mental Health, under the supervision of staff at the Connecticut Department of Mental Health and Addiction Services. They did not report to or take direction from clinical staff who were directly responsible for patient care. They had ongoing supervision, including 90 minute, weekly team meeting, conducted by study supervisors and the mentors' direct supervisor. Inclusion criteria: 18 years or older; two or more psychiatric hospitalisations in previous 18 months; documented DSM‐IV diagnosis of schizophrenia, schizoaffective disorder, psychotic disorder not otherwise specified, bipolar disorder or major depressive disorder, and willing to accept random assignment. Exclusions: unable to give signed, written consent; unable to speak English; unavailable because of imminent incarceration; primary DM‐IV axis I diagnosis of substance abuse or dependence or an axis II diagnosis alone. |
|
| Participants |
Clients: 89 participants randomised, 15 withdrew consent leaving an intention to treat sample of 74 (intervention n = 38, 45% male; control n = 36, 58% male). Mean age: intervention: 42.4 years (SD 11.5); control: 38.7 years (SD 8.4) . Principal diagnoses: Main diagnoses were psychotic disorder: intervention: 68%, control: 69%, and mood disorders: intervention: 32%, control 31%. Description consumer‐providers: All 8 consumer‐providers were in recovery from a severe mental illness, openly self‐identify as having a history of mental illness, demonstrated strong interpersonal skills, and willing to work in the community and complete a paid training program. |
|
| Interventions |
Study aim: To determine whether recovery mentor support services are effective in promoting recovery and social integration among psychiatrically disabled individuals who experience high rates of inpatient hospitalization. Intervention aim: Consumer‐provider were to deliver support for participants (peer companion model), with the aim to reduce inpatient hospitalizations. Role of consumer‐providers: Consumer‐providers gave support for clients. Consumer‐providers delivered non‐clinical activities determined by the clients' interests. Consumer‐provider caseload not described. Intervention: Mentors were instructed not to aim for any specific goal other than to support their clients (n = 38). Recovery mentors were trained to use their own first‐hand experiences as a basis on which to provide support to participants. Frequency of contact determined by mentee in collaboration with mentor. 13 of 38 intervention‐group patients had no contact with their mentee. Data for 55% of intervention‐group patients showed that mean frequency of contact was 13.43 contacts (SD 11.46), over nine months. Mean total hours of contact: 24.15 hours (SD 17.41). Control: (n = 36) Direct clinical care received by both groups consisted of what was available to them through their own efforts and resources. Most of the clinical care was delivered in the public sector via community‐based organizations that are funded by the DMHAS either through a state facility or grants to private, nonprofit community‐based, mental healthcare centres. Generally clinical care consisted of medication, psycho‐education and case management, and supportive psychotherapy. Duration: Nov 2006 to Nov 2008. Fidelity: 13 (34%) of clients had no contact with their mentor during study period despite being assigned to mentor arm. Consumer involvement outside of the intervention: None. Changes in trial protocol: None described. |
|
| Outcomes | Outcomes assessed at 3 and 9 months. Number of hospitalizations Number of days in hospital Trial protocol outcomes listed included: Sense of community Motivation for change Social functioning Hope Self determination Functional status Treatment relationship |
|
| Notes | Contacted authors regarding secondary outcomes, who advised that data were collected and authors are currently drafting a manuscript for these outcomes. Power calculation: Not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization scheme generated with SAS statistical software with a 50‐50 split between recovery mentor and treatment as usual for 120 participants." |
| Allocation concealment (selection bias) | Low risk | "Each randomized assignment was separated and placed in consecutive order in a sealed, numbered envelope by staff (who were not directly linked to the study) at the Program for Recovery and Community Health." |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Unclear risk | It is unclear if participants were aware of the purpose of the study. |
| Blinding (performance bias and detection bias) All other outcomes | High risk | Supervisors of mentors also participated in some follow‐up evaluations and were not blind to participants' treatment status. |
| Incomplete outcome data (attrition bias) up to 6 months | Unclear risk | No 3‐month data published as yet (at January 2013). |
| Incomplete outcome data (attrition bias) post 6 months | High risk | Primary outcomes have been reported, it appears that data for all participants in the intention to treat sample have been reported. Authors note, however, they did not have verifiable data on whether patients were hospitalised at other facilities during the follow up period. |
| Selective reporting (reporting bias) | Unclear risk | Secondary outcomes listed in trial protocol not yet reported (at January 2013), including: Sense of community; Motivation for change; Social functioning; Hope; Self determination; Functional status; Treatment relationship. |
| Groups comparable at baseline? | Low risk | "The two groups did not differ on most variables at baseline", however, marital status was different between groups (intervention: 21% currently married; control 3% currently married). |
| No contamination between treatment groups? | Unclear risk | Not described. |
Solomon 1995.
| Methods | RCT Setting: Community mental health centre Philadelphia, USA. Funding: National Institute of Mental Health. Recruitment (clients): All clients on the roster of a community mental health centre (July 1990 ‐ July 1991) that met the criteria for intensive case management and who were at risk for hospitalisation were invited to participate. 128 eligible, 32 refused. Recruitment (consumer‐providers): Unclear. Training/support: Both teams received training required by all intensive case managers within the mental health system. This includes a continuing education program. Both teams also received additional training on consumer issues, team building, and other topics pertinent to the service model. Inclusion criteria: Diagnosed major mental illness, significant treatment history, Global Assessment Scale score of 40 or below (patients over 35 years old), or 60 or below (patients 35 years or younger). Exclusions: None stated. |
|
| Participants |
Clients: 96 participants (52% male). Mean age 41 (SD 14.4). Never married (76%). Less than high school education (48%). Income source: supplemental security income (62%), social security disability income (16%). Principal diagnosis: Schizophrenia (86%), major affective disorder (13%), or unspecified psychotic disorder (1%). Other characteristics: Homeless in past year (11%) or during lifetime (21%). Arrest in past year (18%) or during lifetime (42%). Living arrangement: community rehabilitation facilities (24%), boarding homes (18%), with parents (17%). Complies with medication most or all of the time (91%). History includes state hospitalisation (18%), lifetime hospitalizations (7%). Mean age at first hospitalisation 27 (SD 5.8); mean baseline BPRS score 31 (SD 9.5), and mean income 479 (323.6). Treatment receiving: Intensive case management. Description consumer‐providers: All consumer‐providers had a major mental health disorder as defined in the DSM‐III‐R; at least one prior psychiatric hospitalisation and a minimum of 14 days psychiatric hospitalisation, or at least 5 psychiatric emergency service contacts over a year, regular contact with community mental health services, psychosocial services, or other outpatient treatment for a primary diagnosis of the mental illness. The consumer‐provider team was older with a broader representation of educational experience, age and race than the control team. |
|
| Interventions |
Study aim: To determine if satisfaction with general mental health treatment would be greater for clients of the consumer‐provider case management teams compared with clients of non‐consumer case managers, and if individual characteristics of case managers may significantly affect satisfaction with treatment for clients of mental health services. Intervention aim: Designed to compare the outcomes of clients served by two teams of case managers. To determine whether a team of mental health service consumer‐providers delivered intensive case management services differently than a team of professional case managers. Role of consumer‐provider: Case management operated as a part of a consumer‐run advocacy and service organisation which had a consumer director, 4 case managers (3 consumer‐provider case managers and 1 non‐consumer case manager). The non‐consumer later left and was replaced with a consumer‐provider. In the 2nd year, a full‐time clinical director and part time psychiatrist were hired. Intervention: (n = 48) Consumer‐provider case management team. Team comprised 4 case managers that met 3 times a week. Each team member had their own clients. Case managers saw clients in their own environments and provided individualised social support for community living. Case management was based on the ACT model. Case managers routinely interacted with health professionals, community and social welfare staff, benefits administrators, families and housing providers to plan or monitor services. Control: (n = 48) Non‐consumer case management team. Team comprised 4 case managers that met biweekly and also met with another team of intensive case managers monthly. Also based on the ACT model. Fidelity: Not described. Consumer involvement outside of the intervention: None. Changes in trial protocol: None described. |
|
| Outcomes | Outcomes assessed at baseline and after one and two years follow up. Lehman's Quality of Life Interview (QOLI) Brief Psychiatric Rating Scale (BPRS) Client satisfaction: 16 items on a 4 point scale (very helpful, helpful, somewhat helpful, not at all helpful). Scores ranged from 1‐4, higher scores better Working Alliance Inventory (WAI): client‐assessed and case manager‐assessed Emergency service use Hospital admission Outpatient treatment services Rehabilitation services Service provision (time allocation and location of case management services) |
|
| Notes | Service provision and use of services (eg outpatient treatment services and rehabilitation services) were measured in units of time (one time unit is 15 minutes), reported values were converted and presented as number of hours in the final analysis. Power calculation: Not described. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...randomly assigned" Insufficient information to determine whether adequate sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Participants had to provide informed consent and were likely to be aware of purpose of study. |
| Blinding (performance bias and detection bias) All other outcomes | Unclear risk | "...researchers were not blinded to the intervention status of participants" |
| Incomplete outcome data (attrition bias) up to 6 months | Low risk | 90/96 participants followed up. Reasons for losses were provided however it is unclear whether losses were balanced across groups. Unlikely to be a source of bias. |
| Incomplete outcome data (attrition bias) post 6 months | Low risk | As above. |
| Selective reporting (reporting bias) | High risk | Outcome data presented as pooled results for entire sample rather than results for separate treatment groups. |
| Groups comparable at baseline? | Low risk | "There were no differences between the clients of the two teams on clinical characteristics, social indicators, social network, living arrangements, quality of life, and demographics, with the exception of gender...baseline variables found no significant differences by gender" |
| No contamination between treatment groups? | Low risk | Both teams operated in the same catchment area but were based at different sites. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bedell 1980 | Allocation to treatment groups not randomised |
| Bruxner 2010 | Study suspended due to recruitment problems (correspondence with J Robinson July 2012) |
| Campbell 2004 | Intervention not integrated within statutory mental health setting (Consumer‐operated services as an alternative to statutory mental health service) |
| Castelein 2008 | Intervention not integrated within statutory mental health setting (nurse and peer led self‐help group); Comparison group differed on more factors than consumer‐provider alone |
| Chatterjee 2011 | Lay health workers were not current or past consumers of mental health services (confirmed by communication with Chatterjee S, 2012) |
| Cook 2012a | Comparison group differed on more factors than consumer‐provider alone |
| Cook 2012b | (Identified from van Gestel 2012) Intervention not integrated within statutory mental health setting (peer‐led course) |
| Davidson 2004 | Intervention not integrated within statutory mental health setting (independent social support). Also, befriending only (confirmed by correspondence with author). |
| Dennis 2003 | Intervention not integrated within statutory mental health setting (maternal child health) |
| Dennis 2009 | Intervention not integrated within statutory mental health setting (immunisation clinic) |
| Draine 1995 | Intervention not integrated within statutory mental health setting (forensic) |
| Dumont 2002 | Intervention not integrated within statutory mental health setting (consumer‐run crisis hostel as an alternative to statutory mental health service) |
| Felton 1995 | Allocation to treatment groups was quasi‐randomised |
| Forchuk 2005 | Comparison group differed on more factors than consumer‐provider alone |
| Galanter 1988 | Intervention not integrated within statutory mental health setting (independent peer‐led self‐help group) |
| Greenfield 2008 | Comparison group differed on more factors than consumer‐provider alone |
| Hartley 2011 | Allocation to treatment groups was quasi‐randomised |
| Hunkeler 2000 | Intervention not integrated within statutory mental health setting (primary care) |
| Jonikas 2011 | Comparison group differed on more factors than consumer‐provider alone |
| Kaufmann 1995a | Intervention not specifically for mental health (employment) |
| Klein 1997 | Allocation to treatment groups was quasi‐randomised |
| Krebaum 1999a | Retrospective program evaluation, not prospective randomised trial (confirmed in correspondence with author, 12 July 2012) |
| Lafave 1996 | Comparison group differed on more factors than consumer‐provider alone |
| Landers 2011 | Allocation to treatment groups was not randomised |
| Lehman 1997 | Comparison group differed on more factors than consumer‐provider alone |
| Lehman 1999 | Intervention not specifically for mental health (homelessness) |
| Lehman 2002 | Intervention not specifically for mental health (employment support) |
| Liberman 1998 | Comparison group differed on more factors than consumer‐provider alone |
| Liviniemi 2001 | No comparison group |
| Ludman 2007 | Intervention not integrated within statutory mental health setting (peer support education as an alternative to statutory mental health service) |
| Macias 2006 | Intervention not specifically for mental health (employment support) |
| McCorkle 2008 | Allocation to treatment groups was quasi‐randomised |
| Powell 2001 | Intervention not integrated within statutory mental health setting (independent peer‐led self‐help group) |
| Quinlivan 1995 | Comparison group differed on more factors than consumer‐provider alone |
| Reynolds 2004 | Comparison group differed on more factors than consumer‐provider alone |
| Rowe 2007 | Intervention not integrated within statutory mental health setting (forensic) |
| Sacks 2008 | Participants not clients of a statutory mental health service (substance abuse) |
| Salyers 2010 | Comparison group differed on more factors than consumer‐provider alone |
| Schmidt 2006 | Allocation to treatment groups was quasi‐randomised |
| Seeman 2001 | Intervention not integrated within statutory mental health setting (perinatal) |
| Segal 2010 | Both intervention and comparison group involved consumer providers |
| Segal 2011 | Both intervention and comparison group involved consumer providers |
| Simon 2011 | Intervention not integrated within statutory mental health setting (research institute) |
| Stefancic 2007 | Intervention not specifically for mental health (housing) |
| Straughan 2006 | Intervention not integrated within statutory mental health setting (independent peer‐led recovery group) |
| Sytema 2007 | Comparison group differed on more factors than consumer‐provider alone |
| van Gestel 2012 | Intervention not integrated within statutory mental health setting (peer‐led course); wait‐list control group received no treatment at all (ie. not 'service as usual') |
| Young 2005 | Allocation to treatment groups was quasi‐randomised |
Characteristics of studies awaiting assessment [ordered by study ID]
Kroon 2011.
| Methods | Randomised controlled trial. |
| Participants | People with severe mental illness. |
| Interventions | A user‐run recovery group and short recovery courses, added to care as usual. |
| Outcomes | Empowerment, mental health confidence, connectedness, quality of life, depressive symptoms. |
| Notes | Need additional information; emailed authors (May 2012) and awaiting response (January 2013). |
Stone 1979.
| Methods | Controlled study (no further details). |
| Participants | Inpatients at Florida Mental Health Institute, aged between 18 and 54, with a minimum of three months' hospitalization or three different hospitals. |
| Interventions | Small group, peer management inpatient treatment |
| Outcomes | Rehospitalization incidence and duration, staff satisfaction. |
| Notes | Unable to obtain abstract for either reference. Southeastern Psychological Association (SEPA) was unable to provide additional information (January 2013). |
Characteristics of ongoing studies [ordered by study ID]
Chinman 2012.
| Trial name or title | PEers Enhancing Recovery (PEER) |
| Methods | Cluster RCT |
| Participants | Veterans with mental illness (US) |
| Interventions | Behavioral: Adding a Consumer Provider to Intensive Case Management Teams |
| Outcomes | Primary: Behaviour and Symptom Identification Scale (BASIS‐24) Secondary: Mental Health Recovery Measure (MHRM) Patient Activation Measure Recovery Assessment: Person in Recovery Version Illness Management and Recovery Scale: Client Self‐Rating Quality of Life Interview |
| Starting date | October 2008 |
| Contact information | Matthew Chinman (chinman@rand.org) |
| Notes | Authors advised results data soon to be published (Jan 2013) |
Tondora 2010.
| Trial name or title | Culturally responsive person‐centred care for psychosis. |
| Methods | Randomised controlled trial. |
| Participants | Self‐identified as African and/or Latino, over 18 receiving outpatient services following psychosis. N = 290. |
| Interventions | Standard care plus facilitation of person‐centred care (with peer mentor) compared to standard care, or standard care plus facilitation of person‐centred care with peer mentor and community inclusion activities. |
| Outcomes | Symptoms; clinical and functional status; quality of life; illness self‐management; satisfaction with services. |
| Starting date | January 2008 |
| Contact information | Rebecca Miller (rebecca.miller@yale.edu) |
| Notes | Funded by National Institute of Mental Health. Trial complete, data not yet published. Awaiting response from authors on use of unpublished data (January 2013). |
Differences between protocol and review
The protocol (Simpson 2003c) and review were prepared by different author teams. The initial protocol had planned to include randomised and quasi‐randomised controlled trials. The final review has been limited to randomised controlled trials.
Systematic data collection and presentation of adverse outcomes was not pre‐specified by the original authors in the protocol, however the current review authors have included adverse events as a primary outcome of this review.
When the original selection criteria were applied to potentially relevant studies, we identified a group of studies that compared two different types of mental health service interventions where one of the interventions involved a consumer‐provider and the alternate intervention did not. These trials are unable to provide information about the effect of a consumer‐provider as there are other variables that might explain differences in outcomes between the two different interventions. We have therefore excluded these studies from the review (please refer to studies listed as "comparison group differed on more factors than consumer‐provider alone" in the Characteristics of excluded studies).
Contributions of authors
VP: Screened search results, selected studies, extracted and entered quantitative data, conducted analysis and interpretation of results, drafted review text.
DL: Screened search results, selected studies, extracted and entered quantitative and qualitative data, checked analysis and interpretation of results, drafted review text, updated searches.
SH: Conducted qualitative data extraction and analysis, oversaw analysis and interpretation of results, contributed to draft review.
MP: Screened and selected studies, extracted data, drafted and edited review text, updated searches.
SEH: Contributed to mapping of outcomes, and interpretation of results.
RR: Screened and selected studies, extracted data.
LB: Extracted data, contributed to draft review.
The authors of the protocol for this review (Simpson 2003c) (Emma Simpson, Michael Barkham, Simon Gilbody and Allan House) were not involved in the review.
Sources of support
Internal sources
-
La Trobe University, Australia.
Office space and IT facilities for DL, VP, SH, MP, RR
External sources
-
National Health and Medical Research Council, Australia.
Salary support to RR, SEH
-
Department of Health, Victoria, Australia.
Salary support to MP, SH
Declarations of interest
Three authors (MP, SH, RR) are also editors of the Cochrane Consumers and Communication Review Group. They were not involved in decision‐making regarding publication of this review.
SEH is funded via a National Health and Medical Research Council training fellowship. Orygen Youth Health Research Centre receives funds from the Colonial Foundation.
New
References
References to studies included in this review
Bright 1999 {published data only}
- Bright JI, Baker KD, Neimeyer RA. Professional and paraprofessional group treatments for depression: a comparison of cognitive‐behavioral and mutual support interventions. Journal of Consulting and Clinical Psychology 1999;67(4):491‐501. [DOI] [PubMed] [Google Scholar]
Clarke 2000 {published data only}
- Clarke GN, Herinckx HA, Kinney RF, Paulson RI, Cutler DL, Lewis K, et al. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Mental Health Services Research 2000;2(3):155‐64. [DOI] [PubMed] [Google Scholar]
- Herinckx H, Kinney R, Clarke G, Paulson R. Assertive community treatment versus usual care in engaging and retaining clients with severe mental illness. Psychiatric Services 1997;48(10):1297‐306. [DOI] [PubMed] [Google Scholar]
- Paulson R, Clarke G, Herinckx H, Kinney R, Lewis K, Oxman E. First year outcomes from a randomised trial comparing consumer and non‐consumer assertive community treatment teams with usual care [conference abstract]. Schizophrenia 1996: Breaking down the Barriers 4th International Conference, Vancouver, BC, Canada October 6‐9 1996.
- Paulson R, Herinckx H, Demmler J, Clarke G, Cutler D, Birecree E. Comparing practice patterns of consumer and non‐consumer mental health service providers. Community Mental Health Journal 1999;35(3):251‐69. [DOI] [PubMed] [Google Scholar]
Craig 2004 {published data only}
- Craig T, Doherty I, Jamieson‐Craig R, Boocock A, Attafua G. The consumer‐employee as a member of a Mental Health Assertive Outreach Team. I. Clinical and social outcomes. Journal of Mental Health 2004;13(1):59‐69. [Google Scholar]
- Doherty I, Craig T, Attafua G, Boocock A, Jamieson‐Craig R. The consumer‐employee as a member of a Mental Health Assertive Outreach Team II Clinical and social outcomes. Journal of Mental Health 2004; Vol. 13, issue 1:71‐81.
Gordon 1979 {published data only}
- Edmunson ED, Bedell JR, Archer RP, Gordon RE. Integrating skill building and peer support in mental health treatment: the Early Intervention and Community Network Development projects. In: Jeger AM, Slotnick RS editor(s). Community Mental Health and Behavioral Ecology. New York: Plenum Press, 1982:127‐39. [Google Scholar]
- Edmunson ED, Bedell JR, Gordon RE. The Community Network Development Project: bridging the gap between professional aftercare and self‐help. In: Gartner A, Riesman F editor(s). The Self‐Help Revolution. New York: Human Sciences Press, 1984:195‐203. [Google Scholar]
- Gordon R, Edmunson E, Bedell J, Goldstein N. Peer mutual aid networks reduce rehospitalization of mental patients. Self‐Help Reporter (New York) 1979 (March‐April);3(2). [Google Scholar]
- Gordon R, Edmunson E, Bedell J, Goldstein N. Reducing rehospitalization of state mental patients: peer management and support. Journal of the Florida Medical Association 1979;66(9):927‐33. [PubMed] [Google Scholar]
Kaufmann 1995 {published data only}
- Kaufmann CL, Schulberg HC, Schooler NR. Chapter 14: Self‐help group participation among people with severe mental illness. Prevention in Human Services 1995;11(2):315‐31. [Google Scholar]
O'Donnell 1999 {published data only}
- O'Donnell M, Parker G, Proberts M, Matthews R, Fisher D, Johnson B, et al. A study of client‐focused case management and consumer advocacy: the Community and Consumer Service Project. Australian and New Zealand Journal of Psychiatry 1999;33(5):684‐93. [DOI] [PubMed] [Google Scholar]
- O'Donnell M, Proberts M, Parker G. Development of a consumer advocacy program. Australian and New Zealand Journal of Psychiatry 1998;32(6):873‐9. [DOI] [PubMed] [Google Scholar]
Rivera 2007 {published data only}
- Rivera J, Sullivan A, Valenti S. Adding consumer‐providers to intensive case management: does it improve outcome?. Psychiatric Services 2007;58(6):802‐9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Rogers 2007 {published data only}
- Johnsen MT, McDonel G, Herr E. Common ingredients as a fidelity measure. In: Clay SS editor(s). On Our Own, Together: Peer Programs for People with Mental Illness. Nashville (TN): Vanderbilt University Press, 2005:213‐38. [Google Scholar]
- Rogers ES, Teague GB, Lichenstein C, Campbell J, Lyass A, Chen R, et al. Effects of participation in consumer‐operated service programs on both personal and organizationally mediated empowerment: results of multisite study. Journal of Rehabilitation Research & Development 2007;47(6):785‐99. [DOI] [PubMed] [Google Scholar]
Sells 2006 {published data only}
- Jewell C, Davidson L, Rowe M. The paradox of engagement: how political, organizational, and evaluative demands can hinder innovation in community mental health services. Social Service Review 2006;80(1):4‐26. [DOI: 10.1086/498837] [DOI] [Google Scholar]
- Sells D, Black R, Davidson L, Rowe M. Beyond generic support: Incidence and impact of invalidation in peer services for clients with severe mental illness. Psychiatric Services 2008; Vol. 59, issue 11:1322‐7. [DOI: 10.1176/appi.ps.59.11.1322] [DOI] [PubMed]
- Sells D, Davidson L, Jewell C, Falzer P, Rowe M. The treatment relationship in peer‐based and regular case management for clients with severe mental illness. Psychiatric Services 2006; Vol. 57, issue 8:1179‐84. [DOI: 10.1176/appi.ps.57.8.1179] [DOI] [PubMed]
Sledge 2011 {published data only}
- Sledge WH, Lawless M, Sells D, Wieland M, O'Connell MJ, Davidson L. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatric Services 2011;62(5):541‐4. [DOI] [PubMed] [Google Scholar]
Solomon 1995 {published data only}
- Solomon P, Draine J. Consumer case management and attitudes concerning family relations among persons with mental illness. Psychiatric Quarterly 1995c; Vol. 66, issue 3:249‐61. [DOI] [PubMed]
- Solomon P, Draine J. Family perceptions of consumers as case managers. Community Mental Health Journal 1994;30(2):165‐76. [DOI] [PubMed] [Google Scholar]
- Solomon P, Draine J. One‐year outcomes of a randomized trial of consumer case management. Evaluation and Program Planning 1995;18(2):117‐27. [Google Scholar]
- Solomon P, Draine J. Perspectives concerning consumers as case managers. Community Mental Health Journal 1996;32(1):41‐7. [DOI] [PubMed] [Google Scholar]
- Solomon P, Draine J. Satisfaction with mental health treatment in a randomized trial of consumer case management. Journal of Nervous and Mental Disease 1994;182(3):179‐84. [DOI] [PubMed] [Google Scholar]
- Solomon P, Draine J. Service delivery differences between consumer and nonconsumer case managers in mental health. Research on Social Work Practice 1996;6(2):193‐207. [Google Scholar]
- Solomon P, Draine J. The efficacy of a consumer case management team: 2‐year outcomes of a randomized trial. Journal of Mental Health Administration 1995;22(2):135‐46. [DOI] [PubMed] [Google Scholar]
- Solomon P, Draine J, Delaney MA, Solomon P, Draine J, Delaney MA. The working alliance and consumer case management. Journal of Mental Health Administration 1995;22(2):126‐34. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bedell 1980 {published data only}
- Bedell JR, Archer RP. Peer managed token economies: evaluation and description. Journal of Clinical Psychology 1980;36(3):716‐22. [DOI] [PubMed] [Google Scholar]
Bruxner 2010 {published and unpublished data}
- Bruxner A. The development of a project designed to test the feasibility and effects of a peer support intervention in young people being discharged from a first episode psychosis treatment centre. Early Intervention in Psychiatry 2010;4:56. [Google Scholar]
- Robinson J, Bruxner A, Harrigan S, Bendall S, Killackey E, Tonin V, et al. Study protocol: the development of a pilot study employing a randomised controlled design to investigate the feasibility and effects of a peer support program following discharge from a specialist first‐episode psychosis treatment centre. BMC Psychiatry 2010;10(37):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J, Bruxner A, Harrigan S, Bendall S, Killackey E, Tonin V, et al. The development, design, and testing of a peer support intervention in youth being discharged from a first episode psychosis clinic. Australian and New Zealand Journal of Psychiatry 2010;44:A43. [Google Scholar]
Campbell 2004 {published data only}
- Campbell J. Consumer‐operated services program (COSP) multisite research initiative: overview and preliminary findings. http://www.power2u.org/downloads/COSPVAREPORT.pdf (accessed 28 Jan 2011) May 2004.
Castelein 2008 {published data only}
- Castelein S, Bruggeman R, Busschbach J, Gaag M, Stant A, Knegtering H, et al. The effectiveness of peer support groups in psychosis: a randomized controlled trial. Acta Psychiatrica Scandinavica 2008;118(1):64‐72. [DOI] [PubMed] [Google Scholar]
- Stant A, Castelein S, Bruggeman R, Busschbach J, Gaag M, Knegtering H, et al. Economic aspects of peer support groups for psychosis. Community Mental Health Journal 2011;47:99‐105. [DOI] [PubMed] [Google Scholar]
Chatterjee 2011 {published and unpublished data}
- Balaji M, Chatterjee S, Koschorke M, Rangaswamy T, Chavan A, Dabholkar H, et al. The development of a lay health worker delivered collaborative community based intervention for people with schizophrenia in India. BMC Health Services Research 2012;12(42). [DOI: 10.1186/1472-6963-12-42] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S, Leese M, Koschorke M, McCrone P, Naik S, John S, et al. Collaborative community based care for people and their families living with schizophrenia in India: protocol for a randomised controlled trial. Trials 2011;12(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G. A randomised trial comparing the clinical and cost effectiveness of usual, facility based care compared to an additional collaborative community care package for people and their families living with schizophrenia in India (ISRCTN 56877013). http://apps.who.int/trialsearch/trial.aspx?trialid=ISRCTN56877013 2009.
Cook 2012a {published data only}
- Cook JA, Steigman P, Pickett S, Diehl S, Fox A, Shipley P, et al. Randomized controlled trial of peer‐led recovery education using Building Recovery of Individual Dreams and Goals through Education and Support (BRIDGES). Schizophrenia Research 2012;136(1‐3):36‐42. [DOI] [PubMed] [Google Scholar]
Cook 2012b {published data only}
- Cook JA, Copeland ME, Jonikas JA, Hamilton MM, Razzano LA, Grey DD, et al. Results of a randomized controlled trial of mental illness self‐management using Wellness Recovery Action Planning. Schizophrenia Bulletin 2012;38(4):881‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davidson 2004 {published and unpublished data}
- Davidson L, Shahar G, Stayner DA, Chinman MJ, Rakfeldt J, Tebes JK. Supported socialization for people with psychiatric disabilities: Lessons from a randomized controlled trial. Journal of Community Psychology 2004; Vol. 32, issue 4:453‐77. [DOI: 10.1002/jcop.20013] [DOI]
- Shahar G, Davidson L. Depressive symptoms erode self‐esteem in severe mental illness: a three‐wave, cross‐lagged study. Journal of Consulting and Clinical Psychology 2003;71(5):890‐900. [DOI] [PubMed] [Google Scholar]
- Shahar G, Kidd S, Styron TH, Davidson L. Consumer support and satisfaction with mental health services in severe mental illness: the moderating role of morale. Journal of Social & Clinical Psychology 2006;25(9):945‐62. [Google Scholar]
Dennis 2003 {published data only}
- Dennis C. The effect of peer support on postpartum depression: a pilot randomized controlled trial. Canadian Journal of Psychiatry 2003;48(2):115‐24. [DOI] [PubMed] [Google Scholar]
Dennis 2009 {published data only}
- Dennis CL, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, et al. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ 2009;338:a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Draine 1995 {published data only}
- Draine JN. Case management for homeless mentally ill adult offenders: a re‐examination of random field trial data. Philadelphia, PA: University of Pennsylvania, 1995. [ProQuest AAI9615035] [Google Scholar]
- Solomon P, Draine J. One‐year outcomes of a randomized trial of case management with seriously mentally ill clients leaving jail. Evaluation Review 1995;19(3):256‐73. [Google Scholar]
- Solomon P, Draine J, Meyerson A. Jail recidivism and receipt of community mental health services. Hospital and Community Psychiatry 1994;45(8):793‐7. [DOI] [PubMed] [Google Scholar]
Dumont 2002 {published data only}
- Dumont J, Jones K. Findings from a consumer/survivor defined alternative to psychiatric hospitalization. Outlook 2002;Spring:4‐6. [Google Scholar]
Felton 1995 {published data only}
- Felton CJ, Stastny P, Shern DL, Blanch A, Donahue SA, Knight E, et al. Consumers as peer specialists on intensive case management teams ‐ impact on client outcomes. Psychiatric Services 1995;46(10):1037‐44. [DOI] [PubMed] [Google Scholar]
Forchuk 2005 {published data only}
- Forchuk C, Martin ML, Chan YL, Jensen E. Therapeutic relationships: from psychiatric hospital to community. Journal of Psychiatric and Mental Health Nursing 2005;12(5):556‐64. [DOI] [PubMed] [Google Scholar]
Galanter 1988 {published data only}
- Galanter M, Galanter M. Zealous self‐help groups as adjuncts to psychiatric treatment: a study of Recovery, Inc. American Journal of Psychiatry 1988;145(10):1248‐53. [DOI] [PubMed] [Google Scholar]
Greenfield 2008 {published data only}
- Arntzen B, Greenfield TK, Sundby E. Early experiences at Sacramento's consumer run crisis residential program. Journal of the California Alliance for the Mentally Ill 1995; Vol. 6, issue 3:35‐6.
- Greenfield TK, Stoneking BC, Humphreys K, Sundby E, Bond J. A randomized trial of a mental health consumer‐managed alternative to civil commitment for acute psychiatric crisis. American Journal of Community Psychology 2008; Vol. 42, issue 1‐2:135‐44. [DOI: 10.1007/s10464-008-9180-1] [DOI] [PMC free article] [PubMed]
Hartley 2011 {published data only}
- Hartley S, Haddock G. Self‐help therapy and recovery in psychosis: Methodological considerations and service user involvement in a partially randomised preference trial. Trials 2011;12(S1):A84. [Google Scholar]
Hunkeler 2000 {published data only}
- Hunkeler E, Meresman J, Hargreaves W, Fireman B, Berman W, Kirsch A, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Family Medicine 2000;9(8):700‐8. [DOI] [PubMed] [Google Scholar]
Jonikas 2011 {published data only}
- Cook JA, Copeland ME, Jonikas JA, Hamilton MM, Razzano LA, Grey DD, et al. Results of a randomized controlled trial of mental illness self‐management using Wellness Recovery Action Planning. Schizophrenia Bulletin 2012;136:36‐42. [DOI: 10.1093/schbul/sbr012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey DD, Cook JA, Hamilton MM, Jonikas JA. Randomized controlled trial of a peer‐led recovery intervention for mental illness self‐management. Journal of Mental Health Policy and Economics 2011;14:S9. [Google Scholar]
- Jonikas JA, Grey DD, Copeland ME, Razzano LA, Hamilton MM, et al. Improving propensity for patient self‐advocacy through Wellness Recovery Action Planning: results of a randomized controlled trial. Community Mental Health Journal 2011;Dec:ns. [DOI: 10.1007/s10597-011-9475-9] [DOI] [PubMed] [Google Scholar]
Kaufmann 1995a {published data only}
- Kaufmann CL. The self help employment center ‐ some outcomes from the first year. Psychosocial Rehabilitation Journal 1995;18(4):145‐62. [Google Scholar]
Klein 1997 {published data only}
- Klein AR. The significance of peer social support in intensive case management. Philadelphia, PA: University of Pennsylvania, 1997. [ProQuest AAI9637397] [Google Scholar]
- Klein AR, Cnaan RA, Whitecraft J. Significance of peer social support with dually diagnosed clients: findings from a pilot study. Research on Social Work Practice 1998;8:529‐51. [Google Scholar]
Krebaum 1999a {published and unpublished data}
- Krebaum SR. Mental health consumers as case management aides in the transition from hospital to community: outcome of consumers served. Dallas, TX: University of Texas Southwestern Medical Center, 1999. [Google Scholar]
Lafave 1996 {published data only}
Landers 2011 {published data only}
- Landers GM, Zhou M. An analysis of relationships among peer support, psychiatric hospitalization, and crisis stabilization. Community Mental Health Journal 2011;47:106‐12. [DOI] [PubMed] [Google Scholar]
Lehman 1997 {published data only}
- Lehman AF, Dixon LB, DeForge B, Kernan E. Assertive community treatment for homeless persons with schizophrenia and other chronic mental disorders [conference abstract]. Schizophrenia Research (The Vth International Congress on Schizophrenia Research, Wormsprings, VA USA, 6 ‐12 April, 1995). 1995; Vol. 1, 2:128.
- Lehman AF, Dixon LB, Kernan E, DeForge BR, Postrado LT. A randomized trial of assertive community treatment for homeless persons with severe mental illness. Archives of General Psychiatry 1997; Vol. 54, issue 11:1038‐43. [DOI] [PubMed]
Lehman 1999 {published data only}
Lehman 2002 {published data only}
- Lehman AF, Goldberg R, Dixon L B, McNary S, Postrado L, Hackman A, et al. Improving employment outcomes for persons with severe mental illnesses. Archives of General Psychiatry 2002;59(2):165‐72. [DOI] [PubMed] [Google Scholar]
Liberman 1998 {published data only}
Liviniemi 2001 {published data only}
- Liviniemi L, Niemelä N. Elements of community care in mental health work: "Vertaansa Vailla" project [Finnish] [Yhteisöhoidon elementtejä mielenterveystyössä: Esimerkkinä Vertaansa Vailla ‐ projekti]. Sairaanhoitaja ‐ Sjuksköterskan 2001;74(3):11‐12. [Google Scholar]
Ludman 2007 {published data only}
- Ludman E, Simon G, Grothaus L, Luce C, Markley D, Schaefer J. A pilot study of telephone care management and structured disease self‐management groups for chronic depression. Psychiatric Services 2007;58(8):1065‐72. [DOI] [PubMed] [Google Scholar]
Macias 2006 {published data only}
- Macias C, Rodican C, Hargreaves W, Jones D, Barreira P, Wang Q. Supported employment outcomes of a randomized controlled trial of ACT and clubhouse models. Psychiatric Services 2006;57(10):1406‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCorkle 2008 {published data only}
- McCorkle B, Rogers E, Dunn E, Lyass A, Wan Y. Increasing social support for individuals with serious mental illness: evaluating the compeer model of intentional friendship. Community Mental Health Journal 2008;44(5):359‐66. [DOI] [PubMed] [Google Scholar]
Powell 2001 {published data only}
- Powell TJ, Yeaton W, Hill EM, Silk KR. Predictors of psychosocial outcomes for patients with mood disorders: the effects of self‐help group participation. Psychiatric Rehabilitation Journal 2001;25(1):3‐11. [DOI] [PubMed] [Google Scholar]
Quinlivan 1995 {published data only}
Reynolds 2004 {published data only}
- Reynolds W, Lauder W, Sharkey S, Maciver S, Veitch T, Cameron D, et al. The effects of a transitional discharge model for psychiatric patients. Journal of Psychiatric & Mental Health Nursing 2004; Vol. 11, issue 1:82‐8. [DOI] [PubMed]
- Sharkey S, Maciver S, Cameron D, Reynolds W, Lauder W, Veitch T. An exploration of factors affecting the implementation of a randomized controlled trial of a transitional discharge model for people with a serious mental illness. Journal of Psychiatric and Mental Health Nursing 2005;12(1):51‐6. [DOI] [PubMed] [Google Scholar]
Rowe 2007 {published data only}
- Rowe M, Bellamy C, Baranoski M, Wieland M, O'Connell M, Benedict P, et al. A peer‐support, group intervention to reduce substance use and criminality among persons with severe mental illness. Psychiatric Services 2007;58(7):955‐61. [DOI] [PubMed] [Google Scholar]
Sacks 2008 {published data only}
- Sacks S, McKendrick K, Sacks JY, Banks S, Harle M. Enhanced outpatient treatment for co‐occurring disorders: main outcomes. Journal of Substance Abuse Treatment 2008;34(1):48‐60. [DOI] [PubMed] [Google Scholar]
Salyers 2010 {published data only}
- Salyers MP, McGuire AB, Rollins AL, Bond GR, Mueser KT, Macy VR. Integrating assertive community treatment and illness management and recovery for consumers with severe mental illness. Community Mental Health Journal 2010;46(4):319‐29. [DOI] [PubMed] [Google Scholar]
Schmidt 2006 {published data only}
- Schmidt LT. Comparison of service outcomes of case management teams with and without a consumer provider. Newark, NJ: University of Medicine and Dentistry of New Jersey, 2005. [ProQuest AAT 3181928] [Google Scholar]
- Schmidt LT, Gill KJ, Pratt CW, Solomon P. Comparison of service outcomes of case management teams with and without a consumer provider. American Journal of Psychiatric Rehabilitation 2008;11:310‐29. [Google Scholar]
Seeman 2001 {published data only}
- Seeman MV. Group oriented interpersonal therapy reduced postpartum depression in women at risk. Evidence‐Based Mental Health 2001;4(4):118. [Google Scholar]
Segal 2010 {published and unpublished data}
- Segal SP, Silverman CJ, Temkin TL. Self‐help and community mental health agency outcomes: a recovery‐focused randomized controlled trial. Psychiatric Services 2010;61(9):905‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Segal 2011 {published and unpublished data}
- Segal SP, Silverman CJ, Temkin TL. Outcomes from consumer‐operated and community mental health services: a randomized controlled trial. Psychiatric Services 2011;62(8):915‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2011 {published data only}
- Simon GE, Cutsogeorge D, Ludman EJ, Operskalski B, Goodale LC, Savarino J, et al. An online recovery plan program: can peer coaching increase participation?. Psychiatric Services 2011;62(6):666‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stefancic 2007 {published data only}
- Stefancic A, Tsemberis S. Housing first for long‐term shelter dwellers with psychiatric disabilities in a suburban county: a four‐year study of housing access and retention. Journal of Primary Prevention 2007;28(3‐4):265‐79. [DOI] [PubMed] [Google Scholar]
Straughan 2006 {published data only}
- Straughan H, Buckenham M. In‐Sight: an evaluation of user‐led, recovery‐based, holistic group training for bipolar disorder. Journal of Public Mental Health 2006;5(3):29‐43. [Google Scholar]
Sytema 2007 {published data only}
van Gestel 2012 {published and unpublished data}
- ISRCTN47331661. Recovery ... you do that yourself: a randomised controlled trial for assessing the effects of a consumer‐run course on the recovery of persons with serious mental illnesses. http://www.controlled‐trials.com/isrctn/pf/47331661 (accessed 28 Jan 2011).
- Gestel‐Timmermans H, Brouwers EPM, Assen MALM, Nieuwenhuizen C. Effects of a peer‐run course on recovery from serious mental illness: a randomized controlled trial. Psychiatric Services 2012;63(1):54‐60. [DOI] [PubMed] [Google Scholar]
- Gestel‐Timmermans J, Brouwers E, Assen M, Nieuwenhuizen C. Effects and feasibility of a peer‐run course on the recovery of people with major psychiatric problems: a randomised controlled trial and feasibility study. Psychiatrische Praxis 2011;38. [DOI: 10.1055/s-0031-1277755] [DOI] [Google Scholar]
- Gestel‐Timmermans JAWM. Recovery is Up to You: Evaluation of a Peer‐run Course [PhD thesis]. Tranzo, The Netherlands: Tilburg University, 2011. [Google Scholar]
- Gestel‐Timmermans JAWM, Brouwers EPM, Nieuwenhuizen C. Recovery Is Up To You, a peer‐run course. Psychiatric Services 2010;61(9):944‐5. [DOI] [PubMed] [Google Scholar]
Young 2005 {published data only}
- Young AS, Chinman M, Forquer SL, Knight EL, Vogel H, Miller A, et al. Use of a consumer‐led intervention to improve provider competencies. Psychiatric Services 2005;56(8):967‐75. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Kroon 2011 {published data only}
- Kroon H, Boevink W. Effectiveness of recovery programs. Psychiatrische Praxis 2011;38. [DOI: 10.1055/s-0031-1277754] [DOI] [Google Scholar]
Stone 1979 {unpublished data only}
- Donoghue B, Stone A, Rust A, Cone W. Peer management inpatient treatment of chronic psychiatric patients: a preliminary report of a controlled study [unpublished paper]. Florida Mental Health Institute, Tampa 1979.
- Stone A, Donoghue B, Rust A, Cone W. Peer management in patient treatment of chronic psychiatric patients: controlled study with follow‐up. [to be presented at SEPA, New Orleans] 1979.
References to ongoing studies
Chinman 2012 {published and unpublished data}
- Chinman M. The impact of adding Consumer Providers to intensive case management teams. Psychiatric Services [submitted]. [DOI] [PubMed] [Google Scholar]
- Chinman M, Lucksted A, Gresen R, Davis M, Losonczy M, Sussner B, et al. Early experiences of employing consumer‐providers in the VA. Psychiatric Services 2008;59(11). [DOI: 10.1176/appi.ps.59.11.1315] [DOI] [PubMed] [Google Scholar]
- Chinman M, Shoai R, Cohen A. Using organizational change strategies to guide peer support technician implementation in the Veterans Administration. Psychiatric Rehabilitation Journal 2009;33(4 Special Issue):269‐77. [DOI: 10.2975/33.4.2010.269-277] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs. Promoting recovery using mental health consumer providers [PEers Enhancing Recovery (PEER) ‐ NCT00781079]. ClinicalTrials.gov [www.clinicaltrials.gov] 2010.
Tondora 2010 {published data only}
- Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illness: a review of evidence and experience. World Psychiatry 2012;11:123‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tondora J, O'Connell M, Miller R, Bellamy C, Andres‐Hyman R. A clinical trial of peer‐based culturally responsive person‐centered care for psychosis for African Americans and Latinos. Clinical Trials 2010;7(4):368‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Barrett‐Lennard 1962
- Barrett‐Lennard GT. Dimensions of therapist response as causal factors in therapeutic change. Psychological Monographs 1962; Vol. 76: 43.
Beck 1979
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guilford Press, 1979. [Google Scholar]
Becker 1993
- Becker M, Diamond R, Sainfort F. A new patient focused index for measuring quality of life in persons with severe and persistent mental illness. Quality of Life Research 1993;2(4):239‐51. [DOI] [PubMed] [Google Scholar]
Brown 2010
- Brown LD, Wituk S, Meissen G. Consumer‐run drop‐in centers: current state and future directions. In: Brown LD, Wituk S editor(s). Mental Health Self‐Help: Consumer and Family Initiatives. New York: Springer, 2010:155‐67. [Google Scholar]
Campbell 2008a
- Campbell P. Service user involvement. In: Stickley T, Basset T editor(s). Learning About Mental Health Practice. Chichester: John Wiley & Sons, 2008:291‐309. [Google Scholar]
Campbell 2008b
- Campbell J. Key ingredients of peer programs identified. http://www.power2u.org/downloads/COSP‐CommonIngredients.pdf May 2008 (accessed 14 Feb 2013).
Chamberlain 1993
- Chamberlain A. Working towards user‐led services through a mental health forum. Community Health Action 1993;8(Spring):6‐8. [Google Scholar]
Chinman 2001
- Chinman MJ, Weingarten R, Stayner D, Davidson L. Chronicity reconsidered: improving person‐environment fit through a consumer‐run service. Community Mental Health Journal 2001;37(3):215‐29. [DOI] [PubMed] [Google Scholar]
Chinman 2010
- Chinman M, Shoai R, Cohen A. Using organizational change strategies to guide peer support technician implementation in the Veterans Administration. Psychiatric Rehabilitation Journal 2010;33(4):269‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Church 1989
- Church K, Reville D. User involvement in the mental health field in Canada. Canada's Mental Health 1989;37(2):22‐5. [PubMed] [Google Scholar]
CONSORT 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cook 1995
- Cook JA, Jonikas JA, Razzano L. A randomized evaluation of consumer versus nonconsumer training of state mental health service providers. Community Mental Health Journal 1995;31(3):229‐38. [DOI] [PubMed] [Google Scholar]
Cook 2011
- Cook JA. Peer‐delivered wellness recovery services: from evidence to widespread implementation. Psychiatric Rehabilitation Journal 2011;35(2):87‐9. [DOI] [PubMed] [Google Scholar]
Coulter 2011
- Coulter A. Engaging Patients in Healthcare. Maidenhead, UK: Open University Press, 2011. [Google Scholar]
Cozza 1997
- Cozza M, Amara M, Butera N, Infantino G, Monti A M, Provenzano R. [The patient and family satisfaction with the department of mental health in Rome]. Epidemiologia e Psichiatria Sociale 1997;6(3):173‐83. [DOI] [PubMed] [Google Scholar]
Crawford 2002
- Crawford MJ, Rutter D, Manley C, Weaver T, Bhui K, Fulop N, et al. Systematic review of involving patients in the planning and development of health care. BMJ 2002;325:1263‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crawford 2003
- Crawford MJ, Aldridge T, Bhui K, Rutter D, Manley C, Weaver T, et al. User involvement in the planning and delivery of mental health services: a cross‐sectional survey of service users and providers. Acta Psychiatrica Scandinavica 2003;107(6):410‐4. [DOI] [PubMed] [Google Scholar]
Dale 2008
- Dale J, Caramlau IO, Lindenmeyer A, Williams SM. Peer support telephone calls for improving health. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD006903.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davidson 2012
- Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry 2012;11:123‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Department 1999
- Department of Health. Patient and public involvement in the new NHS. http://www.doh.gov.uk/pub/docs/doh/ppinvolvement.pdf. London: Department of Health, 1999 (accessed Nov 2003).
Department 2001
- Department of Health. Involving patients and the public in healthcare: a discussion document. http://www.doh.gov.uk/pdfs/involvingpatients.pdf. Department of Health, 2001 (accessed Nov 2003).
Derogardis 1977
- Derogardis LR. SCL‐90 manual R (revised) version. Baltimore: Johns Hopkins University School of Medicine, 1977. [Google Scholar]
Derogatis 1974
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a measure of primary symptom dimensions. Modern Problems of Pharmacopsychiatry 1974;7:79‐110. [DOI] [PubMed] [Google Scholar]
Derogatis 1983
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine 1983;13(3):595‐605. [PubMed] [Google Scholar]
Doughty 2011
- Doughty C, Tse S. Can consumer‐led mental health services be equally effective? An integrative review of CLMH services in high‐income countries. Community Mental Health Journal 2011;47:252‐66. [DOI] [PubMed] [Google Scholar]
Dow 1995
- Dow MG, Ward JC. Assessment of consumer satisfaction: current practices and the development of the Behavioral Healthcare Rating of Satisfaction scale. Washington, DC, 1995. [Google Scholar]
Everett 1998
- Everett B. Participation or exploitation? Consumers and psychiatric survivors as partners in planning mental health services. International Journal of Mental Health 1998;27(1):80‐97. [Google Scholar]
Fisk 2000
- Fisk D, Rowe M, Brooks R, Gildersleeve D. Integrating consumer staff members into a homeless outreach project: critical issues and strategies. Psychiatric Rehabilitation Journal 2000;23(3):244‐52. [Google Scholar]
Geller 1998
- Geller JL, Brown J‐M, Fisher WH, Anonymous, Manning TD. A national survey of 'consumer empowerment' at the state level. Psychiatric Services 1998;49(4):498‐503. [DOI] [PubMed] [Google Scholar]
Graley 1994
- Mental Health Task Force User Group, Graley R, Nettle M, Wallcraft J eds. Building on experience: a training pack for mental health service users working as trainers, speakers and workshop facilitators. Heywood: Department of Health, 1994. [Google Scholar]
Greenfield 1989
- Greenfield TK, Attkisson CC. Progress toward a multifactorial service satisfaction scale for evaluating primary care and mental health services. Evaluation and Program Planning 1989;12:271–8. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, (March 2011). [Google Scholar]
Hoult 1983
- Hoult J, Reynolds I, Charbonneau‐Powis M, Weekes P, Briggs J. Psychiatric hospital versus community treatment: the results of a randomized trial. Australian and New Zealand Journal of Psychiatry 1983;17:160‐7. [DOI] [PubMed] [Google Scholar]
Hovarth 1989
- Hovarth A, Greenberg L. Development and validation of the working alliance inventory. Journal of Counseling Psychology 1989;36:223‐33. [Google Scholar]
Kaufmann 1993
- Kaufmann CL, Ward‐Colasante C, Farmer J. Development and evaluation of drop‐in centers operated by mental health consumers. Hospital & Community Psychiatry 1993;44(7):675‐8. [DOI] [PubMed] [Google Scholar]
Larsen 1979
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Evaluation and Program Planning 1979;2(3):197‐207. [DOI] [PubMed] [Google Scholar]
Lecomte 1999
- Lecomte T, Wilde JB, Wallace CJ. Mental health consumers as peer interviewers. Psychiatric Services 1999;50(5):693‐5. [DOI] [PubMed] [Google Scholar]
Lehman 1988
- Lehman A. A quality of life interview for the chronically mentally ill. Evaluation and Program Planning 1988;111:51–62. [Google Scholar]
Lehman 1994
- Lehman A, Kernan E, Postrado L. Toolkit for Evaluating. Cambridge, MA: The Evaluation Centre, 1994. [Google Scholar]
Lewin 2010
- Lewin S, Munabi‐Babigumira S, Glenton C, Daniels K, Bosch‐Capblanch X, Wyk BE, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD004015.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lyons 1996
- Lyons JS, Cook JA, Ruth AR, Karver M, Slagg NB. Service delivery using consumer staff in a mobile crisis assessment program. Community Mental Health Journal 1996;32(1):33‐40. [DOI] [PubMed] [Google Scholar]
Mowbray 1988
- Mowbray CT, Chamberlain P, Jennings M, Reed C. Consumer‐run mental health services: results from five demonstration projects. Community Mental Health Journal 1988;24(2):151‐6. [DOI] [PubMed] [Google Scholar]
Mowbray 1996
- Mowbray CT, Moxley DP, Thrasher S, Bybee D, McCrohan N, Harris S, et al. Consumers as community support providers: issues created by role innovation. Community Mental Health Journal 1996;32(1):47‐67. [DOI] [PubMed] [Google Scholar]
Mowbray 1998
- Mowbray CT, Moxley DP, Collins M. Consumers as mental health providers: first person accounts of benefits and limitations. The Journal of Behavioural Health Sciences and Research 1998;25:397‐411. [DOI] [PubMed] [Google Scholar]
Nilsen 2006
- Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD004563.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Donnell 1998
- O'Donnell M, Proberts M, Parker G. Development of a consumer advocacy program. Australian and New Zealand Journal of Psychiatry 1998;32(6):873‐9. [DOI] [PubMed] [Google Scholar]
Overall 1962
- Overall JE, Gorham DR. The Brief Psychiatric Rating. Psychological Reports 1962;19:799‐812. [Google Scholar]
Perkins 1997
- Perkins R, Buckfield R, Choy D. Access to employment: a supported employment project to enable mental health service users to obtain jobs within mental health teams. Journal of Mental Health 1997;6(3):307‐18. [Google Scholar]
Pfeiffer 2011
- Pfeiffer PN, Heisler M, Piette JD, Rogers MAM, Valenstein M. Efficacy of peer support interventions for depression: a meta‐analysis. General Hospital Psychiatry 2011;33:29‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Phelan 1995
- Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T, et al. The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. British Journal of Psychiatry 1995;167(5):589‐95. [DOI] [PubMed] [Google Scholar]
Power 1988
- Power MJ, Champion LA, Aris SJ. The development of a measure of social support: the Significant Others (SOS) Scale. British Journal of Clinical Psychology 1988;27 (Pt 4):349‐58. [DOI] [PubMed] [Google Scholar]
President 2003
- The President's New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America: Final Report. July 2003; Vol. http://govinfo.library.unt.edu/mentalhealthcommission/index.htm (accessed 25 Jan 2013).
Ralph 1992
- Ralph R, Clary B. The Working Alliance Inventory: measuring the relationship between client and case manager. Paper presented at the National Conference on State Mental Health Agency Services Research, Baltimore, MD. October 1992.
Rehm 1985
- Rehm LP, O'Hara MW. Item characteristics of the Hamilton Rating Scale for Depression. Journal of Psychiatric Research 1985;19(1):31‐41. [DOI] [PubMed] [Google Scholar]
Repper 2011
- Repper J, Carter T. A review of the literature on peer support in mental health services. Journal of Mental Health August 2011;20(4):392‐411. [DOI] [PubMed] [Google Scholar]
Rogers 1997
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer‐constructed scale to measure empowerment among users of mental health services. Psychiatric Services 1997;48(8):1042‐7. [DOI] [PubMed] [Google Scholar]
Rosen 1989
- Rosen A, Hadzi‐Pavlovic D, Parker G. The life skills profile: a measure assessing function and disability in schizophrenia. Schizophrenia Bulletin 1989;15(2):325‐37. [DOI] [PubMed] [Google Scholar]
Salzer 2010
- Salzer MS. Certified peer specialists in the United States behavioural health system: an emerging workforce. In: Brown LD, Wituk S editor(s). Mental Health Self‐Help: Consumer and Family Initiatives. New York: Springer, 2010:169‐91. [Google Scholar]
Segal 1995
- Segal SP, Silverman C, Temkin T. Measuring empowerment in client‐run self‐help agencies. Community Mental Health Journal 1995;31(3):215‐27. [DOI] [PubMed] [Google Scholar]
Sherman 1991
- Sherman PS, Porter R. Mental health consumers as case management aides. Hospital & Community Psychiatry 1991;42(5):494‐8. [DOI] [PubMed] [Google Scholar]
Simpson 2002
- Simpson EL, House AO. Involving users in the delivery and evaluation of mental health services: systematic review. BMJ 2002; Vol. 325, issue 7375:1265. [DOI] [PMC free article] [PubMed]
Simpson 2003a
- Simpson EL, Barkham M, Gilbody S, House A. Involving service users as researchers for the evaluation of adult statutory mental health services. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD004810] [DOI] [Google Scholar]
Simpson 2003b
- Simpson EL, Barkham M, Gilbody S, House A. Involving service users as trainers for professionals working in adult statutory mental health services. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD004813] [DOI] [Google Scholar]
Solomon 1998
- Solomon P, Draine J. Consumers as providers in psychiatric rehabilitation. New Directions for Mental Health Services 1998;79(Fall):65‐77. [DOI] [PubMed] [Google Scholar]
SPIRIT 2013
- Chan A‐W, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stein 1980
- Stein LI, Test MA. Alternative to mental hospital treatment: a conceptual model treatment program and clinical evaluation. Archives of General Psychiatry 1980;37:392‐7. [DOI] [PubMed] [Google Scholar]
Van Ginneken 2011
- Ginneken N, Tharyan P, Lewin S, Rao GN, Romeo R, Patel V. Non‐specialist health worker interventions for mental health care in low‐ and middle‐ income countries. Cochrane Database of Systematic Reviews 2011, Issue 5. [DOI: 10.1002/14651858.CD009149] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Vugt 2012
- Vugt MD, Kroon H, Delespaul PAEG, Mulder CL. Consumer‐providers in assertive community treatment programs: associations with client outcomes. Psychiatric Services 2012;63(5):477‐81. [DOI] [PubMed] [Google Scholar]
Velligan 2005
- Velligan D, Prihoda T, Dennehy E, Biggs M, Shores‐Wilson K, Crismon ML, et al. Brief psychiatric rating scale expanded version: how do new items affect factor structure?. Psychiatry Research 2005;135(3):217‐28. [DOI] [PubMed] [Google Scholar]
ViaHope 2013
- Via Hope: Texas Mental Health Resource. http://www.viahope.org/ (accessed 14 Feb 2013).
Wright‐Berryman 2011
- Wright‐Berryman JL, McGuire AB, Salyers MP. A review of consumer‐provided services on assertive community treatment and intensive case management teams: implications for future research and practice. Journal of the American Psychiatric Nurses Association 2011;17(1):37‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Simpson 2003c
- Simpson EL, Barkham M, Gilbody S, House A. Involving service users as service providers for adult statutory mental health services. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD004807] [DOI] [Google Scholar]


