Abstract
A 79-year-old woman was evaluated for weakness, dysphagia, and elevated levels of creatinine kinase. Her medical history included stage IIIB cervical cancer eight years previously, which improved after undergoing radiotherapy. Two years later, cancer recurred in the right hilar and mediastinal lymph nodes, and the patient was successfully treated with chemotherapy. Physical examinations showed Gottron's sign, the V sign, the Holster sign, and nailfold erythema. Computed tomography revealed left supraclavicular lymphadenopathy, compatible with cancer recurrence. Anti-nuclear matrix protein 2 (NXP2) antibody was found in her sera and a diagnosis of cancer-associated dermatomyositis was thus made. This case suggests that cancer progression over a period of years may have triggered the onset of autoimmunity against NXP2.
Keywords: anti-nuclear matrix protein 2 antibody, dermatomyositis, cervical cancer, cancer-associated myositis
Introduction
Several myositis-specific antibodies are reportedly associated with cancer-associated myositis (CAM) (1). Anti-nuclear matrix protein 2 (NXP2) antibody was first detected in childhood myositis as anti-MJ antibodies (2), and later NXP2 was identified as the corresponding antigen (3). In adult dermatomyositis (DM) patients, anti-NXP2 antibody has been associated with an increased cancer risk (4). More recently, an age-standardized incidence ratio for this antibody was reported to be 22 (5). We encountered a rare case of anti-nuclear matrix protein 2-positive dermatomyositis that developed with a recurrence of cervical cancer that had been diagnosed 8 years earlier after a 6-year period of stable disease.
Case Report
A 79-year-old Japanese woman with a 4-day history of pain in both upper arms was admitted to our hospital with suspected rhabdomyolysis (Day 0). Stage IIIB cervical cancer had been diagnosed 8 years earlier. The cancer had been deemed to be inoperable, but it improved with radiotherapy. Two years later, the cancer recurred in the right hilar and mediastinal lymph nodes, thus leading to a progression to stage IV disease, and the patient was successfully treated with chemotherapy (paclitaxel and carboplatin). Her cancer status had remained as stable disease for 6 years while the patient was followed at the previous hospital. In addition to elevated levels of transaminases and lactate dehydrogenase, her creatinine kinase (CK) level was elevated at 4,540 U/L (normal range, 59-248 U/L). Therapy with fluid replacement was immediately started to prevent heme pigment-induced acute kidney injury. After this therapy, her CK levels seemed to decrease, but muscle weakness progressed (Fig. 1). Dysphagia appeared from Day 8 and the patient deteriorated thereafter. Anti-transcriptional intermediary factor 1 (TIF1)-γ, anti-aminoacyl transfer RNA synthetase, anti-Mi-2, and anti-melanoma differentiation-associated gene 5, anti-nuclear antibodies were absent from her sera. Computed tomography (CT) of the whole body showed left supraclavicular lymphadenopathy (Fig. 2C), and recurrent cervical cancer was suspected. On a retrospective review of the images (Fig. 2A-C), left supraclavicular lymphadenopathy, which had not been visible in a CT scan 13 months earlier (Fig. 2A), was already visible in the CT scan 2 months earlier (Fig. 2B). This change over time was also consistent with cancer recurrence. Magnetic resonance imaging (MRI) of the pelvic region did not show any findings suggestive of cervical cancer recurrence, although a gynecological examination could not be done. When the patient was referred to our department (Day 19), she had difficulty with the expectoration of sputum and muscle weakness, predominantly involving her upper limbs and proximal muscles. Physical examination revealed erythematous lesions on the back of the right hand, compatible with Gottron's sign (Fig. 3A), the V sign (Fig. 3B), the Holster sign on both thighs, and the nailfold erythema. There was prominent edema in both upper arms. Manual muscle testing showed proximal weakness bilaterally; deltoid muscles of 2 (with 5 as the maximum); cervical flexor muscles of 2; and hamstrings of 4. An electromyogram of the left biceps brachii muscle showed fibrillation potentials at rest and the early recruitment of motor unit potentials, which are characteristic features of a myogenic disorder. The T2-weighted image on MRI of the right arm showed high-intensity lesions compatible with muscle inflammation and subcutaneous edema (Fig. 4). The patient was diagnosed with dermatomyositis according to the previous criteria (6,7). We also suspected that cervical cancer recurrence was associated with the development of dermatomyositis, i.e., CAM. Since negative results were obtained for myositis-specific antibodies, serological tests using immunoprecipitation and Western blotting assays (5) for anti-NXP2 and anti-small ubiquitin-like modifier activating enzyme (SAE) antibodies were ordered, and the former were positive. Methylprednisolone pulse therapy, followed by high-dose prednisolone, was immediately started, but she further deteriorated and became dependent on tube feeding on Day 21. Because of her general condition, we refrained from performing further examinations such as biopsies of the lymph node or the muscle. On day 25, we added azathioprine to glucocorticoid therapy, which was reported to be effective as a steroid-sparing agent in polymyositis (8). While her skin lesions disappeared within a few weeks, the dysphagia and muscle weakness remained unchanged. On Day 33, the patient's level of squamous cell carcinoma-associated antigen (SCC) was 1.3 ng/mL (normal range, ≤1.5), but it later increased to >3 (Fig. 1). The CK levels decreased further and normalized on Day 40, but her condition never improved. We did not necessarily consider this discrepancy between muscle enzymes and weakness to be a favorable sign for improvement, because we believed that treatment for cancer would be fundamental for CAM. On Day 45, intravenous immunoglobulin therapy was started for dysphagia but proved to be ineffective. On Day 59, we consulted with radiation oncologists about the indications for radiation therapy. At that time, a CT scan showed the left supraclavicular lymph node to have become further enlarged (Fig. 2D). Radiotherapy to the left supraclavicular lymph node was started on Day 61. On Day 70, she was able to start eating gradually. She was transferred to a rehabilitation hospital, and then was discharged on Day 120. Computed tomography (Fig. 2E) on Day 160 showed a decrease in the size of the left supraclavicular lymph node with a decreasing tendency in levels of SCC (Fig. 1). At the last visit (Day 188), the patient was now able to live on her own while taking daily 9 mg of prednisolone with azathioprine.
Figure 1.
The clinical course of the present case. mPSL: methyl-prednisolone, CK: creatinine kinase, SCC: squamous cell carcinoma-associated antigen, IVIG: intravenous immunoglobulin therapy
Figure 2.
Computed tomography performed at 13 and 2 months previously (A and B, respectively) and on this admission (C), before (D), and after radiation therapy (E). White arrows show the left supraclavicular lymph node.
Figure 3.
Cutaneous findings compatible with Gottron's sign and V sign.
Figure 4.
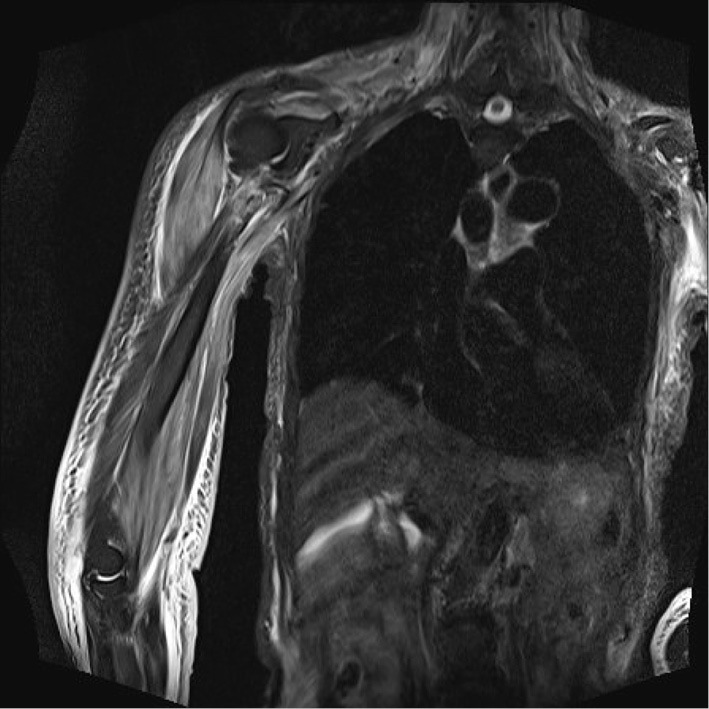
The T2-weighted image on magnetic resonance imaging (MRI) of the right arm.
Discussion
Anti-NXP2 antibodies have been reported to be found in 11-24% of adult dermatomyositis cases (4,9) and they have also been reported to be associated with myalgia (4,9), edema (4,9), proximal and peripheral muscle weakness (4,5), calcification (4,9), and dysphagia (4,9). Importantly, the incidence of malignancy has been reported to be 9% to 25% in large cohort studies (4,5,9). In our case, in addition to malignancy, the patient presented with marked myalgia, edema, and refractory dysphagia, which is relatively typical of anti-NXP2 positive cases. In our case, Gottron's sign contributed to a diagnosis of dermatomyositis, but interestingly, the frequency of Gottron's sign or dermatomyositis-specific skin manifestations is not necessarily high in anti-NXP2 positive cases (4,5), which means that some cases may present with ‘dermatomyositis sine dermatitis’ (5).
In a retrospective analysis of CAM, anti-TIF1γ positive cases were associated with more advanced cancer based on the cancer stage compared to negative cases (10). Another Japanese study described that anti-NXP2 antibody was also associated with malignancy, with all 4 cases of CAM showing advanced cancer (11). In the aforementioned analysis for CAM, two of three cases with anti-NXP2 antibody-positive dermatomyositis had Stage IV cancers (10). Furthermore, both our case and the other unpublished case had Stage IV cancers. These observations suggest that anti-NXP2 antibodies may be associated with advanced cancer, as anti-TIF1-γ antibodies. The malignancies characteristic of anti-NXP2 antibody-positive CAM have not been clarified and ranged from systemic solid tumors, hematological cancers, and skin (4,5,11). Two other cases of cervical cancer have previously been reported in addition to ours (5).
Our patient experienced a recurrence of cervical cancer which had been diagnosed 8 years earlier after a 6-year period of stable disease, and at the same time developed anti-NXP2-positive dermatomyositis. The treatment of cancer metastasis resulted in an improvement of myositis. To our knowledge, no case of anti-NXP2 antibody-positive CAM has developed in association with recurrence after such a long period of stable disease. We thus speculated that cancer progression over a period of years in our case may have triggered autoimmunity against NXP2, thus resulting in the development of dermatomyositis.
Written informed consent for publication was obtained from the patient.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We wish to thank Tadahiro Sato, Keiichi Onishi, and Kanji Matsuura for their assessment and treatment of the case. We also thank Naoko Okiyama, Yuki Ichimura, and Risa Konishi from the Department of Dermatology, Faculty of Medicine, University of Tsukuba, for their measurement of anti-NXP2 and anti-SAE antibodies.
References
- 1. Yang H, Peng Q, Yin L, et al. Identification of multiple cancer-associated myositis-specific autoantibodies in idiopathic inflammatory myopathies: a large longitudinal cohort study. Arthritis Res Ther 19: 259, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oddis CV, Fertig N, Goel A, et al. Clinical and serological characterization of the anti-MJ antibody in childhood myositis [abstract]. Arthritis Rheum 40: S139, 1997. [Google Scholar]
- 3. Targoff IN, Trieu EP, Levy-Neto M, Fertig N, Oddis CV. Sera with autoantibodies to the MJ antigen react with NXP2 [Abstract]. Arthritis Rheum 56: S787, 2007. [Google Scholar]
- 4. Albayda J, Pinal-Fernandez I, Huang W, et al. Antinuclear matrix protein 2 autoantibodies and edema, muscle disease, and malignancy risk in dermatomyositis patients. Arthritis Care Res (Hoboken) 69: 1771-1776, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ichimura Y, Konishi R, Shobo M, et al. Anti-nuclear matrix protein 2 antibody-positive inflammatory myopathies represent extensive myositis without dermatomyositis-specific rash. Rheumatology (Oxford) 61: 1222-1227, 2022. [DOI] [PubMed] [Google Scholar]
- 6. Bohan A, Peter JB. Polymyositis and dermatomyositis. I. N Engl J Med 292: 344-347, 1975. [DOI] [PubMed] [Google Scholar]
- 7. Bohan A, Peter JB. Polymyositis and dermatomyositis. II. N Engl J Med 292: 403-407, 1975. [DOI] [PubMed] [Google Scholar]
- 8. Bunch WT. Prednisone and azathioprine for polymyositis: long-term followup. Arthritis Rheum 24: 45-48, 1981. [DOI] [PubMed] [Google Scholar]
- 9. Rogers A, Chung L, Li S, Casciola-Rosen L, Fiorentino DF. Cutaneous and systemic findings associated with nuclear matrix protein 2 antibodies in adult dermatomyositis patients. Arthritis Care Res (Hoboken) 69: 1909-1914, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ogawa-Momohara M, Muro Y, Mitsuma T, et al. Strong correlation between cancer progression and anti-transcription intermediary factor 1γ antibodies in dermatomyositis patients. Clin Exp Rheumatol 36: 990-995, 2018. [PubMed] [Google Scholar]
- 11. Ichimura Y, Matsushita T, Hamaguchi Y, et al. Anti-NXP2 autoantibodies in adult patients with idiopathic inflammatory myopathies: possible association with malignancy. Ann Rheum Dis 71: 710-713, 2012. [DOI] [PubMed] [Google Scholar]





