Abstract
The demographics of the UK population are changing and so is the need for health care. In this Health Policy, we explore the current health of the population, the changing health needs, and future threats to health. Relative to other high-income countries, the UK is lagging on many health outcomes, such as life expectancy and infant mortality, and there is a growing burden of mental illness. Successes exist, such as the striking improvements in oral health, but inequalities in health persist as well. The growth of the ageing population relative to the working-age population, the rise of multimorbidity, and persistent health inequalities, particularly for preventable illness, are all issues that the National Health Service (NHS) will face in the years to come. Meeting the challenges of the future will require an increased focus on health promotion and disease prevention, involving a more concerted effort to understand and tackle the multiple social, environmental, and economic factors that lie at the heart of health inequalities. The immediate priority of the NHS will be to mitigate the wider and long-term health consequences of the COVID-19 pandemic, but it must also strengthen its resilience to reduce the impact of other threats to health, such as the UK leaving the EU, climate change, and antimicrobial resistance.
Introduction
The UK's National Health Service (NHS) has adapted over time to many changing health needs and to advances in the technical and organisational ability to address them. These changing health needs include major declines in infectious diseases and their evolving nature, as well as the rising importance of non-communicable diseases. Paediatric wards are no longer full of children with gastroenteritis, respiratory infections, and hepatitis A. Instead, these wards now provide specialised neonatal, genetic, and chronic disease services, among others.1 Innovations in the management of mental health and the resulting reconfiguration of services, such as the closure of long-stay institutions, have completely altered treatment pathways, with both positive and negative results. Cardiothoracic surgeons nowadays rarely dilate mitral valves damaged by rheumatic heart disease or resect tuberculous lung cavities; these days, they repair congenital heart disease or do transplants. Orthopaedic surgeons no longer transplant tendons of children affected by polio, they instead replace arthritic joints among older people.2 General practitioners rarely deliver babies in patients' homes but instead contribute clinical expertise to a range of services provided by multi-agency teams based in the community. Dentists very rarely provide full dentures for adults and instead concentrate on prevention and provision of restorative care, including implants and bridges.3 Entirely new clinical careers and specialties have emerged, such as specialist nurses, interventional radiologists, and palliative care specialists, while geriatricians, managing the complex needs of frail and ageing patients, work alongside a growing number of superspecialists.4
International comparative studies, particularly in earlier decades, indicate that the NHS has been relatively good at such adaptations.5 Its system of funding manages to avoid many perverse incentives seen in fee-for-service systems that encourage lucrative interventions to persist long after they have become obsolete, and professional associations, such as the Royal Colleges, emphasise maintaining high standards of training and research rather than negotiating terms and conditions, as is the case with some of their equivalents elsewhere. However, some would argue that progress has been slow and inadequate in adapting to epidemiological transition (eg, in mental health and the rise in dementia) and in adopting research and innovation at pace (eg, for stroke management). More recently, designated funding for health services research has helped build capacity enormously, relative to what exists in many other countries, but there remain many gaps in the evidence base. A culture of evaluation and audit has been promoted and has developed extensively in certain areas, especially in areas supported by systematic national data collection—eg, within the national clinical audit programme. This research capacity is now needed to understand and develop strategies to mitigate the potentially long-lasting physical and mental health impacts of the COVID-19 pandemic.6
The goals of a health system were set out in the World Health Report in 2000.7 They include improving health outcomes, responding to legitimate public expectations, and achieving fair financing. The third of these is addressed elsewhere in the Commission report. The first and second require an NHS that is cognisant of the changing needs of the population and can adapt quickly and flexibly to them, on the basis of evidence; when evidence is not available, the NHS should take steps to generate it. Subsequent thinking, developed more fully in the WHO Tallinn Charter,8 describes mutual relationships between health systems, population health, and economic growth.9 Put simply, the goal of society should be to create a health system that promotes better health and, through improved lives, secures economic growth, which in turn secures revenues to support appropriate health-care provision for all, as well as associated developments elsewhere, such as in social care. Health and health care can therefore be both inputs to and outputs from the economy.
Yet, although it seems obvious that a key objective of the NHS should be to maximise the health of the UK population to the extent that this is possible for a health system to achieve, this interpretation has not always been shared by its leadership. The mission of the NHS has, in the past, been framed as the more limited, but potentially more tractable, objective of ensuring the provision of high-quality and safe health care to all in response to expressed need within available resources. This longstanding mismatch between the need for a service that optimises population health and a structure focused predominantly on health-care provision only might well have contributed to the UK's relatively poor performance on health outcomes.
It is impossible, in a single paper, to provide a comprehensive analysis of the health of the UK population and its implications for the NHS. Consequently, it has been necessary to be somewhat selective. This paper proceeds as follows. We begin with an assessment of the current situation and how it has developed, starting with the most widely used summary measure of the health of the population: life expectancy. We then review some areas that have important implications for the NHS. These areas are mental health, maternal and child health, oral health (an area that has long existed on the margins of the NHS), and the growing challenge of multimorbidity, with major implications for models of service delivery. Further on, we look at three ways in which the health of the population is still changing: ageing, the composition of the working population, and the burden of disease. The NHS is, in many respects, responding to failures in other areas of policy. Consequently, in a third section, we examine the scope for prevention, including measures to tackle the social determinants of health. Finally, looking ahead, we examine in the concluding section two immediate threats to the NHS: the COVID-19 pandemic and leaving the EU.
The health of the population
Life expectancy in the UK
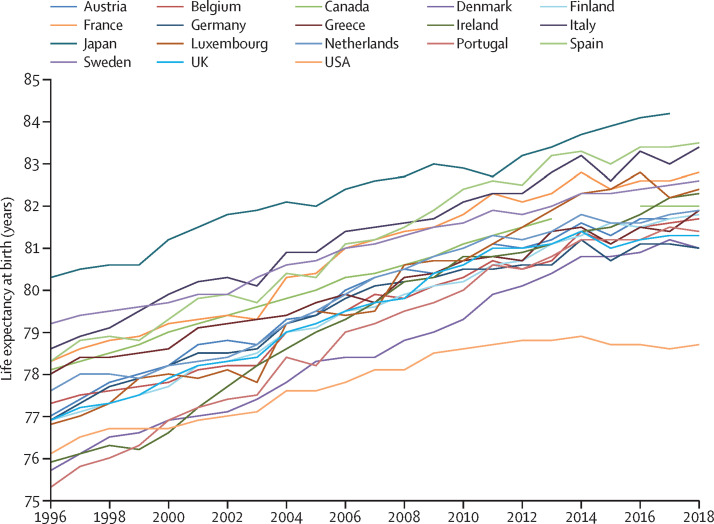
The health of the UK population is now lagging behind that of many comparable countries. Having been in the middle of the range of high-income countries in 1960, life expectancy at birth is now close to the bottom (figure 1 ). Since 2010, the rate of increase in life expectancy at birth has slowed markedly.10 A 2019 analysis compared life expectancy in England and Wales with that in 22 other high-income countries,11 and showed how England and Wales diverged markedly from the comparator group between 2011 and 2016. This divergence was driven to a similar extent by diverging mortality in people of working age and older people. Although more recent data are lacking for some comparator countries, the situation in the UK now gives substantial cause for concern; there have been continuing increases in death rates in several age groups and regions, and the infant mortality rate in England and Wales rose each year in 2014–17, something that has not happened for more than a century.12
Figure 1.
Trends in life expectancy at birth in the UK and comparable high-income countries
Source: Organisation for Economic Co-operation and Development.
The reasons why the UK is falling behind other high-income countries have been debated intensely. Some of the decline probably reflects historical trends, such as the timing of the smoking epidemic,11 but there is increasing evidence pointing to a link with the wide-ranging austerity measures since 2010 that have affected many areas of public policy. For example, although the explanation for rising infant mortality is disputed, it has been noted that the increase is greatest in the poorest areas.13 There have been substantial cuts to funding for local authorities, with resulting social care service reductions that particularly affect older people and those living in poverty.14, 15 An exceptional surge in numbers of deaths in 2015 also coincided with widespread capacity problems across the NHS and, although the particular strain of influenza circulating that year might have played a role, influenza seems unlikely to have been the only reason for this particular spike in mortality.16 A further spike occurred in 2018. Importantly, although the slowing is not unique and has been seen in some but not all European countries, it has been more pronounced in the UK than elsewhere, and it is not a survival asymptote of maximum life expectancy being reached, as the UK has not achieved the same levels as other comparable high-income countries. Within the UK, when measured by geography or socioeconomic indicators, it is apparent that there is much scope for the health of the most disadvantaged to improve substantially in terms of healthy and disability-free life expectancy. Although differences in life expectancy between the richest and poorest people in the UK narrowed during the 2000s, these differences have widened since 2011.17 The impact of the COVID-19 pandemic on life expectancy is yet to be established, but the combination of excess mortality directly attributable to the acute effects of the virus, emerging evidence of long-lasting health problems caused by the virus,18 and delayed diagnosis of many conditions such as cancer caused by the postponement of screening and reduced access to health-care services19 will probably lead to a sustained reduction in life expectancy in many countries. The knock-on effects on the economy, particularly those that exacerbate existing inequalities, will also have longer-term indirect effects. As the UK has had one of the highest death rates attributable to the COVID-19 pandemic so far, the gap in life expectancy between the UK and other developed nations might grow in the coming years.
There are also large differences between the four UK nations (appendix p 1). All have experienced a recent slowing of the rate of increase in life expectancy at birth. Life expectancy has consistently been higher in England than in the other three nations, with Scotland lagging far behind. Between 1998 and 2018, the gain in life expectancy at birth has been much smaller for women than for men. For example, in England, life expectancy increased by 4·3 years for men but only by 3·1 years for women. In Scotland, the gap was even greater, at 4·2 years for men and 2·7 years for women. For both sexes, these gains were among the smallest in industrialised countries. This discrepancy is driven, to a considerable extent, by stagnating or falling life expectancy among women aged 75 years and older, who have been affected especially harshly by austerity policies.20
Life expectancy is, of course, derived from data on deaths. It can be combined with data on people still alive to generate measures of disability-free life expectancy (DFLE) and healthy life expectancy (HLE). DFLE is an estimate of the number of years lived without a long-lasting physical or mental health condition that restricts daily activities. HLE is an estimate of the number of years lived in very good or good general health, based on how individuals perceive their general health. England has the highest life expectancy for both women (83·1) and men (79·6), and Scotland has the lowest life expectancy for both women (81·1) and men (77·0). England has the highest HLE and DFLE for both women (HLE 63·8, DFLE 62·2) and men (63·4, 63·1), whereas Wales has the lowest DFLE for women (59·5) and men (59·9), the lowest HLE for women (62·0), and second-lowest HLE for men (61·4; appendix p 2).
Within the four nations of the UK, there is especially poor health among populations in areas that have gone through deindustrialisation since the 1980s, such as the west of Scotland, parts of Northern Ireland, south Wales, and the northeast and northwest of England. Analysis by geography and deprivation shows that, although life expectancy varies by as much as 6 years between the regions of England, most of the difference is accounted for by levels of deprivation.21 This analysis also showed that, even though all the regions of England are subject to broadly similar underlying health policies, regulations, and laws, and all are served by the NHS, outcomes such as life expectancy and years lived with a disability in the more prosperous regions of the UK are similar to those in the best performing advanced high-income countries, such as Sweden and Australia. By contrast, in the less prosperous regions of the UK, these outcomes lag behind the worst-performing advanced high-income countries, such as Denmark and Greece.21 Similarly, disability-free life expectancy varies substantially within each UK nation, the consequence being that, in many parts of the UK, the average person cannot expect to reach the statutory retirement age in good health.22 There are also inequalities between ethnic groups, with estimates suggesting that differences in disability-free life expectancy, at 11·5 years, are twice as large as differences in life expectancy.23 Chinese men and women have the highest disability-free life expectancy at birth, whereas Bangladeshi men and Pakistani women have the lowest. The COVID-19 pandemic has exacerbated these health inequalities, particularly for Black and minority ethnic groups who have experienced persistently elevated mortality rates from COVID-19.24 Differential exposure to SARS-CoV-2 influenced by occupation and housing conditions, differential severity of COVID-19 influenced by existing health conditions, and differential interactions with the health service have all been suggested as potential contributing factors.25, 26
The scale and nature of these differences point to the importance of influences outside the health-care system on health outcomes.22 The Dahlgren and Whitehead model highlights the potential effect of the wider social determinants of health, such as housing, sanitation, unemployment, education, and food production.27 Austerity measures adopted since 2010 have had a disproportionate impact on the poor,28 creating insecurity of income, employment, housing,29 and even food supply, as revealed by the growth of food banks.30 Addressing these social determinants of ill health will require wide-ranging actions across many sectors and at every stage of the human life course, while recognising that disadvantage can be passed down generations, risking a downward spiral.31 These actions must account for intersectionality, whereby some individuals have a combination of characteristics (all of which disadvantage them), and the existence of a health gradient between rich and poor. These considerations point to the need for what is termed proportionate universalism,22 in which provision of services is universal, but measures are taken to increase uptake by those in most need.
Mental health
The burden of disease attributable to mental illness, including what are termed common mental illnesses (ie, anxiety, depression, panic disorder, phobias, and obsessive-compulsive disorder), has been growing over the past 25 years.32 The COVID-19 pandemic has also had a profound impact on mental health, with many individuals suffering from anxiety, isolation, and difficulties in accessing mental health support.33 High-quality data are needed to understand this effect, particularly for susceptible groups, such as older people, young people, people with pre-existing mental health issues, and health-care workers.34 To mitigate against long-term consequences for mental health, supportive measures are needed, such as providing widespread access to emergency psychological support and increased investment in mental health services.35 The mental health impacts of the COVID-19 pandemic have important implications for health inequalities and the wider economy. Mental illness is more common in socioeconomically deprived populations36 and is the leading cause of lost days of work in the UK; mental ill-health at work is estimated to cost the UK economy between £74 billion and £99 billion per year,37, 38 with important consequences for the labour-intensive health sector.
The mental health needs of the older population are substantial. Although the age-specific prevalence of dementia appears to be decreasing slightly,39 population ageing means that the absolute number of older adults experiencing cognitive decline due to Alzheimer's disease or other types of dementia will rise;40 prevalence of dementia increases from 2% for people aged 65–69 years to 18% for those aged 85–89 years.13 However, older people's mental health needs do not just relate to dementia. Depression is the most common mental health disorder in this age group, with an estimated prevalence of 22% in men and 28% in women aged 65 years and older and more than 40% in people living in care homes.41 There is also a high prevalence of anxiety disorder.42 Other disorders, such as bipolar disorder and psychosis, are less common but nonetheless significant. Research shows that older adults with depression are significantly less likely to be diagnosed and treated than younger adults with the condition,43 and services and funding for mental health care for older people is generally considered less of a priority than it is for working-age adults.44
There is growing evidence of a high burden of mental illness among British children and adolescents, to the point that the situation has been described as a crisis.45 Data from 2017 in England showed that one in eight individuals aged between 5 and 19 years had at least one mental illness and that one in twenty met criteria for two or more mental illnesses.46 The same data show a gradual increase in mental illness in young people since 1999, with the prevalence increasing with age, particularly on transition to adolescence and secondary school.46 Of particular concern is the high level of mental illness in girls aged 17–19 years. Nearly one in four in this group have a diagnosable mental illness, and more than half of them reported self-harming behaviour or suicide attempts. Universities have reported a huge increase in pressure on student mental health services and rising numbers of student suicides,47 and research shows an increase in adolescent girls presenting to UK Accident and Emergency departments with self-harm.48
The reasons for the increasing burden of mental illness in young people are complex. Social media, the impending threat of environmental catastrophe and political instability, uncertainty about future prospects, higher rates of family breakdown, and academic pressure have all been proposed as causative factors. Unrealistic social pressure to excel in all areas of life, promoted by social media and an ethos of consumerism, is another toxic, relatively new phenomenon. However, it is crucial to try to address this area of growing need as it is well established that around half of mental illnesses start before the age of 14 years and three-quarters are established by the age of 24 years,49 particularly because adolescence and young adulthood are pivotal life stages for key decisions regarding education, employment, and relationships.
The burden of disease due to alcohol and illicit drug use has increased across the UK in recent years. Alcohol-related deaths in the UK increased to an age-standardised rate of 12·2 per 100 000 people in 2017, which is similar to 2008 when alcohol-related deaths were at the highest recorded levels.50 Scotland consistently has the highest rate of alcohol-related deaths in the UK, at 20·5 per 100 000 in 2017, although this number has substantially reduced from a peak of 28·5 per 100 000 in 2006.50 Drug-related deaths in England and Wales have increased from an age-standardised rate of 42·9 per 1 000 000 in 1993 to 66·1 per 1 000 000 in 2017.51 In comparison, Scotland's incidence of drug-related deaths is more than three times the rate in England and Wales, at 192·6 per 1 000 000 in 2017,52 and is the highest drug-related death rate recorded in the EU. There are also substantial inequalities in alcohol-related and drug-related deaths across the UK. For example, more than half of the drug-related deaths in Scotland occur among people from the most deprived quintile,53 and the rate of alcohol-related deaths is more than three times higher in the most deprived quintile than in the least deprived quintile in England. These increases in alcohol-related and drug-related deaths have occurred during a period when drug and alcohol services are under intense financial pressure. For example, in England, local authorities cut budgets by 18% in real terms between 2013–14 and 2017–18,54 which contributed to an 11% reduction in people accessing treatment over the same period.
Maternal and child health
Maternal mortality in the UK is higher than it is in many countries in central and northern Europe (appendix p 3). Within the UK, there are substantial inequalities in maternal mortality between different ethnic groups and between groups with different levels of deprivation.55 The maternal mortality rate in women from a Black ethnic background is five times higher than that in White women, while the rate in women from an Asian ethnic background is double that in White women. Between the most and least deprived groups, there is a doubling in maternal mortality. Rather than narrowing, these trends have been widening over the past decade.55
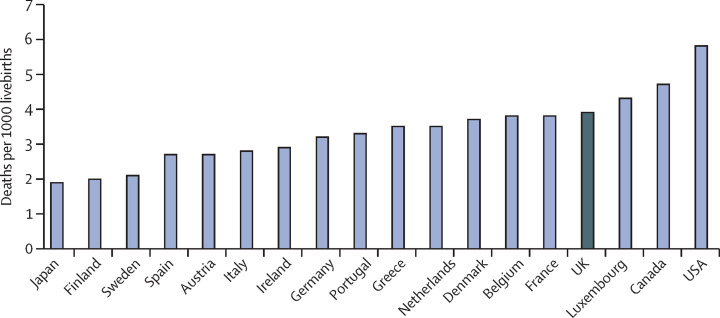
The UK's high mortality from conditions such as asthma, epilepsy, pneumonia, and meningococcal disease in childhood, compared with other European countries,56, 57 also suggests a problem with paediatric care, with infant mortality lagging behind many other high-income countries (figure 2 ).58 A recent, extremely detailed comparison with Sweden found that newborn babies in the UK had many more problems at birth than their counterparts in Sweden did, many of which could be traced to their worse socioeconomic status.59 Influences on health outcomes start in utero, and there is a clear social gradient in the extent to which children can access positive experiences in their early years.22 As already mentioned, since 2010, the UK government has chosen to implement prolonged austerity policies, including reductions in entitlements to welfare provision, with measures that have impacted particularly on the most vulnerable.60 Concerns have been expressed about the substantial increase in suicide rates among adolescents in England and Wales since 2010.61 Child poverty in the UK, as of 2017–18, was 30% and has been increasing since 2013–14, when it was 27%.62 This poverty rate is predicted to rise over the next few years, and children in single-parent families, with three or more siblings, in households where no one is in work, or in rented or social housing are known to be at particular risk of poverty.63
Figure 2.
Infant mortality in the UK and comparable high-income countries
Data are from 2018 or the latest year available. Source: Organisation for Economic Co-operation and Development.
Oral health
Oral diseases (eg, dental decay, periodontal [gum] diseases, and oral cancers) are highly prevalent chronic conditions that have a considerable impact on quality of life and are costly to health-care systems. The Global Burden of Disease study has highlighted that dental decay in adults is the most prevalent chronic health condition globally—overall, it is estimated that 3·5 billion people are affected by dental diseases.64 A 2019 analysis shows that the treatment of dental diseases among EU countries costs in excess of €90 billion per year, the third most expensive condition behind diabetes (€119 billion) and cardiovascular diseases (€111 billion).65 In recent decades, there has been a striking change in oral diseases among the UK population. When the NHS was first created, the state of oral health in the UK was appalling, with the complete removal of all teeth (edentulism) a relatively common occurrence for even young adults, often taking place before marriage. Nowadays, fewer than 5% of adults in the UK have no natural teeth, and overall oral health in both children and adults has improved greatly.66 The increased retention of natural teeth is a positive change but, as individuals age and become more frail, complex and costly dental treatment is often required. Stark socioeconomic and geographical inequalities in oral health exist. Steep and persistent social gradients are found for oral conditions in both children and adults, and oral health is worse in Northern Ireland and Scotland than it is in Wales and England.67 Oral diseases are caused by the broader social determinants in society and shared risk factors, such as consumption of sugars, tobacco, and alcohol.
In the UK, dental services are organised and funded in a different manner than medical services are. The vast majority of the 40 000 dentists in the UK work in primary care, providing general dental services to the population. Across the UK, different payment systems exist but co-payments operate in all countries, according to which adult patients contribute to the costs of their dental treatment. Children and exempt adults do not pay for their dental care. Patterns of dental attendance are strongly influenced by socioeconomic status, and concerns over the cost of treatment are a major barrier to accessing dental services.68
Multimorbidity
Older people are, individually, more likely to be healthy than they were in the past. However, the absolute numbers with ill health are increasing. Many will remain healthy by virtue of being treated for hypertension or diabetes, which averts the sequelae of these conditions. Others, although not in perfect health, experience considerable alleviation of their symptoms. The corollary of this and of earlier detection of chronic diseases and their risk factors is that ever more people experience multimorbidity, requiring some health care for multiple disorders, even if they are only reviewed in primary care every few months.36 Research in the UK estimates that around 23% of the population meet current criteria for multimorbidity, a figure that increases with age and attention to early diagnosis—around two-thirds of people older than 65 years meet these criteria, with nearly half having three or more conditions.36 There have been several attempts to classify commonly occurring clusters of conditions. Some diseases frequently co-exist and share common causes, but there is also considerable heterogeneity, and illnesses can also be completely unrelated. Chronic physical conditions often co-exist with mental health disorders—particularly with dementia—with evidence that the relationship is bidirectional.69 There is a clear association between multimorbidity and socioeconomic deprivation, and people living in deprived areas are likely to develop multimorbidity 10–15 years earlier than those living in more affluent areas.36
Multimorbidity has profound implications for how health care is delivered, as it demands a holistic approach delivered by multidisciplinary teams. The model of primary care, with its generalist approach, has found it easier to respond to this challenge than some models used in other countries, but the disadvantage, in a country that has somewhat fewer medical specialists than many others (despite growth in specialist posts in recent years), is that it might be difficult to obtain specialist expertise when needed. Unfortunately, the accessibility of primary care is now being threatened, with insufficient historical investment in these services. To compound the problem, chronic staffing shortages coupled with administrative overload add to falling morale and cause physical and psychological burnout. Such outcomes lead to growing problems in recruiting and retaining general practitioners and community nurses.
The changing health needs of the population
The UK's ageing population
Some changes in future health profiles can be predicted with relative certainty, such as the ageing of the population and, to some extent, a relative fall in those aged 18–65 years, albeit with caveats about future migration.70 Forecasting with some confidence is possible when the association between risks and disease are known and have long time periods, as is the case with smoking. Such forecasting is more difficult when lags between exposure and outcome are short, as with many of the consequences of hazardous drinking, and where public policies can have a major impact in the short term.
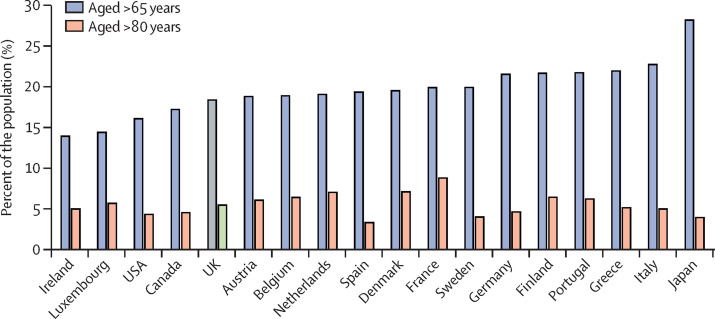
Although the UK does not have a particularly high proportion of older people relative to other high-income countries, with the share of people older than 65 years and people older than 80 years falling from 4th to 12th between 1995 and 2016 in one comparison of 17 countries (figure 3 ), it will eventually face similar challenges as other countries. Ageing per se does not necessarily affect health-care utilisation or add pressure to constrained NHS resources unless it is associated with increased chronic illness and higher rates of multiple long-term conditions.71
Figure 3.
Percentage of population at older ages in selected high-income countries, 2018
Source: Organisation for Economic Co-operation and Development.
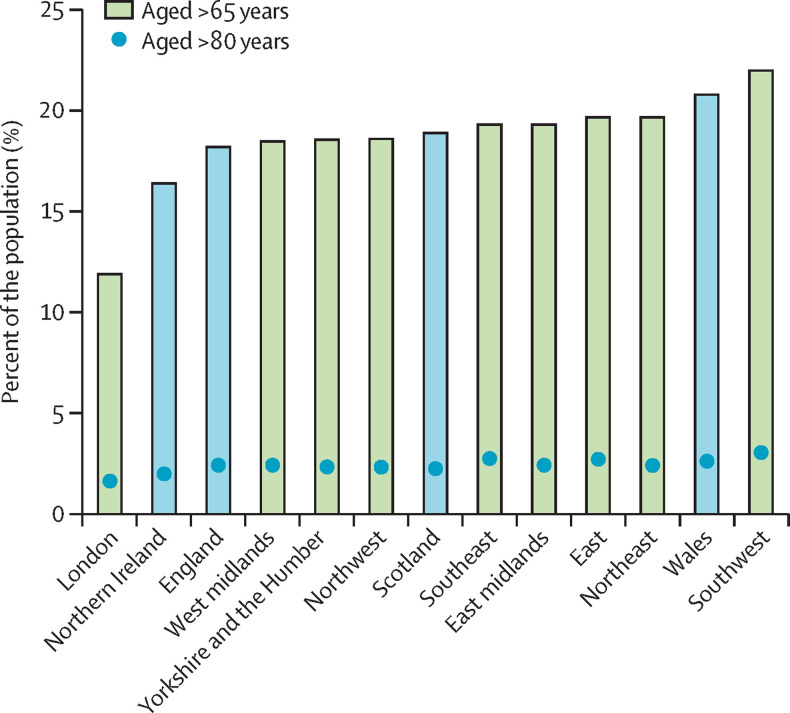
Considerable variation exists within the UK, with the largest share of older and very old people in the southwest of England and the smallest share in the northeast of England (figure 4 ). There is also a sizable discrepancy in the age distribution of different ethnic groups (appendix p 3). Both the geographical and ethnic spread of the older population matters, as it leads to specific pressure points on NHS access, as well as contributing to the unequal distribution of ill-health within the UK. As ethnicity is not recorded on death certificates in the UK, it is not possible to routinely report on life expectancy stratified by ethnicity. However, some recent studies that have used various techniques to try to estimate life expectancy by ethnicity show significant discrepancies between groups, which vary by region.73, 74, 75
Figure 4.
Percentage of population aged 65+ years and 85+ years, 2019
Source: Office for National Statistics.72
The working population
The participation of women in the labour force is at an all-time high.76 Thus, as the share of the population who are of working age declines, there is little scope to draw even more into the workforce, an important consideration given their major contribution to the health and care workforce. However, caution is needed. Old-age dependency ratio, a frequently cited measure, has been used in sometimes apocalyptic predictions, typically to argue for the unsustainability of the welfare state. Yet it assumes an economically (and socially) inactive stage of life beyond 65 years of age that is no longer the case. The raising of the retirement age in the UK and many other countries has changed such calculations considerably, even before taking into account the work and informal care of spouses, parents, adult children, and grandchildren provided by older people, sometimes with competing demands.77, 78 There are, however, many uncertainties about the future composition of the UK population. The experience of Japan,79 a country that has had very little immigration albeit for different reasons, is concerning, as the young are attracted to major centres for their early working careers, while older people remain in rural or coastal regions, creating a skill gap for care.
In this context, the UK Government's stated goal of reducing migration from the hundreds of thousands to the tens of thousands is a clear cause for concern. The NHS has a long history of relying on foreign recruitment in response to workforce shortfalls. For example, in light of ongoing uncertainty about future EU citizen arrangements, there has been a 90% reduction in nurses from other EU member states joining the UK's register in 2017–18 compared with 2016–17.80 Growing numbers of medical posts remain unfilled, with the government refusing visas to non-EU doctors with job offers and even to those training in this country.81 The social care sector is also heavily dependent on foreign recruitment, yet senior care workers are currently not on the government's so-called shortage occupation list.82
Changing burden of disease
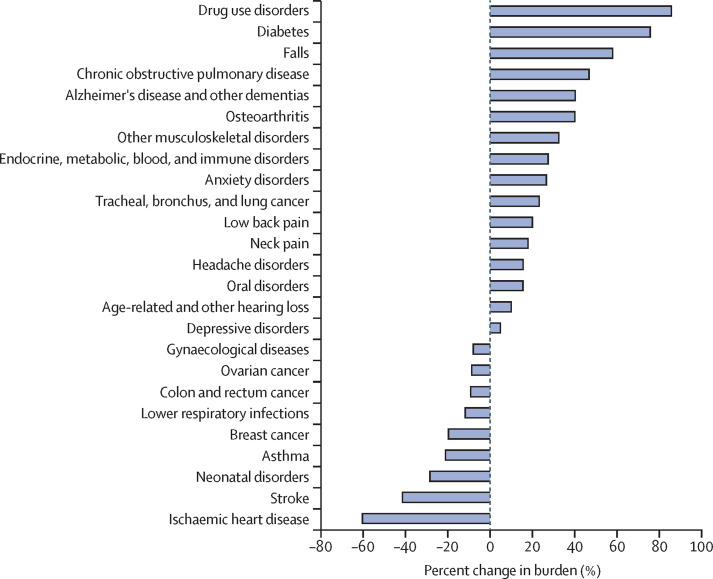
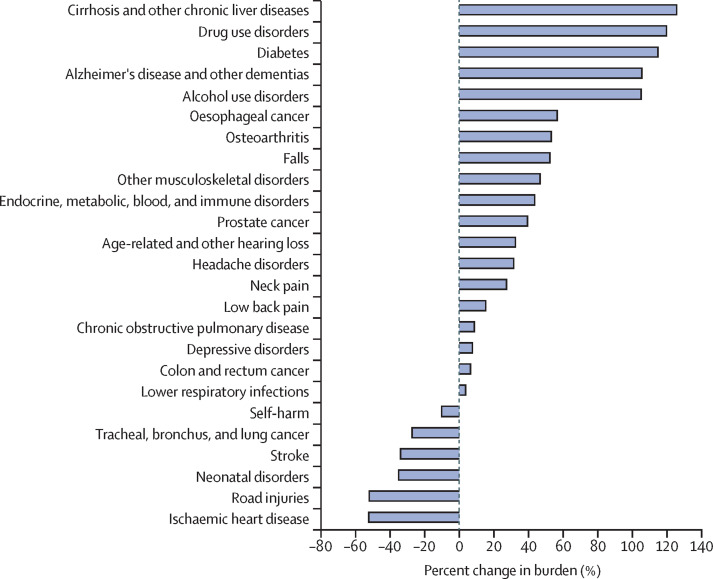
The combination of trends in underlying population health, the application of effective preventive interventions, and advances in health care have led to a shift in the predominant share of the burden of ill-health worldwide from conditions causing premature mortality to conditions that cause disability. Health systems everywhere must adapt to the changing nature of health need. The Global Burden of Disease study captures this idea in its analysis of disability-adjusted life years (DALYs). Figure 5, Figure 6 show the percentage change in burden attributed to the top 25 causes of DALYs in the UK for both genders from 1990 to 2019. For both men and women, there have been substantial increases in disease burden due to drug use disorders. In men, these addiction problems have been exacerbated further by increases in disease burden due to alcohol use disorders. Addiction services have struggled to meet this rising demand in the context of ongoing funding cuts over the past decade.83 This situation has had implications for NHS services, as harmful drinking has contributed to the increase in disease burden due to liver cirrhosis. Smoking rates have fallen markedly, reducing the future risk of many smoking-related diseases such as stroke and myocardial infarctions, which have been declining for several decades. However, the benefits of this change are yet to be felt, with increases in disease burden due to chronic obstructive pulmonary disease seen in both men and women. Conversely, rates of obesity at younger ages are increasing, with implications for a range of common disorders, such as diabetes, cancer, and dementia.
Figure 5.
Percentage change in burden due to the top 25 causes of DALYs in women in the UK, 1990–2019
Source: Global Burden of Disease. DALY=disability-adjusted life year.
Figure 6.
Percentage change in burden due to the top 25 causes of DALYs in men in the UK, 1990–2019
Source: Global Burden of Disease. DALY=disability-adjusted life year.
The proportion of the population aged 65 years and older is predicted to increase from 18·5% in 2019 to 23·9% in 2039.84 Assuming no change in age-specific utilisation, this would increase demand for health and social care in particular.85 The changing population structure has already led to an absolute increase in numbers of deaths, as predicted, after many years of decline.86 A major component of health costs is driven by proximity to death, not by chronological age; many older people are now healthier than their counterparts in previous generations. However, the absolute number of older people with multiple conditions is set to increase substantially over the next few decades, potentially more so as the emphasis on early detection continues. As premature mortality reduces, disabling conditions whose prevalence increases sharply with age (eg, sensory deficits, mobility problems, cognitive decline, and incontinence) will progressively accrue, leading to complex multimorbidity. These trends in common conditions have been brought together with population ageing in a dynamic model.85 This model predicts that the number of people with four or more conditions will increase between 2015 and 2035 by 21% in those aged 65–74 years, 130% in those aged 75–84 years, and 470% in those aged 85 years and older. The changing nature of demand for health and social care that results is a challenge for any health system and requires an explicit response, even more so for a health-care system that encourages people to seek earlier medical care for conditions, sometimes before they are clinically manifest. Therefore, the concern is less ageing per se, but ageing with multiple preventable conditions leading to poor health and wellbeing.
Reducing the need for health care
The need for a preventive focus
One of the key messages of the Tallinn Charter8 was that effective prevention could reduce the need for health care and thus the need for scarce resources. Effective prevention was also a key message of the Wanless Report, commissioned by the UK Treasury,87 which forecast the potential to moderate future NHS expenditure if what it called a fully engaged policy could be adopted. This concept, of investing in health improvement to reduce future costs, also features prominently in the NHS Long-Term Plan.88 An additional consideration is the compelling evidence linking better health to economic growth through higher labour force participation and productivity.89 There are many examples of successes in implementing health-promoting policies in Europe.90
The countries of the UK have been among the leaders internationally in many of the most effective policies to reduce harms associated with use of hazardous substances, such as tobacco, alcohol, and, most recently, junk food. Governments have recognised that the most effective policies are those based on price, availability, and marketing. Examples include minimum alcohol pricing in Scotland and Wales, above-inflation increases in tobacco taxation, a ban on smoking in public places, point-of-sale displays, the sugar tax, and standardised cigarette packaging. However, these face powerful lobbying activities by the corresponding industries, both directly and through several think tanks that they fund.91, 92 For a brief period, the alcohol and food industries benefitted from the creation of so-called responsibility deals, in which the UK Government sought to engage with them in official forums. However, the government's own evaluation found that industry representatives typically proposed the least effective measures and opposed those known to be effective.93 These responsibility deals did lead to pledges from many companies to reduce salt content in food and contributed to a reduction in overall salt intake in the UK of 11% between 2006 and 2014.94 However, eventually, key health advocacy organisations withdrew.
Moving forward, there is a need for more joint approaches that bring together different groups working on, for example, tobacco, alcohol, or diet to secure maximum benefit from shifting population norms on the five healthy living imperatives (not smoking, adhering to alcohol guidelines, maintaining a healthy weight, staying physically active, and eating a healthy diet) that influence rates of non-communicable diseases. This strategy will require policies that address these issues specifically and others that take a concerted approach to the upstream determinants of health, including both the well recognised social determinants of health and, even more now, the commercial determinants,95 by looking at how powerful vested interests can subvert health policies. It is also necessary to address the political determinants of health, such as austerity, welfare, and immigration regimes, and the environmental determinants, such as the design of health-promoting cities.
Addressing the social determinants of health
Although successive governments have adopted effective public health policies, these have struggled in the face of wider societal problems. Consequently, despite noted successes in areas such as tobacco control, the UK ranked only 12th overall in an assessment of public health policies across the European region of WHO.96 Looking ahead, there is clearly a need to address the underlying social determinants of health, or the conditions in which people are born, grow, live, work, and age,22 with policies that address precariousness of employment, income, housing, and food security.97 The UK has high rates of child poverty, lax building standards, and underinvestment in social housing, contributing to many people living in substandard accommodation and, since 2010, a marked rise in food insecurity.30 Other social problems relate to the employment market: although the introduction of a minimum wage was associated with a demonstrable improvement in mental health,98 and official unemployment rates are low, there are growing numbers of people who remain below the minimum wage, a practice that is illegal but rarely policed.99 Growing numbers of people also face severe uncertainty about income and employment in what is termed the gig economy, characterised by piecework and limited employment rights. Against this background of the erosion of wider welfare policies and falling public expenditure in other areas of welfare, the NHS is increasingly left as the one remaining pillar of the UK welfare state.
Health care is an important route through which health improvements can be channelled, but other sectors remain important in addressing health promotion and inequalities. There is compelling evidence in many areas that health-promoting policies work, especially those that involve all relevant sectors, enshrined in the concept of Health in All Policies. Wales is pioneering this approach through the Wellbeing of Future Generations Act 2015 and the Public Health Act 2017.100, 101 As a major employer, this is an area where the NHS could play a crucial role, although such an approach would require a substantial culture change in an organisation that is more often associated with high levels of work-related stress and burnout. Health-promoting policies do have the potential not only to alleviate suffering but also to reduce further the demand on the NHS if there is the political will to implement them.
Immediate threats to the NHS
The need for a resilient NHS
The initial version of this paper argued that the NHS must prepare for the unexpected and ensure it was resilient in the face of potential threats, including a pandemic,102 especially given the threat posed by the loss of links with European agencies such as the European Centre for Disease Prevention and Control and the European Monitoring Centre for Drugs and Drug Addiction.103, 104 The COVID-19 pandemic has, tragically, revealed that the UK was less prepared than it could have been.
As of April, 2021, the UK was among the worst affected countries in the world, measured by deaths attributed directly to COVID-19 or by excess all-cause mortality (the preferred measure for international comparisons). There will be many lessons to learn from the response: confused messaging by ministers; outsourcing of essential functions to companies lacking expertise; fragmentation of the NHS and public health and social care systems; elevated mortality rates among Black and minority ethnic groups; fraught relationships between central and local government, as well as with devolved nations; serious failures in the procurement of essential items, from ventilators to test kits and personal protective equipment; and entire new but largely unused hospital facilities.105 The response and efforts of those working in the NHS should also be recognised as exceptional, including repurposing existing hospital facilities, rapidly expanding access to teleconsultations, reallocating staff, sharing knowledge about the emerging clinical characteristics of this disease, implementing a world-leading clinical trial programme, and the rapid vaccination of the population triaged by risk factors such as age and comorbodities.106 Impacts in parts of the social care sector, especially in care homes, have been devastating and responses by staff similarly exceptional, again with many lessons to be learnt.107
The UK's response has, however, come at an enormous cost, both financially and in terms of the long-term consequences for health. These consequences can be considered under five headings: the long-term consequences of the infection on the body; delays in care as a consequence of the suspension of certain NHS services; the health effects of the lockdown; the impact on NHS staff; and the long-term economic impact. In the first category, it is becoming clear that many of those who survive COVID-19 have persisting health problems, many apparently associated with the action of the virus on the vascular endothelium and the associated immune response and hypercoagulability.108 In this respect, some have questioned whether it will come to be compared with polio, which also left a long-lasting legacy of ill-health. In the second category, there was a large reduction in primary care attendances,109 storing up considerable unmet need for the future, and routine surgery has been suspended, leaving a massive backlog to be treated in what was an already struggling system. Delayed diagnosis and treatment of early-stage cancer has been estimated to lead to more than 6000 additional deaths in a year.110 Estimates suggest that 3800 early cancers that would have been picked up on screening have been missed.111 In the third category, prolonged isolation coupled with the cessation of specialist services is likely to contribute to an increased burden of mental illness, while the closure of schools is likely to contribute to mental illness in children and young people.6 The fourth category includes the effects of psychological trauma on NHS and social care staff, including responses more usually seen in survivors of armed conflict.112 Fifth, the pandemic is expected to lead to a long-term reduction in economic growth,113 that could see many of the health problems associated with austerity in the period after 2010 return.97 To add to the problems, the ability of the NHS to respond could be complicated by the need for new ways of working, including greater use of personal protective equipment, social distancing, and remote consultations.
There are also other threats ahead, some more certain than others. One is antimicrobial resistance, an area where the UK has shown global leadership.114 Another is the consequences of a generation transitioning into retirement in a much more precarious financial state than their parents because of closure or reduction of pension schemes and lower levels of home ownership; this generation might struggle to come to terms with their straitened circumstances.90 A third is climate change, with evidence that the climate is changing even faster than predicted, potentially nearing a tipping point of runaway global warming. The COVID-19 pandemic has ushered in a temporary period of reduced carbon emissions; government actions and economic incentives after the pandemic will determine whether carbon emissions continue on the same path.115
In summary, the future is uncertain. Some of the uncertainties can be anticipated to some extent but for others, it is more difficult. The lesson from the COVID-19 pandemic is that the NHS must both anticipate predictable developments and build in sufficient resilience for the unexpected while working with other sectors to develop holistic solutions.
Leaving the EU
The UK's decision to leave the EU will have serious consequences for health116 but, as of April, 2021, these consequences have yet to become fully apparent. Although imports to Great Britain have fallen substantially, the full effect of leaving the EU will not be visible until the UK Government introduces the full range of customs checks it is required to impose but has, for now, delayed. In addition, it is difficult to distinguish the economic effects of leaving the EU from those of the pandemic. The problems ahead can, however, be understood from the near collapse of some exports, such as foodstuffs, since the EU has already imposed checks on its side of the border. The problems are also clear from the issues faced by shops in Northern Ireland, no longer able to depend on their historical supply arrangements with Great Britain. It has also become apparent that many commitments made by the UK Government before leaving the EU, many of them suggesting that particular arrangements will continue as before, have not in fact been honoured, either in part or in whole. While UK scientists will continue to be able to participate in some, but not all, of the EU's research programmes, the Turing scheme is substantially inferior to the ERASMUS+ scheme that it relaces, in terms of mobility of staff and students. A Global Health Insurance Card, to replace the European equivalent, no longer includes the non-EU European Economic Area countries. Some arrangements for data sharing during emergencies with the European Centre for Disease Prevention and Control have been agreed but, again, are much inferior to those that existed previously. Further progress is complicated by the loss of trust in the UK among many politicians in the EU27, given the UK's failure to implement measures it had previously committed to, especially in relation to the Northern Ireland Protocol. This situation has not been helped by the nationalist rhetoric that has accompanied AstraZeneca's failure to deliver to EU countries the quantity of vaccines that it had committed to.117
Beyond the immediate problems, the health of the UK population is affected by many other aspects of public policy. Food quality and safety, agriculture, land management, and environmental regulations are just a few of the areas of concern currently addressed by EU legislation that have substantial implications for human health.118 Of particular concern to health and health services will be the nature of any future international trade agreements. Issues around intellectual property rights, technical barriers to trade, and investor protection need to be thought through carefully,119 and protections for health and health care put in place. It is vitally important that, in the new trade agreements, health is not subverted by commercial interests for economic gain.120 Overall economic performance following departure from the EU will also be very important, with implications not just for the available funds to spend on health, but for the wellbeing of the UK population and the consequent demand for health care.
Conclusion
This Health Policy paper has reviewed the current health of the UK population and the changing health needs and has considered what future challenges lie ahead. From these considerations, we can draw several conclusions. First, despite substantial improvements in life expectancy, many physical and mental health outcomes are suboptimal relative to other high-income countries. Driving this suboptimality is that, across all ages but especially in childhood and old age, the population has high levels of preventable ill-health, which is unfairly distributed across society. As the UK has experienced a relatively high excess mortality rate attributable to COVID-19, the gap in life expectancy between the UK and other developed countries is likely to grow.
Second, in the future, there will be relatively fewer people in the working population, especially if current policies on migration continue, and a sharp rise in people with complex multimorbidity. This trajectory will create a mismatch between needs and capacity to address those needs, both through workforce availability and securing the economic basis for sustainable funding. To address these issues, there needs to be an increased focus on prevention and health promotion that takes a multisectoral approach to the social, political, and commercial causes of poor health. The crucial role the NHS can play by setting an example as a healthy employer, reducing risk factors for chronic diseases, promoting healthy ageing, enhancing confidence, and promoting social engagement should be addressed explicitly. However, the NHS is increasingly operating in an environment in which other sectors—especially social care—are being eroded in terms of expenditure and general infrastructure, instead of being maintained as supportive systems.
Finally, there are many immediate threats that will affect the health of the population and service provision. Crucially, the UK will need to develop strategies to mitigate against the wider and long-term consequences for health of the COVID-19 pandemic. In addition, the UK's departure from the EU, growing antimicrobial resistance, and increasing climate change are all major challenges with significant consequences for the NHS. Other unforeseen risks, such as economic downturn or even conflict, would impact the NHS but are practically difficult to plan for. Instead, the focus should be on building a resilient and preventive health-care service, so that the NHS is better prepared for any future challenges.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
Funding for the LSE–Lancet Commission on the future of the NHS was granted by the LSE Knowledge and Exchange Impact (KEI) fund, which was created using funds from the Higher Education Innovation Fund (HEIF). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Contributors
MM and KD led the working group that prepared the paper. MA and CJ-W managed the processes of the working group, compiled the data and figures, and contributed to editing of the manuscript. All other authors provided critical input into the drafting and editing of the manuscript.
Supplementary Material
References
- 1.Wolfe I, Mckee M. Open University Press; Berkshire, UK: 2013. European child health services and systems: lessons without borders. [Google Scholar]
- 2.McKee M, Healy J. The role of the hospital in a changing environment. Bull World Health Organ. 2000;78:803–810. [PMC free article] [PubMed] [Google Scholar]
- 3.Kleinman ER, Harper PR, Gallagher JE. Trends in NHS primary dental care for older people in England: implications for the future. Gerodontology. 2009;26:193–201. doi: 10.1111/j.1741-2358.2008.00260.x. [DOI] [PubMed] [Google Scholar]
- 4.Dubois C-A, McKee M. Cross-national comparisons of human resources for health—what can we learn? Health Econ Policy Law. 2006;1:59–78. doi: 10.1017/S1744133105001027. [DOI] [PubMed] [Google Scholar]
- 5.Nolte E, McKee M. McGraw-Hill Education; Berkshire, UK: 2008. Caring for people with chronic conditions: a health system perspective. [Google Scholar]
- 6.Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of COVID-19 pandemic response. BMJ. 2020;369 doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO . World Health Organization; Geneva: 2000. The World Health Report 2000. Health systems: improving performance. [Google Scholar]
- 8.WHO The Tallinn charter: health systems for health and wealth. June 27, 2008. http://www.euro.who.int/en/media-centre/events/events/2008/06/who-european-ministerial-conference-on-health-systems/documentation/conference-documents/the-tallinn-charter-health-systems-for-health-and-wealth
- 9.McKee M, Suhrcke M, Nolte E, et al. Health systems, health, and wealth: a European perspective. Lancet. 2009;373:349–351. doi: 10.1016/S0140-6736(09)60098-2. [DOI] [PubMed] [Google Scholar]
- 10.Public Health England A review of recent trends in mortality in England. December, 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/786515/Recent_trends_in_mortality_in_England.pdf
- 11.Leon DA, Jdanov DA, Shkolnikov VM. Trends in life expectancy and age-specific mortality in England and Wales, 1970–2016, in comparison with a set of 22 high-income countries: an analysis of vital statistics data. Lancet Public Health. 2019;4:e575–e582. doi: 10.1016/S2468-2667(19)30177-X. [DOI] [PubMed] [Google Scholar]
- 12.Office for National Statistics Child and infant mortality in England and Wales: 2017. June 17, 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/childhoodinfantandperinatalmortalityinenglandandwales/2017
- 13.Taylor-Robinson D, Lai ETC, Wickham S, et al. Assessing the impact of rising child poverty on the unprecedented rise in infant mortality in England, 2000–2017: time trend analysis. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-029424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loopstra R, McKee M, Katikireddi SV, Taylor-Robinson D, Barr B, Stuckler D. Austerity and old-age mortality in England: a longitudinal cross-local area analysis, 2007–2013. J R Soc Med. 2016;109:109–116. doi: 10.1177/0141076816632215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hiam L, Harrison D, McKee M, Dorling D. Why is life expectancy in England and Wales ‘stalling’? J Epidemiol Community Health. 2018;72:404–408. doi: 10.1136/jech-2017-210401. [DOI] [PubMed] [Google Scholar]
- 16.Hiam L, Dorling D, Harrison D, McKee M. What caused the spike in mortality in England and Wales in January 2015? J R Soc Med. 2017;110:131–137. doi: 10.1177/0141076817693600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marshall L, Finch D, Cairncross L, Bibby J. Mortality and life expectancy trends in the UK: stalling progress. November, 2019. https://www.health.org.uk/publications/reports/mortality-and-life-expectancy-trends-in-the-uk
- 18.Roberts CM, Levi M, McKee M, Schilling R, Lim WS, Grocott MPW. COVID-19: a complex multisystem disorder. Br J Anaesth. 2020;125:238–242. doi: 10.1016/j.bja.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richards M, Anderson M, Carter P, Ebert BL, Mossialos E. The impact of the COVID-19 pandemic on cancer care. Nat Cancer. 2020;1:565–567. doi: 10.1038/s43018-020-0074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hiam L, Dorling D, Harrison D, McKee M. Why has mortality in England and Wales been increasing? An iterative demographic analysis. J R Soc Med. 2017;110:153–162. doi: 10.1177/0141076817693599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newton JN, Briggs ADM, Murray CJL, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2257–2274. doi: 10.1016/S0140-6736(15)00195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marmot M, Goldblatt P, Allen J, et al. The Marmot Review: fair society, healthy lives. February, 2010. http://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review
- 23.Wohland P, Rees P, Nazroo J, Jagger C. Inequalities in healthy life expectancy between ethnic groups in England and Wales in 2001. Ethn Health. 2015;20:341–353. doi: 10.1080/13557858.2014.921892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Office for National Statistics Coronavirus (COVID-19) related deaths by ethnic group, England and Wales: 2 March 2020 to 15 may 2020. June 19, 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbyethnicgroupenglandandwales/2march2020to15may2020
- 25.Devakumar D, Selvarajah S, Shannon G, et al. Racism, the public health crisis we can no longer ignore. Lancet. 2020;395:e112–e113. doi: 10.1016/S0140-6736(20)31371-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Godlee F. Racism: the other pandemic. BMJ. 2020;369 [Google Scholar]
- 27.Whitehead M, Dahlgren G. What can be done about inequalities in health? Lancet. 1991;338:1059–1063. doi: 10.1016/0140-6736(91)91911-d. [DOI] [PubMed] [Google Scholar]
- 28.Cummins I. The Impact of austerity on mental health service provision: a UK perspective. Int J Environ Res Public Health. 2018;15:15. doi: 10.3390/ijerph15061145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reeves A, Clair A, McKee M, Stuckler D. Reductions in the United Kingdom's government housing benefit and symptoms of depression in low-income households. Am J Epidemiol. 2016;184:421–429. doi: 10.1093/aje/kww055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loopstra R, Reeves A, Taylor-Robinson D, Barr B, McKee M, Stuckler D. Austerity, sanctions, and the rise of food banks in the UK. BMJ. 2015;350 doi: 10.1136/bmj.h1775. [DOI] [PubMed] [Google Scholar]
- 31.Organisation for Economic Co-operation and Development. WHO . Organisation for Economic Co-operation and Development; Paris: 2003. Poverty and health. [Google Scholar]
- 32.Baker C. Mental health statistics: prevalence, services and funding in England. https://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN06988
- 33.Cowan K. Survey results: understanding people's concerns about the mental health impacts of the COVID-19 pandemic. April, 2020. https://acmedsci.ac.uk/file-download/99436893
- 34.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.United Nations Policy brief: COVID-19 and the need for action on mental health. May 13, 2020. https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf
- 36.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 37.Health and Safety Executive Working days lost in Great Britain. 2019. http://www.hse.gov.uk/statistics/dayslost.htm
- 38.Farmer P, Stevenson D. Thriving at Work: a review of mental health and employers. Oct 26, 2017. https://www.gov.uk/government/publications/thriving-at-work-a-review-of-mental-health-and-employers
- 39.Matthews FE, Arthur A, Barnes LE, et al. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet. 2013;382:1405–1412. doi: 10.1016/S0140-6736(13)61570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prince M, Knapp M, Guerchet M, et al. Dementia UK: update. November, 2014. https://www.alzheimers.org.uk/sites/default/files/migrate/downloads/dementia_uk_update.pdf
- 41.Stickland N, Gentry T. Hidden in plain sight: the unmet mental health needs of older people. October, 2016. https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/health--wellbeing/rb_oct16_hidden_in_plain_sight_older_peoples_mental_health.pdf
- 42.Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: methodological issues and a review of the literature. J Affect Disord. 2008;109:233–250. doi: 10.1016/j.jad.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 43.Burns A. Better access to mental health services for older people. Oct 9, 2015. https://www.england.nhs.uk/blog/mh-better-access/
- 44.Royal College of Psychiatrists Suffering in silence: age inequality in older people's mental health care. November, 2018. https://www.rcpsych.ac.uk/improving-care/campaigning-for-better-mental-health-policy/college-reports/2018-college-reports/cr221
- 45.Gunnell D, Kidger J, Elvidge H. Adolescent mental health in crisis. BMJ. 2018;361 doi: 10.1136/bmj.k2608. [DOI] [PubMed] [Google Scholar]
- 46.NHS Digital Mental health of children and young people in England, 2017. Nov 22, 2018. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2017/2017
- 47.Universities UK. Minding our future: starting a conversation about the support of student mental health. May 11, 2018. https://www.universitiesuk.ac.uk/policy-and-analysis/reports/Pages/minding-our-future-starting-a-conversation-support-student-mental-health.aspx
- 48.Morgan C, Webb RT, Carr MJ, et al. Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ. 2017;359 doi: 10.1136/bmj.j4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 50.Office for National Statistics Alcohol-specific deaths in the UK: registered in 2017. Dec 4, 2018. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/alcoholrelateddeathsintheunitedkingdom/registeredin2017#comparisons-between-the-four-countries-of-the-uk
- 51.Office for National Statistics Deaths related to drug poisoning in England and Wales: 2017 registrations. Aug 6, 2018. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2017registrations#drug-poisoning-deaths-in-2017-remained-stable
- 52.National Records of Scotland Drug-related deaths in Scotland in 2018. July 16, 2019. https://www.nrscotland.gov.uk/files/statistics/drug-related-deaths/2018/drug-related-deaths-18-pub.pdf
- 53.Barnsdale L, Guonari X, Graham L. The National Drug-Related Deaths Database (Scotland) Report: analysis of deaths occurring in 2015 and 2016. June 12, 2018. https://www.isdscotland.org/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2018-06-12/2018-06-12-NDRDD-Report.pdf
- 54.Rhodes D. Drug and alcohol services cut by £162m as deaths increase. May 11, 2018. https://www.bbc.com/news/uk-england-44039996
- 55.Knight M, Bunch K, Kenyon S, Tuffnell D, Kurinczuk JJ. A national population-based cohort study to investigate inequalities in maternal mortality in the United Kingdom, 2009–17. Paediatr Perinat Epidemiol. 2020;34:392–398. doi: 10.1111/ppe.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shah R, Hagell A, Cheung R. International comparisons of health and wellbeing in adolescence and early adulthood. February, 2019. https://www.nuffieldtrust.org.uk/files/2019-02/1550657729_nt-ayph-adolescent-health-report-web.pdf
- 57.Viner R, Ward J, Cheung R, Wolfe I, Hargreaves D. Child health in 2030 in England: comparisons with other wealthy countries. October, 2018. https://www.rcpch.ac.uk/sites/default/files/2018-10/child_health_in_2030_in_england_-report_2018-10.pdf
- 58.Wolfe I, Thompson M, Gill P, et al. Health services for children in western Europe. Lancet. 2013;381:1224–1234. doi: 10.1016/S0140-6736(12)62085-6. [DOI] [PubMed] [Google Scholar]
- 59.Zylbersztejn A, Gilbert R, Hjern A, Wijlaars L, Hardelid P. Child mortality in England compared with Sweden: a birth cohort study. Lancet. 2018;391:2008–2018. doi: 10.1016/S0140-6736(18)30670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Karanikolos M, Mladovsky P, Cylus J, et al. Financial crisis, austerity, and health in Europe. Lancet. 2013;381:1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- 61.Bould H, Mars B, Moran P, Biddle L, Gunnell D. Rising suicide rates among adolescents in England and Wales. Lancet. 2019;394:116–117. doi: 10.1016/S0140-6736(19)31102-X. [DOI] [PubMed] [Google Scholar]
- 62.UK Department for Work & Pensions Households below average income: an analysis of the UK income distribution, 1994/95–2017/18. March 28, 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/789997/households-below-average-income-1994-1995-2017-2018.pdf
- 63.Corlett A. The living standards outlook. February, 2019. https://www.resolutionfoundation.org/publications/the-living-standards-outlook-2019/
- 64.Kassebaum NJ, Smith AGC, Bernabé E, et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 Countries, 1990–2015: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J Dent Res. 2017;96:380–387. doi: 10.1177/0022034517693566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249–260. doi: 10.1016/S0140-6736(19)31146-8. [DOI] [PubMed] [Google Scholar]
- 66.Steele JG, Treasure ET, O'Sullivan I, Morris J, Murray JJ. Adult Dental Health Survey 2009: transformations in British oral health 1968–2009. Br Dent J. 2012;213:523–527. doi: 10.1038/sj.bdj.2012.1067. [DOI] [PubMed] [Google Scholar]
- 67.Shen J, Wildman J, Steele J. Measuring and decomposing oral health inequalities in a UK population. Community Dent Oral Epidemiol. 2013;41:481–489. doi: 10.1111/cdoe.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Watt RG, Steele JG, Treasure ET, White DA, Pitts NB, Murray JJ. Adult Dental Health Survey 2009: implications of findings for clinical practice and oral health policy. Br Dent J. 2013;214:71–75. doi: 10.1038/sj.bdj.2013.50. [DOI] [PubMed] [Google Scholar]
- 69.The Academy of Medical Sciences Multimorbidity: a priority for global health research. April, 2018. https://acmedsci.ac.uk/policy/policy-projects/multimorbidity
- 70.Astolfi R, Lorenzoni L, Oderkirk J. Organisation for Economic Co-operation and Development; Paris: 2012. A comparative analysis of health forecasting methods. [Google Scholar]
- 71.Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45:431–435. doi: 10.1093/ageing/afw044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Office for National Statistics Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2019. June 24, 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/latest
- 73.Morris M, Woods LM, Rachet B. A novel ecological methodology for constructing ethnic-majority life tables in the absence of individual ethnicity information. J Epidemiol Community Health. 2015;69:361–367. doi: 10.1136/jech-2014-204210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gruer L, Cézard G, Clark E, et al. Life expectancy of different ethnic groups using death records linked to population census data for 4·62 million people in Scotland. J Epidemiol Community Health. 2016;70:1251–1254. doi: 10.1136/jech-2016-207426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rees PH, Wohland PN, Norman PD. The estimation of mortality for ethnic groups at local scale within the United Kingdom. Soc Sci Med. 2009;69:1592–1607. doi: 10.1016/j.socscimed.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 76.Francis-Devine B, Foley N. Women and the economy. March 4, 2020. https://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN06838
- 77.Solomi VL, Casiday RE. In sickness and in health: the strains and gains of caring for a chronically ill or disabled spouse. Chronic Illn. 2017;13:75–87. doi: 10.1177/1742395316664960. [DOI] [PubMed] [Google Scholar]
- 78.Pickard L. Substitution between formal and informal care: a ‘natural experiment’ in social policy in Britain between 1985 and 2000. Ageing Soc. 2012;32:1147–1175. [Google Scholar]
- 79.Coulmas F. Routledge; London: 2007. Population decline and ageing in Japan—the social consequences. [Google Scholar]
- 80.Nursing and Midwifery Council Annual reports and accounts 2017–2018 and strategic plan 2018–2019. Nov 5, 2018. https://www.nmc.org.uk/about-us/reports-and-accounts/annual-reports-and-accounts/
- 81.Kenny S. Restricted Certificates of Sponsorship: key points from data released by UK Visas and Immigration. June 11, 2018. https://www.eversheds-sutherland.com/global/en/what/articles/index.page?ArticleID=en/Employment_and_labour_law/Restricted-certificates-of-sponsorship-key-points
- 82.Patel P. Home Secretary letter to the MAC in response to the shortage occupation lists report. Oct 23, 2020. https://www.gov.uk/government/publications/letter-to-the-mac-on-the-shortage-occupation-lists-report/home-secretary-letter-to-the-mac-in-response-to-the-shortage-occupation-lists-report-accessible-version
- 83.Drummond C. Cuts to addiction services are a false economy. BMJ. 2017;357 doi: 10.1136/bmj.j2704. [DOI] [PubMed] [Google Scholar]
- 84.Office for National Statistics Overview of the UK population: January 2021. Jan 14, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021
- 85.Kingston A, Robinson L, Booth H, Knapp M, Jagger C. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018;47:374–380. doi: 10.1093/ageing/afx201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gomes B, Higginson IJ. Where people die (1974–2030): past trends, future projections and implications for care. Palliat Med. 2008;22:33–41. doi: 10.1177/0269216307084606. [DOI] [PubMed] [Google Scholar]
- 87.Wanless D. HM Treasury; London: 2002. Securing our future health: taking a long-term view, final report. [Google Scholar]
- 88.NHS England NHS Long-Term Plan. Jan 7, 2019. https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/
- 89.Suhrcke M, McKee M, Arce RS, Tsolova S, Mortensen J. Investment in health could be good for Europe's economies. BMJ. 2006;333:1017–1019. doi: 10.1136/bmj.38951.614144.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mackenbach JP, Karanikolos M, McKee M. The unequal health of Europeans: successes and failures of policies. Lancet. 2013;381:1125–1134. doi: 10.1016/S0140-6736(12)62082-0. [DOI] [PubMed] [Google Scholar]
- 91.Williams R, Alexander G, Aspinall R, et al. Gathering momentum for the way ahead: fifth report of the Lancet Standing Commission on Liver Disease in the UK. Lancet. 2018;392:2398–2412. doi: 10.1016/S0140-6736(18)32561-3. [DOI] [PubMed] [Google Scholar]
- 92.McCambridge J, Daube M, McKee M. Brussels Declaration: a vehicle for the advancement of tobacco and alcohol industry interests at the science/policy interface? Tob Control. 2019;28:7–12. doi: 10.1136/tobaccocontrol-2018-054264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Knai C, Petticrew M, Durand MA, Eastmure E, Mays N. Are the Public Health Responsibility Deal alcohol pledges likely to improve public health? An evidence synthesis. Addiction. 2015;110:1232–1246. doi: 10.1111/add.12855. [DOI] [PubMed] [Google Scholar]
- 94.Public Health England Salt reduction programme. Dec 19, 2018. https://publichealthengland.exposure.co/salt-reduction-programme
- 95.McKee M, Stuckler D. Revisiting the corporate and commercial determinants of health. Am J Public Health. 2018;108:1167–1170. doi: 10.2105/AJPH.2018.304510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mackenbach J. Successes and failures of health policy in Europe. Eur J Public Health. 2013;23(suppl 1):23. [Google Scholar]
- 97.McKee M, Reeves A, Clair A, Stuckler D. Living on the edge: precariousness and why it matters for health. Arch Public Health. 2017;75:13. doi: 10.1186/s13690-017-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Reeves A, McKee M, Mackenbach J, Whitehead M, Stuckler D. Introduction of a national minimum wage reduced depressive symptoms in low-wage workers: a quasi-natural experiment in the UK. Health Econ. 2017;26:639–655. doi: 10.1002/hec.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.UK Low Pay Commission Non-compliance and enforcement of the National Minimum Wage. May 7, 2020. https://www.gov.uk/government/publications/non-compliance-and-enforcement-of-the-national-minimum-wage#:~:text=Enforcement%20of%20the%20National%20Minimum%20Wage,-The%20Department%20for&text=Workers%20can%20complain%20about%20underpayment,helpline%20on%200300%20123%201100
- 100.WHO Sustainable development in Wales and other regions in Europe—achieving health and equity for present and future generations. 2017. http://www.euro.who.int/en/publications/abstracts/sustainable-development-in-wales-and-other-regions-in-europe-achieving-health-and-equity-for-present-and-future-generations-2017
- 101.Welsh Government Public Health (Wales) Act 2017. July 3, 2017. http://www.legislation.gov.uk/anaw/2017/2/contents/enacted
- 102.Castleden M, McKee M, Murray V, Leonardi G. Resilience thinking in health protection. J Public Health (Oxf) 2011;33:369–377. doi: 10.1093/pubmed/fdr027. [DOI] [PubMed] [Google Scholar]
- 103.Fahy N, Hervey T, Greer S, et al. How will Brexit affect health services in the UK? An updated evaluation. Lancet. 2019;393:949–958. doi: 10.1016/S0140-6736(19)30425-8. [DOI] [PubMed] [Google Scholar]
- 104.Roman-Urrestarazu A, Yang J, Robertson R, et al. Brexit threatens the UK's ability to tackle illicit drugs and organised crime: what needs to happen now? Health Policy. 2019;123:521–525. doi: 10.1016/j.healthpol.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 105.Horton R. 1st edn. Polity Press; Cambridge, UK: 2020. The COVID-19 catastrophe: what's gone wrong and how to stop it happening again. [Google Scholar]
- 106.Wilkinson E. RECOVERY trial: the UK COVID-19 study resetting expectations for clinical trials. BMJ. 2020;369 doi: 10.1136/bmj.m1626. [DOI] [PubMed] [Google Scholar]
- 107.Rajan S, Comas-Herrera A, Mckee M. Did the UK Government really throw a protective ring around care homes in the COVID-19 pandemic? J Long Term Care. 2020 doi: 10.31389/jltc.53. published online Nov 11. [DOI] [Google Scholar]
- 108.Roberts CM, Levi M, Schilling R, Lim WS, Grocott MPW, McKee M. Covid-19: a complex multisystem clinical syndrome. May 1, 2020. https://blogs.bmj.com/bmj/2020/05/01/covid-19-a-complex-multisystem-clinical-syndrome/ [DOI] [PMC free article] [PubMed]
- 109.Mansfield KE, Mathur R, Tazare J, et al. COVID-19 collateral: indirect acute effects of the pandemic on physical and mental health in the UK. medRxiv. 2020 doi: 10.1101/2020.10.29.20222174. published on Oct 30. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lai AG, Pasea L, Banerjee A, et al. Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency. medRxiv. 2020 doi: 10.1101/2020.05.27.20083287. published on June 1. (preprint). [DOI] [Google Scholar]
- 111.Campbell D. Millions in UK miss cancer screenings, tests and treatments due to Covid-19. June 1, 2020. https://www.theguardian.com/society/2020/jun/01/millions-in-uk-miss-cancer-screenings-tests-and-treatments-due-to-covid-19
- 112.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368 doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 113.McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med. 2020;26:640–642. doi: 10.1038/s41591-020-0863-y. [DOI] [PubMed] [Google Scholar]
- 114.Keown OP, Warburton W, Davies SC, Darzi A. Antimicrobial resistance: addressing the global threat through greater awareness and transformative action. Health Aff (Millwood) 2014;33:1620–1626. doi: 10.1377/hlthaff.2014.0383. [DOI] [PubMed] [Google Scholar]
- 115.Le Quéré C, Jackson RB, Jones MW, et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat Clim Chang. 2020;10:647–653. [Google Scholar]
- 116.Fahy N, Hervey T, Greer S, et al. How will Brexit affect health and health services in the UK? Evaluating three possible scenarios. Lancet. 2017;390:2110–2118. doi: 10.1016/S0140-6736(17)31926-8. [DOI] [PubMed] [Google Scholar]
- 117.McKee M. Covid-19 vaccine wars: developing the AstraZeneca vaccine was a triumph, but then things went wrong. March 26, 2021. https://blogs.bmj.com/bmj/2021/03/26/vaccine-wars-developing-the-astrazeneca-vaccine-was-a-triumph-but-then-things-went-wrong/
- 118.Green L, Edmonds N, Morgan L, et al. The public health implications of Brexit in Wales: a health impact assessment approach. Jan 21, 2019. http://www.wales.nhs.uk/sitesplus/888/news/50275
- 119.van Schalkwyk MCI, Jarman H, Hervey T, Wouters OJ, Barlow P, McKee M. Risks to health and the NHS in the post-Brexit era. BMJ. 2020;369 doi: 10.1136/bmj.m2307. [DOI] [PubMed] [Google Scholar]
- 120.British Medical Association Beyond Brexit—international trade and health. Sept 17, 2018. https://www.bma.org.uk/collective-voice/influence/europe/brexit/bma-brexit-briefings/beyond-brexit-international-trade-and-health
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.