Abstract
Introduction:
Sports injuries are known to present a high risk of spinal trauma. We hypothesized that different sports predispose to different injuries and injury severities.
Methods:
We conducted a retrospective cohort analysis of adult patients who experienced a sports-related traumatic spinal injury (TSI), including spinal fractures and spinal cord injuries (SCIs), encoded within the National Trauma Data Bank from 2011-2014. We used multiple imputation for missing data and estimated multivariable linear and logistic regression models.
Results:
We included 12,031 cases of TSI, which represented 15% of all sports-related trauma. The majority of patients with TSI were male (82%) and the median age was 48 years (interquartile range [IQR]32-57). The most frequent mechanisms of injury in this database were cycling injuries (81%), ski and snowboarding accidents (12%), aquatic sports injuries (3%), and contact sports (3%). Spinal surgery was required during initial hospitalization for 9.1% of TSI patients.
Compared to non-TSI sports-related trauma, TSIs were associated with an average 2.3 day increase in length of stay (95% CI 2.1-2.4;p<0.001) and discharge to or with rehabilitative services (adjusted odds [aOR] 2.6; 95% CI 2.4-2.7;p<0.001). Among sports injuries, TSIs were the cause of discharge to or with rehabilitative services in 32% of cases.
SCI was present in 15% of cases with TSI. Within sports-related TSIs, the rate of SCI was 13% for cycling injuries compared to 41% and 50% for contact sports and aquatic sports injuries, respectively. Patients experiencing SCI had longer length of stay (7.0 days longer; 95% CI 6.7-7.3) and higher likelihood of adverse discharge disposition (aOR 9.69; 95% CI 8.72-10.77) compared to patients with TSI but without SCI.
Conclusion:
Of patients with sports-related trauma discharged to rehab, one-third had TSIs. Cycling injuries were the most common cause, suggesting that policies to make cycling safer may reduce TSI.
Keywords: traumatic spinal injury, sports-related injury, traumatic spinal cord injury
Introduction
Traumatic spine injuries (TSIs) in adults can result in significant morbidity and mortality. These acute injuries to the spinal cord and/or surrounding vertebral column have been estimated to occur globally at a rate of 10.5 cases per 100,000 persons annually based on meta-analysis of multiple cohort studies.1
Neurologic recovery depends not only on injury severity, but also on injury mechanism.2 TSIs in adults most commonly result from road accidents and falls.1 These mechanisms of injury are also most frequently implicated in the subset of TSIs that involve the spinal cord.3, 4
In particular, the morbidity and mortality of TSIs resulting from motor vehicle accidents has already been characterized from multiple perspectives.5-9 However, comparatively little is known about morbidity and mortality of sports-related TSIs.
Sports-related TSIs have recently been studied in the pediatric population.10 However, pediatric patients are thought to be more prone to cervical TSI than adults.11, 12 Additionally, adult TSI patients are less likely to recover than pediatric TSI patients.13 As sports-related trauma increases in prevalence,14 it is important to understand the effect of TSI on morbidity and mortality in adult patients with sports-related trauma.
This study aims to determine the most common mechanisms of injury in adult sport-related TSI, the need for surgical intervention by mechanism of injury, and the clinical burden between TSI and non-TSI sports injuries to help guide clinical management and policy design.
Methods
Study Design
We used the prospectively collected and validated National Trauma Data Bank (NTDB) databases from years 2011 through 2014 to conduct a nationwide, multicenter, retrospective cohort study. This database includes information regarding the initial hospitalization of patients presenting with traumatic injuries. The exposures of interest were TSI with and without spinal cord involvement in adult patients whose trauma was precipitated by participating in any sports-related activity.
Inclusion and Exclusion Criteria
Inclusion criteria were 1) age of at least 18 years at the time of injury; 2) an International Classification of Diseases 9 (ICD-9) external cause of injury code corresponding to a sports-related injury; 3) an ICD-9 diagnosis code for spinal fracture and/or cord injury (as in Appendix 1 and shown previously10). Categories of sports-related injuries included cycling, contact sports, skiing/snowboarding, skateboarding/rollerblading, watersport/swimming, and other. Injuries to individuals struck by motorized vehicles while participating in a sports-related activity were included. However, injuries to individuals operating recreational motorized vehicles were not included. The contact sports category encompassed a variety of mechanisms of injury including pushing, shoving, and physical contact with players or objects taking place in any sport, including American football and rugby.
Statistical Analysis
Our primary outcome of interest was discharge disposition, accounting for both the setting to which the patient was discharged as well as any requirement for rehabilitation with the following categories. Discharge disposition categories included home with no rehabilitation services, home with rehabilitation services, to a short or long-term rehabilitation facility, and transfer to another inpatient hospital. We used this outcome measure as a proxy for the functional status at the time of discharge. We assumed that patients who required a hospital transfer likely required a higher level of care than could be provided at the initial facility and thus would require rehabilitation after discharge. We also evaluated secondary outcomes that included requirement for spinal surgery as defined by ICD-9 procedural codes for laminectomy and/or vertebral fracture repair, requirement for intensive care unit (ICU) admission, length of hospital stay, and mortality during the documented initial hospitalization.
We performed descriptive statistical analyses using t-tests for continuous variables and Chi-squared tests for categorical variables. We used multivariable logistic regression to generate adjusted odds ratios (aORs) characterizing the relationship between various spinal injuries and outcome measures. We also used multivariable linear regression for analysis of continuous outcome variables. Both linear and logistic models were adjusted for age (with linear and quadratic terms), sex, race, ethnicity, insurance type (including Medicare, Medicaid, other governmental plans, no fault automobile, private/commercial insurance, self-pay, and other non-governmental plans), geographic region (Midwest, South, West, and Northeast), obesity, smoking, diabetes, steroid use, Glasgow Coma Score, hypotension (systolic blood pressure under 90) at presentation, concomitant non-spinal injuries diagnosed in abbreviated injury scheme (AIS) zones (categorized to head, face, neck, thoracic, abdominal, upper extremity, and lower extremity injuries), and ICD-9 coding for specific concomitant injuries. We aimed to account for the potential confounding effects of demographics, comorbidities, and injury severity. Covariate information was extracted from the NTDB. All statistical analyses were conducted using R version 3.3.3 (The R Project).
Missing Data
We used multiple imputation via the R “amelia()” package. This package performs multiple ratio imputation via a bootstrapping algorithm using expectation-maximization.15 We performed 10 iterations of the multiple imputation to construct 10 imputed datasets containing demographic information, clinical characteristics, procedures performed during the initial hospitalization, and dispositional information. We generated all statistical estimates from pooling these 10 imputed datasets.
Results
Demographics
We included 80,040 cases of adult sports-related trauma, and 12,031 (15%) of these cases involved sports-related TSI (Table 1). Sports-related TSI patients had a median age of 48 (IQR 32-57). This trended towards patients being slightly older than most adults presenting with any type of sports related injury (median age 43, IQR 27-55). Sports-related TSI patients were predominantly male (81.6%) and white (77.8%), which was comparable to demographics of the full sports-related injury cohort. The plurality of sports-related TSI patients had private insurance coverage (43.4%).
Table 1: Demographics.
The demographic breakdown of the sports-related TSI and overall sports-related trauma cohorts were similar in most respects.
| Total (N = 80040) |
TSI (N = 12031) |
Non-TSI (N = 68009) |
||||
|---|---|---|---|---|---|---|
| Age | Mean | SD | Mean | SD | Mean | SD |
| 43 | 27 | 55 | 48 | 32 | 57 | |
| Sex | N | % | N | % | N | % |
| Male | 63425 | 79.2 | 9817 | 81.6 | 53608 | 78.8 |
| Female | 16575 | 20.7 | 2211 | 18.4 | 14364 | 21.1 |
| Unknown | 40 | 0.0 | 3 | 0.0 | 37 | 0.1 |
| Race | N | % | N | % | N | % |
| White | 59787 | 74.7 | 9366 | 77.8 | 50421 | 74.1 |
| Black/African American | 6416 | 8.0 | 867 | 7.2 | 5549 | 8.2 |
| Asian | 2149 | 2.7 | 290 | 2.4 | 1859 | 2.7 |
| American Indian | 412 | 0.5 | 41 | 0.3 | 371 | 0.5 |
| Pacific Islander | 180 | 0.2 | 22 | 0.2 | 158 | 0.2 |
| Other | 7442 | 9.3 | 886 | 7.4 | 6556 | 9.6 |
| Unknown | 3654 | 4.6 | 559 | 4.6 | 3095 | 4.6 |
| Insurance | N | % | N | % | N | % |
| Private/BCBS Insurance | 34670 | 43.3 | 5217 | 43.4 | 29453 | 43.3 |
| Medicare | 6790 | 8.5 | 1069 | 8.9 | 5721 | 8.4 |
| Medicaid | 7094 | 8.9 | 1013 | 8.4 | 6081 | 8.9 |
| Self-Pay | 13466 | 16.8 | 1589 | 13.2 | 11877 | 17.5 |
| No Fault Automobile | 4522 | 5.6 | 1043 | 8.7 | 3479 | 5.1 |
| Other Government Plan | 2851 | 3.6 | 430 | 3.6 | 2421 | 3.6 |
| Other Non-Governmental Plan | 3147 | 3.9 | 494 | 4.1 | 2653 | 3.9 |
| Unknown | 7163 | 8.9 | 1119 | 9.3 | 6044 | 8.9 |
Mechanism of Injury
Among sports-related TSI patients, the mechanisms of injury included cycling (80.9%), skiing/snowboarding (11.6%), watersports/swimming (2.9%), contact sports (2.8%), skateboarding/rollerblading (1.3%), and other (0.6%) (Figure 1A). The prevalence of spinal cord injury varied considerably across mechanisms of injury (Figure 1B). Watersports/swimming (48.9%) and contact sports (41.3%) had the highest prevalence of traumatic spinal cord injury.
Figure 1A: Mechanisms of Injury.
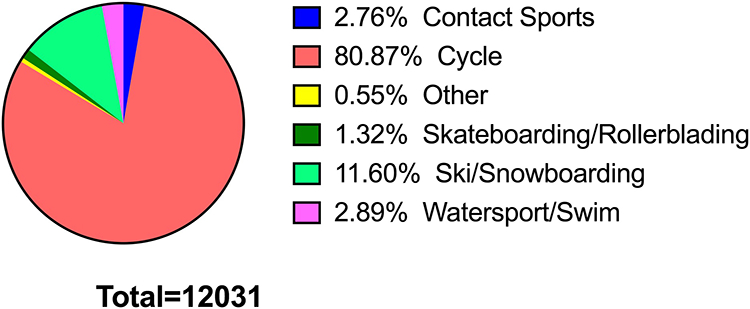
The majority of adult sports-related TSI were attributed to cycling related injuries, with skiing/snowboarding, watersports/swimming, contact sports, skateboarding/rollerblading, and other mechanisms of injury also reflected in this cohort.
Figure 1B: Spinal Cord Injury Prevalence by Mechanism of Injury.
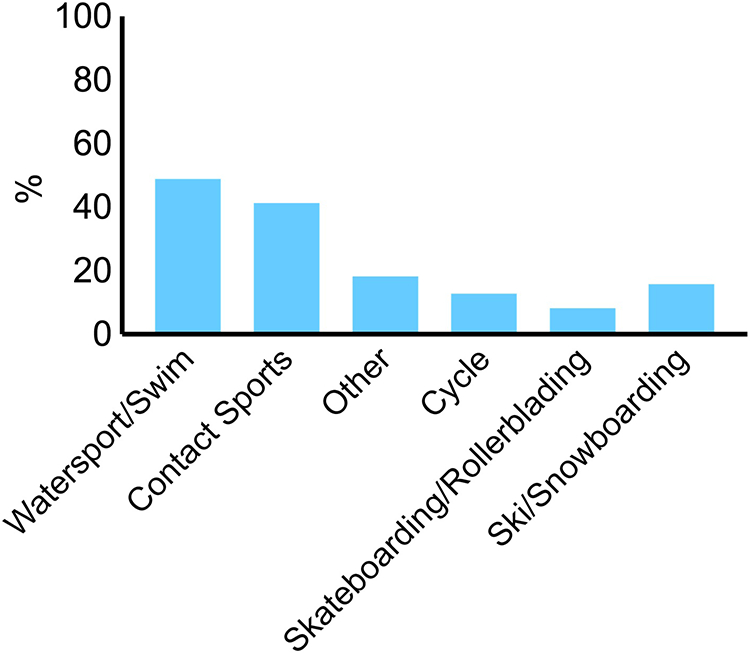
Prevalence of traumatic spinal cord injury among patients with sports-related TSI varied based on mechanism of injury. Traumatic spinal cord injuries were most prevalent in patients with watersports/swimming and contact sports-related injuries.
Overall, most sports-related TSIs could be traced back to motor vehicle accidents (81.0%) and falls (13.7%). Importantly, the individuals participating in sports-related activities were not operating the motor vehicles in question. This mirrored the overall breakdown of sports-related injuries among adults, with 75.6% attributable to motor vehicle accidents and 18.6% attributable to falls.
Clinical Characteristics at Presentation
TSI patients presented with traumatic spinal cord injury (TSCI) in 14.9% of cases. Cervical spine fractures were the most common, occurring among 40.2% of TSI patients. Thoracic (35.8%) and lumbar (29.4%) fractures were also fairly prevalent, with many patients presenting with fractures at multiple spinal levels (3.2%). Among all TSI patients, cervical spine TSCI was also most prevalent (11.6%), followed by thoracic (2.5%) and lumbar SCI (0.9%).
Among sports-related TSI patients, concomitant TBI (38.5%), lower extremity (38.8%), thoracic (37.5%), and upper extremity (37.1%) injuries were the most prevalent. The median Glasgow Coma Score of sports-related TSI patients at presentation was 15 (IQR 15-15), while the median Injury Severity Score was 12 (IQR 8-18).
Hospital Course
Upon admission to the hospital, 9.1% (N=1094) of patients with sports-related TSI required spinal surgery, defined as laminectomy and/or vertebral fracture repair. There was no significant difference in likelihood of undergoing spinal surgery as stratified by mechanism of injury in comparison to contact sports-related TSI (Figure 2).
Figure 2: Odds of Spinal Surgery during Initial Hospitalization by Mechanism of Injury.
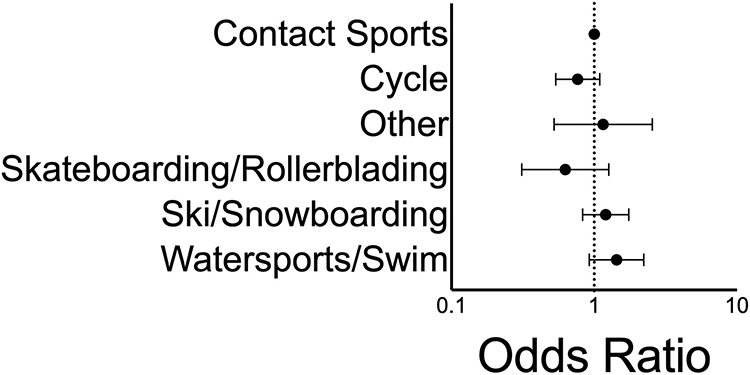
There was no significant difference in likelihood of undergoing spinal surgery, defined as laminectomy and/or vertebral fracture repair, during initial hospitalization as stratified by mechanism of injury. Patients with contact sports-related TSI were the reference group for this analysis.
Male sex (aOR 1.37; 95% CI 1.15-1.64), obesity (aOR 1.58; 95% CI 1.14-2.22), and steroid use prior to admission to the hospital with TSI (aOR 5.53; 95% CI 1.72-17.72) were all associated with increased likelihood of undergoing spinal surgery during the initial hospitalization. Concomitant injuries were also associated with an increased likelihood of spinal surgery, including neck injury (aOR 1.82; 95% CI 1.35-2.45) and thoracic injury (aOR 1.18; 95% CI 1.02-1.36). In contrast, upper extremity injury (aOR 0.80; 95% CI 0.69-0.93), lower extremity injury (aOR 0.74; 95% Ci 0.64-0.85), and traumatic brain injury (aOR 0.60; 95% CI 0.51-0.71) were all associated with reduced odds of undergoing spinal surgery during initial hospitalization.
Length of stay among patients with contact sports-related TSI (median 4 days, IQR 2-8 days) was greater than that of all patients with sports-related injuries (median 2 days, IQR 1-4 days). These differences were statistically significant in an adjusted model, with sports-related TSI patients likely to stay 2.3 days longer (95% CI 2.1-2.4) than patients with non-TSI sports-related injuries (Figure 3). Additionally, patients with sports-related TSCI were likely to stay 7.0 days longer (95% CI 6.7-7.3) than patients with non-TSI sports-related injuries in the same adjusted model.
Figure 3: Length of Stay.
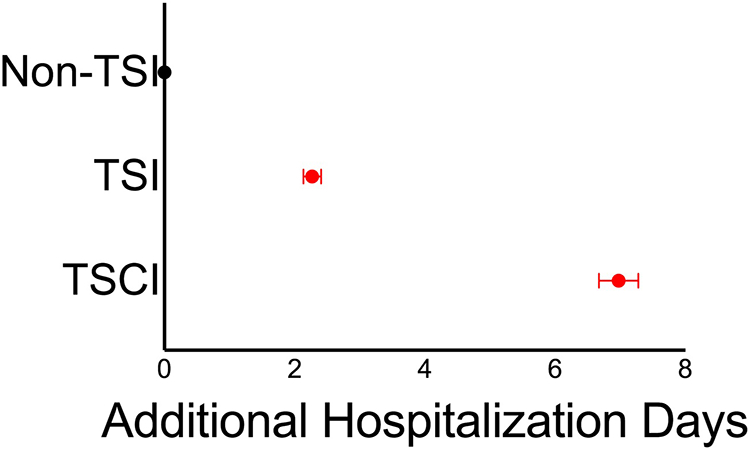
In an adjusted model, patients with sports-related TSI and TSCI had significantly longer hospital stays than patients with non-TSI sports-related injuries.
Hospital Disposition
In comparison to patients with sports-related non-TSI injuries, patients with sports-related TSI were significantly more likely to require ICU care during their initial hospitalization (aOR 2.06; 95% CI 1.95-2.18) (Figure 4). Overall, 17.1% of patients with sports-related injuries experienced adverse discharge disposition, as compared to 32.1% of patients with sports-related TSI. This was defined as transfer to another hospital, discharge to a rehabilitation facility, or discharge home with rehabilitative services. Patients with sports-related TSI were more likely to experience adverse discharge in an adjusted model (aOR 2.56; 95% CI 2.44-2.68) as well. Covariates associated with adverse discharge in the multivariable model included TBI (aOR 1.33; 95% CI 1.27-1.40), skull base fracture (aOR 2.48; 95% CI 2.31-2.66), abdominal injury (aOR 1.32; 95% CI 1.23-1.40), thoracic injury (aOR 1.32; 95% CI 1.26, 1.38), lower extremity injury (aOR 1.82; 95% CI 1.57-2.12), diabetes mellitus (aOR 1.36; 95% CI 1.24-1.49), and obesity (aOR 1.23; 95% CI 1.10-1.39). Interestingly, private insurance coverage (aOR 0.83; 95% CI 0.77-0.90), self-pay insurance coverage (aOR 0.64; 95% CI 0.58-0.69), upper extremity injury (aOR 0.86; 95% CI 0.83-0.90), facial injury (aOR 0.86; 95% CI 0.82-0.90), and smoking (aOR 0.81; 95% CI 0.76-0.86) all appeared protective against adverse discharge in this analysis. Age, sex, race, geographic region, steroid use, and other insurance statuses were not significantly associated with adverse discharge.
Figure 4: Discharge Disposition.
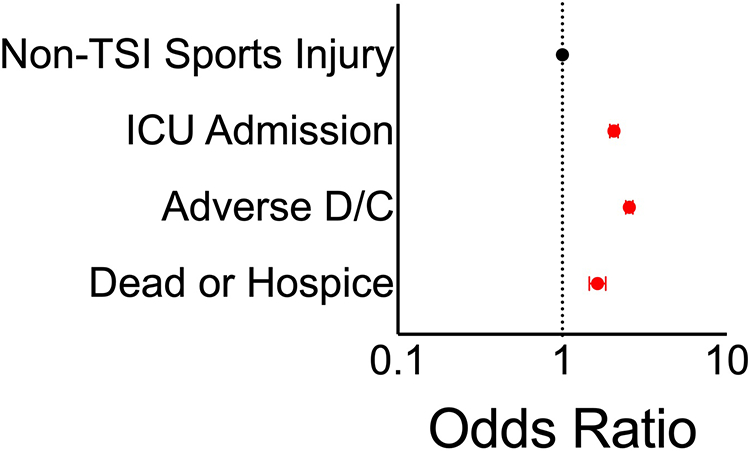
Compared to patients with non-TSI sports-related injuries, patients with sports-related TSI were significantly more likely to require ICU care, to experience adverse discharge, and to die or require hospice care during the initial hospital admission.
Patients with sports-related TSI were also more likely to die during their initial hospitalization (aOR 1.46; 95% CI 1.64-1.84), though the prevalence of deaths overall was low at 2.1% among patients with all sports-related injuries and 4.6% among patients with sports-related TSI.
Compared to patients with TSI, patients with TSCI were also significantly more likely to require ICU care (aOR 5.14; 95% CI 4.50-5.87) as compared to patients with non-TSI sports-related injuries. Patients with TSCI were also more likely to experience adverse discharge (aOR 9.69; 95% CI 8.72-10.77) and death during initial hospitalization (aOR 4.23; 95% CI 3.45-5.18).
Discussion
TSI is a serious traumatic event that can negatively impact patient health and post-hospitalization outcomes; trauma outcomes worsen with increased age. The number of reported TSIs in the adult population continues to increase annually within the United States.16-20 The average adult presenting with TSI between 2007 and 2009 was 50.4 years old and predominantly male.19
Factors significantly associated with adverse discharge include serious concomitant injuries, such as skull base fracture and TBI, which present major challenges to patient recovery. Similarly, lower extremity injury and obesity may limit patient mobility and increase the risk of venous thrombosis. The association of obesity with adverse discharge may also indicate that patients with a predisposition to back pain are at increased risk of experiencing TSI and/or TSCI 21, 22. However, the male predominance in this cohort does not reflect the increased population prevalence of back pain among women.23 The protective effect between private insurance coverage or self-pay insurance coverage against adverse discharge may reflect improved access to healthcare and therefore fewer pre-existing conditions that could complicate recovery from TSI. However, it is unclear how this reasoning could explain the observed protective effect of smoking, so further prospective investigation is required to evaluate the generalizability of these findings. Age, sex, and race had no significant association with, and are therefore not important predictors of hospital disposition.
The prevalence of deaths upon hospitalization in sports-related TSI was significantly higher than mortality in patients with all sports-related injuries. This may be attributed to the clinical characteristics of patients with sports-related TSI, as location and type of injury impacts patient outcome and type of care needed. Sports-related TSI patients were more likely to present with concomitant TBI, lower extremity, thoracic and upper extremity injuries; TBIs with concomitant injuries have been shown to be associated with higher mortality.24, 25
The most common form of TSI in adults is vertebral fracture, most commonly in the cervical region.26, 27 We show that while TSI patients commonly present with cervical fractures, they also present with thoracic and lumbar fractures at similar rates. Understanding the mechanics that produce these injuries after impact can inform the type of protective gear needed for athletes participating in different sports.28-31
The prevalence of TSCI varied between sporting activities, with watersports and contact sports resulting in the highest prevalence of traumatic spinal cord injury within this cohort. Previous studies have identified diving as the primary source of water sports-related injury, highlighting how the lack of protective equipment in this activity and related sports leaves patients more vulnerable to devastating neurologic injury.16, 32 Rugby has similarly been identified as a leading contributor to TSCI, and the relatively high frequency of diving and rugby-related TSCI holds across data from many different countries.33 Low public awareness regarding the risks inherent to these sports may also contribute to the high prevalence of sports-related TSIs, and existing interventions center on improving participant education.34 Current research on sports-related neurological trauma largely centers on high-contact sports such as football and rugby, leaving lower-contact sports understudied by comparison.1 These existing studies provide a model for implementing evidence-based interventions to prevent sports-related trauma; for instance, identifying dangerous head-first tackle techniques in football prompted new regulations prohibiting this behavior at a local and national level.32 Greater funding should be allocated to developing similar interventions for the sports identified in this study.
Notably, most sports-related TSIs were from motor-related cycling accidents where the patient was not operating the vehicle (81.0%). Although many cities with high volume traffic acknowledge the importance of helmet safety and have initiated measures to curb motor vehicle related cycling accidents, including protected bike lanes and helmet laws, there is still a clear disparity between policy and TSI occurrence.35-38 Previous studies reveal a discrepancy between bikers acknowledging the importance of helmet use versus actually choosing to wear helmets, which indicates that helmet advocacy initiatives might improve rates of helmet use.39, 40 This in conjunction with interventions such as improving bike lanes and educating motorists may help to reduce the incidence of cycling-related TSIs.
Falls were identified as the second-most common origin of sports-related TSIs. Though the cause of falls can vary drastically by sport, emphasis on proper technique and maintenance of sports-related surfaces such as roads and fields are two methods to alleviate the severity of falls.41
In addition to causing considerable morbidity among patients, TSI and TSCI in particular can result in tremendous financial burdens for patients and healthcare systems. During initial hospitalization, the cost of receiving treatment and of any required rehabilitative services is most immediate, costing patients on the order of $20,000-$30,000 per year according to published estimates with variation depending on the nature of the injury and patient characteristics. 42, 43 However, indirect costs due to changes in employment status and lost earnings also merit consideration at both the individual and societal level and can account for several million dollars over the lifetime of a single injured individual.44, 45 These financial considerations provide another motivation for reducing sports-related TSI.
Clinical Significance
Strengths:
Using the multicenter NTDB database, we generated a large and diverse cohort of TSI patients, lending generalizability to the trends reported here. The demographics of this study’s cohort – disproportionately male with an average age of 48 years old – mirror those of the average adult TSI patient in the general population. While the conclusions of this study may not be generalizable to younger cohorts, they encapsulate the highest-risk population for TSI nationwide. These data can therefore augment evidence-based funding, advocacy, and patient-care decision-making.
Limitations:
Retrospectively analyzing an aggregated dataset introduces several important limitations to our analysis. While multiple imputation allows estimation of values for missing data, bias can be introduced if the causes of missing data are not considered in the imputation model. Inclusion in the NTDB database requires initial hospitalization data, which necessarily excludes patients who succumb to their injuries before hospitalization can occur. As a result, our analysis of those sports-related TSIs that are not immediately fatal is limited. Additionally, utilizing ICD-9 codes to determine diagnoses introduces the possibility for bias. As compared to some published studies, the proportion of patients with TSI identified to have TSCI in our study was considerably lower, though overestimation of TSCI in TSI patients due to coding limitations has also been described previously. 46, 47 Previous studies also were not restricted to sports-related TSI, which may encompass a non-representative subset of all patients presenting with TSI. Our approach, considering all ICD-9 codes for each patient entry in the National Trauma Data Bank, is consistent with previously published conservative approaches for estimating TSCI incidence.48 Finally, the retrospective examination of discharge disposition does not facilitate analysis of long-term prognosis and survival. In all, these limitations underscore the necessity for future prospective study of patient outcomes after sports-related TSI.
Conclusion
In this study, we highlight the importance of preventing sports-related TSI in the adult population, as well as illuminate factors associated with adverse discharge and poor hospital disposition. Patients with sports-related TSI were significantly more likely to require ICU care and to die during hospitalization, underscoring the devastating potential of such injuries to patient health. Cycling injuries comprised the majority of sports-related TSIs; improving policies and education regarding cyclist safety would likely prove effective interventions.
Supplementary Material
Disclosures:
The authors acknowledge support from the following grants: National Institute of General Medical Sciences T32 GM007753 (BMH) and National Institutes of Health T32 CA009001 (D.J.C.).
Dr. Chi is a consultant for K2M and received clinical or research support from Spineology for the study described. Dr. Groff is a consultant for DePuy Spine, NuVasive Spine, and SpineArt.
Footnotes
Previous Presentations: These findings were presented in poster form at the Congress of Neurological Surgeons 2019 Annual Meeting in San Francisco, CA and in oral presentation format at the New England Neurosurgical Society 2019 Annual Meeting in Brewster, MA.
References
- 1.Kumar R, Lim J, Mekary RA, et al. Traumatic Spinal Injury: Global Epidemiology and Worldwide Volume. World Neurosurg. May 2018;113:e345–e363. doi: 10.1016/j.wneu.2018.02.033 [DOI] [PubMed] [Google Scholar]
- 2.Khorasanizadeh M, Yousefifard M, Eskian M, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine. Feb 15 2019:1–17. doi: 10.3171/2018.10.SPINE18802 [DOI] [PubMed] [Google Scholar]
- 3.Mirzaeva L, Gilhus NE, Lobzin S, Rekand T. Incidence of adult traumatic spinal cord injury in Saint Petersburg, Russia. Spinal Cord. Mar 6 2019;doi: 10.1038/s41393-019-0266-4 [DOI] [PubMed] [Google Scholar]
- 4.Kudo D, Miyakoshi N, Hongo M, et al. An epidemiological study of traumatic spinal cord injuries in the fastest aging area in Japan. Spinal Cord. Jun 2019;57(6):509–515. doi: 10.1038/s41393-019-0255-7 [DOI] [PubMed] [Google Scholar]
- 5.Han GM, Newmyer A, Qu M. Seat belt use to save face: impact on drivers' body region and nature of injury in motor vehicle crashes. Traffic Inj Prev. 2015;16(6):605–10. doi: 10.1080/15389588.2014.999856 [DOI] [PubMed] [Google Scholar]
- 6.Wang H, Liu X, Zhao Y, et al. Incidence and pattern of traumatic spinal fractures and associated spinal cord injury resulting from motor vehicle collisions in China over 11 years: An observational study. Medicine (Baltimore). Oct 2016;95(43):e5220. doi: 10.1097/MD.0000000000005220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silva L, Fernanda Bellolio M, Smith EM, Daniels DJ, Lohse CM, Campbell RL. Motocross-associated head and spine injuries in adult patients evaluated in an emergency department. Am J Emerg Med. Oct 2017;35(10):1485–1489. doi: 10.1016/j.ajem.2017.04.058 [DOI] [PubMed] [Google Scholar]
- 8.McCoy CE, Loza-Gomez A, Lee Puckett J, et al. Quantifying the Risk of Spinal Injury in Motor Vehicle Collisions According to Ambulatory Status: A Prospective Analytical Study. J Emerg Med. Feb 2017;52(2):151–159. doi: 10.1016/j.jemermed.2016.09.024 [DOI] [PubMed] [Google Scholar]
- 9.Ozdol C, Gediz T, Aghayev K. Cranial and spinal injuries in motorcycle accidents: A hospital-based study. Ulus Travma Acil Cerrahi Derg. Mar 2019;25(2):167–171. Cranial and spinal injuries in motorcycle accidents: A hospital-based study. doi: 10.14744/tjtes.2019.46116 [DOI] [PubMed] [Google Scholar]
- 10.Gupta S, Hauser BM, Zaki MM, et al. Morbidity after traumatic spinal injury in pediatric and adolescent sports-related trauma. J Neurosurg Spine. Dec 27 2019:1–7. doi: 10.3171/2019.10.Spine19712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). May 1992;17(5):528–40. [DOI] [PubMed] [Google Scholar]
- 12.Junewick JJ. Cervical spine injuries in pediatrics: are children small adults or not? Pediatr Radiol. Apr 2010;40(4):493–8. doi: 10.1007/s00247-009-1527-8 [DOI] [PubMed] [Google Scholar]
- 13.Parent S, Mac-Thiong JM, Roy-Beaudry M, Sosa JF, Labelle H. Spinal cord injury in the pediatric population: a systematic review of the literature. J Neurotrauma. Aug 2011;28(8):1515–24. doi: 10.1089/neu.2009.1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanford T, McCulloch CE, Callcut RA, Carroll PR, Breyer BN. Bicycle Trauma Injuries and Hospital Admissions in the United States, 1998-2013. JAMA. Sep 1 2015;314(9):947–9. doi: 10.1001/jama.2015.8295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Honaker JKG, Blackwell M. Amelia II: A Program for Missing Data. Journal of Statitical Software. 2011;45(7):1–47. [Google Scholar]
- 16.Ahuja CS, Wilson JR, Nori S, et al. Traumatic spinal cord injury. Nat Rev Dis Primers. Apr 27 2017;3:17018. doi: 10.1038/nrdp.2017.18 [DOI] [PubMed] [Google Scholar]
- 17.Couris CM, Guilcher SJT, Munce SEP, et al. Characteristics of adults with incident traumatic spinal cord injury in Ontario, Canada. Spinal Cord. 2010/January/01 2010;48(1):39–44. doi: 10.1038/sc.2009.77 [DOI] [PubMed] [Google Scholar]
- 18.Furlan JC, Fehlings MG. The Impact of Age on Mortality, Impairment, and Disability among Adults with Acute Traumatic Spinal Cord Injury. Journal of Neurotrauma. 2009/October/01 2009;26(10):1707–1717. doi: 10.1089/neu.2009.0888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selvarajah S, Hammond ER, Haider AH, et al. The Burden of Acute Traumatic Spinal Cord Injury among Adults in the United States: An Update. Journal of Neurotrauma. 2014/February/01 2013;31(3):228–238. doi: 10.1089/neu.2013.3098 [DOI] [PubMed] [Google Scholar]
- 20.Wong AWK, Ng S, Dashner J, et al. Relationships between environmental factors and participation in adults with traumatic brain injury, stroke, and spinal cord injury: a cross-sectional multi-center study. Quality of Life Research. 2017/October/01 2017;26(10):2633–2645. doi: 10.1007/s11136-017-1586-5 [DOI] [PubMed] [Google Scholar]
- 21.Lean ME, Han TS, Seidell JC. Impairment of health and quality of life in people with large waist circumference. Lancet. Mar 21 1998;351(9106):853–6. doi: 10.1016/s0140-6736(97)10004-6 [DOI] [PubMed] [Google Scholar]
- 22.Muthuri S, Cooper R, Kuh D, Hardy R. Do the associations of body mass index and waist circumference with back pain change as people age? 32 years of follow-up in a British birth cohort. BMJ Open. Dec 12 2020;10(12):e039197. doi: 10.1136/bmjopen-2020-039197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang YX, Wang JQ, Kaplar Z. Increased low back pain prevalence in females than in males after menopause age: evidences based on synthetic literature review. Quant Imaging Med Surg. Apr 2016;6(2):199–206. doi: 10.21037/qims.2016.04.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leitgeb J, Mauritz W, Brazinova A, Majdan M, Wilbacher I. Impact of concomitant injuries on outcomes after traumatic brain injury. Arch Orthop Trauma Surg. May 2013;133(5):659–68. doi: 10.1007/s00402-013-1710-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MirHojjat K, Mahmoud Y, Mahsa E, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. Journal of Neurosurgery: Spine SPI. 2019;30(5):683–699. doi: 10.3171/2018.10.SPINE18802 [DOI] [PubMed] [Google Scholar]
- 26.AlHuthaifi F, Krzak J, Hanke T, Vogel LC. Predictors of functional outcomes in adults with traumatic spinal cord injury following inpatient rehabilitation: A systematic review. The Journal of Spinal Cord Medicine. 2017/05/04 2017;40(3):282–294. doi: 10.1080/10790268.2016.1238184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bérubé M, Albert M, Chauny J-M, et al. Development of theory-based knowledge translation interventions to facilitate the implementation of evidence-based guidelines on the early management of adults with traumatic spinal cord injury. Journal of Evaluation in Clinical Practice. 2015/December/01 2015;21(6):1157–1168. doi: 10.1111/jep.12342 [DOI] [PubMed] [Google Scholar]
- 28.Herriman M, Schweitzer ME, Volpp KG. The Need for an Intervention to Prevent Sports Injuries: Beyond “Rub Some Dirt on It”. JAMA Pediatrics. 2019;173(3):215–216. doi: 10.1001/jamapediatrics.2018.4602 [DOI] [PubMed] [Google Scholar]
- 29.Westermann RW, Kerr ZY, Wehr P, Amendola A. Increasing Lower Extremity Injury Rates Across the 2009-2010 to 2014-2015 Seasons of National Collegiate Athletic Association Football: An Unintended Consequence of the “Targeting” Rule Used to Prevent Concussions? The American Journal of Sports Medicine. 2016/December/01 2016;44(12):3230–3236. doi: 10.1177/0363546516659290 [DOI] [PubMed] [Google Scholar]
- 30.Bigdon SF, Gewiess J, Hoppe S, et al. Spinal injury in alpine winter sports: a review. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2019/July/19 2019;27(1):69. doi: 10.1186/s13049-019-0645-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bonfield CM, Shin SS, Kanter AS. Helmets, head injury and concussion in sport. The Physician and Sportsmedicine. 2015/July/03 2015;43(3):236–246. doi: 10.1080/00913847.2015.1039922 [DOI] [PubMed] [Google Scholar]
- 32.Chan CW, Eng JJ, Tator CH, Krassioukov A, Spinal Cord Injury Research Evidence T. Epidemiology of sport-related spinal cord injuries: A systematic review. The journal of spinal cord medicine. 2016;39(3):255–264. doi: 10.1080/10790268.2016.1138601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan CW, Eng JJ, Tator CH, Krassioukov A, Spinal Cord Injury Research Evidence T. Epidemiology of sport-related spinal cord injuries: A systematic review. J Spinal Cord Med. May 2016;39(3):255–64. doi: 10.1080/10790268.2016.1138601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anghelescu A Prevention of diving-induced spinal cord injuries-preliminary results of the first Romanian mass media prophylactic educational intervention. Spinal Cord Ser Cases. 2017;3:17018. doi: 10.1038/scsandc.2017.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bolen JR, Kresnow M, Sacks JJ. Reported bicycle helmet use among adults in the United States. Arch Fam Med. Jan-Feb 1998;7(1):72–7. doi: 10.1001/archfami.7.1.72 [DOI] [PubMed] [Google Scholar]
- 36.Persaud N, Coleman E, Zwolakowski D, Lauwers B, Cass D. Nonuse of bicycle helmets and risk of fatal head injury: a proportional mortality, case–control study. Canadian Medical Association Journal. 2012;184(17):E921–E923. doi: 10.1503/cmaj.120988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bambach MR, Mitchell RJ, Grzebieta RH, Olivier J. The effectiveness of helmets in bicycle collisions with motor vehicles: A case–control study. Accident Analysis & Prevention. 2013/04/01/ 2013;53:78–88. doi: 10.1016/j.aap.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 38.Kim D, Kim K. The Influence of Bicycle Oriented Facilities on Bicycle Crashes within Crash Concentrated Areas. Traffic Injury Prevention. 2015/January/02 2015;16(1):70–75. doi: 10.1080/15389588.2014.895924 [DOI] [PubMed] [Google Scholar]
- 39.Matsui Y, Oikawa S, Hosokawa N. Effectiveness of wearing a bicycle helmet for impacts against the front of a vehicle and the road surface. Traffic Injury Prevention. 2018/October/03 2018;19(7):773–777. doi: 10.1080/15389588.2018.1498089 [DOI] [PubMed] [Google Scholar]
- 40.Zibung E, Riddez L, Nordenvall C. Helmet use in bicycle trauma patients: a population-based study. European Journal of Trauma and Emergency Surgery. 2015/October/01 2015;41(5):517–521. doi: 10.1007/s00068-014-0471-y [DOI] [PubMed] [Google Scholar]
- 41.Chen Y, Tang Y, Allen V, DeVivo MJ. Fall-induced spinal cord injury: External causes and implications for prevention. The journal of spinal cord medicine. 2016;39(1):24–31. doi: 10.1179/2045772315Y.0000000007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gamblin A, Garry JG, Wilde HW, et al. Cost Analysis of Inpatient Rehabilitation after Spinal Injury: A Retrospective Cohort Analysis. Cureus. Sep 24 2019;11(9):e5747. doi: 10.7759/cureus.5747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D. Health care costs for patients with chronic spinal cord injury in the Veterans Health Administration. J Spinal Cord Med. 2007;30(5):477–81. doi: 10.1080/10790268.2007.11754581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cao Y, Krause JS. Estimation of indirect costs based on employment and earnings changes after spinal cord injury: an observational study. Spinal Cord. Aug 2020;58(8):908–913. doi: 10.1038/s41393-020-0447-1 [DOI] [PubMed] [Google Scholar]
- 45.National Spinal Cord Injury Statistical Center, Facts and Figures at a Glance. 2020. [Google Scholar]
- 46.Kelly ML, He J, Roach MJ, Moore TA, Steinmetz MP, Claridge JA. Regionalization of Spine Trauma Care in an Urban Trauma System in the United States: Decreased Time to Surgery and Hospital Length of Stay. Neurosurgery. Dec 1 2019;85(6):773–778. doi: 10.1093/neuros/nyy452 [DOI] [PubMed] [Google Scholar]
- 47.Hagen EM, Rekand T, Gilhus NE, Gronning M. Diagnostic coding accuracy for traumatic spinal cord injuries. Spinal Cord. May 2009;47(5):367–71. doi: 10.1038/sc.2008.118 [DOI] [PubMed] [Google Scholar]
- 48.Jain NB, Ayers GD, Peterson EN, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. Jun 9 2015;313(22):2236–43. doi: 10.1001/jama.2015.6250 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


