Abstract
A 29‐year‐old man presented to our hospital with severe eosinophilic asthma. He needed a short OCS burst for exacerbation of asthma once every 1 or 2 months, although he used a high dose of inhaled corticosteroids and a long‐acting beta‐2 agonists. Chest CT showed multiple mucous plugs with bronchiectasis, but further examination found that he did not meet the diagnostic criteria for allergic bronchopulmonary aspergillosis. After starting dupilumab for his severe eosinophilic asthma, his asthma control improved without exacerbation. Furthermore, most mucus plugs disappeared on chest CT after 16 weeks from initiating dupilumab. This case suggests that dupilumab may be an effective treatment against mucus plugs associated with severe eosinophilic asthma.
Keywords: dupilumab, mucus plugs, severe asthma
We report a case of severe asthma in which the introduction of dupilumab improved the mucus plugs in addition to asthma control.
INTRODUCTION
Patients with severe asthma present with dyspnea and wheezing for severe airway obstruction and often require a short oral corticosteroid (OCS) burst. A previous report has shown the presence of mucus plugs on computed tomography (CT) in patients with severe asthma, which caused airflow limitation. 1 However, an effective treatment for mucus plugs remains unclear. Herein, we report a case of severe asthma in which the introduction of dupilumab improved the mucus plugs in addition to asthma control.
CASE REPORT
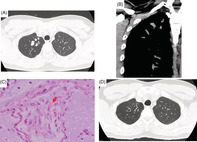
A 29‐year‐old man presented to our hospital with severe eosinophilic asthma. He developed asthma at 25 years of age and was diagnosed with eosinophilic sinusitis at 26 years of age. He was treated with a high dose of inhaled corticosteroids (ICS) with a combination of long‐acting beta‐2 agonists; however, he needed a short OCS burst for exacerbation of asthma once every 1 or 2 months. At age 29 years, a chest CT was performed for a right chest bruise that revealed high‐attenuation mucous (HAM) plugs (CT density: 82 Hounsfield unit) in some bronchi (Figure 1A, B). He was suspected to have allergic bronchopulmonary aspergillosis (ABPA) and was referred to our department for further investigations. Pulmonary function tests showed airflow limitation with forced expiratory volume % in 1 s (FEV1%) of 46.4%, and fractional exhaled nitric oxide (FeNO) was elevated to 226 ppb. Histological examination of mucus plugs obtained by bronchoscopy revealed many eosinophils and Charcot Leyden crystals (Figure 1C); however, no fungi were found both pathologically and in culture. Furthermore, blood tests showed elevated peripheral blood eosinophil counts of 1425/μL and periostin of 106 ng/ml, but no elevation of non‐specific IgE or specific IgE to fungi, including Aspergillus. Aspergillus precipitating antibody was also negative. Based on these results, he met the probable category of ABPA diagnosis criteria by Asano et al but did not meet that by Rosenberg and the International Society of Human and Animal Mycology (ISHAM).
FIGURE 1.
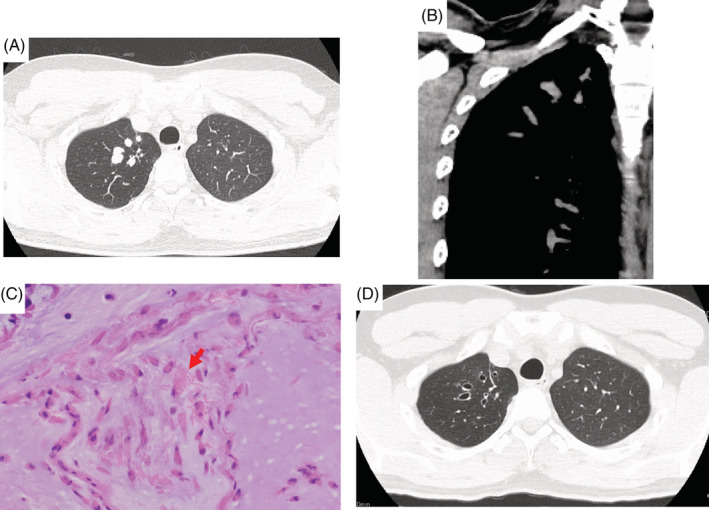
(A, B) Chest computed tomography (CT) at the first visit. High‐attenuation mucus plugs were found mainly in the right upper bronchus on chest CT. (C) Histological finding of mucus plug (red arrow: Charcot Leyden crystal). (D) Chest CT scan 6 months after starting dupilumab
Dupilumab 600 mg, followed by 300 mg every 2 weeks was initiated because of frequent short OCS bursts due to asthma exacerbations Subsequently, the patient coughed up many mucus plugs for a few days, and did not need any short OCS burst after the initiation of dupilumab. Peripheral blood eosinophil counts transiently elevated to 2077/μl at 8 weeks after initiation of dupilumab, but decreased to 868/μl at 16 weeks. Asthma control test (ACT) improved from 15 to 20 points, FEV1 from 2.22 to 3.7 L, FeNO from 226 to 34, the nasal mushroom score from 3 to 1 in each bilateral nasal cavity, nasal obstruction severity score from 2 to 1, compared to that before starting Dupilumab. Moreover, chest CT scan showed the disappearance of most mucus plugs and mucus plug score 1 decreased from 9 to 3 (Figure 1D).
DISCUSSION
To the best of our knowledge, this is the first report of successful treatment with dupilumab for mucus plugs in severe asthma. Mucus plugs are found in more than half of patients with severe asthma on chest CT scans and are associated with airflow limitation. 1 Previous reports have shown that airflow limitation can persist even with ICS and systemic steroid administration in cases with high mucus plugs, and that 82% of asthma patients with mucus plugs have mucus plugs even after 3 years. 1 , 2 These studies indicate that mucus plugs have a negative impact on asthma patients in the long term and are one of the important treatment targets in severe asthma. However, ICS and systemic steroids are not useful for treatment of mucus plugs, as seen in the present case, and the establishment of effective treatment remains a clinical challenge.
A previous study reported that type 2 cytokines are strongly associated with the formation of mucus plugs. IL‐13, an important type 2 cytokine, has variable effects on airway inflammation in severe asthma. IL‐13 stimulates the airway epithelium to secrete cysteine‐rich MUC5AC mucin and to increase the transportation of thiocyanate into the airway lumen. 3 The thiocyanate reacts with eosinophil peroxidase and hydrogen peroxidase and promotes the cross‐linking of mucins and mucus gel stiffening, resulting in the formation of mucus plugs. 1 Furthermore, the epithelial tethering of MUC5AC‐rich mucus impairs the mucociliary transport in asthma. 4 These findings may explain why dupilumab, which blocks IL‐13 receptors, could successfully remove mucus plugs quickly and prevent its relapse even without corticosteroids. Similar to our case, Svenningsen S et al. reported that dupilumab improved mucus plug scores and ventilation heterogeneity, suggesting the effectiveness of dupilumab in airflow obstruction. 5 IL‐5 is also involved in the formation of mucus plugs by activating the eosinophils and releasing granule proteins. Mepolizumab, an anti‐IL‐5 antibody, and benralizumab, an anti‐IL‐5Rα antibody may also be effective against mucous plugs. Further studies are needed for the development of effective treatments for mucus plugs in asthma patients.
Herein, we report a case of severe asthma with mucus plugs that was successfully treated with dupilumab. IL‐13 is one of the key cytokines involved in the formation of mucus plugs, and dupilumab may be an effective therapeutic option for mucus plugs in asthma patients.
AUTHOR CONTRIBUTIONS
Moriyasu Anai, Chieko Yosida, Kei Muramoto, Koichi Saruwatari, Yusuke Tomita, Hidenori Ichiyasu, and Takuro Sakagami wrote the manuscript.
CONFLICT OF INTEREST
None declared.
ETHICS STATEMENT
The authors declare that appropriate written informed consent was obtained for the publication of this manuscript and accompanying images.
ACKNOWLEDGMENTS
We are grateful to Editage for their assistance. This case was presented as a poster at The Japanese Society of Allergology 4th Kyushu‐Okinawa Branch Regional Meeting, 2022.
Anai M, Yoshida C, Izumi H, Muramoto K, Saruwatari K, Tomita Y, et al. Successful treatment with dupilumab for mucus plugs in severe asthma. Respirology Case Reports. 2022;11:e01074. 10.1002/rcr2.1074
Associate Editor: Kazuyuki Nakagome
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Dunican EM, Elicker BM, Gierada DS, Nagle SK, Schiebler ML, Newell JD, et al. Mucus plugs in patients with asthma linked to eosinophilia and airflow obstruction. J Clin Invest. 2018;128(3):997–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tang M, Elicker BM, Henry T, Gierada DS, Schiebler ML, Huang BK, et al. Mucus plugs persist in asthma, and changes in mucus plugs associate with changes in airflow over time. Am J Respir Crit Care Med. 2022;205(9):1036–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dunican EM, Watchorn DC, Fahy JV. Autopsy and imaging studies of mucus in asthma. Lessons learned about disease mechanisms and the role of mucus in airflow obstruction. Ann Am Thorac Soc. 2018;15(Suppl 3):S184–s91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bonser LR, Zlock L, Finkbeiner W, Erle DJ. Epithelial tethering of MUC5AC‐rich mucus impairs mucociliary transport in asthma. J Clin Invest. 2016;126(6):2367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Svenningsen S, Hauder Haider EA, Eddy RL, Parraga G, Nair P. Normalisation of MRI ventilation heterogeneity in severe asthma by dupilumab. Thorax. 2019;74(11):1087–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


