Abstract
In 2020, Coronavirus disease 2019 (COVID-19) pandemic has brought a huge impact in daily life and has prompted people to take preventive measures. In the summertime, however, the Japanese government has cautioned that some COVID-19 pandemic conditions may affect the risk to heatstroke. This study investigated how the COVID-19 pandemic setting affected heatstroke-related ambulance dispatches (HSAD). Daily HSAD data and relevant weather parameters from June to September from 2016 to 2020 of 47 prefectures in Japan were obtained from the Fire and Disaster Management Agency (FDMA) database. A binary variable representing COVID-19 impact was created, whereby years 2016 to 2019 were coded as 0, while 2020 as 1. We employed a two-stage analysis in elucidating the impact of COVID-19 pandemic on HSAD. Firstly, we regressed HSAD with the COVID-19 binary variable after adjusting for relevant covariates to obtain prefecture-specific effect estimates. Prefecture-specific estimates were subsequently pooled via random effects meta-analysis in generating the pooled estimate. Pooled Relative Risk (RR) of HSAD during the COVID-19 pandemic was 0.78 (95% Confidential Interval [CI], 0.75–0.82). We found an overall statistically significant decrease in HSAD risk during the COVID-19 pandemic in Japan. Specifically, the decrease in the risk of HSAD may be linked to the COVID-19 precautionary measures such as stay-home request and availability of alternative consultation services, which may have decreased the direct exposure of the population to extreme heat.
Keywords: COVID-19, Heatstroke, Ambulance dispatch, Protective effects, Precautionary measure
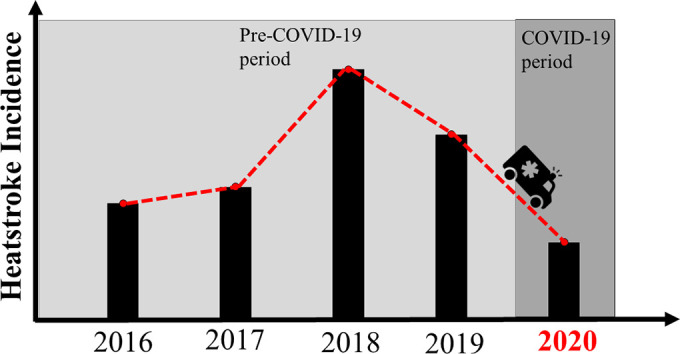
Graphical abstract
1. Introduction
Globally, a devastating and prolonged pandemic of coronavirus disease 2019 (COVID-19) has brought a huge impact in daily life, leaving many cases of incidence and mortality (Lai et al., 2020). In Japan, the number of COVID-19 newly-confirmed cases peaked in the first week of August 2020 and has been a decreasing trend across the country (NIID, 2020). As of October 11, 2020, the total number of confirmed COVID-19 cases and deaths are at 88.2 thousand and 1.6 thousand, respectively (MHLW, 2020c). In response to COVID-19, the Japanese government has made several policy adaptation and requests, such as telework, temporary closure of schools, cancellation of large-scale events (Shaw et al., 2020). The Ministry of Health, Labour and Welfare (MHLW) enacted a recommendation on specific preventive measures for individuals, such as social distance, wearing masks and ventilating indoor space as part of the pandemic response (MHLW, 2020a).
While facing COVID-19 pandemic, heat-related illnesses have been a serious public health concern under a changing climate (Sanderson et al., 2017). Annual temperature in the country has increased by 1.19 °C in the last 100 years (MOEJ, 2018). As temperatures increase, several heat-sensitive health outcomes are at risk of increasing, such is the case for heat-stroke ambulance dispatch (HSAD), which has been increasing since 2010 with record-breaking number of cases at 95,137 in 2018 (MIC, 2019; MOEJ, 2018). Additionally, the number of deaths due to heatstroke has also been increasing reaching 1581 deaths in 2018 (MHLW, 2019). Several previous studies have reported that older people are more vulnerable to heat exposure (Ito et al., 2018; Kuzuya, 2013; Yokota and Miyake, 2016). Based on recent nationally-representative data, people aged more than 65 years old account for 52% of HSAD cases in 2019 and 81.5% of death due to heatstroke in 2018 (MHLW, 2019; MIC, 2019). As a country which has entered the super-aged society, heatstroke is recognized as a serious public health concern and has led to an increase in heat awareness in recent years (Martinez et al., 2011).
In response to the current situation, MHLW has made public warnings particularly for the possibility in the increase of heatstroke cases during summertime under the new lifestyle in the COVID-19 period. Prior to summer, an MHLW-led technical working group has cautioned that several preventive measures under the COVID-19 setting, such as open room ventilation, in the absence of air conditioning, as well as wearing snug-fit masks when outdoors, may possibly contribute to the predisposition of heat-related illnesses, such as heatstroke (MHLW, 2020).
Previous studies have documented the association of HSAD and meteorological parameters, such as maximum and average temperature, during the summer season in Japan (Fuse et al., 2014; Murakami et al., 2012; Ng et al., 2014). However, to the best of our knowledge, no study has been done to examine whether the current COVID-19 period conditions have affected the risk of HSAD.
2. Methods
2.1. Data source
Daily HSAD data in June to September from 2016 to 2020 of the 47 prefectures in Japan were obtained from the Fire and Disaster Management Agency (FDMA) database (FDMA, 2020b). All HSAD data were obtained as aggregated daily counts from the FMDA, which are reported by the prefectural governments. Heat stroke-related diagnoses are coded using the International Classification of Diseases (ICD) 10. Specifically, the following diagnoses are reported and aggregated as heat stroke: “heatstroke and sun stroke” (T67.0), “heat syncope” (T67.1), “heat cramp” (T67.2), “heat exhaustion, anhidrotic” (T67.3), “heat fatigue, unspecified” (T67.5), “heat fatigue, transient” (T67.6), “heat edema” (T67.7), and “other effects of heat and light” (T67.8) (FDMA, 2020c; JAAM, 2015). Whereas, relevant meteorological parameters such as (average/minimum/maximum) temperature (in degrees Celsius; °C) and relative humidity (in %) in the study period were obtained from the Atmospheric Environment Regional Observation System (AEROS) (AEROS, 2020). We utilized a binary variable to collectively represent the impact of COVID-19 period/conditions, whereby 2016 to 2019 were coded with 0 and 2020 was 1.
2.2. Data management and analysis
Health outcome and exposure data were compiled and managed in Microsoft Excel. We employed a two-stage analysis to assess the impact of COVID-19 conditions on HSAD. In the first-stage analysis, we examined the prefecture-specific associations by utilizing a generalized linear model with a quasi-Poisson distribution accounting for overdispersion. Prefecture-specific HSAD was regressed with the COVID-19 indicator variable after adjusting for the relevant covariates. In this study, maximum temperature and relative humidity were treated as a priori confounders (Murakami et al., 2012; Ng et al., 2014), together with the day of the week (DOW), holiday, month and date (for the day of the year); as shown in Eq. (1).
| (1) |
Whereby, Y t is the daily HSAD; α is the intercept; COVID19 is a binary variable; MaxTemp thr is the maximum temperature with threshold; Humidity is relative humidity; DOW is a categorical variable of day of the week; Holiday is a binary variable of national holiday in Japan; Month is a categorical variable representing the months of June to September; Date is the temporal variable representing continuous time; ε is the error term; all beta coefficients of the relevant independent variables are represented as (β 1, β 2, β 3, β 4, β 5, β 6, and β 7). In the second-stage analysis, we performed a random effects meta-analysis to pool the prefecture-specific effects estimates. Temperature was assumed with a threshold due to the discernable increasing pattern after a possible change point, as shown in Fig. S1. We examined the possible change point temperature whereby we observe a sharp increase in the number of HSAD cases. Prefecture-specific absolute temperatures were transformed to relative temperatures using an empirical cumulative distribution function which is inherent to the “base” package of R statistical programming (R Core Team, 2020). Prefecture-specific relative temperatures were utilized for a change point detection via a segmented regression implemented through the “segmented” package (Muggeo, 2003). These change point temperatures were then treated as the prefecture-specific thresholds of the relative temperature (Table S1). We then plotted the distribution of the prefecture-specific thresholds (Fig. S2). After observing an apparent skewed distribution of the thresholds, we took the median value of this distribution, which was at the 80th temperature percentile. We implemented the prefecture-specific threshold specification for the absolute temperature using prefecture-specific 80th temperature percentile as an upper threshold point, which was parameterized through the onebasis function in the “dlnm” package (Gasparrini, 2011). In brief, the association of HSAD and absolute maximum temperature below 80th temperature percentile is assumed to be null, whereas beyond the threshold is assumed to follow linear functional shapes.
We also considered the additional control for PM2.5 in the model, however, due to the unavailability of the 2019 data, we did not include it in the final model. The non-inclusion of the PM2.5 into the final model is also supported by the sensitivity analysis in Table S2. In brief, since current publicly available PM2.5 data is only available from 2016 to 2018 and 2020, we shortened the period to 2016–2018 for the non-pandemic setting, instead of the 2016–2019. There is no significant difference among the prefecture-specific estimates and the pooled estimate, even after adjusting for PM2.5 (in Table S2). We assumed that this non-significant difference after PM2.5 adjustment would also be the same in context of the 2016–2019 period. A more detailed description can be found in the accompanying text of Table S2. In this study, p-value of 0.05 was considered as statistically significant. All analyses were performed using R statistical programming (R Core Team, 2020).
3. Results
Summary statistics for HSAD and meteorological parameters of the 47 prefectures are provided in Table 1 . While overall mean daily HSAD cases of the 47 prefectures in pre-pandemic and pandemic periods are nearly similar (mean = 11.2 and mean = 11.3, respectively), pre-pandemic (2016–2019) variations in daily HSAD were slightly higher than during the pandemic (standard deviation = 23.7 and standard deviation = 22.8, respectively). Highest maximum temperature was observed in 2018 with 29.8 °C, while the lowest one was in 2017 with 29.2 °C. On the other hand, relative humidity was lowest in 2017 with 73.8%, with the highest record of the study period in 2019 at 76.7%.
Table 1.
Annual summary statistics of daily HSAD and meteorological parameters during summer (June to September) in 47 prefectures.a
| Pre-COVID-19 |
COVID-19 |
|||||
|---|---|---|---|---|---|---|
| Year | 2016 | 2017 | 2018 | 2019 | Total (2016–2019) | 2020 |
| HSAD (cases/day) | 8.31 | 8.65 | 16.2 | 11.7 | 11.2 | 11.3 |
| (±12.9) | (±14.1) | (±34.4) | (±25.5) | (±23.7) | (±22.8) | |
| Maximum temp (°C) | 29.5 | 29.2 | 29.8 | 29.3 | 29.4 | 29.6 |
| (±3.99) | (±3.95) | (±4.69) | (±3.95) | (±4.16) | (±4.02) | |
| Humidity (%) | 75.7 | 73.8 | 75.1 | 76.7 | 75.3 | 77.4 |
| (±10.4) | (±10.8) | (±10.7) | (±9.82) | (±10.5) | (±10.3) | |
Mean (±standard deviation); degrees Celsius (°C); percentage (%); HSAD ≣ heat stroke ambulance dispatch.
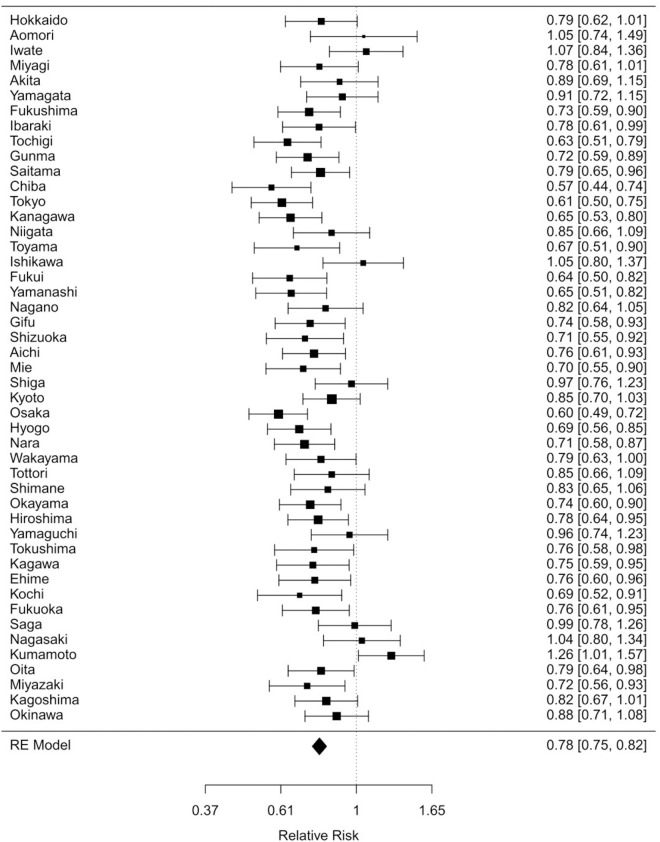
A more detailed summary statistic for all study prefectures are listed in Table S3 of the Supplementary Materials. Majority of the prefecture-level estimates, in Fig. 1 , indicated potential protective effect for HSAD, with lowest relative risk (RR) recorded in Chiba (RR = 0.57, 95% CI: 0.44–0.74). Kumamoto, on the other hand, recorded a statistically significant highest RR of 1.01 (95% CI: 1.26–1.57). Pooled effects estimate from the random effects meta-analysis indicated an overall protective effect with an RR of 0.78 (95% CI: 0.75–0.82), with significant moderate heterogeneity (I2 = 48.74%).
Fig. 1.
Forest plot of prefecture-specific relative risk estimates.
Prefecture-specific estimates are reflected by the horizontal error bars. The dotted black line crossing the prefecture-specific estimates are set at RR = 1. The lowermost diamond-shaped symbol represents the pooled effects estimate. Majority of the prefectures indicate a negative association of COVID-19 pandemic and the risk of HSAD, except for Kumamoto, whereby risks were found to be positively and statistically significant.
4. Discussion
We found an overall statistically significant decrease in HSAD risk during the COVID-19 pandemic in Japan. Under the COVID-19 pandemic, non-binding self-restriction requests were issued by the Japanese government because the legislation in Japan does not allow its government to apply an enforcement of a forced lockdown (Shaw et al., 2020). However, some studies conducted in Japan actually have observed some behavioral changes, such as hand hygiene, social distancing, and even going-out self-restriction under certain contexts (Machida et al., 2020; Parady et al., 2020). Along with preventive strategies for heatstroke and COVID-19, it is possible that behavioral changes followed by a raised awareness of staying healthy may have been a protective influence on HSAD, either apparent reduction of HSAD or possible reduction of heatstroke itself, during the COVID-19 pandemic setting. The potential factors behind the overall reduction may be linked to the precautionary measures in response to COVID-19, namely: stay-home request and availability of alternative consultation services.
4.1. Stay-home request
The frequency of HSAD in outdoor settings, which mostly occur in roads (15.6%) and general outdoor public areas (12.5%), may have simply decreased by staying indoors longer (MIC, 2019). Whereas for HSAD occurring in indoor settings, some studies reported inconsistent results on self-perceptions of risks for heat impacts and changes in their preventive practices (Bassil and Cole, 2010). A few studies found preventive measures, such as staying in an air-conditioned space, were practiced among vulnerable people who recognized their risk to heat (Kosatsky et al., 2009). It is plausible that the stay-home request with increased public warnings for heatstroke may have led to a reduced risk in HSAD both in outdoor and indoor settings.
4.2. Alternative consultation services
Based on previous studies conducted in Japan and the United States, the number of patients transported by ambulance or visited emergency departments have decreased due to increasing concerns about the risk of contracting COVID-19 (Boserup et al., 2020; Katayama et al., 2020; Lange et al., 2020). In Japan, call centers and consultation centers for COVID-19 have been established as alternative consultation service to triage suspected cases properly (MHLW, 2020b).
4.3. Potential increase in HSAD risk: case of Kumamoto
While several prefectures indicated a decrease in the risk of HSAD during the COVID-19 pandemic, it is interesting to note that Kumamoto prefecture exhibited a statistically significant increase (RR = 1.01; 95% CI: 1.26–1.57). The increase in the risk may possibly be related to the record-breaking rainfall which occurred in the Kyushu region due to seasonal rain front, causing thousands of houses damaged completely or partially and prolonged power outage notably in some areas of Kumamoto prefecture (FDMA, 2020a; JMA, 2020; Kyushu Electric Power Co., 2020). Hundreds to thousands of households in the areas could not use air-conditioners, and even to operate shelters in this year, preventive measures to prevent both COVID-19 and heatstroke were required (Kumamoto Prefectural Government, 2020; Kyushu Electric Power Co., 2020), which may have further increased the HSAD risk. While this is an isolated case, the potential for a natural hazard to amplify temperature-related health risks should be explored in future studies which present similar scenarios.
This study has several limitations. First, the finer scale geographical data was not available, the addition of these data, whenever possible, is warranted due to the possible disproportionate effect of heat across a geographical domain. Second, given the ecological nature of the study, several personal-level characteristics were not considered. The apparent statistically significant low-to-moderate heterogeneity (I2 = 48.74%) (Higgins et al., 2003) may be related to several unaccounted factors varying between prefectures, which, however, is beyond the scope of this study. Future studies may potentially examine this through further analyses with suitable meta-regressors.
Amidst these limitations, the study has several strengths. To the best of our knowledge, this is the first study to examine the impact of the COVID-19 pandemic setting on HSAD. Likewise, the multi-location setting allows for a more robust estimate with increased precision. We believe that the study results provide insightful observations on the impact of the COVID-19 pandemic setting on HSAD and its implication with the currently best available data. Also, results from this study would provide a platform to further understand the individual-level characteristics which could explain such protective effect.
5. Conclusion
COVID-19 pandemic setting resulted to a decrease in HSAD in Japan. The decrease in HSAD may possibly be attributed to several precautionary measures targeting to COVID-19.
CRediT authorship contribution statement
Koya Hatakeyama: Study conceptualization, data curation, statistical analysis, writing-original draft; Junko Ota: Study conceptualization, data curation, writing-original draft; Yoshiko Takahashi: Study conceptualization, data curation, writing-original draft; Saki Kawamitsu: Study conceptualization, data curation; Xerxes Seposo: Study conceptualization, data curation, statistical analysis, writing-original draft, reviewing and editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: SCOTT SHERIDAN
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2021.145176.
Appendix A. Supplementary data
Supplementary material
References
- AEROS . 2020. Atmospheric Environmental Regional Observation System: AEROS. 2020, Japan. [Google Scholar]
- Bassil K.L., Cole D.C. Effectiveness of public health interventions in reducing morbidity and mortality during heat episodes: a structured review. Int. J. Environ. Res. Public Health. 2010;7:991–1001. doi: 10.3390/ijerph7030991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020;38:1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FDMA . 2020. Damage Caused by Heavy Rainfall in July 2020 and Response Status of Fire Department (54th Report) [Google Scholar]
- FDMA . Vol. 2020. FDMA; Japan: 2020. Fire and Disaster Management Agency. [Google Scholar]
- FDMA . In: Survey of the Number of People Transported to Emergency Rooms Due to Heat Stroke During the Summer (夏期における熱中症による救急搬送人員の調査) Office of Emergency Planning FaDMA消, editor. Fire and Disaster Management Agency; 2020. [Google Scholar]
- Fuse A., Saka S., Fuse R., Araki T., Kin S., Miyauchi M., et al. Weather data can predict the number of heat stroke patient. Nihon Kyukyu Igakukai Zasshi. 2014;25:757–765. [Google Scholar]
- Gasparrini A. Vol. 43. 2011. Distributed Lag Linear and Non-linear Models in R: The Package dlnm. 2011; p. 20. [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito Y., Akahane M., Imamura T. Impact of temperature in summer on emergency transportation for heat-related diseases in Japan. Chin. Med. J. 2018;131:574–582. doi: 10.4103/0366-6999.226061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JAAM . In: Medical Practice Guidelines for Heat Stroke (熱中症診療ガイドライン) Medicine JAfA, editor. Japanese Association for Acute Medicine; 2015. [Google Scholar]
- JMA . 2020. Prompt Report on Heavy Rain in July 2020. [Google Scholar]
- Katayama Y., Kiyohara K., Kitamura T., Hayashida S., Shimazu T. Influence of the COVID-19 pandemic on an emergency medical service system: a population-based, descriptive study in Osaka, Japan. Acute Medicine & Surgery. 2020;7 doi: 10.1002/ams2.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosatsky T., Dufresne J., Richard L., Renouf A., Giannetti N., Bourbeau J., et al. Heat awareness and response among Montreal residents with chronic cardiac and pulmonary disease. Canadian Journal of Public Health. 2009;100:237–240. doi: 10.1007/BF03405548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumamoto Prefectural Government . 2020. Meeting of Kumamoto Prefecture Disaster Countermeasures Headquarters Regarding Heavy Rainfall in July 2020 (20th Meeting) [Google Scholar]
- Kuzuya M. Heatstroke in older adults. Japan Medical Association Journal. 2013;56:193–198. [Google Scholar]
- Kyushu Electric Power Co . 2020. I. Disaster Response. [Google Scholar]
- Lai C.C., Wang C.Y., Wang Y.H., Hsueh S.C., Ko W.C., Hsueh P.R. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int. J. Antimicrob. Agents. 2020;55:105946. doi: 10.1016/j.ijantimicag.2020.105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange S.J., Ritchey M.D., Goodman A.B., Dias T., Twentyman E., Fuld J., et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January–May 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machida M., Nakamura I., Saito R., Nakaya T., Hanibuchi T., Takamiya T., et al. Changes in implementation of personal protective measures by ordinary Japanese citizens: a longitudinal study from the early phase to the community transmission phase of the COVID-19 outbreak. Int. J. Infect. Dis. 2020;96:371–375. doi: 10.1016/j.ijid.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez G.S., Imai C., Masumo K. Local heat stroke prevention plans in Japan: characteristics and elements for public health adaptation to climate change. Int. J. Environ. Res. Public Health. 2011;8:4563–4581. doi: 10.3390/ijerph8124563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MHLW, MHLW, editors. Yearly Trends of Death Due to Heatstroke by Age Group From Vital Statistics. Vol. 2020. MHLW; Japan: 2019. [Google Scholar]
- MHLW . Vol. 2020. MHLW; 2020. Preventive Actions against Heatstroke for 2020. [Google Scholar]
- MHLW . Vol. 2020. MHLW; Japan: 2020. Example of the New Lifestyle in the COVID19 Period. [Google Scholar]
- MHLW, MHLW, editors. For National Citizens (COVID-19 Infection) Vol. 2020. MHLW; Japan: 2020. [Google Scholar]
- MHLW . Vol. 2020. MHLW; Japan: 2020. Outbreak Status Within the Country. [Google Scholar]
- MIC . Vol. 2020. MIC; Japan: 2019. Situations of Heatstroke-related Ambulance Dispatches During May to September in 2019. [Google Scholar]
- MOEJ . 2018. Synthesis Report on Observations, Projections and Impact Assessments of Climate Change. [Google Scholar]
- Muggeo V.M.R. Estimating regression models with unknown break-points. Stat. Med. 2003;22:3055–3071. doi: 10.1002/sim.1545. [DOI] [PubMed] [Google Scholar]
- Murakami S., Miyatake N., Sakano N. Changes in air temperature and its relation to ambulance transports due to heat stroke in all 47 prefectures of Japan. J. Prev. Med. Public Health. 2012;45:309–315. doi: 10.3961/jpmph.2012.45.5.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng C.F., Ueda K., Ono M., Nitta H., Takami A. Characterizing the effect of summer temperature on heatstroke-related emergency ambulance dispatches in the Kanto area of Japan. Int. J. Biometeorol. 2014;58:941–948. doi: 10.1007/s00484-013-0677-4. [DOI] [PubMed] [Google Scholar]
- NIID . Vol. 2020. NIDD; Japan: 2020. Current Situation of Infection, September 9, 2020. [Google Scholar]
- Parady G., Taniguchi A., Takami K. Travel behavior changes during the COVID-19 pandemic in Japan: analyzing the effects of risk perception and social influence on going-out self-restriction. Transportation Research Interdisciplinary Perspectives. 2020;7:100181. doi: 10.1016/j.trip.2022.100649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing. [Google Scholar]
- Sanderson M., Arbuthnott K., Kovats S., Hajat S., Falloon P. The use of climate information to estimate future mortality from high ambient temperature: a systematic literature review. PLoS One. 2017;12:e0180369. doi: 10.1371/journal.pone.0180369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw R., Y-k Kim, Hua J. Governance, technology and citizen behavior in pandemic: lessons from COVID-19 in East Asia. Progress in Disaster Science. 2020;6:100090. doi: 10.1016/j.pdisas.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokota H., Miyake Y. The problems of heat stroke in the aging society from the Heat stroke Surveillance Committee of the Japanese Association for Acute Medicine (JAAM) Journal of the Japanese Council of Traffic Science. 2016;15:3–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material