Abstract
Objectives
To examine changes in Social Media (SoMe) use among urology residency applicants before and after the COVID-19 pandemic.
Methods
We distributed surveys to individuals who applied to our residency program for application cycles ending in 2018, 2019, and 2021. The surveys included questions about applicants’ SoMe use and perceptions of programs’ SoMe use during the application process, both before (2018/2019) and after (2021) the COVID-19 pandemic. The primary outcome was SoMe use for professional purposes.
Results
We received survey responses from 33% (162 of 496) and 29% (84 of 294) of applicants from the 2018/2019 and 2021 cohorts, respectively. There was a significant increase in professional SoMe use in the 2021 cohort (80%) compared with the 2018/2019 cohort (44%) (P < .001). In 2021 compared to 2018/2019, more applicants used SoMe to connect directly with residents (69% vs 34%, P < .001) and with faculty members (65% vs 15%, P < .001). Applicants in 2021 compared to 2018/2019 more often found SoMe to be useful for making decisions about applying to (33% vs 10%), interviewing at (26% vs 7%), and ranking programs (20% vs 9%) (all P < .05). Twitter was the most common platform for applicants to access program information, increasing from 38% to 71%.
Conclusion
The COVID-19 pandemic ushered in a period of unprecedented SoMe usage among urology applicants, who used it to learn about and connect with residency programs in new ways. The use of SoMe by residency programs has become an important component of trainee recruitment and is likely to continue in the future.
Social Media (SoMe) use has rapidly expanded within the urological community over the last decade. Urologists use SoMe platforms such as Facebook, Twitter, Instagram, and LinkedIn for networking, communicating at conferences, sharing research, and disseminating clinical information. Twitter is the most commonly used platform in professional settings amongst urologists, exemplified by a nearly fivefold increase in the volume of posts at the American Urological Association (AUA) annual meetings from 2013-2018.1 , 2 Sharing urological research over SoMe has become so prolific that article citations are now positively correlated with Twitter mentions, and researchers have developed predictive models of publication impact based on SoMe metrics.3 , 4 SoMe has also been useful to crowdsource advice for challenging cases and to share clinical practice guidelines.5 , 6
Additionally, SoMe has an important role in urological training and graduate medical education. Millennials (those born between the early-1980 and mid-1990) constitute the majority of current and upcoming urology trainees, and this generation has been defined by the ubiquity of technology, mobile devices, and social media in their lives. Multiple surveys have shown that SoMe has a significant influence on residents’ urological knowledge acquisition and is important for career development.7, 8, 9 Urology residency programs have recognized this importance, and the majority now have dedicated program Twitter accounts. Activity from these accounts has even been associated with departmental reputation scores.10 , 11
Despite the prevalence and importance of SoMe in urological training, little is known about its utility in recruiting future urology residents. Medical students leverage SoMe to learn about residency programs, demonstrate their interest, and engage directly with residents and faculty online. During the 2020-2021 application cycle, SoMe became particularly relevant to medical students, as the COVID-19 pandemic limited in-person interactions, mandated virtual interviews, and prohibited visiting sub-internships. Improving our understanding of SoMe use among applicants would be highly useful in future recruitment efforts. In this study, we examine the impact of the COVID-19 pandemic on SoMe use among urology residency applicants.
MATERIALS AND METHODS
We distributed surveys (Supplementary Material) via email to all individuals who applied to our urology residency program for application cycles ending in 2018, 2019, and 2021. The surveys reached 790 applicants out of 1398 who registered for the AUA Residency Match Program for those three cycles.12 The surveys were distributed after the conclusion of the AUA match results, and responses were anonymized to protect participants. Surveys were administered on the Qualtrics platform (Qualtrics International Inc, Provo, UT).
The surveys queried applicants about basic demographic information, SoMe use during the residency application and interview processes, and attitudes toward residency programs’ SoMe use. In 2021, we added questions about changes to the residency application process related to the COVID-19 pandemic and about SoMe use in future application cycles. Incomplete survey responses were excluded.
In order to determine the impact of the COVID-19 pandemic on SoMe use, we separated the survey responses into a pre-pandemic cohort (responses from 2018 and 2019) and a pandemic cohort (responses from 2021). The primary outcome was professional usage of SoMe. This was considered a positive outcome if the response to the question, “How would you describe the usage of your social media accounts?” indicated professional use only or a combination of professional and personal use.
Descriptive statistics were summarized using medians and percentages. X2 tests and Wilcoxon rank-sum tests were used to compare categorical variables and ranked responses, respectively. A multivariable logistic regression model was constructed to evaluate the association between application cohort and professional SoMe use while controlling for demographic factors.
The primary objective of the study was initially descriptive, so no power analysis was done at first (during the 2018 and 2019 distributions). However, during the COVID-19 pandemic, we amended the objective to analyze the impact of the pandemic on SoMe usage. At this point, we conducted a power analysis to determine the required sample size. A 2019 study examining the role of SoMe in the application process for anesthesia residency reported that 45% used SoMe to research programs during the application process.13 Assuming a similar pre-pandemic rate, a X2 test with a two-sided significance level of 0.05 required a sample size of 192 responses in order to detect a 20% increase in SoMe use with 80% power.
Statistical analysis was completed using Stata 16 (StataCorp, College Station, TX). Sample size calculation was performed using G*Power 3.1 (Dusseldorf, Germany). Tests with a P value < .05 were considered statistically significant. This study was approved by the Columbia University Institutional Review Board.
RESULTS
Applicant Demographics
A total of 496 and 294 applicants were sent surveys in the 2018/2019 and 2021 cohorts, respectively. One hundred sixty-two applicants (33%) responded in 2018/2019, and 84 applicants (29%) responded in 2021. The majority of respondents in both 2018/2019 and 2021 identified as male (65% and 55%, respectively, Table 1 ). The mean age was 27.0 (SD = 1.9) and 27.6 (SD = 2.1) for the 2018/2019 and 2021 cohorts, respectively.
Table 1.
Applicant demographics by cohort*
| 2018/2019 N = 162 | 2021 N = 84 | P value | |
|---|---|---|---|
| Gender (%) | .102 | ||
| Male | 106 (65) | 46 (55) | |
| Female | 56 (35) | 38 (45) | |
| Mean age (SD) | 27.0 (1.9) | 27.6 (2.1) | .027 |
| Ethnicity (%) | <.001 | ||
| African American; non–Hispanic black | 11 (7) | 3 (4) | |
| Caucasian; non–Hispanic white | 87 (54) | 34 (40) | |
| East Asian | 18 (11) | 16 (19) | |
| Hispanic | 7 (4) | 18 (21) | |
| Middle Eastern/North African | 10 (6) | 4 (5) | |
| South Asian | 16 (10) | 3 (4) | |
| Other | 13 (8) | 6 (7) | |
| Number of Applications (%) | .042 | ||
| <50 | 16 (10) | 11 (13) | |
| 50-70 | 50 (31) | 15 (18) | |
| 70-90 | 51 (31) | 20 (24) | |
| >90 | 45 (28) | 38 (45) | |
| Number of Interviews (%) | <.001 | ||
| <5 | 6 (4) | 27 (32) | |
| 5-10 | 16 (10) | 12 (14) | |
| 10-15 | 55 (34) | 11 (13) | |
| 15-20 | 60 (37) | 23 (27) | |
| >20 | 25 (15) | 11 (13) |
X2 tests used for hypothesis testing with categorical variables. Wilcoxon rank-sum tests used for continuous variables.
Applicant SoMe Usage
The percentage of respondents who had any social media accounts was 95% in both the 2021 cohort and the 2018/2019 cohort. The use of SoMe for professional purposes increased significantly in the 2021 cohort, compared with the 2018/2019 cohort (80% vs 44%, P < .001, Table 2 ). On multivariable logistic regression controlling for age and gender, applicants in the 2021 cohort were significantly more likely to use SoMe professionally, compared to applicants in the 2018/2019 cohort (OR 4.68, 95% CI 2.49-8.78, P < .001, Supplementary Table 1).
Table 2.
Applicant and program some use*
| 2018/2019 N = 162 | 2021 N = 84 | P-value | |
|---|---|---|---|
| Applicant SoMe Usage | |||
| Any SoMe accounts (%) | 154 (95) | 80 (95) | .951 |
| Professional SoMe use (%) | 72 (44) | 67 (80) | <.001 |
| SoMe connections (%) | |||
| With applicant(s) | 118 (73) | 64 (76) | .570 |
| With residents(s) | 55 (34) | 58 (69) | <.001 |
| With faculty | 25 (15) | 55 (65) | <.001 |
| With program coordinator(s) | 7 (4) | 31 (37) | <.001 |
| Privacy settings changed (%) | 79 (49) | 35 (42) | .290 |
| Posted on SoMe about interview process | 40 (25) | 29 (35) | .104 |
| Perceptions of Program SoMe Usage | |||
| Percentage of programs with SoMe resources available (%) | <.001 | ||
| 1%-25% | 54 (33) | 7 (8) | |
| 26%-50% | 50 (31) | 7 (8) | |
| 51%-75% | 32 (20) | 36 (43) | |
| 76%-100% | 10 (6) | 34 (40) | |
| No response | 16 (10) | 0 (0) | |
| Programs’ SoMe resources were useful when deciding: | |||
| Whether to apply to a program (%) | <.001 | ||
| Yes | 10 (6) | 28 (33) | |
| No | 137 (85) | 37 (44) | |
| Maybe | 15 (9) | 19 (23) | |
| Whether to interview at a program (%) | <.001 | ||
| Yes | 12 (7) | 22 (26) | |
| No | 137 (85) | 45 (54) | |
| Maybe | 13 (8) | 17 (20) | |
| How to rank a program (%) | .019 | ||
| Yes | 14 (9) | 17 (20) | |
| No | 126 (78) | 53 (63) | |
| Maybe | 22 (14) | 14 (17) | |
| SoMe platform most likely to access to learn about a residency program (%) | <.001 | ||
| 61 (38) | 60 (71) | ||
| 33 (20) | 4 (5) | ||
| 22 (14) | 9 (10) | ||
| YouTube channel | 23 (14) | 10 (12) | |
| Other | 7 (4) | 2 (2) | |
| No response | 16 (10) | 0 (0) |
X2 tests used for hypothesis testing.
Of the various SoMe platforms, there was significantly more frequent use of Twitter (P < .001) and LinkedIn (P = .036) in 2021 compared to 2018/2019 (Table 3 ). Half of applicant's pre-pandemic did not have a Twitter account, whereas in 2021 45% reported using Twitter at least once a day. There was a significant decrease in the frequency of Doximity use (P < .001), with 52% of 2018/2019 applicants using it at least once per month compared to 32% of the 2021 cohort. There was no significant difference in the frequency of Facebook or Instagram use.
Table 3.
Applicant some use by platform and frequency*
| No account | < 1/y | At least 1x/y | At least 1x/mo | At least 1x/wk | At least 1x/d | P-value | |
|---|---|---|---|---|---|---|---|
| Facebook Use (%) | |||||||
| 2018/2019 N = 162 |
18 (11) | 2 (1) | 6 (4) | 10 (6) | 29 (18) | 97 (60) | .081 |
| 2021 N = 84 |
7 (8) | 2 (2) | 8 (10) | 5 (6) | 24 (29) | 38 (45) | |
| Twitter Use (%) | |||||||
| 2018/2019 N = 162 |
81 (50) | 7 (4) | 15 (9) | 16 (10) | 13 (8) | 30 (19) | <.001 |
| 2021 N = 84 |
14 (17) | 1 (1) | 4 (5) | 9 (11) | 18 (21) | 38 (45) | |
| LinkedIn Use (%) | |||||||
| 2018/2019 N=162 |
74 (46) | 18 (11) | 37 (23) | 28 (17) | 5 (3) | 0 (0) | .036 |
| 2021 N = 84 |
28 (33) | 9 (11) | 23 (27) | 18 (21) | 5 (6) | 1 (1) | |
| Instagram Use (%) | |||||||
| 2018/2019 N = 162 |
40 (25) | 4 (2) | 6 (4) | 5 (3) | 25 (15) | 82 (51) | .150 |
| 2021 N = 84 |
12 (14) | 0 (0) | 3 (4) | 7 (8) | 14 (17) | 48 (57) | |
| Doximity Use (%) | |||||||
| 2018/2019 N = 162 |
40 (25) | 11 (7) | 26 (16) | 67 (41) | 18 (11) | 0 (0) | <.001 |
| 2021 N = 84 |
32 (38) | 15 (18) | 10 (12) | 24 (29) | 2 (2) | 1 (1) |
Wilcoxon rank-sum tests used for hypothesis testing
The proportion of applicants who made SoMe connections (“friends” or “follows”) with other applicants did not significantly differ between the application cycles. However, the proportion of applicants who connected with residents more than doubled in 2021 compared to 2018/2019 (69% vs 34%, P < .001). Connections with faculty members increased by more than fourfold (65% vs 15%, P < .001), and connections with program coordinators increased by more than ninefold (37% vs 4%, P < .001). There was no significant difference in the applicants who changed their SoMe privacy settings in 2021 compared to pre-pandemic during the application season (49% vs 51%, P = .290).
Of the 80 survey respondents in 2021 who reported using SoMe, 59 (74%) reported that application changes due to the COVID-19 pandemic (eg, virtual interviews, lack of away rotations) directly caused them to increase their SoMe use. Additionally, 32 (40%) reported posting original content about urology on SoMe, such as slides about a topic or a link to their own manuscript.
Perceptions of Program SoMe Usage
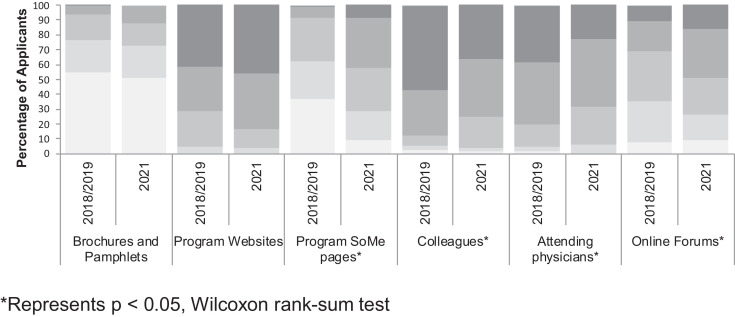
The median percentage of programs reported to have SoMe resources available increased significantly, from 26-50% in 2018/2019 to 51%-75% in 2021 (P < .001) (Table 2). The proportions of applicants who found SoMe to be useful when deciding whether to apply to, whether to interview at, and how to rank a particular program were also significantly higher in 2021 than in 2018/2019. Applicants in 2021 were most likely to access program information on Twitter (71%), compared to 38% of applicants in 2018/2019 (P < .001). The majority of applicants felt that program websites, colleagues, and attending physicians were the most important resources to gather program-specific information ( Fig. 1 ). However, the importance of SoMe in information gathering increased significantly, with 43% rating SoMe as “extremely important” or “very important” in 2021, compared with 9% in 2018/2019 (P < .001).
Figure 1.
Importance of residency resources for prospective applicants. *Represents P < .05, Wilcoxon rank-sum test.
The posts on program SoMe pages that applicants found to be most useful were videos describing different aspects of the program or faculty (27%), followed by pictures of residents socializing (15%) (Supplementary Table 2). While 42% of applicants did not find any program SoMe practices to negatively influence their perceptions of a program, high frequency of posts and posting pictures/screenshots of applicants without their consent were the most commonly cited negative practices (15% and 17%, respectively).
Impressions and Future Directions
In the 2021 cohort, 39% of applicants felt that SoMe engagement had neither a positive nor a negative impact on their application and match prospects (Supplementary Table 3). The most commonly cited positive impact of SoMe was its ability to make applicants more visible to programs (32%). The most commonly cited negative impact of SoMe was feeling overshadowed by other applicants who were more active (55%). Looking to future application cycles, 21% of applicants would like to see more interaction between applicants and programs on SoMe, with 39% desiring a similar amount of interaction and 39% desiring less interaction.
COMMENT
Urology residency applicants are increasingly using SoMe for professional networking. The frequency of Twitter uses in particular underwent marked growth, with median usage increasing from “less than once a year” to “greater than once a week.” The percentage of applicants who used Twitter grew from 50%-83% between the 2018/2019 and 2021 cohorts. For United States. adults ages 18-29, Twitter use only grew from 40%-42% during 2018-2021.14 , 15 Facebook use decreased in this age group, while Instagram and LinkedIn use both increased slightly. More broadly, overall rates of SoMe use in this age group of the general U.S. population decreased from 88% (2018) to 84% (2021). Compared to prior cycles, the number of SoMe connections between applicants and residents, faculty, and program coordinators grew dramatically. As applicants gather information about training programs online, SoMe is an increasingly important resource, and applicants are incorporating information from SoMe as they make decisions about where to apply, where to interview, and how to rank programs.
Social media habits among urology residency applicants, particularly during the 2020-2021 virtual application cycle, have not been well described. Our results showing increased professional SoMe uses are consistent with anecdotal experiences and other specialties seeing SoMe utilized to connect residency programs with prospective applicants. In a 2018 study of applicants applying for ophthalmology residency at Penn State University, almost half of respondents expressed that SoMe was helpful and desired an increase in program SoMe use to disseminate program information.16 In another study from Mayo Clinic surveying anesthesiology residency applicants for the 2017-2018 cycle, 45% of respondents used SoMe to research prospective programs.13 Finally, a study assessing applicants to an integrated Plastic and Reconstructive Surgery program in 2018 found that nearly three-fourths of respondents followed a residency SoMe account, with particular interest in resident life.17
The virtual application environment created by the COVID-19 pandemic heavily drove the rise in SoMe use, as reported by the vast majority of applicants in our survey. In a year when the in-person components of the application cycle were replaced with virtual open houses, virtual sub-internships, and virtual interviews, SoMe offered an easy and convenient platform for programs to share information, showcase their departments’ accomplishments, and connect with applicants.18, 19, 20 Other surgical subspecialties that traditionally required away rotations and evaluation letters from other institutions have similarly responded to the challenges of COVID-19. A 2020 study assessing otolaryngology resident recruitment during the pandemic found that over one-third of otolaryngology department and residency Twitter accounts were created in 2020, with the majority advertising virtual open house meet-and-greets.21 Urology applicants most commonly turned to departmental Twitter accounts to access updates and program information.
Twitter also emerged as a platform for students to share their own original content with programs and fellow applicants, allowing the applicants to gain visibility in a virtual setting. Students were noted to participate in COVID-born virtual urology lecture series, such as the New York Section AUA Educational Multi-institutional Program for Instructing Residents (EMPIRE) and UCSF Urology Collaborative Online Video Didactics (COViD).22 They also flocked to participate in the “UroStream” online mentoring program that linked students and residents to write “Tweetorial” threads of posts on various urological topics. Applicants’ creativity and resilience were on full display like never before.
While SoMe certainly helped connect applicants and residency programs in a cycle restricted by the pandemic, its heavily increased use also carries potential pitfalls that require further consideration. A recent study revealed that more than 11% of urology residents and fellows meet criteria for Social Media Disorder (SMD), a problem characterized by addiction to and compulsive use of SoMe.7 The majority of our survey respondents expressed feelings of being overshadowed by other applicants on SoMe, and as SoMe use becomes increasingly more important (or perceived as more important), the risk of disordered use may rise. Furthermore, while our survey revealed applicant perceptions of program SoMe use, the question of how programs perceive applicant SoMe use remains. As evident from the recent retraction of an article examining the prevalence of “unprofessional” SoMe use among young vascular surgeons, applicant SoMe use could be at risk for scrutiny and biased subjective judgments unrelated to professional competency.23 Should programs begin weighing applicant SoMe use in the evaluation of their candidacy, medical students should be encouraged to review and adopt SoMe professional guidelines. These include those published by BJU International, the European Association of Urology, and the American Urological Association.24, 25, 26 Finally, the rapid growth of SoMe connections between applicants and programs raises the important question of how SoMe use should be viewed in a residency match that emphasizes equity, exemplified by existing rules limiting post-interview communication.
Our study has several limitations. Our survey responses represent 31% of our program's applicants and 18% of all 1,398 students who registered for the match during these three cycles. Thus, our results may not be generalizable to the entire applicant population. Our study had a slightly higher percentage of female respondents than the overall applicant pools for the respective time periods.27, 28, 29 However, gender was not found to be a significant predictor of professional SoMe use on multivariable logistic regression. Self-selection and response bias are potential concerns as well, though we attempted to limit response bias by ensuring anonymity and administering the survey following the match to alleviate any concerns that responses would affect the results. Additionally, we did not administer the survey in 2020, limiting our ability to measure the precise trends over time. Finally, while we report significant changes following a landmark event, we cannot definitively establish causation to link the COVID-19 pandemic to the rise in SoMe among residency applicants.
Despite these limitations, this study offers important insights into the rising role of SoMe in the urology residency application process. This information can help programs better understand the evolving landscape of SoMe in order to optimize their online presence for their applicants. While the COVID-19 pandemic certainly created an unusual environment for residency applications, the extent to which this increased SoMe usage will continue in future application cycles has yet to be determined. Going forward, as applicants experience increasing pressure to use SoMe to connect with programs, it would be enlightening to further understand how applicants are using SoMe for their own promotion and whether programs find it to be a useful avenue to gather information about them.
CONCLUSION
Urology residency applicants are increasingly using SoMe to learn about and connect with residency programs. Twitter, in particular, has emerged as an essential resource for networking and information dissemination during the application process. The use of SoMe by residency programs has become an important component of trainee recruitment.
Footnotes
Declarations of interest: None
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.urology.2021.05.019.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Loeb S, Carrick T, Frey C, Titus T. Increasing social media use in urology: 2017 american urological association survey. Eur Urol Focus. 2020;6:605–608. doi: 10.1016/j.euf.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Matta R, Doiron C, Leveridge MJ. The dramatic increase in social media in urology. J Urol. 2014;192:494–498. doi: 10.1016/j.juro.2014.02.043. [DOI] [PubMed] [Google Scholar]
- 3.Hayon S, Tripathi H, Stormont IM, Dunne MM, Naslund MJ, Siddiqui MM. Twitter mentions and academic citations in the urologic literature. Urology. 2019;123:28–33. doi: 10.1016/j.urology.2018.08.041. [DOI] [PubMed] [Google Scholar]
- 4.Sathianathen NJ, Lane R, 3rd, Condon B, Murphy DG, Lawrentschuk N, Weight CJ, et al. Early online attention can predict citation counts for urological publications: The #UroSoMe_score. Eur Urol Focus. 2020;6:458–462. doi: 10.1016/j.euf.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Koo K, Shee K, Gormley EA. Following the crowd: patterns of crowdsourcing on Twitter among urologists. World J Urol. 2019;37:567–572. doi: 10.1007/s00345-018-2405-5. [DOI] [PubMed] [Google Scholar]
- 6.Loeb S, Roupret M, Van Oort I, N'dow J, Gurp Mv, Bloemberg J, Darraugh J, Ribal MJ, et al. Novel use of twitter to disseminate and evaluate adherence to clinical guidelines by the european association of urology. BJU Int. 2017;119:820–822. doi: 10.1111/bju.13802. [DOI] [PubMed] [Google Scholar]
- 7.Dubin JM, Greer AB, Patel P, et al. Global survey of the roles and attitudes toward social media platforms amongst urology trainees. Urology. 2021;147:64–67. doi: 10.1016/j.urology.2020.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Rivas JG, Socarras MR, Patruno G, et al. Perceived role of social media in urologic knowledge acquisition among young urologists: a european survey. Eur Urol Focus. 2018;4:768–773. doi: 10.1016/j.euf.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Salem J, Borgmann H, Baunacke M, et al. Widespread use of internet, applications, and social media in the professional life of urology residents. Can Urol Assoc J. 2017;11:E355–e366. doi: 10.5489/cuaj.4267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chandrasekar T, Goldberg H, Klaassen Z, Wallis CJD, Leong JY, Liem S, Teplitsky S, Noorani R, Loeb S, et al. Twitter and academic Urology in the United States and Canada: a comprehensive assessment of the Twitterverse in 2019. BJU Int. 2020;125:173–181. doi: 10.1111/bju.14920. [DOI] [PubMed] [Google Scholar]
- 11.Ciprut S, Curnyn C, Davuluri M, Sternberg K, Loeb S. Twitter activity associated with U.S. news and world report reputation scores for urology departments. Urology. 2017;108:11–16. doi: 10.1016/j.urology.2017.05.051. [DOI] [PubMed] [Google Scholar]
- 12.2021. Urology and Specialty Matches.https://www.auanet.org/education/auauniversity/for-residents/urology-and-specialty-matches PublishedAccessed February 15, 2021. [Google Scholar]
- 13.Renew JR, Ladlie B, Gorlin A, Long T. The Impact of Social Media on Anesthesia Resident Recruitment. J Educ Perioper Med. 2019;21:E632. [PMC free article] [PubMed] [Google Scholar]
- 14.Pew Research Center; Washington, DC: 2018. Social Media Use in 2018. [Google Scholar]
- 15.Pew Research Center; Washington, DC: 2021. Social Media Use in 2021. [Google Scholar]
- 16.Goerlitz-Jessen M, Behunin N, Montijo M, Wilkinson M. Recruiting the digital-age applicant: the impact of ophthalmology residency program web presence on residency recruitment. J Acad Ophthalmol. 2018;10:e32–e37. [Google Scholar]
- 17.Steele TN, Galarza-Paez L, Aguilo-Seara G, David LR. Social media impact in the Match: A survey of current trends in the United States. Arch Plast Surg. 2021;48:107–113. doi: 10.5999/aps.2020.00836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang J, Key P, Deibert CM. Improving the Residency Program Virtual Open House Experience: A Survey of Urology Applicants. Urology. 2020;146:1–3. doi: 10.1016/j.urology.2020.08.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kenigsberg AP, Khouri RK, Jr., Kuprasertkul A, Wong D, Ganesan V, Lemack GE. Urology residency applications in the COVID-19 Era. Urology. 2020;143:55–61. doi: 10.1016/j.urology.2020.05.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Margolin EJ, Gordon RJ, Anderson CB, Badalato GM. Reimagining the away rotation: A 4-week virtual subinternship in urology. J Surg Educ. 2021 doi: 10.1016/j.jsurg.2021.01.008. [DOI] [PubMed] [Google Scholar]
- 21.DeAtkine AB, Grayson JW, Singh NP, Nocera AP, Rais-Bahrami S, Greene BJ. #ENT: otolaryngology residency programs create social media platforms to connect with applicants during covid-19 pandemic. Ear Nose Throat J. 2020 doi: 10.1177/0145561320983205. [DOI] [PubMed] [Google Scholar]
- 22.Smigelski M, Movassaghi M, Small A. Urology virtual education programs during the covid-19 pandemic. Curr Urol Rep. 2020;21:50. doi: 10.1007/s11934-020-01004-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hardouin S, Cheng TW, Mitchell EL, Raulli SJ, Jones DW, Siracuse JJ, Farber A, et al. RETRACTED: Prevalence of unprofessional social media content among young vascular surgeons. J Vasc Surg. 2020;72:667–671. doi: 10.1016/j.jvs.2019.10.069. [DOI] [PubMed] [Google Scholar]
- 24.Social media best practices. american urological association. http://auanet.mediaroom.com/index.php?s=20294. Accessed April 2021.
- 25.Borgmann H, Cooperberg M, Murphy D, Loeb S, N'Dow J, Ribal MJ, Woo H, Rouprêt M, Winterbottom A, Wijburg C, Wirth M, Catto J, Kutikov A, et al. Online professionalism-2018 update of european association of urology (@uroweb) recommendations on the appropriate use of social media. Eur Urol. 2018;74:644–650. doi: 10.1016/j.eururo.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 26.Murphy DG, Loeb S, Basto MY, Challacombe B, Trinh Q-D, Leveridge M, Morgan T, Dasgupta P, Bultitude M, et al. Engaging responsibly with social media: the BJUI guidelines. BJU Int. 2014;114:9–11. doi: 10.1111/bju.12788. [DOI] [PubMed] [Google Scholar]
- 27.2019 Urology Residency Match Statistics. American Urological Association.https://www.auanet.org/documents/education/specialty-match/2019-Urology-Residency-Match-Statistics.pdf. Accessed April 27, 2021.
- 28.2018 Urology Residency Match Statistics. American Urological Association.https://www.auanet.org/Documents/education/specialty-match/2018-Urology-Residency-Match-Statistics.pdf. Accessed April 27, 2021.
- 29.2021 Urology Residency Match Statistics. American Urological Association.https://www.auanet.org/documents/education/specialty-match/2021-Urology-Residency-Match-Statistics.pdf. Accessed April 27, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.