Abstract
Background
This systematic review was conducted to map the literature on all the existing evidence regarding individual and ecological determinants of maternal mortality in the world and to classify them based on the income level of countries. Such a systematic review had not been conducted before.
Methods
We conducted an electronic search for primary and review articles using “Maternal Mortality” and “Determinant” as keywords or MeSH terms in their Title or Abstract, indexed in Scopus, PubMed, and Google with no time or geographical limitation and also hand searching was performed for most relevant journals. STROBE and Glasgow university critical appraisal checklists were used for quality assessment of the included studies. Data of the determinants were extracted and classified into individual or ecological categories based on income level of the countries according to World Bank classification.
Results
In this review, 109 original studies and 12 review articles from 33 countries or at global level met the inclusion criteria. Most studies were published after 2013. Most literature studied determinants of low and lower-middle-income countries. The most important individual determinants in low and lower-middle-income countries were location of birth, maternal education, any delays in health services seeking, prenatal care and skilled birth attendance. Household-related determinants in low-income countries included improved water source and sanitation system, region of residence, house condition, wealth of household, and husband education. Additionally, ecological determinants including human resources, access to medical equipment and facilities, total fertility rate, health financing system, country income, poverty rate, governance, education, employment, social protection, gender inequality, and human development index were found to be important contributors in maternal mortality. A few factors were more important in higher-income countries than lower-income countries including parity, IVF births, older mothers, and type of delivery.
Conclusion
A comprehensive list of factors associated with maternal death was gathered through this systematic review, most of which were related to lower-income countries. It seems that the income level of the countries makes a significant difference in determinants of maternal mortality in the world.
Keywords: Maternal mortality, Income level, Countries, Determinants, Systematic review
Introduction
Maternal mortality is an important public health indicator, reflecting not only poor health condition of mothers and poor quality of health care services, but also in macro levels, it indicates poor economic, social, cultural, and political status in a community and also poor status of women in their society [1–3]. Nowadays, improving maternal health is the priority of most communities and organizations, including the World Health Organization (WHO) [4]. The fifth goal of the eight Millennium Development Goals (MDGs) focused on the reduction of maternal mortality by 75% from 1990 to 2015. Despite intense political attention of the countries toward the MDG5, most of them are still far from achieving their MDG5 targets [3]. The global estimates indicate that 295,000 (UI 279,000 to 340,000) maternal deaths occurred in 2017; 35% lower than 2000 when maternal deaths were estimated at 451,000 (UI 431,000 to 485,000) [5]. Thus, another target for maternal mortality reduction was set by the WHO to reach a global maternal mortality ratio (MMR) below 70 by 2030, which requires reducing global MMR by an average of 7.5% each year from 2015 to 2030. This means that to achieve this goal, maternal mortality must be reduced by more than three times the 2.3% annual rate of reduction observed globally between 1990 and 2015, which would be a difficult task for many countries [6].
Based on the existing evidence, there are significant variations in MMR of countries based on their development and income level [5, 7]. Annually, half a million women die from pregnancy-related deaths, of which 99% happen in developing countries while most of them are preventable [8]. This variation is portrayed by WHO; while MMR has never been passed over 115 cases in Europe, America, and Western Pacific regions since 1990, it has always been over 500 cases in Africa [9].
In order to plan effectively and progress systematically in the reduction of MMR, having a broad knowledge about determinants of maternal mortality is an unavoidable need for policymakers and researchers. These determinants may distantly include socio-economic and cultural factors or intermediately include health status, reproductive status, access to health services, and health care behavior factors, or approximately include biological causes of death [10]. Causes of maternal death, based on the International Classification of Diseases-Maternal Mortality ( ICD-MM), are classified to direct (e.g., pregnancies with abortive outcome) or indirect (e.g., cardiac disease) causes in six groups by WHO [4, 11], with no diversity among them.
The existing review studies on determinants of maternal mortality are generally old, or are non-systematic reviews or only reviewed selected determinants [6, 10, 12]. Recently, only a few studies reviewed the determinants systematically, such as the study of Yakubu et al. [13], but only focused on some micro determinants or other study on limited number of determinants [14, 15]. Given that maternal death is a multidisciplinary phenomenon and different factors are involved, we tried to comprehensively review and overview all determinants, with no limitation, in high quality studies which would be of higher applicability for policymakers and researchers. The aim of this study was to conduct a systematic review on individual and ecological determinants of maternal mortality in the world and to classify them based on the income level of countries. In addition to summarizing distant and intermediate determinants of death in individual or ecological level, we also tried to answer this question that how these determinants might vary among mothers living in countries with various development level.
Methods
Inclusion criteria
All types of studies, except descriptive studies, that aimed to identify determinants of maternal mortality were included. In these studies the relationship of possible determinants with maternal mortality was statistically tested. Studies that only focused on the cause of maternal mortality as an approximate determinant, published in non-English journals, or when their full-texts were unavailable were excluded. We considered WHO definition for maternal mortality as “death of a woman while pregnant or beyond 42 weeks of gestation, irrespective of duration and site of pregnancy, due to any cause related to pregnancy or its management, but not due to accidental causes” [9]. No time limit was considered in searches.
Search strategy
To identify relevant studies, an electronic literature search was first conducted on “PubMed” and “Scopus” databases. Then, some of the most relevant journals were searched specifically (Table 1). Additionally, references of included articles were screened.
Table 1.
Sources and search terms and the number of studies identified in each (last searched in 5th August 2021)
| Searching | Sources | Database /journals |
Document types | Key words and Meshes | Publication identified | Final included |
|---|---|---|---|---|---|---|
| Electronic Searching | PubMed | Database | All types | (“Maternal Mortality”[MeSH]) AND determinant* [Title/Abstract] | 50 | 52 |
| Review | (“Maternal Mortality”[Title/Abstract]) AND determinant* [Title/Abstract] | 42 | ||||
| Scopus | Database | Original | (“Maternal Mortality”) AND determinant* | 723 | ||
| Review | (“Maternal Mortality”) AND determinant* | 87 | ||||
| BMC public health | Journal | All types | (“Maternal Mortality”) AND determinant* | 204 | 23 | |
| Maternal and child nutrition | Journal | All types | (“Maternal Mortality”[Abstract]) AND determinant* [Abstract] | 83 | ||
| Maternal and Child Health Journal | Journal | All types | (“Maternal Mortality”) AND determinant* | 91 | ||
| BMC Pregnancy and Childbirth | Journal | All types | (“Maternal Mortality”) AND determinant* | 397 | ||
| PLoS (One/ Medicine/ Neglected Tropical Diseases/ Pathogens/ Genetics/ Computational Biology) | Journal | All types | (“Maternal Mortality”[Title]) AND determinant* [Title] | 126 | ||
| Hand Searching | Bibliography of the included papers | - | - | - | 1855 | 30 |
| - | - | - | - | 16 | ||
| Total | - | - | 3658 | 121 | ||
Except for PubMed database in which “Maternal Mortality” was searched using MeSH term, this term was searched just as a keyword in the rest of search procedure (Table 1). All articles retrieved from electronic databases and other studies were entered into EndNote X8 for further selection.
Study selection
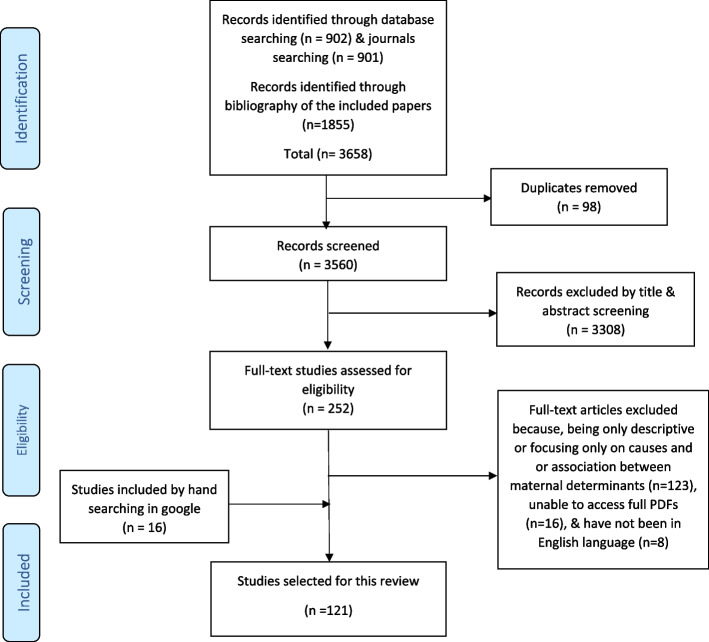
The process of identification and selection of studies is shown in Fig. 1. Initially, 902 and 901 studies were found through electronic searching in databases and journals, respectively. Furthermore, 1855 records were identified based on the bibliography of the included studies. Duplicate studies (n = 98) were removed. Then, screening of titles and abstracts was done by the researchers and studies not relevant were excluded (n = 3308). Then, the assessment of the full text of articles was done for eligibility of 252 studies. Based on the exclusion criteria, 123 studies were excluded due to being only descriptive and not reporting statistical results of relationship between independent variables and maternal mortality (except for review articles), or only focusing on biological causes of maternal deaths, or focusing on the relationship between determinants rather than their relationship with mortality. 16 studies were also excluded as their full-text were not found [16–31] and eight others were not in English [32–39]. In addition, 16 relevant articles were added through searching on Google. Finally, 121 relevant studies obtained from electronic databases, bibliographies, and hand searching were selected based on the inclusion criteria (Table 1 and Fig. 1). No study was excluded after quality assessment. Two reviewers (R.Z. and A.H.) performed the literature searching, checking the inclusion and exclusion criteria and selection of studies and finally data extraction, all phases independently. To reach consensus in the case of variations, in all stages of this review, the reviewers met frequently for discussion, and in the case of lasting disagreement, the third reviewer (M.T.), has been intervened.
Fig. 1.
PRISMA flow diagram for systematic review
Quality assessment
We used the STROBE checklist for original studies and also for ecological studies. It is designed for quality assessment of observational studies especially cohort, case–control, or cross-sectional studies based on 22 items [40]. There were some limitations in quality assessment of the included studies; i.e., some items of this checklist related to participants (item 6), or sample sizes (item 10), or reasons for non-participation (item 13) were not reported in ecological studies that used MMR as a dependent variable. Considering those items as “can’t tell”, the quality scores of those studies decreased. Other items such as clearly defining potential confounders in item 7, reporting potential sources of bias in item 9, way of handling quantitative variables in item 11, and reporting statistical methods used to control confounders or missing data in item 12 of the STROBE checklist were the main limitations of the selected studies, which were not often reported in their methodology. In some included studies, their limitations were not mentioned in the discussion. Each question in this checklist had one score, so the highest quality of the article would obtain score 22.
We used the critical appraisal checklist from Glasgow University [41] for the quality assessment of review articles. As shown in Table 3, except for two studies containing nine review articles, the quality assessment was not performed for the rest of them, and their results were not reported precisely because determinants of maternal mortality were not based on the confidence interval. It is worth noting that the quality of the studies was independently assessed by two researchers in different places. Then, discrepancies were resolved by participation of a third researcher to reduce the risk of bias.
Table 3.
Summary of characteristics and findings of review studies
| Publication date/ Ref | Date | Type of review | Number of included studies |
Key findings (factors associated with maternal death) |
Quality of studiesa | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Did the review address a clearly focused issue? | Did the authors look for the appropriate sort of papers? | Do you think the important, relevant studies were included? | Did the reviews authors do enough to assess the quality of the included studies? | If the results of the review have been combined, was it reasonable to do so? | What is the overall result of the review? | How precise are the results? | Can the results be applied to the local population? | Were all important outcomes considered? | Are the benefits worth the harms and costs? | |||||
| 1.2020 [150] | 2005–2015 | SR | 25 | Low socio-economic status family, rural and remote areas, teenagers and unmarried women, perceptions related to pregnancy, delivery and death, perception related to family planning, practice related to pregnancy and delivery, gender inequity, perception related to midwife performance and health services | Y | Y | CT | Y | Y | N | Y | CT | Y | Y |
| 2.2019 [151] | - | SR | 29 | Preterm of gestational age, obesity, quality of care, immune pregnancy ratio, human development index, gender inequality in education, access to improved water source, fertility rate | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| 3.2019 [152] | 2007–2019 | SR | 7 | Age, parity, domestic violence, inadequate antenatal care, place of delivery, education, healthcare provider qualification, delays in arrival at health facilities, unemployment, socioeconomic status, no antenatal care, having been referred, distance to health facilities, social autonomy, media exposure, family planning, nutrition, religion, ethnicity, wealth index, water quality, sanitation and hygiene | Y | Y | Y | N | Y | Y | Y | N | Y | Y |
| 4. 2018 [13] | since 2000 | SR | 33 | Parity, education, fertility level, maternal age at birth, status of women, income/poverty, access to electricity or access to improved water sources and sanitation | Y | Y | Y | N | Y | Y | Y | Y | CT | Y |
| 5. 2016 [14] | - | SR | 62 | harmful traditional beliefs and practices; early marriage, high parity and female illiteracy | Y | Y | Y | Y | CT | Y | CT | Y | CT | CT |
| 6. 2014 [15] | Since 1980 | SR | 14 | water and sanitation system | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 7. 2017 [153] | - | NR | 38 | Factors including education, sociocultural practices (e.g. criminalization of marriage blow 18, and Promoting women’s rights), social services (e.g. Improved health care access and quality), and health care (access, utilization, and quality), and income or employment | Y | Y | Y | N | Y | Y | N | Y | Y | Y |
| 8. 2015 [154] | NR | - | Economic growth, Poverty, Inequality, Local infrastructure, education, Access to public health information, Fertility rates, Average age of first pregnancies, Urbanization, Women’s empowerment, income, living condition, Affordability of services, health status, Age & age of first pregnancy, birth spacing, previous fetal loss, urban location, and proximity to services at the community or social and individual levels, access to family planning, antenatal support, delivery & post birth care, and quality of services, and demand of this services | Y | Y | Y | N | Y | Y | Y | CT | Y | Y | |
| 9. 2006 [155] | 1975–2001 | NR | 9 | Mode of delivery may not associated with maternal mortality | Y | Y | C | N | CT | Y | N | CT | Y | CT |
| 10. 1998 [12] | in 1996 | NR | - | Wife seclusion, Age, universal female illiteracy, harmful traditional medical beliefs and practice, inadequate facilities to deal with obstetric emergencies, a deteriorating economy & policy | Y | N | N | N | Y | Y | N | Y | CT | CT |
| 11. 1992 [10] | in1992 | NR | - | Distant determinants (education, occupation, income, social and legal autonomy, wealth and community resources), and intermediate determinants (use of family planning, use of prenatal care, use of modern care for labor and delivery, use of harmful traditional practices, use of illicit) and induced abortion, location of services, range of services available, quality of care, access to information about services, age, parity, marital status, nutritional status, infections and parasitic disease, and prior history of pregnancy complications | Y | Y | N | N | CT | Y | N | Y | CT | CT |
| 12. 1991 [6] | 1980–1990 | NR | - | Poor sanitation, lack of clean water, poor transportation, lack of medical facilities, malnutrition, poverty, increased work load, frequent pregnancy, low status of women, early marriage, lack of legal abortion, & no acceptance of contraception | Y | Y | CT | N | Y | Y | N | Y | Y | CT |
SR Systematic Review, NR Narrative Review, Y Yes, N No, CT Can’t Tell
aGlasgow university critical appraisal checklist [41] was used for quality assessment of these review articles
Data extraction
We extracted the required data from the included review articles and original articles using a purposefully designed data extraction form. Year of publication, number of maternal deaths, time span of the study, setting, design, and methods, and maternal mortality determinants were extracted from the included studies as shown in the Tables 2 and 3.
Table 2.
Summary of characteristics and findings of original studies (Chronologically ordered)
| Date of pub/ Ref |
N of deaths, setting & date |
Income | Design | Key findings | Quality (0–22) | |
|---|---|---|---|---|---|---|
| Factors Associated | Factors Not associated | |||||
|
1 2021 [42] |
N = 43 Indonesia 2017–2019 |
LM | Case–control | Education, parity, age, family income | Occupation | 20 |
|
2 2021 [43] |
N = - China 2013–2018 |
LM | Ecological | GDP per capita, rate of delivery in maternal and child health hospital, rate of cesarean section, rate of low birth weight | - | 19 |
|
3 2021 [44] |
N = - India 1997–2017 |
L | Ecological | Place of residence, education, region of residence, wealth index, health insurance coverage, caste | Religion, number of members in the household | 21 |
|
4 2021 [45] |
N = - 54 African countries 2006–2018 |
L | Ecological | Gender inequality index, current health expenditure as a percentage of GDP, density of skilled health professional, type of delivery, lifestyle, gender inequities, the proportion of skilled birth attendant | - | 17 |
|
5 2020 [46] |
N = 47 Pakistan 2013–2017 |
L | XS | Poverty, prenatal care, education, long distance, delay in acquiring blood/blood products, delay in surgery | - | 16 |
|
6 2020 [47] |
N = 367 Cameron 2004–2011 |
L | Ecological | Community education, community wealth, age, parity, social autonomy, domestic violence, distance to facility, media exposure, contraception type, education, religion, ethnicity, type of residence, wealth index, water quality | 18 | |
|
7 2020 [48] |
N = 33 Indonesia, 2015–2017 |
LM | XS | Education, age, occupation, maternity period, parity, distance from health center | - | 20 |
|
8 2020 [49] |
N = 14,892 South Africa 2007–2015 |
L | Ecological | Age, education, marital status, occupation, place of death | - | 19 |
|
9 2020 [50] |
N = - China 2004–2016 |
LM | Longitudinal | Level of development of provinces, proportion of illiteracy, average annual household consumption, proportion of college educated, maternity health insurance coverage, premarital check-up, maternal health profiles creation rate, coverage of maternal systematic management, prenatal care, postpartum visit rate, hospital delivery rate, delivery attended by professionals rate | Public budget in health sector per capita, density of specialized maternal and child health hospitals, density of health providers in specialized maternal and child health hospitals | 22 |
|
10 2019 [51] |
N = 8075 Indonesian (rural) 2010 census |
LM | XS | Age, education, health service access, number of midwives working in the village, doctors working at health center | Education of the household head, spouse employment, midwives working at health centers | 19 |
|
11 2019 [52] |
N = - Brazil 2013 |
UM | Ecological | Human Development Index (HDI), proportion of family health care strategy implementation, caesarean rate | - | 17 |
|
12 2019 [53] |
N = - USA 2007–2015 |
H | Ecological | Rural residents, type of health insurance, type of delivery, racism, poverty | - | 19 |
|
13 2019 [54] |
N = 810 Nigeria 2008–2013 |
L | XS | Education, community wealth, media exposure, religion, distance to facility, contraception type, ethnicity, type of residence, wealth index, water quality, age | - | 18 |
|
14 2019 [55] |
N = - India 2016–2017 |
L | Case control | Age, parity, provider of labor | Place of death/delivery, time of occurrence | 19 |
|
15 2019 [56] |
N = 150 India 2013–2014 |
L | XS | Occupation, husband’s occupation, accesses to health services | - | 18 |
|
16 2019 [57] |
N = 59 Ethiopia 2014–2017 |
L | Case–control | Obstetric, husbands education, antenatal care, home delivery, place of residence, parity | Place of death, state of pregnancy at time of death | 20 |
|
17 2018 [58] |
N = 100 Zambia 2010–2015 |
L | Case–control | Presence or absence of risk condition, antenatal care, presence of complications, any delay to seek health care, delay type, Parity, gestational age, care time, sought traditional health care, marital status, education | - | 20 |
|
18 2018 [59] |
N = - USA 1997–2012 |
H | Ecological | Education, African American race, prenatal care visits, state median income, ethnicity, un insurance rates | Age and cesarean-section rates | 20 |
|
19 2018 [60] |
N = 312 South African 2000–2014 |
LM | Longitudinal | Wealth index, source of drinking water, education, period of death, area and number of deliveries, period of death 2000–2006 | Age, distance to the nearest clinic | 18 |
| 20. 2018 [61] |
n = 91 Nigeria 2014 |
LM | XS | Type of facility, booking status for antenatal care, referral, Parity & number of early pregnancy loss | Occupation, Place of delivery, complication in index pregnancy & Mode of delivery | 21 |
| 21. 2017 [62] |
n = 16 Ethiopia 2011–2014 |
L | XS | Place of delivery, occurrence of hypo volume shock, & postoperative severe anemia | - | 21 |
| 22. 2017 [63] |
n = 1103 Nigeria 2013 |
LM | XS | Wealth index, residence, community women’s education, autonomy, spousal educational difference, highest educational attainment, age, religion, & attitudes towards domestic violence | Economic empowerment | 21 |
| 23. 2017 [64] |
- China 2002–2014 |
UM | Ecological | Social and economic environment (GDP per capita, rate of urbanization and highway per land, the average travelling time to the nearest hospital), Health human resources, health infrastructure, & maternal health care service | - | 20 |
| 24. 2017 [65] |
n = 16 China 2011 |
UM | XS | Mode of delivery including operative vaginal delivery, non-indicated intrapartum, indicated antepartum, & indicated intrapartum | Non-Indicated antepartum as a mode of delivery | 20 |
| 25. 2017 [66] |
n = 39 Indonesia 2017 |
LM | Case–control | Late decision making, complication, standard ANC visit, high risk pregnancy, & high educational level | Late transportation providing, employment status & Late handling in medical facilities | 19 |
| 26. 2017 [67] |
- Ecuador 2014 |
UM | Ecological | GDP, percentage of households with children who do not attend school, percentage of households with electricity, percentage of indigenous population, & total fertility rate | Poverty with unsatisfied basic needs, Average household income, Percentage of households with inadequate services, & Average persons per bedroom | 18 |
| 27. 2017 [68] |
- low-income countries 2012- 2015 |
L | Ecological | Total fertility rate, skilled birth attendance | Corruption index, GDP per capita, & empowerment measures | 17 |
| 28. 2017 [69] |
N = 37 Indonesia 2010–2012 |
LM | XS | Education, Referral status, location of death, history of maternal systemic illness, Type of labor (e.g. spontaneous), pregnancy complications, & puerperium complications | Labor complications, maternal age, parity, pregnancy interval, total antenatal care, first labor assistance, spouse occupation & residence | 16 |
| 29. 2017 [70] |
n = 360 Nigeria - |
LM | XS | Place of consultation, who pays the treatment costs, awareness of pregnancy complications and knowledge of the place of antenatal care treatment | - | 15 |
| 30. 2016 [71] |
n = 73 Brazil 2009–2012 |
UM | Case–control | Mode of delivery, premature delivery, gravidity, education, and age | Skin color, type of hospital, & region of residence | 21 |
| 31. 2016 [72] |
N = 34 Iran 2009—2013 |
UM | XS | Gravidity | Residence, type of birth, birth attendant, and mother’s age and place of birth | 19 |
| 32. 2016 [73] |
- LMICs 1990 -2010 |
- | Ecological | Gender equality, infrastructure, education, water and sanitation, GDP per capita, fertility, Immunization, & health services delivery | - | 19 |
| 33. 2016 [74] |
n = 89 Cameroon 2011–2014 |
LM | Case–control | Inadequate antenatal care, pre-existing co-morbidities, place of delivery, healthcare provider qualification, and delays in arrival at health facilities | Age, marital status, occupation, mothers education, religion, residence, way of transport, & parity | 19 |
| 34. 2016 [75] |
328 Turkey 2002–2013 |
UM | Longitudinal study | Cesarean delivery | - | 19 |
| 35. 2016 [76] |
- East Mediterranean 2004–2011 |
- | Ecological | GDP Per Capita, health expenditure as % of GDP, Literacy rate among Female adults aged 15 + , Birth attended by skilled health providers, Primary Healthcare units and Centers, & Urbanization Rate | Total Fertility Rate (TFR) | 17 |
| 36. 2016 [77] |
n = 313 Uganda 2011 |
L | XS | Mothers education, age, region of residence, number of visits | - | 14 |
| 37. 2015 [78] |
n = 62 Ethiopia 2012–2013 |
L | Case–control | Member of women’s development army, husband’s involvement score, ever used contraceptives before the last pregnancy, & any previous medical illnesses, | Involved in health care decision making, Number of antenatal care visits, & Previous pregnancy-related complications | 20 |
| 38. 2015 [79] |
- Global 2000–2010 |
- | Ecological | % of access to water, % of access to sanitation systems, birth attention by a healthcare professional, having corrupt government, total Health expenditure (Q2 vs Q1), & fertility rate (Q4 vs Q1) | total Health expenditure (Q3 & Q4 vs Q1), Human resource & fertility rate (Q3 & Q2 vs Q1) | 20 |
| 39. 2015 [80] |
n = 135 UK 2009–2012 |
H | Case–control | Inadequate use of antenatal care, substance misuse, medical comorbidities, previous pregnancy problems, & Indian ethnicity | Age, parity, BMI, employment status, & result of the birth | 20 |
| 40. 2015 [81] |
n = 28 Ghana 2013 |
LM | XS | Age, residence, parity, education, religion, antenatal care, lack of communication between facilities, lack of equipment, inadequate treatment, patient & facility delay | Occupation of mothers | 19 |
| 41. 2015 [82] |
n = 402 LMICs 2010–2013 |
- | Longitudinal | Age, parity, Birth attendant, education, lack of antenatal care, & caesarean section delivery | - | 19 |
| 42. 2015 [83] |
- Global 2010 |
- | Ecological | Private sector and trade, governance, education, employment and social protection, economic policy and debt, health- service expenditure, environment- agriculture and Production, education-efficiency, &private sector- private infrastructure | - | 19 |
| 43. 2015 [84] |
n = 51 Ethiopia 2012–2013 |
L | XS | Population density | - | 18 |
| 44. 2015 [85] |
n = 35 Indonesia 2013–2014 |
LM | Case–control | High risk of health status (nutritional status, anemia, disease history and previous pregnancy complications) | - | 17 |
| 45. 2015 [86] |
n = 13 Ethiopia 2014 |
L | XS | Occupation, ethnicity, age, and religion | Marital and educational status | 16 |
| 46. 2015 [87] |
- China 1996–2009 |
LM | Ecological | Increased hospital delivery rate, decreased male illiteracy rate, increased GDP | - | 15 |
| 47. 2014 [88] |
n = 109 China 2010–2011 |
UM | Case–control | Maternal age, education, gravidity, parity, marital status, having health insurance, antenatal care, family income, mode of delivery, not registered in healthcare system, no decision on ANC attendance made by woman, not received follow-up reminders to attend ANC, not knowing the recommendation to deliver in hospital, not knowing the danger signs of delivery, not knowing to register the pregnancy and to attend antenatal care (ANC), & unplanned pregnancy | Complications during pregnancy | 21 |
| 48. 2014 [89] |
- European Union 1981–2010 |
- | Ecological | Government healthcare expenditure | - | 20 |
|
49 2014 [90] |
n = 209 Malawi 2001–2002 |
L | Case–control | Condition on admission, outcome of birth, number of days in hospital, transfusion, evacuation, & birth weight | High parity | 20 |
| 50. 2014 [91] |
n = 140 Brazil 2009 -2010 |
UM | XS | Delay in seeking health services, quality of medical care (including absence of blood products, lack of medication, difficulty in communicating between hospital and regulatory center, lack of trained staff, difficulty in monitoring, improper patient management, and delays in starting treatment, diagnosis and transfer) | Refuse to treatment, Unsafe abortion, health service accessibility | 20 |
| 51. 2014 [92] |
n = 150 Kenya 2004–2011 |
L | Case–control | Age, education, history of underlying medical conditions, contraceptives, gravidity, mode of delivery, birth attendant, pregnancy stage, number of ANC visits, comorbid complication, referral, & pulse | - | 19 |
| 52. 2014 [93] |
N = 37 Iran 2006 -2014 |
LM | XS | Maternal age, gravidity and preterm of gestational age | Type of delivery and birth attendant | 18 |
| 53. 2014 [94] |
n = 226 Brazil 2000–2002 |
UM | Case–control | Type of hospital deliveries, mode of delivery, & residence | Age, education | 18 |
| 54. 2014 [95] |
n = 35 Indonesia 2013–2014 |
LM | Case–control | Age at marriage, education, occupation, gender and culture (e.g. involving in decision-making) | - | 17 |
| 55. 2014 [96] |
- LMICs 1990–2010 |
- | Ecological | GDP per capita, doctors per 100 people, prenatal care, access to sanitation system, total fertility rate, female total years schooling, total years schooling in both sexes, Power consumption per capita, roads paved, & Published scientific papers annually | Poverty, government effectiveness index, skilled birth attendance, measles immunization, HIV prevalence, health expenditure per capita, out-of-pocket health spending, access to clean water, contraceptive prevalence, percentage of women in parliament, female labor force participation | 13 |
| 56. 2013 [97] |
n = 486 Global 2010- 2011 |
- | XS | Marital status, age, schooling, number of previous births, number of previous caesarean sections, onset of labour, & mode of delivery | - | 21 |
| 57. 2013 [98] |
n = 62 Ethiopia 2010–2012 |
L | Case–control | Level of education, residence, distance to nearby hospital, ANC registration history, age of the women, types of birth attendants, length of labor from admission & mode of delivery | - | 17 |
| 58. 2013 [99] |
- Madagascar 1993–2007 |
L | Panel study | Primary clinics [4], time to the Hospital (hours), population, births (number divided by 1,000), female literacy, female wages (weekly, national currency divided by 1,000), income, poverty gap, & without toilet (number per households) | Doctors (per 1,000 population) | 15 |
| 59. 2012 [100] |
n = 7 Sub-Saharan Africa 2010–2011 |
- | XS | Parity | Maternal age | 19 |
| 60. 2012 [101] |
- Iran 2001–2008 |
LM | Ecological | Male literacy, unemployment, & female literacy | Proportion of midwives, urban residency | 17 |
| 61. 2012 [102] |
- Chile 1957 to 2007 |
LM | Time-series | Education, TFR, delivery by skilled attendants, & clean water, sanitary sewer | GDP per capita | 16 |
| 62. 2012 [103] |
1129 China 1996–2009 |
LM | Longitudinal | Prenatal care, gestational age, pregnancy tendency(wanted/ unwanted), place of death, income, residence & education | - | 15 |
| 63. 2011 [104] |
n = 363 Global 2004–2005 |
- | XS | Maternal age, marital status, parity, government health expenditure, Gravidity, & Education | - | 21 |
| 64. 2011 [83] |
n = 328 France 2001–2006 |
H | Case–control | Residence, maternal age, parity, hospitalization during pregnancy, induced laboar, type of delivery, emergency cesarean, preterm delivery, & multiple birth | Work status, marital status | 21 |
| 65. 2011 [105] |
- Iran 2004–2006 |
LM | Ecological | Human development index, difference in illiteracy rate in women and men | Gini coefficient | 20 |
| 66. 2011 [106] |
- Global 2001–2008 |
- | Ecological | Access to improved sanitation and water, corruptive government, health expenditure, & total fertility rate | - | 18 |
| 67. 2011 [107] |
- Nepal 1996–2006 |
L | Ecological | % Professional delivery care, % hospital delivery, % health facility delivery, % emergency obstetric care facility delivery, % caesarean section delivery, % met need for emergency obstetric care, mean birth order, mean wealth quintile, mean total children born, mean age at first birth, mean hemoglobin, % anemia moderate/severe, % any birth preparation, Human Development Index, Gender Empowerment Measure, General Fertility Rate | GDP | 18 |
| 68. 2010 [108] |
n = 47 Africa 2004 |
L | Case–control | Travel times more than 4 h from hospital | Travel times between 2–4 h from hospital | 21 |
| 69. 2010 [109] |
n = 32 India 2003–2004 |
L | Case–control | Percentage of people under poverty line, mothers age, number of pregnancy, & place of delivery | Education, prenatal care | 20 |
| 70. 2010 [110] |
- high and middle income 1936–2005 |
Time-series | GDP per capita | - | 16 | |
| 71. 2010 [111] |
n = 46 India 2003–2006 |
L | Retrospective cohort | Mode of delivery, parity, age | - | 16 |
| 72. 2009 [112] |
N = 339 china 1997 |
LM | XS | Average number of village doctors, proportion of villages without doctors, percent of minority groups | - | 20 |
| 73. 2009 [113] |
- Ethiopia 1995–2008 |
L | Time series | GDP per capita, adult literacy rate, total fertility rate, number of doctors per 100,000 population, number of nurse per 100,000 population, hospitals per 100,000 population, skilled birth attendance, postnatal care coverage, prenatal care coverage, & Recurrent Health Expenditure per capita | - | 20 |
| 74. 2009 [114] |
n = 148 Spain 1996–2005 |
H | XS | Maternal age | - | 19 |
| 75. 2009 [115] |
- Sub-Saharan Africa 1997 – 2006 |
- | Ecological | Infant mortality (deaths per 1000 live births), antenatal care coverage (%), births attended by skilled health personnel, access to an improved water source, adult literacy rate, contraceptive prevalence, ratio of female rate to male rate, primary enrolment rate, primary enrolment rate, female, education index, Gross National Income per capita ($),out-of-pocket expenditure on Health, per-capita government expenditure on health ($) | Access to improved sanitation, public expenditure on health (%GNP), public expenditure on education (%GNP), external resources for Health, government expenditure on Health | 17 |
| 76. 2009 [116] |
n = 112 Nigeria 2003–2007 |
L | XS | Parity, antenatal care, literacy | Maternal age | 16 |
| 77. 2008 [117] |
n = 45 Tanzania 1995–1996 |
L | Case–control | Maternal age, ethnic and religious affiliation, and low formal education of the husbands | - | 21 |
| 78. 2008 [118] |
n = 267 France 1996–2001 |
H | Case–control | Nationality, age, parity, work status, hospitalization during pregnancy | Marital status | 21 |
| 79. 2008 [119] |
n = 387 Burkina Faso 2002–2006 |
L | XS | Antenatal care coverage | Asset index quintile, distance to hospital, distance to health facility, caesarean section rate, institutional birth rate | 19 |
| 80. 2008 [120] |
n = 84 Nigeria 2003–2004 |
L | Case–control | Long labor, grand multi parity, Higher occupational status, No antenatal care | Age, birth interval | 15 |
| 81. 2007 [121] |
n = 769 Bangladesh 1976–2005 |
L | Retrospective cohort | Pregnancy order, maternal age (years), household asset quintile among less/ least poor people, completed years of formal education of mother, service area | Religion, household asset quintile among poorer or poor people | 20 |
| 82. 2007 [122] |
n = 70 India 1993–1995 |
L | Case–control | Age, education of wife, education of husband, type of family, parity, antenatal care receiving, place of delivery, mode of transport used to reach the health facility, complication during pregnancy & distance of the health facility from residence | Caste, age at marriage of women | 18 |
| 83. 2007 [123] |
n = 84 Argentina 2002 |
UM | Case–control | Age, gravidity, Obstetrics-gynecology specialist on 24-h active duty, Availability of essential obstetric care, Length of hospitalization (days), Presence of residency program, & Previous gestations | Education, marital status, cesarean section | 18 |
| 84. 2007 [124] |
- China 1990–2000 |
L | Time series | modern delivery methods, GDP per capita, illiteracy rate, hospital delivery, clean drinking water | contraceptive use & Prenatal care | 15 |
| 85. 2006 [125] |
- Africa’s countries 1990–2010 |
- | Ecological | CNP per capita, policy instability | - | 19 |
| 86. 2006 [126] |
n = 153 Senegal 1997–2000 |
L | XS | Previous Caesarean section, prenatal visits, referral for delivery, mode of delivery, transfusion | Age, parity | 18 |
| 87. 2006 [127] |
- Global 2003 |
- | Ecological | Human development index, Gender-Related Development Index, female literacy rate, combined primary, secondary, and tertiary enrolment ratio, & Infant mortality rates |
Gender Empowerment Measure, Total fertility rate, female professional and technical workers, ratio of estimated female to male earned incomes, female political involvement, & women participation in parliament |
13 |
| 88. 2005 [128] |
- US 1994–2001 |
H | Ecological | Specialist ratio per 10,000 live birth, obstetric/ provider ratio per 10,000 live birth, general obstetric/gynecologist ratio per 10,000 live birth, poverty, Percent mothers without a high school diploma, Percent teenage mothers, & intercept | Color of skin, Percent mothers without adequate PNC | 14 |
| 89. 2004 [129] |
- Global 2004 |
- | Ecological | Nurse density, doctor density, & Gross national income per person | Female adult literacy, & poverty | 20 |
| 90. 2004 [130] |
- Sub-Saharan Africa 1990–2003 |
- | Ecological |
(GNP) per capita, health expenditure per capita, births attended by skilled health personnel & life expectancy at birth |
HIV/AIDS prevalence, Total fertility rate, Political stability | 19 |
| 91. 2004 [131] |
- developing countries 1984 |
L | Ecological | Poverty, education, type of floor, type of toilet, & source of water | - | 16 |
| 92. 2003 [132] |
n = 59 Indonesia 1996–1999 |
L | Case–control | Residence, employment status, availability of toilet facility, & time of initial visit to antenatal care facilities | Race, religion, travel time to hospital, availability of automobile, access to clean water, Antenatal care, education, facilities, birth interval, & age at first delivery | 19 |
| 93. 2002 [133] |
- Nigeria 1990–1999 |
L | Ecological | Place of residence and literacy level | poor obstetric history (abortion, stillbirth and premature birth) | 19 |
| 94. 2002 [134] |
n = 85 Guinea-Bissau 1990 |
L | Case–control | distance from the regional hospital, region of residence, Birth interval, Distance to health center, health post in village & result of the birth | Age, parity, & Access to latrines | 18 |
| 95. 2002 [135] |
n = 104 Nigeria 1990–1999 |
L | XS | Age, parity, & Booking status | - | 13 |
| 96. 2001 [136] |
- Global 1998 |
- | Ecological | Fertility rate, immunization with DPT, Urban population, & female working in industry | - | 18 |
| 97. 2001 [137] |
- Global 1988–1997 |
- | Ecological | GNP per capita, physician and nurse per 1000 people, female literacy, & skilled birth attendance | - | 16 |
| 98. 2000 [138] |
- Global - |
Ecological | Income per capita, health expenditure, antenatal care, receiving trained assistance at childbirth, female gross primary-school enrollment rate, & female gross secondary-school enrollment rate | - | 17 | |
| 99. 1999 [139] |
- less developed countries 1970–1990 |
L | Ecological | education relative to men, age at first marriage, reproductive autonomy, GDP per capita, total fertility rate, economic growth, Contraceptive prevalence, population per doctor, Health attendants, & male to female ratio secondary school enrollment | Foreign calories per capita investment | 15 |
| 100. 1999 [140] |
n = 583 Accra-Ghana 1990–1997 |
L | XS | Vaginal delivery, postpartum timing of death, age, & formal education | Cesarean delivery, instrumental delivery, antepartum timing of death, intrapartum timing of death, residence, marital status, parity | 13 |
| 101. 1998 [141] |
n = 261 Pakistan 1991–1993 |
L | Case–control | Age, Parity, Previous history of fetal loss, access to electricity, accessibility of essential obstetric care, & Number of rooms in the house | Husbands literacy, & birth attendant | 20 |
| 102. 1998 [142] |
n = 121 India 1993–1995 |
L | Case–control | Overall distance travelled from home to appropriate treatment facility, distance of first health service contact, & distance between first heath service contact and appropriate treatment facility, place of delivery, type of attendants, & husbands education | Use of contraceptives, women education, age, & higher economic status | 18 |
| 103. 1997 [143] |
N = 218 Pakistan 1989–1992 |
L | Case–control | Household assets, Distance from nearest hospital, Housing Construction material, Availability of electricity, Water supply, Marital status, Age, Gravidity, & Obstetric History | Education, Husband’s education, Employment status | 21 |
| 104. 1997 [144] |
n = 152 Senegal 1986–1987 |
LM | Case–control | Medical equipment, late referral, no antenatal visits, Any complication during pregnancy, Previous C-section, Never treated previously, & Previously hospitalized | No one available at time of admission, Prenatal visit to a specialized center | 18 |
| 105. 1997 [145] |
- Global 1987—1990 |
- | Ecological | Human development index including life expectancy, education, & GDP per capita | - | 17 |
| 106. 1996 [146] |
n = 1341 England and Wales 1970–1985 |
H | XS | Age, & place of birth | - | 20 |
| 107. 1994 [147] |
- Global 1979- 1981 |
- | Ecological | a households without sanitation, total calories consumed, & total fat residual, | fat calories consumed, medical personnel available, no safe water, hospital beds available, literacy rate | 17 |
| 108. 1994 [148] |
n = 271 India 1984–1992 |
L | XS | Gestational age, Level of consciousness, & convulsions | - | 16 |
| 109. 1993 [149] |
159 Zimbabwe 1989–1990 |
LM | Case–control | Marital status in rural, head of household in rural, catholic religion in urban, still birth, & history of abortion in urban | Marital status, education, guardian family, religion, income, gravidity, parity, result of birth (live birth), wanted pregnancy, history of abortion | 17 |
Strobe-checklist tool was used for quality assessment of original studies
LMICs Low- and Middle-Income Countries, L Low income, LM Lower Middle income, UM Upper Middle income, H Higher income, XS Cross sectional study
Data analysis
The included studies were developed with diverse objectives, used various methods and different statistical techniques, and included participants with different characteristics and were widely distributed among countries. This diversity made formal meta-analysis almost impossible. Some of the included studies were developed with similar objectives, and participants had similar characteristics and used similar methods and measures, but we also classified the determinants of maternal mortality into three main individual, household, and community levels to be higher applicability for policymakers and researchers.
Classification of the included studies based on income levels of countries
We classified each original study based on low-, lower-middle-, upper-middle-, and high-income countries according to World Bank classification. Some points considered in this classification; for example, if a study in a country was in a specific income group for a some years and then its level changed for next years, we chose the income group that were for a longer period. In the study of Simo ˜es et al. [94], Brazil was in the upper-middle-income group for two years (2000–2001) and then changed as a lower-middle-income country in 2002; thus we considered Brazil in the upper-middle-income group. If a study included different countries in two different income groups, we chose the group with more countries. For example, in the study of Graham et al. [131], among 11 different countries, only two countries were in lower-middle group and the rest were in low-income group; so, we considered it as a low-income country. We also chose the last years of income level for the studies that used the same number of years for two different levels of income. For example, in the study of Taguchi et al. [77], Indonesia was lower-middle-income country for two years (1996 and 1997) and was low-income for the other two years (1998 and 1999), so we considered Indonesia as low-income country. Studies with more than two income groups in different countries were considered as global/regional studies, illustrated in the last column of Table 4.
Table 4.
Summary of determinants of maternal mortality according to the Table 2
A Associated, N Not associated, O Observational studies (including case–control, cross sectional & retrospective cohort studies), L Longitudinal studies (including prospective cohort, panel and time-series studies), E Ecological studies
aThese studies used more than two types of different income level groups among different countries. The colors shows the association of the determinants based on numbers of the studies, total sample sizes & sometimes quality of the included studies (
 There was significant relationship,
There was significant relationship,
 there was no consensus &
there was no consensus &
 there was not significant relationship). Strobe-checklist tool were used for quality assessment of these original studies
there was not significant relationship). Strobe-checklist tool were used for quality assessment of these original studies
Results
The results of this systematic review are structured here in two main sections; first, according to Tables 2 and 3, which are a summary of all included original studies and review articles, respectively, and provide a description of the characteristics of included studies. Then, maternal mortality determinants are reported for review articles and original studies, summarized at individual, household, and community levels by income groups in Table 4.
Description of the included studies
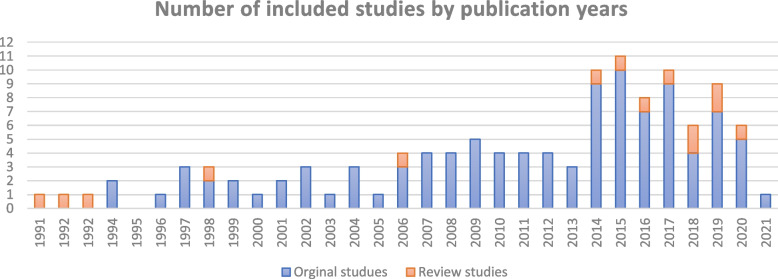
Of 121 included studies, 12 were review articles (Table 3) and the rest were original studies (Table 2) in which 33%, 28%, 27%, 10%, and 2% were ecological, case–control, cross-sectional, longitudinal (including prospective cohort, panel and time-series studies), and cohort studies, respectively. Among the 12 review articles, six of them with a total of 160 studies were conducted systematically and the rest were narrative reviews (Table 3). Most of the literature evaluated the determinants of maternal mortality globally with special focus on low- and lower-middle-income countries. Moreover, the results by countries show that most of the included original studies have been conducted in China, followed by Niagara and Indonesia (details provided in Fig. 2), and most of them were published after 2013 (Fig. 3).
Fig. 2.
Number of included studies by setting
Fig. 3.
Number of included studies by publication years during 1991–2021
Determinants of maternal mortality in the world
In this section, first the results of the review articles then the original study’s findings are reported based on determinant levels and income levels of countries.
Based on our review articles, some macro factors such as economic growth, poverty, inequality, improved water and sanitation, education, accessibility of health care services, etc. (details are shown in Table 3), and some micro factors such as age, parity, type of delivery, early marriage, etc. have led to maternal mortality.
Maternal mortality determinants based on individual, household, and community levels
Determinants at individual level mainly show the health status and reproductive-demographic characteristics of deceased mothers. A summary of the determinants of mothers who died due to pregnancy-related reasons, based on original studies, is described in Table 4. As shown in column three of the table, among demographic factors, maternal age over 34 or below 18 is one of the main factors affecting pregnancy-related deaths, and nearly 70% of 36 examined studies with 7632 aggregate deaths confirmed this association. In addition, higher gravidity and cesarean delivery (as opposed to natural delivery) were recognized as significant threatening factors in 90% and nearly 75% of the studies, respectively. Furthermore, the results of this review show that mothers attended by skilled birth personnel, under prenatal care, as well as educated women are less likely to die from pregnancy-related causes. Moreover, delay in seeking health services and making decisions for delivery in all the eight observational evidences and factors related to mothers’ health (including the history of underlying disease, medical comorbidities, having complications during pregnancy or postpartum period, and hospitalization during pregnancy) were significant contributors according to most studies. However, in a few studies, some variables such as BMI, race, skin color, and caste were not recognized as associated factors. In contrast, each of the factors of birth weight, substance misuse, nationality, and previous pregnancy history were significant factors in one study, which we refused to include in Table 4. At this level, there is no consensus on the effect of age at marriage, age at first birth, birth weight, and postnatal care coverage. Details about other determinants at this level were described in Table 4.
Determinants at household level show that improved water sources and sanitation systems were the main contributors in most studies. In addition, low family income or wealth, and rural residence were associated factors in nearly 87% and 70% of studies, respectively. Also in this level, access to electricity in all the evaluated studies, and higher levels of husband education were recognized as significant factors in 80% of the observational studies (details in Table 4). Other factors mainly related to the condition of living, including the type of flour and toilet, building material of the house, and type of family were the associated factors, which are not shown in Table 4.
At community or social levels, poor human resources in 73% of the examined studies, and poor accessibility or availability of health facilities (including the number of hospitals, primary health care, hospital beds, and equipment, etc.) in 79% of the 19 examined studies were the main contributors that threaten maternal health. Moreover, health expenditure shares (including higher share of out-of-pocket or private expenditures, and lower share of total health of GDP or public expenditures) and higher total fertility rate per woman were other associated factors in 89% and 77% of the included studies, respectively. In this category, there is no consensus on the effect of quality of services, and less use of contraception (details in Table 4). A few of the selected studies also recognized other factors such as life expectancy, need for emergency obstetric care, total calories consumed, and fat residuals as significant factors, which we refused to enter in Table 4. In terms of economic factors that were mainly studied in ecological studies, lower-income countries levels (GNP or GDP) in 89% of the studies, unemployment rate in all studies, and poverty in 57% of the examined studies were significant threatening factors. However, income inequality and foreign investment are not known as significant factors. In contrast, debt rate, agricultural production indices, and private-sector infrastructure were other contributors in a study, which we refused to enter in Table 4. In addition, results show that maternal mortality was also caused by social, political, and cultural factors. Thus, levels of education and governance (corruption index, instability, voice and accountability, etc.) were the main contributors in five ecological studies. Also, gender inequality and human development index both in four original studies were known as main factors in this category (details in Table 4). Also, other factors such as paved roads, annually published scientific papers, percentage of the indigenous population, and education efficiency were significant factors, which we refused to enter in Table 4.
Maternal mortality determinants based on income levels of countries
A summary of our findings is shown in Table 4. As it shows, the attributable risk of maternal death is varied based on income levels and development levels of countries; more than 80% of the examined studies and all four ecological studies found poor income levels of countries (GDP/GNP) and human development index strongly associated with maternal death, respectively.
Among the factors at individual levels, prenatal care, delay in decisions, type of delivery, and hospitalization during pregnancy in most studies (except the type of delivery in lower-middle income group) were significant factors in all different income levels. In six out of seven global studies, skilled birth attendance was a significant contributor in low-income, less developed or developing countries. Also, maternal education as another main factor, was an essential contributor in low and lower-middle-income countries, and more than 80% and 70% of the examined studies have shown a significant relationship, respectively. However, there is no consensus on this factor in upper-middle-income countries. Some factors like history of underlying disease, medical comorbidities, high-risk pregnancy, length of labor, and pregnancy stage were recognized as risk factors in low or lower-middle-income countries (Table 4).
Based on this review, most studies statistically accepted that less access to clean water and improved sanitation negatively affected maternal death in low and lower-middle-income countries, respectively. In addition, in poor countries, improvement in the availability or accessibility of health services and health expenditure shares were essential determinants in the reduction of maternal death. Based on our findings, reduction in the share of out-of-pocket and private health expenditures and increase in the share of total health expenditures as a percentage of GDP and public expenditures were most responsible for pregnancy-related deaths, particularly in low-income countries as well as other income groups. Moreover, the risk of pregnancy-related death was highly significant among the population below poverty line in all existing evidence, and the use of contraception in many studies in low-income countries. However, poverty in upper-middle-income countries was not significantly associated with maternal death. Moreover, gender inequality and gender empowerment measures (autonomy, economic empowerment, and attitudes towards violence) in low and lower-middle-income countries were associated contributors in most studies. However, gender empowerment measures did not affect maternal death in two ecological studies, and there is no consensus on the significance of gender inequality in our global studies. Details of the other variables is shown in Table 4.
Discussion
This study aimed to review and overview maternal mortality determinants in the world and categorize them based on income levels of countries. Our included studies show that most of these studies were conducted ecologically and were case–control studies and 58% of them were carried out in low and lower-middle-income countries.
According to the result of this study, maternal age, gravidity, type of delivery, education of mothers, pregnancy care, skilled birth attendance, and maternal health status are the main factors at individual level. At family level, factors such as access to improved water and sanitation, region of residence, family income or wealth, and other factors related to living conditions were significantly associated with maternal death. However, the systematic review conducted in Iran [156] failed to find the place of living as a risk factor because of having more access to primary health care among rural women in Iran. At community or social level, availability of health services, total fertility rate, health expenditures shares, income level, governance, inequality and education were main contributors.
Our review shows that women aged 18–34 years were less likely to die as compared with age groups of 35–49 or under 18 years. A possible reason for the high risk of maternal death among women aged 35–49 years is due to weakened uterus and anemia, and becoming pregnant is too risky for women older than 35 years and studies showed that the majority of women in this age group were not educated. Studies indicate that most maternal deaths occurred in women with no antenatal care and delay in seeking health services. This may be due to lack of awareness about the seriousness of maternal health. The type of delivery can also affect maternal mortality, as most cases of obstetric hemorrhage and emergency postpartum hysterectomy are associated with CS deliveries [75].
Among original studies, two observational studies in lower-middle income countries [93, 144], and an observational study in the west of Iran [93], as upper middle-income country, demonstrate that skilled birth attendance has no significant relationship with maternal mortality. However, it doesn’t seem that skilled birth attendance has no effects on maternal mortality at this income level as those studies were conducted with a small sample size and limited time span. A longitudinal study in Chile, as a lower middle-income level country, showed this factor as a significant contributor in adjusted models. Some global or regional studies, mainly including less developed or developing countries, accepted this factor [76, 130, 138].
Based on our findings, households’ access to improved water and sanitation especially in low-income countries were negatively associated with maternal death. In line with this, Benova et al. [15] suggested that women in households with poor sanitation were 3.14 times more likely to die compared to women with better sanitation. The concept is that poor access to sanitation and water can provide the conditions for the prevalence of infectious diseases, which can directly affect maternal death. Studies also show that access to improved sanitation is associated with income level of countries [79, 115]; a study shows that clean water and sanitation access improved by 14% due to economic growth in low and middle-income countries from 1990 to 2010 [73]. Based on WHO data [157], access to improved sanitation and water was always over 98% among high-income countries since 1990, while in low-income countries, access to clean water fluctuated around 46% to 66%, and access to sanitation fluctuated around 13% to 28% from 1990 to 2015.
Governance is one of the key factors that affects maternal mortality. Governance can be described as a set of traditions and conventions that determines the practice of authority in a particular country. It comprises not only the processes through which governments are selected, held accountable, monitored, and replaced, but also the capacity of governments to efficiently manage resources and formulate, implement, and enforce appropriate policies and regulations. In addition, governance regulates the level of respect received by the citizens and the state for conventions and laws that govern the economic and social interactions in the community. Through better governance, public spending can effectively and efficiently enhance health and education outcomes.
Some economic and health system-related factors such as the Gross National Income per capita and per capita government expenditure on health showed an inverse correlation with MMR. In contrast, private sector and out-of-pocket health expenditure showed a significant direct correlation with MMR: the more private sectors and out-of-pocket health expenditures in a country, the higher the MMR. Since appropriate government financing can ensure better access to some essential maternal health services, greater levels of health expenditure will be required for developing countries to achieve MDG on maternal mortality. Between 1995 and 2014, the average total health expenditure (%GDP) varied from 5% in low-middle income countries, 48% of which was paid by public expenditure, to nearly 11% in high-income countries, 61% of which was paid by public expenditure. Based on WHO statistics, the average out-of-pocket share (% total health expenditure) varied from nearly 41% in low-middle income countries to nearly 15% in high-income countries in the same period [158].
According to the literature, poverty positively affects maternal mortality as an economic factor, especially in the low-income countries. According to the evidence, poverty is linked to maternal mortality through malnutrition [99]. Malnutrition has been associated with anemia that is one of the main causes of maternal death [159]. Malnutrition may lead to chronic iron deficiency and anemia, which can make women prone to hemorrhage and infections [160]. Furthermore, women who experience malnutrition early in life are usually smaller, which increases the likelihood of obstructed labor [160].
Also, low human development index (HDI) in all evaluated studies was recognized as a significant contributing factor. HDI is one of the powerful indexes, which is a geometric means with three dimensions of life expectancy at birth, education, and GDP per capita. Much evidence shows that MMR reflects the general health status of a country and its development [130].
Moreover, education as a social factor is the other main contributor. As seen in Table 4, among 20 studies that examined the effects of education on maternal mortality at community level, only one did not confirm this. This shows that education is influential in reducing maternal mortality. Educated women are more exposed to having an informed reproductive behavior, and they access reproductive health facilities frequently and timely. When women are educated, they increasingly improve their status, gain autonomy, awareness, responsibility, and control their fertility and reproductive activities such as in the use of contraceptives, prenatal and postnatal care, and health facility delivery [13]. Literature also shows that education in low and lower-middle-income countries is essential, which may have happened due to the low level of social and economic infrastructures in them.
Other factors including households’ income, employment, urbanization, inequalities, gender empowerment, human resource, availability of services were the other main factors particularly in less developed or developing countries (Table 4).
To the best of our knowledge, this is the first systematic review to present a robust summary of individual and ecological determinants of maternal mortality in the world based on income level of the countries. We used a sensitive search strategy in different sources, and finally identified 121 studies (109 original studies and 12 review articles). However, this review has several potential limitations. As the main limitation of this study, we only included studies in English with access to full-text documents. To compensate this, we did a rigorous search on different electronic databases, journals, and paper references, and the abstracts of excluded studies were reviewed to reduce bias. As with any systematic review, we may have missed some studies due to relatively a short list of search terms. Also, some studies did not provide access to the full text and thus they had to be excluded from this review. However, we minimized this by exhausting the search process through key terms, and the search strategy employed multiple academic and grey literature databases. As another limitation, all included studies had analytical observational and review design, so the cause-effect relation between determinants and maternal mortality could not be established. The results of this review can help researchers to understand the main determinants of maternal mortality based on income level of the countries and provide an appropriate space for research. This study can also provide comprehensive views for policymakers to reduce maternal mortality.
Conclusions
This review aims to comprehensively show the determinants of maternal mortality. The results of this study demonstrate the individual-level factors (e.g., age and parity), household-level factors such as region of residence, access to improved water etc., and community-level factors such as socio-economic, cultural, and health care system factors associated with maternal mortality. Based on extracted determinants, providing health services by making them affordable and available, access to quality health care, access to prenatal care, family planning care, and emergency obstetric care, increasing education levels, improving the condition of living and infrastructures, and the use of contraception can play an important role in the reduction of maternal mortality. Further studies are recommended to reach a consensus regarding certain determinants such as age at marriage, postnatal care coverage, etc.
Acknowledgements
Not applicable.
Authors’ contributions
MT, RZ conceived and planned the study. MT, RZ performed the data analysis. RZ, MT wrote the initial draft of the manuscript. MT and AH searched the literature. MT, RZ, and AH applied inclusion and exclusion criteria, extracted data, and appraised study quality. AH commented on this draft and critically revised the draft. All authors read and approved the final draft of the manuscript.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors completed the ICMJE Unified Competing Interest form (available upon request from the corresponding author), and declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Maryam Tajvar, Email: mtajvar@tums.ac.ir.
Alireza Hajizadeh, Email: a_hajizadeh@razi.tums.ac.ir.
Rostam Zalvand, Email: zalvandr@alumnus.tums.ac.ir.
References
- 1.Lawson GW, Keirse MJ. Reflections on the maternal mortality millennium goal. Birth. 2013;40(2):96–102. doi: 10.1111/birt.12041. [DOI] [PubMed] [Google Scholar]
- 2.Sliwa K, Anthony J. Late maternal deaths: a neglected responsibility. Lancet. 2016;387(10033):2072–2073. doi: 10.1016/S0140-6736(16)30391-9. [DOI] [PubMed] [Google Scholar]
- 3.Moazzeni MS. Maternal mortality in the Islamic Republic of Iran: on track and in transition. Matern Child Health J. 2013;17(4):577–580. doi: 10.1007/s10995-012-1043-6. [DOI] [PubMed] [Google Scholar]
- 4.WHO, UNICEF, UNFPA, World Bank Group, and the United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Geneva: World Health Organization; 2015.
- 5.World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization. 2019. https://apps.who.int/iris/handle/10665/327595. License: CC BY-NC-SA 3.0 IGO.
- 6.Stokoe U. Determinants of maternal mortality in the developing world. Aust N Z J Obstet Gynaecol. 1991;31(1):8–16. doi: 10.1111/j.1479-828x.1991.tb02754.x. [DOI] [PubMed] [Google Scholar]
- 7.Organization WH. Trends in maternal mortality: 1990–2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. 2015. [Google Scholar]
- 8.World Health Organization. Maternal mortality rates: a tabulation of available data. 2nd Edn. WHO document No FHE186.3, 1986: I.
- 9.World Health Organization. The WHO application of ICD-10 to deaths during pregnancy, childbirth and the puerperium: ICD-MM. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 10.McCarthy J, Maine D. A framework for analyzing the determinants of maternal mortality. Stud Fam Plann. 1992;23(1):23–33. [PubMed] [Google Scholar]
- 11.Doris C. The WHO Application of ICD-10 to deaths during pregnancy, childbirth and the puerperium: ICD-MM. 2013. [Google Scholar]
- 12.Wall LL. Dead mothers and injured wives: the social context of maternal morbidity and mortality among the Hausa of northern Nigeria. Studies in family planning. 1998. pp. 341–59. [PubMed] [Google Scholar]
- 13.Yakubu Y, Nor NM, Abidin EZ. A systematic review of micro correlates of maternal mortality. Rev Environ Health. 2018;33(2):147–161. doi: 10.1515/reveh-2017-0050. [DOI] [PubMed] [Google Scholar]
- 14.Odekunle FF. Maternal Mortality Burden: The Influence of Socio-Cultural Factors. Int J Health Sci Res (IJHSR) 2016;6(12):316–324. [Google Scholar]
- 15.Benova L, Cumming O, Campbell OM. Systematic review and meta-analysis: association between water and sanitation environment and maternal mortality. Tropical Med Int Health. 2014;19(4):368–387. doi: 10.1111/tmi.12275. [DOI] [PubMed] [Google Scholar]
- 16.Ganatra BR, Hirve SS. Unsafe motherhood: the determinants of maternal mortality. J Indian Med Assoc. 1995;93(2):47–48. [PubMed] [Google Scholar]
- 17.Li Q, Fottler MD. Determinants of maternal mortality in rural China. Health Serv Manage Res. 1996;9(1):45–54. doi: 10.1177/095148489600900105. [DOI] [PubMed] [Google Scholar]
- 18.Makokha AE. Medico-social and socio-demographic factors associated with maternal mortality at Kenyatta National Hospital, Nairobi, Kenya. J Obstet Gynaecol East Cent Africa. 1991;9(1):3–6. [PubMed] [Google Scholar]
- 19.Rajaram P, Agrawal A, Swain S. Determinants of maternal mortality: a hospital based study from south India. Indian J Matern Child Health. 1995;6(1):7–10. [PubMed] [Google Scholar]
- 20.Vallenas G. Maternal mortality in Peru. Rev Peru Poblacion. 1993;3:33–56. [PubMed] [Google Scholar]
- 21.Högberg U, Wall S, Broström G. The impact of early medical technology on maternal mortality in late 19th century Sweden. Int J Gynecol Obstet. 1986;24(4):251–261. doi: 10.1016/0020-7292(86)90081-0. [DOI] [PubMed] [Google Scholar]
- 22.Kaunitz AM, Spence C, Danielson T, Rochat RW, Grimes DA. Perinatal and maternal mortality in a religious group avoiding obstetric care. Am J Obstet Gynecol. 1984;150(7):826–831. doi: 10.1016/0002-9378(84)90457-5. [DOI] [PubMed] [Google Scholar]
- 23.Urassa E, Lindmark G, Nystrom L. Maternal mortality in Dar es Salaam, Tanzania: Socio-economic, obstetric history and accessibility of health care factors. Afr J Health Sci. 1995;2(1):242–249. [PubMed] [Google Scholar]
- 24.Kwast BE, Liff JM. Factors associated with maternal mortality in Addis Ababa, Ethiopia. Int J Epidemiol. 1988;17(1):115–121. doi: 10.1093/ije/17.1.115. [DOI] [PubMed] [Google Scholar]
- 25.Ni H, Rossignol AM. Maternal deaths among women with pregnancies outside of family planning in Sichuan, China. Epidemiology. 1994;5:490–4. [PubMed] [Google Scholar]
- 26.Mbizvo MT, Fawcus S, Lindmark G, Nyström L, Group MMS Operational factors of maternal mortality in Zimbabwe. Health Policy Plan. 1993;8(4):369–78. [Google Scholar]
- 27.Caldwell JC. Cultural and social factors influencing mortality levels in developing countries. Ann Am Acad Pol Soc Sci. 1990;510(1):44–59. [Google Scholar]
- 28.Caldwell JC. Education as a factor in mortality decline an examination of Nigerian data. Population studies. 1979. pp. 395–413. [Google Scholar]
- 29.Okwerekwu FE. Maternal mortality in Nigerian women aged 35 years and above. J Obstet Gynaecol Res. 1991;17(1):37–44. doi: 10.1111/j.1447-0756.1991.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 30.Jain AK. Measuring the effect of fertility decline on the maternal mortality ratio. Stud Fam Plann. 2011;42(4):247–260. doi: 10.1111/j.1728-4465.2011.00288.x. [DOI] [PubMed] [Google Scholar]
- 31.Amini-Rarani M, Mansouri A, Nosratabadi M. Decomposing educational inequality in maternal mortality in Iran. Women Health. 2021;61(3):244–253. doi: 10.1080/03630242.2020.1856294. [DOI] [PubMed] [Google Scholar]
- 32.Arregocés SN, Molina RT. Inequalities and sociodemographic characteristics of maternal mortality in la Guajira, Colombia, 2010–2012. Rev Panam Salud Publica. 2015;37(4–5):239–244. [PubMed] [Google Scholar]
- 33.Herrera Torres MDC, Cruz Burguete JL, Robledo Hernández GP, Gómez GM. The household economy: A determinant of maternal death among indigenous women in Chiapas, Mexico. Rev Panam Salud Publica. 2006;19(2):69–78. doi: 10.1590/s1020-49892006000200001. [DOI] [PubMed] [Google Scholar]
- 34.Salazar E, Buitrago C, Molina F, Alzate CA. Trend in mortality from external causes in pregnant and postpartum women and its relationship to socioeconomic factors in Colombia, 1998–2010. Rev Panam Salud Publica. 2015;37(4–5):225–231. [PubMed] [Google Scholar]
- 35.Yepes FJ, Gómez JG, Zuleta JJ, Londoño JL, Acosta-Reyes JL, Sánchez-Gómez LH, et al. Healthcare and maternal morbidity and mortality: a hospital-based case-control study in two regions of Colombia (Bogotá and Antioquia), 2009–2011. Cad Saude Publica. 2016;32(11):e00080215. doi: 10.1590/0102-311X00080215. [DOI] [PubMed] [Google Scholar]
- 36.Powell-Jackson T, Gao Y, Ronsmans C, Zhou H, Wang Y, Fang H. Health-system determinants of declines in maternal mortality in China between 1996 and 2013: a provincial econometric analysis. Lancet. 2015;386:S15. [Google Scholar]
- 37.Leite RMB, Araújo TVBD, Albuquerque RMD, Andrade ARSD, Duarte Neto PJ. Risk factors for maternal mortality in an urban area of Northeast Brazil. Cad Saude Publica. 2011;27(10):1977–85. doi: 10.1590/s0102-311x2011001000011. [DOI] [PubMed] [Google Scholar]
- 38.Liang J, Li W, Wang Y, Zhou G, Wu Y, Zhu J, et al. Analysis of maternal mortality in China from 1996 to 2000. Zhonghua Fu Chan Ke Za Zhi. 2003;38(5):257–260. [PubMed] [Google Scholar]
- 39.Audu L, Ekele B. A ten year review of maternal mortality in Sokoto, northern Nigeria. West Afr J Med. 2002;21(1):74–76. [PubMed] [Google Scholar]
- 40.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 41.Uo G. Critical appraisal checklist for a systematic review. 2014. [Google Scholar]
- 42.Sesunan AS, Respati SH, Sulistyowati S. Maternal Mortality in Klaten Regency (Determinant Factors Analysis) J Matern Child Health. 2021;6(2):183–196. [Google Scholar]
- 43.Li D, Yu C, Song C, Ning W, Xu Y, Ge H, et al. Maternal mortality ratio in Jiangsu Province, China: recent trends and associated factors. BMC Pregnancy Childbirth. 2021;21(1):447. doi: 10.1186/s12884-021-03897-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhatia M, Dwivedi LK, Banerjee K, Bansal A, Ranjan M, Dixit P. Pro-poor policies and improvements in maternal health outcomes in India. BMC Pregnancy Childbirth. 2021;21(1):389. doi: 10.1186/s12884-021-03839-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yaya S, Anjorin SS, Adedini SA. Disparities in pregnancy-related deaths: Spatial and Bayesian network analyses of maternal mortality ratio in 54 African countries. BMJ Global Health. 2021;6(2):e004233. doi: 10.1136/bmjgh-2020-004233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Noor S, Wahid N, Ali S, Ali S. Maternal Mortality: A 5-year analysis at a District Headquarter Hospital in Pakistan. J Ayub Med Coll Abbottabad: JAMC. 2020;32 1(4):S655–S8. [PubMed] [Google Scholar]
- 47.Meh C, Thind A, Terry AL. Ratios and determinants of maternal mortality: a comparison of geographic differences in the northern and southern regions of Cameroon. BMC Pregnancy Childbirth. 2020;20(1):194. doi: 10.1186/s12884-020-02879-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Syairaji M, Salim MF. Spatial Analysis for Maternal Mortality in Special Region of Yogyakarta, Indonesia. International Proceedings the 2nd International Scientific Meeting on Health Information Management (ISMoHIM) 2020.
- 49.Bomela NJ. Maternal mortality by socio-demographic characteristics and cause of death in South Africa: 2007–2015. BMC Public Health. 2020;20(1):157. doi: 10.1186/s12889-020-8179-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang X, Ye Y, Fu C, Dou G, Ying X, Qian M, et al. Anatomy of provincial level inequality in maternal mortality in China during 2004–2016: A new decomposition analysis. BMC Public Health. 2020;20(1):758. doi: 10.1186/s12889-020-08830-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cameron L, Suarez DC, Cornwell K. Understanding the determinants of maternal mortality: An observational study using the Indonesian Population Census. PloS one. 2019;14(6):e0217386. doi: 10.1371/journal.pone.0217386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guerra AB, Guerra LM, Probst LF, Gondinho BVC, Ambrosano GMB, Melo EA, et al. Can the primary health care model affect the determinants of neonatal, post-neonatal and maternal mortality? A study from Brazil. BMC Health Services Research. 2019;19(1):133. doi: 10.1186/s12913-019-3953-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK. Rural-urban differences in severe maternal morbidity and mortality in the us, 2007–15. Health Aff. 2019;38(12):2077–2085. doi: 10.1377/hlthaff.2019.00805. [DOI] [PubMed] [Google Scholar]
- 54.Meh C, Thind A, Ryan B, Terry A. Levels and determinants of maternal mortality in northern and southern Nigeria. BMC Pregnancy Childbirth. 2019;19(1):417. doi: 10.1186/s12884-019-2471-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Palimbo A, Salmah AU, Sari A. Determinant factors of maternal mortality from 2016 to 2017 a case-control study in Banjar regency. Indian J Public Health Res Development. 2019;10(1):1188–1192. [Google Scholar]
- 56.Rane TM, Mahanta TG, Baruah M, Baruah SD. Epidemiological study of maternal death in Assam. Clin Epidemiol Global Health. 2019;7(4):634–640. [Google Scholar]
- 57.Sara J, Haji Y, Gebretsadik A. Determinants of maternal death in a pastoralist area of borena zone, oromia region, Ethiopia: Unmatched case-control study. Obstet Gynecol Int. 2019;2019:5698436. doi: 10.1155/2019/5698436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moyo N, Makasa M, Chola M, Musonda P. Access factors linked to maternal deaths in Lundazi district, Eastern Province of Zambia: a case control study analysing maternal death reviews. BMC Pregnancy Childbirth. 2018;18(1):101. doi: 10.1186/s12884-018-1717-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nelson DB, Moniz MH, Davis MM. Population-level factors associated with maternal mortality in the United States, 1997–2012. BMC Public Health. 2018;18(1):1007. doi: 10.1186/s12889-018-5935-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tlou B. Underlying determinants of maternal mortality in a rural South African population with high HIV prevalence (2000–2014): A population-based cohort analysis. PloS one. 2018;13(9):e0203830. doi: 10.1371/journal.pone.0203830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ntoimo LF, Okonofua FE, Ogu RN, Galadanci HS, Gana M, Okike ON, et al. Prevalence and risk factors for maternal mortality in referral hospitals in Nigeria: a multicenter study. Int J Womens Health. 2018;10:69. doi: 10.2147/IJWH.S151784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Astatikie G, Limenih MA, Kebede M. Maternal and fetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture. BMC Pregnancy Childbirth. 2017;17(1):117. doi: 10.1186/s12884-017-1302-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ariyo O, Ozodiegwu ID, Doctor HV. The influence of the social and cultural environment on maternal mortality in Nigeria: Evidence from the 2013 demographic and health survey. PLoS ONE. 2017;12(12):e0190285. doi: 10.1371/journal.pone.0190285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ren Y, Qian P, Duan Z, Zhao Z, Pan J, Yang M. Disparities in health system input between minority and non-minority counties and their effects on maternal mortality in Sichuan province of western China. BMC Public Health. 2017;17(1):750. doi: 10.1186/s12889-017-4765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hou L, Hellerstein S, Vitonis A, Zou L, Ruan Y, Wang X, et al. Cross sectional study of mode of delivery and maternal and perinatal outcomes in mainland China. PLoS ONE. 2017;12(2):e0171779. doi: 10.1371/journal.pone.0171779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fransiska RD, Respati SH, Mudigdo A. Analysis of Maternal Mortality Determinants in Bondowoso District, East Java. J Matern Child Health. 2017;2(1):76–88. [Google Scholar]
- 67.Sanhueza A, Roldán JC, Ríos-Quituizaca P, Acuña MC, Espinosa I. Social inequalities in maternal mortality among the provinces of Ecuador. Rev Panam Salud Publica. 2017;41:e97. doi: 10.26633/RPSP.2017.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lan C-W, Tavrow P. Composite measures of women’s empowerment and their association with maternal mortality in low-income countries. BMC Pregnancy Childbirth. 2017;17(2):337. doi: 10.1186/s12884-017-1492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sembiring M. Maternal Mortality Determinants in Refferal Hospital: Three Years Retrospective Study. Qanun Medika Med J Faculty Med Muhammadiyah Surabaya. 2017;1(02). 10.30651/qm.v1i02.491. [DOI]
- 70.Azuh DE, Azuh AE, Iweala EJ, Adeloye D, Akanbi M, Mordi RC. Factors influencing maternal mortality among rural communities in southwestern Nigeria. Int J Womens Health. 2017;9:179. doi: 10.2147/IJWH.S120184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Esteves-Pereira AP, Deneux-Tharaux C, Nakamura-Pereira M, Saucedo M, Bouvier-Colle M-H, do Carmo Leal M. Caesarean delivery and postpartum maternal mortality: a population-based case control study in Brazil. PloS one. 2016;11(4):e0153396. doi: 10.1371/journal.pone.0153396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Karimzaei T, Zareban I, Jamalzae A-Q, Darban F, Bakhshani KD, Balouchi A. frequency of maternal mortality in urban and rural areas of Iranshahr county (Southeast of Iran) in 2009–2013: A retrospective study. J Clin Diagn Res JCDR. 2016;10(8):QC14. doi: 10.7860/JCDR/2016/19700.8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bishai DM, Cohen R, Alfonso YN, Adam T, Kuruvilla S, Schweitzer J. Factors contributing to maternal and child mortality reductions in 146 low-and middle-income countries between 1990 and 2010. PLoS ONE. 2016;11(1):e0144908. doi: 10.1371/journal.pone.0144908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Egbe T, Dingana T, Halle-Ekane G, Atashili J, Nasah B. Determinants of maternal mortality in Mezam division in the north west region of Cameroon: a community-based case control study. Int J Trop Dis Health. 2016;15:1–15. [Google Scholar]
- 75.Uzuncakmak C, Ozcam H. Association between maternal mortality and cesarean section: Turkey experience. PLoS ONE. 2016;11(11):e0166622. doi: 10.1371/journal.pone.0166622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bayati M, Vahedi S, Esmaeilzadeh F, Kavosi Z, Jamali Z, Rajabi A, et al. Determinants of maternal mortality in Eastern Mediterranean region: A panel data analysis. Med J Islam Repub Iran. 2016;30:360. [PMC free article] [PubMed] [Google Scholar]
- 77.Atuhaire R, Kaberuka W. Factors Contributing to Maternal Mortality in Uganda. Afr J Econ Rev. 2016;4(2):43–57. [Google Scholar]
- 78.Godefay H, Byass P, Graham WJ, Kinsman J, Mulugeta A. Risk factors for maternal mortality in rural Tigray, northern Ethiopia: A case-control study. PLoS ONE. 2015;10(12):e0144975. doi: 10.1371/journal.pone.0144975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pinzón-Flórez CE, Fernández-Niño JA, Ruiz-Rodríguez M, Idrovo ÁJ, López AAA. Determinants of performance of health systems concerning maternal and child health: a global approach. PLoS ONE. 2015;10(3):e0120747. doi: 10.1371/journal.pone.0120747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nair M, Kurinczuk J, Brocklehurst P, Sellers S, Lewis G, Knight M. Factors associated with maternal death from direct pregnancy complications: a UK national case–control study. BJOG Int J Obstet Gynaecol. 2015;122(5):653–62. doi: 10.1111/1471-0528.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mbiniwaya M. Review of Maternal Deaths Audit in Effia Nkwanta Regional Hospital in the Western Region: University of Ghana. 2015. [Google Scholar]
- 82.Bauserman M, Lokangaka A, Thorsten V, Tshefu A, Goudar SS, Esamai F, et al. Risk factors for maternal death and trends in maternal mortality in low-and middle-income countries: a prospective longitudinal cohort analysis. Reprod Health. 2015;12(2):S5. doi: 10.1186/1742-4755-12-S2-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sajedinejad S, Majdzadeh R, Vedadhir A, Tabatabaei MG, Mohammad K. Maternal mortality: a cross-sectional study in global health. Glob Health. 2015;11(1):4. doi: 10.1186/s12992-015-0087-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Godefay H, Byass P, Kinsman J, Mulugeta A. Understanding maternal mortality from top–down and bottom–up perspectives: Case of Tigray Region, Ethiopia. J Global Health. 2015;5(1):010404. doi: 10.7189/jogh.05.010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ikhtiar M, Yasir Y. Analysis of Maternal Mortality Determinants in Gowa District South Sulawesi Province. Indo Am J Public Health. 2015;3(3):113–115. [Google Scholar]
- 86.Weyesa J, Tadesse A, Eba T, Minta M, Gudu H. Prevalence and risk factors associated with maternal mortality in Mizan-Aman Hospital, Bench Maji, Southwest Ethiopia. J Womens Health Care. 2015;4(274):2167–0420.1000. [Google Scholar]
- 87.Du Q, Lian W, Næss Ø, Bjertness E, Kumar BN, Shi S-H. The trends in maternal mortality between 1996 and 2009 in Guizhou, China: ethnic differences and associated factors. J Huazhong Univ Sci Technol [Med Sci]. 2015;35(1):140–6. doi: 10.1007/s11596-015-1403-8. [DOI] [PubMed] [Google Scholar]
- 88.Zhang J, Zhang X, Qiu L, Zhang R, Hipgrave DB, Wang Y, et al. Maternal deaths among rural–urban migrants in China: a case–control study. BMC Public Health. 2014;14(1):512. doi: 10.1186/1471-2458-14-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maruthappu M, Ng K, Williams C, Atun R, Agrawal P, Zeltner T. The association between government healthcare spending and maternal mortality in the European Union, 1981–2010: a retrospective study. BJOG Int J Obstet Gynaecol. 2015;122(9):1216–24. doi: 10.1111/1471-0528.13205. [DOI] [PubMed] [Google Scholar]
- 90.Kanyighe C, Tadesse E, Changole J, Bakuwa E, Malunga E, Channon A, et al. Determinants of post-partum maternal mortality at Queen Elizabeth Central Hospital, Blantyre, Malawi: a case-control study 2001–2002. Afr J Reprod Health. 2008;12(3):35–48. [PubMed] [Google Scholar]
- 91.Pacagnella RC, Cecatti JG, Parpinelli MA, Sousa MH, Haddad SM, Costa ML, et al. Delays in receiving obstetric care and poor maternal outcomes: results from a national multicentre cross-sectional study. BMC Pregnancy Childbirth. 2014;14(1):159. doi: 10.1186/1471-2393-14-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yego F, D’Este C, Byles J, Williams JS, Nyongesa P. Risk factors for maternal mortality in a Tertiary Hospital in Kenya: a case control study. BMC Pregnancy Childbirth. 2014;14(1):38. doi: 10.1186/1471-2393-14-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Poorolajal J, Alafchi B, Vosoogh RN, Hamzeh S, Ghahramani M. Risk factors for maternal mortality in the west of Iran: a nested case-control study. Epidemiol Health. 2014;36:e2014028. doi: 10.4178/epih/e2014028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Simões PP, Almeida RMV. Maternal mortality and accessibility to health services by means of transit-network estimated traveled distances. Matern Child Health J. 2014;18(6):1506–1511. doi: 10.1007/s10995-013-1391-x. [DOI] [PubMed] [Google Scholar]
- 95.Ikhtiar M. Study on Health Social Determinants as Cause of Maternal Mortality in Gowa District, South Sulawesi. Int J Sci Res Publ. 2013;1–6.
- 96.Kuruvilla S, Schweitzer J, Bishai D, Chowdhury S, Caramani D, Frost L, et al. Success factors for reducing maternal and child mortality. Bull World Health Organ. 2014;92:533–544. doi: 10.2471/BLT.14.138131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Souza JP, Gülmezoglu AM, Vogel J, Carroli G, Lumbiganon P, Qureshi Z, et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): a cross-sectional study. Lancet. 2013;381(9879):1747–1755. doi: 10.1016/S0140-6736(13)60686-8. [DOI] [PubMed] [Google Scholar]
- 98.Gidey G, Bayray A, Gebrehiwot H. Patterns of maternal mortality and associated factors; A case-control study at public hospitals in Tigray region, Ethiopia, 2012. Int J Pharm Sci Res. 2013;4(5):1918. [Google Scholar]
- 99.Hernandez JC, Moser CM. Community level risk factors for maternal mortality in Madagascar. African J Reprod Health. 2013;17(4):118–29. [PubMed] [Google Scholar]
- 100.Chu K, Cortier H, Maldonado F, Mashant T, Ford N, Trelles M. Cesarean section rates and indications in sub-Saharan Africa: a multi-country study from Medecins sans Frontieres. PLoS ONE. 2012;7(9):e44484. doi: 10.1371/journal.pone.0044484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zolala F, Heidari F, Afshar N, Haghdoost AA. Exploring maternal mortality in relation to socioeconomic factors in Iran. Singapore Med J. 2012;53(10):684. [PubMed] [Google Scholar]
- 102.Koch E, Thorp J, Bravo M, Gatica S, Romero CX, Aguilera H, et al. Women’s education level, maternal health facilities, abortion legislation and maternal deaths: a natural experiment in Chile from 1957 to 2007. PLoS ONE. 2012;7(5):e36613. doi: 10.1371/journal.pone.0036613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.You F, Huo K, Wang R, Xu D, Deng J, Wei Y, et al. Maternal mortality in Henan Province, China: changes between 1996 and 2009. PLoS ONE. 2012;7(10):e47153. doi: 10.1371/journal.pone.0047153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Karlsen S, Say L, Souza J-P, Hogue CJ, Calles DL, Gülmezoglu AM, et al. The relationship between maternal education and mortality among women giving birth in health care institutions: analysis of the cross sectional WHO Global Survey on Maternal and Perinatal Health. BMC Public Health. 2011;11(1):606. doi: 10.1186/1471-2458-11-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tajik P, Nedjat S, Afshar NE, Changizi N, Yazdizadeh B, Azemikhah A, et al. Inequality in maternal mortality in Iran: an ecologic study. Int J Prev Med. 2012;3(2):116. [PMC free article] [PubMed] [Google Scholar]
- 106.Muldoon KA, Galway LP, Nakajima M, Kanters S, Hogg RS, Bendavid E, et al. Health system determinants of infant, child and maternal mortality: A cross-sectional study of UN member countries. Glob Health. 2011;7(1):42. doi: 10.1186/1744-8603-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hussein J, Bell J, Iang MD, Mesko N, Amery J, Graham W. An appraisal of the maternal mortality decline in Nepal. PLoS ONE. 2011;6(5):e19898. doi: 10.1371/journal.pone.0019898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pirkle CM, Fournier P, Tourigny C, Sangaré K, Haddad S. Emergency obstetrical complications in a rural African setting (Kayes, Mali): the link between travel time and in-hospital maternal mortality. Matern Child Health J. 2011;15(7):1081–1087. doi: 10.1007/s10995-010-0655-y. [DOI] [PubMed] [Google Scholar]
- 109.Gupta SD, Khanna A, Gupta R, Sharma NK, Sharma ND. Maternal mortality ratio and predictors of maternal deaths in selected desert districts in Rajasthan: a community-based survey and case control study. Womens Health Issues. 2010;20(1):80–85. doi: 10.1016/j.whi.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 110.Ensor T, Cooper S, Davidson L, Fitzmaurice A, Graham WJ. The impact of economic recession on maternal and infant mortality: lessons from history. BMC Public Health. 2010;10(1):727. doi: 10.1186/1471-2458-10-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kamilya G, Seal SL, Mukherji J, Bhattacharyya SK, Hazra A. Maternal mortality and cesarean delivery: an analytical observational study. J Obstet Gynaecol Res. 2010;36(2):248–253. doi: 10.1111/j.1447-0756.2009.01125.x. [DOI] [PubMed] [Google Scholar]
- 112.Du Q, Nass O, Bergsjo P, Kumar BN. Determinants for high maternal mortality in multiethnic populations in western China. Health Care Women Int. 2009;30(11):957–970. doi: 10.1080/07399330903052137. [DOI] [PubMed] [Google Scholar]
- 113.Abraha MW, Nigatu TH. Modeling trends of health and health related indicators in Ethiopia (1995–2008): a time-series study. Health Res Policy and Syst. 2009;7(1):29. doi: 10.1186/1478-4505-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Fernández MÁL, Cavanillas AB, Dramaix-Wilmet M, Soria FS, Campos JDMD, Guibert DH. Increase in maternal mortality associated with change in the reproductive pattern in Spain: 1996–2005. J Epidemiol Commun Health. 2009;63(6):433–8. doi: 10.1136/jech.2008.082735. [DOI] [PubMed] [Google Scholar]
- 115.Alvarez JL, Gil R, Hernández V, Gil A. Factors associated with maternal mortality in Sub-Saharan Africa: an ecological study. BMC Public Health. 2009;9(1):462. doi: 10.1186/1471-2458-9-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kullima AA, Kawuwa MB, Audu BM, Geidam AD, Mairiga AG. Trends in maternal mortality in a tertiary institution in Northern Nigeria. Ann Afr Med. 2009;8(4):221–4. doi: 10.4103/1596-3519.59575. [DOI] [PubMed] [Google Scholar]
- 117.Evjen-Olsen B, Hinderaker SG, Lie RT, Bergsjø P, Gasheka P, Kvåle G. Risk factors for maternal death in the highlands of rural northern Tanzania: a case-control study. BMC Public Health. 2008;8(1):52. doi: 10.1186/1471-2458-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Philibert M, Deneux-Tharaux C, Bouvier-Colle MH. Can excess maternal mortality among women of foreign nationality be explained by suboptimal obstetric care? BJOG Int J Obstet Gynaecol. 2008;115(11):1411–8. doi: 10.1111/j.1471-0528.2008.01860.x. [DOI] [PubMed] [Google Scholar]
- 119.Hounton S, Menten J, Ouédraogo M, Dubourg D, Meda N, Ronsmans C, et al. Effects of a Skilled Care Initiative on pregnancy-related mortality in rural Burkina Faso. Tropical Med Int Health. 2008;13(s1):53–60. doi: 10.1111/j.1365-3156.2008.02087.x. [DOI] [PubMed] [Google Scholar]
- 120.Olopade F, Lawoyin T. Maternal mortality in a Nigerian maternity hospital. Afr J Biomed Res. 2008;11(3):267–73.
- 121.Chowdhury ME, Botlero R, Koblinsky M, Saha SK, Dieltiens G, Ronsmans C. Determinants of reduction in maternal mortality in Matlab, Bangladesh: a 30-year cohort study. Lancet. 2007;370(9595):1320–1328. doi: 10.1016/S0140-6736(07)61573-6. [DOI] [PubMed] [Google Scholar]
- 122.Aggarwal A, Pandey A, Bhattacharya B. Risk factors for maternal mortality in Delhi slums: A community-based case-control study. Indian J Med Sci. 2007;61(9):517. [PubMed] [Google Scholar]
- 123.Ramos S, Karolinski A, Romero M, Mercer R. A comprehensive assessment of maternal deaths in Argentina: translating multicentre collaborative research into action. Bull World Health Organ. 2007;85(8):615–622. doi: 10.2471/BLT.06.032334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li J, Luo C, Deng R, Jacoby P, De Klerk N. Maternal mortality in Yunnan, China: recent trends and associated factors. BJOG Int J Obstet Gynaecol. 2007;114(7):865–74. doi: 10.1111/j.1471-0528.2007.01362.x. [DOI] [PubMed] [Google Scholar]
- 125.Andoh S, Umezaki M, Nakamura K, Kizuki M, Takano T. Correlation between national income, HIV/AIDS and political status and mortalities in African countries. Public Health. 2006;120(7):624–633. doi: 10.1016/j.puhe.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 126.Dumont A, Gaye A, Bernis LD, Chaillet N, Landry A, Delage J, et al. Facility-based maternal death reviews: effects on maternal mortality in a district hospital in Senegal. Bull World Health Organ. 2006;84:218–24. doi: 10.2471/blt.05.023903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McAlister C, Baskett TF. Female education and maternal mortality: a worldwide survey. J Obstet Gynaecol Can. 2006;28(11):983–990. doi: 10.1016/S1701-2163(16)32294-0. [DOI] [PubMed] [Google Scholar]
- 128.Sullivan SA, Hill EG, Newman RB, Menard MK. Maternal-fetal medicine specialist density is inversely associated with maternal mortality ratios. Am J Obstet Gynecol. 2005;193(3):1083–1088. doi: 10.1016/j.ajog.2005.05.085. [DOI] [PubMed] [Google Scholar]
- 129.Anand S, Bärnighausen T. Human resources and health outcomes: cross-country econometric study. Lancet. 2004;364(9445):1603–1609. doi: 10.1016/S0140-6736(04)17313-3. [DOI] [PubMed] [Google Scholar]
- 130.Buor D, Bream K. An analysis of the determinants of maternal mortality in sub-Saharan Africa. J Womens Health. 2004;13(8):926–938. doi: 10.1089/jwh.2004.13.926. [DOI] [PubMed] [Google Scholar]
- 131.Graham WJ, Fitzmaurice AE, Bell JS, Cairns JA. The familial technique for linking maternal death with poverty. Lancet. 2004;363(9402):23–27. doi: 10.1016/S0140-6736(03)15165-3. [DOI] [PubMed] [Google Scholar]
- 132.Taguchi N, Kawabata M, Maekawa M, Maruo T, Dewata L. Influence of socio-economic background and antenatal care programmes on maternal mortality in Surabaya. Indo Tropical Med Int Health. 2003;8(9):847–852. doi: 10.1046/j.1365-3156.2003.01101.x. [DOI] [PubMed] [Google Scholar]
- 133.Adamu YM, Salihu HM, Sathiakumar N, Alexander GR. Maternal mortality in Northern Nigeria: a population-based study. Eur J Obstet Gynecol Reprod Biol. 2003;109(2):153–159. doi: 10.1016/s0301-2115(03)00009-5. [DOI] [PubMed] [Google Scholar]
- 134.Høj L, Da Silva D, Hedegaard K, Sandström A, Aaby P. Factors associated with maternal mortality in rural Guinea-Bissau. A longitudinal population-based study. BJOG Int J Obstet Gynaecol. 2002;109(7):792–9. [PubMed] [Google Scholar]
- 135.Okonta P, Okali U, Otoide V, Twomey D. Exploring the causes of and risk factors for maternal deaths in a rural Nigerian referral hospital. J Obstet Gynaecol. 2002;22(6):626–629. doi: 10.1080/0144361021000020394. [DOI] [PubMed] [Google Scholar]
- 136.Herrera LR, Kakehashi M. An international data analysis on the level of maternal and child health in relation to socioeconomic factors. Hiroshima J Med Sci. 2001;50(1):9–16. [PubMed] [Google Scholar]
- 137.Robinson JJ, Wharrad H. The relationship between attendance at birth and maternal mortality rates: an exploration of United Nations’ data sets including the ratios of physicians and nurses to population, GNP per capita and female literacy. J Adv Nurs. 2001;34(4):445–455. doi: 10.1046/j.1365-2648.2001.01773.x. [DOI] [PubMed] [Google Scholar]
- 138.Shiffman J. Can poor countries surmount high maternal mortality? Stud Fam Plann. 2000;31(4):274–289. doi: 10.1111/j.1728-4465.2000.00274.x. [DOI] [PubMed] [Google Scholar]
- 139.Shen C, Williamson JB. Maternal mortality, women’s status, and economic dependency in less developed countries: a cross-national analysis. Soc Sci Med. 1999;49(2):197–214. doi: 10.1016/s0277-9536(99)00112-4. [DOI] [PubMed] [Google Scholar]
- 140.Obed S, Wilson J, Sakay A. Determinants of maternal mortality in eclampsia at Korle Bu Teaching Hospital Accra, Ghana. Ghana Med J. 1999;33(3):886–889. [Google Scholar]
- 141.Midhet F, Becker S, Berendes HW. Contextual determinants of maternal mortality in rural Pakistan. Soc Sci Med. 1998;46(12):1587–1598. doi: 10.1016/s0277-9536(97)10137-x. [DOI] [PubMed] [Google Scholar]
- 142.Ganatra B, Coyaji K, Rao V. Too far, too little, too late: a community-based case-control study of maternal mortality in rural west Maharashtra, India. Bull World Health Organ. 1998;76(6):591. [PMC free article] [PubMed] [Google Scholar]
- 143.Fikree FF, Midhet F, Sadruddin S, Berendes HW. Maternal mortality in different Pakistani sites: ratios, clinical causes and determinants. Acta Obstet Gynecol Scand. 1997;76(7):637–645. doi: 10.3109/00016349709024603. [DOI] [PubMed] [Google Scholar]
- 144.Garenne M, Mbaye K, Bah MD, Correa P. Risk factors for maternal mortality: a case-control study in Dakar hospitals (Senegal) Afr J Reprod Health. 1997;1:14–24. [PubMed] [Google Scholar]
- 145.Lee K-S, Park S-C, Khoshnood B, Hsieh H-L, Mittendorf R. Human development index as a predictor of infant and maternal mortality rates. J Pediatr. 1997;131(3):430–3. doi: 10.1016/s0022-3476(97)80070-4. [DOI] [PubMed] [Google Scholar]
- 146.Ibison JM, Swerdlow AJ, Head JA, Marmot M. Maternal mortality in England and Wales 1970–1985: an analysis by country of birth. BJOG Int J Obstet Gynaecol. 1996;103(10):973–80. doi: 10.1111/j.1471-0528.1996.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 147.Hertz E, Hebert JR, Landon J. Social and environmental factors and life expectancy, infant mortality, and maternal mortality rates: results of a cross-national comparison. Soc Sci Med. 1994;39(1):105–114. doi: 10.1016/0277-9536(94)90170-8. [DOI] [PubMed] [Google Scholar]
- 148.Arora R, Ganguli R, Swain S, Oumachigui A, Rajaram P. Determinants of maternal mortality in eclampsia in India. Aust N Z J Obstet Gynaecol. 1994;34(5):537–539. [Google Scholar]
- 149.Mbizvo MT, Fawcus S, Lindmark G, Nyström L, Group MMS Maternal mortality in rural and urban Zimbabwe: social and reproductive factors in an incident case-referent study. Soc Sci Med. 1993;36(9):1197–205. doi: 10.1016/0277-9536(93)90240-5. [DOI] [PubMed] [Google Scholar]
- 150.Takaeb AEL. Exploration of Socio-Cultural Determinants of Maternal Mortality in Indonesia. In 5th International Conference on Tourism, Economics, Accounting, Management and Social Science (TEAMS 2020). Atlantis Press; 2020. p. 482–87.
- 151.Zalvand R, Yaseri M, Mosadeghrad AM, Tajvar M. Determinants of maternal mortality in iran 1990–2015: A longitudinal study. Tehran Univ Med J. 2019;77(2):82–91. [Google Scholar]
- 152.Wirsiy FS, Ako-Arrey DE, Njukeng PA, Tendongfor N, Manjong FT, Lukong LK, et al. Maternal Mortality in Cameroon: A Critical Review of its Determinants. J Gynaecol Neonatal. 2019;2(1):106. [Google Scholar]
- 153.Najafizada SAM, Bourgeault IL, Labonté R. Social Determinants of Maternal Health in Afghanistan: A Review. Cent Asian J Global Health. 2017;6(1):240. doi: 10.5195/cajgh.2017.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Cameron L, Cornwell K. Understanding the Causes of Maternal Mortality in Indonesia: A Review of Research on the Determinants and Trends in Maternal Mortality in the Asia-Pacific Region. 2016. [Google Scholar]
- 155.Vadnais M, Sachs B. Maternal Mortality with Cesarean Delivery: A Literature Review. Semin Perinatol. 2006;30:242–6. [PubMed] [Google Scholar] [DOI] [PubMed]
- 156.Zalvand R, Tajvar M, Pourreza A, Asheghi H. Determinants and causes of maternal mortality in Iran based on ICD-MM: a systematic review. Reprod Health. 2019;16(1):16. doi: 10.1186/s12978-019-0676-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Srinivas KSN, Murali R. Risk factors associated with pih: Adjusted odds ratios by multiple logistic regression analysis. Int J Pharm Res. 2019;11:89–95. [Google Scholar]
- 158.Muhammad Ardian CL, Davik FI. Antenatal care quality analysis using the european foundation quality for management method in the hospitals in surabaya. Indian J Public Health Res Dev. 2019;10(10):907–911. [Google Scholar]
- 159.Brabin BJ, Hakimi M, Pelletier D. An analysis of anemia and pregnancy-related maternal mortality. J Nutr. 2001;131(2):604S–S615. doi: 10.1093/jn/131.2.604S. [DOI] [PubMed] [Google Scholar]
- 160.Rush D. Nutrition and maternal mortality in the developing world–. Am J Clin Nutr. 2000;72(1):212S–S240. doi: 10.1093/ajcn/72.1.212S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.