Abstract
American Indians are at increased risk for cardiovascular disease (CVD) in adulthood, and levels of physical activity and body mass index (BMI) associate with CVD risk. Recent research indicates that one’s mindset may play a role in determining health behaviors and outcomes. In a sample of 105 American Indian college students, greater growth health mindset associated with lower BMI. Bootstrapping analyses revealed a significant indirect effect of health mindset on BMI through levels of physical activity. These findings suggest that interventions aiming to promote growth health mindsets may be successful in reducing risk for CVD for American Indian college students.
American Indian (AI) populations are at disproportionate risk for obesity and related diseases including cardiovascular disease (Espey et al., 2014), both of which are positively affected by engagement in physical activity (Slater et al., 2010). One’s decision to engage in physical activity may be affected by their mindset about health. A “mindset” is a group of beliefs or assumptions held by an individual about the world which influences both their perceptions and actions. There are two unique types of mindsets: fixed and growth. These divergent mindsets can change the way in which different individuals respond to the same set of circumstances. An individual with a fixed mindset believes that certain attributes such as intelligence are not modifiable, whereas an individual with a growth mindset believes that intelligence can be changed through effort or behavior. Mindsets have been shown to be predictors of important outcomes across numerous domains including in the context of stress responses (Jamieson, Mendes, Blackstock & Schmader, 2010; Jamieson, Nock & Mendes, 2012; John-Henderson, Rheinschmidt, Mendoza-Denton & Francis, 2014), education (Yeager et al., 2019; Yeager et al., 2016), and personal relationships (Dweck, 2012; Van Tongeren & Burnett, 2018; Yeager et al., 2011). In all of these domains holding a “growth” mindset associated with more adaptive and productive outcomes, particularly in the face of difficulties or challenge, compared to holding a “fixed” mindset.
Mindsets themselves appear to be susceptible to intervention, and shifts towards growth mindsets have associated with positive changes in outcomes and behaviors (Halperin, Russell, Trzesniewski, & Dweck, 2011; Heyman & Dweck, 1992; Howe et al., 2019; Yeager et al., 2019). Positive changes from a growth mindset appear to help those who face well documented systematic disadvantages such as low socioeconomic status (Sisk et al., 2018) suggesting this cognitive tool may be particularly beneficial for disadvantaged or stigmatized groups. As noted previously, mindsets can also shape perceptions and behavior, and so interventions that aim to change behaviors, may increase their efficacy by promoting a growth orientation.
In the domain of health, findings from a growing body of work suggest that mindsets affect motivation and effort towards the initiation of health behaviors. For example, growth mindsets about fitness predict both self-reported previous exercise habits and future exercise intentions (Orvidas, Burnette, & Russell, 2018). Mindsets about weight have also shown to predict health-relevant outcomes. Individuals who believe weight is malleable exhibit better self-regulation following a dieting setback (Burnette, 2010), and inducing growth mindsets about weight experimentally associated with a positive change in dietary choices in a lab setting (Ehrlinger, Burnette, Park, Harrold, & Orvidas, 2017). Separately, there is initial evidence that individual differences in lay beliefs about the underlying cause of obesity may contribute to incidence of obesity and to differences in behavioral patterns related to risk for obesity. McFerran and Mukhopadhyay (2013) found that individuals who believed obesity was the result of lack of exercise, rather than a result of dietary choices, consumed more food in an experimental setting and were more likely to be overweight compared to individuals who believed that poor diet was the main cause of obesity.
In line with this, an individual’s mindset about health as a broad construct, or the degree to which they believe that health is malleable and susceptible to change via effort and behavior, may affect the likelihood that they will engage in health behaviors that may improve health and reduce risk for disease. Health mindsets may be particularly important for populations who are at increased risk for future ill-health. Previous work found that the relationship between growth health mindsets and health relevant outcomes was stronger for African Americans compared to Non-Hispanic White Americans (Thomas, Burnette & Hoyt, 2019) and it has been suggested that individuals from more vulnerable populations may be more likely to adopt a fixed view of health because of their life circumstances (Mueller, Rowe & Zuckerman, 2017).
Based on this work, it is possible that the relationship between health mindsets and health-relevant outcomes may be particularly evident for health disparity populations. American Indians (AIs) are disproportionately affected by cardiovascular disease (Espey, Jim & Cobb, 2014), and risk for CVD is related to both physical activity levels and one’s body mass index (BMI). Individuals who are overweight or obese early in the life-span are at increased risk for cardiovascular disease in adulthood (Baker, Olsen & Sorensen, 2007; Must, Jacques, Dallal, Bajema, & Dietz, 1995), and in adults increased body mass index (BMI) associates with an increase in various CVD risk factors (Loprinzi, Crespo, Andersen & Smit, 2015). Levels of physical activity are consistently associated with BMI (Levin et al., 2003), and previous work indicates an association between mindsets about health and exercise frequency (Orvidas, Burnette, Russell, 2018). As such, physical activity is one health behavior that could decrease risk for CVD for AIs, acting as a mediator between mindsets about health and health-relevant outcomes such as BMI.
As noted previously, previous work has examined the relationship between lay beliefs or mindsets about particular health outcomes or health-behaviors (i.e. obesity, fitness, weight, exercise). However, mindsets about health more broadly, have not been investigated as a predictor of objectively measured health behaviors outside of the laboratory and health-relevant outcomes. As such, the work described here, makes a theoretical contribution, by considering whether one’s view of health broadly speaking, as fixed or modifiable through effort and behavior, predicts a health behavior in daily life- objective levels of physical activity over a week, and body mass index. The proposed conceptual model is displayed in Figure 1. The use of an objective measure of physical activity, in place of self-reported exercise, advances existing work methodologically since self-report measures may be biased and be more reflective of intentions rather than actual behavioral patterns. Further, to date, this is the first study to explore health mindsets and their role in shaping risk factors for disease in AIs, an at-risk population (Espey et al. 2014). Specifically, we examine the relationship between health mindsets and BMI in AIs, exploring the possibility that growth health mindsets may associate with lower BMI, in part by associating with a greater amount of physical activity.
Figure 1.
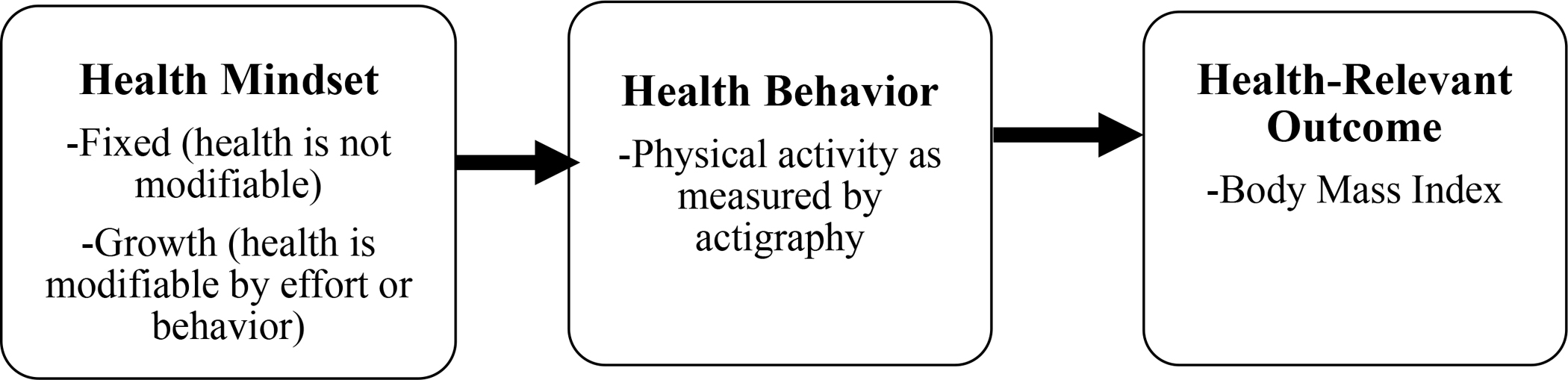
Full conceptual model
Methods.
AI students were recruited through flyers placed across a large state university. All procedures were approved by the University Institutional Review Board. Participants were paid $30 for their participation in this research. The study was advertised as an investigation focused on understanding the experience of AI college students. Interested participants were invited to the lab for a one-hour session. After providing informed consent, they completed a screening questionnaire to determine eligibility for the study. Students with self-reported sleep or chronic health conditions were excluded from this research. A research assistant obtained measures of height and weight for calculation of body mass index. Participants then completed a demographic questionnaire and a health mindset scale. Finally, research assistants placed a wrist accelerometer (Actigraph GT9X link, Pensascola, FL) on the participants’ non-dominant hand. Accelerometers were initialized using ActiLife (version 6, Penascola, FL) in 60 second epochs. The Actigraph GT9X link is a device that detects and records movement through the use of an accelerometer. Participants wore the watch continuously for 7 days, after which they returned to the lab to return the device and received compensation for their participation.
Measures
Health Mindsets.
To measure health mindsets, we used a modified version of previously used scales developed by Dweck and colleagues (Dweck, Chiu & Hong, 1995 & Dweck, 2006). Participants were instructed to report their agreement with each of the following statements on a 6-point Likert scale (1-strongly agree, 6- strongly disagree: “Your body has a certain amount of health, and you really can’t do much to change it,” “Your health is something about you that you can’t change very much,” and “You can try to make yourself feel better, but you can’t really change your basic health.” Higher scores on the health mindset scale reflect growth health mindsets, while lower numbers reflect a fixed health mindset.
Actigraphy measured Physical Activity.
The sleep period was excluded and the levels of physical activity were defined according to the cut-off points outlined by Freedson et al, 1998. Light physical activity was defined as between 101 and 1951 counts per minute, and activity greater than or equal to 1952 counts per minute was defined as moderate to vigorous physical activity (MVPA) (Cain et al. 2013; Lindamer et al., 2008). Participants were excluded from analyses if the accelerometers were not worn for at least 10 hours per day (excluding the sleep period) for at least 5 days (n=3).
Body Mass Index.
A trained research assistant obtained a measure of height and weight in order to calculate participant Body Mass Index (BMI).
Current Depressive Symptoms.
Previous work documents a relationship between depressive symptoms and BMI (Noh, Kwon, Park & Kim, 2015; Xie, Chou, Johnson & Krailo, 2002). Based on this relationship, we used Beck’s Depression Inventory (BDI-II) as a measure of current depressive symptoms to examine relationships between depressive symptoms and our outcomes of interest. The BDI-II is a 21-item questionnaire widely used to assess subclinical and clinical depression (Beck, Steer, Ball & Ranieri, 1996). Each item includes 4 response options. As an example, participants are asked to select which of the following 4 statements most accurately reflects how they have been feeling in the last 2 weeks, including today: (0) I am not particularly discouraged about the future, (2) I feel I have nothing to look forward to, and (3) I feel the future is hopeless and that things cannot improve. A total score is derived by summing all of the responses, and higher scores reflect more depressive symptoms (possible range = 0–63).
Socioeconomic status.
Past work indicates a relationship between a socioeconomic status (SES) and BMI (Bradshaw, Kent, Henderson & Setar, 2017) and SES was one of the strongest moderators of the effects of a growth mindset intervention (Sisk et al., 2018). Based on these relationships, we collected a measure of subjective socioeconomic status using the MacArthur’s scale of subjective socioeconomic status (Adler, Epel, Castellazzo, & Ickovics, 2000) to investigate relationships between SES and our measures of interest. Participants were asked to place an “X” on a nine-rung ladder to indicate their perception of their Socioeconomic Status (SES) relative to the rest of the United States. Participants were told that those at the top of the ladder had the most money, the most education, and the most respected jobs, whereas those at the bottom were the worst off, with the least money, the least education, and the least respected job or no job (M(SD)= 5.85[1.83]).
Statistical Analyses
Statistical analyses were conducted using SPSS (IBM: Version 24). Linear regression models were used to conduct the main analyses. Continuous covariates were centered prior to use in statistical models.
Health mindset was modeled as a continuous predictor. We tested our primary hypotheses using a linear regression with health mindset predicting BMI. Next, to test for indirect effects of health mindsets on BMI through levels of measured physical activity, we used a bootstrapping approach (Preacher & Hayes, 2004). Specifically, a point estimate of the indirect effect was derived from the mean of 5000 estimates of the indirect pathways, and 95% confidence intervals (CIs) were computed using the cutoffs for the 2.5% highest and lowest scores of the distribution. Indirect effects were considered significant when the CI did not include 0.
Results
Participants were 105 AI college students ranging in age from 18–38 years of age (M[SD]=21.56[4.04]). Fifty-eight percent of the participants identified as female. Our reported analyses include participants with all of the predictors. Descriptive statistics for the sample are listed in Table 1. We examined bivariate relationship between our variables of interest. Our outcome variable, BMI, was significantly related to depressive symptoms, health mindsets, light physical activity, and moderate to vigorous physical activity. Bivariate correlations between main variables of interest are reported in Table 2.
Table 1.
Descriptive Statistics (N=105).
| Mean | SD | % | |
|---|---|---|---|
|
| |||
| Age | 21.56 | 4.04 | |
| Sex (% female) | 58% | ||
| Subjective SES (range:1–10) | 5.05 | 2.03 | |
| Current depressive symptoms | 11.75 | 8.29 | |
| Health Mindset (range:3–18) | 10.03 | 4.57 | |
| Light Physical Activity (min/day) | 160.32 | 63.18 | |
| Moderate to Vigorous Physical Activity (min/day) | 55.33 | 33.82 | |
| Body Mass Index | 26.43 | 5.17 | |
Note: SES: Socioeconomic Status
Table 2.
Correlation Matrix for Key Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1.Age | -- | .06 | −.03 | .03 | .01 | .02 | −.01 | −.07 |
| 2.Gender | -- | .01 | −.04 | −.03 | −.10 | −.07 | −.05 | |
| 3.Subjective SES | -- | −.10 | .10 | −.18 | .05 | −.10 | ||
| 4. Depressive symptoms | -- | −.22* | .12 | .25* | .20* | |||
| 5. Body Mass Index | -- | −.58** | −.66** | −.75** | ||||
| 6.Health Mindset | -- | .36** | .48** | |||||
| 7. LPA/week | -- | .65** | ||||||
| 8. MVPA /week | -- | |||||||
Note: Gender: Male=1, Female=2, SES= Socioeconomic Status, LPA= Light Physical Activity, MVPA= Moderate to Vigorous Physical Activity
p < .05 (two-tailed).
p < .01 (two-tailed).
Health mindset and levels of physical activity
In a linear regression model, participants’ health mindset predicted levels of both light and moderate to vigorous physical activity (β = .36 t(97) = 3.74, p <.001, R2 = 0.13) and (β = .47, t(97) = 5.34, p <.001, R2 = 0.23) respectively. Specifically, growth mindset was related to higher levels of both light and moderate to vigorous physical activity.
Health mindset and BMI
In a separate linear regression, participants’ health mindset associated with BMI (β = −.58, t(97) = −6.94, p <.001, R2 = 0.33), with growth mindset associating with lower BMI.
Role of Physical activity levels in relationship between health mindset and BMI
Using the previously described method (Preacher & Hayes, 2004), we found a significant indirect effect of health mindset on BMI through levels of both light and moderate to vigorous activity (indirect effect (SE)=−.21 (.05), 95% CI = [−.31, −.11]) and (indirect effect (SE)=−.36(.07), 95% CI = [−.50, −.23]) respectively.
Discussion
To our knowledge, the findings reported here represent the first investigation of the relationship between general views of health as fixed or modifiable (i.e. health mindsets), an objective measure of physical activity outside of the lab, and a marker of disease risk, BMI, in a health disparity population, American Indians. By examining mindsets about the plasticity of health broadly speaking, this work is focused on a predictor that is upstream from the focus of previous investigations in this area (i.e. mindsets or lay beliefs about specific health behaviors or health outcomes). This novel focus is important since engagement in a health behavior may not depend specifically on their beliefs or mindsets about a particular health behavior or condition, but instead may be driven by the degree to which an individual believes that their general health is fixed or modifiable.
The findings from this research provide initial evidence that for AI college students, differences in health mindset (i.e. the degree to which one views health as fixed) are associated with differences in BMI, and this relationship is in part accounted for by differences in actigraphy derived measures of physical activity. Specifically, a “growth” mindset of health is linked to lower BMI and higher levels of physical activity. The pattern of our findings are in line with relationships observed previously indicating that mindset shapes behaviors and effort (Dweck, 2006; Mangels, Butterfield, Lamb, Good & Dweck, 2006; Meppelder, Hodes, Kef & Schuengel, 2014; Mueller & Dweck, 1998), physiological and psychological responses (Jamieson, Mendes, Blackstock, & Schmader, 2010; John-Henderson et al., 2014; John-Henderson et al., 2015) and measures of academic performance (Broda et al., 2018).
While there is considerable existing research on the ability for mindsets to shape outcomes across multiple domains, these findings add to a relatively new focus on mindsets about health. Our data indicates that in AI college students, one’s mindset about health (i.e. fixed or modifiable) associates with differences in a risk factor for future CVD, body mass index (BMI). Importantly, our findings point to a potential behavioral pathway that contributes to this association. By objectively measuring levels of physical activity over the course of a week, we found evidence that a growth health mindset associated with higher levels of light and moderate to vigorous physical activity over the monitoring period. Given previous work indicating that brief interventions aiming to shift mindsets towards a growth orientation associated with positive changes in outcomes that persisted over time (Walton & Cohen, 2011;Yeager et al., 2019; Yeager et al., 2016), it is possible that similar interventions designed to promote growth health mindsets may positively affect levels of physical activity, and in doing so may reduce disease risk for at-risk populations. For example, based on the accessibility and demonstrated feasibility of mindset interventions (Walton & Cohen, 2011), researchers have highlighted the potential for health mindset interventions (i.e. promoting growth health mindsets) to be used by health care providers to improve health outcomes and have identified health mindset research as an important avenue of future research (Mueller, Rowe & Zuckerman, 2017; Sujka, St Peter & Mueller, 2018).
While there are significant strengths to this research including use of actigraphy-derived measure of physical activity and focus on a health disparity population, there are also important limitations to note. First, while the American Indian sample is a strength of this research given the disproportionate incidence of CVD in this population, it is unknown whether similar relationships would be observed across other racial or ethnic groups. Further, participants in this sample were relatively young. Future research should investigate these relationships later in the life-span when risk for CVD increases. At the same time, identification of individuals who are at risk early in life would allow for prevention before disease is present. Additionally, our sample was comprised of American Indians in a college setting. As such it remains unknown whether these relationships would be affected by environmental context such as whether individuals are living in an urban environment or whether they live in a tribal community on a reservation. It is also important to note that modelling mediation analyses with cross-sectional data could provide biased and misleading results (Maxwell & Cole, 2007). Future research should investigate these relationships using a longitudinal design to better understand causal relationships between mindset and health behavior. Finally, future work should aim for a larger sample size. In spite of these limitations, these findings provide support for the development of interventions focused on shifting mindsets as an upstream factor that may precede health behaviors, which in turn shape markers associated with disease risk.
Funding
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number P20GM103474. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Baker JL, Olsen LW, Sorensen TI (2007) Childhood body-mass index and the risk of coronary heart disease in adulthood. New England Journal of Medicine 357(23): 2329–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broda M, Yun J, Schneider B, et al. (2018) Reducing Inequality in Academic Success for Incoming College Students: A Randomized Trial of Growth Mindset and Belonging Interventions. Journal of Research on Educational Effectiveness 11(3): 317–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette JL (2010) Implicit theories of body weight: Entity beliefs can weigh you down. Personality and Social Psychology Bulletin 36(3): 410–422. [DOI] [PubMed] [Google Scholar]
- Dweck CS, Chiu C, Hong Y (1995) Implicit theories and their role in judgments and reactions: A world from two perspectives. Psychological Inquiry 6(4): 267–285. [Google Scholar]
- Dweck C (2006). Mindset: The New Psychology of Success. New York, NY: Random House Publishing Group. [Google Scholar]
- Dweck CS, Chiu CY, Hong YY (1995) Implicit Theories: Elaboration and extension of the model. Psychological Inquiry 6: 322–333. [Google Scholar]
- Dweck CS (2006) Mindset: The new psychology of success. New York, NY: US: Random House. [Google Scholar]
- Dweck CS (2012) Mindsets and Human Nature: Promoting Change in the Middle East, the Schoolyard, the Racial Divide, and Willpower. American Psychologist 67(8):614–622. [DOI] [PubMed] [Google Scholar]
- Espey DK. Jim MA, Cobb N, et al. (2014). Leading causes of death and all-cause mortality in American Indians and Alaska natives. American Journal of Public Health 104: S303–S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlinger J, Burnette J, Park J, Harrold M, & Orvidas K. (2017). Incremental theories of weight and healthy eating behavior. Journal of Applied Social Psychology 47(6): 320–330. [Google Scholar]
- Freedson PS, Melanson E, Sirard J (1998) Calibration of the computer science and applications, Inc. accelerometer. Medical &Science in Sport & Exercise 30(5): 777–781. [DOI] [PubMed] [Google Scholar]
- Halperin E, Russell AG, Trzesniewski KH, Dweck CS (2011) Promoting the Middle East peace process by changing beliefs about group malleability. Science 333(6050):1767–9. [DOI] [PubMed] [Google Scholar]
- Jamieson JP, Mendes WB, Blackstock E, et al. (2010) Turning the knots in your stomach into bows: Reappraising arousal improves performance on the GRE. Journal of Experimental Social Psychology 46(1): 208–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson JP, Nock MK, Mendes WB (2012) Mind over matter: Reappraising arousal improves cardiovascular and cognitive responses to stress. Journal of Experimental Psychology: General 141(3): 417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John-Henderson NA, Rheinschmidt ML, & Mendoza-Denton R (2014) Cytokine responses and math performance: the role of stereotype disconfirmation and stress reappraisals. Journal of Experimental Social Psychology 56: 203–206. [Google Scholar]
- John-Henderson NA, Stellar JE, Mendoza-Denton R, Francis DD (2015) The role of interpersonal processes in shaping inflammatory responses to social-evaluation. Biological Psychology 110: 134–137. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Reeder BA, Elliot S, et al. (2012) Body mass index and risk of cardiovascular disease, cancer and all-cause mortality. Canadian journal of Public Health, 103(2), 147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton GM, Cohen GL (2011) A brief social-belonging intervention improves academic and health outcomes of minority students. Science 331: 1447–1451. [DOI] [PubMed] [Google Scholar]
- Levin S, Lowry R, Brown DR, et al. (2003). Physical activity and body mass index among U.S. Adolescents. Youth Risk Behavior Survey, 1999. Archives of Pediatric Adolescent Medicine 157(8): 816–820. [DOI] [PubMed] [Google Scholar]
- Loprinzi PD, Crespo CJ, Andersen RE, et al. (2015) Association of Body Mass Index with Cardiovascular Disease Biomarkers. American Journal of Preventive Medicine 48(3): 338–344. [DOI] [PubMed] [Google Scholar]
- Mangels JA, Butterfield B, Lamb J, et al. (2006) Why do beliefs about intelligence influence learning success? A social cognitive neuroscience model. Social Cognitive and Affective Neuroscience 1(2): 75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods 12: 23–44. [DOI] [PubMed] [Google Scholar]
- Mcferran B, & Mukhopadhyay A. (2013). Lay Theories of Obesity Predict Actual Body Mass. Psychological Science 24(8): 1428–1436. [DOI] [PubMed] [Google Scholar]
- Meppelder Hodes MW, Kef S, and Schuengel C (2014) Expecting Change: Mindset of Staff Supporting Parents with Mild Intellectual Disabilities. Research in Developmental Disabilities 35(12): 260–268. [DOI] [PubMed] [Google Scholar]
- Mueller CM, Dweck CS (1998) Praise for intelligence can undermine children’s motivation and performance. Journal of Personality and Social Psychology 75(1): 33–52 [DOI] [PubMed] [Google Scholar]
- Must A, Jacques PF, Dallal GE, et al. (1992) Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. New England Journal of Medicine 327(19): 1350–1355. [DOI] [PubMed] [Google Scholar]
- Mueller C, Rowe ML, Zuckerman B (2017). Mindset matters for parents and adolescents. JAMA Pediatrics 171: 415–416. [DOI] [PubMed] [Google Scholar]
- Noh JW, Kwon YD, Park J, & Kim J. (2015). Body mass index and depressive symptoms in middle aged and older adults. BMC Public Health 15: 310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orvidas K, Burnette J, Russell V (2018) Mindsets applied to fitness: Growth beliefs predict exercise efficacy, value and frequency. Psychology of Sport & Exercise 36: 156–161. [Google Scholar]
- Paunesku D, Walton GM, Romero C, Smith EN, Yeager DS, Dweck CS (2015) Mindset interventions are scalable interventions for academic underachievement. Psychological Science (26)6: 784–793. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments and Computers 36: 717–731. [DOI] [PubMed] [Google Scholar]
- Sisk VF, Burgoyne AP, Sun J, Butler JL, & Macnamara BN (2018). To what extent and under which circumstances are growth mind-sets important to academic achievement? Two meta-analyses. Psychological Science, 29(4): 549–571. [DOI] [PubMed] [Google Scholar]
- Sujka J, St Peter S, Mueller C (2018). Do health beliefs affect pain perception after pectus excavatum repair? Pediatric Surgery International 34(12): 1363–1367. [DOI] [PubMed] [Google Scholar]
- Thomas FN, Burnette JL, & Hoyt CL (2019). Mindsets of health and healthy eating intentions. Journal of Applied Social Psychology, 49(6): 372–380. [Google Scholar]
- Van Tongeren DR, Burnette JL (2018) Do you believe happiness can change? An investigation of the relationship between happiness mindsets, well-being and satisfaction. The Journal of Positive Psychology 13(2): 101–109. [Google Scholar]
- Walton GM, Cohen GL (2011). A brief social-belonging intervention improves academic and health outcomes of minority students Science 331 (6023):1447–1451. [DOI] [PubMed] [Google Scholar]
- Xie B, Chou C, Johnson CA, Krailo MD. (2002). Effects of perceived peer isolation and social support on the relationship between body mass index and depressive symptoms. American Journal of Epidemiology 155: S3. [DOI] [PubMed] [Google Scholar]
- Yeager DS, Romero C, Paunesku D, et al. (2016) Using design thinking to improve psychological interventions: the case of the growth mindset during the transition to high school. Journal of Educational Psychology 108(3): 374–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, Hanselma P, Walton GM, et al. (2019) A national experiment reveals when a growth mindset improves achievement. Nature, 573, 364–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, Walton GM, Brady ST, et al. (2016) Teaching a lay theory before college narrows achievement gaps at scale. Proceedings of the National Academy of Sciences of the United States of America 113 E3341–E3348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, Trzesniewski K, Tim K, et al. (2011) Adolescents’ Implicit Theories Predict Desire for Vengeance After Peer Conflicts: Correlational and Experimental Evidence. Developmental Psychology 47(4): 1090–1107. [DOI] [PubMed] [Google Scholar]


