Abstract
The COVID-19 pandemic has caused financial stress and disrupted daily life more quickly than any prior economic downturn and on a scale beyond any prior natural disaster. This study aimed to assess the impact of the pandemic on psychological distress and identify vulnerable groups using longitudinal data to account for pre-pandemic mental health status. Clinically significant psychological distress was assessed with the Kessler-6 in a national probability sample of adults in the United States at two time points, February 2019 (T1) and May 2020 (T2). To identify increases in distress, psychological distress during the worst month of the past year at T1 was compared with psychological distress over the past 30-days at T2. Survey adjusted logistic regression was used to estimate associations of demographic characteristics at T1 (gender, age, race, and income) and census region at T2 with within-person increases in psychological distress.
The past-month prevalence of serious psychological distress at T2 was as high as the past-year prevalence at T1 (10.9% vs. 10.2%). Psychological distress was strongly associated across assessments (X2(4) = 174.6, p < .0001). Increase in psychological distress above T1 was associated with gender, age, household income, and census region. Equal numbers of people experienced serious psychological distress in 30-days during the pandemic as did over an entire year prior to the pandemic. Mental health services and research efforts should be targeted to those with a history of mental health conditions and groups identified as at high risk for increases in distress above pre-pandemic levels.
Keywords: COVID-19 pandemic, Mental health, Psychological distress, Longitudinal study
1. Introduction
There is reason to be concerned about a rapid and possibly sustained negative impact of the COVID-19 pandemic on mental health (Raker et al., 2020). The financial and social stressors, including unemployment and isolation, have affected more people over a shorter period than any prior economic downturn or natural disaster. Evidence suggests that there are negative mental health effects of even short periods of unemployment(Cygan-Rehm et al., 2017), which many people experienced early in the pandemic. In addition, studies have documented immediate adverse effects of natural disasters(Goldmann and Galea, 2014; North, 2014), including pandemics(Brooks et al., 2020) on mental health. The literature also suggests that there are strong predictors of vulnerability to the mental health effects of disasters, including pre-disaster mental health status(Goldmann and Galea, 2014; North, 2014).
There is little data yet available on psychological distress during the COVID-19 pandemic and, as is often the case in disaster research(Parker et al., 2019), no studies with longitudinal assessments that allow within-person comparisons with pre-pandemic mental health status. Elevated distress during the pandemic was reported in a web survey conducted in Italy(Mazza et al., 2020). Two studies of U.S. national samples, one of psychological distress and one of depressive symptoms, found threefold higher prevalence of poor mental health status compared to prior periods, but those studies used repeated cross-sectional designs in which data was collected using different samples and methodologies at each time point(Ettman et al., 2020; McGinty et al., 2020). Longitudinal data are needed to prospectively assess meaningful worsening of mental health status during the pandemic, relative to individuals' own pre-pandemic mental health status. Information on the extent and predictors of psychological distress during the early phase of the pandemic will be important for targeting interventions and resources to vulnerable groups and tracking the pandemic's long-term health effects.
In this study, we use longitudinal data from a nationally representative sample of the United States adult population to compare psychological distress experienced during the pandemic with the highest level of distress respondents had experienced during a 12-month period prior to the pandemic. This comparison allows us to identify not only individuals with high distress, but those whose distress was meaningfully elevated above the highest level of distress they experienced over an entire year pre-pandemic. Examining within-person change allows us to better understand the mental health impact of the pandemic.
2. Methods
2.1. Sample
Data come from the Rand American Life Panel (ALP), a probability-based representative sample of U.S. adults age 20 and over. The baseline (T1) survey, conducted in February 2019, N = 2555, had a participation rate of 65%. Of these, n = 1870, or 73%, were interviewed in May of 2020 (T2). The T2 assessment was conducted about 8 weeks following the declaration of a national emergency related to COVID-19 in the United States on March 13, 2020 (Carman and Nataraj, 2020). All study procedures were approved by the Rand IRB.
2.2. Psychological distress
Psychological distress was assessed using the Kessler-6 (K6), a commonly used instrument designed to identify clinically significant psychiatric conditions(Kessler et al., 2003). Internal consistency (α) was 0.91 at T1 and 0.89 at T2. K6 scores were classified using established cut-offs (Furukawa et al., 2008): no/low distress (LD:0–7), mild/moderate distress (MD: 8–12), and serious distress (SD:13–24). K6 score during the worst month of the past year assessed at T1 was compared with psychological distress in the past-30 days assessed at T2. Respondents were considered to have had an increase in distress if they moved from LD at T1to MD or SD at T2 or from MD at T1 to SD at T2.
2.3. Statistical analysis
Analyses used sampling weights generated to account for non-response and match the 2019-wave demographics to the 2019 Current Population Survey, as described in ALP technical documentation(Pollard and Baird, 2017). The distribution of psychological distress at T1 and T2 and the probabilities of within-person transitions between levels of psychological distress between T1 and T2 were calculated. Unadjusted comparisons between T1 and T2 were conducted using survey-adjusted chi-square tests. A survey-adjusted logistic regression model was used to estimate associations between an increase in psychological distress at T2 relative to T1 and demographic characteristics at T1 (gender, age, race, and income) and census region at T2.
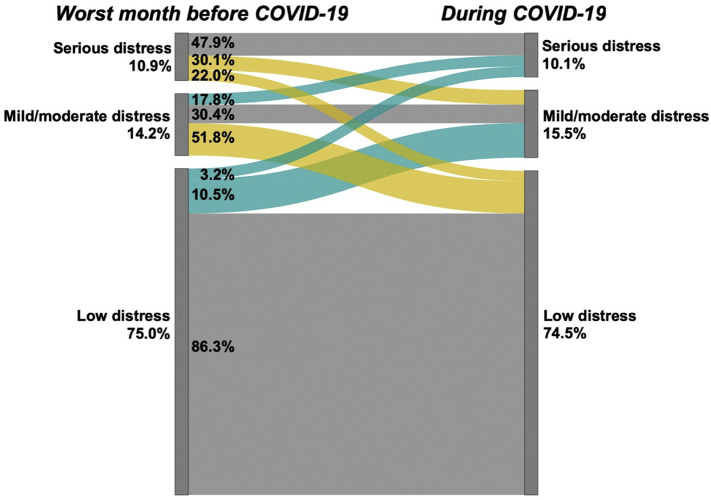
3. Results
Fig. 1 shows the distribution of psychological distress at the two study time points and individual change between categories over time. The prevalence of psychological distress in the past 30-days at T2 did not differ from the prevalence of psychological distress during the worst month of the past year at T1. For instance, the prevalence of SD was 10.9% (95% CI 7.6% -14.0%) during the worst month pre-pandemic and 10.1% (95% CI 6.9% - 13.3%) during the pandemic. The prevalence of SD at T2 did not differ from that at T1for any demographic group examined (p > .3 for all comparisons, data not shown).
Fig. 1.
Individual Change in Psychological Distress during the COVID-19 Pandemic, American Life Panel, N = 1870 Percents outside the bars represent population prevalence at each time point. Percents within the bars represent the proportions at each level of distress at T1 who transitioned to each level of distress at T2; these proportions are also reflected in the width of the bars. Turquoise bards indicate increases in distress, yellow bars indicate decreases in distress and grey bars indicate no change. Psychological distress assessed with the Kessler-6, with categorization as defined in the text. The pre-COVID-19 assessment was conducted in February 2019 and referred to the worst month of the past year. The COVID-19 assessment was conducted in May 2020 and referred to the past 30 days. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Analysis of within-person change found that psychological distress during the pandemic was strongly related to psychological distress during the worst month of the year at T1 (X2 (4) = 174.6, p < .0001). People with SD at T1 were more likely to have SD at T2 compared with those with LD or MD at T1 (47.9% vs. 17.8% and 3.2% respectively). Although risk of SD is relatively low among those with LD at T1 (3.2%), they comprise a substantial minority of those with SD at T2 (23.4%).
An increase in psychological distress at T2 relative to T1 was found in 12.8% (95% CI 9.9%–15.7%) of the sample. Increase in distress was more common among women compared with men, those under 60 compared with those over 60 and Hispanics compared with other racial/ethnic groups (Table 1 ). The associations of increase in distress with gender and age were sustained in the adjusted model, but that with race/ethnicity was not. In addition, adjusted odds of an increase in distress were about twice as high in those with household incomes of $35-$60 K relative to those with incomes over $100 K (OR = 2.2, 95% CI 1.0–4.6) and less than half as high among those in the South relative to those in New England (OR = 0.4, 95% CI 0.2–0.8).
Table 1.
Increase in psychological distress during the pandemic over the highest level of distress pre-pandemic.
| Individual characteristics | Increase above T1 |
X2 |
p-value |
Adjusted odd ratio |
||
|---|---|---|---|---|---|---|
| % | se | OR | 95% CI | |||
| Gender | ||||||
| Female | 17.7 | 2.3 | 4.45 | 0.035 | 1.87 | (1.1,3.1) |
| Male | 10.6 | 2.2 | Reference | |||
| Age | ||||||
| Ages 20–39 | 20.8 | 4.6 | 10.99 | 0.004 | 2.4 | (1.4,4.2) |
| Ages 40–59 | 14.4 | 2.0 | 1.7 | (1.0,2.8) | ||
| Ages 60 and up | 8.7 | 1.3 | Reference | |||
| Race-ethnicity | ||||||
| Hispanic | 25.2 | 6.5 | 12.49 | 0.006 | 1.9 | (0.9,4.0) |
| NH-black | 11.5 | 3.2 | 0.8 | (0.4,1.6) | ||
| NH-other | 14.5 | 4.9 | 1.0 | (0.4,2.4) | ||
| NH-white | 11.8 | 1.4 | Reference | |||
| Income | ||||||
| ≤ $35 K | 15.4 | 2.6 | 3.09 | 0.378 | 1.4 | (0.7,3.0) |
| $35 K-$60 K | 18.2 | 3.9 | 2.2 | (1.0,4.6) | ||
| $60 K-$99 K | 14.9 | 4.3 | 1.4 | (0.7,3.0) | ||
| ≥ $100 K | 10.2 | 2.4 | Reference | |||
| Census region | ||||||
| South | 10.0 | 1.7 | 7.14 | 0.068 | 0.4 | (0.2,0.8) |
| Midwest | 11.3 | 2.7 | 0.6 | (0.3,1.2) | ||
| West | 18.4 | 4.3 | 0.8 | (0.4,1.6) | ||
| New England | 18.7 | 3.9 | Reference | |||
OR = odds ratio; se = standard error; CI=Confidence Interval; NH=Non-Hispanic. Increase in psychological distress defined as movement from no/low distress to mild/moderate or severe distress or from mild/moderate to severe distress.
4. Discussion
This is the first longitudinal study of psychological distress during the COVID-19 pandemic in a nationally representative sample of U.S. adults. The prevalence of SD, indicative of a clinical need, during the pandemic exceeded levels that would be expected in the absence of the pandemic; the 30-day prevalence of SD in May 2020 did not differ from the past-year prevalence of SD assessed with the same instrument in February 2019. In other words, equal numbers of people experienced SD in 30-days during the pandemic as experienced SD over an entire year prior to the pandemic. For comparison, the 30-day prevalence of SD is typically found to be about half the 12-month prevalence, when both are assessed at the same time(Hedden et al., 2012). Elevated prevalence occurred across all demographic groups examined. Elevated psychological distress has been observed in prior disasters(Goldmann and Galea, 2014), but has never before been seen for a persistent and complex stressor affecting the entire U.S. population.
SD at T1 is a strong predictor of SD at T2, consistent with prior research on psychiatric sequelae of natural disasters(North and Pfefferbaum, 2013). In this study, risk for SD during the pandemic among those with SD during a year before the pandemic was almost 3 times higher than among those reporting MD and 15 times higher than among those reporting LD during the pre-pandemic year. People with prior mental health problems are clearly a high-risk group. However, there is substantial variability in within-person change over time; about half (52.1%) of those with SD at T1 had LD or MD at T2 despite the pandemic. It is also important to note that about half of those with SD during the pandemic had not experienced SD during the year prior to the pandemic.
Particular attention should focus on groups at elevated risk for increases in distress relative to prior levels. Higher risk of an increase in psychological distress among respondents younger than 60 suggest that distress may be driven more by economic stressors than fears specific to the disease, since older individuals are widely reported to be at higher risk of morbidity and mortality related to the virus. This finding is reinforced by the vulnerability observed in respondents in the low-middle range of household incomes, close to or below the U.S. median and above $35,000. People in this group may have been at most risk for loss of income or stressful employment conditions(McQuarrie, 2020). Risk for an increase in distress was lower in the Souththan in the NortheastThe geographic difference may have been driven by concerns about the virus itself, the economic consequences of social distancing which were implemented more slowly in the southern states(Kates et al., 2020), or even differing politically inflected interpretations of the threat, given that political affiliation is predictive of social distancing policies(Adolph et al., 2020). Further follow-up studies covering the time period during which the pandemic became more widespread in the southern United States will shed further light on this finding.
We found that Hispanics were more likely to report an increase in psychological distress than other racial/ethnic groups. This finding adds to evidence from the one prior study of psychological distress during the COVID-19 pandemic that Hispanic population of the US has been disproportionately affected(McGinty et al., 2020). The finding of high risk among Hispanics was not sustained in our adjusted model, although the magnitude of the difference between Hispanics and Non-Hispanic Whites remained large. Our finding of higher risk among women is consistent with prior studies of psychiatric disorders following disasters(North, 2016).
Limitations of this study should be considered. The T1 assessment was about 1 year prior to the pandemic and based on a recall period of 12-month prior to T1. While there is no systematic bias in use of this time period, there may have been variations in psychological distress between assessments that are not captured here. Second, participation was limited to individuals who could complete the survey in English. Studies examining psychological distress in non-English speakers during this time are needed. Third, specific exposures and their relationships with change in distress could not be examined in this study.
5. Conclusion
The mental health impact of the COVID-19 pandemic is unprecedented with respect to its nation-wide scale. However, during the period of time covered in this survey, the first two months following the declaration of a national emergency in the United States, the epidemiological patterns of mental health effects are more similar than different to those observed in prior studies of the mental health consequences of disasters. Most notably, during this period serious psychological distress was highly elevated in the general population, with particularly high risk among people with prior psychiatric conditions(North, 2016). Clinical services should be targeted to this population. Services can also be targeted to population groups at high risk for elevated psychological distress during the pandemic, including people vulnerable to the economic consequences of social distancing. Prior research suggests that many who experience psychological distress immediately following a disaster return to pre-disaster levels over time(Pietrzak et al., 2012), and a similar pattern has been observed in trajectories of distress in the U.S. since March of 2020(Daly and Robinson, 2020). However the pandemic's influence on economic stressors, disruption of usual activities and subsequent effects on population health may continue for an extended period and affect different regions of the country at different points in time. Tracing patterns of persistence of serious psychological distress will provide important information to guide the national public health response to the COVID-19 pandemic.
Providing services each month of the crisis to as many people as typically experience SD in a 12-month period, with normal pathways to care disrupted by social distancing, is an enormous challenge. Policy makers and practitioners may need to plan for strategic resource distribution to address the most serious clinical needs, reduce stress on providers, and direct resources to address persistent economic distress.
The following is the supplementary data related to this article.
Sample characteristics.
Declaration of Competing Interest
None.
Acknowledgments
This research was supported by grants from the National Institute on Minority Health and Health Disparities (R01 MD010274, PI: Breslau) and National Institute of Mental Health (R01 MH104381, PI: Collins)
References
- Adolph C., Amano K., Bang-Jensen B., Fullman N., Wilkerson J. 2020. Pandemic Politics: Timing State-Level Social Distancing Responses to COVID-19. medRxiv:2020.03.30.20046326. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carman K.G., Nataraj S. RAND; Santa Monica, CA: 2020. 2020 American Life Panel Survey on Impacts of COVID-19: Technical Documentation. [Google Scholar]
- Cygan-Rehm K., Kuehnle D., Oberfichtner M. Bounding the causal effect of unemployment on mental health: nonparametric evidence from four countries. Health Econ. 2017;26:1844–1861. doi: 10.1002/hec.3510. [DOI] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2020 doi: 10.1016/j.jpsychires.2020.10.035. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. e2019686-e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T.A., Kawakami N., Saitoh M., Ono Y., Nakane Y., Nakamura Y., Tachimori H., Iwata N., Uda H., et al. The performance of the Japanese version of the K6 and K10 in the world mental health survey Japan. Int. J. Methods Psychiatr. Res. 2008;17:152–158. doi: 10.1002/mpr.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annu. Rev. Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Hedden S., Gfroerer J.C., Barker P., Smith S., Pemberton M.R., Saavedra L.M., Forman-Hoffman V.L., Ringeisen H., Novak S.P. Center for Behavioral Health and Statistics and Quality Data Review March; 2012. Comparison of NSDUH Mental Health Data and Methods with Other Data Sources. [PubMed] [Google Scholar]
- Kates J., Michaud J., Tobert J. Kaiser Family Foundation; 2020. Stay-At-Home Orders to Fight COVID-19 in the United States: The Risks of a Scattershot Approach. [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.L.T., Manderscheid R.W., et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuarrie K. The Average Salary of Essential Workers in 2020: How Much Are Essential Workers Earning Compared to the Average Income in their State? 2020. Business.org
- North C.S. Current research and recent breakthroughs on the mental health effects of disasters. Curr. Psych. Rep. 2014;16:481. doi: 10.1007/s11920-014-0481-9. [DOI] [PubMed] [Google Scholar]
- North C.S. Disaster mental health epidemiology: methodological review and interpretation of research findings. Psychiatry. 2016;79:130–146. doi: 10.1080/00332747.2016.1155926. [DOI] [PubMed] [Google Scholar]
- North C.S., Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310:507–518. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- Parker A.M., Edelman A.F., Carman K.G., Finucane M.L. On the need for prospective disaster survey panels. Disaster Med. Public Health Prep. 2019:1–3. doi: 10.1017/dmp.2019.94. [DOI] [PubMed] [Google Scholar]
- Pietrzak R.H., Tracy M., Galea S., Kilpatrick D.G., Ruggiero K.J., Hamblen J.L., Southwick S.M., Norris F.H. Resilience in the face of disaster: prevalence and longitudinal course of mental disorders following hurricane Ike. PLoS One. 2012;7 doi: 10.1371/journal.pone.0038964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M., Baird M.D. RAND Corporation; Santa Monica, CA: 2017. The RAND American Life Panel: Technical Description. [Google Scholar]
- Raker E.J., Zacher M., Lowe S.R. Lessons from hurricane Katrina for predicting the indirect health consequences of the COVID-19 pandemic. Proc. Natl. Acad. Sci. 2020;117:12595. doi: 10.1073/pnas.2006706117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sample characteristics.