Abstract
Objective
This study offers meta-analytic data on the potential association between epilepsy and depression especially for the prevalence of depression in epilepsy or vice versa.
Methods
The relevant studies were searched and identified from nine electronic databases. Studies that mentioned the prevalence and/or incidence of epilepsy and depression were included. Hand searches were also included. The search language was English and the search time was through May 2022. Where feasible, random-effects models were used to generate pooled estimates.
Results
After screening electronic databases and other resources, 48 studies from 6,234 citations were included in this meta-analysis. The period prevalence of epilepsy ranged from 1% to 6% in patients with depression. In population-based settings, the pooled period prevalence of depression in patients with epilepsy was 27% (95% CI, 23–31) and 34% in clinical settings (95% CI, 30–39). Twenty studies reported that seizure frequency, low income, unemployment of the patients, perception of stigma, anxiety, being female, unmarried status, disease course, worse quality of life, higher disability scores, and focal-impaired awareness seizures were risk factors for depression.
Conclusion
Our study found that epilepsy was associated with an increased risk of depression. Depression was associated with the severity of epilepsy.
Introduction
Epilepsy is a common neurological disorder in which abnormal electrical discharges in the brain can lead to recurrent seizures [1]. Epileptic seizures are generally rare with an annual incidence of approximately 0.3‰ for newly diagnosed epilepsy and 0.55‰ for unprovoked seizures [2]. In epilepsy, depression is the most common psychiatric comorbidity. Depression affects around one‐third of these cases and impacts quality of life [3]. Depression is the most common psychiatric disorder, and it occurs in 14.1% of females and 14.8% of males worldwide [4]. Depression is more frequent in patients with epilepsy compared to the general population [5]. Epilepsy and depression both can influent individual’s interpersonal communication, social activities and can increase the risk of sudden attacks [4,6]. Some studies indicate that epilepsy and depression are bidirectional [7]. The reported prevalence of depression in patients with epilepsy (PWE) varies between 10.7 to 44%, and it can reach 54% in refractory epilepsy [8]. However, the association between depression and epilepsy have not yet been comprehensively described.
The epidemiology and risk factors of depression in patients with epilepsy are unclear and vice versa. Understanding the epidemiology of depression and epilepsy is important in reducing disability and protecting patients’ health and safe. Our study offers a comprehensive and systematic review of the prevalence, incidence, and reported risk factors for depression with epilepsy and epilepsy with depression. We further studied direct associations between depression and epilepsy.
Methods
Protocol and registration
We registered this systematic review on the Prospective Register of Systematic Reviews (PROSPERO) on April, 2022 (#CRD42022327256). This systematic review and meta-analyses were reported with a predetermined protocol and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Information sources
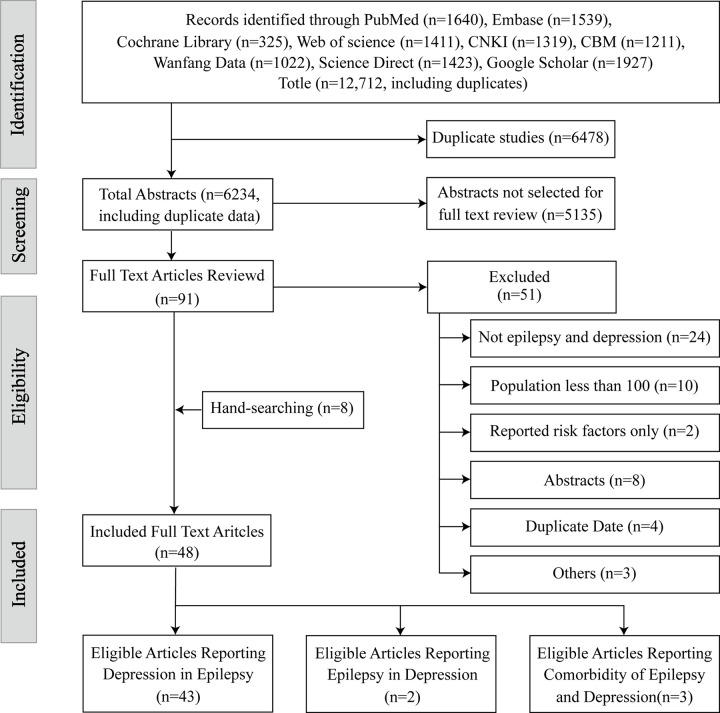
Nine databases were searched from inception to May 15, 2022 (Fig 1). EndNote X9 was used to export and manage references. Search terms included awakening epilepsy, epilepsia, epileptic, epilepticus, seizure disorder, epilepsy, cryptogenic epilepsies, cryptogenic epilepsies, aura, depression, depressive symptoms, symptom depressive, emotional depression, etc. In addition, reference lists and bibliographies from cited documents were manually searched for additional articles. Hand searches were also included. The search language was English. A complete description of our search strategy is available as a S1 File.
Fig 1. PRISMA flow diagram.
Study selection
Two reviewers independently studied the titles, abstracts, and full text reviews to find potentially eligible reviews. The eligibility criteria included the following: (a) a clearly recognized diagnostic criteria for epilepsy and depression; (b) a sample size over 100; (c) reported prevalence or incidence of epilepsy in depression, vice versa, or both; the data had to be able to be extracted. The exclusion criteria included the following: (a) reporting only risk factors; (b) no focus on epilepsy and depression; or (c) duplicated studies. The most comprehensive version was selected from duplicate data. Disagreements between reviewers were solved by discussion. If agreement could not be reached, then a third senior study author resolved the issue.
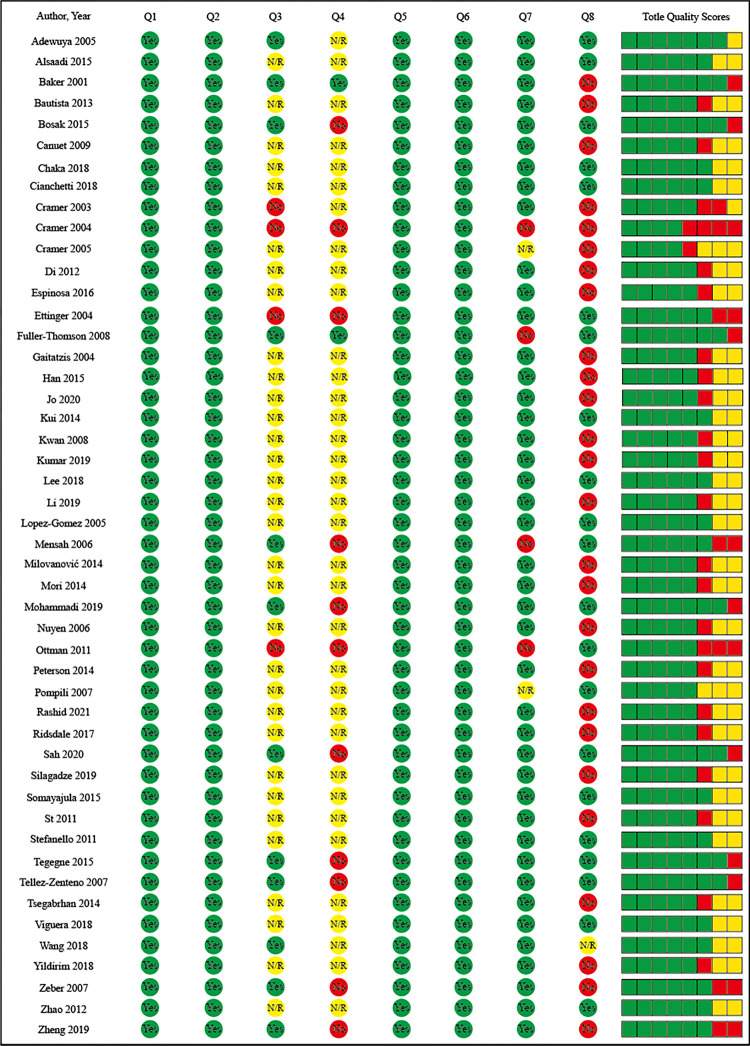
Data extraction and study quality
Two authors extracted data independently in duplicate using a standard data abstraction form. Data were extracted by two authors, and the details were as follows: authors and study country, sample size, case size, mean age, age range, female, epileptic diagnostic criteria, depressive diagnostic criteria, data collection period, and prevalence. Research quality indicators related to sample representativeness, conditional evaluation, and statistical methods were extracted and provide the basis for conditional heterogeneity evaluation. Assessments of study quality were performed according to Subota et al [9]; see Fig 2.
Fig 2. The quality scores of included studies.
Q1: Target Population described? Q2: Cases from entire population or probability sampling? Q3: Response rate >70%? Q4: Non-responders clearly described? Q5: Is the sample representative of the population? Q6: Were data collection methods standardized? Q7: Were validated criteria used to assess the presence/absence of disease? Q8: Are the estimates of prevalence and incidence given with confidence intervals?
Data synthesis and analysis
Depression in epilepsy, epilepsy in depression, or both were analyzed separately for each condition. The Cochrane Q statistic was calculated to assess the significance between study heterogeneity, and I2 was used to quantify the magnitude of between-study heterogeneity. When I2<50%, the pooled estimate and 95% confidence intervals (CIs) were calculated using a fixed-effect model. A random-effects model was used when I2>50%. Subgroup analysis was performed by sample resource and diagnostic criteria of depression. Our main outcomes were prevalence, confidence intervals, and percentage prevalence. All analyses were completed using Review Manager 5.4.
Results
There were 12,712 studies preliminarily assessed for eligibility; 6,478 duplicate studies were excluded from Endnote X9. Here, 91 studies were screened at the full-text levels, and 48 studies were included. The reason for elimination was that they did not report depression or epilepsy (n = 24), were composed of a study sample of less than 100 (n = 10), reported duplicate data (n = 4), only reported risk factors of depression or epilepsy (n = 2), only contained an abstract (n = 8), or other reasons (n = 3). Manually checking the reference lists led to eight articles included in the systematic review for a total of 48 (Fig 1). The prevalence of epilepsy in depression was included in two articles (Table 1), the prevalence of depression in epilepsy was included in 43 articles (Table 2), and three articles recorded the comorbid relationship between epilepsy and depression (Table 3).
Table 1. Studies reporting on the prevalence and incidence of epilepsy in depression (n = 2).
| Author, year (country, region) | Sample (n) | Case (n) |
Age (year) |
Female (n) | Diagnostic criteria epilepsy | Diagnostic criteria depression | Years of data collection | Prevalence |
|---|---|---|---|---|---|---|---|---|
| Mohammadi 2019 IRAN [10] |
521 | 29 | 6–18 | 313 | NR | NR | 2016–2017 | 5.6% |
| Nuyen 2006 The Netherlands [11] |
6641 | 50 | NR | 4452 | diagnosis by general practitioner | NR | NR | 0.75% |
Table 2. Studies reporting on the prevalence and incidence of depression in epilepsy (n = 43).
| Author, year (country, region) | Sample (n) | Case (n) |
Age (year) |
Female (n) |
Diagnostic criteria epilepsy | Diagnostic criteria depression | Years of data collection | Prevalence |
|---|---|---|---|---|---|---|---|---|
| Adewuya 2005 Nigeria [12] |
102 | 29 | 12–18 | 37 | NR | DSM-Ⅳ | NR | 28.43% |
| Alsaadi 2015 United Arab Emirates [13] |
186 | 50 | 18–65 | 105 | NR | PHQ-9 | 2014.9–2015.1 | 26.88% |
| Baker 2001 UK [14] |
669 | 163 | NR | 345 | Physician diagnosis | HAD | NR | 24.36% |
| Bautista 2013 USA [15] |
200 | 71 | ≥18 | 156 | NR | NIDDI-E | 2012.6–2012.8 |
35.50% |
| Bosak 2015 Poland [16] |
289 | 84 | NR | 49 | NR | BDI | NR | 29.06% |
| Canuet 2009 Japan [17] |
114 | 51 | 18–80 | 49 | Imaging | BDI-II | 2006.6–2008.5 | 44.73% |
| Chaka 2018 Ethiopia [18] |
422 | 185 | ≥18 | 173 | NR | PHQ-9 | 2015.4–2015.5 | 43.83% |
| Cianchetti 2018 Italy [19] |
326 | 30 | 8–18 | 171 | NR | SAFA-D | NR | 9.20% |
| Cramer 2003 USA [20] |
683 | 240 | NR | NR | NR | CES-D | 2001.1 | 35.13% |
| Cramer 2004 USA [21] |
649 | 206 | ≥18 | NR | Seizure Severity Scale and QOLIE-89 | CES-D | 2001.1 | 31.74% |
| Cramer 2005 USA [22] |
201 | 74 | 19–75 | 113 | QOLIE10 | HADS | NR | 36.81% |
| Di 2012 Spanish [23] |
121 | 25 | ≥18 | 80 | Imaging | MINI | NR | 20.66% |
| Espinosa 2016 Colombia [24] |
220 | 86 | 18–79 | 106 | ILAE 2014 | NDDI-E | 2014.9–2015.3 | 39.09% |
| Ettinger 2004 USA [25] |
775 | 283 | >18 | 365 | Self-reported prior diagnosis of epilepsy | CES-D | 2001.1–2002.4 | 36.51% |
| Fuller-Thomson 2009 Canada [26] | 781 | 110 | ≥12 | 401 | A health professional | CIDI-SF | 2000–2001 | 14.08% |
| Gaitatzis 2004 UK [27] | 5834 | 1063 | ≥16 | NR | ICD-9 | NR | 1995.1.1–1998.12.31 | 18.22% |
| Han 2015 Korea [28] | 391 | 267 | 18–79 | 187 | NR | BDI | NR | 68.28% |
| Jo 2020 Korea [29] | 126 | 38 | >18 | 62 | ILAE 2014 | PHQ-9 | 2018.10–2018.12 | 30.15% |
| Kui 2014 China [30] | 215 | 65 | ≥18 | 84 | ILAE | DSM-Ⅳ | NR | 30.23% |
| Kwan 2009 China [31] | 247 | 94 | 18–76 | 133 | NR | HADS | 2007.3–2007.6 | 38.05% |
| Lee 2018 Korea [32] | 141 | 60 | >18 | 68 | ILAE 2014 | HADS | NR | 42.55% |
| Li 2019 China [33] | 461 | 138 | ≥18 | 248 | ILAE | CNDDI-E | 2017.1–2017.11 | 29.93% |
| Lopez-Gomez 2005 Mexico [34] | 241 | 103 | NR | 116 | ILAE | BDI | 2002.3–2003.3 | 42.73% |
| Mensah 2006 UK [35] | 499 | 139 | 18–78 | 252 | NR | HADS | NR | 27.85% |
| Milovanović 2014 Serbia [36] | 203 | 67 | 18–65 | 118 | ILAE 2001 | BDI-II | NR | 33.00% |
| Mori 2014 Japan [37] | 463 | 85 | ≥16 | 247 | NR | IDS-SR | 2009.10.2–2011.4.1 | 18.35% |
| Ottman 2011 USA [38] | 3488 | 1134 | ≥18 | 2125 | NR | NR | 2008.1–2008.4 | 32.51% |
| Peterson 2014 Australia [39] |
279 | 80 | ≥18 | 165 | NR | HADS | NNR | 28.67% |
| Pompili 2007 Italy [40] | 103 | 43 | 19–78 | 72 | NR | BDI | NR | 41.74% |
| Rashid 2021 India [41] | 449 | 180 | 18–75 | 219 | ILAE | MINI | 2018.1–2020.3 | 40.08% |
| Ridsdale 2017 UK [42] | 403 | 113 | 16–85 | 219 | QOLIE-31 | HADS | NR | 28.03% |
| Silagadze 2019 Georgia [43] |
130 | 31 | 18–56 | 68 | NDDI-E ILAE | ICD-10 | NR | 23.84% |
| Somayajula 2015 India [44] |
165 | 27 | >16 | 62 | ILAE | ICD-10 | 2011.5–20014.4 | 16.36% |
| Stefanello 2011 Brazil [45] |
153 | 32 | ≥13 | NR | ILAE | HAD | 2006.5–2007.12 | 20.91% |
| Tegegne 2015 Ethiopia [46] |
415 | 136 | ≥18 | 186 | NR | HADS | 2013.4–2013.5 | 32.77% |
| Tellez-Zenteno 2007 Canada [47] | 253 | 44 | ≥15 | NR | An interviewer asking directly | DSM-IV | 2002.5–2002.12 | 17.39% |
| Tsegabrhan 2014 Ethiopia [48] |
300 | 148 | >18 | 117 | NR | BDI-II | 2012.8–2012.10 | 49.33% |
| Viguera 2018 USA [49] | 1763 | 584 | ≥18 | 952 | ICD-9-CM | PHQ-9 | 2007.10.1–20128.13 | 33.12% |
| Wang 2018 China [50] | 458 | 241 | ≥18 | 100 | NR | C-NDDI-E | NR | 52.62% |
| Yildirim 2018 Turkey [51] | 302 | 139 | 15–73 | 170 | NR | BDI | NR | 46.02% |
| Zeber 2007 USA [52] | 13699 | 2961 | ≥18 | 503 | ICD-9 | ICD-9 | 1996.10.1–1999.9.30 | 21.61% |
| Zhao 2012 China [53] | 140 | 36 | 15–71 | 70 | ILAE 1989 | HAMD | 2007.8–2008.2 | 25.71% |
| Zheng 2019 China [54] | 184 | 36 | ≥18 | 84 | ILAE 2001 | BDI | 2014.6–2016.1 | 19.56% |
Abbreviation: ILAE = International League Against Epilepsy; QOLIE = the Quality of Life in Epilepsy Inventory; ICD = International Classification of Diseases; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders; BDI = Beck Depression Inventory; HADS = Hospital Anxiety and Depression Scale; PHQ = the patient health questionnaire; CES-D = the Center for Epidemiologic Studies Depression scale; CIDI-SF = Composite International Diagnostic Interview short‐form; NDDI-E = Neurological Disorders Depression Inventory for Epilepsy; CNDDI-E = Chinese version of the Neurological Disorders Depression Inventory for Epilepsy; IDS-SR = the Inventory of Depressive Symptomatology Self Report.
Table 3. Studies reporting on the prevalence and incidence of depression and epilepsy (n = 3).
| Author, year (country, region) | Sample (n) | Case (n) |
Age (year) |
Female (n) | Diagnostic criteria epilepsy | Diagnostic criteria depression | Years of data collection | Prevalence |
|---|---|---|---|---|---|---|---|---|
| Kumar 2019 USA [55] | 120 | 69 | ≥18 | 81 | A self‐reported diagnosis of epilepsy | DSM-5 | NR | 57.70% |
| Sah 2020 Nepal [56] | 142 | 44 | 18–68 | 55 | clinically confirmed epilepsy |
HAMD | 2018.4–2018.9 | 30.98% |
| St 2011 Canada [57] | 7253 | 2044 | 0.03–96 | 3481 | ICD-9-CM ICD-10-CA |
NR | 1996.4.1–2004.3.31 | 28.18% |
ICD-9-CM, the International Classification of Diseases, Version 9, Clinical Modification; ICD-10-CA, the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Canada; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; HAMD, Hamilton Depression Scale.
Epilepsy in depression
Two studies reported the prevalence of epilepsy in patients with depression—one from the Netherlands and one from Iran. Both studies used data from an administrative database. One study reported both the incidence rate of depression in epilepsy and the incidence rate of epilepsy in depression [11]; the other reported the rates of depression in children and adolescents in Iran [10]. There were relatively few studies, and the aggregated overall prevalence was not calculated.
Depression in epilepsy
Forty-three papers reported a prevalence estimate for depression with epilepsy. The 43 included studies from the United States (n = 8), China (n = 7), the United Kingdom (n = 4), Ethiopia (n = 3), Korea (n = 3), Canada (n = 2), India (n = 2), Japan (n = 2), Australia (n = 1), Brazil (n = 1), Colombia (n = 1), Georgia (n = 1), Italy (n = 1), Mexico (n = 1), Nigeria (n = 1), Poland (n = 1), Serbia (n = 1), Spain (n = 1), Turkey (n = 1), and the United Arab Emirates (n = 1). Among the 43 reports on the incidence rate of depression in epilepsy, 21 describe the demographic and clinical characteristics of epileptic patients in detail (Table 4).
Table 4. Demographic and clinical characteristics of epileptic patients (n = 21).
| Author, year (country, region) |
Sample (n) | Female (%) | Education (%) | Unemployment (%) |
Unmarried (%) |
|
|---|---|---|---|---|---|---|
| Less than high school | High school and above | |||||
| Bautista 2013 USA [15] | 200 | 63.60 | 23.60 | 76.40 | NR | 40.30 |
| Bosak 2015 [16] | 289 | 58.50 | 31.10 | 68.90 | 61.50 | 56.40 |
| Chaka 2018 [18] | 422 | 40.90 | 80.80 | 19.20 | 9.70 | 50.20 |
| Cramer 2005 USA [22] | 201 | 56.20 | 18.20 | 81.80 | 17.30 | NR |
| Espinosa 2016 Colombia [24] | 220 | 48.10 | NR | NR | 85.50 | |
| Fuller-Thomson 2009 Canada [26] | 781 | 51.40 | 40.90 | 59.10 | NR | 48.90 |
| Han 2015 Korea [28] | 391 | 47.80 | 19.10 | 80.90 | 37.10 | 54.10 |
| Jo 2020 Korea [29] | 126 | 48.40 | NR | 25.40 | NR | |
| Kui 2014 China [30] | 215 | 39.00 | 65.10 | 34.90 | 34.80 | 39.10 |
| Lee 2018 Korea [32] | 141 | 48.20 | 22.00 | 78.00 | 14.20 | 51.80 |
| Li 2019 China [33] | 461 | 53.80 | 42.80 | 57.20 | 58.00 | 65.90 |
| Milovanovć 2014 Serbia [36] | 203 | 58.10 | 23.10 | 76.90 | 25.10 | 58.10 |
| Peterson 2014 Australia [39] | 279 | 59.10 | 47.30 | 52.70 | 51.60 | 41.60 |
| Ridsdale 2017 UK [42] | 403 | 54.20 | 47.50 | 52.50 | 49.20 | 51.00 |
| Silagadze 2019 Georgia [43] | 130 | 52.30 | 66.20 | 33.80 | NR | NR |
| Somayajula 2015 India [44] | 165 | 37.60 | 59.40 | 40.60 | 6.70 | 62.40 |
| Tegegne 2015 [46] | 415 | 44.80 | 82.40 | 17.60 | NR | 61.40 |
| Tsegabrhan 2014 Ethiopia [48] | 300 | 39.00 | 55.70 | 44.30 | 21.70 | 53.30 |
| Wang 2018 China [50] | 458 | 40.60 | 87.10 | 12.90 | NR | 25.80 |
| Yildirim 2018 Turkey [51] | 302 | 56.00 | 58.00 | 42.00 | 26.00 | 55.00 |
| Zheng 2019 China [54] | 184 | 45.65 | 61.40 | 38.60 | 26.60 | 47.20 |
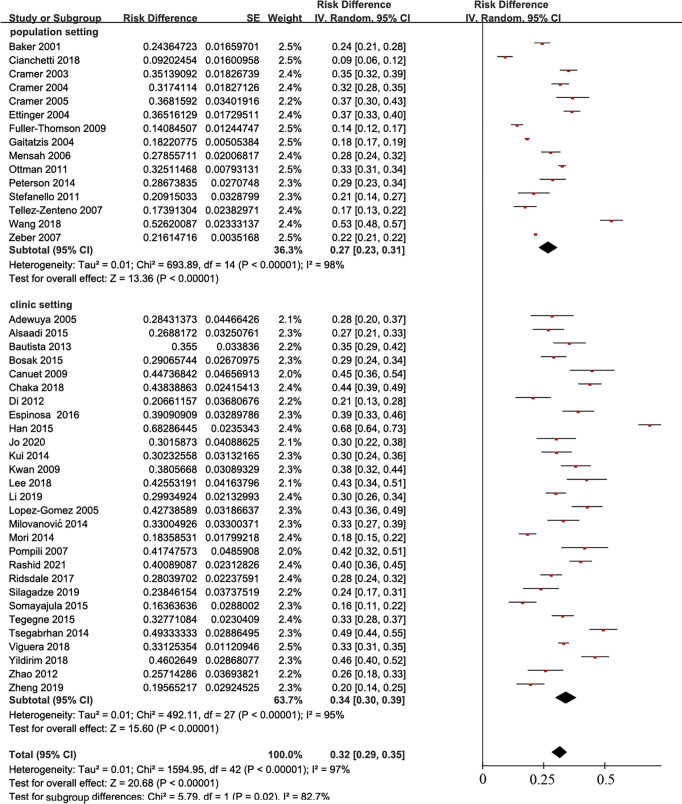
Among the 43 reports on the incidence rate of depression in epilepsy, 15 were based on a population survey [14,19–22,25–27,35,38,39,45,47,50,52], and 28 were clinical studies [12,13,15–18,23,24,28–34,36,37,40–44,46,48,49,51,53,54]. In a population-based environment, the combined prevalence of epilepsy in depression patients was 27% (95% CI, 23–31), while the prevalence was 34% in the clinic (95% CI, 30–39) (Fig 3).
Fig 3. Overall prevalence of depression among persons with epilepsy in population setting and clinic setting.
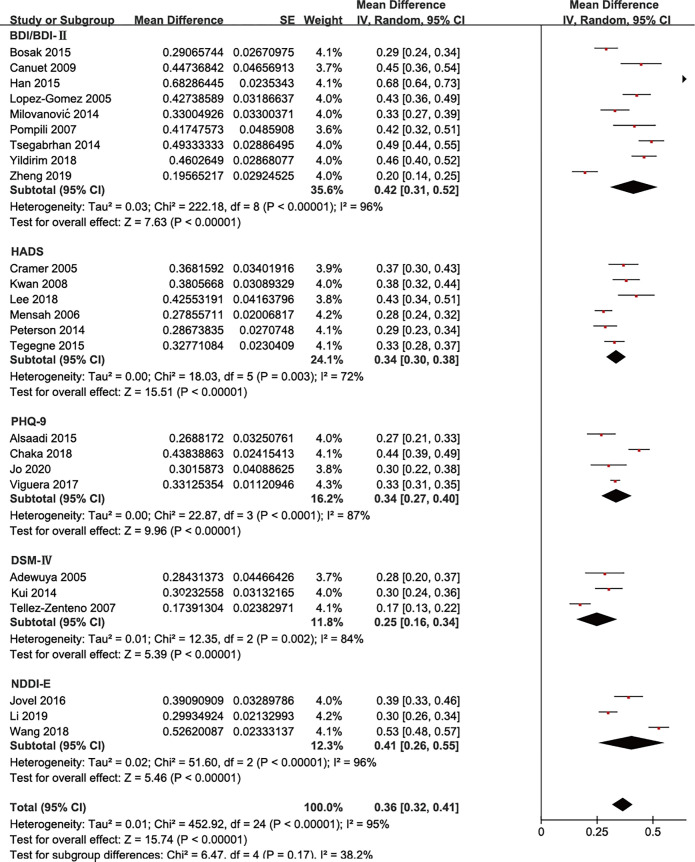
Depression is diagnosed with different scales: Beck Depression Inventory (BDI and BDI-Ⅱ), Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition (DSM-Ⅳ)), Hospital Anxiety and Depression Scale (HADS), Neurological Disorders Depression Inventory for Epilepsy (NDDI-E), Patient Health Questionnaire nine-item (PHQ-9), etc. The estimates of depression included here had significant subgroup differences (P<0.0001, I2 = 94.5%). However, there is no significant subgroup difference when eliminating scales used only once or twice (Fig 4).
Fig 4. Overall prevalence of depression among persons with epilepsy by different depression diagnostic tool.
Twenty studies explored the risk factors of depression in patients with epilepsy (Table 4). Seizure frequency, low income, unemployment, perception of stigma, anxiety, being female, unmarried status, disease course, worse quality of life, higher disability scores, and focal-impaired awareness seizures were risk factors for depression. Eight studies identified seizure frequency as risk factors for depression in PWE [18,19,24,37,39,46,50,53]. Eight of the articles reported that lower income and unemployment are associated with depression in PWE [10,19,31,34,35,39,45,46]. Six studies found that the perception of stigma was associated with depression in PWE [13,16,19,37,46,53].
Comorbid epilepsy and depression
Three studies reported the comorbidity of epilepsy and depression [55–57]. Geographically, the three studies were from the United States, Nepal, and Canada. One study acquired data through registries, and two utilized a hospital clinic review. The aggregated overall prevalence was not estimated because of low sample size. One study examined risk factors and found that drug use remained an important predictor of depression among patients with epilepsy (P = 0.002); the odds of having depression in patients receiving polytherapy were 3.82-fold higher than in those receiving monotherapy (95% CI, 1.61–9.05, P = 0.002) [56].
Discussion
The median incidence of epilepsy was 50.4 per 100,000 every year ([IQR] 33.6–75.6) [58]; it is estimated that 3.8% of the population suffer from depression. There were more studies on the incidence of depression with epilepsy than epilepsy with depression. This may because depression predicts a worse response to treatment during epilepsy [59] and because people with depression face greater suicide risk [60]; thus, many studies focus on depression with epilepsy. Three studies reported comorbidity, but they do not have specific samples or cases. Few studies reported on occurrence of epilepsy with depression and comorbidity, and a pooled overall prevalence evaluation could not be calculated.
This association may be causal or there may be common pathogenic mechanisms underlying depression and epilepsy. Depression is the most common psychiatric comorbidity in patients with epilepsy [61], and it may explain the worse response to epilepsy treatment [62].
Epilepsy is associated with increasing incidence of depression. Our meta-analysis found that the pooled overall period prevalence of depression in epilepsy based on population (27%, 95% CI, 0.23–0.31) was lower than that based on clinical evaluation (34%, 95% CI, 0.30–0.39). The difference between them was statistically significant (P = 0.01). The diagnosis of depression is based on many different scales [63]. Epilepsy is diagnosed through the patient’s clinical symptoms as well as imaging and electroencephalogram changes [64]; however, some population-based diagnoses of epilepsy use questionnaires. We believe that the diagnosis of epilepsy based on clinical features is more accurate than population settings. This condition can perhaps explain the big heterogeneity in the findings because epilepsy was associated with depression [65].
We did subgroup analysis for scales of depression to estimate whether different depression scales affect the above results. The subgroup analysis showed different incidence rates using different scales. These range from 30% to 34% and were statistically significant (P<0.0001). However, we do not believe that this difference represents a difference in the detection rates of these scales. First, the I2 of the results is 97%. Second, some scales were only used once in our cohort of papers. However, some studies have shown that the clinical use of NDDI-E, HADS, and other scales is not the main driver for these inconsistent results [41]. Thus, we eliminated studies that included these factors and obtained more reasonable results, i.e., no statistical difference between subgroups (Fig 4).
A meta-analysis reported that epilepsy was associated with an increased risk of depression [66]. Risk factors for depression in epilepsy were summarized based on the literature to further investigate the factors influencing the association between epilepsy and depression. There were 20 studies reporting risk factors about depression in epilepsy (Table 5). Seizure frequency, low income, unemployment, and perception of stigma were associated with depression in PWE. A study found that seizure frequency (P = 0.36) was not associated with depression [13]. This article did not limit the disease course during the inclusion criteria for patients with epilepsy, which is the main factor influencing depression in patients with epilepsy.
Table 5. Risk factors of depression with epilepsy (n = 20).
| Author, year | Sample (n) |
Age range studied | Risk factors | Examined factors | Statistical method | Depression scales |
|---|---|---|---|---|---|---|
| Adewuya 2005 [12] | 102 | 12–18 | Frequency of seizures, number of antiepileptic drugs, perception of stigma | Age, gender, level of education/class, age of onset of illness, duration of epilepsy, seizure type, types of AEDs, number of AEDs | Regression analysis | DSM-Ⅳ |
| Alsaadi 2015 [13] | 186 | 18–65 | Age, gender | Marital status, nationality, seizure frequency age, gender, epilepsy classification, number of seizures in the 6 months prior to the clinic visit |
Multi regression mode | PHQ-9 |
| Bosak 2015 [16] | 289 | NR | Age, frequent seizures, use medications |
Age, gender, marital status, education level, occupational activity, use of antidepressant | Logistic regression modeling | BDI |
| Chaka 2018 [18] | 422 | ≥18 | Female, single, perceived stigma, medication adherence, current substance use | Age, gender, ethnicity, marital status, religion, residence, education, occupation, with whom living now | Logistic regression analysis |
PHQ-9 |
| Cianchetti 2018 [19] | 326 | 8–18 | Severity and duration of the epilepsy | Sex, education, epilepsy severity, disease duration, antiepileptic treatment |
Chi-square or Fisher’s exact test | SAFA-D |
| Espinosa 2016 [24] | 220 | 18–79 | Unemployed | Age, sex, education, marital status, and occupational activity, risk factors for epilepsy, age of diagnosis, type of seizures, frequency of seizures, treatment with antiepileptic drugs, and therapeutic response |
A multiple linear regression model | NDDI-E |
| Kui 2014 [30] | 215 | >18 | Employment status, presence of chronic medical illnesses, drug responsiveness | Education, marriage status, employment status, gender, age, age at seizure onset, duration of epilepsy, seizure type, aetiology of epilepsy, epileptic family history, previous status epilepticus, EEG findings, neuroimaging findings outcome of epilepsy, chronic medical illnesses | A binary logistic regression |
DSM-Ⅳ |
| Lee 2018 [32] | 141 | >18 | Higher neuroticism, lower self-esteem, marital status, and lower extroversion |
Gender, age at the first seizure onset, marriage, job, economic class, presence vs. absence of perceived stigma | Stepwise linear regression model | HADS |
| Lopez-Gomez 2005 [34] | 241 | NR | Seizure frequency | Age, gender, marital status, educational degree, or type of economic activity |
A logistic regression model | BDI MADRS |
| Mensah 2006 [35] | 499 | 18–78 | Unemployment | Gender, marital status, or monotherapy or polytherapy antiepileptic medication | A stepwise multiple regression analysis | HADS |
| Milovanović 2014 [36] | 203 | 18–65 | Educational level | Age, educational level, occupational status, marital status, epilepsy history, seizure types, seizure frequency, comorbidity, drug treatment | Hierarchical multiple regression analysis | BDI-II |
| Peterson 2014 [39] | 279 | ≥18 | Employment status, high levels of social stigma, ineffective control of seizures | Gender, employment, marital status, education | Pearson correlations and block recursive regression | HADS |
| Somayajula 2015 [44] | 165 | >16 | Married | Gender, married, unemployment, graduate age | Logistic regression | ICD-10 |
| Stefanello 2011 [45] | 153 | ≥13 | Unemployment, fewer years of schooling, age above 41 | Age, gender, marital status, occupation schooling, economic group | Logistic regression analysis |
HAD |
| Tegegne 2015 [46] | 415 | ≥18 | Using poly-therapy of anticonvulsants, perceived stigma, inability to read or write |
Age, gender, marital status, residence, religion, ethnicity, educational status, occupation, monthly income, frequency of seizure | Logistic regression analysis | HADS |
| Tsegabrhan 2014 [48] | 300 | >18 | Epilepsy‑related perceived stigma, high seizure frequency, low educational status | Age, duration of illness, marital status, educational status, occupation, place of residence, seizure frequency, type of AEDs, epilepsy‑related perception of stigma | Bivariate logistic regression |
BDI‑II |
| Viguera 2018 [49] | 1763 | ≥18 | Age, black race, lower income, lower health-related quality-of-life, higher LSSS score (worse severity) |
Age, gender, race, marital status, household median income, patient-reported health-related quality of life, disease-specific performance scale |
Univariate logistic regression models | PHQ-9 |
| Wang 2018 [50] | 458 | ≥18 | Income, frequent seizures | Gender, marital status, age, income, education, age at seizure onset, polytherapy | NR | C-NDDI-E |
| Yildirim 2018 [51] | 302 | 15–73 | Female, lower education and income levels, never employed, higher seizure frequency |
Gender, marital status, educational level, occupation, income level, seizure frequency, seizure type, medication, family history of epilepsy | A multivariate linear regression |
BDI |
| Zhao 2012 [53] | 140 | 15–71 | Complex partial seizures, number of seizure types | Gender, seizure type, seizure frequency, number of anti-epilepsy drugs | NR | HAMD |
Although there are fewer studies reporting the incidence of epilepsy with depression in our meta-analysis, some studies suggest that depression is associated with epilepsy. Depression in epilepsy can change the response to treatment, aggravate the condition, reduce the quality of life, and increase the risk of suicidal tendencies among patients with epilepsy [61]. A study reported that major depression was associated with a sixfold increased risk of unprovoked seizures (95% CI, 1.56–22) [67].
This work focused more on the relationship between epilepsy and depression and the risk factors for depression in patients with epilepsy. Our study found that people pay more attention to the prevalence of depression in epilepsy than that epilepsy in depression. Moreover, it has been reported that epilepsy and depression share a common pathogenic mechanism [7]; thus, we believe that our study has implications for clinical work.
There are some limitations in this article. A wide variety of age ranges from 0.03 to 96 were sampled; this decreased the number of studies that could be pooled for further analyses. The studies had varied clinical diagnostic criteria used for depression or epilepsy. MINI is most frequently used in diagnosis of depression as gold standard [41]. Some studies suggested that PHQ-9, NDDI-E and HAMD did not differ statistically from MINI in the diagnosis of depression [23,41]. No studies have yet reported whether statistical differences exist between different diagnostic methods of epilepsy—this may influence the rate of depression in epilepsy or vice versa.
Conclusion
Our study found that epilepsy was associated with an increased risk of depression. We worked with a limited number of studies, and their number was unevenly distributed among the three groups (depression in epilepsy, epilepsy in depression, and comorbidity); however, we can still draw some conclusions. Epilepsy is associated with an incidence of depression, and depression is associated with the severity of epilepsy. We thus need pay more attention to mental health for patients with epilepsy. The treatment of depression requires a more positive method, and interpretation of this meta-analysis requires caution. There was a large heterogeneity among the studies, and it may influence our results. More studies are needed in distinct populations and with accurate estimates to inform public health policy and prevention. This can help define health resource needs in these populations.
Supporting information
(PDF)
(PDF)
Data Availability
All relevant data are within the article and its Supporting Information files.
Funding Statement
1. The S&T Program of Hebei (grant no. 20567625H) provided computer and related software for this work, and Lin Pei is the recipient of the funding awards. 2. Pei Lin National Famous and Old Chinese Medicine Expert Inheritance Studio provided databases search costs, and Lin Pei is the recipient of the funding awards. 3. Postgraduate Innovation Funding Project of Hebei University of Chinese Medicine (grant no. XCXZZBS2022011) provided training funding for the meta-analysis, and Shao-kun Qin is the recipient of the funding awards.
References
- 1.Nevitt SJ, Sudell M, Cividini S, Marson AG, Tudur Smith C. Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data. Cochrane Database Syst Rev. 2022;4(4):Cd011412. doi: 10.1002/14651858.CD011412.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88(3):296–303. doi: 10.1212/WNL.0000000000003509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maguire MJ, Marson AG, Nevitt SJ. Antidepressants for people with epilepsy and depression. Cochrane Database Syst Rev. 2021;4(4):Cd010682. doi: 10.1002/14651858.CD010682.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu Y, Sun G, Yang F, Guan Z, Zhang Z, Zhao J, et al. Baicalin regulates depression behavior in mice exposed to chronic mild stress via the Rac/LIMK/cofilin pathway. Biomed Pharmacother. 2019;116:109054. doi: 10.1016/j.biopha.2019.109054 [DOI] [PubMed] [Google Scholar]
- 5.Mazarati AM, Pineda E, Shin D, Tio D, Taylor AN, Sankar R. Comorbidity between epilepsy and depression: role of hippocampal interleukin-1beta. Neurobiol Dis. 2010;37(2):461–67. doi: 10.1016/j.nbd.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ping X, Qin SK, Liu SN, Lu Y, Zhao YN, Cao YF, et al. Effects of Huazhuo Jiedu Shugan Decoction on cognitive and emotional disorders in a rat model of epilepsy: possible involvement of AC-cAMP-CREB signaling and NPY expression. Evid Based Complement Alternat Med. 2019;2019:4352879. doi: 10.1155/2019/4352879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Błaszczyk B, Czuczwar SJ. Epilepsy coexisting with depression. Pharmacol Rep. 2016;68(5):1084–92. doi: 10.1016/j.pharep.2016.06.011 [DOI] [PubMed] [Google Scholar]
- 8.Lacey CJ, Salzberg MR, D’Souza WJ. What factors contribute to the risk of depression in epilepsy?—Tasmanian Epilepsy Register Mood Study (TERMS). Epilepsia. 2016;57(3):516–22. doi: 10.1111/epi.13302 [DOI] [PubMed] [Google Scholar]
- 9.Subota A, Pham T, Jette N, Sauro K, Lorenzetti D, Holroyd-Leduc J. The association between dementia and epilepsy: a systematic review and meta-analysis. Epilepsia. 2017;58(6):962–72. doi: 10.1111/epi.13744 [DOI] [PubMed] [Google Scholar]
- 10.Mohammadi MR, Alavi SS, Ahmadi N, Khaleghi A, Kamali K, Ahmadi A, et al. The prevalence, comorbidity and socio-demographic factors of depressive disorder among Iranian children and adolescents: to identify the main predictors of depression. J Affect Disord. 2019;247:1–10. doi: 10.1016/j.jad.2019.01.005 [DOI] [PubMed] [Google Scholar]
- 11.Nuyen J, Schellevis FG, Satariano WA, Spreeuwenberg PM, Birkner MD, van den Bos GA, et al. Comorbidity was associated with neurologic and psychiatric diseases: a general practice-based controlled study. J Clin Epidemiol. 2006;59(12):1274–84. doi: 10.1016/j.jclinepi.2006.01.005 [DOI] [PubMed] [Google Scholar]
- 12.Adewuya AO, Ola BA. Prevalence of and risk factors for anxiety and depressive disorders in Nigerian adolescents with epilepsy. Epilepsy Behav. 2005;6(3):342–47. doi: 10.1016/j.yebeh.2004.12.011 [DOI] [PubMed] [Google Scholar]
- 13.Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Almaskari B, et al. Prevalence of depression and anxiety among patients with epilepsy attending the epilepsy clinic at Sheikh Khalifa Medical City, UAE: a cross-sectional study. Epilepsy Behav. 2015;52(Pt A):194–99. doi: 10.1016/j.yebeh.2015.09.008 [DOI] [PubMed] [Google Scholar]
- 14.Baker GA, Jacoby A, Buck D, Brooks J, Potts P, Chadwick DW. The quality of life of older people with epilepsy: findings from a UK community study. Seizure. 2001;10(2):92–99. doi: 10.1053/seiz.2000.0465 [DOI] [PubMed] [Google Scholar]
- 15.Bautista RE, Erwin PA. Analyzing depression coping strategies of patients with epilepsy: a preliminary study. Seizure. 2013;22(9):686–91. doi: 10.1016/j.seizure.2013.05.004 [DOI] [PubMed] [Google Scholar]
- 16.Bosak M, Turaj W, Dudek D, Siwek M, Szczudlik A. Depressogenic medications and other risk factors for depression among Polish patients with epilepsy. Neuropsychiatr Dis Treat. 2015;11:2509–17. doi: 10.2147/NDT.S91538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canuet L, Ishii R, Iwase M, Ikezawa K, Kurimoto R, Azechi M, et al. Factors associated with impaired quality of life in younger and older adults with epilepsy. Epilepsy Res. 2009;83(1):58–65. doi: 10.1016/j.eplepsyres.2008.09.001 [DOI] [PubMed] [Google Scholar]
- 18.Chaka A, Awoke T, Yohannis Z, Ayano G, Tareke M, Abate A, et al. Determinants of depression among people with epilepsy in central Ethiopia. Ann Gen Psychiatry. 2018;17:27. doi: 10.1186/s12991-018-0197-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cianchetti C, Bianchi E, Guerrini R, Baglietto MG, Briguglio M, Cappelletti S, et al. Symptoms of anxiety and depression and family’s quality of life in children and adolescents with epilepsy. Epilepsy Behav. 2018;79:146–53. doi: 10.1016/j.yebeh.2017.11.030 [DOI] [PubMed] [Google Scholar]
- 20.Cramer JA, Blum D, Reed M, Fanning K. The influence of comorbid depression on seizure severity. Epilepsia. 2003;44:1578–84. doi: 10.1111/j.0013-9580.2003.28403.x [DOI] [PubMed] [Google Scholar]
- 21.Cramer JA, Blum D, Fanning K, Reed M, Epilepsy Impact Project G. The impact of comorbid depression on health resource utilization in a community sample of people with epilepsy. Epilepsy Behav. 2004;5(3):337–42. doi: 10.1016/j.yebeh.2004.01.010 [DOI] [PubMed] [Google Scholar]
- 22.Cramer JA, Brandenburg N, Xu X. Differentiating anxiety and depression symptoms in patients with partial epilepsy. Epilepsy Behav. 2005;6(4):563–69. doi: 10.1016/j.yebeh.2005.02.017 [DOI] [PubMed] [Google Scholar]
- 23.Di Capua D, Garcia-Garcia ME, Reig-Ferrer A, Fuentes-Ferrer M, Toledano R, Gil-Nagel A, et al. Validation of the Spanish version of the Neurological Disorders Depression Inventory for Epilepsy (NDDI-E). Epilepsy Behav. 2012;24(4):493–96. doi: 10.1016/j.yebeh.2012.06.005 [DOI] [PubMed] [Google Scholar]
- 24.Espinosa Jovel CA, Ramirez Salazar S, Rincon Rodriguez C, Sobrino Mejia FE. Factors associated with quality of life in a low-income population with epilepsy. Epilepsy Res. 2016;127:168–74. doi: 10.1016/j.eplepsyres.2016.08.031 [DOI] [PubMed] [Google Scholar]
- 25.Ettinger A, Reed M, Cramer J. Depression and comorbidity in community-based patients with epilepsy or asthma. NEUROLOGY. 2004;63:1008–14. doi: 10.1212/01.wnl.0000138430.11829.61 [DOI] [PubMed] [Google Scholar]
- 26.Fuller-Thomson E, Brennenstuhl S. The association between depression and epilepsy in a nationally representative sample. Epilepsia. 2009;50(5):1051–58. doi: 10.1111/j.1528-1167.2008.01803.x [DOI] [PubMed] [Google Scholar]
- 27.Gaitatzis A, Carroll K, Majeed A, Sander JW. The epidemiology of the comorbidity of epilepsy in the general population. Epilepsia. 2004;45(12):1613–22,. doi: 10.1111/j.0013-9580.2004.17504.x [DOI] [PubMed] [Google Scholar]
- 28.Han SH, Kim B, Lee SA, Korean Qo LiESG. Contribution of the family environment to depression in Korean adults with epilepsy. Seizure. 2015;25:26–31. doi: 10.1016/j.seizure.2014.11.011 [DOI] [PubMed] [Google Scholar]
- 29.Jo S, Kim HJ, Kim HW, Koo YS, Lee SA. Sex differences in factors associated with daytime sleepiness and insomnia symptoms in persons with epilepsy. Epilepsy Behav. 2020;104(Pt A):106919. doi: 10.1016/j.yebeh.2020.106919 [DOI] [PubMed] [Google Scholar]
- 30.Kui C, Yingfu P, Chenling X, Wenqing W, Xiuhua L, Di S. What are the predictors of major depression in adult patients with epilepsy? Epileptic Disord. 2014;16(1):74–79. doi: 10.1684/epd.2014.0634 [DOI] [PubMed] [Google Scholar]
- 31.Kwan P, Yu E, Leung H, Leon T, Mychaskiw MA. Association of subjective anxiety, depression, and sleep disturbance with quality-of-life ratings in adults with epilepsy. Epilepsia. 2009;50(5):1059–66. doi: 10.1111/j.1528-1167.2008.01938.x [DOI] [PubMed] [Google Scholar]
- 32.Lee SA, Jeon JY, No SK, Park H, Kim OJ, Kwon JH, et al. Factors contributing to anxiety and depressive symptoms in adults with new-onset epilepsy. Epilepsy Behav. 2018;88:325–31. doi: 10.1016/j.yebeh.2018.10.005 [DOI] [PubMed] [Google Scholar]
- 33.Li Q, Chen D, Zhu LN, Wang HJ, Xu D, Tan G, et al. Depression in people with epilepsy in West China: status, risk factors and treatment gap. Seizure. 2019;66:86–92. doi: 10.1016/j.seizure.2019.02.014 [DOI] [PubMed] [Google Scholar]
- 34.Lopez-Gomez M, Ramirez-Bermudez J, Campillo C, Sosa AL, Espinola M, Ruiz I. Primidone is associated with interictal depression in patients with epilepsy. Epilepsy Behav. 2005;6(3):413–16. doi: 10.1016/j.yebeh.2005.01.016 [DOI] [PubMed] [Google Scholar]
- 35.Mensah SA, Beavis JM, Thapar AK, Kerr M. The presence and clinical implications of depression in a community population of adults with epilepsy. Epilepsy Behav. 2006;8(1):213–19. doi: 10.1016/j.yebeh.2005.09.014 [DOI] [PubMed] [Google Scholar]
- 36.Milovanovic M, Martinovic Z, Toskovic O. Determinants of quality of life in people with epilepsy in Serbia. Epilepsy Behav. 2014;31:160–66. doi: 10.1016/j.yebeh.2013.12.015 [DOI] [PubMed] [Google Scholar]
- 37.Mori Y, Kanemoto K, Onuma T, Tanaka M, Oshima T, Kato H, et al. Anger is a distinctive feature of epilepsy patients with depression. The Tohoku journal of experimental medicine. 2014;232(2):123–28. doi: 10.1620/tjem.232.123 [DOI] [PubMed] [Google Scholar]
- 38.Ottman R, Lipton RB, Ettinger AB, Cramer JA, Reed ML, Morrison A, et al. Comorbidities of epilepsy: results from the Epilepsy Comorbidities and Health (EPIC) survey. Epilepsia. 2011;52(2):308–15. doi: 10.1111/j.1528-1167.2010.02927.x [DOI] [PubMed] [Google Scholar]
- 39.Peterson CL, Walker C, Shears G. The social context of anxiety and depression: exploring the role of anxiety and depression in the lives of Australian adults with epilepsy. Epilepsy Behav. 2014;34:29–33. doi: 10.1016/j.yebeh.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 40.Pompili M, Lester D, Innamorati M, Girardi P. Depression, hopelessness and suicide risk among patients suffering from epilepsy. Ann Ist Super SanItà. 2007;43 (4):425–29. [PubMed] [Google Scholar]
- 41.Rashid H, Katyal J, Sood M, Tripathi M. Depression in persons with epilepsy: a comparative study of different tools in Indian population. Epilepsy Behav. 2021;115:107633. doi: 10.1016/j.yebeh.2020.107633 [DOI] [PubMed] [Google Scholar]
- 42.Ridsdale L, Wojewodka G, Robinson E, Landau S, Noble A, Taylor S, et al. Characteristics associated with quality of life among people with drug-resistant epilepsy. J Neurol. 2017;264(6):1174–84. doi: 10.1007/s00415-017-8512-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Silagadze K, Kasradze S, Silagadze T, Lomidze G. Validation of a Georgian version of the Neurological Disorders Depression Inventory for Epilepsy (NDDI-E). Epilepsy Behav. 2019;101(Pt A):106587. doi: 10.1016/j.yebeh.2019.106587 [DOI] [PubMed] [Google Scholar]
- 44.Somayajula S, Vooturi S, Jayalakshmi S. Psychiatric disorders among 165 patients with juvenile myoclonic epilepsy in India and association with clinical and sociodemographic variables. Epilepsy Behav. 2015;53:37–42. doi: 10.1016/j.yebeh.2015.09.024 [DOI] [PubMed] [Google Scholar]
- 45.Stefanello S, Marín-Léon L, Fernandes PT, Li LM, Botega NJ. Depression and anxiety in a community sample with epilepsy in Brazil. Arq Neuropsiquiatr. 2011;69(2-B):342–48. [DOI] [PubMed] [Google Scholar]
- 46.Tegegne MT, Mossie TB, Awoke AA, Assaye AM, Gebrie BT, Eshetu DA. Depression and anxiety disorder among epileptic people at Amanuel Specialized Mental Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. 2015;15:210. doi: 10.1186/s12888-015-0589-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tellez-Zenteno JF, Patten SB, Jette N, Williams J, Wiebe S. Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia. 2007;48(12):2336–44. doi: 10.1111/j.1528-1167.2007.01222.x [DOI] [PubMed] [Google Scholar]
- 48.Tsegabrhan H, Negash A, Tesfay K, Abera M. Co-morbidity of depression and epilepsy in Jimma University specialized hospital, Southwest Ethiopia. Neurology India. 2014;62(6):649–55. doi: 10.4103/0028-3886.149391 [DOI] [PubMed] [Google Scholar]
- 49.Viguera AC, Fan Y, Thompson NR, Lapin B, Chaitoff A, Griffith SD, et al. Prevalence and predictors of depression among patients with epilepsy, stroke, and multiple sclerosis using the Cleveland Clinic Knowledge Program within the neurological institute. Psychosomatics. 2018;59(4):369–78. doi: 10.1016/j.psym.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 50.Wang HJ, Tan G, Deng Y, He J, He YJ, Zhou D, et al. Prevalence and risk factors of depression and anxiety among patients with convulsive epilepsy in rural West China. Acta neurologica Scandinavica. 2018;138(6):541–47. doi: 10.1111/ane.13016 [DOI] [PubMed] [Google Scholar]
- 51.Yildirim Z, Ertem DH, Ceyhan Dirican A, Baybas S. Stigma accounts for depression in patients with epilepsy. Epilepsy Behav. 2018;78:1–6. doi: 10.1016/j.yebeh.2017.10.030 [DOI] [PubMed] [Google Scholar]
- 52.Zeber JE, Copeland LA, Amuan M, Cramer JA, Pugh MJ. The role of comorbid psychiatric conditions in health status in epilepsy. Epilepsy Behav. 2007;10(4):539–46. doi: 10.1016/j.yebeh.2007.02.008 [DOI] [PubMed] [Google Scholar]
- 53.Zhao T, Sun MY, Yu PM, Zhu GX, Tang XH, Shi YB, et al. Evaluation of clinical aspects and quality of life as risk factors for depression in patients with epilepsy. Seizure. 2012;21(5):367–70. doi: 10.1016/j.seizure.2012.03.006 [DOI] [PubMed] [Google Scholar]
- 54.Zheng Y, Ding X, Guo Y, Chen Q, Wang W, Zheng Y, et al. Multidisciplinary management improves anxiety, depression, medication adherence, and quality of life among patients with epilepsy in eastern China: a prospective study. Epilepsy Behav. 2019;100(Pt A):106400. doi: 10.1016/j.yebeh.2019.07.001 [DOI] [PubMed] [Google Scholar]
- 55.Kumar N, Lhatoo R, Liu H, Colon-Zimmermann K, Tatsuoka C, Chen P, et al. Depressive symptom severity in individuals with epilepsy and recent health complications. J Nervous Mental Dis. 2019;207(4):284–90. doi: 10.1097/NMD.0000000000000963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sah SK, Rai N, Sah MK, Timalsena M, Oli G, Katuwal N, et al. Comorbid depression and its associated factors in patients with epilepsy treated with single and multiple drug therapy: a cross-sectional study from Himalayan country. Epilepsy Behav. 2020;112:107455. doi: 10.1016/j.yebeh.2020.107455 [DOI] [PubMed] [Google Scholar]
- 57.St Germaine-Smith C, Liu M, Quan H, Wiebe S, Jette N. Development of an epilepsy-specific risk adjustment comorbidity index. Epilepsia. 2011;52(12):2161–67. doi: 10.1111/j.1528-1167.2011.03292.x [DOI] [PubMed] [Google Scholar]
- 58.Ngugi AK, Kariuki SM, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Incidence of epilepsy: a systematic review and meta-analysis. Neurology. 2011;77(10):1005–12. doi: 10.1212/WNL.0b013e31822cfc90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kanner AM. Depression and epilepsy: do glucocorticoids and glutamate explain their relationship? Curr Neurol Neurosci Rep. 2009;9(4):307–12. doi: 10.1007/s11910-009-0046-1 [DOI] [PubMed] [Google Scholar]
- 60.Bell GS, Sander JW. Suicide and epilepsy. Curr Opin Neurol. 2009;22(2):174–78. doi: 10.1097/WCO.0b013e328328f8c3 [DOI] [PubMed] [Google Scholar]
- 61.Kanner AM. Depression and epilepsy: a new perspective on two closely related disorders. Epilepsy Curr. 2006;6(5):141–46. doi: 10.1111/j.1535-7511.2006.00125.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hitiris N, Mohanraj R, Norrie J, Sills GJ, Brodie MJ. Predictors of pharmacoresistant epilepsy. Epilepsy Res. 2007;75(2–3):192–96. doi: 10.1016/j.eplepsyres.2007.06.003 [DOI] [PubMed] [Google Scholar]
- 63.Thijs RD, Surges R, O’Brien TJ, Sander JW. Epilepsy in adults. Lancet. 2019;393(10172):689–701. doi: 10.1016/S0140-6736(18)32596-0 [DOI] [PubMed] [Google Scholar]
- 64.Gill SJ, Lukmanji S, Fiest KM, Patten SB, Wiebe S, Jetté N. Depression screening tools in persons with epilepsy: a systematic review of validated tools. Epilepsia. 2017;58(5):695–705. doi: 10.1111/epi.13651 [DOI] [PubMed] [Google Scholar]
- 65.Chu C. Association between epilepsy and risk of depression: a meta-analysis. Psychiatry Res. 2022;312:114531. doi: 10.1016/j.psychres.2022.114531 [DOI] [PubMed] [Google Scholar]
- 66.Yang Y, Yang M, Shi Q, Wang T, Jiang M. Risk factors for depression in patients with epilepsy: a meta-analysis. Epilepsy Behav. 2020;106:107030. doi: 10.1016/j.yebeh.2020.107030 [DOI] [PubMed] [Google Scholar]
- 67.Hesdorffer DC, Hauser WA, Annegers JF, Cascino G. Major depression is a risk factor for seizures in older adults. Ann Neurol. 2000;47(2):246–49. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the article and its Supporting Information files.