Abstract
Background
The increasing menace of the COVID-19 epidemic led to an atmosphere of anxiety around the world, however the evidence among Chinese students aged 12 to 18 years has been limited.
Methods
A total of 373216 junior and senior high school students were recruited using a cluster sampling method in Zhengzhou, Xinxiang, Xinyang city of Henan Province, China, during February 4-12, 2020. Presence of anxiety symptoms was determined by Generalized Anxiety Disorder tool (GAD-7). Multiple logistic regression was performed to estimate the potential risk factors.
Results
Among the participants, junior and senior high school students were found to have anxiety symptoms, producing an overall prevalence of 9.89%. The prevalence was lower in female than in male (9.66% vs. 10.11%) and the prevalence was higher for junior high school students than senior high school students (13.89% vs. 12.93%). The prevalence of anxiety symptoms was highest among rural students and lowest among urban students (11.33% vs. 8.77%). The cognitive level was negatively associated with the prevalence of anxiety symptoms. After adjusting for potential confounders, age, gender, residential location, worried level, fear level and behavior status were found to be associated with anxiety symptoms.
Limitations
Prevalence may be skewed by assessing anxiety symptoms using self-reported scales rather than clinical interviews.
Conclusions
This large-scale study assesses the prevalence of anxiety symptoms and its potential influencing factors in junior and senior high school students. These findings suggest that governments need to pay more attention to the mental health of young people in combating COVID-19.
Keywords: Anxiety, COVID-19, China, Factors, Prevalence, Students
1. Introduction
In December 2019, a novel coronavirus (COVID-19) has been identified (Lu et al., 2020), which raised global concern (Wang et al., 2020a). It spreads widely and rapidly and causes an outbreak of acute infectious pneumonia (Bao et al., 2020). Given its high person-to-person transmission rate, multiple appropriate measures (including social distancing, quarantine, and isolation) were implemented in many cities and rural areas in China during the Spring Festival. Although many measures might have moderated the spread of severe acute respiratory syndrome coronavirus Type 2 (SARS-COV-2), which causes COVID-19, they can also have a negative impact on the economy, employment, and public health (Brooks et al., 2020). The increasing menace of the epidemic led to an atmosphere of anxiety around the world due to disrupted travel plans, social isolation, media information overload and panic buying of necessity goods (Ho et al., 2020).
Anxiety disorders are one of the most common and disabling mental health conditions that are distributed across the globe (Baxter et al., 2013, Baxter et al., 2014, Kessler et al., 2007, Whiteford et al., 2010, Wittchen et al., 2010). In addition, the previous study had reported anxiety disorders may increase the risk of cancer, cardiovascular disease and some forms of anxiety have been associated with a lower risk of death (Batelaan et al., 2016; Eaton et al., 2013; Miloyan et al., 2016; Mykletun et al., 2009; Wang et al., 2020c). It is already evident that the direct and indirect psychological and social effects of the COVID-19 pandemic are widespread and could affect mental health now and future (González-Sanguino et al., 2020; Holmes et al., 2020; Khadse et al., 2020; Mattila et al., 2021; Stepowicz et al., 2020). The increasing number of confirmed cases and the growing number of provinces and countries affected by the outbreak have contributed to the increasing prevalence of public anxiety (Li et al., 2020). However, the effects of the COVID-19 pandemic on mental health could differ between population groups (Pan et al., 2020). Although there is growing empirical evidence of mental health complications of COVID-19 in adults, our knowledge of the impact of the pandemic on the mental health of young people remains very limited (Nearchou et al., 2020). In particular, adolescents are a vulnerable group that is presenting with more and more complex issues (Membride, 2016). Additionally, there is more and more evidence that the prevalence of adolescent emotional disorders is increasing (Glowinski and D'Amelio, 2016). The study indicated that most universal, selective, and indicated prevention programs are effective in reducing symptoms of anxiety in adolescents (Neil and Christensen, 2009).
As a province with the largest educational population in China, Henan province has an educational population of 28.53 million. It has a border with Hubei province and the two provinces have close exchanges with each other. The situation of epidemic prevention and control in the education system is very serious. Therefore, the present study included 373216 junior and senior high school students in Henan Province during the COVID-19 outbreak and aimed to assess the prevalence of anxiety symptoms and identify the potential risk and protective factors contributing to anxiety. According to past experience, winter and spring are likely to be the peak of the outbreak. Therefore, from the perspective of current global epidemic prevention and control, the Spring Festival in 2021 will still be affected by COVID-19. This may assist government agencies and healthcare professionals in safeguarding the psychological well-being of the junior and senior high school students in the face of COVID-19 outbreak expansion in China and different parts of the world.
2. Methods
2.1. Study participants
We conducted this cross-sectional study in order to investigate the impact of the COVID-19 pandemic on the anxiety symptoms from February 4, 2020 and February 12, 2020. Junior and senior high school students aged 12-18 years were recruited by using a cluster sampling method in Zhengzhou, Xinxiang, Xinyang city of Henan Province, China, and invited to participate in the online survey through an online survey platform (“SurveyStar”, Changsha Ranxing Science and Technology, Shanghai, China). After excluding the data of participants aged<12 years or aged>18 years or those who took ≤100 s to fully respond to the questions (n = 34276), finally, a total of 373216 participants were included in the analysis. These regions can represent the overall conditions of Henan Province.
2.2. Data collection
A standard questionnaire was designed to collect basic socio-demographic information (sex, age, grade, and residential location), the cognitive level was reflected to the subjects’ understanding of the epidemic characteristics of the COVID-19, including “will it be passed from person to person”, “route of transmission”, and “quarantine for several days after exposure”, each of these questions was divided into two groups: correct and wrong, mental state (worry and fear), a specific anxiety symptoms and other factors. Residential location was divided into 3 categories: city, rural and country-level city. The worried and fear levels (including “extremely” “very” “somewhat’” “not so” and “not at all”), assigned a score to each response on 5-point Likert scale (Gupta and Maity, 2021). High level was defined as 4-5 points, moderate level was defined as 3 points, and low or none level was defined as 1-2 points. Behavioral status reflected the change of people's lifestyle after knowing about the epidemic, which including “whether to increase the frequency of hand washing”, “going out wearing a mask”, “whether to give up the Spring Festival to visit relatives or travel because of the epidemic”, and “going out for dinner”. Behavioral status was divided into 3 levels: all correct, not all correct and all wrong (Li et al., 2020).
Anxiety symptoms were assessed by using the Chinese version of Generalized Anxiety Disorder tool (GAD-7) which is a simple and highly effective self-assessment tool for anxiety symptoms (Löwe et al., 2008). Participants were asked how often seven symptoms had appeared in your life over the past two weeks on a 21-point scale ranging from “not at all” (0 points), “several days” (1 points), “more than half the days” (2 points) and “nearly every day” (3 points). The scores for symptom severity were 5–9 for mild, 10–14 for moderate, and 15–21 for severe (Spitzer et al., 2006). A score of 10 or greater on the GAD-7 represents a reasonable cut point for identifying cases of GAD (Li et al., 2020).
2.3. Statistical analysis
Continuous variables were shown as means ± standard deviation (SD), and categorical variables were expressed as frequencies (%). Student's t-tests were performed to examine the difference in continuous variables, and the significance of the difference in categorical variables was assessed by chi-squared test.
The logistic regression model was used to estimate odds ratios (ORs) and 95% confidence intervals (CIs). Multivariable adjustment modelling was performed in this study: Model 1 was crude model. Model 2 was adjusted for age, gender, residential location, worried level, fear level and behavior status. All data were analyzed using SPSS and Excel and software version 21.0 (SPSS Inc., Chicago) and two‐tailed P values <0.05 were considered statistically significant.
3. Results
3.1. Basic characteristics of participants
Among 373216 participants included 244193 junior high school students and 129023 senior high school students (12-18 years old) were invited to participate in the online survey during the outbreak of COVID-19 in China. Table 1 showed the characteristics of participants and their associations with anxiety status. As compared to participants without anxiety symptoms, participants with anxiety symptoms were different from the proportion of sex, grade, residential location, worried level, fear level and behavior status (all P<0.05).
Table 1.
Characteristics of the study participants by anxiety status.
| Characteristics | All participants n=373216 | No-anxiety n=336298 | Anxiety n=36918 | P value |
|---|---|---|---|---|
| Age (years) | 15.24±1.59 | 15.26±1.60 | 15.06±1.58 | 0.009 |
| Gender (%) | <0.001 | |||
| Male | 193507(51.85) | 173943(51.72) | 19564(52.99) | |
| Female | 179709(48.15) | 162355(48.28) | 17354(47.01) | |
| Grade (%) | <0.001 | |||
| Junior | 244193(65.43) | 217703(64.74) | 26490(71.75) | |
| Senior | 129023(34.57) | 118595(35.26) | 10428(28.25) | |
| Residential location | <0.001 | |||
| City | 161576(43.29) | 147405(43.83) | 14171(38.39) | |
| Rural | 140737(37.71) | 124794(37.11) | 15943(43.18) | |
| Country-level city | 70903(19.00) | 64099(19.06) | 6804(18.43) | |
| Worried level (%) | <0.001 | |||
| High | 284399(76.20) | 250130(74.38) | 34269(92.82) | |
| Moderate | 66182(17.73) | 64195(19.09) | 1987(5.38) | |
| Low/none | 22635(6.06) | 21973(6.53) | 662(1.79) | |
| Fear level (%) | <0.001 | |||
| High | 194047(51.99) | 162755(48.40) | 31292(84.76) | |
| Moderate | 128397(34.40) | 124308(36.96) | 4089(11.08) | |
| Low/none | 50772(13.60) | 49235(14.64) | 1537(4.16) | |
| Behavior status (%) | <0.001 | |||
| All correct | 185958(49.83) | 167570(49.83) | 18388(49.81) | |
| Not all correct | 186662(50.01) | 168222(50.02) | 18440(49.95) | |
| All wrong | 596(0.16) | 506(0.15) | 90(0.24) |
Data were presented as mean (SD) normal distribution continuous variables and numbers (percentages) for categorical variables; P values calculated using student's t-test and chi-square.
Compared with No-anxiety, P <0.05
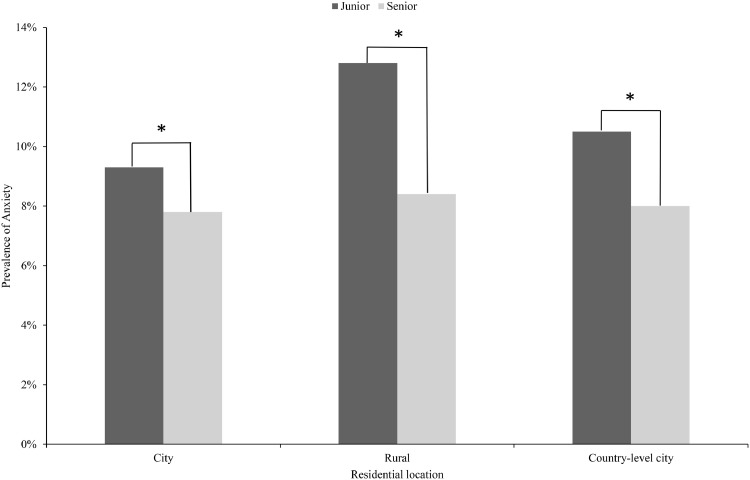
3.2. Prevalence of anxiety symptoms
The overall anxiety symptoms prevalence was 9.89% among junior and senior high school students during COVID-19 pandemic in China. The prevalence was lower in females than males (9.66% vs. 10.11%). Fig. 1 showed the prevalence of anxiety symptoms in participants by residential location and grade. The highest prevalence of anxiety symptoms was 12.80% found in participant lived in rural among junior high school students, and 8.40% found in participant lived in rural among senior high school students. The lowest prevalence of anxiety symptoms was 9.30% found in participant lived in city among junior high school students, and 7.80% found in participant lived in city among senior high school students. In brief, during the COVID-19 period, the proportion of junior high school students with anxiety symptoms was higher than that of senior high school students. Participants lived in city have the lowest prevalence of anxiety symptoms and participants lived in rural have the highest prevalence of anxiety symptoms among junior and senior high school students.
Fig. 1.
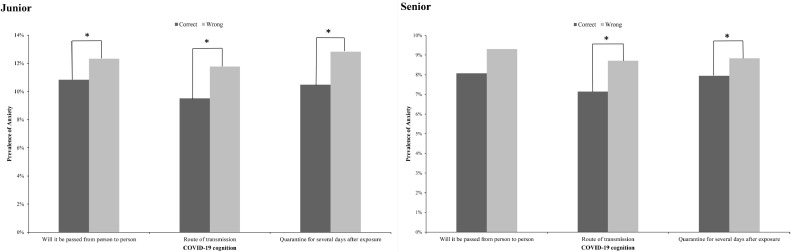
Fig. 2 showed the three most basic cognitive problems associated with the COVID-19. As can be seen from the figure, there is a difference in the prevalence of anxiety symptoms between those who answered the cognitive questions correctly and those who answered them incorrectly, in junior and senior high school students respectively. Students who lacked correct recognition of the COVID-19 were more prone to anxiety symptoms.
Fig. 2.
3.3. Anxiety symptoms
The proportion of students with different levels of anxiety symptoms were shown in Table 2 . Mild and moderate anxiety were most common. In junior high school students, the rate of mild anxiety was 28.06%, and that of moderate anxiety was 7.35%. Similarly, in senior high school students, the rate of mild anxiety was 29.43%, and that of moderate anxiety was 5.72%.
Table 2.
The rate of different severities of anxiety symptoms.
| Anxiety level | All participants | Junior students | Senior students | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| None | 229811 | 61.58 | 149193 | 61.10 | 80618 | 62.48 |
| Mild | 106487 | 28.53 | 68510 | 28.06 | 37977 | 29.43 |
| Moderate | 25332 | 6.79 | 17949 | 7.35 | 7383 | 5.72 |
| Severe | 11586 | 3.10 | 8541 | 3.50 | 3045 | 2.36 |
| Mild to serve | 143405 | 38.42 | 95000 | 38.90 | 48405 | 37.51 |
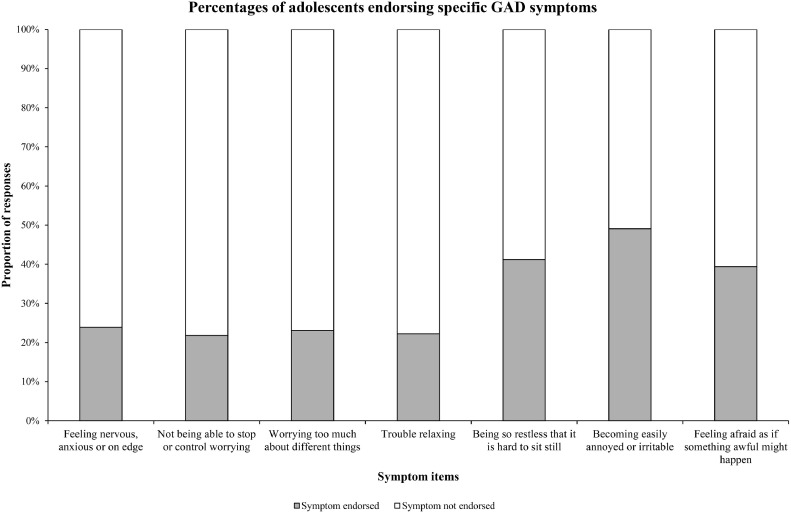
Fig. 3 showed there was a difference in response rates among the seven GAD symptoms in anxiety participants. Obviously, being so restless that it is hard to sit still (41.2%), becoming easily annoyed or irritable (49.1%), feeling afraid as if something awful might happen (39.4%) are the most common symptoms.
Fig. 3.
3.4. The positive or risk factors of anxiety symptoms
Table 3 presented the results of multivariable logistic regression analysis. Compared with male among junior and senior high school students, female had 8% [OR 0.92 (95% CI; 0.89-0.94)] and 16% [OR 0.84 (95% CI; 0.81-0.88)] reduced odds of anxiety. In junior high school students, compared with participants lived in city, participants lived in rural had 30% increased likelihood (OR 1.30 [95% CI 1.26–1.34]), just like participants lived in country-level city had 11% increased likelihood (OR 1.11[95% CI 1.07-1.15]). Compared with high worry level among junior and senior high school students, moderate worry level had 40% [OR 0.60 (95% CI; 0.56-0.64)] and 34% [OR 0.66 (95% CI; 0.61-0.73)] reduced odds of anxiety, low/none worry level had 39% [OR 0.61 (95% CI; 0.55-0.68)] and 22% [OR 0.78 (95% CI; 0.67-0.92)] reduced odds of anxiety. Similarly, compared with high fear level among junior and senior high school students, moderate fear level had 79% [OR 0.21 (95% CI; 0.20-0.22)] and 80% [OR 0.20 (95% CI; 0.19-0.21)] reduced odds of anxiety, low/none fear level had 79% [OR 0.21 (95% CI; 0.20-0.23)] and 81% [OR 0.19 (95% CI; 0.17-0.21)] reduced odds of anxiety. However, compared with high behavior status level among junior and senior high school students, moderate behavior status level had 4% increased likelihood (OR 1.04 [95% CI 1.01-1.07]) and 6% increased likelihood (OR 1.06 [95% CI 1.01-1.10]), just like low behavior status level had 172% increased likelihood (OR 2.72[95% CI 2.01-3.68]) and 193% increased likelihood (OR 2.93[95% CI 1.97-4.35]).
Table 3.
Independent association of characteristics of study participants and anxiety during the COVID-19 epidemic in Henan province.
| Characteristics | All participants OR (95%CI) | Junior students OR (95%CI) | Senior students OR (95%CI) | |||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Gender | ||||||
| Male | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) |
| Female | 0.95(0.93-0.97)* | 0.89(0.87-0.91)* | 0.96(0.93-0.98)* | 0.92(0.89-0.94)* | 0.94(0.90-0.98)* | 0.84(0.81-0.88)* |
| Residential location | ||||||
| City | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) |
| Rural | 1.33(1.30-1.36)* | 1.20(1.17-1.23)* | 1.44(1.40-1.48)* | 1.30(1.26-1.34)* | 1.08(1.03-1.13)* | 0.97(0.93-1.02) |
| Country-level city | 1.10(1.07-1.14)* | 1.06(1.03-1.10)* | 1.15(1.11-1.20)* | 1.11(1.07-1.15)* | 1.03(0.98-1.09) | 1.00(0.94-1.05) |
| Worried level | ||||||
| High | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) |
| Moderate | 0.23(0.22-024)* | 0.62(0.59-0.65)* | 0.22(0.21-0.23)* | 0.60(0.56-0.64)* | 0.24(0.22-0.26)* | 0.66(0.61-0.73)* |
| Low/none | 0.22(0.20-0.24)* | 0.66(0.60-0.72)* | 0.20(0.18-0.22)* | 0.61(0.55-0.68)* | 0.26(0.23-0.30)* | 0.78(0.67-0.92)* |
| Fear level | ||||||
| High | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) |
| Moderate | 0.17(0.17-0.18)* | 0.20(0.20-0.21)* | 0.17(0.17-0.18)* | 0.21(0.20-0.22)* | 0.18(0.17-0.19)* | 0.20(0.19-0.21)* |
| Low/none | 0.16(0.15-0.17)* | 0.20(0.19-0.21)* | 0.16(0.15-0.17)* | 0.21(0.20-0.23)* | 0.17(0.15-0.18)* | 0.19(0.17-0.21)* |
| Behavior status | ||||||
| All correct | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) |
| Not all correct | 1.00(0.98-1.02) | 1.04(1.02-1.07)* | 1.00(0.97-1.02) | 1.04(1.01-1.07)* | 1.00(0.96-1.04) | 1.06(1.01-1.10)* |
| All wrong | 1.62(1.29-2.03)* | 2.80(2.20-3.56)* | 1.53(1.16-2.03)* | 2.72(2.01-3.68)* | 1.87(1.28-2.72)* | 2.93(1.97-4.35)* |
Abbreviation: OR, odds ratio; CI, confidence interval.
Model 1: no adjustment.
Model 2: adjusted for age, gender, residential location, worried level, fear level and behavior status.
P<0.05.
4. Discussion
This was a large-scale cross-sectional epidemiological study based in Henan Province, which has the largest educational population in China, investigating the prevalence of anxiety symptoms in 373,216 junior and senior high school students during the COVID-19 outbreak. Our study showed that the overall prevalence of anxiety symptoms in junior and senior high school students was 9.89% (10.85% for junior high school students and 8.08% for senior high school students). Age, gender, grade, residential location, worried level, fear level and behavior status were found to be associated with anxiety symptoms among junior and senior high school students.
Given an overall global prevalence of anxiety disorders estimated to be normally around 7.3% (Santabárbara et al., 2020), however, our results suggest that anxiety symptoms prevalence in junior and senior high school students was 9.89% during the COVID-19 outbreak. It might be caused by epidemic prevention and control measures during COVID-19 period. At the beginning of the COVID-19 outbreak in China, about one-third reported moderate-to-severe anxiety. Female gender, student status, and specific physical symptoms were associated with a greater psychological impact of the outbreak and higher levels of stress, anxiety, and depression (Wang et al., 2020b). Another data showed that a large-scale survey of college students in China demonstrates that about 45% students have probable acute stress, anxiety or depressive symptoms during the COVID-19 epidemic (Ma et al., 2020). As is supposed above, the anxiety symptoms are likely to affect more populations during this pandemic, and we should try to assess the impact of COVID-19 on other vulnerable populations, such as adolescents, to maintain the mental health of vulnerable populations.
Our study showed that participants who lived in city have the lowest prevalence of anxiety and participants who lived in rural have the highest prevalence of anxiety among junior and senior high school students. It may be because the high level of socioeconomic status of urban student's parents. A large body of study have shown that socioeconomic status has a strong protective effect on physical and mental health outcomes (Burgard et al., 2013; Dowd et al., 2011; Morris et al., 1994). Parents' emotions can affect their children. Meanwhile, the prevalence of anxiety in junior high school students is higher than that in senior high school students. Therefore, we should pay more attention to protect the psychological status of rural students, by developing interventions and prevention and control measures. The prevalence of anxiety was also significantly higher among students with low cognition. This suggests that we need to strengthen the promotion of COVID-19 knowledge, especially in the transmission route, where the awareness rate is low. Through publicity and education, students can have a more comprehensive understanding of COVID-19, so as to protect themselves from life habits such as hand washing, exercise and nutrition, and reduce the influence of COVID-19 on anxiety among students.
Moreover, we subdivided the level of anxiety, and the results showed that most students were mild anxiety, while only a few students were moderate to severe anxiety. Of note, among the anxious students, being so restless that it is hard to sit still (41.2%), becoming easily annoyed or irritable (49.1%), feeling afraid as if something awful might happen (39.4%) are the most common symptoms. So, we suggested that the health department could provide an online psychological intervention platform where students can seek online psychological support when they have the above three symptoms.
To our knowledge, this is a large sample study of the prevalence of anxiety symptoms in junior and senior high school students. Secondly, as a province with the largest education population in China, Henan province has a border with Hubei province and close contacts between the two provinces, which is representative of students' anxiety during the period of the COVID-19. Thirdly, we used the standardized questionnaire (GAD-7) to diagnose anxiety. Finally, we excluded the participants who not meeting the requirements of this study to make our results more realistic.
Nevertheless, there are some limitations that should be considered when interpreting our results. First, although many important variables were already considered and adjusted, the possibility of other potential confounding factors remain cannot be ruled out. Second, prevalence may be skewed by assessing anxiety symptoms using self-reported scales rather than clinical interviews. Third, the presence of anxiety symptoms was determined by Generalized Anxiety Disorder tool (GAD-7), which is a simple and highly effective self-assessment tool for anxiety symptoms. However, a single screening tool does not guarantee the reliability and validity of the study. Fourth, the cognitive level reflected the subjects’ understanding of the epidemic characteristics of the COVID-19, but the validity of the cognitive level has not been guaranteed. Finally, the participants in this study were junior and senior high school students, which may limit the extension of our findings to other grade students.
In conclusion, among junior and senior high school students in China, rate of anxiety symptoms was not optimal during the COVID-19 epidemic, especially for students living in rural areas. These findings suggest that governments need to pay more attention to the mental health of young people in combating COVID-19. In the follow-up work, factors including age, gender, grade, residential location, cognitive level, worried level, fear level, and behavior status may be considered as part of the overall management of anxiety symptoms.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgments
Acknowledgements
The authors thank the participants for their supports during the study.
Author statement
Qingqing Xu and Zhenxing Mao designed research; Hualiang Lin, Xian Wang, Xiaomin Lou, Chongjian Wang, Dandan Wei and Juan Wang collected the data; Qingqing Xu analyzed the data and drafted the manuscript; Zhenxing Mao, Cuiping Wu, Pengling Liu and Keliang Fan revised the manuscript. Cuiping Wu had primary responsibility for final content. All authors read and approved the final manuscript.
Role of funding source
This work was supported by the National Natural Science Foundation of China (82041021).
References
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30309-3. e37-e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batelaan N.M., Seldenrijk A., Bot M., van Balkom A.J., Penninx B.W. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br. J. Psychiatry. 2016;208:223–231. doi: 10.1192/bjp.bp.114.156554. [DOI] [PubMed] [Google Scholar]
- Baxter A.J., Scott K.M., Vos T., Whiteford H.A. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol. Med. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Baxter A.J., Vos T., Scott K.M., Ferrari A.J., Whiteford H.A. The global burden of anxiety disorders in 2010. Psychol. Med. 2014;44:2363–2374. doi: 10.1017/S0033291713003243. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard S.A., Elliott M.R., Zivin K., House J.S. Working conditions and depressive symptoms: a prospective study of US adults. J. Occup. Environ. Med. 2013;55:1007–1014. doi: 10.1097/JOM.0b013e3182a299af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd J.B., Albright J., Raghunathan T.E., Schoeni R.F., Leclere F., Kaplan G.A. Deeper and wider: income and mortality in the USA over three decades. Int. J. Epidemiol. 2011;40:183–188. doi: 10.1093/ije/dyq189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton W.W., Roth K.B., Bruce M., Cottler L., Wu L., Nestadt G., Ford D., Bienvenu O.J., Crum R.M., Rebok G., Anthony J.C., Muñoz A. The relationship of mental and behavioral disorders to all-cause mortality in a 27-year follow-up of 4 epidemiologic catchment area samples. Am. J. Epidemiol. 2013;178:1366–1377. doi: 10.1093/aje/kwt219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowinski A.L., D'Amelio G. Depression Is a Deadly Growing Threat to Our Youth: Time to Rally. Pediatrics. 2016;138 doi: 10.1542/peds.2016-2869. [DOI] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.A., Muñoz M. Mental health consequences of the Covid-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020 doi: 10.1016/j.pnpbp.2020.110219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A.K., Maity C. Efficacy and safety of Bacillus coagulans LBSC in irritable bowel syndrome: A prospective, interventional, randomized, double-blind, placebo-controlled clinical study [CONSORT Compliant] Medicine (Baltimore). 2021;100:e23641. doi: 10.1097/MD.0000000000023641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Ann. Acad. Med. Singap. 2020;49:155–160. [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Angermeyer M., Anthony J.C., R D.E.G., Demyttenaere K., Gasquet I., G D.E.G., Gluzman S., Gureje O., Haro J.M., Kawakami N., Karam A., Levinson D., Medina Mora M.E., Oakley Browne M.A., Posada-Villa J., Stein D.J., Adley Tsang C.H., Aguilar-Gaxiola S., Alonso J., Lee S., Heeringa S., Pennell B.E., Berglund P., Gruber M.J., Petukhova M., Chatterji S., Ustün T.B. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- Khadse P.A., Gowda G.S., Ganjekar S., Desai G., Murthy P. Mental Health Impact of COVID-19 on Police Personnel in India. Indian J. Psychol. Med. 2020;42:580–582. doi: 10.1177/0253717620963345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Miao Y., Zeng X., Tarimo C.S., Wu C., Wu J. Prevalence and factors for anxiety during the coronavirus disease 2019 (COVID-19) epidemic among the teachers in China. J. Affect. Disord. 2020;277:153–158. doi: 10.1016/j.jad.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care. 2008;46:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., Zhao J., Li Y., Chen D., Wang T., Zhang Z., Chen Z., Yu Q., Jiang J., Fan F., Liu X. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020;29 doi: 10.1017/S2045796020000931. e181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattila E., Peltokoski J., Neva M.H., Kaunonen M., Helminen M., Parkkila A.K. COVID-19: anxiety among hospital staff and associated factors. Ann. Med. 2021;53:237–246. doi: 10.1080/07853890.2020.1862905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Membride H. Mental health: early intervention and prevention in children and young people. Br. J. Nurs. 2016;25:556–557. doi: 10.12968/bjon.2016.25.10.552. 552-554. [DOI] [PubMed] [Google Scholar]
- Miloyan B., Bulley A., Bandeen-Roche K., Eaton W.W., Gonçalves-Bradley D.C. Anxiety disorders and all-cause mortality: systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2016;51:1467–1475. doi: 10.1007/s00127-016-1284-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J.K., Cook D.G., Shaper A.G. Loss of employment and mortality. BMJ. 1994;308:1135–1139. doi: 10.1136/bmj.308.6937.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mykletun A., Bjerkeset O., Overland S., Prince M., Dewey M., Stewart R. Levels of anxiety and depression as predictors of mortality: the HUNT study. Br. J. Psychiatry. 2009;195:118–125. doi: 10.1192/bjp.bp.108.054866. [DOI] [PubMed] [Google Scholar]
- Nearchou F., Flinn C., Niland R., Subramaniam S.S., Hennessy E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil A.L., Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin. Psychol. Rev. 2009;29:208–215. doi: 10.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Pan K.Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., Rhebergen D., Oppen P.V., Giltay E.J., Penninx B. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Lasheras I., Lipnicki D.M., Bueno-Notivol J., Moreno M.P., López-Antón R., De la Cámara C., Lobo A., Gracia-García P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020 doi: 10.1016/j.pnpbp.2020.110207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stepowicz A., Wencka B., Bieńkiewicz J., Horzelski W., Grzesiak M. Stress and Anxiety Levels in Pregnant and Post-Partum Women during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17249450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y.H., Li J.Q., Shi J.F., Que J.Y., Liu J.J., Lappin J.M., Leung J., Ravindran A.V., Chen W.Q., Qiao Y.L., Shi J., Lu L., Bao Y.P. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol. Psychiatry. 2020;25:1487–1499. doi: 10.1038/s41380-019-0595-x. [DOI] [PubMed] [Google Scholar]
- Whiteford H.A., Degenhardt L., Rehm J., Baxter A.J., Ferrari A.J., Erskine H.E., Charlson F.J., Norman R.E., Flaxman A.D., Johns N., Burstein R., Murray C.J., Vos T. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study. Lancet. 2010;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Jacobi F., Rehm J., Gustavsson A., Svensson M., Jönsson B., Olesen J., Allgulander C., Alonso J., Faravelli C., Fratiglioni L., Jennum P., Lieb R., Maercker A., van Os J., Preisig M., Salvador-Carulla L., Simon R., Steinhausen H.C. The size and burden of mental disorders and other disorders of the brain in Europe. Eur. Neuropsychopharmacol. 2010;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]