Abstract
It is known that discrete events causing extreme societal and economic pressures as well as technological opportunity are major driving factors of innovation. Due to the presence of both of these factors during the COVID-19 pandemic it was hypothesized that there would be significant on-going innovation throughout society during the pandemic, with many of the innovations having the ability to have long-term societal impact. Analysis of literature and patent databases determined sectors of accelerated innovation to include manufacturing, personal protective equipment and digital technologies. The ability of flexible and advanced manufacturing technologies to provide more adaptable production capabilities that are less susceptible to disruption, make it likely that these technologies will be incorporated further, changing the way many manufacturing firms operate. Collaboration has increased, demonstrating increases in problem-solving efficiency; however, concerns around intellectual property is likely to reduce the long-term impact of these procedural changes. Advancements in personal protective equipment and disinfection technologies may have the long-term impact of reducing waste production and triggering changes in cleaning protocols throughout society. Digital technologies such as telemedicine, data collection, artificial intelligence and communication technologies were found to have undergone significant innovation, with possible impacts such as large-scale systemic shifts, and changes in how governments, corporations, the scientific community and the public interact.
Keywords: COVID-19, Technological innovation, Telemedicine, Artificial intelligence, 3D Printing
1. Introduction
It has previously been shown that the majority of innovations are developed in response to discrete events and new technological opportunities [1]. In this context, innovation is defined as a creative response requiring the commitment of resources to the development of new products or processes [1]. The coronavirus disease 2019 (COVID-19) pandemic can be assumed to be a discrete event that has caused pressures that are known to drive innovation such as declines in profit, increased demand of specialized products, and supply chain disruptions [1]. This pandemic has also occurred at a time of technological opportunity, due to progressive on-going research in fields such as advanced manufacturing, robotics, and digital technologies and the inception of their corresponding implementation into various sectors of society. As the impact of the COVID-19 pandemic has expanded well beyond the boundaries of the healthcare system, societal and economic impacts of the pandemic have influenced every aspect of individuals’ lives across the globe [2]. Policies imposed due to the pandemic including mandatory quarantines, physical distancing, and travel limitations have transformed daily life, disrupting educational institutions, large and small corporations, and governmental institutions [[2], [3], [4]]. Considering the combination of these factors, it was hypothesized that the COVID-19 pandemic would be a driving force of innovation throughout society, with many of the innovations demonstrating the potential for long-term impact.
In order to explore the impacts of COVID-19 on innovation a literature-based output approach was used. Literature and US and Canadian patent database searches were conducted with the World Health Organization's (WHO) declaration of the COVID-19 pandemic (March 11, 2020) selected as a start date [5]. Results from the literature and patent databases searches were then sorted based on their field of impact and categories with a significant number of contributions were further analyzed. This search demonstrated that in the medical field, research related to COVID-19 diagnosis, treatment, drug development and vaccine production is ongoing at an unprecedented rate [6,7]. Within five months of SARS-CoV-2 being discovered, there were over 200 therapies in development, with 38 having reached clinical trials [7]. Although the importance of this medical research cannot be overstated, much of this research was considered to be limited in long-term social impact, separate from its use in combating COVID-19. The increased rate of research and innovation related to diagnosis and treatment has been documented and will not be further discussed here; however, in reviewing this literature, innovation related to the operation and collaboration of companies involved in this research became evident and is discussed [7,8]. The literature and patent searches demonstrated that other sectors undergoing significant innovation included advanced manufacturing technologies, personal protective equipment, and digital technologies. As innovation in these fields have the ability to have long-term societal impact these categories were selected for further analysis and discussion.
At this point in the pandemic, society is beginning to adapt to the new normal; however, there has been little time to reflect on long-term impacts of on-going innovation. As analysis of major historical innovation often relates major technological shifts to the evolution of economies and societies, it is important to take the time to consider how current innovation related to a significant current event may have long-term societal impacts [1]. This work aims to provide an overview of innovative procedures and technologies implemented during the pandemic and provide a starting point in analyzing the possibility of long-term societal impact of these innovations.
2. Manufacturing
Societal and economic impacts significantly altered consumer demand for various items with crisis-critical goods (PPE, diagnostic tests, ventilators etc.) becoming a global priority [[8], [9], [10]]. In order to adapt to the change in demand, many manufacturing companies were driven by governmental order, need to retain profitability, or willingness to prioritize public health, to shift production focus and methodology [3,8]. In doing this, large scale manufacturing companies demonstrated an ability to leverage their resources and specialized knowledge, and cooperate with competitors in order to support healthcare systems [8,11]. However, new entrants into manufacturing of crisis-critical goods were not limited to large manufacturing companies [8,12,13]. Many educational institutions, smaller corporations, and hobbyists became involved in manufacturing efforts to meet healthcare demands for certain products, often by leveraging advanced manufacturing techniques such as 3D printing [11,14].
2.1. Organizational shifts
In order to meet healthcare systems’ demand for crisis-critical equipment large-scale manufacturing shifts in production were required [8,11]. Manufacturers from sectors including automotive, aerospace, home appliance, fashion and luxury goods have all become involved in the production of these critical goods [8]. Companies with specialized manufacturing equipment, relevant expertise, or with flexible/diverse technology and resources all adapted to the circumstances and prioritized the production of products required to protect global health [8]. Other firms contributed by forming new collaborations, sharing their intellectual property, pledging to keep intellectual property related to COVID-19 available until the end of the pandemic, or providing open source designs [8]. Research groups, small organizations, and individuals with access to resources that could be applied to production also became voluntarily involved with fabrication of in-demand products as they prioritized healthcare [8,12]. All of these shifts demonstrate creative methods of adapting to uncertain circumstances.
Many manufacturing firms possess diverse and advanced equipment integrated as part of their normal manufacturing process [11]. Having access to the flexible technological capability provided by this equipment has demonstrated its importance in recent months, as it allowed organizations to shift production to focus on providing unprecedented levels of many specialized healthcare products [11]. This was illustrated by manufacturers previously involved in the production of chemical, luxury, and alcoholic goods as many were able to leverage their technological capabilities to efficiently shift focus to the production of sanitizers and disinfectants [8]. For example, Louis Vuitton voluntarily decided to modify its perfume production lines to produce hand sanitizer, to be delivered free to health professionals, while distilleries across the globe modified their production lines to develop alcohol disinfectants and sanitizers [15,17]. The companies involved in these initiatives were not limited to international conglomerates, as much smaller businesses, such as Eight Oaks Farm Distillery, a family-owned distillery located in Pennsylvania, was one of the first distilleries to become involved in hand sanitizer production [17].
In a similar way, textile companies became involved with producing critical care products, as brands such as Zara, Prada, and Gucci switched production to development of protective face masks and medical gowns [[18], [19], [20]]. Individuals also became heavily involved with the production of PPE for health professionals. For example, Hackney Wick Scrubs Hub, a grass-roots project started by four women, has now provided over 3800 sets of scrubs to healthcare professionals as well as a template for the fabrication of basic PPE for public production [21].
The responsiveness of these companies and initiatives was made possible due to access to adaptable technology and expertise both on large and small scales [22]. As many corporations are struggling to maintain profitability during the COVID-19 pandemic and are unable to shift their production capabilities, it is likely that more organizations will look into implementing flexible technologies into their production process in the future [22]. This shift toward more advanced manufacturing technologies to allow for greater manufacturing flexibility could have a lasting impact on society by causing a shift in the skills required in different career paths. Automation has already replaced many manufacturing jobs in industries such as automotives, while increasing the demand for skills related to programming and equipment maintenance. Further implementation of flexible manufacturing equipment will require flexible workers, able to adapt to the development of a wider range of products [23]. This could lead to manufacturing firms that actively adapt to demand on a daily basis, allowing for smoother interactions between supply and demand. These organizational shifts also represent a shift in corporate ideologies, as many of the fabricated products were provided for free, demonstrating that the shift in production was not driven by a profit mentality. This change in corporate mentality is even more evident when looking at the increase in collaboration and cooperation between various organizations.
2.2. Collaboration
Due to the pathology of COVID-19, the pandemic caused global demand for ventilators to increase beyond global supply [24]. In the UK, the government required the production of over 15 000 new ventilator units [25]. In order to meet this demand, the UK Ventilator Challenge was developed, and a consortium of over 60 entities including industrial, technical and engineering firms was formed [25]. While some of the companies involved in the consortium contributed through providing increased manufacturing capacity, part sourcing, and technology for assembly, other collaborators focused on the production and improvement of technology related to non-invasive breathing aids [24]. For example, Dyson demonstrated its ability to apply its specialized knowledge of air flow in vacuums to the production of ventilators, and successfully invented a novel ventilator in 10 days [26].
Development related to the formulation of vaccines and treatments for COVID-19 has required unparalleled collaboration between pharmaceutical companies and research institutions. An example of this is the ChAdOx1 consortium, led by the Jenner Institute [27]. This consortium is focused on the production of an adenoviral vaccine, and includes entities such as Cobra Biologics, Rocky Mountain Laboratories, Halix BV (Netherlands) and Oxford University, and is funded by UK Research and Innovation (UKRI), and the Chinese Academy of Medical Sciences among others [27]. Other collaborations related to the production of vaccines include Clover and GSK, with GSK benefitting from Clover's large-scale manufacturing capacity, and Clover benefitting from access to GSK's protein-based vaccine candidate [28]. Oxford University is also collaborating with the Memorial Sloan Kettering Cancer Center, the University of British Columbia, PostEra, and Enamine to develop new drug therapies for COVID-19 [29]. Collaborations related to diagnostic testing and monitoring such as the collaborations between Bosch Healthcare Solutions (Germany) and Randox Laboratories (Northern Ireland) have led to the production of advanced point-of-care diagnostic tests, some of which are able to deliver results in under 3 h [30,31].
Previously, many of the organizations involved in consortiums such as the UK Ventilator Challenge were direct competitors, constantly vying to be the first to produce new findings and products; however, in the circumstances of a global pandemic these manufacturing firms have demonstrated an increasing willingness to collaborate. This ideological shift has led to increased research and production efficiency, as research-focused organizations often lack large-scale manufacturing and testing abilities, and manufacturing organizations often lack the specific knowledge required for advanced research and the manufacture of products outside of their normal domain. The societal impact of the maintenance of these collaborative attitudes beyond the conclusion of the COVID-19 pandemic could lead to more efficient research in other fields as the strengths of both research and manufacturing organizations are combined to allow for development of highly effective solutions to global problems. However, it is considered unlikely that these collaborative attitudes will be sustained to a similar degree once governmental and societal pressure decreases, though this crisis does indicate that the application of these pressures can lead to collaborative global action. Currently, some organizations have expressed concerns related to the protection of intellectual property once the pandemic concludes [8].
2.3. Advanced manufacturing techniques
While the formation of consortiums and increased collaboration was able to increase production rate, the pandemic has also provided a driving force for the implementation of more advanced manufacturing technologies [11,22]. Not only do more advanced manufacturing techniques have the ability to increase production rate, they also limit the number of individuals required for the manufacture of goods [11]. In the circumstances of a pandemic, this helps limit viral transmission by increasing physical distancing, which further helps to reduce production disruptions due to infectious diseases [11,32]. For example, use of artificial intelligence and wireless connectivity in the manufacturing sector, along with advanced robotics, allows for fully autonomous manufacture of goods [11]. Production lines incorporating advanced technologies are adaptable allowing for more efficient shifts in response to changing circumstances [11,22]. Challenges with implementation of these technologies include advancing the technological capabilities to the required level of autonomy, improving wireless communication systems to allow for the required data transfer, and ensuring that the equipment is modularized and flexible to allow for widespread application [33].
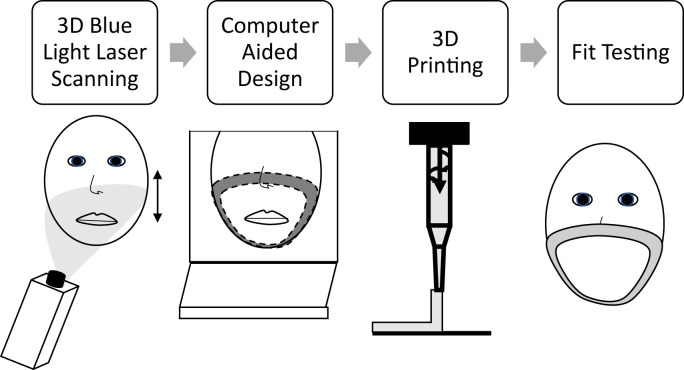
During the COVID-19 pandemic, 3D printing technologies have been identified and utilized as an innovative approach for solving many of the critical supply shortages and improving on current technologies and processes [11,14]. 3D scanning technologies may use white or blue light, with blue light providing better precision due to increased ability to filter interference [34]. These technologies provide the ability to design customized products in real-time, while 3D printing technologies allow for production of products on-site and on-demand by a wide-range of individuals and corporations due to the accessibility of 3D printing technologies [11,35]. 3D printing and 3D blue-light laser scanning have been implemented for the production of customized fitted masks, improving contact pressure and ensuring a better fit (Fig. 1 ) [36,37].
Fig. 1.
3D scanning and printing pathway for customized face masks.
As COVID-19 is most commonly transmitted via respiratory droplets, a perfect seal is required to protect healthcare professionals working in high-risk areas [38]. Due to recent research into 3D-printable materials, various thermoplastic elastomeric materials are available for mask production [14,39,40]. Face shields have also been printed using 3D technology to meet demand [14]. RAISE3D along with researchers at the University of North Carolina have created a protocol for home printing of face masks using transparent, lightweight materials, allowing anyone with a 3D printer to contribute to the production of crisis-critical supplies [40,41].
Other areas where 3D printing has been applied to meet demand include in vitro models, COVID-19 specimen collection kits, ventilator valves, and ventilators themselves [14,42]. While swabs can be fabricated from printable materials, fully 3D printed biosensors are currently being researched [14,43]. These advanced biosensors would provide rapid and inexpensive point-of-care diagnostic abilities which would be highly beneficial in resource-limited settings such as pandemics [43]. Mologic, a developer of rapid diagnostic technologies in the UK, has developed hand-held diagnostic technology, capable of providing results within 10 min that is fabricated through use of 3D printing [44]. In Italy, volunteers produced ventilator valves through 3D printing in order to combat shortage of the critical ventilator accessory, while Volkswagen (VW) identified 3D printing as a method for producing ventilators [45,46]. As VW has 125 industrial 3D printers at its disposal, the automaker was able to fabricate a wide range of products with the provision that it was provided with a design [46].
Advanced manufacturing technologies have become an area of focus for research, innovation, and implementation due to the economic and societal pressures imposed by the COVID-19 pandemic; however, there has been some concern over the quality and regulation of goods produced via 3D printing. Governments have outlined various standards and policies to better guide production; however, regulatory enforcement may be weak during time constrained settings [47]. Due to this, products produced may not consistently provide the protection required by healthcare professionals; however, implementation of autonomous and intelligent manufacturing has been highlighted as a method to protect workers and reduce future production line disruptions, while increasing manufacturing flexibility. Specifically, 3D printing technologies have been used to fabricate a wide range of products including face masks, face shields, elements of diagnostic tests, and ventilators. As access to 3D printing technology has increased in the last decade to be relatively widespread, users of 3D printing technology have ranged from individual hobbyists to large corporations. As the economic impact caused by the COVID-19 pandemic has generated significant interest in the implementation and use of advanced manufacturing technologies, it is likely that these technologies will be implemented and incorporated into society at an accelerated rate post-pandemic. This may have a long-term impact on manufacturing and society, as individuals will be able to become involved in the manufacture of goods. This pandemic has also initiated the development of regulations for 3D printed goods in various sectors, which will open new manufacturing opportunities for corporations. Table 1 summarizes the discussed impacts of COVID-19 on manufacturing ideologies and technologies.
Table 1.
Summary of manufacturing adaptations and technological implementation.
| Adaptation | Field | Cause | Highlights | Concerns | Ref. |
|---|---|---|---|---|---|
| Organizational Shifts | Chemical | Sanitizers | Efficient adaptation to changing circumstances and demand was made possible by incorporated flexible and diverse manufacturing technologies | Requirement of advanced modularized equipment and a capable information network | [8,11,12,[15], [16], [17], [18], [19], [20], [21], [22]] |
| Disinfectants | |||||
| Textile | PPE | ||||
| Grass Roots | PPE | ||||
| Automotive | Ventilators | ||||
| Aerospace | Ventilators | ||||
| Home Appliance | Ventilators | ||||
| Collaboration | Ventilators | Manufacturing Capacity | Ideological shift of businesses leading to increased willingness to collaborate in order to solve international problems | Intellectual property concerns after the conclusion of the pandemic | [8,[24], [25], [26], [27], [28], [29], [30], [31]] |
| Part Sourcing | |||||
| Assembly | |||||
| Novel Devices | |||||
| Vaccines/Drugs/Diagnostics | Specialized Knowledge | ||||
| Testing Capacity | |||||
| Production Capacity | |||||
| Funding | |||||
| Advanced Manufacturing Techniques | Intelligent Manufacturing | Autonomous Production | Allows for greater protection of workers while reducing supply chain and production disruptions | Regulatory concerns regarding products developed through 3D printing | [11,14,22,[32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47]] |
| 3D Printing | On-Demand Production | ||||
| Customization | |||||
| Specialized Products | |||||
| Grass Roots Initiatives |
3. Personal protective equipment and disinfection
Frontline healthcare workers are at a high risk of exposure to COVID-19, and as such must wear effective PPE such as masks, face shields, and respirators in order to avoid infection [13]. Much of the PPE currently used by healthcare professionals is meant to be disposed of after one use, and as such healthcare workers have required a large supply of PPE and have generated a large amount of waste [48]. Many governments have also recommended or mandated the use of masks by the general public further adding to demand [49,50]. While many organizations have focused on new methods of producing PPE in order to meet demand, other entities have focused on improving the technology currently in use [37,[51], [52], [53]].
N95 respirator masks, which are required by healthcare professionals in high-risk environments are personalized, fit-tested, and have a filter which is meant to be disposed of after each use [13,54]. The rapid depletion of these masks and filters during treatment of infectious diseases leads to resource constraints that put health care workers at risk [13]. As the demand for these healthcare grade masks has significantly increased with the COVID-19 pandemic many organizations have developed projects focused on the development of N95 alternatives that are reusable [[53], [54], [55]]. One such project is Stanford University's Pneumask which is focused on the production of a reusable full-face snorkel mask in order to reduce demand of N95 respirator masks [55]. A team at the University of Saskatchewan (U of S) also became involved with the 3D printing of masks as alternatives to the N95 masks required by health-care workers [56]. Prototypes of the U of S designed masks, which uses a flexible liner to allow for the mask to conform to different faces, is being tested by medical personnel for comfort, fit and quality [56].
Other innovations related to mask technologies have included the design of new masks, such as a protective oculo-respirator that covers the nose, eyes and mouth, that can be washed and disinfected, as well as masks that screen the wearer for coronavirus [51,57]. Investigation into methods of reuse of N95 masks has also been undertaken by research teams across the globe. Cobalt-60 gamma irradiation, steam sterilization, and ultraviolet germicidal irradiation have all been investigated as decontamination techniques that allow for mask reuse with mixed results [[58], [59], [60]]. While successful decontamination procedures would currently help reduce mask demand and further protect health care personnel, research and innovation in mask design will help to reduce healthcare waste moving forward.
Many of the procedures currently used to treat more severe symptoms of COVID-19 are high-risk, aerosol generating procedures [61]. Aerosol generating procedures, such as ventilation and intubation, put health care workers at greater risk, due to the requirement of close contact and the formation of greater volumes of aerosolized droplets, which are postulated to be the main form of transmission of COVID-19 [61,62]. In order to protect health care personnel from infection during high-risk procedures, protective tent-like structures have been developed [61]. These low-cost “corona curtains” help protect health care professionals by reducing the spread of aerosolized droplets, allowing for aerosol generating procedures to be completed at lower risk to the health care worker [61].
Significant research and innovation have also been seen in the field of disinfecting procedures. As infectious respiratory droplets exist in the air and can deposit on surfaces, disinfection is required in order to reduce spread of the disease [62]. Procedures such as germicidal ultraviolet air disinfection, which has shown effectiveness in reducing tuberculosis, influenza, and measles transmission, has been recommended for application in reducing the spread of COVID-19 [13,63]. Other organizations have worked to deploy disinfection robots that use hydrogen peroxide vapor and/or ultraviolet light to disinfect surfaces [52,64,65]. These robots have been deployed in hospitals and other high-risk areas to decontaminate entire hospital rooms including high-touch surfaces such as bed rails, trays and call buttons [52]. The use of robots helps decrease possible exposure of cleaning staff and the general public while also ensuring rigorous and effective decontamination [52].
PPE and disinfecting procedures are important components of combatting infectious diseases such as COVID-19. As the pandemic caused unprecedented demand, and resources became limited, research and innovation were required to combat supply shortages. Advancements in PPE technology allows for greater protection of healthcare workers and reduces demand and waste. Healthcare personnel are being further protected through the invention of new devices that reduce the spread of aerosolized droplets during high-risk procedures. Healthcare systems have also adapted to the circumstances by implementing advanced disinfection procedures and technologies. The incorporation of improved PPE technology and disinfection technologies will remain long after the COVID-19 pandemic concludes, helping to protect healthcare professionals and patients in the future while reducing the production of medical waste. Outside of the healthcare field, the implementation of air disinfection technologies will likely be investigated further for applications where air is recirculated and individuals are in close proximity, such as air travel. Widespread use of disinfection technologies to other institutions such as governmental and educational institutions may also become more common-place as society becomes more conscious of disease transmission. Table 2 summarizes the discussed research and innovation of PPE and protective alternatives.
Table 2.
Summary of the innovation of PPE and protective alternatives driven by COVID-19.
| Adaptation | Focus | Products and Procedures | Benefits | Concerns | Ref. |
|---|---|---|---|---|---|
| Use | Novel Reusable Products | Masks | Reduction of healthcare waste and demand for supplies moving forward | Regulatory and efficacy concerns over novel products and disinfection techniques | [13,37,[48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60],66] |
| Respirators | |||||
| Disinfection Procedures | Gamma Irradiation | ||||
| Steam Sterilization | |||||
| Ultraviolet Irradiation | |||||
| Alternatives and Additions | Novel Protective Products | Aerosol Protections | Increased protection provided to healthcare professionals and patients | Effectiveness and adaptability of technology | [52,[61], [62], [63], [64], [65]] |
| Air Disinfection | |||||
| Disinfection Robots |
4. Digital technologies
With governmental policies forcing offices, businesses, educational institutions, and some medical facilities to close, societal pressure has driven the innovative use and implementation of digital technologies in order to maintain some sense of normalcy and human connection [4,12,32,67]. Due to governmental policies related to physical distancing and gathering limits, many individuals have had to adapt to remote work and virtual communication, increasing society's reliance on digital technologies [2,4,32,67]. This increased reliance has led to greater general acceptance of digital technologies by society in many aspects.
Telemedicine, which had been struggling to find a foothold due to various regulatory and financial issues has become widely integrated and accepted [68,69]. New programs and apps have been developed and implemented for use in data collection, disease tracking, and epidemiological modelling, while artificial intelligence has been implemented in diagnosis and sorting technologies [8,70,71]. The pandemic has also driven research into the importance of communication and influence of communication methods in order to understand societal adherence to policies and the spread of misinformation [72,73]. While digital technologies have been steadily improving and being incorporated into society prior to the COVID-19 pandemic, societal pressure caused by the novel circumstances has led to widespread acceptance and integration of these technologies with the ability for substantial long-term impact [74].
4.1. Telemedicine
While COVID-19 caused cancellations and rescheduling of elective operations across the world, many individuals still require healthcare [75]. Telemedicine, defined as two-way live communication between a patient and provider utilizing audio and visual equipment and/or software, has evolved as a solution to this provision of continued healthcare while minimizing risk of exposure and transmission of COVID-19 [69,76,77]. Pre-pandemic, telemedicine had been implemented in some areas; however, barriers including lack of patient and provider acceptance, technical problems, and regulatory framework had slowed implementation [69,76]. With COVID-19 containment acting as a driving force, innovative approaches have been applied to expanding the availability of telemedicine, including virtual visits, teleproctoring, and mental health resources [69,78].
In the time and resource constrained settings caused by a global pandemic, telemedicine is beneficial for monitoring COVID-19 positive patients with mild or moderate symptoms, check-ups of high-risk patients, as well as standard chronic disease reviews, and administrative appointments [69,78]. This removes the need for travel, reduces the risk of transmission, and reduces the number of individuals gathered in waiting rooms, further protecting the public and healthcare workers [69]. While emergency rooms have seen a significant decrease in use, some practitioners fear that those requiring emergency medical attention are not seeking it due to fear of infection [68]. Use of telemedicine for virtual triaging provides an option for afflicted individuals to be examined to determine if medical attention is required [68]. Virtual triaging can also reduce treatment delay, as the examining doctor will be fully apprised of the medical requirements of the individual before they arrive for medical treatment [68,79]. Use of telemedicine for standard check-ups and patient monitoring is critical in pandemic scenarios; however, the time and cost savings provided, as well as public acceptance, make it likely that these applications will endure following the pandemic [75].
While non-critical procedures were rescheduled, many individuals could not have their procedures delayed [80]. Proctors, or supervisors with expertise in a certain procedure, are often present during complex operations in order to supervise and provide their input as required [81]. As travel restrictions made it impossible for some proctors to be present for planned operations, teleproctoring has been used to ensure the expertise of the proctor is still available in real-time [80]. Digital transmission systems that provide live feeds as well as telestration (live editing of images) have been developed to allow for efficient teleproctoring, which may reduce the need for in-person proctoring in the future [80].
The pandemic also interrupted counselling services such as those for eating disorders, addiction, and mental health [76,82,83]. Additional stress caused by the pandemic, coupled with the closing of many centers that provide counselling services, has exacerbated symptoms of those suffering from various disorders and addictions [83,84]. Continued treatment of those suffering from eating disorders has required increased communication between physicians, psychologists, patients and families using telemedicine, while continued care of those suffering from addiction has required the loosening of some regulations to allow for audio only telemedicine for basic treatment [76,82,85].
Health professionals are under extreme stress and have a high risk of suffering from post-traumatic stress symptoms similar to those who worked during the SARS outbreak [83,84,86]. Patients and uninfected individuals may also be suffering from lack of human contact caused by physically distancing policies. Online psychological counselling services have been widely established in order to combat the impacts of the pandemic on mental health, and a variety of media including video-conferencing, smartphone apps, and text-messaging have been shown to have a positive impact on mental health [84,87]. More advanced technology, such as robotics and virtual reality systems have also been employed in telemedicine, with virtual reality allowing individuals to feel as though they are in the same space as others due to the greater sense of social presence [11,88,89].
While implementation of telemedicine had previously been stalled by lack of acceptance by the public, providers and regulatory bodies, the COVID-19 pandemic made telemedicine capabilities essential [69,79]. As telemedicine increases patient and physician safety, while allowing for continued care and communication, patients and physicians have come to accept telemedicine, and even prefer it to face-to-face meetings for some tasks [75,79]. Physicians have found that telemedicine is more efficient and just as effective for some appointments, allowing for them to speak to more patients in a day [75]. Although telemedicine should not replace all appointments due to the lack of ability for physicians to do a full diagnostic exam or check-up, telemedicine could be used to replace many administrative appointments and general diagnoses, increasing the efficiency of the healthcare system moving forward [75].
Telemedicine has already had a marked positive impact on the healthcare system during the pandemic; however, there are concerns around data security, privacy, and regulation with its continued use [69,76]. As healthcare information is highly protected, advanced digital security systems will be required in order to allow the permanent integration of telemedicine into healthcare systems [69]. Regulatory bodies will also need to review their protocols and adapt them for situations were telemedicine is beneficial. Although there are still significant concerns with telemedicine, the economic and societal benefits reaped from more efficient healthcare systems makes it likely that the implementation of telemedicine will persist past the resolution of this crisis forever changing the structure of healthcare systems [75,80].
4.2. Data collection
One of the main requirements for controlling an infectious disease is tracking and modelling its transmission; however, accurate models require significant amounts of epidemiological data [90]. The required data for modelling and tracking of COVID-19 have been collected through various means and made readily available through many different open-source agreements [8,11,91]. Advanced computational methods and digital technologies such as mobile apps, the Internet of Things (IoT), and data mining algorithms have all been designed to help generate and make sense of all of the data produced during the pandemic [11,92]. However, large scale data collection and analysis has also brought privacy concerns to the forefront of many peoples’ minds [90].
Mobile phone data and big-data analysis have previously been used to predict the spread of infectious diseases such as Ebola and tuberculosis [93,94]. Contact tracing was used as a core surveillance tactic in the control of Ebola, with mobile apps playing a significant role in its success, due to data being more complete, accurate, and timely [93]. Owing to mobile apps’ previous success in helping to manage the spread of infectious diseases, it is not surprising that various digital and mobile applications were rapidly designed and implemented for the COVID-19 pandemic. Many of these applications are related to the acceptance of telemedicine as they focus on self-triage and self-scheduling to aid in following physical distancing policies, as well as providing mobile diagnostics and contact tracing [95,96].
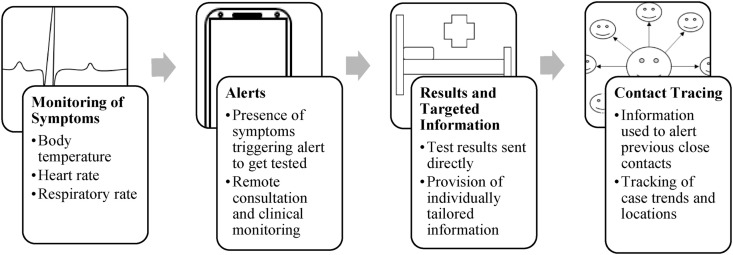
COVID-19 symptom tracking apps use self-reported information to provide information about the prevalence of COVID-19 cases in a given area [32,97]. Other apps allow for the collection and storage of temperature data for possible early diagnosis (Fig. 2 ) [32,98]. Similar to mobile applications, some organizations have developed biosensor technology for detection and monitoring of COVID-19 symptoms, including body temperature and respiration rate for early detection of illness and home monitoring [99]. These technologies can help limit the spread of disease while also reducing the load on hospitals by allowing patients to be monitored while remaining at home [99].
Fig. 2.
Use of mobile data collection for telemedicine applications including early diagnosis, monitoring, and contact tracing.
Some governmental apps, such as Singapore's “Trace Together”, focus on contact tracing by using mobile data location to determine whether individuals have been in locations with or after an individual who has tested positive for COVID-19 [100]. Apple and Google have collaborated on a similar app that requests that individuals voluntarily submit COVID-19 test results. Mobile phones with the app which had recently been in the vicinity of the individual with the confirmed case would then immediately be alerted via a text message [32]. Further digital innovations, such as the IoT and Big Data, have been employed, with IoT being used for enforcement of quarantines and mask-wearing through drone surveillance, as well as monitoring of patients quarantining at home [11,92]. Experts are also actively researching how to utilize Big Data for efficient drug development, and more accurate pandemic modelling as it is capable of updating data from patients under treatment on a real-time basis [91].
Concerns related to these technologies include their dependence on a large percentage of the population being in possession of a mobile phone, and reliance on self-reported data leading to possible inaccuracies [32,93,94]. The implementation of data collection technologies such as applications that utilize mobile phone data and/or collect healthcare information have increased societal concern over privacy and security, as people are being requested to prioritize public healthcare measures over their own personal privacy [32,90,92,96]. Individuals in many countries are having to balance invasion of privacy with increased sense of safety and communication related to the transmission of COVID-19 [101,102]. These concerns are further enhanced by the use of these technologies for quarantine and policy enforcement as advanced surveillance and facial recognition technologies have been heavily criticized due to abuse of power related to the technology [32,71,90,92]. While innovation related to data collection is currently highlighting the balance required between public safety and individual freedoms, the long-term impacts of normalizing these methods of data collection must be considered in terms of future policy and regulatory decisions.
4.3. Artificial intelligence
Artificial intelligence (AI) systems and deep learning neural networks (DNNs) can effectively sort through large data-sets to identify certain features [103]. These advanced algorithms allow devices to take data input and learn to distinguish patterns without supervision [103]. Based on the learnt patterns, AI systems are able to react and respond to changing circumstances in real time [103]. Benefits of applying AI in diagnostics and medical imaging interpretation, predictive modelling, and social control, had been identified before the onset of the COVID-19 pandemic; however, the COVID-19 pandemic has functioned as a driving force for greater innovation and integration of AI technologies [11,104,105].
Accurate and rapid diagnosis of COVID-19 is required to limit the spread of the disease and provide effective treatment to afflicted individuals [104]. Use of AI and DNN technologies to analyze chest x-rays and chest CT scans has demonstrated accuracy rates around 95%, exceeding human accuracy while providing immediate results [104,[106], [107], [108]]. The use of AI also allows for a contactless imaging workflow, as the imaging technician is able to provide positioning instructions through the use of cameras and microphones, with AI being used to identify the pose of the patient and automatically optimize scanning parameters [109].
From the images and diagnosis, AI has also been shown to be able to predict the likely severity and mortality risk of an infected individual, helping to inform treatment methods for the individual [104,110]. Another innovative approach related to the application of AI during COVID-19, is implementation of COVID-19 in communication systems for other workflows [111]. Response pathways, such as those related to acute strokes, have been put under pressure due to COVID-19 [111]. AI has been employed to speed up image analysis, interpretation and decision making in order to help reduce this pressure [111].
AI has also demonstrated its abilities as part of early warning, predictive, and tracking systems in relation to COVID-19, with two AI-based models succeeding in triggering alerts before the WHO and Program for Monitoring Emerging Diseases (PMED) [104]. Although the lack of historical data makes modelling the spread of COVID-19 difficult, AI forecasting has been successfully modified to predict epidemic trends [104,112]. With a large volume of data being generated due to the COVID-19 pandemic, AI has also been employed to help filter out noise and misinformation, with certain algorithms being designed to aid researchers and clinicians in finding the references and research they require [104,113].
Predictive modelling and future analysis will allow for assessment of the effectiveness of policies such as physical distancing and quarantines, which may help inform responses to future pandemics, while the ability to efficiently sift through all of the generated literature to find the information required will expedite research related to treatments and vaccine production. Implementation of AI into healthcare will help increase efficiency of the system further improving healthcare post-pandemic. Societal acceptance and further implementation and use of AI technologies in applications such as modelling and information filtering have the ability to increase the rate of scientific research and help reduce the spread of misinformation. Concerns related to the greater implementation of AI systems include the creation of biases in the algorithms due to biases in the information used to train the AI system [114]. These concerns must be considered as AI technologies are implemented in a broader range of applications in order to avoid incorrect or biased sorting and decision-making. However, it is likely that AI will be further implemented into many systems that require the filtering or modelling of large data sets to increase efficiency.
4.4. Communication and misinformation
Previous pandemics such as SARS and Ebola have demonstrated just how important communication is in handling public health threats, with countries and cities with superior communication systems faring significantly better [[115], [116], [117]]. Global communication between governments and researchers and communication with the public both play important roles in managing pandemics. Governmental communication allows for discussion of effective policies, scientific communication allows for greater collaboration and productivity in developing vaccines and therapeutics, and effective communication with the public helps control fear and uncertainty and ascertain compliance with governmental policies [117].
Many innovative approaches have been used to ensure effective communication during the COVID-19 pandemic. On the scientific research side, a call for open sharing of relevant literature has led to organizations such as Nature, The Lancet, and various companies providing free access to COVID-19 literature [8]. Organizations have also collaborated to release the Covid-19 Open Research Dataset (CORD-19) which collects peer-reviewed and pre-print papers related to COVID-19 in one place [118]. The dataset is actively updated in order to consolidate existing research and allow for researchers to find the information they need rapidly [118]. Communication between clinicians has also been researched and improved with the implementation of clinical newsletters and virtual education opportunities, helping clinicians lean on other members of their medical teams [119].
Communication with the public is extremely important in managing the outcome of a disease as it impacts compliance with policies, risk perception, and panic [117]. With the remarkable speed of information sharing possible through social media platforms, it is important that information is shared in a clear, accurate and timely manner [116]. Risk of infection, outcome of infection, lack of protection or prevention measures, rapid increases in reported cases or deaths, uncertainty regarding disease information, and suspicion that risks are being downplayed, can all contribute to greater societal fear, which can lead to activities such as panic buying and distrust of the government [117,120]. In order to provide easy access to understandable information, many interactive graphics and dashboards have been developed by both scientific and governmental organizations [[121], [122], [123]]. The use of technology for communication for hearing impaired individuals has also been made more common, due to the use of masks making it difficult for hearing impaired individuals to communicate [124]. For example, apps providing speech-to-text capabilities or direct connection to a translator have been made available in all emergency departments in Regina and Saskatoon, along with other parts of Saskatchewan [124].
However, even with all of the communication strategies being employed, the sheer volume of information has caused problems, including the sharing of misinformation and the formation of counterfeit products, sparking innovative approaches for managing misinformation [73,125,126]. As previously discussed, AI technologies can be used to sort through the large amount of information being shared with the goal of flagging pieces of information that are false, allowing for them to be removed or corrected [73]. The extent and volume of misinformation being shared during the COVID-19 pandemic has sparked significant research into how misinformation is generated and shared in order for organizations to be better prepared to combat the spread of misinformation in the future [72,73,120]. However, discussions around the moderation of information has also led to concerns regarding free speech, as controversial opinions may be censored by biased AI systems and moderators.
As the world has had to go digital for education, work, social connections, and information gathering, digital communication has become increasingly important. Researchers and clinicians have implemented innovative new forms of communication in order to ensure efficient and effective responses to the pandemic, while various organizations have developed methods of translating scientific understanding for the general public. The increased understanding of the importance of being able to share scientific information with layman audiences may have an impact on the operation of scientific communities as they strive to keep the public informed and updated regarding their work, in order to increase public support in future circumstances that require the public to trust science. Related to this, the ability to manage misinformation will become just as important as the digital technologies themselves. While the moderation of information being shared related to the pandemic is by no means perfect, with various conspiracy theories and pieces of misinformation gaining traction, COVID-19 has managed to trigger a new age of discussion into information moderation, that will continue long past the conclusion of the COVID-19 pandemic [73]. However, policies and regulations around information moderation will require evaluation to ensure that information moderation is unbiased, with the process of evaluation likely to require further in-depth discussion in the future, with possibilities for long-term impact. Table 3 summarizes the discussed innovations around digital technologies.
Table 3.
Summary of digital innovations driven by the COVID-19 pandemic.
| Technology | Application | Use | Benefits | Concerns | Ref. |
|---|---|---|---|---|---|
| Telemedicine | Virtual Visits | Out-Patient Monitoring | Improvement of efficiency of the healthcare system while reducing risk of transmission for patients and physicians | Regulatory and standard of care issues | [68,69,[75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89]] |
| Standard Reviews | |||||
| Administrative Appointments | |||||
| Virtual Triage | |||||
| Teleproctoring | Telestration | Provision of input from experts in extraneous circumstances | Technical and communication requirements | ||
| Mental Health Resources | Eating Disorders | Provision of on-going care in stressful circumstances | Access concerns | ||
| Addiction | |||||
| Post Traumatic Stress | |||||
| Isolation | |||||
| Data Collection | Mobile Applications | Disease Modelling and Tracking | More accurate disease modelling and tracking improves response times | Privacy and security of collected data | [8,11,32,71,[90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102]] |
| Contact Tracing | |||||
| Symptom Tracking/Early Diagnosis | Reliance on mobile phones disadvantages those with lower income | ||||
| Alerts | |||||
| Real-Time Modelling | |||||
| Drones/Facial Recognition | Surveillance | Advanced surveillance improves adherence to public health policies | Fears of living in a surveillance society | ||
| Enforcement | |||||
| Artificial Intelligence | Medical Imaging | Diagnoses | Improved healthcare efficiency, modelling, expedition of scientific research and flagging of misinformation for more effective responses to pandemic circumstances | Bias in data sets leading to biased analysis and decision-making | [11,[103], [104], [105], [106], [107], [108], [109], [110], [111], [112], [113], [114]] |
| Contactless Workflow | |||||
| Forecasting | Predictive Disease Modelling | ||||
| Disease Severity | |||||
| Information Sorting | Misinformation | Censorship of conflicting opinions | |||
| Scientific Research | |||||
| Communication and Misinformation | Governmental Communication | Increased Collaboration | Improved research efficiency and compliance with public health policies to increase effectiveness of response | Intellectual property rights | [8,72,73,[115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126]] |
| Scientific Communication | Open Resources | ||||
| Public Communication | Policy Compliance | Misinformation leading to increased fear, panic and lack of faith in governmental policies | |||
| Fear Management | |||||
| Misinformation | Flagging by AI |
5. Conclusions
The COVID-19 pandemic has had drastic societal and economic impacts. The adaption of society to this historical event in the making and all of the negative pressures that it incorporates has resulted in significant research, innovation and implementation of various technologies and processes, many of which are likely to have long-term societal impacts.
Manufacturing is one aspect of society that has been drastically impacted by the COVID-19 pandemic. In order to adapt to demand shifts, manufacturing firms with access to flexible, diverse and specialized equipment shifted their production focus and methodology. Collaborative mentalities have also increased, with competitors often working together to meet a set goal, or various corporations with complementary specialties partnering to problem-solve in a more efficient manner. Advanced manufacturing systems including those that incorporate AI, and robotics are also being investigated with renewed interest due to their lack of susceptibility to disruption during infectious disease outbreaks. 3D printing specifically, has demonstrated its flexibility in the production of various products, and its ability to be utilized by large corporations and individual hobbyists alike. As manufacturing flexibility, increased collaboration, and incorporation of advanced manufacturing technologies has been proven to provide corporations with means to adapt to extreme and changing circumstances, it is expected that these innovative approaches will be sustained post-pandemic will the potential to impact the availability of careers, the rate of global problem-solving, and manufacturing processes for a wider range of products.
Flaws in PPE technology such as its inability to be re-used and lack of suitable alternatives triggered significant research and innovation as many parties worked to solve these issues. Novel mask designs and methods for production have been proven to be effective in increasing the available supply of PPE, while methods for maintaining mask viability after disinfection have been validated, reducing demand and waste. Advanced technologies related to air decontamination and disinfection have been implemented in hospitals to better protect patients and healthcare workers. These technologies are not limited to this pandemic, as better PPE and reusable PPE can easily be expanded to other fields such as research, helping to limit the production of waste in the future while providing increased protection to the user and incorporation of disinfection technologies is likely to be expanded into other sectors of society as the public becomes more health-conscious.
As society has become highly dependent on digital technologies, increased acceptance and necessity has led to the implementation of these technologies in many different applications. Telemedicine, which had previously been facing many hurdles to implementation has been fully incorporated into many healthcare systems in order to allow for continued care and monitoring of patients. The continued use of telemedicine programs is expected after the conclusion of the pandemic due to the increased efficiency it offers; however, there are still regulatory concerns as well as concerns regarding the level of care provided, and privacy of personal information. Data collection abilities have been significantly improved with mobile applications being used for medical applications such as monitoring, diagnosis, and contact tracing, while advanced surveillance technologies are being used for policy enforcement. These technologies have caused increased discussion around personal privacy rights and fears of a surveillance society that may limit their application in the future. AI systems have been implemented in healthcare for diagnosis and modelling as well as information management systems for filtering of information. AI is likely to be further implemented as society continues to become increasingly digital, and will likely be heavily applied in the moderation of information; however, this has triggered concerns regarding biased sorting and moderation due to programmed bias. The large extent of information generated by situations such as a pandemic have also driven a greater research interest into communication and misinformation as communication has been shown to be highly important in combatting infectious diseases. Improvements made in communication technologies, and a new found understanding of the importance in communicating scientific principles clearly, is likely to force lasting changes on how scientific information is communicated regularly to the public.
While this work is not an exhaustive list of innovations and research triggered by the COVID-19 crises, it is clear that the societal and economic circumstances have resulted in significant innovation and implementation of technologies. COVID-19 has demonstrated that necessity is in fact the driver of change, and although this pandemic will be resolved, it is likely that many of the research and innovations that occurred due to the crisis will remain having long-term impacts on society.
Credit author statement
Amanda Zimmerling: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Visualization, Funding acquisition. Xiongbiao Chen: Conceptualization, Writing – review & editing, Supervision, Funding acquisition.
Declaration of competing interest
None.
Acknowledgments
This study was supported by the Natural Sciences and Engineering Research Council (NSERC) through an Undergraduate Student Research Award to Zimmerling and Saskatchewan Health Research Foundation (SHRF) via a Research Connections COVID-19 Rapid Response Grant to Zimmerling and Chen.
The funding sources had no involvement in the research and preparation of this work.
Biographies
Amanda Zimmerling completed her BSc. in Materials Engineering at the University of Alberta in June 2020. She has been accepted into the Direct-Entry PhD program for Biomedical Engineering starting Fall 2020. She is also the recipient of a Deans Research Award at the University of Saskatchewan for her previous undergraduate research in tissue engineering and development of novel materials for 3D printing. Her PhD research will be focussed on the use of 3D printing technologies in combatting infectious diseases such as COVID-19.
Dr. Chen is a Professor with the Department of Mechanical Engineering and Division of Biomedical Engineering, University of Saskatchewan (USask), Canada. He received his Ph.D. degree from USask in 2002 and was then working on his Post-Doctorate with Queen's University, Canada. In 2003 he joined USask as an Assistant Professor, then was promoted to Associate Professor and Full Professor in 2007 and 2010, respectively. His teaching and research interests include 3D bioprinting, tissue engineering, and mechatronics. Dr. Chen is a Fellow of the Canadian Academy of Engineering (CAE).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.techsoc.2021.101541.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Taalbi J. What drives innovation? Evidence from economic history. Res. Pol. 2017;46(8):1437–1453. doi: 10.1016/j.respol.2017.06.007. [DOI] [Google Scholar]
- 2.Haleem A., Javaid M., Vaishya R. Effects of COVID-19 pandemic in daily life. Current Medicine Research and Practice. 2020;10(2):78–79. doi: 10.1016/j.cmrp.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris M., Bhatti Y., Buckley J., Sharma D. Fast and frugal innovations in response to the COVID-19 pandemic. Nat. Med. 2020 doi: 10.1038/s41591-020-0889-1. [DOI] [PubMed] [Google Scholar]
- 4.Hsiang S., Allen D., Annan-Phan S., Bell K., Bolliger I., Chong T., Druckenmiller H., Huang L., Hultgren A., Krasovich E., Lau P., Lee J., Rolf E., Tseng J., Wu T. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020 doi: 10.1038/s41586-020-2404-8. http://www.ncbi.nlm.nih.gov/pubmed/32512578 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . World Health Organization; 11 Mar 2020. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19-11 March 2020.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Online]. Available: [Google Scholar]
- 6.Udugama B., Kadhiresan P., Kozlowski H., Malekjahani A., Osbourne M., Li V., Chen H., Mubareka S., Gubbay J., Chan W. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020;14(4):3822–3835. doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 7.Bryan K., Lemus J., Marshall G. Innovation during a crisis: evidence from COVID-19. SSRN Electronic Journal. 2020 doi: 10.2139/ssrn.3587973. [DOI] [Google Scholar]
- 8.Tietze F., Vimalnath P., Aristodemou L., Molloy J. Centre for Technology Management Working Paper Series; 2020. Crisis-Critical Intellectual Property: Findings from the COVID-19 Pandemic. no. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Majid B., Hammoumi A., Motahhir S., Lebbadi A., Ghzizal A. Preliminary design of an innovative, simple, and easy-to-build portable ventilator for COVID-19 patients. Euro-Mediterranean Journal for Environmental Integration. 2020;5(2):3–6. doi: 10.1007/s41207-020-00163-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ranney M., Griffith V., Jha A. Critical supply shortages- the need for ventilators and personal protective equipment during the covid-19 pandemic. N. Engl. J. Med. 2020;41(1) doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 11.Javaid M., Haleem A., Vaishya R., Bahl S., Suman R. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes and Metabolic Syndrome: Clin. Res. Rev. 2020;14(4):419–422. doi: 10.1016/j.dsx.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spear R., Erdi G., Parker M., Anastasiadis M. Interface; 2020. Innovations in Citizen Response to Crises: Volunteerism and Social Mobilization during COVID-19. [Google Scholar]
- 13.Nathavitharana R., Patel P., Tierney D., Mehrotra P., Lederer P., Davis S., Nardell E. Innovation and knowledge sharing can transform COVID-19 infection prevention response. J. Hosp. Med. 2020;15(5):299–301. doi: 10.12788/jhm.3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ishack S., Lipner S. Applications of 3D printing technology to address COVID-19- related supply shortages. Am. J. Med. 2020 doi: 10.1016/j.amjmed.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.BBC News . 16 March 2020. Coronavirus: Louis Vuitton Owner to Start Making Hand Sanitizer.https://www.bbc.com/news/business-51868756 [Online]. Available: [Google Scholar]
- 16.BBC News . 3 April 2020. Coronavirus Isle of Man: Distillery Switches from Gin to Hand Sanitizer.https://www.bbc.com/news/world-europe-isle-of-man-52150281 [Online]. Available: [Google Scholar]
- 17.Jones A. 24 March 2020. Distilleries across Canada Fight COVID-19 by Making Hand Sanitizer.https://www.ctvnews.ca/health/coronavirus/distilleries-across-canada-fight-covid-19-by-making-hand-sanitizer-1.4867110 [Online]. Available: [Google Scholar]
- 18.Russell C. Forbes; 19 March 2020. Zara Owner Starts Making Protective Face Masks to Fight Coronavirus.https://www.forbes.com/sites/callyrussell/2020/03/19/zara-owner-starts-making-protective-face-masks-to-fight-coronavirus/#c23553766765 [Online]. Available: [Google Scholar]
- 19.Bramley E. The Gaurdian; 24 March 2020. Prada the Latest Fashion Brand to Make Medical Face Masks.https://www.theguardian.com/fashion/2020/mar/24/prada-the-latest-fashion-brand-to-make-medical-face-masks [Online]. Available: [Google Scholar]
- 20.Ouyang I. South China Morning Post; 24 March 2020. Luxury Brands Join the Fight against COVID-19 as Retailers Use Their Factories to Churn Out Medical Supplies.https://www.scmp.com/business/companies/article/3076698/luxury-brands-join-fight-against-covid-19-retailers-use-their [Online]. Available: [Google Scholar]
- 21.Kirka D. abc News; 3 May 2020. Scrub Hub to the Rescue: 4 Women Succeed where UK Stumbled.https://abcnews.go.com/Business/wireStory/scrub-hub-rescue-women-succeed-uk-stumbled-70477170 [Online]. Available: [Google Scholar]
- 22.Kumar M., Raut R., Narwane V., Narkhede B. Applications of Industry 4.0 to overcome the COVID-19 operational challenges. Diabetes and Metabolic Syndrome: Clin. Res. Rev. 2020;14(5):1283–1289. doi: 10.1016/j.dsx.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rotman D. Inquiring Minds Topic; July/August 2013. How Technology Is Destroying Jobs. [Google Scholar]
- 24.Pooler M., Hughes L., Neville S., Hollinger P. 30 March 2020. Big Names of UK Engineering in Push to Make 30,000 Ventilators.https://www.ft.com/content/1125e39e-8a76-4769-b6ca-f482efca5bf5 [Online]. Available: [Google Scholar]
- 25.Ventilator Challenge UK . 16 April 2020. VentilatorChallengeUKConsortium.https://www.ventilatorchallengeuk.com/ [Online]. Available: [Google Scholar]
- 26.Jebara P. 27 March 2020. Dyson Designs Ventilator in 10 Days for COVID-19 Patients.https://www.architecturaldigest.com/story/dyson-designs-ventilator-10-days-covid-19-patients [Online]. Available: [Google Scholar]
- 27.Cobra Biologics (Cobra) 31 March 2020. Outsourced Pharma.https://www.outsourcedpharma.com/doc/cobra-biologics-proud-to-be-part-of-a-consortium-rapidly-develop-covid-vaccine-0001 [Online]. Available: [Google Scholar]
- 28.Biopharmaceuticals Clover. 24 February 2020. Clover and GSK Announce Research Collaboration to Evaluate Coronavirus (COVID-19) Vaccine Candidate with Pandemic Adjuvant System.https://www.gsk.com/en-gb/media/press-releases/clover-and-gsk-announce-research-collaboration-to-evaluate-coronavirus-covid-19-vaccine-candidate-with-pandemic-adjuvant-system/ [Online]. Available: [Google Scholar]
- 29.Compass Weizmann. 30 March 2020. Towards a Drug against COVID-19.http://www.weizmann.ac.il/WeizmannCompass/sections/briefs/towards-a-drug-against-covid-19 [Online]. Available: [Google Scholar]
- 30.Li X., Geng M., Peng Y., Meng L., Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. Journal of Pharmaceutical Analysis. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Engineer . 27 March 2020. Bosch Develops Rapid Covid-19 Test.https://www.theengineer.co.uk/bosch-covid-19-test/ [Online]. Available: [Google Scholar]
- 32.O'Leary D. Evolving information systems and technology research issues for COVID-19 and other pandemics. J. Organ. Comput. Electron. Commer. 2020 doi: 10.1080/10919392.2020.1755790. [DOI] [Google Scholar]
- 33.Vaidya S., Ambad P., Bhosle S. Industry 4.0- A glimpse. Procedia Manufacturing. 2018:233–238. doi: 10.1016/j.promfg.2018.02.034. [DOI] [Google Scholar]
- 34.Jeon J., Choi B., Kim C., Kim J., Kim H., Kim W. Three-dimensional evaluation of the repeatability of scanned conventional impressions of prepared teeth generated with white- and blue-light scanners. The Journal of Prothetic Dentistry. 2015;114(4):549–553. doi: 10.1016/j.prosdent.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 35.Wand M., Adams B., Ovsjanikov M., Berner A., Bokeloh M., Jenke P., Guibas L., Seidel H., Schilling A. Efficient reconstruction of nonrigid shape and motion for real-time 3D scanner data. ACM Trans. Graph. 2008;28(2) doi: 10.1145/1516522.1516526. [DOI] [Google Scholar]
- 36.Cai M., Li H., Shen S., Wang Y., Yang Q. Customized design and 3D printing of face seal for an N95 filtering facepiece respirator. J. Occup. Environ. Hyg. 2018;15(3):226–234. doi: 10.1080/15459624.2017.1411598. [DOI] [PubMed] [Google Scholar]
- 37.Sampol C. Medical Expo; 2 April 2020. COVID-19: Developing High Tech Protective Masks.http://emag.medicalexpo.com/covid-19-development-of-high-tech-protective-masks/ [Online]. Available: [Google Scholar]
- 38.Guo Y., Cao Q., Hong Z., Tan Y., Chen S., Jin H., Tan K., Wang D., Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-An update on status. Military Medical Research. 2020;7(1):1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banerjee S., Burbine S., Shivaprakash N., Mead J. 3D-Printable PP/SEBS thermoplastic elastomeric blends: preparation and properties. Polymers. 2019;11(2) doi: 10.3390/polym11020347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bachtiar E., Erol O., Millrod M., Tao R., Gracias D., Romer L., Kang S. 3D printing and characterization of a soft and biostable elastomer with high flexibility and strength for biomedical applications. Journal for the Mechanical Behaviour of Biomaterials. 2020;104 doi: 10.1016/j.jmbbm.2020.103649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grammatis K. RAISE3D; 13 April 2020. How to Make a 3D Printed Mask during the COVID-19 Pandemic.https://www.raise3d.com/case/how-to-make-a-3d-printed-mask-during-the-covid-19-pandemic/ [Online]. Available: [Google Scholar]
- 42.Zimmerling A., Chen X. Bioprinting for combatting infectious diseases. Bioprinting. 2020;20 doi: 10.1016/j.bprint.2020.e00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kadimisetty K., Song J., Doto A., Hwang Y., Peng J., Mauk M., Bushman F., Gross R., Jarvis J., Liu C. Fully 3D printed integrated reactor array for point-of-care molecular diagnostics. Biosens. Bioelectron. 2018;109:156–163. doi: 10.1016/j.bios.2018.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Formlabs . Formlabs; 2020. Prototyping Rapid Diagnostics for COVID-19 with 3D Printing.https://formlabs.com/covid-19-response/covid-19-rapid-diagnostics/ [Online]. Available: [Google Scholar]
- 45.Peters J. The Verge; 17 March 2020. Volunteers Produce 3D-Printed Valves for Life-Saving Coronavirus Treatments.https://www.theverge.com/2020/3/17/21184308/coronavirus-italy-medical-3d-print-valves-treatments [Online]. Available: [Google Scholar]
- 46.Welle Deutche. DW; 21 March 2020. Volkswagen Explores Using 3D Printers to Produce Ventilators.https://www.dw.com/en/volkswagen-explores-using-3d-printers-to-produce-ventilators/a-52867155 [Online]. Available: [Google Scholar]
- 47.Government of Canada . Government of Canada; 18 April 2020. 3D Printing and Other Manufacturing of Personal Protective Equipment in Response to COVID-19.https://www.canada.ca/en/health-canada/services/drugs-health-products/medical-devices/covid-19-unconventional-manufacturing-personal-protective-equipment.html [Online]. Available: [Google Scholar]
- 48.Livingston E., Desai A., Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. Neonatology. 2019;115(2):116–126. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- 49.Government of Canada . Government of Canada; 24 July 2020. Non-medical Masks and Face Coverings: about.https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/about-non-medical-masks-face-coverings.html [Online]. Available: [Google Scholar]
- 50.Cohen J. Science; 27 March 2020. Not Wearing Masks to Protect against Coronavirus Is a 'big Mistake', Top Chinese Scientist Says.https://www.sciencemag.org/news/2020/03/not-wearing-masks-protect-against-coronavirus-big-mistake-top-chinese-scientist-says [Online]. Available: [Google Scholar]
- 51.Whelan K. Medical Expo; 12 March 2020. 3D Printed Face Masks for Mass Screening.http://emag.medicalexpo.com/covid-19-3d-printed-face-masks-for-mass-screening/ [Online]. Available: [Google Scholar]
- 52.Saltmarsh A. Medical Expo; 25 May 2020. Disinfection Robots against COVID-19.http://emag.medicalexpo.com/disinfection-robots-against-covid-19/ [Online]. Available: [Google Scholar]
- 53.Boston Children's Hospital; Harvard Medical School . COVID-19 Our Response to the N95 Shortage. Boston Children's Hospital; 20 March 2020. http://www.childrenshospital.org/research/departments-divisions-programs/departments/surgery/surgical-innovation-fellowship [Online]. Available: [Google Scholar]
- 54.Luan P., Ching C. A reusable mask for coronavirus disease 2019 (COVID-19) Arch. Med. Res. 2020;51 doi: 10.1016/j.arcmed.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bioengineering . Stanford; 2020. Pneumask: Reusable Full-Face Snorkel Mask PPE Project.https://bioengineering.stanford.edu/pneumask-reusable-full-face-snorkel-mask-ppe-project [Online]. Available: [Google Scholar]
- 56.McMillan A. Global News; 21 April 2020. University of Saskatchewan Developing 3D-Printed Masks to Supplement N95s.https://globalnews.ca/news/6850021/usask-3d-printed-masks-n95-coronavirus/ [Online]. Available: [Google Scholar]
- 57.ViriMASK . ViriMASK; 2020. Coronavirus Protective Oculo-Respirator.https://www.virimask.com/ [Online]. Available: [Google Scholar]
- 58.Cramer A., Tian E., Yu S., Galanek M., Lamere E., Li J., Gupta R., Short M. medRxiv; 2020. Disposable N95 Masks Pass Qualitative Fit-Test but Have Decreased Filtration Efficiency after Cobalt-60 Gamma Irradiation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carrillo I., Floyd A., Valverde C., Tingle T., Zabaneh F. Immediate-use steam sterilization sterilizes N95 masks without mask damage. Infect. Control Hosp. Epidemiol. 2020 doi: 10.1017/ice.2020.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O'Hearn K., Gertsman S., Sampson M., Webster R., Tsampalieros A., Ng R., Gibson J., Lobos A., Acharya N., Agarwal A., Boggs S., Chamberlain G., Staykov E., Sikora L., McNally J. OSF; 2020. Decontaminating N95 and SN95 masks with Ultraviolet Germicidal Irradiation (UVGI) does not impair mask efficacy and safety: a Systemic Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hill E., Crockett C., Circh R., Lansville F., Stahei P. Introducing the "Corona Curtain": an innovative technique to prevent airborne COVID-19 exposure during emergent intubations. Patient Saf. Surg. 2020;14(22) doi: 10.1186/s13037-020-00247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang H., Fan C., Li M., Nie H., Wang F., Wang H., Wang R., Xia J., Zheng X., Zuo X., Huang J. COVID-19: a call for physical scientists and engineers. ACS Nano. 2020 doi: 10.1021/acsnano.0c02618. [DOI] [PubMed] [Google Scholar]
- 63.Mphaphlee M., Dharmadhikari A., Jensen P., Rudnik S., Reenen T.v., Pagano M., Leuschner W., Sears T., Milonovva S., Walt M.v. d., Stoltz A., Weyer K., Nardell E. Controlled trial of upper room ultraviolet air disinfection: a basis for new dosing guidelines. Am. J. Respir. Crit. Care Med. 2015;192(4):477–484. doi: 10.1164/rccm.201501-0060OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Robots U. Blue Ocean Robotics; 2018. Reduce Hospital Acquired Infections with the UV Disinfection Robot.http://www.uvd-robots.com/ [Online]. Available: [Google Scholar]
- 65.Manganello K. Xenex; 30 April 2020. First UV Disinfection Technology Proven to Deactivate COVID-19.https://xenex.com/resources/news/xenex-lightstrike-robot-destroys-sars-cov-2-coronavirus-in-2-minutes/ [Online]. Available: [Google Scholar]
- 66.Ringenberg K., Fremming B., Lisco S., Schule T. Protection of anesthesia providers from silent carriers of COVID-19 while minimizing disposable PPE utilization. J. Clin. Anesth. 2020 doi: 10.1016/j.jclinane.2020.109930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Flaxman S., Mishra S., Gandy A., Unwin J., Mellan T., Coupland H., Whittaker C., Zhu H., Berah T., Eaton J., Monod M., Ghani A., Donnelly C., Riley S., Vollmer M., Ferguson N., Okell L., Bhatt S. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020 doi: 10.1038/s41586-020-2405-7. http://www.ncbi.nlm.nih.gov/pubmed/32512579 [DOI] [PubMed] [Google Scholar]
- 68.Kumar A., Patel D., Nissen S., Desai M. Never let a crisis go to waste: implementing virtual innovations during the COVID-19 pandemic for a better tomorrow in healthcare. JACC (J. Am. Coll. Cardiol.): Case Reports. 2020 doi: 10.1016/j.jaccas.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ohannessian R., Duong T., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health and Surveillance. 2020;6(2) doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hutson M. Artificial-intelligence tools aim to tame the coronavirus literature. Nature. 09 June 2020 doi: 10.1038/d41586-020-01733-7. https://www.nature.com/articles/d41586-020-01733-7?utm_source=Nature+Briefing&utm_campaign=691b293313-briefing-dy-20200612&utm_medium=email&utm_term=0_c9dfd39373-691b293313-45410078 [Online]. Available: [DOI] [PubMed] [Google Scholar]
- 71.Morley J., Cowls J., Taddeo M., Floridi L. Ethical guidelines for COVID-19 tracing apps. Nature. 28 May 2020 doi: 10.1038/d41586-020-01578-0. https://www.nature.com/articles/d41586-020-01578-0?utm_source=Nature+Briefing&utm_campaign=82c4c90298-briefing-dy-20200528&utm_medium=email&utm_term=0_c9dfd39373-82c4c90298-45410078 [Online]. Available: [DOI] [PubMed] [Google Scholar]
- 72.Amer P. Coronavirus conversations: science communication during a pandemic. Nature. 27 May 2020 doi: 10.1038/d41586-020-01589-x. https://www.nature.com/articles/d41586-020-01589-x?utm_source=Nature+Briefing&utm_campaign=82c4c90298-briefing-dy-20200528&utm_medium=email&utm_term=0_c9dfd39373-82c4c90298-45410078 [Online]. Available: [DOI] [PubMed] [Google Scholar]
- 73.Ball P., Maxmen A. The epic battle against coronavirus minsinformation and conspiracy theories. Nature. 27 May 2020 doi: 10.1038/d41586-020-01452-z. https://www.nature.com/articles/d41586-020-01452-z?utm_source=Nature+Briefing&utm_campaign=e78775970c-briefing-dy-20200526_COPY_01&utm_medium=email&utm_term=0_c9dfd39373-e78775970c-45410078 [Online]. Available: [DOI] [PubMed] [Google Scholar]
- 74.Javaid M., Haleem A. Industry 4.0 applications in medical field: a brief review. Current Medicine Research and Practice. 2019;9(3):102–109. doi: 10.1016/j.cmrp.2019.04.001. [DOI] [Google Scholar]
- 75.Lee T. Creating the new normal: the clinician response to COVID-19. NEJM Catalyst. 2020:19–21. doi: 10.1056/CAT.20.0076. [DOI] [Google Scholar]
- 76.Barney A., Buckelew S., Mesheriakova V., Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J. Adolesc. Health. 2020;(January) doi: 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Centers for Medicare and Medicaid Services . Medicaid.gov; 2020. Telemedicine.https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html [Online]. Available: [Google Scholar]
- 78.Greenhalgh T., Wherton J., Shaw S., Morrision C. Video consultation for covid-19. The BMJ. 2020;368(March) doi: 10.1136/bmj.m998. [DOI] [PubMed] [Google Scholar]
- 79.Hollander J., Carr B. Virtually perfect? Telemedicine for covid-19. N. Engl. J. Med. 2020;382(18):1677–1679. doi: 10.1056/nejmp2003539. [DOI] [PubMed] [Google Scholar]
- 80.Goel S., Greenbaum A., Patel A., Little S., Parikh R., Ballmoos M.W.v., Lumsden A., Reardon M., Kleiman N. Role of teleproctoring in challenging and innovative structural interventions amidst the COVID-19 pandemic and beyond. JACC Cardiovasc. Interv. 2020 doi: 10.1016/j.jcin.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rosser J., Gabriel N., Herman B., Murayama M. Telementoring and teleproctoring. World J. Surg. 2001;25(11):1438–1448. doi: 10.1007/s00268-001-0129-X. [DOI] [PubMed] [Google Scholar]
- 82.Samuels E., Clark A., Wunsch C., Keeler L., Reddy N., Vanjani R., Wightman R. Innovation during COVID-19: improving addiction treatment access. J. Addiction Med. 2020 doi: 10.1097/adm.0000000000000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Xiang Y., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou X., Snoswell C., Harding L., Bombling M., Edrippulige S., Bai X., Smith A. The role of telehealth in reducing the mental health burden from COVID-19. Telemedicine and e-Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 85.Davis C., Hg K., Oh J., Baeg A., Rajasegaran K., Chew C. Society for Adolescent Health and Medicine; 2020. Caring for Children and Adolescents with Eating Disorders in the Current Coronvirus 19 Pandemic: A Singapore Perspective. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C., Susser E., Lu J., Hoven C. The psychological imact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liu S., Yang L., Zhang C., Xiang Y., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020;7(4):17–18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dialani P. Analystics Insight; 2 April 2020. How Virtual Reality Is Helping to Deal with COVID-19.https://www.analyticsinsight.net/virtual-reality-helping-deal-covid-19/ [Online]. Available: [Google Scholar]
- 89.DVEholographics . Cision; 17 March 2020. New Holographic Virtual Events Will Reach Millions amid Coronavirus (COVID-19) Crisis.https://www.prnewswire.com/news-releases/new-holographic-virtual-events-will-reach-millions-amid-coronavirus-covid-19-crisis-301025496.html [Online]. Available: [Google Scholar]
- 90.Ienca M., Vayena E. On the responsible use of digital data to tackle the COVID-19 pandemic. Nat. Med. 2020;26(4):463–464. doi: 10.1038/s41591-020-0832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bean R. Forbes; 30 March 2020. Big Data in the Time of Coronavirus (COVID-19)https://www.forbes.com/sites/ciocentral/2020/03/30/big-data-in-the-time-of-coronavirus-covid-19/#2a2b871c58fc [Online]. Available: [Google Scholar]
- 92.He S. Immunology and Microbiology; 12 March 2020. Using the Internet of Things to Fight Virus Outbreaks.https://www.technologynetworks.com/immunology/articles/using-the-internet-of-things-to-fight-virus-outbreaks-331992 [Online]. Available: [Google Scholar]
- 93.Danquah L., Hasham N., MacFarlane M., Conteh F., Momoh F., Tedesco A., Jambai A., Ross D., Weiss H. Use of a mobile application for Ebola contact tracing and monitoring in northern Sierra Leone: a proof-of-concept study. BMC Infect. Dis. 2019;19(1) doi: 10.1186/s12879-019-4354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Karimuribo E., Mutagahywa E., Sindato C., Mboera L., Mwabukusi M., Njenga K., Teesdale S., Olsen J., Rweyemamu M. A smartphone app (AfyaData) for innovative one health disease surveillance from community to national levels in africa: intervention in disease surveillance. JMIR Public Health and Surveillance. 2017;3(4) doi: 10.2196/publichealth.7373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Judson T., Odisho A., Neinstein A., Chao J., Williams A., Miller C., Moriarty T., Gleason N., Intinarelli G., Gonzales R. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J. Am. Med. Inf. Assoc. 2020 doi: 10.1093/jamia/ocaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wood C., Thomas M., Budd J., Mashamba-Thompson T., Herbst K., Pillay D., Peeling R., Johnson A., McKendry R., Stevens M. Taking connected mobile-health diagnostic of infectious diseases to the field. Nature. 2019;566(7745):467–474. doi: 10.1021/acsnano.0c02624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.ZOE . Massachusetts General Hospital; ZOE; King's College of London; 2020. COVID Symptom Study.https://covid.joinzoe.com/us [Online]. Available: [Google Scholar]
- 98.Crook J. Verizon; 11 December 2014. Kinsa Raises $9.6M Series A for A Smart Thermometer that Tracks the Spread of Illness.https://techcrunch.com/2014/12/11/kinsa-raises-9-6m-series-a-for-a-smart-thermometer-that-tracks-the-spread-of-illness/ [Online]. Available: [Google Scholar]
- 99.Print R.S.S. Med-Tech innovation; 2 April 2020. Patch for Detection and Monitoring of COVID-19 Symptoms Fast-Tracked.https://www.med-technews.com/news/patch-for-detection-and-monitoring-of-covid-19-testing-fast-/ [Online]. Available: [Google Scholar]
- 100.Government of Singapore . Government of Singapore; 1 June 2020. TraceTogether, Safer Together.https://www.tracetogether.gov.sg/ [Online]. Available: [Google Scholar]
- 101.Charlton J. CTV News; 16 May 2020. Why Contact Tracing Is 'a Skill and an Art' in the Fight against COVID-19.https://saskatoon.ctvnews.ca/why-contact-tracing-is-a-skill-and-an-art-in-the-fight-against-covid-19-1.4942564 [Online]. Available: [Google Scholar]
- 102.Dove N. Global News; 23 April 2020. Saskatchewan Health Ministry Assessing Tech-Based Coronavirus Tracing.https://globalnews.ca/news/6856282/saskatchewan-health-ministry-tech-based-coronavirus-tracing/ [Online]. Available: [Google Scholar]
- 103.Topol E. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 2019;25(1):44–56. doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 104.Naude W. vol. 13110. IZA DP; 2020. Artificial Intelligence against COVID-19: an Early Review. [Google Scholar]
- 105.Petropoulos G. bruegel; 23 March 2020. Artificial Intelligence in the Fight against COVD-19.https://www.bruegel.org/2020/03/artificial-intelligence-in-the-fight-against-covid-19/ [Online]. Available: [Google Scholar]
- 106.Al-Karawi D., Al-Zaidi S., Polus N., Jassim S. MedRxiv; 2020. AI Based Chest X-Ray (CXR) Scan Texture Analysis Algorithm for Digital Test of COVID-19 Patients. [DOI] [Google Scholar]
- 107.Abbas A., Abdelsamea M., Gaber M. medRxiv; 2020. Classification of COVID-19 in Chest X-Ray Images Using DeTraC Deep Convolutional Neural Networks.http://arxiv.org/abs/2003.13815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Li L., Qin L., Xu Z., Yin Y., Wang X., Kong B., Bai J., Lu Y., Fang Z., Song Q., Cao K., Liu D., Wang G., Xu Q., Fang X., Zhang S., Xia J., Xia J. Applied Intelligence; 2020. Artificial Intelligence Distinguishes COVID-19 from Community Acquired Pneumonia on Chest CT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shi F., Wang J., Shi J., Wu Z., Wang Q., Tang Z., He K., Shi Y., Shen D. Review of artifical intelligence techniques in imaging data acquisition, segmentation and diagnosis for COVID-19. IEEE Reviews in Biomedical Engineering. 2020 doi: 10.1109/RBME.2020.2987975. [DOI] [PubMed] [Google Scholar]
- 110.Yan L., Zhang H., Xiao Y., Wang M., Guo Y., Sn C., Tang X., Jing L., Li S., Zhang M., Xiao Y., Cao H., Chen Y., Ren T., Jin J., Wang F., Xiao Y., Huang S., Tan X., Huang N., Jiao B., Zhang Y., Luo A., Cao Z., Xu H., Yuan Y. medRxiv; 2020. Prediction of Criticality in Patients with Severe Covid-19 Infection Using Three Clinical Features: a Machine Learning-Based Prognostic Model with Clinical Data in Wuhan. [DOI] [Google Scholar]
- 111.Nagaratnam K., Harston G., Flossmann E., Canavan C., Geraldes R., Edwards C. Innovative use of artificial intelligence and digital communication in acute stroke pathway in response to COVID-19. Future Healthcare Journal. 2020;7(2) doi: 10.7861/fhj.2020-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yang Z., Zeng Z., Wang K., Wong S., Liang W., Zanin M., Liu P., Cao X., Mai Z., Liang J., Liu X., Li S., Li Y., Ye F., Guan W., Yang Y., Li F., Luo S., Xie Y., Liu B., Wang Z., Zhang S., Wang Y., Zhong N., He J. Modified SEIR and AI prediction of the epidemic trend of COVID-19 in China under public health interventions. J. Thorac. Dis. 2020;12(3):165–174. doi: 10.21037/jtd.2020.02.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hutson M. Artificial-intelligence tools aim to tame the coronavirus literature. Nature. 09 June 2020 doi: 10.1038/d41586-020-01733-7. https://www.nature.com/articles/d41586-020-01733-7?utm_source=Nature+Briefing&utm_campaign=691b293313-briefing-dy-20200612&utm_medium=email&utm_term=0_c9dfd39373-691b293313-45410078 [Online]. Available: [DOI] [PubMed] [Google Scholar]
- 114.Silberg J., Manyika J. McKinsey Global Institute; 2019. Notes from the AI Frontier; Tackling Bias in AI (And in Humans) [Google Scholar]
- 115.Skowronski D., Petric M., Daly P., Parker R., Bryce E., Doyle P., Noble M., Roscoe D., Tomblin J., Yang T., Krajden M., Patrick D., Pourbohloul B., Goh S., Bowie W., Booth T., Tweed A., Perry T., McGeer A., Brunham R. Coordinated response to SARS, vancouver, Canada. Emerg. Infect. Dis. 2006;12(1):155–158. doi: 10.3201/eid1201.050327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wong J., Leo Y., Tan C. COVID-19 in Singapore- current experience critical global issues that require attention and action. J. Am. Med. Assoc. 2020;323(13):1243–1244. doi: 10.1001/jama.2020.2467. [DOI] [PubMed] [Google Scholar]
- 117.Smith R. Responding to global infectious disease outbreaks: lessons for SARS on the role of risk perception, communication and management. Soc. Sci. Med. 2006;63(12):3113–3123. doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hao K. MIT Technology Review; 16 March 2020. Over 24, 000 Coronavirus Research Papers Are Now Available in One Place.https://www.technologyreview.com/2020/03/16/905290/coronavirus-24000-research-papers-available-open-data/ [Online]. Available: [Google Scholar]
- 119.Herrera V., Finkler N., Vincent J. Innovation and transformations in the response to COVID-19: seven areas where clinicians need to lead. NEJM Catalyst. 2020 doi: 10.1056/CAT.20.0087. [DOI] [Google Scholar]
- 120.Ioannidis J. Coronavirus disease 2019: the harms of exaggerated information and non-evidence-based measures. Eur. J. Clin. Invest. 2020;50(4) doi: 10.1111/eci.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hopkins University John. John Hopkins University; 3 June 2020. COVID-19 Map.https://coronavirus.jhu.edu/map.html [Online]. Available: [Google Scholar]
- 122.Nextstrain . Nextstrain; 19 June 2020. Genomic Epidemiology of Novel Coronavirus- Global Subsampling.https://nextstrain.org/ncov/global?utm_campaign=b131faec51-briefing-dy-20200507&utm_medium=email&utm_source=Nature%20Briefing&utm_term=0_c9dfd39373-b131faec51-45243722 [Online]. Available: [Google Scholar]
- 123.Government of Saskatchewan . Government of Saskatchewan; 19 June 2020. Cases and Risk of COVID-19 in Saskatchewan.https://www.saskatchewan.ca/government/health-care-administration-and-provider-resources/treatment-procedures-and-guidelines/emerging-public-health-issues/2019-novel-coronavirus/cases-and-risk-of-covid-19-in-saskatchewan [Online]. Available: [Google Scholar]
- 124.Saskatchewan Health Authority . Saskatchewan Health Authority; 26 May 2020. Opening Communication Doors for Those with Hearing Impairments.https://www.saskhealthauthority.ca/news/stories/Pages/2020/May/Opening-communication-doors-for-those-with-hearing-impairments.aspx [Online]. Available: [Google Scholar]
- 125.Morgan S. World Intellectual Property Review; 23 March 2020. UK Man Charged with Selling Counterfeit COVID-19 Kits.https://www.worldipreview.com/news/uk-man-charged-with-selling-counterfeit-covid-19-kits-19466 [Online]. Available: [Google Scholar]
- 126.Kennedy J. The Conversation; 26 March 2020. Buyer Beware: Counterfeit Markets Can Flourish during a Public Health Crisis.https://theconversation.com/buyer-beware-counterfeit-markets-can-flourish-during-a-public-health-crisis-134492 [Online]. Available: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.