Abstract
Initial reports suggest that mental health problems were elevated early in the COVID-19 pandemic. However, few studies have followed-up participants as the pandemic evolved and examined both between and within person predictors of symptom trajectories. In the current study, adolescents and young adults (N=532) in New York were surveyed monthly between March 27th and July 14th, 2020, a period spanning the first peak and subsequent decline in COVID-19 infection rates in the region. Surveys assessed symptoms of depression and anxiety using the Child Depression Inventory and the Screen for Child Anxiety Related Disorders, as well as experiences related to the pandemic. Multilevel growth modeling indicated that symptoms of depression and anxiety peaked around late April/early May and then decreased through May-July. Some pandemic experiences followed a similar quadratic trajectory, while others decreased linearly across the study. Specific relationships emerged between some types of pandemic experiences and depression and anxiety symptoms. While symptoms of depression and anxiety in youth may have been elevated early in the pandemic, these findings suggest they subsided across Spring-Summer of 2020, with higher levels of both corresponding to a period of peak infection rates and decreases paralleling the decline in pandemic experiences and COVID-19 infection rates.
Keywords: COVID-19, Adolescents, Young adults, Mental health, Depression, Anxiety
1. Introduction
On March 11th 2020, the World Health Organization declared that the escalating novel coronavirus (COVID-19) outbreak had reached the level of pandemic (World Health Organization, 2020), heralding a period of drastic change in the lives of individuals across the globe. The COVID-19 pandemic brought widespread stressors including job loss, restricted activity and social interaction, and substantial changes to the structure of work and education, prompting many to worry about an accompanying mental health crisis (Gruber et al., 2020). Research from early in the pandemic mostly confirmed these fears, finding elevated rates of depression and anxiety, primarily in Asian and European samples (Torales et al., 2020; Vindegaard and Benros, 2020) where the virus first spread, with a few recent reports from the U.S. (Ettman et al., 2020; Holman et al., 2020; Twenge and Joiner, 2020). However, it is unclear whether depression and anxiety remained elevated in the months after the start of the pandemic as this unprecedented crisis evolved.
A small handful of studies have employed longitudinal cohort designs to explore within-person changes in mental health symptoms during the pandemic. Among these, results have been mixed, with some studies showing increases (Gopal et al., 2020; Planchuelo-Gómez et al., 2020; Salfi et al., 2020), some showing decreases (Zhou et al., 2020) and some showing no change (Probst et al., 2020). These inconsistencies are likely due to a number of factors, including differences in the timing of assessment relative to the timeline of the pandemic and shut-down measures, and regional differences in the severity and containment of the COVID-19 outbreak. Just one of these studies was conducted in the U.S., which has led the world in COVID-19 cases and deaths since late March 2020 (McNeil Jr., 2020). Across 3 assessments of a national sample from April 20th to May 22nd, Zhou et al. (2020) found that symptoms of depression and anxiety were higher at later compared to earlier assessment waves. It is unclear how these changes correspond to the timeline of the pandemic, however, as the timing and extent of COVID-19 infection and public response has varied widely across regions within the U.S.
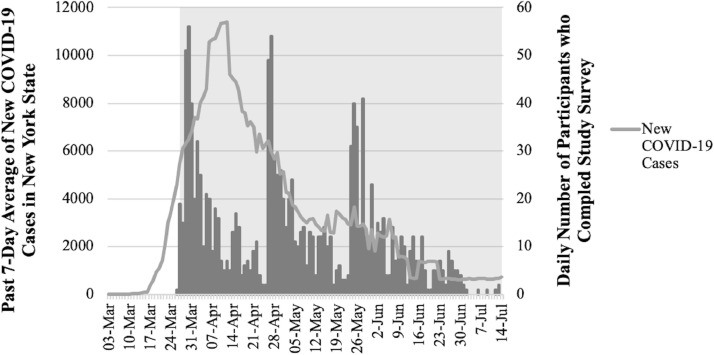
New York State, and particularly New York City and adjacent Long Island, was the first U.S. region to see a dramatic spike in COVID-19 infection. New onset cases escalated sharply through the end of March and early April, with aggressive confinement measures (e.g., shelter-in-place order, mandated wearing of masks in public) leading to a decline in new cases through the end of Spring into early Summer 2020 (Centers for Disease Control, 2020). The current study explores changes in depression and anxiety symptoms in a sample of adolescents and young adults (primarily high school and college students) from Long Island across this critical period in the region (see Fig. 1 , which displays the timing of study participation relative to COVID-19 infection in New York state). Youth may be particularly vulnerable to the disruptions associated with the COVID-19 pandemic, as most have had to abruptly adjust to online learning, many college students had to leave campus and move back home with family, and social interaction was restricted during this critical time of social development (Loades et al., 2020). Further, a few cross-sectional studies have found that younger age is associated with worse mental health during the pandemic (Huang and Zhao, 2020; Wang et al., 2020).
Fig. 1.
Past 7-day averages of new COVID-19 cases in New York State between March 3rd and July 14th, 2020 (left y-axis, light grey line), and number of participants who completed the COVID-19 assessment (right y-axis, dark gray bars). The shaded region shows the dates (April 27th, 2020 and July 14th, 2020) during which participants completed the study surveys. All COVID-19 statistics were obtained daily from the Centers for Disease Control and Prevention COVID-19 Data Tracker (https://covid.cdc.gov/covid-data-tracker/#trends_dailytrends).
Participants in two ongoing longitudinal studies completed up to 3 monthly surveys assessing symptoms of depression and anxiety, along with various experiences related to the pandemic (e.g., life changes, school problems, concern about infection). Surveys were completed between March 27th and July 14th, 2020. We used multilevel growth modeling to capture the trajectory of symptoms and pandemic experiences across Spring-Summer 2020. We then explored predictors of depression and anxiety symptoms across the study period, including age, sex, symptoms of depression and anxiety before the pandemic and both between and within-person effects of pandemic experiences.
2. Methods
2.1. Participants
The sample included 532 adolescents and young adults who participated in one of two longitudinal investigations at Stony Brook University.
2.1.1. Stony brook temperament study (SBTS)
The SBTS is an ongoing longitudinal study designed to explore early antecedents and pathways to depressive and anxiety disorders in a community-based sample of youth from Long Island, New York. Families with a 3-year-old child were contacted through commercial mailing lists and were eligible to participate if the primary caretaker spoke English and was the child's biological parent, and if the child did not have a significant medical disorder or developmental disability. Following the age 3 assessment, families were invited to participate in follow-up assessments when their child was approximately age 6, 9, 12, 15, and 18. Greater detail on the SBTS can be found elsewhere (Klein and Finsaas, 2017). Pre-pandemic symptom scores used as covariates in the current study were taken from the 5th wave of data collection (age 15; n = 450, 73.9% baseline sample; July 2016-2019).
2.2.2. Impact of puberty on affect and neural development across adolescence (iPANDA) project
The iPANDA project is an ongoing, multi-method, longitudinal study aimed at investigating within-subject trajectories of reward sensitivity and depressive symptoms in a large community sample of adolescent girls from Long Island, New York (Burani et al., 2019). Participants were initially recruited using commercial mailing lists, posted flyers, online postings, and word of mouth. Families were eligible to participate if they had a daughter between the ages of 8-14 with no known medical or developmental disability, a biological parent willing to participate, and the ability to read and write English. Following the first (i.e., baseline) wave of data collection (ages 8-14), participants were reassessed at two-year intervals (i.e., ages 10-16 for the second wave and 12-18 for the third wave). Pre-pandemic symptom scores used as covariates in the current study were taken from the second wave of data collection (ages 10-16; n = 263, 83% of the baseline sample; November 2014-August 2017).
2.2. Procedures
All participants in the SBTS and iPANDA project were invited to participate in the current study. Participants were sent three surveys, monthly, via email between late March and mid-June 2020. The three surveys consisted of a battery of questionnaires assessing experiences related to the COVID-19 pandemic and symptoms of depression and anxiety. Participants had approximately one month to complete each survey and received periodic reminders until they completed the survey or it expired. Most participants completed the first survey between March 31st and April 15th (median date = April 4th, range = March 27th – May 15th), the second survey between April 29th and May 14th (median date = May 5th, range = April 27th - June 30th) and the third survey between May 29th and June 14th (median date = June 3rd, range = May 25th – July 14th). The entire study period spanned March 27th to July 14th, 2020.
Written informed consent was obtained from individuals 18-years-old or older prior to completing the first survey. Parents provided consent for participants under the age of 18 prior to contacting the minor directly, who then provided assent before completing the first survey. Study procedures were approved by the Stony Brook University Institutional Review Board.
2.3. Measures
2.3.1. Psychopathology symptoms
Children's Depression Inventory (CDI). The CDI is a 27-item self-report questionnaire designed to assess symptoms of depression occurring in the past 2 weeks in youth ages 7-17 (Kovacs, 1992). Although many of our participants are over the age of 17, we used the CDI to maintain continuity across participants and with prior waves of assessment. Items are rated on a 3-point scale and summed to create a total symptom severity score. Adequate reliability and validity of the CDI has been demonstrated (Dougherty et al., 2018). Additionally, treatment studies have demonstrated that the CDI is sensitive to change across a 2-3 month time period (e.g.,Weisz et al., 1997). In our sample, the CDI possessed excellent internal consistency (α = .90-.91, surveys 1-3).
Screen for Child Anxiety Related Disorders (SCARED). The SCARED is a 41-item inventory designed to measure symptoms of anxiety over the past month in youth aged 8-18 (Birmaher et al., 1997). Participants rate the frequency of anxiety symptoms from almost never (0) to often (2). The SCARED is composed of 5 subscales capturing different clusters of anxiety symptoms that can be summed to create a total anxiety score. In the current study, we focused exclusively on the total score. Similar to the CDI, we used a youth measure of anxiety to maintain continuity across participants and with prior waves of assessment. However, the school phobia subscale was excluded because it was not relevant for the older participants, so the total anxiety score was based on the 37-items from the remaining subscales. The SCARED has demonstrated adequate psychometric properties (Rappaport et al., 2017) and has been shown to be sensitive to change over a 2-3 month period (e.g., Muris et al., 2009). Internal consistency in our sample was excellent (a = .94-.95, surveys 1-3)
2.3.2. Pandemic experiences
We created a survey for the COVID-19 study to capture experiences related to the pandemic, drawing on measures developed to assess the impact of prior natural and man-made disasters on everyday life (e.g., for Hurricane Ike and Hurricane Katrina; Goldmann and Galea, 2014; Norris et al., 2010) and personal accounts reported in local and national news. Twenty-six items were combined to create 5 composites capturing different domains of experience related to the pandemic. The life changes composite included a checklist of 14 changes in life circumstances related to the pandemic (e.g., job moved online, forced to change where you live). Scores ranged from 0-11 (M=3.38, SD=1.67). The infection concerns composite included 2 items probing concern about and perceived likelihood of becoming infected with COVID-19, rated on a Likert-scale from 0 (not at all) to 4 (extremely). Scores ranged from 0-8 (M=2.75, SD=1.49; Cronbach's alpha = .62) The school concerns composite included a checklist of 4 school-related concerns (e.g., online classes being lower quality). Scores ranged from 0-4 (M=1.10, SD=1.09; Cronbach's alpha = .76). The home confinement concerns composite included a checklist of 3 concerns related to being largely restricted to home (e.g., experiencing “cabin fever”). Scores ranged from 0-3 (M=1.23, SD=0.93; Cronbach's alpha = .73). Finally, the basic needs concerns subscale included a checklist of 3 concerns related to having one's basic needs met (e.g., not having enough food or supplies). Scores ranged from 0-3 (M=0.47, SD=0.72; Cronbach's alpha = .71).
2.4. Data analysis
We conducted multilevel growth modeling to assess change in depression, anxiety and pandemic experiences across late March to mid-July 2020. Multilevel growth models combine fixed effects (single population parameter), random effects (variability around that parameter), and time trends to capture inter-individual variability in intra-individual patterns of change (Curran et al., 2010). In the current study, Time was coded as weeks since April 1st, 2020, centering time around this date. This date was chosen as it was an easy reference point for evaluating change across the calendar months, was a significant period of escalation in COVID-19 infection in this region (see Fig. 1), and is near the median date on which the first survey was completed. Convergence issues can arise when observed variances are very large, as was the case for models with Time coded in weeks. Muthén and Muthén (2017) recommend keeping sample variance values within 1-10. Thus, Time was scaled down by dividing the “weeks” value by 4, so that a 1-unit change in Time represented expected change in a 4-week or approximately 1-month period, while preserving differences at the week level (i.e., a 0.25-unit change in Time is equal to 1 week).
First, we fit a series of unconditional growth models to establish the average trajectories of depression and anxiety symptoms and the 5 pandemic experiences composites. For each outcome, we started with a baseline random intercept only model (model 0) to calculate intraclass correlations coefficients (ICC)1 1 and saved model fit information for comparisons to more complex models. In the next model (model 1), we added a fixed slope effect representing the average rate of linear change in the outcome across the study. Then we added a random slope effect (model 2) to capture individual variability in the rate of linear change and estimated covariance between the random intercept and slope. In the final model (model 3), we added a fixed curve effect to capture quadratic change in the outcome. Models with random curve effects were not identified for our data.
We used the following criteria to determine which growth model best captured the trajectory of each outcome. First, we conducted likelihood ratio tests (LRT) to compare the fit of nested models (model 0 is nested within model 1, which is nested within model 2, which is nested within model 3). A significant LRT indicates that the added effect improves model fit over the less complex model. Next, we considered whether the added effect was statistically significant. The most complex model that met these criteria was selected as the best-fitting model.
To identify factors that impacted the trajectories of depression and anxiety, we fit conditional growth models of the two symptom scores, adding predictors to the best fitting unconditional growth model. To separate within- and between-person effects of the pandemic experience composites, we included both a person-mean centered version of the composites (i.e., subtracting each person's average composite score from their score at each wave) as a level one, time-varying predictor and the person means of the composites as level two, time invariant predictors. This allowed us to examine both the impact of reporting greater pandemic experiences at a given time-point relative to one's average levels and of reporting greater pandemic experiences on average relative to other individuals across spring-summer (Curran and Bauer, 2011). We also included age, female sex, and depression and anxiety symptom scores from the prior (pre-pandemic) wave of data collection as level two, time-invariant predictors. In addition, we included interactions of the slope and curve effects with all time-invariant predictors. With the exception of female sex, all time invariant predictors were grand mean centered.
All models were computed with version 1.1-23 of lme4 (Bates et al., 2014) and version 3.1-3 of lmerTest (Kuznetsova et al., 2016) packages for R using Full Information Maximum Likelihood estimation, which produces unbiased estimates (when data are missing at random) using all data available (Enders, 2013), allowing us to include participants who did not complete all 3 surveys.
3. Results
3.1. Sample characteristics
A total of 532 participants (340 and 192 from the SBTS and iPANDA project, respectively) completed at least 1 survey for the COVID study (505 completed the first survey, 432 the second survey, and 402 the third survey; 360 completed all 3 surveys, 88 completed 2 surveys and 84 completed 1 survey). Participants ranged in age from 12-22 years old (M = 17.34, SD = 1.5) and were predominantly female (69%) and in high school (63.7%). Most participants were White/Non-Hispanic (82%), with a college educated parent (62.4%) and were not working at the time of the survey (91.2%). Compared to the SBTS sample, iPANDA participants were older on average, t(530) = 114.67, p < .001, more likely to have a college educated parent, χ2(1) = 11.23, p = .001, and be employed during the study, χ2(1) = 10.75, p < .001, and less likely to be in high school, χ2(1) = 96.60, p < .001. Participants who completed 1, 2 or all 3 surveys for the COVID-19 study did not differ on any demographic variables.
3.2. Unconditional growth models
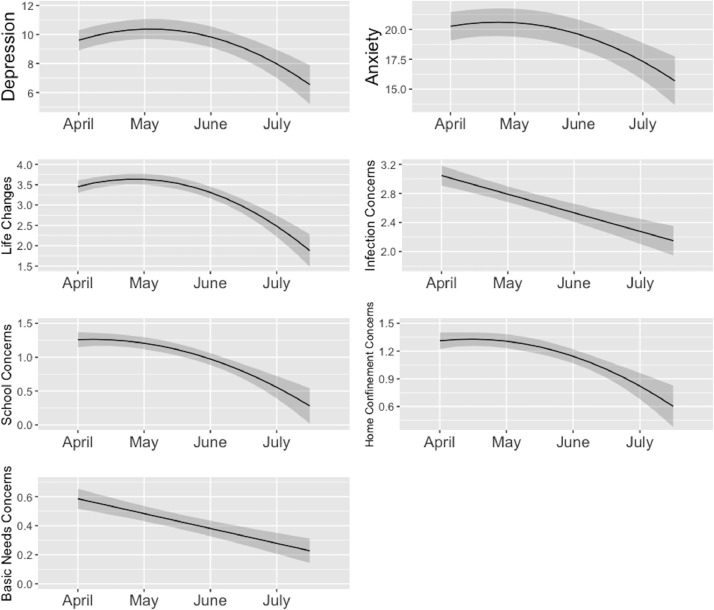
Table 1 displays the results of all unconditional growth models. Fig. 2 displays the model-estimated trajectories for each outcome from the best-fitting model.
Table 1.
Unconditional multilevel growth models of symptoms and pandemic experience composites.
| Outcome | Model | Intercept | Intercept Variance | Time (Slope) | Time (Slope) Variance | Intercept- Slope Correlation | Time (Curvature) | AIC | BIC | Deviance | χ2Diff |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | |||||||||||
| Depression | 1 | 10.04(0.4) | 55.37 | -0.19(0.1) | – | – | – | 8192.9 | 8213.6 | 8184.9 | 3.31 |
| ICC = .841 | 2 | 10.07(0.4) | 53.68 | -0.21(0.1) | 1.15* | .06 | – | 8184.5 | 8215.6 | 8172.5 | 12.39* |
| 3 | 9.60(0.4) | 53.34 | 1.43(0.3)* | 1.24* | .09 | -0.66(0.1)* | 8156.4 | 8192.7 | 8142.4 | 30.09* | |
| Anxiety | 1 | 20.67(0.6) | 167.76 | -0.62(0.2)* | – | – | – | 9322.9 | 9343.6 | 9314.9 | 16.32* |
| ICC = .887 | 2 | 20.71(0.6) | 162.92 | -0.64(0.2)* | 2.86* | .05 | – | 9311.6 | 9342.7 | 9299.6 | 15.33* |
| 3 | 20.26(0.6) | 162.58 | 0.96(0.5)* | 3.12* | .06 | -0.64(0.2)* | 9299.4 | 9335.7 | 9285.4 | 14.15* | |
| Pandemic Experiences | |||||||||||
| Life Changes | 1 | 3.63(0.1) | 1.54 | -0.20(0.0)* | – | – | – | 4839.3 | 4860.1 | 4831.3 | 31.32* |
| ICC = .536 | 2 | 3.63(0.1) | 1.56 | -0.20(0.0)* | 0.11* | -.14 | – | 4836.0 | 4867.2 | 4824.0 | 7.23* |
| 3 | 3.45(0.1) | 1.61 | 0.43(0.1)* | 0.15* | -.19 | -0.25(0.0)* | 4799.6 | 4836.0 | 4785.6 | 38.44* | |
| Infection Concerns | 1 | 3.04(0.1) | 1.11 | -0.26(0.0)* | – | – | – | 4509.2 | 4529.9 | 4501.2 | 56.28* |
| ICC = .473 | 2 | 3.05(0.1) | 1.53 | -0.26(0.0)* | 0.22* | -.49* | – | 4490.2 | 4521.3 | 4478.2 | 22.95* |
| 3 | 3.05(0.1) | 1.53 | -0.28(0.1)* | 0.22* | -.49* | 0.01(0.0) | 4492.1 | 4528.4 | 4478.1 | 0.08 | |
| School Concerns | 1 | 1.33(0.0) | 0.58 | -0.20(0.0)8 | – | – | – | 3761.5 | 3782.3 | 3753.5 | 60.49* |
| ICC = .450 | 2 | 1.33(0.1) | 0.93 | -0.19(0.0)* | 0.10* | -.64* | – | 3737.4 | 3768.6 | 3725.4 | 28.15* |
| 3 | 1.26(0.1) | 0.92 | 0.04(0.1) | 0.10* | -.61* | -0.09(0.0)* | 3728.4 | 3764.8 | 3714.4 | 11.00* | |
| Home Confinement Concerns | 1 | 1.37(0.0) | 0.40 | -0.13(0.0)* | – | – | – | 3335.9 | 3356.7 | 3327.9 | 35.46* |
| ICC = .460 | 2 | 1.37(0.0) | 0.47 | -0.13(0.0)* | 0.02 | -.39 | – | 3338.1 | 3369.3 | 3326.1 | 1.81 |
| 3 | 1.31(0.0) | 0.47 | 0.07(0.1) | 0.02 | -.38 | -0.08(0.0)* | 3329.0 | 3365.3 | 3315.0 | 11.11* | |
| Basic Needs Concerns | 1 | 0.59(0.0) | 0.24 | -0.10(0.0)* | – | – | – | 2664.7 | 2685.5 | 2656.7 | 38.78* |
| ICC = .447 | 2 | 0.59(0.0) | 0.37 | -0.10(0.0)* | 0.02* | -.77* | – | 2646.9 | 2678.1 | 2634.9 | 21.78* |
| 3 | 0.60(0.0) | 0.37 | -0.16(0.0)* | 0.02* | -.79* | 0.02(0.0) | 2647.2 | 2683.6 | 2633.2 | 1.76 | |
Note: Model 1 = linear growth model with a fixed slope; Model 2 = linear growth model with a random slope; Model 3 = quadratic growth model with a random slope and fixed curvature; χ2Diff = likelihood ratio test comparing fit of nested models as follows: model 1 is compared to a model with the random intercept as the only predictor (results not shown), model 2 is compared to model 1, model 3 is compared to model 2; Time is coded as months since April 1st, 2020; Acronyms are defined as follows: AIC = Akaike Information Criteria, BIC = Bayesian Information Criteria, ICC = intraclass correlation; Significant time effects and likelihood ratio tests are bolded*.
Fig. 2.
Model-estimated trajectories of symptoms of depression and anxiety and pandemic experiences from April-July 2020.
3.2.1. Psychopathology symptoms
Change in symptoms of depression across the study is best captured by the quadratic model (model 3). The model is characterized by initial linear increase (positive slope effects), t(822) = 4.54, p < .001, with variability in the rate of linear change (95% CI = 0.44-2.13), followed by accelerated decline (negative curve effects), t(818) = -5.56, p < .001. Similar to depression, change in symptoms of anxiety is best captured by the quadratic model, which is characterized by initial linear increase (positive slope effects), t(814) = 42.12, p = .034, with variability in the rate of linear change (95% CI = 1.32-5.11), followed by accelerated decline (negative curve effects), t(809) = -3.80, p < .001. The correlation of the random intercept and slope effect is not significant for either of the best-fitting models, indicating that symptom levels in early April are not associated with the rate of linear change in symptoms across April-July 2020.
3.2.2. Pandemic experiences
The quadratic model also provides the best fit for the Life Changes, School Concerns and Home Confinement Concerns composites. The best-fitting model for Life Changes is characterized by initial linear increase (positive slope effects), t(860) = 3.79, p < .001, with variability in the rate of linear change (95% CI = 0.06-0.32), followed by accelerated decline (negative curve effects), t(850) = -6.05, p < .001. The best-fitting model for School Concerns is characterized by no initial linear change on average (non-significant slope effects), t(879) = 0.54, p = .591, with variability in the rate of linear change (95% CI = 0.05-0.15), followed by accelerated decline (negative curve effects), t(865) = -3.37, p < .001. The best-fitting model for Home Confinement Concerns is characterized by no initial linear change (non-significant slope effects), t(900) = 1.17, p = .241, with no variability in the rate of linear change (95% CI = 0.00-0.05), followed by accelerated decline (negative curve effects), t(859) = -3.35, p < .001. The random intercept-slope correlation is not significant for Life Change or Home Confinement Concerns; however, it is significant for School Concerns (r = -.61, 95% CI = -.72- -.47), indicating that higher levels of School Concerns in early April are associated with steeper linear decreases in School Concerns.
The random linear growth model fit best for Infection Concerns and Basic Needs Concerns. The best-fitting model for Infection Concerns is characterized by linear decline across the study (negative slope effects), t(429) = -6.87, p < .001, with variability in the rate of linear change (slope variance = 0.22; 95% CI = 0.12-0.31). The best-fitting model for Basic Needs Concerns is similarly characterized by linear decline across the study (negative slope effects), t(387) = -6.11, p < .001, with variability in the rate of linear change (slope variance = 0.02; 95% CI = 0.002-0.04). The random intercept-slope correlation is significant for both Infection Concerns (r = -.49, 95% CI = -.62- -.32) and Basic Needs Concerns (r = -.77, 95% CI = -1.00- -.59), indicating that higher levels of Infection and Basic Needs Concerns in early April are associated with steeper linear decreases in Infection and Basic Needs Concerns, respectively.
3.3. Conditional growth models
Table 2 displays the results of the conditional growth models of depression and anxiety symptoms.
Table 2.
Conditional multilevel growth models of depression and anxiety symptoms.
| Depression | Anxiety | |||||
|---|---|---|---|---|---|---|
| Effect Estimate (SE) | Variance of Random Effect | Covariance of Random Effects | Effect Estimate (SE) | Variance of Random Effect | Covariance of Random Effects | |
| Intercept | 8.63(0.5)* | 25.80* | -.02 | 17.10(0.9)* | 75.33* | 0.07 |
| Time (Slope) | 0.91(0.6) | 1.21* | – | 0.99(0.9) | 2.71* | – |
| Time (Curvature) | -0.38(0.2) | – | – | -0.43(0.3) | – | – |
| Main Effect Estimate (SE) | Slope Interaction Estimate (SE) | Curvature Interaction Estimate (SE) | Main Effect Estimate (SE) | Slope Interaction Estimate (SE) | Curvature Interaction Estimate (SE) | |
| Time Invariant Covariates | ||||||
| Age | -0.24(0.2) | -0.83(0.2)* | 0.30(0.1)* | -1.36(0.3)* | -0.10(0.3) | 0.12(0.1) |
| Female | 0.89(0.7)* | 0.34(0.8) | -0.12(0.3) | 3.70(1.1)* | -0.34(1.1) | -0.10(0.4) |
| Pre-pandemic Depression | 0.53(0.1)* | -0.01(0.1) | 0.00(0.0) | 1.72(0.1) | 0.09(0.1) | -0.04(0.0) |
| Pre-pandemic Anxiety | 0.07(0.0)* | 0.04(0.0) | -0.01(0.0) | 0.57(0.1)* | 0.00(0.1) | 0.00(0.0) |
| Mean Life Changes | 0.15(0.2) | 0.49(0.3) | -0.18(0.1) | 0.07(0.4) | 0.31(0.4) | -0.09(0.1) |
| Mean Infection Concerns | 0.32(0.3) | 0.06(0.3) | -0.05(0.1) | 0.80(0.4) | 0.38(0.4) | -0.18(0.2) |
| Mean School Concerns | 1.88(0.3)* | 0.50(0.4) | -0.21(0.2) | 1.82(0.6)* | -0.07(0.6) | 0.11(0.2) |
| Mean Home Confinement Concerns | 1.05(0.4)* | -0.03(0.4) | -0.04 (0.2) | 0.32(0.6) | 0.34(0.6) | -0.06(0.2) |
| Mean Basic Needs Concerns | 0.88(0.6) | -0.37(0.6) | 0.21(0.2) | 2.17(0.9)* | -0.37(0.9) | 0.09(0.4) |
| Time Varying Covariates | ||||||
| Life Changes | -0.13(0.1) | 0.10(0.2) | ||||
| Infection Concerns | 0.18(0.1) | 0.41(0.2)* | ||||
| School Concerns | 0.60(0.2)* | 0.21(0.2) | ||||
| Home Confinement Concerns | 0.44(0.2)* | 0.31(0.3) | ||||
| Basic Needs Concerns | -0.16(0.2) | 0.02(0.3) | ||||
Note: SE = standard error; Time is coded as months since April 1st, 2020; significant effects are bolded*.
3.3.1. Depression
After controlling for age, sex, pre-pandemic symptoms of depression and anxiety and concurrent pandemic experiences, the slope, t(771) = 1.48, p =.139, and curve, t(760) = -1.56, p = .119, effects for depression were no longer significant, however, there remains significant variability in the slope (95% CI = 0.43-2.07). There were significant main effects of pre-pandemic depression, t(537) = 8.52, p < .001, and anxiety, t(515) = 2.20, p = .028, indicating that higher symptoms of depression and anxiety before the pandemic are associated with more severe symptoms of depression on April 1st (when Time = 0).
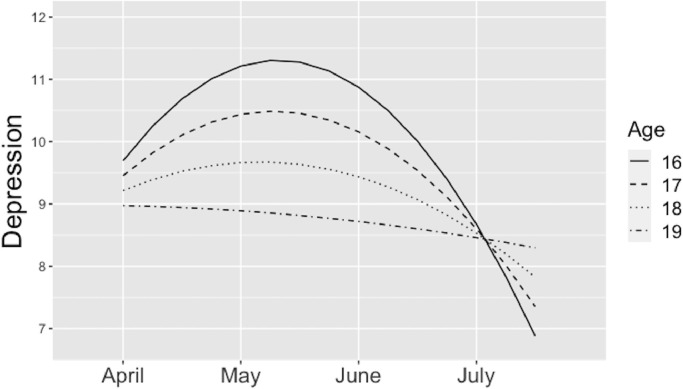
Although the main effect of age is not significant, there were significant interaction effects of age with the slope, t(778) = -3.56, p < .001, and curve, t(761) = 3.55, p < .001, of depression. To probe these interactions, we estimated the simple slopes for participants at ages 16, 17, 18 and 19, as 87% of participants fall within this age range. Fig. 3 displays the model-estimated trajectories of depression for each age group. Change in depression is characterized by a positive slope for 16-, (estimate = 2.45, SE = 0.49, t = 5.01, p < .001), 17- (estimate = 1.62, SE = 0.35, t = 4.61, p < .001), and 18-year-olds (estimate = 0.79, SE = 0.34, t = 2.32, p = .02), but a non-significant slope for 19-year-olds (estimate = -0.04, SE = 0.47, t = -0.09, p = .93), and negative curve effects for 16- (estimate = -0.93, SE = 0.18, t = -5.15, p < .001), 17- (estimate = -0.63, SE = 0.13, t = -4.76, p < .001), and 18-year-olds (estimate = -0.34, SE = 0.13, t = -2.62, p = .01), but not 19-year-olds (estimate = -0.04, SE = 0.17, t = -0.25, p = .80).
Fig. 3.
Model-estimated trajectories of depression symptoms for different age groups.
In terms of pandemic experiences, significant main effects were observed for (time invariant) mean School Concerns, t(540) = 5.49, p < .001, and Home Confinement Concerns, t(531) = 2.67, p = .008, indicating that individuals reporting greater School and Home Confinement Concerns, on average, had more severe depression symptoms in early April. Additionally, significant main effects were observed for (time-varying) deviations from individuals’ mean levels of School Concerns, t(747) = 3.90, p < .001, and Home Confinement Concerns, t(736) = 2.57, p = .01, indicating that greater than average (for that person) School and Home Confinement Concerns were associated with more severe depression symptoms over the spring and early summer.
3.3.2. Anxiety
Similar to depression, after controlling for age, sex, pre-pandemic symptoms and concurrent pandemic experiences, the slope, t(758) = 1.10, p = .273, and curve, t(748) = -1.22, p = .224, effects for anxiety were no longer significant, however, there remains significant variability in the slope (95% CI = 0.97-4.67). Significant main effects were found for age, t(537) = -3.96, p < .001, sex, t(527) = 3.40, p = .001, and pre-pandemic anxiety, t(508) = 11.12, p < .001, indicating that younger age, female sex and higher symptoms of anxiety before the pandemic are associated with more severe symptoms of anxiety on April 1st.
Significant main effects were observed for (time invariant) mean School Concerns, t(535) = 3.21, p = .001, and Basic Needs Concerns, t(540) = 2.39, p = .017, indicating that individuals reporting greater School and Basic Needs Concerns, on average, had more severe anxiety symptoms in early April. Additionally, significant main effects were observed for (time-varying) deviations in Infection Concerns, t(738) = 2.55, p = .011, indicating that greater than average (for that person) Infection Concerns were associated with more severe anxiety symptoms over the spring and early summer. No significant interaction effects were found between any of the time invariant predictors and the slope and curve effects.
Sensitivity analyses controlling for demographic variables that differed between samples and study (i.e., SBTS vs. iPANDA) produced substantively identical results.
4. Discussion
The current study explored patterns of within-person change in symptoms of depression and anxiety and pandemic experiences of youth living in Long Island, New York from late March to mid-July 2020, a critical period in the course of the COVID-19 pandemic in this region. Results suggest that, on average, symptoms of depression and anxiety increased slightly through April to a peak around late April/early May, and then decreased at an accelerating rate through July. Life changes due to COVID-19, such as having to move or being laid-off from work, followed a similar pattern of slight peaking followed by accelerating decline through July. Concerns about school and being confined at home did not show an initial increase in April, but declined at an accelerating rate across May-July, and concerns about becoming infected with COVID-19 and having one's basic needs met decreased linearly across April-July 2020.
Peaking of depression and anxiety symptoms and pandemic-related life changes occurred a few weeks later than the peak in COVID-19 infections in New York (see Fig. 1). This suggests that the impact of increasing infection rates on individuals’ lives occurs through downstream mechanisms that trail infection rates (e.g., policy changes, spread of information). We make this comparison cautiously, however, because our assessments probe pandemic experiences and anxiety symptoms over the past month and depressive symptoms over the past two weeks, so the timing of changes is not precise. Regardless, we see a clear pattern where symptoms of depression and anxiety and pandemic experiences were greater in April, when the rates of COVID-19 are highest and soon after a number of important community-level changes occurred in this region (e.g., school and business shut-downs). These symptoms and experiences then decreased across May-July as infection rates rapidly declined.
These findings shed light on why previous studies have reported conflicting patterns of change in mental health symptoms and stress across the pandemic. Depending on the timing of assessment, prior studies may have captured an early period of increase or a later period of decline that doesn't represent the overall pattern of change during the pandemic. For example, Salfi et al. (2020) found that symptoms of depression and anxiety increased over a one-month period spanning roughly week 3-7 of home confinement measures in Italy. We similarly found that symptoms increased from about week 2-6 of the New York state shutdown.
Notably, we observed significant variance in the random intercepts and slopes of all of our growth models, suggesting that there is significant variability between individuals in the level of symptoms and pandemic experiences in early April and the subsequent rate of change across Spring-Summer. Explaining these individual differences is critical for identifying subgroups who are more vulnerable to negative impacts of the pandemic. In the current paper, we made preliminary attempts to account for these individual differences, though much remains to be explored.
First, we found significant intercept-slope correlations for some of the pandemic experiences composites. Participants with higher initial levels of concern about infection with COVID-19, school problems and having one's basic needs met demonstrated steeper declines in these pandemic experiences across the study. This could in part reflect regression to the mean. In our conditional growth models of depression and anxiety symptoms, we found that female sex and younger age (for anxiety only), and higher pre-pandemic symptom levels were associated with more severe symptoms in early April. We also found that age could partially explain variance in the slope of depression, with younger participants (16-18-year-olds) showing a peaking in symptoms in early May and older participants (19-year-olds) showing no change in symptoms across the study. Research on prior disasters has consistently identified female sex, prior mental health conditions and younger age as predictors of worse mental health following the disaster (Goldmann and Galea, 2014), and it appears that the COVID-19 pandemic is no exception (Vindegaard and Benros, 2020).
Finally, greater school and home confinement concerns were associated with higher levels of depression symptoms, both within and between persons. In other words, reporting a greater average level of concern about school and being stuck at home across spring-summer was associated with more severe depression symptoms in early April. Further, reporting a higher degree of these concerns relative to one's average level was associated with more severe concurrent symptoms of depression. Individuals reporting greater school and basic needs concerns on average reported greater anxiety symptoms in early April and greater infection concerns than average for an individual were associated with more severe concurrent anxiety symptoms across Spring-Summer. These findings suggest that adverse pandemic experiences indeed accompany more severe symptoms in youth and that some domains of experience are more/less relevant to specific types of mental health problems. For example, the loneliness and isolation of being confined to one's home may be more relevant to risk for depression, whereas problems with online school possess both elements of danger (e.g., of not passing classes) relevant to risk for anxiety and loss (e.g., the education and associated opportunities one is missing out on) specific to risk for depression (Brown et al., 1993; Finlay-Jones and Brown, 1981; Kendler et al., 2003). However, the direction of association cannot be determined with this data. Additional survey follow-ups currently underway will allow us to clarify this.
It is notable that, in this sample of adolescents and young adults, the school concerns composite was associated with greater severity of both depression and anxiety symptoms. This suggests that, for youth, the impact of the pandemic on school functioning has been particularly detrimental. Future research on adult populations should explore whether the transition to online work has had a similar effect. Moreover, basic needs concerns might have an even greater impact on the mental health of individuals who are older and more likely to be responsible for other individuals in their household.
4.1. Limitations
The many strengths of this study (e.g., timing, location, longitudinal nature, extensive assessment of pandemic experiences and capturing both their within and between-person associations with symptoms) should be considered in light of its limitations. First, each individual completed a maximum of three surveys. Additional surveys would allow us to establish the direction of effects. Although we observed statistically significant changes in symptom levels, it is not clear how clinically meaningful these changes were. Our sample was relatively homogenous with respect to race, ethnicity, education and employment status, limiting generalizability to populations that are non-white, employed and college-aged but not attending school. Finally, a large proportion of SBTS and iPANDA project participants declined to participate in the COVID-19 study, and attrition analyses suggest that these participants differ substantially in their demographic profiles. Sensitivity analyses suggest the study findings do not change substantively after controlling for demographic variables; however, we cannot account for unmeasured differences in the samples that could impact the generalizability of these results.
4.2. Conclusion
The current study provides an initial picture of how symptoms of depression and anxiety and pandemic experiences in adolescents and young adults changed across Spring-Summer of 2020, a significant period in the course of the ongoing COVID-19 pandemic in Long Island, New York. Results suggest that, while symptoms were elevated early in the pandemic, they subsequently declined. Further, the trajectories of symptoms paralleled the trajectories of pandemic experiences and rates of COVID-19 infection in New York, suggesting that fluctuations in the pandemic accompany fluctuations in mental health problems. Further research is needed to establish the direction of associations, as well as moderators of these relationships.
Author contribution
D.N.K. and B.D.N. developed the study concept. D.N.K., B.D.N., A.K.S. and M.T.H. contributed to the study design. M.T.H. drafted the paper and performed the data analysis and interpretation. T.M.O. contributed to data analysis and interpretation. D.N.K., B.D.N., A.K.S. and T.M.O. provided critical revisions.
Funding
This work was supported by NIMH grants R01 MH069942 (Daniel N. Klein) and NIMH grant R01 MH097767 (Brady D. Nelson)
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
In the context of longitudinal data nested within persons, the ICC is the proportion of variance due to between-person (vs. within-person) differences. Larger ICCs indicate greater variance between persons and thus greater stability within persons across time.
References
- Bates, D., Mächler, M., Bolker, B., & Walker, S. (2014). Fitting linear mixed-effects models using lme4. arXiv. org. preprint]. doi, 10.
- Birmaher B., Khetarpal S., Brent D., Cully M., Balach L., Kaufman J., Neer S.M. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brown G.W., Harris T., Eales M. Aetiology of anxiety and depressive disorders in an inner-city population. 2. Comorbidity and adversity. Psychol. Med. 1993;23(1):155–165. doi: 10.1017/s0033291700038940. [DOI] [PubMed] [Google Scholar]
- Burani K., Klawohn J., Levinson A.R., Klein D.N., Nelson B.D., Hajcak G. Neural response to rewards, stress and sleep interact to prospectively predict depressive symptoms in adolescent girls. J. Clin. Child Adolesc. Psychol. 2019:1–10. doi: 10.1080/15374416.2019.1630834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. (2020). United States COVID-19 cases and deaths by state. Retrieved from https://www.cdc.gov/covid-data-tracker/.
- Curran P.J., Bauer D.J. The disaggregation of within-person and between-person effects in longitudinal models of change. Ann. Rev. Psychol. 2011;62:583–619. doi: 10.1146/annurev.psych.093008.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran P.J., Obeidat K., Losardo D. Twelve frequently asked questions about growth curve modeling. J. Cogn. Dev. 2010;11(2):121–136. doi: 10.1080/15248371003699969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty L.R., Klein D.N., Olino T.M. In: A Guide to Assessments that Work. Mash J.H.E., editor. Oxford University Press; New York: 2018. Depression in children and adolescents; pp. 99–130. [Google Scholar]
- Enders C.K. In: Structural equation modeling: A second course. 2nd ed. Hancock G.R., Muelle R.O., editors. Information Age Publishing; Charlotte, NC: 2013. Analyzing structural equation models with missing data; pp. 493–519. [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. e2019686-e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay-Jones R., Brown G.W. Types of stressful life event and the onset of anxiety and depressive disorders. Psychol. Med. 1981;11(4):803–815. doi: 10.1017/s0033291700041301. [DOI] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Ann. Rev. Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Gopal A., Sharma A.J., Subramanyam M.A. Dynamics of psychological responses to COVID-19 in India: a longitudinal study. PloS one. 2020;15(10) doi: 10.1371/journal.pone.0240650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J., Prinstein M.J., Clark L.A., Rottenberg J., Abramowitz J.S., Albano A.M., ..., Davila J. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am. Psychol. 2020 doi: 10.1037/amp0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman E.A., Thompson R.R., Garfin D.R., Silver R.C. The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the US. Sci. Adv. 2020:eabd5390. doi: 10.1126/sciadv.abd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Hettema J.M., Butera F., Gardner C.O., Prescott C.A. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch. Gen. Psychiatry. 2003;60(8):789–796. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Klein D.N., Finsaas M.C. The stony brook temperament study: early antecedents and pathways to emotional disorders. Child Dev. Perspect. 2017;11(4):257–263. doi: 10.1111/cdep.12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. North Tonawanda; NY: 1992. Children's Depression Inventory: Multi-Health Systems. [Google Scholar]
- Kuznetsova, A., Brockhoff, P., & Christensen, R. (2016). Tests in linear mixed effects models version. Cran. URL https://cran.r-project.org/web/packages/lmerTest/lmerTest.pdf.
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., ..., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020 doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil D.G., Jr. The U.S. now leads the world in confirmed coronavirus cases. N. Y. Times. 2020 https://www.nytimes.com/2020/03/26/health/usa-coronavirus-cases.html Retrieved from. [Google Scholar]
- Muris P., Mayer B., Den Adel M., Roos T., van Wamelen J. Predictors of change following cognitive-behavioral treatment of children with anxiety problems: A preliminary investigation on negative automatic thoughts and anxiety control. Child Psychiatry Hum. Dev. 2009;40(1):139–151. doi: 10.1007/s10578-008-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. Authors; Los Angeles, CA: 2017. Mplus: Statistical Analysis with Latent Variables: User's Guide (Version 8) [Google Scholar]
- Norris F.H., Sherrieb K., Galea S. Prevalence and consequences of disaster-related illness and injury from Hurricane Ike. Rehabil. Psychol. 2010;55(3):221. doi: 10.1037/a0020195. [DOI] [PubMed] [Google Scholar]
- Planchuelo-Gómez, Á., Odriozola-González, P., Irurtia, M.J., & de Luis-García, R. (2020). Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. [DOI] [PMC free article] [PubMed]
- Probst T., Budimir S., Pieh C. Depression in and after COVID-19 lockdown in Austria and the role of stress and loneliness in lockdown: a longitudinal study. J. Affect. Disord. 2020;277:962. doi: 10.1016/j.jad.2020.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappaport B., Pagliaccio D., Pine D., Klein D., Jarcho J. Discriminant validity, diagnostic utility, and parent-child agreement on the screen for child anxiety related emotional disorders (SCARED) in treatment-and non-treatment-seeking youth. J. Anxiety Disord. 2017;51:22–31. doi: 10.1016/j.janxdis.2017.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi F., Lauriola M., Amicucci G., Corigliano D., Viselli L., Tempesta D., Ferrara M. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol. Stress. 2020 doi: 10.1016/j.ynstr.2020.100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. anxiety. 2020;37(10):954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain, Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz J.R., Thurber C.A., Sweeney L., Proffitt V.D., LeGagnoux G.L. Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. J. Consult. Clin. Psychol. 1997;65(4):703. doi: 10.1037//0022-006x.65.4.703. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020). WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Retrieved from https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
- Zhou Y., MacGeorge E.L., Myrick J.G. Mental health and its predictors during the early months of the CoViD-19 pandemic experience in the United States. Int. J. Environ. Res. Public Health. 2020;17(17):6315. doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]