Abstract
Few people have paid attention to community epidemic prevention workers in the postpandemic era of COVID-19. This study aimed to explore the prevalence and risk factors for mental health symptoms in community epidemic prevention workers during the postpandemic era. Mental health status was evaluated by the Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, Chinese Perceived Stress Scale, Insomnia Severity Index, and Maslach Burnout Inventory-General Survey. The results showed that a considerable proportion of community epidemic prevention workers reported symptoms of depression (39.7%), anxiety (29.5%), high stress (51.1%), insomnia (30.8%), and burnout (53.3%). The prevalence of depression and anxiety in community epidemic prevention workers was higher than in community residents. Among community epidemic prevention workers, short sleep duration was a risk factor for depression, anxiety, high stress and insomnia. Concurrent engagement in work unrelated to epidemic prevention and current use of hypnotics were risk factors for depression, anxiety and insomnia. Our study suggests that during the postpandemic era, the mental health problems of community epidemic prevention workers are more serious than those of community residents. Several variables, such as short sleep duration and concurrent engagement in work unrelated to epidemic prevention, are associated with mental health among community epidemic prevention workers.
Keywords: COVID-19, Community epidemic prevention workers, Mental health symptoms, Depression, Anxiety, Insomnia
1. Introduction
The coronavirus disease 2019 (COVID-19) outbreak emerged in China in December 2019. The COVID-19 pandemic has seriously threatened people's physical and mental health, caused widespread public panic and captured global attention (Peng et al., 2020; Wang et al., 2020). COVID-19 has infected over 93 million people and caused more than 2 million deaths globally across 219 countries, areas, or territories through January 19, 2021 according to data from the World Health Organization (WHO) (World Health Organization, 2021). People have experienced severe psychological distress and been under unprecedented pressure due to the pandemic (Bao et al., 2020).
Since April 2020, the COVID-19 epidemic has been well controlled in China. China has entered the normal stage of epidemic prevention and control. Cities are now turning their attention back to socioeconomic development. However, the number of COVID-19 cases is increasing around the world. A new wave of COVID-19 infections will likely be imported from abroad (Tian et al., 2020). The WHO Director-General said we needed to empower, educate and engage communities and persist with using the same tools that we have been advocating since day one: find, isolate, test and care for cases and trace and quarantine their contacts (World Health Organization, 2020). Communities have played an important role in preventing the spread of COVID-19, not only in the early stage of the pandemic but also in the normal period of prevention due to rapid early detection, the quarantine of residents, and the rigorous implementation of comprehensive multidisciplinary measures (Zhang et al., 2020c,2020d).
Community containment was implemented on an unprecedented large-scale in China (Wilder-Smith and Freedman, 2020). Community containment strategies for management, tracking, and quarantine were strictly, effectively, and cooperatively implemented by a team that included public safety bureau officials, general practitioners, and community managers (Zhang et al., 2020c). Community epidemic prevention workers were responsible for confirming each individual's identity; checking their temperature; helping with the screening, registration and transportation of patients with confirmed or suspected cases; educating individuals about COVID-19; providing supplies for residents who were isolated at home or in hotels; collecting and reporting information and data about COVID-19; disinfecting the environment and objects; and so on. In addition to the anti-epidemic measures, complex economic community activities were also constantly unfolding in the reopening phase in China (Zhang et al., 2020d). Therefore, community epidemic prevention workers might need to hold multiple jobs.
Previous studies have found that during the early or late stage of the COVID-19 outbreak, different populations, from the general public to healthcare workers, had varying degrees of psychological disturbances, such as depression, anxiety, stress and insomnia (Pappa et al., 2020; Shi et al., 2020; Zhang et al., 2020a, 2020b; Zhou et al., 2020b). Community epidemic prevention workers might be at high risk of psychological problems due to the overwhelming workload, vulnerability to viral infection and fear of spreading the virus to their family members or friends. One study in China reported that the prevalence of depressive and anxiety symptoms among community epidemic prevention workers during the early stage of the COVID-19 outbreak was 51.4% and 16.0%, respectively (Guo et al., 2020). However, the psychological impact on community epidemic prevention workers during the postpandemic era has not yet been examined. To address this gap, the purpose of our study was to investigate the prevalence of mental health symptoms and related potential risk factors in community epidemic prevention workers during the postpandemic era of COVID-19 in China. The ultimate goal of this survey was to evaluate the mental health burden of community epidemic prevention workers during the postpandemic era of COVID-19 and provide potential guidance for the maintenance of mental well-being in this population.
2. Methods
2.1. Study design
This cross-sectional survey was conducted from August 28 to September 7, 2020, using anonymous online questionnaires via the Wenjuanxing platform with a snowball sampling strategy. The survey link was pushed to some WeChat groups of community epidemic prevention workers by one of the researchers who also participated in the control of COVID-19. In addition to their own participation, respondents were also asked to share this survey with their colleagues and other community epidemic prevention workers they know. At the same time, we shared the survey form at varieties of social network groups to recruit community residents and encouraged respondents to invite their family or friends to participate in this survey. Before collecting the data, all respondents were informed about the purpose of the research, data privacy and intended scientific use of the data. The study was approved by the ethics committee of the Third People's Hospital of Zhongshan (approval number: 2020SYLL031). Written informed consent was obtained online at the beginning of answering the questionnaire.
2.2. Participants
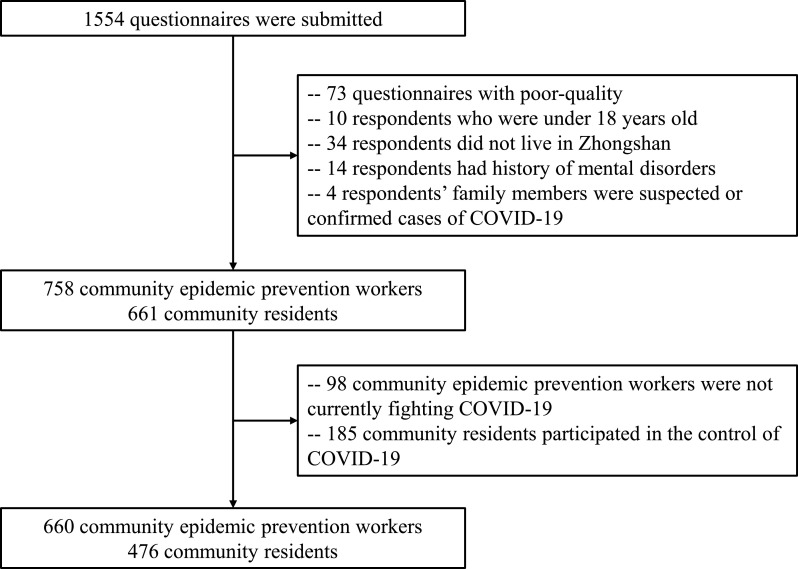
The inclusion criteria were different between community epidemic prevention workers and community residents. All community epidemic prevention workers were aged ≥ 18 years, living in Zhongshan, Guangdong, China and currently fighting COVID-19. Community residents were aged ≥ 18 years, living in Zhongshan City and never participated in the epidemic control of COVID-19. The exclusion criteria of these two groups of participants were as follows: (1) a history of psychiatric illnesses; (2) suspected or confirmed cases of COVID-19; (3) family members with suspected or confirmed cases of COVID-19. Details of the questionnaire screening are shown in the flow chart (Fig. 1 ). Finally, 660 community epidemic prevention workers and 476 community residents were included in the present study.
Fig. 1.
Flow chart of questionnaire screening.
In this study, community epidemic prevention workers are defined as individuals who took part in the community epidemic control of COVID-19, including community workers, community medical practitioners, police, public officials and volunteers.
2.3. Measurements
The questionnaire consisted of 7 domains: (1) demographic data; (2) COVID-19 epidemic-related information; (3) Patient Health Questionnaire-9 (PHQ-9); (4) Generalized Anxiety Disorder-7 (GAD-7); (5) Chinese Perceived Stress Scale-14 (CPSS-14); (6) Insomnia Severity Index (ISI); and (7) Maslach Burnout Inventory-General Survey (MBI-GS). Clinical symptoms were measured as outlined below.
2.3.1. Depression
Depressive symptoms were evaluated using the Chinese versions of the Patient Health Questionnaire-9 (PHQ-9) (Sun et al., 2017) on a 4-point Likert scale ranging from 0 (never) to 3 (nearly every day). It is a self-reported questionnaire that assesses whether individuals are bothered by the given symptoms during the previous two weeks. The total PHQ-9 score is interpreted as follows: normal (0–4), mild (5–9), moderate (10–14), and severe (15–27) depression. The PHQ-9 has been diffusely used in Chinese populations and has shown satisfactory validity and reliability (Wang et al., 2014).
2.3.2. Anxiety
The Generalized Anxiety Disorder-7 (GAD-7) is a 7-item self-assessment questionnaire that measures the severity of anxiety. The frequency of anxiety symptoms during the previous two weeks is assessed using a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The total GAD-7 score is divided into 0–4 (normal), 5–9 (mild), 10–14 (moderate), and 15–21 (severe). It has also been widely used in China, and good reliability and validity have been confirmed (Yu et al., 2018).
2.3.3. Perceived stress
The Chinese version of the Perceived Stress Scale (CPSS), which has excellent reliability and validity among Chinese populations (Yang and Huang, 2003), was used to analyze levels of perceived stress among respondents. Symptoms in the past month are assessed in the survey and includes 14 self-reported items. Each item has 5-point responses (0–4). Total score ranges from 0 to 56. A higher score indicates greater perceived stress. A total score ≥ 26 is indicative of a high level of stress (Ge et al., 2020; Yang and Huang, 2003).
2.3.4. Insomnia
The Insomnia Severity Index (ISI) is a self-rated scale that measures sleep quality in the last two weeks and includes 7 items. The total score is divided into 0–7 (no clinically significant insomnia), 8–14 (subthreshold insomnia), 15–21 (moderately severe clinical insomnia), and 22–28 (severe clinical insomnia) (Bastien et al., 2001).
2.3.5. Job burnout
Participants completed a Chinese version of the Maslach Burnout Inventory-General Survey (MBI-GS) (Wu et al., 2007), a 15-item self-reported measurement of job burnout that comprises three dimensions: emotional exhaustion (EE), depersonalization (DP) and diminished professional accomplishment (PA). The items are scored on a 7-point Likert scale from 0 (never) to 6 (each day). The cutoffs of burnout subscales were determined based on a previous study (He et al., 2017): EE (low: ≤ 10, moderate: 11–14, high: ≥ 15); DP (low: ≤ 8, moderate: 9–11, high: ≥ 12); and PA (low: ≤ 18, moderate: 19–21, high: ≥ 22). Higher ratings on the EE and DP dimensions and lower ratings on the PA dimension indicate higher levels of burnout. Job burnout state was defined under one or more of the three conditions-a high level of EE, a high level of DP, or a low level of PA (Eckleberry-Hunt et al., 2018). The Chinese version of the MBI-GS has been widely used in Chinese occupational burnout studies and has demonstrated good reliability and validity (Xie et al., 2011).
2.4. Statistical analysis
Descriptive statistics were used to present the variables. Frequency and percentage were used for categorical variables. Mean ± standard deviation (SD) or median (quartile range) was used for continuous variables. Inferential statistics, including independent sample t-tests, Mann-Whitney U tests and Chi-square tests, were used to examine whether there was any difference between community epidemic prevention workers and community residents in any of the parameters examined. Furthermore, unadjusted logistic regression and multivariable logistic regression analyses (forward LR) were adopted to explore factors potentially related to depression, anxiety, high stress, insomnia and burnout in community epidemic prevention workers. In the multivariable logistic regression model, odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Variables with a P value < 0.10 in the unadjusted logistic regression analysis and those that might carry crucial information were added into the multivariable logistic regression model. SPSS 23.0 statistical software (SPSS Inc., Chicago, United States) was used to performed the statistical analysis. Significance was evaluated at p < 0.05, two-tailed.
3. Results
3.1. Demographic and epidemic-related characteristics of community epidemic prevention workers and community residents
Table 1 shows the demographic and epidemic-related characteristics of participants. Finally, 1136 eligible subjects were enrolled in the analysis (Fig. 1). The respondents consisted of 660 community epidemic prevention workers and 476 community residents who were gender and age matched. The majority of subjects from both groups were women, with a mean age of 35.4 ± 7.2 years, ranging from 19 to 64 years. Of the total number of respondents, 891 (78.4%) were married. There was a significantly higher ratio of community epidemic prevention workers who held a university degree (88.8%) compared to community residents (58.6%) (p < 0.001). In the past two weeks, significantly more community epidemic prevention workers had nighttime sleep durations of less than 7 h (39.2% vs 26.1%) and focused on COVID-19 > 2 h every day (48.3% vs 18.9%) compared to community residents (p < 0.001). In addition, over 80% of participants from both groups worked more than 7 h per day. For community residents, 24 (5%) respondents had quarantine experience, which was significantly higher than that of community epidemic prevention workers (1.5%) (p = 0.001). Significantly more community epidemic prevention workers had direct contact with confirmed or suspected COVID-19 cases (7.6% vs 0.2%, p < 0.001) and currently used hypnotics to improve sleep quality (3.3% vs 0.6%, p = 0.002) compared to community residents. Nevertheless, there were no significant differences in the use of antidepressants or anxiolytics, the perceived need for mental health care or history of chronic diseases between the two groups. Furthermore, 413 (62.6%) community epidemic prevention workers’ duration of epidemic prevention was over 6 months, and 441 (66.8%) concurrently engaged in work unrelated to epidemic prevention.
Table 1.
Demographic characteristics and epidemic-related information of community epidemic prevention workers and community residents.
| Variables | Community epidemic prevention workers (n = 660, 58.1%) | Community residents (n = 476, 41.9%) | Statistics (χ2/t/z) | P |
|---|---|---|---|---|
| Gender | 3.515 | 0.061 | ||
| Male | 213 (32.3%) | 129 (27.1%) | ||
| Female | 447 (67.7%) | 347 (72.9%) | ||
| Age (years) | ||||
| Mean (SD) | 35.3 (7.3) | 35.5 (7.1) | - 0.345a | 0.73 |
| 18 - 39 | 476 (72.1%) | 368 (77.3%) | 3.9 | 0.048* |
| ≥ 40 | 184 (27.9%) | 108 (22.7%) | ||
| Marital status | 6.134 | 0.105 | ||
| Single | 131 (19.8%) | 70 (14.7%) | ||
| Married | 507 (76.8%) | 384 (80.7%) | ||
| Divorced | 19 (2.9%) | 20 (4.2%) | ||
| Widowed | 3 (0.5%) | 2 (0.4%) | ||
| Education | 150.149 | < 0.001* | ||
| Middle school or below | 3 (0.5%) | 47 (9.9%) | ||
| High school | 64 (9.7%) | 133 (27.9%) | ||
| University | 586 (88.8%) | 279 (58.6%) | ||
| Postgraduate university degree | 7 (1.1%) | 17 (3.6%) | ||
| Daily working hours | ||||
| Mean (SD) | 7.8 (1.4) | 7.6 (2.8) | 0.894a | 0.372 |
| < 7 | 125 (18.9%) | 92 (19.3%) | 0.027 | 0.87 |
| ≥ 7 | 535 (81.1%) | 384 (80.7%) | ||
| Sleep duration per night (hours) | ||||
| Mean (SD) | 6.8 (0.9) | 7.2 (1.1) | - 5.786a | < 0.001* |
| < 7 | 259 (39.2%) | 124 (26.1%) | 21.536 | < 0.001* |
| ≥ 7 | 401 (60.8%) | 352 (73.9%) | ||
| Time to think about COVID-19 per day (hours) | ||||
| Median (IQR) | 1.5 (1.0, 4.0) | 1.0 (0.5, 1.0) | - 13.639b | < 0.001* |
| < 2 | 341 (51.7%) | 386 (81.1%) | 103.927 | < 0.001* |
| ≥ 2 | 319 (48.3%) | 90 (18.9%) | ||
| Have you had direct contact with confirmed or suspected cases of COVID-19? | 34.991 | < 0.001* | ||
| Yes | 50 (7.6%) | 1 (0.2%) | ||
| No | 610 (92.4%) | 475 (99.8%) | ||
| Have you ever experienced quarantine? | 18.395 | < 0.001* | ||
| Centralized | 4 (0.6%) | 1 (0.2%) | ||
| Home | 6 (0.9%) | 23 (4.8%) | ||
| None | 650 (98.5%) | 452 (95.0%) | ||
| History of chronic diseases | 0.059 | 0.808 | ||
| Yes | 34 (5.2%) | 23 (4.8%) | ||
| No | 626 (94.8%) | 453 (95.2%) | ||
| Use of hypnotics | 9.388 | 0.002* | ||
| Yes | 22 (3.3%) | 3 (0.6%) | ||
| No | 638 (96.7%) | 473 (99.4%) | ||
| Use of antidepressants or anxiolytics | 0.186 | 0.666 | ||
| Yes | 4 (0.6%) | 2 (0.4%) | ||
| No | 656 (99.4%) | 474 (99.6%) | ||
| Perceived need for mental health treatment | 0.254 | 0.614 | ||
| Yes | 70 (10.6%) | 55 (11.6%) | ||
| No | 590 (89.4%) | 421 (88.4%) | ||
| Duration of epidemic prevention (months) | ||||
| Mean (SD) | 6.2 (2.0) | NA | NA | NA |
| < 3 | 57 (8.6%) | |||
| 3 - 6 | 190 (28.8%) | |||
| > 6 | 413 (62.6%) | |||
| Concurrent engagement in work unrelated to epidemic prevention | ||||
| Yes | 441 (66.8%) | NA | NA | NA |
| No | 219 (33.2%) |
Abbreviations: SD, standard deviation; IQR, Interquartile range; COVID-19, coronavirus disease 2019; NA, not available.
Unless otherwise specified, data were compared with Chi-squared test.
independent samples t-test.
Mann-Whitney U test
P < 0.05
3.2. PHQ-9, GAD-7, CPSS-14 and ISI scores of community epidemic prevention workers and community residents
Table 2 shows the PHQ-9, GAD-7, CPSS-14 and ISI scores of the study respondents. The median PHQ-9 scores of community epidemic prevention workers and community residents were 3 (IQR 0-8) and 2 (IQR 0-6), respectively. A total of 107 (16.3%) community epidemic prevention workers and 34 (7.1%) community residents received a score of 10 or higher, indicating moderate to severe depressive symptoms.
Table 2.
PHQ-9, GAD-7, CPSS-14 and ISI scores of community epidemic prevention workers and community residents.
| Variables | Community epidemic prevention workers (n = 660, 58.1%) | Community residents (n = 476, 41.9%) | Statistics (χ2/t/z) | P |
|---|---|---|---|---|
| Patient Health Questionnaire (PHQ-9) | ||||
| Median (IQR) | 3 (0, 8) | 2 (0, 6) | - 3.987b | < 0.001* |
| No (0 - 4) | 398 (60.3%) | 322 (67.6%) | 21.02 | < 0.001* |
| Mild (5 - 9) | 155 (23.5%) | 120 (25.2%) | ||
| Moderate (10 - 14) | 69 (10.5%) | 22 (4.6%) | ||
| Severe (15 - 27) | 38 (5.8%) | 12 (2.5%) | ||
| Generalized Anxiety Disorder (GAD-7) | ||||
| Median (IQR) | 1 (0, 6) | 0 (0, 4) | - 3.423b | 0.001* |
| No (0 - 4) | 465 (70.5%) | 375 (78.8%) | 10.045 | 0.018* |
| Mild (5 - 9) | 131 (19.8%) | 66 (13.9%) | ||
| Moderate (10 - 14) | 42 (6.4%) | 23 (4.8%) | ||
| Severe (15 - 21) | 22 (3.3%) | 12 (2.5%) | ||
| Chinese Perceived Stress Scale (CPSS-14) | ||||
| Mean CPSS-14 score | 24.3 (8.3) | 23.1 (7.3) | 2.365a | 0.018* |
| Low (≤ 25) | 323 (48.9%) | 244 (51.3%) | 0.596 | 0.44 |
| High (≥ 26) | 337 (51.1%) | 232 (48.7%) | ||
| Insomnia Severity Index (ISI) | ||||
| Median (IQR) | 5 (1, 8) | 4 (1, 7) | - 1.413b | 0.158 |
| No clinically significant insomnia (0 - 7) | 457 (69.2%) | 359 (75.4%) | 6.799 | 0.079 |
| Subthreshold insomnia (8 - 14) | 169 (25.6%) | 98 (20.6%) | ||
| Moderately severe clinical insomnia (15 - 21) | 31 (4.7%) | 15 (3.2%) | ||
| Severe clinical insomnia (22 - 28) | 3 (0.5%) | 4 (0.8%) |
Abbreviations: IQR, Interquartile range.
Unless otherwise specified, data were compared with Chi-squared test.
independent samples t-test
Mann-Whitney U test
P < 0.05
The median GAD-7 scores of community epidemic prevention workers and community residents were 1 (IQR 0-6) and 0 (IQR 0-4), respectively. Sixty-four (9.7%) community epidemic prevention workers and 35 (7.3%) community residents received a score of 10 or above, demonstrating moderate to severe anxiety symptoms.
The mean CPSS-14 score of community epidemic prevention workers (24.3 ± 8.3) was higher than that of community residents (23.1 ± 7.3) (p = 0.018). A total of 337 (51.1%) community epidemic prevention workers and 232 (48.7%) community residents received a score of 26 or higher, revealing high stress symptoms.
The median ISI scores of community epidemic prevention workers and community residents were 5 (IQR 1–8) and 4 (IQR 1–7), respectively. Thirty-four (5.2%) community epidemic prevention workers and 19 (4.0%) community residents received a score of 15 or above, suggesting that they had moderately severe to severe clinical insomnia.
3.3. MBI-GS scores of community epidemic prevention workers and community residents
Table 3 shows the MBI-GS scores of the study respondents. Fifty-five community residents were excluded because they were students, retirees and unemployed people. Finally, a total of 421 residents and 660 community epidemic prevention workers were analyzed in this section. The mean MBI-GS EE score of community epidemic prevention workers (9.2 ± 6.3) was significantly higher than that of community residents (8.0 ± 5.3) (p = 0.001). A total of 102 (15.5%) community epidemic prevention workers and 43 (10.2%) community residents received a score of 15 or higher, indicating a high level of emotional exhaustion. However, there were no significant differences in the rates of MBI-GS DP, MBI-GS PA and burnout between the two groups (p > 0.05). In our sample, 352 (53.3%) community epidemic prevention workers and 234 (55.6%) community residents met the criterion for burnout.
Table 3.
MBI-GS scores of community epidemic prevention workers and community residents.
| Variables | Community epidemic prevention workers (n = 660, 61.1%) | Community residents (n = 421, 38.9%) | Statistics (χ2/t) | P |
|---|---|---|---|---|
| Maslach Burnout Inventory - General Survey (MBI-GS) | ||||
| Mean MBI-GS Emotional Exhaustion score | 9.2 (6.3) | 8.0 (5.3) | 3.294a | 0.001* |
| MBI-GS (Emotional Exhaustion) | 8.782 | 0.012* | ||
| low (≤ 10) | 454 (68.8%) | 323 (76.7%) | ||
| moderate (11 - 14) | 104 (15.8%) | 55 (13.1%) | ||
| high (≥ 15) | 102 (15.5%) | 43 (10.2%) | ||
| Mean MBI-GS Depersonalization score | 5.2 (5.2) | 4.9 (4.8) | 1.004a | 0.316 |
| MBI-GS (Depersonalization) | 2.341 | 0.31 | ||
| low (≤ 8) | 534 (80.9%) | 354 (84.1%) | ||
| moderate (9 - 11) | 51 (7.7%) | 31 (7.4%) | ||
| high (≥ 12) | 75 (11.4%) | 36 (8.6%) | ||
| Mean MBI-GS Professional Accomplishment score | 21.5 (10.0) | 20.6 (10.1) | 1.366a | 0.172 |
| MBI-GS (Professional Accomplishment) | 3.667 | 0.160 | ||
| low (≤ 18) | 299 (45.3%) | 205 (48.7%) | ||
| moderate (19 - 21) | 52 (7.9%) | 42 (10.0%) | ||
| high (≥ 22) | 309 (46.8%) | 174 (41.3%) | ||
| Burnout | 0.524 | 0.469 | ||
| Yes | 352 (53.3%) | 234 (55.6%) | ||
| No | 308 (46.7%) | 187 (44.4%) |
Note: 55 community residents were excluded because they were students, retirees and unemployed people. Finally, a total of 421 residents and 660 community epidemic prevention workers were analyzed in this section.
Unless otherwise specified, data were compared with Chi-squared test.
independent samples t-test
P < 0.05
3.4. Factors related with symptoms of depression, anxiety, high stress, insomnia, and job burnout in community epidemic prevention workers
Results of the unadjusted logistic regression analysis are shown in Supplemental Table 1. As shown in Table 4 , multivariable logistic regression analysis revealed that older age was a protective factor for the depressive symptoms (p < 0.001, OR = 0.438, 95% CI: 0.293–0.654), anxiety (p = 0.005, OR = 0.538, 95% CI: 0.350 –0.829) and high stress (p < 0.001, OR = 0.444, 95% CI: 0.309–0.637). Being married was a protective factor for the symptoms of burnout (p < 0.001, OR = 0.420, 95% CI: 0.277–0.635). Having nighttime sleep durations longer than 7 h was still a protective factor for the symptoms of depression (p < 0.001, OR = 0.537, 95% CI: 0.379–0.760), anxiety (p < 0.001, OR = 0.439, 95% CI: 0.303–0.637), high stress (p < 0.001, OR = 0.419, 95% CI: 0.293–0.600) and insomnia (p < 0.001, OR = 0.374, 95% CI: 0.230–0.608). Concurrent engagement in work unrelated to epidemic prevention was a risk factor for the symptoms of depression (p < 0.001, OR = 2.621, 95% CI: 1.790–3.838), anxiety (p < 0.001, OR = 2.538, 95% CI: 1.655–3.891), and insomnia (p < 0.001, OR = 2.070, 95% CI: 1.383–3.099). The current use of hypnotics was significantly associated with symptoms of depression (p = 0.001, OR = 8.226, 95% CI: 2.305–29.356), anxiety (p = 0.002, OR = 5.070, 95% CI: 1.850–13.895) and insomnia (p = 0.001, OR = 5.902, 95% CI: 2.061–16.899). In addition, the self-perceived need for mental health care conveyed a high risk of having depression (p < 0.001, OR = 5.655, 95% CI: 3.129–10.220), anxiety (p < 0.001, OR = 7.146, 95% CI: 4.031–12.671), high stress (p < 0.001, OR = 3.936, 95% CI: 2.171–7.136), insomnia (p < 0.001, OR = 4.473, 95% CI: 2.601–7.695) and job burnout (p < 0.001, OR = 2.882, 95% CI: 1.637–5.073).
Table 4.
Multivariable logistic regression analysis (forward LR) of risk factors associated with symptoms of depression, anxiety, high stress, insomnia, and job burnout in community epidemic prevention workers (n = 660).
| Variables | Depressiona | Anxietyb | High stressc | Insomniad | Job burnoute |
|---|---|---|---|---|---|
| Gender (reference: Male) | |||||
| Female | NA | NA | Non-significant | NA | NA |
| Age (reference: 18 - 39) | |||||
| ≥ 40 | 0.438 (0.293 - 0.654) | 0.538 (0.350 - 0.829) | 0.444 (0.309 - 0.637) | NA | NA |
| p < 0.001 | p = 0.005 | p < 0.001 | |||
| Marital status (reference: Single) | |||||
| Married | Non-significant | Non-significant | Non-significant | NA | 0.420 (0.277 - 0.635) |
| P < 0.001 | |||||
| Divorced | Non-significant | Non-significant | Non-significant | NA | Non-significant |
| Widowed | Non-significant | Non-significant | Non-significant | NA | Non-significant |
| Education (reference: Postgraduate university degree) | |||||
| Middle school or below | Non-significant | NA | NA | NA | NA |
| High school | |||||
| University | |||||
| Daily working hours (reference: < 7) | |||||
| ≥ 7 | Non-significant | Non-significant | Non-significant | Non-significant | Non-significant |
| Sleep duration per night (reference: < 7) | |||||
| ≥ 7 | 0.537 (0.379 - 0.760) | 0.439 (0.303 - 0.637) | 0.419 (0.293 - 0.600) | 0.374 (0.230 - 0.608) | Non-significant |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | ||
| Time to think about COVID-19 per day (reference: < 2) | |||||
| ≥ 2 | NA | Non-significant | Non-significant | NA | NA |
| History of chronic diseases (reference: No) | |||||
| Yes | NA | NA | NA | Non-significant | NA |
| Duration of epidemic prevention (reference: < 3) | |||||
| 3 - 6 | Non-significant | Non-significant | Non-significant | Non-significant | Non-significant |
| > 6 | |||||
| Concurrent engagement in work unrelated to epidemic prevention (reference: No) | |||||
| Yes | 2.621 (1.790 - 3.838) | 2.538 (1.655 - 3.891) | Non-significant | 2.070 (1.383 - 3.099) | Non-significant |
| p < 0.001 | p < 0.001 | p < 0.001 | |||
| Use of hypnotics (reference: No) | |||||
| Yes | 8.226 (2.305 -29.356) | 5.070 (1.850 - 13.895) | Non-significant | 5.902 (2.061 - 16.899) | NA |
| p = 0.001 | p = 0.002 | p = 0.001 | |||
| Use of antidepressants or anxiolytics (reference: Yes) | |||||
| No | NA | Non-significant | NA | Non-significant | NA |
| Perceived need for mental health treatment (reference: No) | |||||
| Yes | 5.655 (3.129 - 10.220) | 7.146 (4.031 - 12.671) | 3.936 (2.171 - 7.136) | 4.473 (2.601 - 7.695) | 2.882 (1.637 - 5.073) |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
Abbreviations: NA = not available (variables that were not analyzed because they were not statistically significant in the unadjusted logistic regression model)
Depression was defined as Patient Health Questionnaire-9 score of 5 or higher.
Anxiety was defined as Generalized Anxiety Disorder-7 score of 5 or higher.
High perceived stress was defined as Chinese Perceived Stress Scale score of 26 or higher.
Insomnia was defined as Insomnia Severity Index score of 8 or higher.
Job burnout state was defined under one or more of the three conditions — a Maslach Burnout Inventory-General Survey emotional exhaustion score of 15 or higher, depersonalization score of 12 or higher, or professional accomplishment score of 18 or below.
4. Discussion
Our study primarily found that (1) during the postpandemic era of the COVID-19 epidemic in China, the prevalence of depression, anxiety, high stress, insomnia and burnout in community epidemic prevention workers was 39.7%, 29.5%, 51.1%, 30.8% and 53.3%, respectively. Moreover, the symptoms of depression and anxiety in community epidemic prevention workers were more serious than those in community residents. (2) In community epidemic prevention workers, older age was a protective factor for symptoms of depression, anxiety and high stress, while being married was a protective factor for burnout. (3) Short sleep duration (< 7 h) was a risk factor for depression, anxiety, high stress and insomnia in community epidemic prevention workers. (4) Both concurrent engagement in work unrelated to epidemic prevention and current use of hypnotics were risk factors for depression, anxiety and insomnia in community epidemic prevention workers. (5) The perceived need for mental health care was a risk factor for depression, anxiety, high stress, insomnia and burnout in community epidemic prevention workers.
In the present study, a significant proportion of community epidemic prevention workers experienced depression, anxiety and insomnia symptoms, and more than 50% reported high stress and burnout. However, compared to a previous survey conducted in frontline healthcare staff during the early stage of the COVID-19 epidemic outbreak (Lai et al., 2020), the rates of depression (39.7% vs 50.4%), anxiety (29.5% vs 44.6%) and insomnia symptoms (30.8% vs 34.0%) were lower in our study. Differences in the time points of conducting mental health assessments may be responsible for this inconsistency. After taking effective preventive measures, the level of psychological distress may decrease over time. In addition, a previous study during the late period of the COVID-19 pandemic outbreak at the beginning of April 2020 suggested that depressive symptoms, anxiety symptoms, moderate to severe levels of stress and insomnia were 45.6%, 20.7%, 60.8% and 27.0% in frontline health professionals, respectively, similar to our results (Tian et al., 2020). Compared to community residents, we found that community epidemic prevention workers experienced higher symptoms of depression and anxiety. Zhou et al. (2020a) demonstrated that frontline medical staff reported higher incidences of depression and anxiety than the general population. Additionally, our study indicated that more than half (53.3%) of community epidemic prevention workers exhibited symptoms of burnout, which was in accordance with a recent study on intensive care unit specialists (51%) (Azoulay et al., 2020). As a result of the COVID-19 pandemic, epidemic prevention workers were under overwhelming workload pressure, which might be the primary reason for job burnout (Moazzami et al., 2020). It is noteworthy that burnout is highly associated with physical and mental fatigue, lack of motivation, difficulty concentrating, irritability, sleep disorders, depression, anxiety and job dissatisfaction (Piko, 2006; Van Laethem et al., 2015; Wang et al., 2015). This suggests that we should pay more attention to the mental health of community epidemic prevention workers.
Moreover, our study identified several risk factors for mental health symptoms in community epidemic prevention workers. We found that short sleep duration was a risk factor for depression, anxiety, high stress and insomnia symptoms in community epidemic prevention workers, which was partially consistent with a previous study on home-quarantined Chinese university students (Tang et al., 2020). Short sleep duration has been demonstrated to be associated with psychological disorders (Bao et al., 2017; Brostrom et al., 2018). Short sleep duration also predicted anxiety in response to stress exposure (Kalmbach et al., 2019). The present study also found that community epidemic prevention workers currently using hypnotics reported more severe depressive, anxious, and insomnious symptoms. 8.4% of community epidemic prevention workers used hypnotics to help them fall asleep. Su et al. (2004) found that the use of hypnotics was one of the risk factors associated with insomnia. Moreover, it is worth noting that insomnia increases the risk for depression and anxiety (Hertenstein et al., 2019). Our study also found that community epidemic prevention workers who concurrently engaged in work unrelated to epidemic prevention had higher risk to report depressive, anxious and insomnious symptoms, which was partially consistent with a prior study. Bruns et al. (2019) showed that multiple job holdings were associated with a greater probability of experiencing depression and stress. In addition, we found that 10.6% of community epidemic prevention workers reported a current need for mental health care, which was in accordance with previous research showing that the 12-month prevalence of perceived need for mental health care ranged from 11.6 to 17% in the general Canadian population (Sareen et al., 2005). Our findings also suggested that the perceived need for mental health care was a risk factor for all measured mental health symptoms, including depression, anxiety, high stress, insomnia and burnout. Compared to individuals without needs for mental health care, those with needs for mental health care had significant depressive, anxious, distress and suicide symptoms (Orr et al., 2018; Sareen et al., 2005). This illustrates that community epidemic prevention workers’ self-perceived need for mental health treatment needs urgent attention.
In addition, the present study identified two protective factors for mental health problems in community epidemic prevention workers. We found that older age was a protective factor for the symptoms of depression, anxiety and high stress, which was consistent with a previous study on Chinese frontline medical staff during the COVID-19 epidemic (Zhou et al., 2020a). However, Hao et al. (2020) found that levels of depression, anxiety and stress were not related to age. Differences in the characteristics of the study subjects or differences in the study protocol might be responsible for these discrepancies. In addition, in our current study, being married was a protective factor for burnout, which was in agreement with previous studies (Canadas-De la Fuente et al., 2018; Gabbe et al., 2018; Guenette and Smith, 2018). This might be attributed to the fact that individuals have good social support from the family environment of a couple lifestyle, protecting them from negative attitudes towards workmates at the workplace (Canadas-De la Fuente et al., 2018).
Several limitations of our study should be mentioned. First, this was an online investigation with a snowball sampling strategy in Zhongshan, which was not based on random selection of samples. Thus, further surveys based on a wider geographic area should be conducted. Second, this was a cross-sectional study that did not show causal relationships, and further prospective cohort studies should be conducted. Third, the participants’ self-reports were used to value mental health status, and clinical diagnoses should be used in further study.
Despite the limitations mentioned above, to our knowledge, this is the first study that examined the psychological impact on community epidemic prevention workers during the postpandemic era of COVID-19 in China. Our study provides a reference for mental health policies in China and other countries.
In conclusion, mental health problems are common among community epidemic prevention workers in China during the postpandemic era, despite the setting of a well-contained COVID-19 pandemic. Among community epidemic prevention workers, a perceived need for mental health treatment is a risk factor for all measured mental health problems. Furthermore, short sleep duration, current use of hypnotics and concurrent engagement in work unrelated to epidemic prevention are risk factors, while older age and being married are protective factors for certain psychological disturbances. Timely and appropriate implementation of effective psychosocial services are key to improving the mental health status of this population. Meanwhile, we should adjust their work arrangements to ensure rest.
Role of funding source
This work was supported by the National Natural Science Foundation of China (Grant No. 81701341), the National Key Research and Development Program of China (Grant No. 2016YFC0906300), Science and Technology Plan Project of Guangdong Province (Grant No. 2019B030316001). The funding source had no role in the study design, analysis or interpretation of data or in the preparation of the report or decision to publish.
CRediT authorship contribution statement
Chunyu Yang: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Weijian Liu: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Yihua Chen: Data curation, Writing – review & editing. Jie Zhang: Data curation, Writing – review & editing. Xiaomei Zhong: Data curation, Writing – review & editing. Qifeng Du: Data curation, Writing – review & editing. Jianlong Zhang: Data curation, Writing – review & editing. Jingrong Mo: Data curation, Writing – review & editing. Zhenjie Chen: Data curation, Writing – review & editing. Yuping Ning: Visualization, Writing – review & editing, Data curation. Baoguo Du: Visualization, Writing – review & editing, Data curation, Supervision.
Declaration of Competing Interest
All authors declare no actual or potential conflicts of interest.
Acknowledgment
We thank for all the participants in this study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2021.114132.
Appendix. Supplementary materials
References
- Azoulay E., De Waele J., Ferrer R., Staudinger T., Borkowska M., Povoa P., Iliopoulou K., Artigas A., Schaller S.J., Hari M.S., Pellegrini M., Darmon M., Kesecioglu J., Cecconi M., Esicm Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann. Intensive Care. 2020;10:110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y.P., Han Y., Ma J., Wang R.J., Shi L., Wang T.Y., He J., Yue J.L., Shi J., Tang X.D., Lu L. Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: meta-analysis and systematic review. Neurosci. Biobehav. Rev. 2017;75:257–273. doi: 10.1016/j.neubiorev.2017.01.032. [DOI] [PubMed] [Google Scholar]
- Bastien C., Vallières A., Morin C. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Brostrom A., Wahlin A., Alehagen U., Ulander M., Johansson P. Sex-specific associations between self-reported sleep duration, depression, anxiety, fatigue and daytime sleepiness in an older community-dwelling population. Scand. J. Caring Sci. 2018;32:290–298. doi: 10.1111/scs.12461. [DOI] [PubMed] [Google Scholar]
- Bruns A., Pilkauskas N. Multiple job holding and mental health among low-income mothers. Womens Health Issues. 2019;29:205–212. doi: 10.1016/j.whi.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadas-De la Fuente G.A., Ortega E., Ramirez-Baena L., De la Fuente-Solana E.I., Vargas C., Gomez-Urquiza J.L. Gender, marital status, and children as risk factors for burnout in nurses: a meta-analytic study. Int. J. Environ. Res. Public Health. 2018;15 doi: 10.3390/ijerph15102102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckleberry-Hunt J., Kirkpatrick H., Barbera T. The problems with burnout research. academic medicine: journal of the association of. Am. Med. Coll. 2018;93:367–370. doi: 10.1097/acm.0000000000001890. [DOI] [PubMed] [Google Scholar]
- Gabbe S.G., Hagan Vetter M., Nguyen M.C., Moffatt-Bruce S., Fowler J.M. Changes in the burnout profile of chairs of academic departments of obstetrics and gynecology over the past 15 years. Am. J. Obstet. Gynecol. 2018;219 doi: 10.1016/j.ajog.2018.06.012. 303 e301-303 e306. [DOI] [PubMed] [Google Scholar]
- Ge Y., Xin S., Luan D., Zou Z., Bai X., Liu M., Gao Q. Independent and combined associations between screen time and physical activity and perceived stress among college students. Addict Behav. 2020;103 doi: 10.1016/j.addbeh.2019.106224. [DOI] [PubMed] [Google Scholar]
- Guenette J.P., Smith S.E. Burnout: job resources and job demands associated with low personal accomplishment in United States radiology residents. Acad. Radiol. 2018;25:739–743. doi: 10.1016/j.acra.2017.12.002. [DOI] [PubMed] [Google Scholar]
- Guo J., Q.C., Zhao Y., et al. Status of anxiety and depressive symptoms and its influencing factors among coronavirus disease 2019 community prevention and control staff: a cross-sectional study in Bao'an District of Shenzhen, China. Chin. J. Soc. Med. 2020;37:459–464. doi: 10.3969/j.issn.1673-5625.2020.05.003. [DOI] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S., Zhang Y., Zhan J., Wang C., Du X., Yin G., Cao B., Ning Y., Soares J., Zhang X. Burnout and cognitive impairment: associated with serum BDNF in a Chinese Han population. Psychoneuroendocrinology. 2017;77:236–243. doi: 10.1016/j.psyneuen.2017.01.002. [DOI] [PubMed] [Google Scholar]
- Hertenstein E., Feige B., Gmeiner T., Kienzler C., Spiegelhalder K., Johann A., Jansson-Frojmark M., Palagini L., Rucker G., Riemann D., Baglioni C. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med. Rev. 2019;43:96–105. doi: 10.1016/j.smrv.2018.10.006. [DOI] [PubMed] [Google Scholar]
- Kalmbach D.A., Abelson J.L., Arnedt J.T., Zhao Z., Schubert J.R., Sen S. Insomnia symptoms and short sleep predict anxiety and worry in response to stress exposure: a prospective cohort study of medical interns. Sleep Med. 2019;55:40–47. doi: 10.1016/j.sleep.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moazzami B., Razavi-Khorasani N., Dooghaie Moghadam A., Farokhi E., Rezaei N. COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J. Clin. Virol. 2020;126 doi: 10.1016/j.jcv.2020.104345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr J., Bernstein C.N., Graff L.A., Patten S.B., Bolton J.M., Sareen J., Marriott J.J., Fisk J.D., Marrie R.A., Burden C.T.i.D.t. Factors associated with perceived need for mental health care in multiple sclerosis. Mult. Scler. Relat. Disord. 2018;25:179–185. doi: 10.1016/j.msard.2018.07.043. [DOI] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng M., Mo B., Liu Y., Xu M., Song X., Liu L., Fang Y., Guo T., Ye J., Yu Z., Deng Q., Zhang X. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. J. Affect. Disord. 2020;275:119–124. doi: 10.1016/j.jad.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piko B.F. Burnout, role conflict, job satisfaction and psychosocial health among hungarian health care staff: a questionnaire survey. Int. J. Nurs. Stud. 2006;43:311–318. doi: 10.1016/j.ijnurstu.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Sareen J., Cox B.J., Afifi T.O., Clara I., Yu B.N. Perceived need for mental health treatment in a nationally representative Canadian sample. Can. J. Psychiatry. 2005;50:643–651. doi: 10.1177/070674370505001011. [DOI] [PubMed] [Google Scholar]
- Shi L., Lu Z.A., Que J.Y., Huang X.L., Liu L., Ran M.S., Gong Y.M., Yuan K., Yan W., Sun Y.K., Shi J., Bao Y.P., Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su T.P., Huang S.R., Chou P. Prevalence and risk factors of insomnia in community-dwelling Chinese elderly: a Taiwanese urban area survey. Aust. N. Z. J. Psychiatry. 2004;38:706–713. doi: 10.1080/j.1440-1614.2004.01444.x. [DOI] [PubMed] [Google Scholar]
- Sun X., Li Y., Yu C., Li L. [Reliability and validity of depression scales of Chinese version: a systematic review] Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38:110–116. doi: 10.3760/cma.j.issn.0254-6450.2017.01.021. [DOI] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian T., Meng F., Pan W., Zhang S., Cheung T., Ng C.H., Li X.H., Xiang Y.T. Mental health burden of frontline health professionals treating imported patients with COVID-19 in China during the pandemic. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720002093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Laethem M., Beckers D.G., Kompier M.A., Kecklund G., van den Bossche S.N., Geurts S.A. Bidirectional relations between work-related stress, sleep quality and perseverative cognition. J. Psychosom. Res. 2015;79:391–398. doi: 10.1016/j.jpsychores.2015.08.011. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/s0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Liu Y., Wang L. Nurse burnout: personal and environmental factors as predictors. Int. J. Nurs. Pract. 2015;21:78–86. doi: 10.1111/ijn.12216. [DOI] [PubMed] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2014;36:539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Wilder-Smith A., Freedman D. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2021. Coronavirus disease (COVID-19) pandemic. https://www.who.int/zh/emergencies/diseases/novel-coronavirus-2019 (accessed 19 January 2021).
- World Health Organization, 2020. WHO Director-General's opening remarks at the media briefing on COVID-19 - 12 October 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—12-october-2020 (accessed 12 October 2020).
- Wu S., Zhu W., Wang Z., Wang M., Lan Y. Relationship between burnout and occupational stress among nurses in China. J. Adv. Nurs. 2007;59:233–239. doi: 10.1111/j.1365-2648.2007.04301.x. [DOI] [PubMed] [Google Scholar]
- Xie Z., Wang A., Chen B. Nurse burnout and its association with occupational stress in a cross-sectional study in Shanghai. J. Adv. Nurs. 2011;67:1537–1546. doi: 10.1111/j.1365-2648.2010.05576.x. [DOI] [PubMed] [Google Scholar]
- Yang T., Huang H. [An epidemiological study on stress among urban residents in social transition period] Zhonghua Liu Xing Bing Xue Za Zhi. 2003;24:760–764. [PubMed] [Google Scholar]
- Yu W., Singh S., Calhoun S., Zhang H., Zhao X., Yang F. Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden. J. Affect. Disord. 2018;234:89–96. doi: 10.1016/j.jad.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S.X., Liu J., Afshar Jahanshahi A., Nawaser K., Yousefi A., Li J., Sun S. At the height of the storm: healthcare staff's health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav. Immun. 2020;87:144–146. doi: 10.1016/j.bbi.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X.M., Zhou H.E., Zhang W.W., Dou Q.L., Li Y., Wei J., Hu R., Liu J., Cheng A.S.K. Assessment of coronavirus disease 2019 community containment strategies in Shenzhen, China. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.12934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Cao P., Meng J., Qiu J., Hu Q., Cheng L. Exploration of the evaluation and optimization of community epidemic prevention in Wuhan based on a DEA model. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17207633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Wang W., Sun Y., Qian W., Liu Z., Wang R., Qi L., Yang J., Song X., Zhou X., Zeng L., Liu T., Li Z., Zhang X. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: workload should be concerned. J. Affect. Disord. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Zhou Y., Song Y., Ren L., Ng C.H., Xiang Y.T., Tang Y. Tackling the mental health burden of frontline healthcare staff in the COVID-19 pandemic: china's experiences. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720001622. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.