Abstract
Introduction: Corona Virus Disease 2019 (COVID-19) quarantine has been associated with depression, anxiety, and stress symptoms. We hypothesize these symptoms might even be more pronounced in the elderly, who may be particularly sensitive to social isolation. However, certain individuals might be more resilient than others due to their coping mechanisms, including religious coping.
Objectives: We aimed to examine the levels of perceived stress, depressive, and anxiety symptoms in older adults under COVID-19 quarantine in Qatar; and to identify the sociodemographic, psychological, and clinical factors associated with mental health outcomes, with a focus on the role of resilience, and religiosity.
Methods: A cross-sectional study assessing depressive, anxiety, and stress symptoms as well as resilience, and religiosity through a phone survey in adults aged 60 years or more under COVID-19 quarantine in the State of Qatar, in comparison to age and gender-matched controls.
Results: The prevalence of depressive, anxiety, and stress symptoms in elderly subjects under COVID-19 quarantine in Qatar was not significantly different from the prevalence in gender and age-matched controls. In the quarantined group, higher depressive, anxiety, and stress scores were associated with the female gender and with lower resilience scores but were not linked to age, psychiatric history, medical history, duration of quarantine, or religiosity.
Conclusion: The elderly population does not seem to develop significant COVID-19 quarantine-related psychological distress, possibly thanks to high resilience and effective coping strategies developed through the years.
Keywords: elderly, COVID-19, mental health, depression, anxiety, stress, resilience, spirituality
Introduction
As the Corona Virus Disease 2019 (COVID-19) spread across the globe, a fear of potential deleterious mental health consequences arose. These consequences might particularly affect vulnerable populations, including the elderly (Depoux et al., 2020). Many factors might contribute to the COVID-19-related psychological distress: factors directly associated with the disease itself (fear of being contaminated, of contaminating others, of dying or of losing a loved one), as well as factors related to the consequences of isolation, quarantine, and the economic implications of the pandemic (Afshar Jahanshahi et al., 2020, Qiu et al., 2020, Zandifar and Badrfam, 2020, Wang et al., 2020). In the elderly, both factors might be even more pronounced, and the effects of quarantine and isolation in the elderly, in particular, can be serious (Armitage and Nellums, 2020). Indeed, older age has been associated with a greater risk of COVID-19-related complications and death (Jutzeler et al., 2020), which might make the elderly population more vulnerable to the infection and its consequences on their health. Besides, social disconnectedness and perceived isolation in older people have been associated with increased depression and anxiety symptoms (Santini et al., 2020). Some of these consequences might be long-term (Vahia et al., 2020).
Furthermore, social isolation in older adults has also been shown to be associated with increased medical service care, as well as higher risk of hypertension, cardiovascular disease, neurocognitive disorders, and autoimmune diseases (Armitage and Nellums, 2020, Gerst-Emerson and Jayawardhana, 2015). In most Muslim countries, including Qatar, collective prayers in mosques, including Friday prayers, have been suspended to reduce the risk of transmission (Faith, 2020). This can be an additional factor with detrimental effects on the mental health of the elderly, in particular. Indeed, spirituality and religiosity play a central role for the population in general, and the elderly in particular in Gulf Cooperation Council countries, including Qatar (Al-Kandari, 2011).
Despite the potentially more harmful effects of quarantine on the elderly than on younger individuals, very few studies focused on COVID-19 quarantine mental health outcomes in this age category (Armitage and Nellums, 2020).
Different coping strategies are used by people to alleviate the psychological burden of this pandemic, among which spiritual and religious coping (Gilbert et al., 2020, Polizzi et al., 2020).
Religious coping refers to the use of religion-based strategies to deal with stressful events. These strategies can include the use of beliefs, behaviors, as well as individual and collective religious activities. Spiritual coping involves a wider range of strategies, not necessarily related to one particular religion. Religious and spiritual coping have been typically associated with more positive outcomes to stressful events (Ano and Vasconcelles, 2005, Gall and Guirguis-Younger, 2013).
Religious coping might be one of the main coping strategies in the elderly, and more religiosity is associated with fewer depressive symptoms in older than in younger adults (Stearns et al., 2018).
In Qatar, as in most countries in the region, religion plays a central role in well-being. Indeed, higher religiosity is associated with better subjective well-being in young adults in Qatar (Abdel-Khalek, 2013). We believe this link might be even more pronounced in the elderly, but studies in this age group in Qatar are lacking.
To the best of our knowledge, until the time of writing this manuscript, there has been no published study anywhere in the world that specifically addressed the mental health outcomes in the elderly under COVID-19 quarantine and examined their associations with resilience and religiousity.
Our study aims to examine the psychological distress (perceived stress, depressive, and anxiety symptoms) in older adults currently under quarantine in the State of Qatar due to the COVID-19 pandemic; and to examine the sociodemographic, psychological and clinical factors associated with mental health outcomes, with a focus on the role of religiosity and religious coping.
Methods
We carried out a cross-sectional study involving subjects aged 60 years and above who have been in COVID-19 quarantine in Qatar between June and August 2020.
Inclusion criteria for the quarantine group: all participants aged 60 and above under quarantine in Qatar for at least seven days, who consented to the study, and who were Arabic-speaking, regardless of their medical or psychiatric history.
In Qatar, quarantine was required not only for contacts of probable or confirmed COVID-19 cases, but also for international travelers. Between June and August 2020, Qatar has implemented phases to gradually lift the lockdown. During these phases, quarantine requirements were gradually eased. The initial requirement of a 14-day quarantine for all travelers in a hotel or a quarantine center was gradually eased with the possibility of a home quarantine for travelers from low-risk countries, and with the possibility of a hotel quarantine of seven days, followed by a home quarantine depending on the COVID swab results (Reuters June 15 2020). These recommendations took into account the World Health Organization recommendations for resuming international travel suggesting to implement quarantine measures for travelers based on risk assessment and consideration of local circumstances (World Health Organization, 2020).
Based on the alleviation of the quarantine requirements in the State of Qatar, we chose to only include subjects who spent at least seven days in quarantine in a hotel or a quarantine center.
The list of individuals aged 60 and above was obtained from quarantine centers in the State of Qatar. The lead investigator examined the list and selected all eligible participants who met the inclusion/exclusion criteria through preliminary screening. The list was, then, split between four team members who called each of the potential participants on the list.
For each participant, a list of potential controls matched for age and gender was obtained among individuals scheduled for a screening visit at the Ophthalmology Department in Hamad Medical Corporation (HMC) in the same period (June to August 2020).
We excluded all potential controls who were or had been under COVID-19 quarantine. The same inclusion criteria that we defined for participants under quarantine were also applied to controls. In addition, we also chose to exclude any controls who had any uncontrolled psychiatric or chronic medical condition to ensure a better comparability with the quarantine group, since COVID-19 quarantine centers did not have any patients with uncontrolled psychiatric or medical conditions, who were generally transferred to hospitals for a more suitable care.
Simple randomization was, then, used to select one control individual for each quarantined subject from the list of potential controls. If the initially selected control could not be reached, did not meet the inclusion/exclusion criteria, or did not accept to take part in the study, another control was selected by simple randomization, until a control was enrolled. The survey was conducted over the phone. If the participants did not answer the phone call, three other phone call attempts were made during the same week, at different times of the day.
When the potential participant was reached, the interviewer followed a pre-established phone script. Participants were given information about the study, assessed for inclusion/exclusion criteria, then asked about their consent. They were given the option to ask to be called again on a date and at a time of their choosing if they needed more time to think about the decision to take part in the study. Phone calls lasted between 20 and 30 minutes for participants who completed the survey.
Once the subjects gave their consent to participate in the study, they were invited to answer questions about:
-
•
basic sociodemographic data, history of chronic medical illness (recorded as a binary yes/no variable), and psychiatric history (recorded as a binary yes/no variable)
-
•
duration of COVID-19 quarantine.
-
•
depressive, and anxiety symptoms and stress levels using the Depression, Anxiety, and Stress Scale in its 21-item Arabic version (DASS-21), with seven items corresponding to rach of depression, anxiety, and stress symptoms respectively (Ali et al., 2017). Each of these three scores (depression, anxiety, and stress) ranges between 0 and 21, with higher scores being indicative of higher levels of symptoms. To detect symptoms of depression, anxiety, and stress, we used cutoff scores of 4, 3, and 7, respectively (Lovibond and Lovibond, 1995). DASS-21 was previously used in the elderly and was shown to be reliable in this population (Wood et al., 2010). The Arabic version was shown to have a Cronbach's alpha coefficient of 0.88, a coefficient of reproducibility of 0.77, and item-discriminations between 0.14 and 0.43 (Ali et al., 2017).
-
•
resilience using the Arabic version of Connor-Davidson Resilience Scale-10 (CD-RISC-10). The CD-RISC-10 is a well-established instrument consisting of 10 five-point Likert-scale items. Total scores range from 0 to 40, with higher scores indicating higher resilience (Campbell-Sills and Stein, 2007). The scale demonstrated psychometric robustness in the elderly, with high internal consistency (Cronbach's alpha coefficient of 0.85), high test-retest reliability (intra-class correlation coefficient or ICC of 0.87) as well as good convergent and discriminant validity (Cosco et al., 2016, Connor and Davidson, 2003). Resilience is currently conceptualized as a state-trait mixed psychological variable (Ye et al., 2020). However, the CD-RISC was developed in a time where resilience used to be mainly conceptualized as a trait. The CD-RISC is, hence, mostly a validated measure of trait resilience (O'Donohue et al., 2019).
-
•
religiosity and religious involvement using the Arabic version of the Belief into Action Scale (BIAC). The BIAC is a scale which assesses religiosity and religious involvement, focusing on the amount of time, efforts, and financial resources the person spends on religious activities (Koenig et al., 2015). It consists of 10 questions, with the first question is rated one or 10 depending on the response, and the nine other items are each rated on a 1–10 scale. The total score ranges between 10 and 100, with higher scores indicating higher religious involvement.The Arabic BIAC was shown to be a reliable tool to examine religious involvement in Muslim Arabic-speaking populations, with high internal consistency (Cronbach's alpha coefficient of .80), high test-retest reliability (ICC of 0.88 for the total score), as well as adequate convergent validity (medium correlations with the Hoge Intrinsic Religiosity Scale and the Muslim Religiosity Scale: r = 0.52, and r = 0.58 respectively) (Alakhdhair et al., 2016).
Ethical considerations
The study was approved by Hamad Medical Corporation Institutional Review Board, (MRC-05-056). Informed consent was obtained from all participants, and participants were able to withdraw from the study any time during the call, or even after the phone call by contacting the Principal Investigator by e-mail or phone.
Statistical analysis
Statistical analysis was performed using SPSS v26 (IBM Corp., Armonk, NY, USA).
For descriptive statistics of the categorical variables, we calculated absolute and relative frequencies. For descriptive statistics of the different continuous variables used in this study, we calculated the mean and the standard deviation. for normally distributed variables, and the median and the interquartile range (IQR) for non-normally distributed variables.
To compare the prevalence of depressive, anxiety, and stress symptoms between groups, we used McNemar's test. To compare the scores of resilience and religiosity between groups, we used the t-test for paired samples.
To examine associations between the different scores of the scales used in the study (DASS-21, CD-RISC-10 and BIAC), we used Spearman's non-parametric bivariate correlations (since the resilience and religiosity scores did not follow a normal distribution as per the Shapiro-Wilk's test).
To examine the factors associated with depressive, anxiety and stress symptoms, we constructed multiple linear regression models with the DASS-21 depression, anxiety, and stress subscores respectively as dependent variables; and with age, gender, medical history (as a binary variable defined by the presence or absence of a chronic illness), psychiatric history, duration of quarantine, CD-RISC-10, and BIAC scores as dependent variables.
For each of these multiple linear regression models, we determined the unstandardized regression coefficients (B), their 95% confidence intervals (CIs), the partial coefficients (r), as well as the p values. Multiple linear regression assumptions (including linearity, normality of residuals, homoscedasticity, and the absence of multicollinearity) were checked.
Holm-Bonferroni's method was used to correct for multiple comparisons. The defined significance level α was 0.05.
Results
General characteristics of the sample
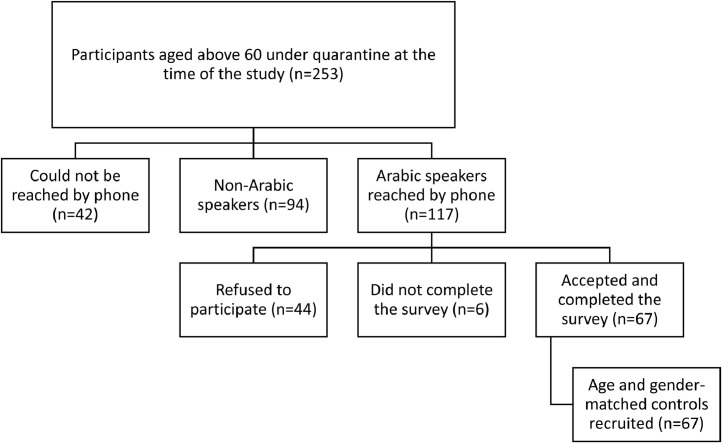
Out of 253 potential participants who were aged more than 60, and were under COVID-19 quarantine in Qatar at the time of the study, 67 participants were recruited after applying the inclusion/exclusion criteria and the informed consent procedure ( Figure 1 ).
Figure 1.
Recruitment process and participants’ flow chart
The mean age of recruited participants was 65.5±5.7 years (minimum: 60, maximum: 90), and 53.7% (n=36) were male. Around two-thirds (62.7%, n=42) were Qatari, the remaining participants being from various other Arab nationalities. Most of the participants were married (86.6%, n=58), and most had a primary or secondary level of education (62.7%, n=42). Only five individuals (7.5%) reported positive psychiatric history: two cases were previously diagnosed with a depressive disorder, and three with an anxiety disorder. The median duration of quarantine (in days) was 14 with an IQR of 6. Most participants (86.7%, n=58) had at least one chronic medical condition. The most common medical conditions among participants were hypertension (62.7%, n=42), diabetes mellitus (56.7%, n=38), and dyslipidemia (32.8%, n=22).
We did not find any significant differences between groups with regards to marital status, medical history, or psychiatric history.
Depressive, anxiety, stress symptoms, resilience, and religiosity in elderly subjects under COVID-19 quarantine and age and gender-matched controls ( Table 1 ).
Table 1.
Depressive, anxiety, stress symptoms, resilience, and religiosity in elderly subjects under COVID-19 quarantine and age and gender-matched controls
| Elderly subjects under quarantine | Matched controls | p | |
| Prevalence of depressive symptoms, n(%) | 11(16.4%) | 6(9.0%) | 0.332a |
| Prevalence of anxiety symptoms, n(%) | 14(20.9%) | 14(20.9%) | 1.000a |
| Prevalence of stress symptoms, n(%) | 7(10.4%) | 10(14.9%) | 0.581a |
| Resilience (CD-RISC-10 score), median (IQR) | 34(9) | 29(5) | <0.001b |
| Religiosity (BIAC score), median (IQR) | 61(15) | 59(18) | 0.487b |
a: Mc Nemar's test; b: Paired-samples t-test
BIAC: Belief into Action Scale; CD-RISC-10: Connor-Davidson Resilience Scale-10; IQR: interquartile range
In elderly subjects under COVID-19 quarantine, the prevalence of depressive symptoms was 16.4% the prevalence of anxiety symptoms was 20.9%, and the prevalence of stress was 10.4%. None of the three symptom categories differed between the elderly individuals under COVID-19 quarantine and their age and gender-matched controls. Resilience was significantly higher in elderly subjects under COVID-19 quarantine (median=34, IQR=9 vs median=29, IQR=5, p<0.001), but religiosity did not differ significantly between groups (median=61, IQR=15 vs median=59, IQR=18, p=0.487).
Correlations between depressive, anxiety, stress symptoms, resilience, and religiosity in elderly subjects under COVID-19 quarantine ( Table 2 )
Table 2.
Non-parametric correlations between depressive, anxiety, stress symptoms, resilience, and religiosity in elderly subjects under COVID-19 quarantine
| DASS-21 Depression | DASS-21 Anxiety | DASS-21 Stress | CD-RISC-10 | ||
| DASS-21 Anxiety | Rho | 0.533 | |||
| p | 0.000 | ||||
| DASS-21 Stress | Rho | 0.779 | 0.689 | ||
| p | 0.000 | 0.000 | |||
| CD-RISC-10 | Rho | -0.381 | -0.236 | -.0375 | |
| p | 0.010 | 0.274 | 0.011 | ||
| BIAC | Rho | 0.155 | 0.093 | 0.095 | 0.021 |
| p | 0.843 | 1.000 | 1.000 | 1.000 |
p values were adjusted for multiple comparisons using Holm-Bonferroni's method.
BIAC: Belief into Action Scale; CD-RISC-10: Connor-Davidson Resilience Scale-10; DASS-21: Depression, Anxiety, and Stress Scale.
We found moderate to moderately strong positive bivariate correlations between DASS-21 depressive, anxiety and stress scores (rho values ranging between 0.533 and 0.779 with Holms-Bonferroni-adjusted p values <0.001). We also found significant weak negative correlations between resilience scores and depressive (rho=-0.381, p=0.010) and stress symptoms (rho=-0.375, p=0.011). However, no association was found between resilience and anxiety scores. Religiosity scores as measured by BIAC were not associated with any of the DASS-21 scores, or with resilience.
Multiple linear regression analysis: factors associated with depressive, anxiety, or stress symptoms in elderly subjects under COVID-19 quarantine ( Table 3 )
Table 3.
Multiple linear regression analysis: factors associated with depressive, anxiety, or stress symptoms in elderly subjects under COVID-19 quarantine.
| Dependent variable: DASS-21 depressive score | ||||
| B | 95%CI for B | Partial r | p | |
| Gender | -1.863 | [-3.211,-0.516] | -0.339 | 0.008 |
| Age | 0.017 | [-0.101,0.135] | 0.037 | 0.777 |
| Medical history (chronic illness) | -0.971 | [-2.791,0.849] | -0.138 | 0.290 |
| Psychiatric history | -0.518 | [-3.152,2.117] | -0.051 | 0.696 |
| Duration of quarantine | 0.026 | [-0.059,0.111] | 0.080 | 0.541 |
| CD-RISC-10 | -0.209 | [-0.336,-0.082] | -0.394 | 0.002 |
| BIAC | 0.030 | [-0.027,0.086] | 0.136 | 0.298 |
| Dependent variable: DASS-21 anxiety score | ||||
| B | 95%CI for B | Partial r | p | |
| Gender | -1.663 | [-2.912,-0.415] | -0.328 | 0.010 |
| Age | 0.023 | [-0.087,0.132] | 0.054 | 0.677 |
| Medical history (chronic illness) | 0.727 | [-0.960,2.413] | 0.112 | 0.392 |
| Psychiatric history | 0.630 | [-1.811,3.072] | 0.067 | 0.607 |
| Duration of quarantine | 0.016 | [-0.062,0.095] | 0.054 | 0.680 |
| CD-RISC-10 | -0.147 | [-0.265,-0.029] | -0.309 | 0.015 |
| BIAC | 0.015 | [-0.037,0.067] | 0.075 | 0.565 |
| Dependent variable: DASS-21 stress score | ||||
| B | 95%CI for B | Partial r | p | |
| Gender | -2.354 | [-4.001,-0.706] | -0.349 | 0.006 |
| Age | 0.040 | [-0.104,0.184] | 0.072 | 0.582 |
| Medical history (chronic illness) | -0.912 | [-3.137,1.312] | -0.106 | 0.415 |
| Psychiatric history | 1.432 | [-1.789,4.652] | 0.115 | 0.377 |
| Duration of quarantine | 0.002 | [-0.102,0.106] | 0.005 | 0.972 |
| CD-RISC-10 | -0.256 | [-0.412,-0.101] | -0.394 | 0.002 |
| BIAC | 0.029 | [-0.040,0.098] | 0.110 | 0.397 |
BIAC: Belief into Action Scale; CD-RISC-10: Connor-Davidson Resilience Scale-10; CI: Confidence interval; DASS-21: Depression, Anxiety, and Stress Scale.
In multiple linear regression analysis, higher depressive scores were significantly associated with the female gender (B=-1.863[-3.211,-0.516], r=-0.339, p=0.008), and with lower resilience scores B=-0.209[-0.336,-0.082], r=-0.394, p=0.002), but not with age, psychiatric history, medical history, duration of quarantine, or religiosity. The adjusted R square was 0.162.
Similarly, higher anxiety scores were significantly associated with the female gender (B=-1.663[-2.912,-0.415], r=-0.328, p=0.010), and with lower resilience scores (B=-0.147[-0.265,-0.029], r=-0.309, p=0.015), but not with age, psychiatric history, medical history, duration of quarantine, or religiosity. The adjusted R square was 0.109.
Likewise, higher stress scores were significantly associated with the female gender (B=-2.354[-4.001,-0.706], r=-0.349, p=0.006), and with lower resilience scores (B=-0.256[-0.412,-0.101], r=-0.394, p=0.002), but not with age, psychiatric history, medical history, duration of quarantine, or religiosity. The adjusted R square was 0.186.
Discussion
In this cross-sectional study, we found that the prevalence of depressive, anxiety, and stress symptoms in elderly subjects under COVID-19 quarantine in Qatar did not differ from the prevalence in gender and age-matched controls. In the quarantined group, higher depressive, anxiety and stress scores were associated with the female gender as well as with lower resilience scores, but were not linked to age, psychiatric history, medical history, duration of quarantine, or religiosity.
Depressive, anxiety, stress symptoms in elderly subjects under COVID-19 quarantine
The prevalence of depressive, anxiety and stress symptoms in the elderly subjects under COVID-19 quarantine was not particularly high (16.4% for depression, 20.9% for anxiety, and 10.4% for stress), and did not significantly differ from the prevalence in age and gender-matched controls. Most participants showed no significant signs of psychological distress. This finding echoes the results of a similar study conducted during the confinement phase of the COVID-19 in Northern Spain which found similarly low rates of depressive, anxiety and stress symptoms in individuals aged 60 or more (Picaza Gorrochategi et al., 2020). Likewise, another Spanish study found that, during the COVID-19 outbreak, individuals aged 60 or more were not more likely to experience anxiety symptoms, and even exhibited fewer depressive and acute stress symptoms than their younger counterparts (Garcia-Fernandez et al., 2020). Moreover, loneliness (as a consequence of quarantine) was not found to be associated with any symptoms of psychological distress (Garcia-Fernandez et al., 2020).
Similarly, older age was found to be associated with fewer depressive symptoms among quarantined Chinese individuals during the COVID-19 outbreak (Peng et al., 2020). A nationwide multicenter cross-sectional Chinese study examining 19,372 individuals under interpersonal isolation found that the age group 35-49 years had more pronounced depressive and anxiety symptoms than other age groups (in particular individuals aged 65+) (Wang et al., 2020). Many other studies which examined psychological distress in the general population (across different age groups) during the COVID-19 outbreak found older age to be a protective factor against COVID-19-related psychological distress in Spain (Garcia-Portilla et al., 2020, Gonzalez-Sanguino et al., 2020), Canada (Findlay et al., 2020, Nwachukwu et al., 2020), and Egypt (El-Zoghby et al., 2020), or at least did not find older age to be associated with poorer mental health outcomes (Mazza et al., 2020, Pearman et al., 2020).
Taken together, these findings are unexpected, since many potential factors would, at least in theory, make the elderly more prone to psychological distress under quarantine. These factors include higher COVID-19 mortality rates, potentially more pronounced effects of social isolation, as well as brain ageing (Jutzeler et al., 2020, Vahia et al., 2020). One possible explanation for the relatively low psychological distress in the elderly might include the fact that the professional impact of the pandemic mainly affects middle-aged adults, and relatively spares older subjects who are often retired (Wang et al., 2020). Another plausible explanation is the existence of protective factors, among which resilience, proactive and religious coping may play an important role (Pearman et al., 2020).
Factors associated with depressive, anxiety, and stress symptoms in elderly subjects under COVID-19 quarantine
In our study, we found that the female gender and lower resilience were the main factors associated with depressive, anxiety, and stress symptoms in elderly individuals under COVID-19 quarantine. The female gender is a well-established risk factor for lifetime depressive and anxiety disorders, even though the gender differences seem to be less pronounced in late life (Kiely et al., 2019). Most studies assessing the COVID-19-related psychological distress in the general population reported the female gender to be a risk factor (Gonzalez-Sanguino et al., 2020, Findlay et al., 2020, El-Zoghby et al., 2020, Mazza et al., 2020). Nonetheless, findings in the elderly were less consistent, with certain studies reporting an association between the female gender and poorer COVID-19-related mental health (Garcia-Portilla et al., 2020), and others finding no such association (Picaza Gorrochategi et al., 2020, Garcia-Fernandez et al., 2020).
In the present study, higher resilience scores were associated with lower depressive, anxiety, and stress scores. This finding replicates previous studies highlighting the role of psychological resilience as a protective factor from late-life depression and anxiety (Laird et al., 2019, Zhong et al., 2016). While psychological resilience was initially conceptualized as a stable trait, it is now widely accepted that resilience is more likely to be a dynamic capacity which is shaped and affected by internal and external factors (Laird et al., 2019). It is possible that, as they advance in age, older individuals gain cumulative life experience, which helps them develop and refine efficient coping strategies, thus bolstering their psychological resilience (Pearman et al., 2020). Coping strategies that might be mostly used by the elderly in the context of the COVID-19 pandemic might include proactive coping (Pearman et al., 2020), as well as spiritual and religious coping (Koenig, 2020). Proactive coping was previously reported to be associated with less pronounced COVID-19-related stress in older individuals (Pearman et al., 2020). Positive religious coping, intrinsic religiosity and trust in God were also found to be associated with lower COVID-19-related stress levels (Pirutinsky et al., 2020). In Qatar, as in Muslim and Arab societies in the region, religion plays a central role (Al-Kandari, 2011), especially in the elderly. Hence, we expected religiosity to be associated with better mental health outcomes, but this was not the case in our sample. It is possible that this is simply due to a type 2 error. Another possible explanation is that BIAC mostly emphasizes the religious practices and community religious activities, more than the individual spiritual aspects of religion (Koenig et al., 2015). Community religious activities mainly were suspended because of the pandemic, and people were not able to use these activities as potential coping mechanisms during the quarantine period, and more generally during the COVID-19 outbreak (Faith, 2020). This might have deprived many elderly individuals from potential coping mechanisms they were used to.
The finding that depressive, anxiety, and stress symptoms were higher in female participants and those with lower resilience can help identify at-risk groups for quarantine-associated psychological distress. These at-risk groups can benefit from brief psychoeducational and psychosocial interventions, which can be conducted over the phone or over digital applications (Brooks et al., 2020).
Strengths and limitations
This is one of very few studies about mental health outcomes in the elderly population under COVID-19 quarantine. To the best of our knowledge, this is also the first study trying to examine religiosity as a potential protective factor from stress, depression, and anxiety in quarantined elderly individuals. Contrarily to most previous studies which did not have any control group, we recruited age and gender-matched controls to help disentangle the effects of quarantine from the general effects of the pandemic. Other strengths include the use of well-validated scales, as well as the recruitment of all consenting elderly individuals under COVID-19 quarantine in Qatar who met the inclusion/exclusion criteria during the time of the study. However, certain limitations need to be acknowledged. Indeed, even though we tried to have a recruitment process as exhaustive as possible, the sample size was relatively small. This is probably due to the sociodemographic of the country: only 1.3% of the population was aged 65 years or more, as per June 2020 statistics (Planning and Statistics Authority - Qatar 2020). Moreover, we did not include participants who were not Arabic speakers. This was motivated by the fact that most non-Arabic speakers spoke languages that none of the investigators spoke. In addition,the scales used in the present study were not always validated in these languages. The addition of a younger adult group under quarantine could have helped highlight the possible specificities of the elderly psychological reaction to quarantine. In addition, phone calls were conducted by different members of the team, and the inter-rater reliability was not formally assessed. However, all interviewers followed the same phone script, and the scales consisted of self-questionnaires administered over the phone, which probably limited the risk of measurement bias.
Last, we cannot rule out the possibility of selection and response biases having affected the results of the study. Indeed, it is possible that stress, depressive or anxiety symptoms might have affected the decision to participate in the study. Moreover, it is possible that social-desirability bias might have affected certain patients’ answers (Johnson et al., 2000).
Conclusions
Unexpectedly, it does not appear that the elderly population develops significant psychological distress associated with COVID-19 quarantine, and more generally with the COVID-19 pandemic. High resilience and effective coping strategies developed through the years likely help the elderly get through the mental burden of the pandemic with relatively few symptoms. Even though we did not find that religiosity was associated with better mental health outcomes in elderly subjects under quarantine, we believe that the suspension of most community religious activities during the pandemic might have deprived many individuals from this potentially effective coping mechanism.
Funding
None
CRediT authorship contribution statement
Sami Ouanes: Conceptualization, Methodology, Data curtion, Formal analysis, Writing – original draft. Rajeev Kumar: Conceptualization, Methodology, Supervision, Writing – review & editing. Esraa Saleh Idriss Doleh: Data curtion, Writing – review & editing. Malek Smida: Data curtion, Writing – review & editing. Abdulaziz Al-Kaabi: Data curtion, Writing – review & editing. Ahmad Medawi Al-Shahrani: Data curtion, Writing – review & editing. Ghassan Ahmed Mohamedsalih: Data curtion, Writing – review & editing. Nagi Eltagi Ahmed: Data curtion, Writing – review & editing. Ahmed Assar: Data curtion, Writing – review & editing. Mohamed Adil Shah Khoodoruth: Conceptualization, Writing – review & editing. Mohammed AbuKhattab: Conceptualization, Writing – review & editing. Muna Al Maslamani: Conceptualization, Writing – review & editing. Majid Ali AlAbdulla: Conceptualization, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors report no conflicts with any product mentioned or concept discussed in this article.
Acknowledgements
None.
References
- Depoux A, Martin S, Karafillakis E, Bsd RP, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. 2020 doi: 10.1093/jtm/taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afshar Jahanshahi A, Mokhtari Dinani M, Nazarian Madavani A, Li J, Zhang SX. The distress of Iranian adults during the Covid-19 pandemic - More distressed than the Chinese and with different predictors. medRxiv. 2020:2020.04.03.20052571. [DOI] [PMC free article] [PubMed]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian journal of psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jutzeler CR, Bourguignon L, Weis CV, Tong B, Wong C, Rieck B, et al. Comorbidities, clinical signs and symptoms, laboratory findings, imaging features, treatment strategies, and outcomes in adult and pediatric patients with COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;37 doi: 10.1016/j.tmaid.2020.101825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–e70. doi: 10.1016/S2468-2667(19)30230-0. [DOI] [PubMed] [Google Scholar]
- Vahia IV, Blazer DG, Smith GS, Karp JF, Steffens DC, Forester BP, et al. COVID-19, Mental Health and Aging: A Need for New Knowledge to Bridge Science and Service. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2020 doi: 10.1016/j.jagp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. American journal of public health. 2015;105(5):1013–1019. doi: 10.2105/AJPH.2014.302427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith Alyanak O. Politics and the COVID-19 Pandemic: The Turkish Response. Medical Anthropology. 2020:1–2. doi: 10.1080/01459740.2020.1745482. [DOI] [PubMed] [Google Scholar]
- Al-Kandari YY. Religiosity, social support, and health among the elderly in Kuwait. Journal of Muslim Mental Health. 2011;6(1) [Google Scholar]
- Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boëlle P-Y, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. The Lancet. 2020;395(10227):871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polizzi C, Lynn S, Perry A. Stress and Coping in the Time of COVID-19: Pathways to Resilience and Recovery. Clinical Neuropsychiatry. 2020;17(2):59–62. doi: 10.36131/CN20200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. Journal of clinical psychology. 2005;61(4):461–480. doi: 10.1002/jclp.20049. [DOI] [PubMed] [Google Scholar]
- Gall TL, Guirguis-Younger M. APA handbook of psychology, religion, and spirituality (Vol 1): Context, theory, and research. APA handbooks in psychology®. American Psychological Association; Washington, DC, US: 2013. Religious and spiritual coping: Current theory and research; pp. 349–364. [Google Scholar]
- Stearns M, Nadorff DK, Lantz ED, McKay IT. Religiosity and depressive symptoms in older adults compared to younger adults: Moderation by age. Journal of affective disorders. 2018;238:522–525. doi: 10.1016/j.jad.2018.05.076. [DOI] [PubMed] [Google Scholar]
- Abdel-Khalek AM. The relationships between subjective well-being, health, and religiosity among young adults from Qatar. Mental Health, Religion & Culture. 2013;16(3):306–318. [Google Scholar]
- Reuters . June 15 2020. Qatar to lift lockdown in four phases from.https://www.reuters.com/article/us-health-coronavirus-qatar/qatar-to-lift-lockdown-in-four-phases-from-june-15-idUSKBN23F2KD [Available from: [Google Scholar]
- World Health Organization . 2020. Public health considerations while resuming international travel.https://www.who.int/news-room/articles-detail/public-health-considerations-while-resuming-international-travel [Available from: [Google Scholar]
- Ali AM, Ahmed A, Sharaf A, Kawakami N, Abdeldayem SM, Green J. The Arabic Version of The Depression Anxiety Stress Scale-21: Cumulative scaling and discriminant-validation testing. Asian journal of psychiatry. 2017;30:56–58. doi: 10.1016/j.ajp.2017.07.018. [DOI] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Wood BM, Nicholas MK, Blyth F, Asghari A, Gibson S. The utility of the short version of the Depression Anxiety Stress Scales (DASS-21) in elderly patients with persistent pain: does age make a difference? Pain Med. 2010;11(12):1780–1790. doi: 10.1111/j.1526-4637.2010.01005.x. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Cosco TD, Kaushal A, Richards M, Kuh D, Stafford M. Resilience measurement in later life: a systematic review and psychometric analysis. Health Qual Life Outcomes. 2016;14:16. doi: 10.1186/s12955-016-0418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depression and anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Ye ZJ, Zhang Z, Zhang XY, Tang Y, Chen P, Liang MZ, et al. State or trait? Measuring resilience by generalisability theory in breast cancer. Eur J Oncol Nurs. 2020;46 doi: 10.1016/j.ejon.2020.101727. [DOI] [PubMed] [Google Scholar]
- O'Donohue JS, Mesagno C, O'Brien B. How can stress resilience be monitored? A systematic review of measurement in humans. Current Psychology. 2019 [Google Scholar]
- Koenig HG, Wang Z, Al Zaben F, Adi A. Belief into Action Scale: A comprehensive and sensitive measure of religious involvement. Religions. 2015;6(3):1006–1016. [Google Scholar]
- Alakhdhair S, Sheets V, Geib R, Alkhuwaildi A, Koenig HG. Psychometric properties of the Arabic version of the Belief into Action Scale. Mental Health, Religion & Culture. 2016;19(8):846–857. [Google Scholar]
- Picaza Gorrochategi M, Eiguren Munitis A, Dosil Santamaria M, Stress Ozamiz Etxebarria N. Anxiety, and Depression in People Aged Over 60 in the COVID-19 Outbreak in a Sample Collected in Northern Spain. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2020;28(9):993–998. doi: 10.1016/j.jagp.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Fernandez L, Romero-Ferreiro V, Lopez-Roldan PD, Padilla S, Rodriguez-Jimenez R. Mental Health in Elderly Spanish People in Times of COVID-19 Outbreak. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2020;28(10):1040–1045. doi: 10.1016/j.jagp.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng M, Mo B, Liu Y, Xu M, Song X, Liu L, et al. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. Journal of affective disorders. 2020;275:119–124. doi: 10.1016/j.jad.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, et al. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: A nationwide multicenter cross-sectional study. European psychiatry : the journal of the Association of European Psychiatrists. 2020;63(1):e77. doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Portilla P, de la Fuente Tomas L, Bobes-Bascaran T, Jimenez Trevino L, Zurron Madera P, Suarez Alvarez M, et al. Are older adults also at higher psychological risk from COVID-19? Aging & mental health. 2020:1–8. doi: 10.1080/13607863.2020.1805723. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Lopez-Gomez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, behavior, and immunity. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findlay LC, Arim R, Kohen D. Understanding the Perceived Mental Health of Canadians During the COVID-19 Pandemic. Health Rep. 2020;31(4):22–27. doi: 10.25318/82-003-x202000400003-eng. [DOI] [PubMed] [Google Scholar]
- Nwachukwu I, Nkire N, Shalaby R, Hrabok M, Vuong W, Gusnowski A, et al. COVID-19 Pandemic: Age-Related Differences in Measures of Stress, Anxiety and Depression in Canada. Int J Environ Res Public Health. 2020;17(17) doi: 10.3390/ijerph17176366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Zoghby SM, Soltan EM, Salama HM. Impact of the COVID-19 Pandemic on Mental Health and Social Support among Adult Egyptians. J Community Health. 2020;45(4):689–695. doi: 10.1007/s10900-020-00853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, et al. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int J Environ Res Public Health. 2020;17(9) doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearman A, Hughes ML, Smith EL, Neupert SD. Age Differences in Risk and Resilience Factors in COVID-19-Related Stress. The journals of gerontology Series B, Psychological sciences and social sciences. 2020 doi: 10.1093/geronb/gbaa120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiely KM, Brady B, Byles J. Gender, mental health and ageing. Maturitas. 2019;129:76–84. doi: 10.1016/j.maturitas.2019.09.004. [DOI] [PubMed] [Google Scholar]
- Laird KT, Lavretsky H, Paholpak P, Vlasova RM, Roman M, St Cyr N, et al. Clinical correlates of resilience factors in geriatric depression. International psychogeriatrics /IPA. 2019;31(2):193–202. doi: 10.1017/S1041610217002873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong X, Wu D, Nie X, Xia J, Li M, Lei F, et al. Parenting style, resilience, and mental health of community-dwelling elderly adults in China. BMC Geriatr. 2016;16:135. doi: 10.1186/s12877-016-0308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG. Ways of Protecting Religious Older Adults from the Consequences of COVID-19. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2020;28(7):776–779. doi: 10.1016/j.jagp.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirutinsky S, Cherniak AD, Rosmarin DH. COVID-19, Mental Health, and Religious Coping Among American Orthodox Jews. J Relig Health. 2020;59(5):2288–2301. doi: 10.1007/s10943-020-01070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planning and Statistics Authority - Qatar. Quarterly Bulletin -Population Statistics -Second Quarter- 2020, accessed on 09/26/2020. [Available from: https://www.psa.gov.qa/en/statistics/Statistical%20Releases/Population/Population/2020/Population_Social_Statistics_Q2.pdf.
- Johnson LC, Beaton R, Murphy S, Pike K. Sampling Bias and Other Methodological Threats to the Validity of Health Survey Research. International Journal of Stress Management. 2000;7(4):247–267. [Google Scholar]