Abstract
Waste management has come to the fore in the whole world with the increasing impact of the Covid-19 pandemic along with concerns about human health, environmental threats, and socio-economic factors, etc. Medical waste is one of the waste types that need special management processes including particularly collection, storage, separation, and disposal. Healthcare activities create a great amount of medical waste deriving from the hospitals. This study aims to determine the hospital that carries out medical waste management in the most effective way in Erzurum, Turkey. To handle intense uncertainty in the evaluation process, the case is analyzed by Intuitionistic Fuzzy Multi-Criteria Decision-Making (IFMCDM) methods. The present study contributes to the literature by focusing on a real case problem under IF environment in a Group Decision-Making (GDM) framework. Additionally, based on the literature review and expert judgments, the evaluation criteria relevant to the case are defined in this paper. To this end, a four-phased integrated methodology that involves Intuitionistic Fuzzy Weighted Averaging (IFWA), IF Analytical Hierarchy Process (IFAHP), IF Technique for Order Preference by Similarity to Ideal Solution (IFTOPSIS) and One-Dimensional Sensitivity Analysis, is conducted. Firstly, IFWA is aimed to express the significance levels of decision makers (DMs) based on their knowledge, qualifications and experiences. Secondly, IFAHP is used to calculate the importance weights of the decision criteria and IFTOPSIS is preferred to rank the available hospitals. Then, sensitivity analysis is employed to display robustness. According to the results, the most important criteria are Qualified personnel, Health institution infrastructure, and Control of waste, respectively and the most efficient hospital is determined.
Keywords: Medical waste management, IFMCDM, IFAHP, IFTOPSIS, GDM
1. Introduction
In this century, due to the increasing human population and the development of technology, the production and consumption diversity has increased and this situation has caused environmental pollution that damages the ecological balance such as unplanned urbanization, excessive consumption, and misuse of natural resources. The rapid consumption and pollution of limited natural resources have become a threat not only to humans but also to all living things. Wastes are at the center of environmental pollution, which accelerates and develops threats. Also, considering the socio-economic and environmental sustainability and obligation to leave a livable habitat for future generations, waste management planning and implementation issues stand out for the whole world. In this context, waste management has emerged as an essential problem in the ongoing Covid-19 pandemic process due to the provision of the necessary living conditions for the continuation of life, the ability of hospitals to meet the health requirements, as well as the effective management of supply chains in all sectors.
The term waste is defined as materials that are destroyed, considered to be destroyed, or necessary to be destroyed under national/international laws and provisions [1]. Wastes are durable and nondurable substances of different types and sizes, which are released into nature by living things and whose amount of pollution can vary according to their type. The increase in waste causes concerns about the environment, humans and other living things in the world. The collection, minimization and recycling of wastes need to be managed in advance where they are produced [2,3].
In the relevant literature and practice, special importance has been given to the classification of medical wastes due to their collection, transportation and disposal activities. Considering the adverse situations that may occur as a conclusion of the misclassification of medical wastes [[4], [5], [6]], they are sorted in a manner with national/international standard codes. Because medical wastes need to be sorted carefully and treated separately from other wastes owing to the existence of harmful contents and special regulations.
In Turkey, medical waste safety rules related to the implementation and management were identified in the “Medical Waste Control Regulation” prepared by the Ministry of Environment and Forestry. Responsibilities for the disposal of medical wastes belong to metropolitan municipalities in metropolitan cities, municipalities in non-metropolitan areas, or persons and organizations which are authorized. The first regulations on medical waste in Turkey have started in 1993 and this regulation was updated in 2005 concerning the EU directives [7]. Later, other institutions and organizations for waste management were opened in Turkey. According to the data of 2018, there are 3 incineration plants in Turkey located in Istanbul, Ankara and Kocaeli. There are 60 sterilization centers licensed and temporarily certified in our country. Considering the amount of waste by years in Turkey (2012–2018) consisting 9% of medical waste is seen to be caused by the Erzurum province and there is an institution with a temporary activity certificate carrying out medical waste disposal works [8]. In fact, a great number of medical waste occurs in hospitals. Based on this situation, medical waste management issue in hospitals needs to be examined in Erzurum. Incorrect planning and execution of the medical waste management process can lead to major health complications and environmental problems in the future.
The medical waste management process requires the evaluation of many different qualitative and quantitative criteria consisting of social, economic, organizational and strategic factors together. Particularly, the opinions of those with a say in the determination and application of the medical waste management procedure, as well as the expertise of decision makers (DMs), may differ and be ambiguous. Intuitionistic Fuzzy Multi-Criteria Decision-Making (IFMCDM) techniques that take into account the knowledge, expertise and hesitation levels of the DMs have been preferred to solve such problems. Hence, the motivation for performing this research is to handle uncertainties on the medical waste management problem under the IF environment whose existence is proven in the literature.
In this context, this study aims to determine the hospital in Erzurum that carries out medical waste management the most effectively and efficiently by IFMCDM methods. Additively, Group Decision Making (GDM) is used to solve the problem with Intuitionistic Fuzzy Weighted Averaging (IFWA) to minimize the bias and identify the significance levels of DMs. In the present study, integration of Analytical Hierarchy Process (AHP) and Technique for Order Preference by Similarity to Ideal Solution (TOPSIS) methods under IF environment were proposed in the application of the case. This study attempts to be the first in relevant literature by conducting a case study of medical waste management in Erzurum province through an IFMCDM approach. Therefore evaluation criteria are developed specifically for the case in question by literature review and expert opinions. This integrated approach not only takes advantage of IF sets but also utilizes a GDM framework step by step.
The remaining of the study are as follows. In the second part, the background of the medical waste management issue is explained. Followingly, a literature review including medical waste management and IFAHP-IFTOPSIS studies are summarized. In the fourth part, methodology and summary information about IFAHP and IFTOPSIS methods are presented. Then, in the application part, a case study consisting of six hospitals is executed for the proposed method. In the last part, suggestions are made regarding the results and future research topics.
2. Background of the medical waste management
Wastes have been categorized in many types in the literature according to their environment, hazard status, source, components, and physical/chemical properties. Also, medical wastes are classified as pathological, pharmaceuticals, infectious wastes, etc. [9]. There are also comprehensive classification studies [[6], [10], [11], [12], [13]] in the literature.
Medical wastes can be defined as substances that come from health institutions, laboratories, and, clinics and result from the physiological and biological needs of the human body [[1], [14]]. Medical wastes can be used under different names such as medical waste [15]; Kargar et al., 2020), healthcare waste [16,17], and hospital waste [18,19]. In addition, medical wastes can be classified as hazardous or non-hazardous concerning the harmful materials they contain and the rising of hazardous waste indicates major efforts to safely collect, transport, and dispose of them [20]. The amount and composition of medical wastes may vary depending on the activity level of the generated establishment, the type of facility, size, location, policies, waste management method, technology, waste regulations, infrastructure, and also the development levels of the countries [[10], [21], [22], [23]].
Medical wastes mostly affect doctors, nurses, caregivers, other hospital staff, patient visitors, cleaning staff, municipal staff working in waste transportation, waste disposal staff, and separators that separate waste from garbage. In addition, medical wastes can have unfavorable impacts on the environment, soil, water, air, and ecosystem. Due to their characteristics, medical wastes should be treated separately from domestic solid wastes, temporarily stored in separate locations, transported, collected and disposed of with special processes. However, it is seen that such management procedures, are not performed due to cost increases [24]. Also, legal legislation, disposal, and applicability of medical waste management issue is attempted to be explained in detail for practitioners in different countries [[18], [25], [26], [27], [28], [29]].
Hospitals have great responsibilities in medical waste management. Effective and efficient medical waste management cannot be achieved only by a very good working or well-equipped hospital; but by the continuous application of well-regulated medical waste management activities and internal service principles [6]. The purpose of appropriate medical waste management is to preserve human health and the environment, and reduce the amount of waste by recycling and separating them correctly according to their characteristics and regulations [16,30]. Medical wastes may rise risks and cause damage and danger in organizations that do not have appropriate waste management. The reason why this subject is given so much importance in the literature is that the entire population and future generations may be negatively affected as a result of incorrect waste management.
Collection, transportation time, road length, transportation capacity and planning of vehicles, and disposal types play an important role in effective medical waste management. In addition, the data obtained during this whole process are important health data. Therefore, these big data should be recorded, stored and protected against unrelated persons and organizations. This safety measure also plays an important role in an effective medical waste management process. As a matter of fact, it has been stated in studies that harmful factors that can affect information security in health services [31] and the damages that occur if this big data is not recorded correctly or lost can be very large [32,33].
In this regard, durable websites [34], blockchain technologies [35,36], reliable software [37] and software technologies [38] are some of the tools that can be used.
When waste disposal systems in the world are examined, it can be said that there are various applications. For example, in the USA, medical wastes are classified very well, separated from their source and minimized. Some wastes are stored regularly, while some are incinerated [39]. Various techniques, microwave in Germany and the Philippines, thermal treatment in France, chemical disinfection in Ireland, autoclave in Australia, pyrolysis in Japan, incineration in Greece, Netherlands, Malaysia, and Singapore are used (https://www.epd.gov.hk/, 2020). Also, incineration techniques are commonly used in Vietnam, Thailand and Korea [40,41]. In China, hospitals do not have the right to destroy their own medical waste according to legal regulations and private companies do this work [42]. When the data are analyzed in Turkey, burial and incineration methods are mostly used [43]. These methods that are used in waste disposal have advantages and disadvantages in themselves. Unsuitable management of disposal activities may lead to diseases such as cancer, cholera, hepatitis, and infections, etc. along with environmental problems [44].
Considering all these issues, it is remarkable that medical waste management processes require to be paid more attention and regulations should be controlled continuously and properly for minimizing the harmful effects of these activities. Especially, it is important to consider this process in the hospitals where medical wastes are produced mostly and which are the first places that come to mind.
3. Literature review
The literature review has been examined under two headings such as studies on medical waste management and IFAHP-IFTOPSIS methods.
3.1. Studies on medical waste management
Medical waste management is one of the popular topics recently being studied in the world. Considering the related literature, many studies have been printed on this area. The topic has been examined from various perspectives in many countries with different methods. Therefore, in this section, a comprehensive literature review is presented, including a continental grouping of relevant references.
When the studies on waste management in America were examined, [39], researched the functionality of applied medical waste management in USA [45]. studied the environmental damage caused by medical wastes [2]; studied on the amount and composition of hospital waste. In Brazil, [[46], [47], [48], [49], [50]], evaluated the improvements in medical waste management. In these studies, statistical methods were generally used.
In Europe, various papers were performed in Portugal [26]; England [51]; Greece [[12], [13], [52]]; Croatia [1]; Germany [53]; Hungary [54]; Spain [[28], [55]]; Sweden [54]; Poland [[29], [56]]. According to these studies it was observed that waste management processes and waste disposal methods were mainly focused and statistical methods were generally conducted. In addition, the AHP method which is one of the MCDM approaches was used by Ref. [13].
Some studies on medical waste management in Far and Middle East are summarized as follows: In Iran [[57], [58], [59], [60], [61], [62]]; Kargar et al., 2020); Iraq [63]; Jordan [[4], [64], [65], [66], [67]]; India [[68], [69], [70], [71], [72]]; Indonesia [73]; Korea [40,74]; China [[42], [75], [76]]; Taiwan [10,77,78]; Morocco [27]; Pakistan [79,80]; Malaysia [44]; Palestine [81]; Myanmar [18]; Singapore [82], it was seen that the current status of national and international standards, legal legislation on waste management and especially the education level of those concerned in waste management were studied. Regarding these studies, disposal issues, deficiencies in practice, insufficiency of education, and hospital situations have been examined. AHP [61], fuzzy goal programming (Kargar et al., 2020), route scheduling [65], statistical methods and, case studies were used for these purposes.
When the papers in Africa were considered; in Tanzania [83]; Nigeria [[5], [84], [85], [86], [87], [88], [89]]; Republic of South Africa [[14], [90], [91], [92], [93], [94]]; Botswana (Emmunuel, 2007 [95]; Bangladesh [[96], [97], [98], [99], [100]]; Kenya [[101], [102], [103]]; Ghana [[104], [105], [106], [107]]; Ethiopia [[108], [109], [110]] usually the determination of waste amounts and improvement of the waste management process were searched. In these studies, statistical methods were mostly used, and serious problems in waste transportation, storage and especially separation points were investigated [111].
The first legal regulations on medical waste in Turkey started with the “Regulation on the Control of Medical Wastes” (Official Gazette, 1993). In the following years, studies were carried out in the literature with a wide perspective that can be expressed as follows. Some studies in the field of waste disposal [[112], [113], [114]], determined that there are deficiencies at the point of waste disposal. In addition, referencing the studies on waste management, waste control, waste collection, and transportation process [[30], [69], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124]], it can be interpreted as there are processes to be improved, but the medical waste management process is better than in Africa and other Asian countries. In related studies, statistical methods and the AHP method by Ref. [121] were carried out. On the other hand, for selecting medical waste disposal methods in Turkey [25] used the Fuzzy MCDM approach based on fuzzy measure and integral, [125], employed Analytical Network Process (ANP) and ELECTRE II techniques, [126]; utilized mixed integer linear programming.
Moreover, there are different studies objected to evaluating other issues of medical waste management such as investigating the dangers and environmental problems that may be caused by medical waste [[127], [128], [129]], explaining the importance and necessity of waste classification [[6], [24]], examining all aspects of waste management, and comparing medical waste disposal methods [[130], [131], [132]], examining medical waste management during the pandemic period [[75], [76], [133], [134], [135], [136], [137], [138], [139]].
According to the papers introduced in the literature review, some of the statistical and MCDM methods (mostly AHP), and also theoretical issues of medical waste management are utilized. To the best of the author's knowledge, it is remarkable that IFMCDM methods are never used in this area. The subject of medical waste management is frequently used in developing countries. Conducting such a study for Turkey, one of the developing countries seems to be necessary for the evaluation of health care institutions.
3.2. Studies on IFAHP – IFTOPSIS methods
One of the points that make medical waste studies different in the literature is the differentiation of the used methods. Although there are some studies using software packages (ITHINK) [81], and statistical methods [92], mathematical models [140] few studies consider MCDM methods [[13], [61], [121], [141]]. Therefore, there is no research in which this issue is evaluated with an intuitive point of view and used the integrated IFAHP-IFTOPSIS method. The studies in the field of IFTOPSIS-IFAHP are presented in Table 1 .
Table 1.
Literature review of IFAHP-IFTOPSIS.
| Study | Subject | Illustrative or Case Study | GDM | IF operator |
|---|---|---|---|---|
| [142] | Production technology evaluation | Illustrative | + | IFWA |
| [143] | Human capital indicator evaluation | Illustrative | – | – |
| [144] | Web site evaluation | Case study | + | IFWA |
| [145] | Product development partner selection | Case study | + | IFWA |
| [146] | Production strategy selection | Case study | – | – |
| [147] | Supplier selection | Illustrative | – | – |
| [148] | Neuroimaging techniques selection | Case study | + | IFWA |
| [149] | Vehicle corridor selection | – | IFWA | |
| [150] | Terminal location selection | Case study | + | IFWA |
| [151] | Supply chain sustainability assessment | Case study | – | – |
| [152] | Green supplier selection | Case study | – | – |
| [153] | Risk assessment | Case study | – | – |
As can be seen in Table 1, there are few studies in the literature in which IFAHP and IFTOPSIS techniques are used together. Also, there is no previous paper examining medical waste management issues with the integrated IFAHP-IFTOPSIS method within the GDM framework.
The scientific contributions of this article can be summarized as follows: In the literature, IFAHP and IFTOPSIS techniques are never used in medical waste management studies, in addition, no studies are using an IFMCDM approach on this issue. In relation to other methods such as statistical, mathematical, qualitative, etc. this paper proposes an integrated IFMCDM method that uses the expert knowledge and deals with hesitancies of DMs and uncertainties deriving from the decision process. It considers many complex evaluation criteria and alternatives together by taking the advantage of the combination of IFAHP-IFTOPSIS. Therefore, the present study is the first attempt to contribute to the literature by using IFMCDM methods in medical waste management dealing with hospital performances. Additively, the real case of Erzurum province in Turkey is considered for the first time in this study.
4. Methodology
The Fuzzy Sets Theory [154] is used to solve complex decision problems involving vagueness, fuzzy judgments of DMs and inadequate knowledge about the decision process. In relavant literature, it is noticed that fuzzy sets can be fallen behind in some cases such as collecting subjective opinions of humans and facing ambiguity and difficulty to calculate the superiority of the alternative over the others [155]. In this context, Intuitionistic Fuzzy Sets (IFS) can handle these problems in a beneficial and effective way. IFS are generally utilized to identify the judgments of DMs properly and mitigate the uncertainty and vagueness inherent in their opinions. Applying IFS theory, it is assigned a membership degree, a non-membership degree and a hesitation degree to define every factor affecting the problem [156]. The hesitation degree is practical to deal with the ambiguity in decision problems [157]. Such numbers like triangular, trapezoidal, and interval valued fuzzy numbers that are used to state the instability of consensus are not always sufficient to express the vagueness that arises in different degree of knowledge and qualification of the DMs [156]. Group decision making (GDM) that can integrate all the opinions of each DM to attain the importance of criteria and ranking of decision alternatives, is a useful way to cope with these difficulties. Also, GDM helps to overcome conflicts by Intuitionistic Fuzzy Weighted Averaging (IFWA) [20]. In short, to achieve an agreement on GDM problems, IFGDM tends to be an efficient technique from many perspectives.
The advantages of the proposed IFGDM model in this paper are summarized as follows: (1) It provides to clarify DMs’ opinions in decision problems that consist of ambiguity and uncertainty, (2) it integrates the judgments of DMs by using GDM to reach a sufficient degree of agreement and mitigate the decision-making mistakes, (3) it carries out the qualified angles of IFAHP, IFTOPSIS and IFGDM effectively in the decision problem so as to handle the disadvantages.
The use of the proposed integrated IFMCDM is motivated by two factors. In the beginning, intuitionistic fuzzy logic aids to reduce ambiguity in expert data. Second, integrating two or more MCDM approaches would be more efficient because each method has its own benefits and drawbacks and may produce different outcomes. The basic advantages of IFAHP are that it allows both group and individual studies and makes pairwise comparisons of the criteria in a hierarchical structure. Furthermore, the IFAHP method not only develops the objectivity of expert opinions but also handles decision problems by including hesitant judgments on the evaluation criteria. The integration of the IFTOPSIS method strengthens the methodology, covers the vagueness, and also provides the selection of the best alternative which is the closest to the ideal solution.
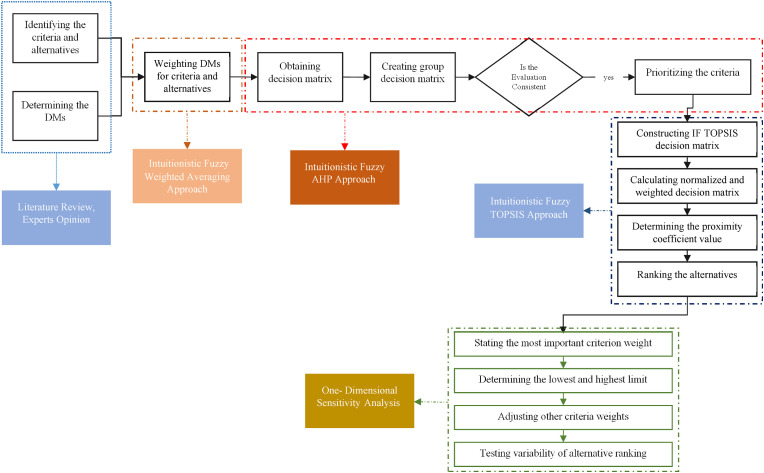
The proposed integrated methodology involves four main stages which are IFWA, IFAHP, IFTOPSIS and One-Dimensional Sensitivity Analysis. A visual demonstration of the methodology is presented in Fig. 1 .
Fig. 1.
The proposed integrated methodology.
4.1. IFWA
In the proposed GDM context, firstly, it is objected to impress that the significance levels of DMs vary on their knowledge, qualifications and experiences. For this purpose, IFWA operation is applied and the significance of DMs is identified as linguistic terms which are identified by IF numbers to estimate the weights of DMs. The weight of the k. DM is shown below.
| (1) |
λk ≥ 0, k = 1,2, …l and
The linguistic terms used for the evaluation of DMs are given in Supplementary Table 1.
4.2. IFAHP
IFAHP is used to calculate the importance weights of the decision criteria in this study. The method is able to solve the complex problems involving vagueness in the decision process that the DMs are faced with. The steps of the IFAHP method can be summarized below [156].
Step 1: Obtaining the evaluation of DMs: After the hierarchy is formed and linguistic terms are converted to an IF matrix, the IFAHP linguistic terms shown in Supplementary Table 2 are used to construct a pairwise comparison matrix.
Step 2: Creating the group decision matrix: At first, for each decision maker the individual pairwise matrix is obtained, and then this is aggregated to create a group decision matrix () by using Eq. (2). Resulting matrix of each criterion refers to the IFAHP weights, and the resulting matrix of each alternative on each criterion defines the weights of alternatives.
| (2) |
Step 3: Calculating the consistency ratio (CR): To control the consistency, Eq. (3) is used to calculate the CR. Also, Random Index (RI) values are shown in Supplementary Table 3.
| (3) |
Here, n is the number of matrix components and is the hesitation value. If the CR value is smaller than or equal to 0.10, it is agreeable. If not, the evaluations are not consistent and should be revised.
Step 4: Combining multi-level weights: The global weight of each alternative () is determined via Eq. (4) by using overall criteria weights () and overall weights of each alternative on the sub-criteria (),
| (4) |
Step 5: Ranking the criteria and alternatives: values are ordered via entropy weights [157] as acquired by using Eq. (5).
| (5) |
4.3. IFTOPSIS
IFTOPSIS method is preferred to rank the available alternatives of this study. The steps of the method are explained as follows [158]:
Step 1: Constructing an IFTOPSIS decision matrix: It is calculated by integrating the assessments of the DMs for alternatives. In the assessment step, all opinions of the DMs are aggregated as group data in order not to lose information. The linguistic terms presented in Supplementary Table 4 is utilized to reflect the DMs' preferences for each alternative.
| (6) |
Rij= ( , (i = 1,2, …m; j = 1,2, …n), where R is the member of the integrated decision matrix.
| (7) |
Step 2: Calculating normalized and weighted IFTOPSIS decision matrix: These matrices are calculated by using Eqs. (8), (9), respectively.
| (8) |
| (9) |
r'ij= ( , (i = 1,2, …m; j = 1,2, …n), Ŕ is the element of the combined decision matrix.
Step 3: Specifying the positive and negative ideal solutions: A* refers to positive ideal solution while A− refers to negative ideal solution as calculated by Eq. (10), (11), respectively.
| (10) |
| (11) |
| (12) |
| (13) |
| (14) |
| (15) |
| (16) |
| (17) |
Step 4: Calculation of positive (Si*) and negative (Si−) difference measurements: Two methods such as Hamming and Euclidean can be used to obtain this measurement. In this application, Hamming method is favored and calculated as follows.
| (18) |
| (19) |
Step 5: Determination of proximity coefficient for each alternative: It is obtained via using Eq. (19) below.
| Ci* = ((Si−) / (Si*+ Si−)), 0≤ Ci*≤1, I = 1,2, …,m | (20) |
Step 6: Ranking the alternatives: Alternatives are ordered according to the seniority of the proximity coefficients.
4.4. One-dimensional sensitivity analysis in MCDM
Sensitivity analysis is realized with the aim of identifying the stability of the outcomes achieved by MCDM methods in the existence of uncertainty [159]. In MCDM problems, criteria weights are generally obtained by several methods (AHP, ANP, etc.), which are subjective and consists of uncertain opinions of DMs due to their nature. Sensitivity analysis validates the robustness of the results, and detects the most important criterion that changes the final ranking of alternatives. Also, it presents the stability of the rankings in the presence of differentiation in the criteria weights [160]. In this paper, a one-dimensional sensitivity analysis is executed to define the effects of the weight variation in the most important criteria on the ranking of the alternatives. Thusly, the weight of the most significant criterion is set at a proper distance and all remaining criteria weights are defined equally in order to provide the weight contribution constraint . represents the most important criterion and can be decreased to 0 and increased up to . It is obtained by Eq. (16) where and mean the highest and lowest criterion weights, respectively [159]:
| (21) |
5. Application: Evaluating medical waste management performance for hospitals in Erzurum
In the application, the steps of the proposed group decision methodology shown in Fig. 1 have been carried out respectively.
5.1. Case definition
In Turkey, 9% of medical waste originates from Erzurum which is the largest city of the East Anatolian region and has various hospitals providing health care services to many nearby provinces. Meanwhile, a large amount of medical waste is generated as a result of the hospital's activities. It is important to consider this issue in Erzurum, as the poor planning of the medical waste management process causes many problems such as increasing costs, health deterioration and environmental pollution that negatively affect living things. In this context, evaluation criteria were determined specific to the Erzurum case by literature research and expert opinions, and alternatives were stated as hospitals. Detailed information on the case study is presented in the following stages.
5.2. Identifying the criteria and alternatives
The first step in MCDM models is forming the purpose of the model and identifying the criteria and alternatives. The clear expression of the purpose is the most essential issue providing the accuracy of the model, and resulting a preliminary stage for clarification of criteria and alternatives. Based on this, it is aimed to determine the hospital that performs waste medical management activities the most properly. In this direction, the criteria and alternatives are specified followingly.
5.2.1. Criteria
The evaluation criteria of this study are stated as factors affecting the medical waste management process. In this context, the criteria are presented in Table 2 by considering the literature review and expert opinions.
Table 2.
Main and sub-criteria of medical waste management.
| Criteria | Sub-Criteria | Description | References |
|---|---|---|---|
| Organizational Criteria (C1) |
C11- Existence, content and implementation of the medical waste management plan | There may be differences between hospitals in terms of how the process will be carried out due to the lack of a medical waste management plan in hospitals or containing deficiencies in processes. Even if the ministry determines the basic draft on this subject, there may be differences in the application from hospital to hospital. | [[42], [161]] |
| C12- Supply chain management and finance | Due to the difficulties in procuring the special equipment (boxes, bags) required for the collection of medical wastes separately at the source and also the financing of these products from the budget of the relevant hospital, the financial interests of the institution may be at the forefront during the implementation process. | [14,162] | |
| C13- Health institution infrastructure | During the transportation and storage of medical wastes, wastes should not come into contact with anyone except the relevant personnel. At this point, healthcare institutions should have separate stairs or elevators and they should never be used for other purposes. The physical structure is of great importance in the safe and effective transportation and storage of waste in a health institution. | [[5], [24], [42],121] | |
| C14 -Qualified personnel |
Medical waste management with experts in the field ensures that the process is carried out more effectively and at minimum cost. For example, if an employee involved in the process does a mistake, it can cause harm that may be difficult to compensate. |
[42] |
|
| Waste Related Criteria (C2) |
C21- Type of medical waste | Although municipalities collect and transport household wastes free of charge, medical wastes are paid from the hospital budget or provincial health overheads. This situation led to the tendency of showing medical wastes as domestic wastes. The medical waste production amount of the hospital pushes the nature of the waste to change. | [14,162] |
| C22- Material quality and type | Colored bags in which the wastes are placed must be resistant to heat and pressure. Bags that do not show the required quality during the collection of wastes and sterilization may cause the process to be carried out incorrectly. | [[5], [163]] | |
| C23- Control of wastes |
Although the control and inspection process to be applied in hospitals is determined with the law by the ministry, it may differ in practice. For example, while a hospital checks waste bags every 2 h, another hospital can do it twice a day. Or, sanctions applied to malfunctions during controls and inspections may be among the factors affecting this process. |
[42] |
|
| Non-Organizational Criteria (C3) | C31-Municipality services | The relevant municipality is authorized for the disposal or reuse of medical wastes converted into household waste. Therefore, the size and capabilities of the municipalities are of great importance in the reliable disposal or reuse of medical wastes converted. | [[1], [121],164] |
| C32- Existence, competence and size of waste management facilities in the province | Another criterion in medical waste management is the existence of a waste management facility in that province. Only one firm in Erzurum makes the waste produced in Erzurum and Bayburt provinces harmless. Waste management facilities that can exist in cities and meet all required standards are of great importance in ending this process quickly and reliably. Medical waste that is stored or transported to other provinces is more likely to cause harm. | [[5], [24],164] | |
| C33- Training of the personnel involved in the process | Regular training is given by the Ministry, the hospital or the provincial health directorate regarding the medical waste process. However, it is thought that the training given is insufficient and the importance of this training is not understood or explained sufficiently. The training criterion is valid not only for in-hospital but also for non-hospital process workers. | [[42], [161]] |
5.2.2. Alternatives
Alternatives in the study are the hospitals composed of five public and one private hospital that operates in Erzurum, Turkey. Some information about alternatives is summarized in Supplementary Table 5.
5.3. Estimating DMs weights by IFWA
In this study, DMs are defined as a group of respondents including researchers and practitioners who have satisfactory knowledge, research and experience associated with the medical waste management process. To this end, a comprehensive search and investigation process is executed. It is essential to find out the opinions of the DMs both in weighting the criteria and the alternative ranking. While the criteria are weighted, the assessments of practitioners and researchers should be taken into account together. Therefore, the views of the practitioners are more important in the alternative ranking. Information and importance level of the DMs for criteria weighting and alternative ranking are shown in Table 3 .
Table 3.
Information about DMs for criteria and alternatives.
| Group | Status | Number | Characteristics | Importance level |
|---|---|---|---|---|
| Criteria Evaluation |
Academician | 2 | They are faculty members at various departments of the universities in Turkey who published scientific papers on medical waste and healthcare management. | Important (I) |
| Governmental decision makers | 2 | All of them are a chief physicians of hospitals which are educational research and public hospitals. | Important (I) | |
| Practitioner |
2 |
Company executives who are at the forefront of the medical waste management process. |
Important (I) |
|
| Alternative Ranking | Medical waste management firm manager | 1 | He is the one who records the medical waste from all hospitals. He has a general idea of all hospitals, as he is the first to observe the waste from hospitals. | Very Important (VI) |
| Head of public hospital services | 1 | He has detailed information about the decision-making processes regarding waste management, especially in public patients and the waste infrastructure of hospitals | Important (I) | |
| Provincial health director | 1 | He has knowledge about the medical waste training and financing of hospitals. | Medium Importance (MI) | |
| Medical waste collector | 1 | He has knowledge about the storage and transportation of medical wastes in hospitals. | Medium Importance (MI) | |
| Municipality | 1 | She has detailed information on the processes to be done after the collection of waste from hospitals and the roles of the municipality. | Important (I) |
DMs utilized in the criterion weighting stage are assumed to have equal importance. Besides, the importance weights of the DMs for alternative ranking are calculated through the IFWA application using Eq. (1).
In this sense, since each DM may have a different degree of impact on the decision-making process overall, DMs were separated into three groups. The importance weights of the experts obtained via Eq. (1) are figured out as 0.289 (VI), 0.223 (I), and 0.163 (MI), consecutively.
5.4. Weighting the criteria by IFAHP
Primarily, the first part of the questionnaire was presented to the DMs. Note that sufficient information related to the criteria was also provided to the experts to make them respond to the questions satisfactorily. The questionnaire includes several questions so as to obtain the importance weights of each criterion with pairwise comparisons. In line with the results of this questionnaire, the IFAHP decision matrix and final weights of the main and sub-criteria are demonstrated in Table 4 . Moreover, the CR of the pairwise comparison matrices was found to be less than 0.10.
Table 4.
IFAHP decision matrixes and weights of main and sub-criteria.
| Criterion | C1 |
C2 |
C3 |
Normalized Values |
Weights | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| μ | ϑ | π | μ | ϑ | π | μ | ϑ | π | μ | ϑ | π | ||
| C1 | 0.020 | 0.180 | 0.800 | 0.563 | 0.184 | 0.218 | 0.531 | 0.189 | 0.229 | 0.246 | 0.431 | 0.310 | 0.691 |
| C2 | 0.184 | 0.563 | 0.218 | 0.020 | 0.180 | 0.800 | 0.556 | 0.182 | 0.214 | 0.165 | 0.515 | 0.309 | 0.238 |
| C3 | 0.189 | 0.531 | 0.229 | 0.182 | 0.556 | 0.214 | 0.020 | 0.180 | 0.800 | 0.070 | 0.614 | 0.309 | 0.069 |
| C11 | 0.02 | 0.18 | 0.8 | 0.61 | 0.17 | 0.19 | 0.20 | 0.51 | 0.25 | 0.21 | 0.48 | 0.27 | 0.07 |
| C12 | 0.17 | 0.61 | 0.19 | 0.02 | 0.18 | 0.80 | 0.22 | 0.45 | 0.28 | 0.20 | 0.54 | 0.24 | 0.01 |
| C13 | 0.51 | 0.20 | 0.25 | 0.50 | 0.20 | 0.25 | 0.02 | 0.18 | 0.80 | 0.26 | 0.38 | 0.30 | 0.47 |
| C14 | 0.45 | 0.22 | 0.28 | 0.54 | 0.20 | 0.24 | 0.36 | 0.26 | 0.32 | 0.02 | 0.18 | 0.80 | 0.44 |
| C21 | 0.020 | 0.180 | 0.800 | 0.195 | 0.565 | 0.229 | 0.162 | 0.638 | 0.200 | 0.069 | 0.018 | 0.113 | 0.016 |
| C22 | 0.565 | 0.195 | 0.229 | 0.020 | 0.180 | 0.800 | 0.153 | 0.663 | 0.183 | 0.462 | 0.121 | 0.110 | 0.055 |
| C23 | 0.585 | 0.175 | 0.217 | 0.639 | 0.153 | 0.183 | 0.020 | 0.180 | 0.800 | 0.469 | 0.860 | 0.778 | 0.167 |
| C31 | 0.020 | 0.180 | 0.800 | 0.515 | 0.212 | 0.262 | 0.317 | 0.346 | 0.245 | 0.458 | 0.757 | 0.330 | 0.036 |
| C32 | 0.212 | 0.515 | 0.262 | 0.020 | 0.180 | 0.800 | 0.317 | 0.346 | 0.245 | 0.072 | 0.120 | 0.330 | 0.012 |
| C33 | 0.346 | 0.317 | 0.245 | 0.346 | 0.317 | 0.245 | 0.020 | 0.180 | 0.800 | 0.470 | 0.123 | 0.339 | 0.022 |
Table 4 reveals that Organizational Criteria (C 1 ) has the first priority with a weight of 0.691, followed by Waste Related Criteria (C 2 ) with a weight of 0.238. However, Non- Organizational Criteria (C 3 ) is acquired to be the least important criterion with the value of 0.069.
Also, for sub-criteria underlying Organizational Criteria, Qualified personnel (C 14 ) has the first priority with a weight of 0.357, followed by Health institution infrastructure (C 13 ) with a weight of 0.207. On the other hand, Supply chain management and finance (C 12 ), turned out to be the least significant criterion with a 0.033 importance value.
According to Table 4, for Waste Related Criteria, Control of waste (C 23 ) is the most important sub-criteria with a weight of 0.167, followed by Material quality and type (C 22 ) with 0.055 weight. However type of waste (C 21 ) is revealed to be the fewest important criterion with a 0.016 value.
Lastly, for Non-Organizational Criteria, Municipality services (C 31 ) has the first priority with a weight of 0.036, followed by Training of the personnel involved in the process (C 33 ) with a weight of 0.022. On the other hand, Existence, competence and size of the waste management facilities in the province (C 32 ), is found to be the least significant criterion.
When all sub-criteria are evaluated together, the most effective criteria for the medical waste management process are Qualified personnel (C 14 ), Health institution infrastructure (C 13 ), and Control of waste (C 23 ), consecutively. Existence, competence and size of the waste management facilities in the province (C 32 ), Type of waste (C 21 ), and Training of the personnel involved in the process (C 33 ) turned out to be the least important criteria, respectively.
5.5. Ranking the alternatives by IFTOPSIS
Following the weighting of the criteria, IFTOPSIS was performed to reveal the ranking of the hospitals according to their medical waste management process performance. In the second part of the questionnaire, the DMs were also asked to evaluate each hospital's condition with respect to the criteria. The IFTOPSIS decision matrix shown in Table 5 was designed based on the data obtained from the DMs.
Table 5.
IFTOPSIS decision matrix.
| Alternatives | C11 | C12 | C13 | C14 | C21 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A1 | 0.52 | 0.47 | 0.01 | 0.52 | 0.46 | 0.03 | 0.52 | 0.46 | 0.02 | 0.68 | 0.27 | 0.05 | 0.51 | 0.48 | 0.02 |
| A2 | 0.50 | 0.48 | 0.02 | 0.51 | 0.48 | 0.02 | 0.46 | 0.50 | 0.04 | 0.57 | 0.41 | 0.03 | 0.52 | 0.47 | 0.01 |
| A3 | 0.43 | 0.51 | 0.05 | 0.52 | 0.47 | 0.02 | 0.44 | 0.51 | 0.05 | 0.52 | 0.47 | 0.01 | 0.46 | 0.50 | 0.04 |
| A4 | 0.48 | 0.49 | 0.03 | 0.52 | 0.47 | 0.01 | 0.44 | 0.51 | 0.05 | 0.50 | 0.48 | 0.02 | 0.48 | 0.49 | 0.03 |
| A5 | 0.65 | 0.28 | 0.07 | 0.61 | 0.36 | 0.03 | 0.60 | 0.35 | 0.05 | 0.66 | 0.30 | 0.05 | 0.56 | 0.42 | 0.02 |
| A6 | 0.45 | 0.50 | 0.04 | 0.50 | 0.48 | 0.02 | 0.42 | 0.52 | 0.06 | 0.49 | 0.49 | 0.03 | 0.42 | 0.52 | 0.06 |
| Alternatives | C22 | C23 | C31 | C32 | C33 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A1 | 0.60 | 0.35 | 0.05 | 0.52 | 0.47 | 0.01 | 0.60 | 0.38 | 0.01 | 0.58 | 0.38 | 0.03 | 0.54 | 0.45 | 0.01 |
| A2 | 0.57 | 0.41 | 0.03 | 0.52 | 0.47 | 0.01 | 0.60 | 0.38 | 0.01 | 0.58 | 0.38 | 0.03 | 0.58 | 0.39 | 0.03 |
| A3 | 0.52 | 0.46 | 0.02 | 0.48 | 0.49 | 0.03 | 0.60 | 0.38 | 0.01 | 0.58 | 0.38 | 0.03 | 0.48 | 0.49 | 0.03 |
| A4 | 0.54 | 0.45 | 0.01 | 0.48 | 0.49 | 0.03 | 0.60 | 0.38 | 0.01 | 0.58 | 0.38 | 0.03 | 0.46 | 0.50 | 0.04 |
| A5 | 0.65 | 0.29 | 0.07 | 0.62 | 0.32 | 0.06 | 0.60 | 0.38 | 0.01 | 0.58 | 0.38 | 0.03 | 0.63 | 0.32 | 0.04 |
| A6 | 0.54 | 0.45 | 0.01 | 0.46 | 0.50 | 0.04 | 0.60 | 0.38 | 0.01 | 0.58 | 0.38 | 0.03 | 0.44 | 0.51 | 0.05 |
Followingly, equations (6), (7), (8), (9), (10), (11), (12), (13), (14), (15), (16), (17), (18), (19), (20) were used to calculate the values of the ideal solutions of the alternatives and the results were shown in Table 6 .
Table 6.
Final results of alternatives.
| Alternatives | S+ | S− | CCi |
|---|---|---|---|
| A1 | 1.215 | 1.233 | 0.503 |
| A2 | 1.357 | 1.233 | 0.476 |
| A3 | 1.634 | 1.233 | 0.430 |
| A4 | 1.601 | 1.233 | 0.435 |
| A5 | 0.720 | 1.233 | 0.631 |
| A6 | 1.720 | 1.233 | 0.417 |
According to Table 6, A5 is the most effective hospital in the medical waste management process, followed by A1. Also, A6 has the least performance score in the medical waste management process.
5.6. Conducting the one-dimensional sensitivity analysis
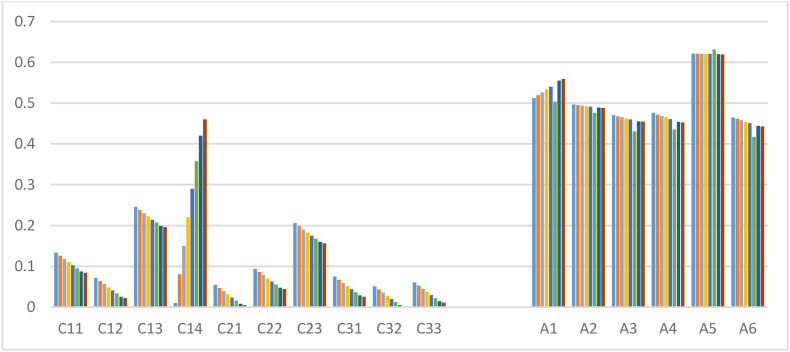
In this study, sensitivity analysis by one-dimensional weight was conducted for discussing the variability of the results. Given the findings of this research, the most important criterion was found as Qualified personnel (C 14 ) with a maximum priority weight of 0.357. In the sensitivity analysis, this weight was adjusted with a proper range, and all other criteria weights were set equally. The weight of the most important criterion was decreased to 0 and increased up to the top limit by using Eq. (20). Hence, the sensitivity analysis is executed through differing the weight of C14 in a range of 0.01 ≤ C14 ≤ 0.46. Consequently, new values of criteria and alternative ranking are obtained as given in Fig. 2 . The weight of C14 cannot be enhanced beyond 0.46 since the weight of C32 (Existence, competence and size of the waste management facilities in the province) criterion becomes negative.
Fig. 2.
Visual graphic of sensitivity analysis.
With respect to the sensitivity analysis results, it can be stated that the variation in criterion weights has no significant effect on the alternative ranking. In this sense, it can be interpreted that the results of the proposed method are robust.
6. Discussion and conclusion
6.1. Discussion
Considering the significance of the criteria obtained by the IFAHP method, Organizational Criteria (C 1 ) has the first priority among the main criteria and Qualified personnel (C 14 ), Health instutition infrastructure (C 13 ), and Control of waste (C 23 ) sub-criteria are the most important within all criteria, respectively. The first stage of the creation of medical waste is in hospitals. Therefore, it is an expected result that organizational criteria are the most important main criterion since they also affect other criteria. Thus, improper management of in-hospital waste management may arise problems that may occur in the next stages of this process. For example, the lack of qualified personnel and poor in-hospital waste management can make the material quality and type criterion related to waste unimportant. On the other hand, health institution infrastructure has great importance at the point of collection, transportation and temporary storage of wastes. For instance, the existence of special elevators for waste can eliminate any risk of infection by transporting medical waste to temporary storage with minimal contact. In addition, qualified personnel is an important factor in the on-site collection, separation and, in-hospital transportation of wastes. Finally, periodic control of wastes and proper inspection can reduce potential errors and prevent problems that may occur.
Regarding the case study involving the six hospitals in Erzurum, A5 is found to be the best performing hospital in the medical waste management process by the IFTOPSIS method. Among the alternatives, A5 hospital is the largest hospital comprising the eastern provinces. Parallel to the high capacity of this hospital, the importance given to the waste management process is high. In this context, equipment and infrastructure with the latest technology have been created. It can be inferred that the appropriate distances of the in-hospital units from each other, training for the new staff, the separation of the waste transportation routes for the institution from the patients and the staff, the support of the supply chain with more than one provider, the maximization of waste control and inspection units put the A5 hospital ahead of other hospitals at the point of medical waste management. In addition, dividing hospital units into small sections facilitates waste management control.
In relevant studies conducted within Turkey [[30], [115], [117], [118], [119], [120], [121], [122], [124]], it is noticed that they generally focus on the waste collection and disposal issues. In this study, the subject of medical waste management is focused on the basis of the case of Erzurum and an evaluation is developed with the IFMCDM perspective.
7. Conclusion
In recent years, the issue of waste management draws attention in terms of increasing environmental problems, concerns about human health and ensuring both economic and environmental sustainability. The impact of waste on the lives and habitats of living things has led all states to organize worldwide regulations and plan waste management process. However, countries have been obliged to do these facilities correctly with legal regulations. Even so, progress has been made in this regard in developed countries, though in developing countries such as Turkey that have a large population, more importance should be given to this issue.
On the other hand, wastes are divided into some classes in the literature according to the danger they create or the transportation and disposal rules. One of these is the medical waste that is required to be managed and planned specifically for the collection, storage, disposal, etc. activities. It is striking that waste management processes especially medical wastes should be given more attention and regulations should be monitored properly for eliminating the harmful effects of these activities. In this context, there is a necessity for research and evaluation of medical waste management.
From this point of view, this study assesses the performance of hospitals operating in the medical waste management process in Erzurum province through the IFMCDM approach. For this purpose, the integrated IFAHP-IFTOPSIS method, which also takes into account the opinions of DMs with hesitation and vagueness was applied. Within the IFGDM framework, the alternative that best fulfills the medical waste management implementations among six hospitals was determined with the field research conducted in line with the criteria identified by a comprehensive literature review.
It is observed that relevant research carried out in Turkey typically concentrates on the problems with waste disposal and collection. The case of Erzurum serves as this study's focal point for medical waste management, and an assessment using the IFMCDM viewpoint is created. At this point, this paper contributes to the literature as it is the first research to study these aspects. In addition, the proposed integrated IFAHP-IFTOPSIS approach has not been used in previous studies.
Moreover, sensitivity analysis conducted in the study revealed that the results of the proposed IFMCDM approach are robust and acceptable to apply to such problems. It was seen that the A5 hospital is the best option under all conditions.
The important difficulty of this study is the challenge experienced in obtaining information about medical waste management from hospital officials due to the current pandemic situation. Also, a limitation of the study can be stated as the number of experts who have equal knowledge about the hospitals included in the application. But, all determined experts had sufficient knowledge and experience level. Finally, it is inherent in MCDM methods that results may change as the experts differ. However, these limitations were eliminated by the sensitivity analysis, and the results were found to be robust.
The conclusions of the study may be a practical guide for hospitals to develop the medical waste management process. Also, this paper is useful for researchers and practitioners who want to develop a decision framework and gain a better understanding of medical waste management. For future research, the study can be handled comparatively for hospitals of different sizes in different provinces. New studies can be considered by changing the MCDM methods benefited in the evaluation of the waste management process, and the criteria used for the evaluation can be updated peculiar to the problem. Additionally, the medical waste management process can be improved by utilizing blockchain technologies in future studies.
Acknowledgements
The authors would like to express their sincere gratitude to the hospital directors in Erzurum and the former health director Erhan Dudu who are the experts of this study, for their valuable suggestions and helpful opinions.
Biographies
Doctorant Sefa Çelik completed his master in Atatürk University at Business Administration Department. He currently works as a Research Assistant in the department of Production Management and Marketing, Faculty of Economics and Administrative Sciences at Atatürk University. He is maintaining his PhD and is in the thesis stage. His master thesis related with occupational health and safety. He studies Multi-Criteria Decision Making Techniques, Production Management and Inventory Management.
Assoc. Dr. İskender Peker completed his master's and doctoral degree in Karadeniz Technical University at Business Administration Department. He currently works as an Associate Professor in the Department of Production Management and Marketing, Faculty of Economics and Administrative Sciences at Gümüşhane University. He teaches undergraduate courses such as Logistics Management, Production management, Inventory Management, Entrepreneurship and Operations research, master's degree courses such as Urban Logistics, Multi-Criteria Decision Making Techniques, Disaster Logistics, doctorate courses such as Fuzzy Logic and Business Applications and Fuzzy Multi-Criteria Decision Making Techniques. He has many articles and papers at national and international level, especially on Logistics-Supply Chain Management and Multi-Criteria Decision Making Techniques. In addition, he has managed undergraduate, graduate and doctoral theses on related topics. He is a member of the Logistics Association (LODER).
Dr. A. Cansu Gök-Kısa completed her undergraduate education at Dokuz Eylül University, Department of Business Administration, and then completed her master's degree in the Department of Quantitative Methods at the same university. She started to work as a research assistant in the Department of Business Administration at Karadeniz Technical University in 2010 and completed her doctorate in this department and graduated at the end of 2015. Since 2016, she has been working at Hitit University, Department of International Trade and Logistics Management. She is a faculty member and conducts undergraduate courses such as Operations Research, Statistics, Logistics Management, Logistics Planning and Modeling, E-Commerce, Transportation Systems and Management, as well as postgraduate courses such as Current Issues in Logistics, Decision Making Techniques, Quality and Process Management. Her fields of study include Multi-Criteria Decision Making, Logistics and Supply Chain Management, Performance Measurement, etc. She has national and international articles and papers on these subject.
Prof. Dr. Gülçin Büyüközkan is the Head of Industrial Engineering Department (Faculty of Engineering and Technology) at Galatasaray University. She graduated from Istanbul Technical University, Industrial Engineering in 1993. She completed her Master's degree in Industrial Engineering from ENSGI (Ecole Nationale Superieure de Génie Industriel) in France in 1996 and from Boğaziçi University in 1997. She continued her doctoral thesis studies in the field of Industrial Engineering in INPG (Institut National Polytechnique de Grenoble), Grenoble, France, thanks to the overseas doctoral scholarship granted to her by the Council of Higher Education. She completed her doctoral dissertation in 1999 by doing some of her thesis studies in Université Laval, Québec, Canada by benefiting from the Région Rhône Alpes European Union Doctoral Fellowship. She has many national and international articles, papers, and book chapters in the fields of industrial engineering, logistics, supply chain, and digitalization. As the Vice-Chairman of the Logistics Association (LODER), Prof. Büyüközkan provides industrial training on various subjects, such as strategic management, logistics, and supply chain, and strategic consultancy services focused on digital transformation, building innovative systems and system improvement; realizes industrial projects. She is also a member of the TÜSİAD Information and Communication Technologies working group.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.seps.2022.101499.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Marinković N., Vitale K., Holcer N.J., Džakula A., Pavić T. Management of hazardous medical waste in Croatia. Waste Manag. 2008;28(6):1049–1056. doi: 10.1016/j.wasman.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 2.Babu B.R., Parande A.K., Rajalakshmi R., Suriyakala P., Volga M. Management of medical waste in India and other countries: a review. J Int Environ Appl Sci. 2009;4(1):65–78. [Google Scholar]
- 3.Demirbas A. Waste management, waste resource facilities and waste conversion processes. Energy Convers Manag. 2011;52(2):1280–1287. [Google Scholar]
- 4.Bdour A., Altrabsheh B., Hadadin N., Al-Shareif M. Assessment of medical wastes management practice: a case study of the northern part of Jordan. Waste Manag. 2007;27(6):746–759. doi: 10.1016/j.wasman.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Coker A., Sangodoyin A., Sridhar M., Booth C., Olomolaiye P., Hammond F. Medical waste management in ibadan, Nigeria: obstacles and prospects. Waste Manag. 2009;29(2):804–811. doi: 10.1016/j.wasman.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 6.Windfeld E.S., Brooks M.S.L. Medical waste management–A review. J Environ Manag. 2015;163:98–108. doi: 10.1016/j.jenvman.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Waste Management Report . 2007. Waste management in Turkey: national regulations and evaluation of implementation results.https://www.sayistay.gov.tr/En/Upload/files/4-TCA_Waste_Management_Report.pdf (06.05.2021 [Google Scholar]
- 8.Environmental Status Reports Environmental status Reports on the Basis of provinces, 2012-2018, environmental impact assessment, general directorate for permit and inspection. Republ. Turk. Minist. Environ. Urban. 2019 https://ced.csb.gov.tr/il-cevre-durumraporlari-i-82671 [Google Scholar]
- 9.WHO . World Health Organization; 2000. The world health report: health systems: improving performance. [Google Scholar]
- 10.Cheng Y.W., Sung F.C., Yang Y., Lo Y.H., Chung Y.T., Li K.C. Medical waste production at hospitals and associated factors. Waste Manag. 2009;29(1):440–444. doi: 10.1016/j.wasman.2008.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shinee E., Gombojav E., Nishimura A., Hamajima N., Ito K. Healthcare waste management in the capital city of Mongolia. Waste Manag. 2008;28(2):435–441. doi: 10.1016/j.wasman.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 12.Tsakona M., Anagnostopoulou E., Gidarakos E. Hospital waste management and toxicity evaluation: a case study. Waste Manag. 2007;27(7):912–920. doi: 10.1016/j.wasman.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 13.Zamparas M., Kapsalis V.C., Kyriakopoulos G.L., Aravossis K.G., Kanteraki A.E., Vantarakis A., Kalavrouziotis I.K. Medical waste management and environmental assessment in the rio university hospital, western Greece. Sustain. Chem. Pharm. 2019;13 [Google Scholar]
- 14.Abor P.A. Medical waste management practices in a southern african hospital. J Appl Sci Environ Manag. 2007;11(3):91–96. doi: 10.1108/09526860810880153. [DOI] [PubMed] [Google Scholar]
- 15.Abd El-Salam M.M. Hospital waste management in el-beheira governorate, Egypt. J Environ Manag. 2010;91(3):618–629. doi: 10.1016/j.jenvman.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Caniato M., Tudor T., Vaccari M. International governance structures for health-care waste management: a systematic review of scientific literature. J Environ Manag. 2015;153:93–107. doi: 10.1016/j.jenvman.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 17.Ruoyan G., Lingzhong X., Huijuan L., Chengchao Z., Jiangjiang H., Yoshihisa S.…Chushi K. Investigation of health care waste management in binzhou district, China. Waste Manag. 2010;30(2):246–250. doi: 10.1016/j.wasman.2008.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aung T.S., Luan S., Xu Q. Application of multi-criteria-decision approach for the analysis of medical waste management systems in Myanmar. J Clean Prod. 2019;222:733–745. [Google Scholar]
- 19.Sawalem M., Selic E., Herbell J.D. Hospital waste management in Libya: a case study. Waste Manag. 2009;29(4):1370–1375. doi: 10.1016/j.wasman.2008.08.028. [DOI] [PubMed] [Google Scholar]
- 20.Büyüközkan G., Göçer F., Karabulut Y. A new group decision making approach with IF AHP and IF VIKOR for selecting hazardous waste carriers. Measurement. 2019;134:66–82. [Google Scholar]
- 21.Chartier Y., Emmanuel J., Pieper U., Pruss A., Rushbrook P., Stringer R. WHO; Geneva: 2014. Safe management of wastes from health-care activities. [Google Scholar]
- 22.Diaz L.F., Savage G.M., Eggerth L.L. Alternatives for the treatment and disposal of healthcare wastes in developing countries. Waste Manag. 2005;25(6):626–637. doi: 10.1016/j.wasman.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Ilyas S., Srivastava R.R., Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.141652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verma L.K., Mani S., Sinha N., Rana S. Biomedical waste management in nursing homes and smaller hospitals in delh. Waste Manag. 2008;28(12):2723–2734. doi: 10.1016/j.wasman.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 25.Dursun M., Karsak E., Karadayı M. A fuzzy MCDM approach for HealthCare waste management. World academy of science. Eng Technol. 2011;5(1):176–182. [Google Scholar]
- 26.Ferreira V., Ribau Teixeira M. ISWA/APESB World Congress; Portugal: 2009. Assessing the medical waste management practices and associated risk perceptions in algarve hospital. [Google Scholar]
- 27.Mbarki A., Kabbachi B., Ezaidi A., Benssaou M. Medical waste management: a case study of the souss-massa-drâa region, Morocco. J Environ Protect. 2013;4(9) [Google Scholar]
- 28.Mosquera M., Andrés-Prado M.J., Rodríguez-Caravaca G., Latasa P., Mosquera M.E. Evaluation of an education and training intervention to reduce health care waste in a tertiary hospital in Spain. Am J Infect Control. 2014;42(8):894–897. doi: 10.1016/j.ajic.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 29.Zimmermann A., Szyca R. Medical waste management in Poland: the legal issues. Pol J Environ Stud. 2011;21(4):1113–1118. [Google Scholar]
- 30.Korkut E.N. Estimations and analysis of medical waste amounts in the city of Istanbul and proposing A new approach for the estimation of future medical waste amounts. Waste Manag. 2018;81:168–176. doi: 10.1016/j.wasman.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Kumar R., Pandey A.K., Baz A., Alhakami H., Alhakami W., Agrawal A., Khan R.A. Fuzzy-based symmetrical multi-criteria decision-making procedure for evaluating the impact of harmful factors of healthcare information security. Symmetry. 2020;12(4):664. [Google Scholar]
- 32.Almulihi A.H., Alassery F., Khan A.I., Shukla S., Gupta B.K., Kumar R. Analyzing the implications of healthcare data breaches through computational technique. Intelli. Automation. Soft Comput. 2022:1763–1779. [Google Scholar]
- 33.Attaallah A., Alsuhabi H., Shukla S., Kumar R., Gupta B.K., Khan R.A. Analyzing the big data security through a unified decision-making approach. Intellı. Automatıon. Soft Comput. 2022;32(2):1071–1088. [Google Scholar]
- 34.Sahu K., Alzahrani F.A., Srivastava R.K., Kumar R. Hesitant fuzzy sets based symmetrical model of decision-making for estimating the durability of web application. Symmetry. 2020;12(11):1770. [Google Scholar]
- 35.Khatri S., Alzahrani F.A., Ansari M.T.J., Agrawal A., Kumar R., Khan R.A. A systematic analysis on blockchain integration with healthcare domain: Scope and challenges. IEEE Access. 2021;9:84666–84687. [Google Scholar]
- 36.Zarour M., Ansari M.T.J., Alenezi M., Sarkar A.K., Faizan M., Agrawal A.…Khan R.A. Evaluating the impact of blockchain models for secure and trustworthy electronic healthcare records. IEEE Access. 2020;8:157959–157973. [Google Scholar]
- 37.Sahu K., Alzahrani F.A., Srivastava R.K., Kumar R. Evaluating the impact of prediction techniques: software reliability perspective. Comput Mater Continua (CMC) 2021;67(2):1471–1488. [Google Scholar]
- 38.Ansari M.T.J., Baz A., Alhakami H., Alhakami W., Kumar R., Khan R.A. P-STORE: extension of STORE methodology to elicit privacy requirements. Arabian J Sci Eng. 2021;46(9):8287–8310. [Google Scholar]
- 39.Klangsin P., Harding A.K. Medical waste treatment and disposal methods used by hospitals in Oregon, Washington, and Idaho. J Air Waste Manag Assoc. 1998;48(6):516–526. doi: 10.1080/10473289.1998.10463706. [DOI] [PubMed] [Google Scholar]
- 40.Jang Y.C., Lee C., Yoon O.S., Kim H. Medical waste management in Korea. J Environ Manag. 2006;80(2):107–115. doi: 10.1016/j.jenvman.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 41.Viswanathan P.K. Report of the postdoctoral research study submitted to the Asian Institute of Technology; Bangkok, January: 2006. A comparative study of smallholder rubber and rubber integrated farm livelihood systems in India and Thailand. [Google Scholar]
- 42.Yong Z., Gang X., Guanxing W., Tao Z., Dawei J. Medical waste management in China: a case study of nanjing. Waste Manag. 2009;29(4):1376–1382. doi: 10.1016/j.wasman.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 43.Yardım N., Dirimeşe V., Varol Ö., Mollahaliloğlu S. Amount of medical waste collected by metropolitan unicipalities: data on 2004 and first six months 2005; methods of collecting, amassing and disposal medical waste in 81 provinces. J. Dokuz Eylul University Med. Faculty. 2006;20(3):165–173. [Google Scholar]
- 44.Ghasemi M.K., Yusuff R.B. Advantages and disadvantages of healthcare waste treatment and disposal alternatives: Malaysian scenario. Pol J Environ Stud. 2016;25(1):17–25. [Google Scholar]
- 45.Lee B.K., Ellenbecker M.J., Moure-Ersaso R. Alternatives for treatment and disposal cost reduction of regulated medical wastes. Waste Manag. 2004;24(2):143–151. doi: 10.1016/j.wasman.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 46.Alves S.B., e Souza A.C., Tipple A.F., Rezende K.C., de Resende F.R., Rodrigues É.G., Pereira M.S. The reality of waste management in primary health care units in Brazil. Waste Manag Res. 2014;32(9):40–47. doi: 10.1177/0734242X14543815. [DOI] [PubMed] [Google Scholar]
- 47.Moreira A.M.M., Günther W.M.R. Assessment of medical waste management at a primary health-care center in São Paulo, Brazil. Waste Manag. 2013;33(1):162–167. doi: 10.1016/j.wasman.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 48.Santos E.D.S., Gonçalves K.M.D.S., Mol M.P.G. Healthcare waste management in A Brazilian university public hospital. Waste Manag Res. 2019;37(3):278–286. doi: 10.1177/0734242X18815949. [DOI] [PubMed] [Google Scholar]
- 49.Schiavi C.S., Soares H.M.D., Silva T.N.D. Sustaınable innovatıon and leadershıp in the treatment of medıcal waste in porto alegre/RS. Revista de Administração da UFSM. 2022;14:1010–1031. [Google Scholar]
- 50.Silva T., Silva M.M., Florencio L., Machado Santos S. A qualitative descriptive case study on home medical waste management in Brazil. J Mater Cycles Waste Manag. 2022:1–10. [Google Scholar]
- 51.Blenkharn J.I. Safe disposal and effective destruction of clinical wastes. J Hosp Infect. 2005;60(4):295–297. doi: 10.1016/j.jhin.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 52.Graikos A., Voudrias E., Papazachariou A., Iosifidis N., Kalpakidou M. Composition and production rate of medical waste from a small producer in Greece. Waste Manag. 2010;30(8–9):1683–1689. doi: 10.1016/j.wasman.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 53.Hansen D., Mikloweit U., Ross B., Popp W. Healthcare waste management in Germany. Int J Integrated Care. 2014;10(1):1–5. [Google Scholar]
- 54.Uloma A.A., Nkem Benjamin I., Kiss I. Knowledge, attitude and practice of healthcare workers towards medical waste management: a comparative study of two geographical areas. J. Waste Manag. Dispos. 2022;5:101. [Google Scholar]
- 55.Insa E., Zamorano M., López R. Critical review of medical waste legislation in Spain. Resour Conserv Recycl. 2010;54(12):1048–1059. [Google Scholar]
- 56.Szyperek W.M. 2022. Analysis and evaluation of medical waste management in Poland (doctoral dissertation, katedra ochrony i kształtowania srodowiska) [Google Scholar]
- 57.Askarian M., Vakili M., Kabir G. Results of a hospital waste survey in private hospitals in fars province, Iran. Waste Manag. 2004;24(4):347–352. doi: 10.1016/j.wasman.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 58.Bahrami H., Malakootian M., Nasab S.D.M., Jaafarzadeh N., Askarian M., Samadi S., Ahmadi N.A. Withdrawn; an overview of the present status of hospital waste management in Kerman, Iran. J. Infect. Public Health. 2014:1876. doi: 10.1016/j.jiph.2014.07.007. 0341. [DOI] [PubMed] [Google Scholar]
- 59.Farzadkia M., Golbaz S., Sajadi H.S. Surveying hospital waste management in Karaj in the year of 2013. J. Hosp. 2015;14(1):105–115. [Google Scholar]
- 60.Jaafari J., Dehghani M.H., Hoseini M., Safari G.H. Investigation of hospital solid waste management in Iran. World Rev Sci Technol Sustain Dev. 2015;12(2):111–125. [Google Scholar]
- 61.Karamouz M., Zahraie B., Kerachian R., Jaafarzadeh N., Mahjouri N. Developing A master plan for hospital solid waste management: a case study. Waste Manag. 2007;27(5):626–638. doi: 10.1016/j.wasman.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 62.Naimi N., Tavakoli Ghochani H., Nekohi N., Ghorbanpour R., Karimkoshte S., Amiri H.…Dolati M. Assessment of medical waste management in hospitals of north Khorasan university of medical Sciences. J. North Khorasan Univ. Med. Sci. 2015;6(4):935–945. [Google Scholar]
- 63.Mensoor M.K. Medical waste management in Iraq: a case study of Baghdad. Waste Dispos. Sustain. Energy. 2020;2(4):329–335. [Google Scholar]
- 64.Abdulla F., Qdais H.A., Rabi A. Site investigation on medical waste management practices in northern Jordan. Waste Manag. 2008;28(2):450–458. doi: 10.1016/j.wasman.2007.02.035. [DOI] [PubMed] [Google Scholar]
- 65.Alshraideh H., Qdais H.A. Stochastic modeling and optimization of medical waste collection in Northern Jordan. J Mater Cycles Waste Manag. 2017;19(2):743–753. [Google Scholar]
- 66.Aukour F.J. Healthcare waste management in Jordan king abdullah university hospital case study. J. Sci. Med. Eng. 2008;20(1):61–77. [Google Scholar]
- 67.Oweis R., Al-Widyan M., Al-Limoon O. Medical waste management in Jordan: a study at the king hussein medical center. Waste Manag. 2005;25(6):622–625. doi: 10.1016/j.wasman.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 68.Das S.K., Biswas R. Awareness and practice of biomedical waste management among healthcare providers in a tertiary care hospital of West Bengal, India. Int J Med Publ Health. 2016;6(1):19–25. [Google Scholar]
- 69.Faizal M., Jayachitra U., Vijayakumar P., Rajasekar M. Optimization of inbound vehicle routes in the collection of bio-medical wastes. Mater Today Proc. 2021;45:692–699. [Google Scholar]
- 70.Manupati V.K., Ramkumar M., Baba V., Agarwal A. Selection of the best healthcare waste disposal techniques during and post COVID-19 pandemic era. J Clean Prod. 2021;281 doi: 10.1016/j.jclepro.2020.125175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Patil A.D., Shektar A.V. Healthcare waste management in India. J. Environ. Manag. 2001;63:211–220. doi: 10.1006/jema.2001.0453. [DOI] [PubMed] [Google Scholar]
- 72.Soyam G.C., Hiwarkar P.A., Kawalkar U.G., Soyam V.C., Gupta V.K. KAP study of bio-medical waste management among health care workers in Delhi. Int. J. Community Med. Public Health. 2017;4(9):3332–3337. [Google Scholar]
- 73.Fikri E., Kurniati I., Wartiniyati W., Prijanto T.B., Syarief O., Khair A.S.E. The phenomenon of medical waste recycling in Indonesia: contact time and chlorine dose as a disinfectant with the bio-indicator Bacillus subtilis and Bacillus stearothermophilus. J. Ecol. Eng. 2021;22(4):47–58. [Google Scholar]
- 74.Oh S.E., Ji K.H., Park S., Kim P., Lee K.M. International comparisons of management systems for medical waste and suggestions for future direction of medical waste management system in Korea. J. Environ. Health Sci. 2017;43(6):532–544. [Google Scholar]
- 75.Singh N., Tang Y., Zhang Z., Zheng C. COVID-19 waste management: effective and successful measures in Wuhan, China. Resour Conserv Recycl. 2020;163 doi: 10.1016/j.resconrec.2020.105071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhao H., Liu H., Wei G., Wang H., Zhu Y., Zhang R., Yang Y. Comparative life cycle assessment of emergency disposal scenarios for medical waste during the COVID-19 pandemic in China. Waste Manag. 2021;126:388–399. doi: 10.1016/j.wasman.2021.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tsai W.T. Analysis of medical waste management and impact analysis of COVID-19 on its generation in Taiwan. Waste Manag Res. 2021:1–7. doi: 10.1177/0734242X21996803. [DOI] [PubMed] [Google Scholar]
- 78.Wang T.C., Ku P., Lu H., et al. Investigation and analysis of medication disposal in hospitals and community pharmacies in taiwan. Sustainability. 2020;12:11. [Google Scholar]
- 79.Ali M., Wang W., Chaudhry N. Application of life cycle assessment for hospital solid waste management: a case study. J Air Waste Manag Assoc. 2016;66(10):1012–1018. doi: 10.1080/10962247.2016.1196263. [DOI] [PubMed] [Google Scholar]
- 80.Ali S., Mahmood U., Malik A.U., Aziz F., Naghman R.B., Ahmed I. Current hospital waste management practices in Pakistan: case study and curative measures. Publ. Health. Prevent. Med. 2015;1(3):125–129. [Google Scholar]
- 81.Al-Khatib I.A., Eleyan D., Garfield J. A system dynamics approach for hospital waste management in A city in A developing country: the case of nablus, Palestine. Environ Monit Assess. 2016;188(9):503. doi: 10.1007/s10661-016-5487-9. [DOI] [PubMed] [Google Scholar]
- 82.Vasistha P., Ganguly R., Gupta A.K. Biomedical waste generation and management in public sector hospital in shimla city. Environ Pollut. 2018;225–232 [Google Scholar]
- 83.Mato R.R.A.M., Kaseva M.E. Critical review of industrial and medical waste practices in dar Es salaam city. Resour Conserv Recycl. 1999;25(3–4):271–287. [Google Scholar]
- 84.Awodele O., Adewoye A.A., Oparah A.C. Assessment of medical waste management in seven hospitals in Lagos, Nigeria. BMC Publ Health. 2016;16(1):269. doi: 10.1186/s12889-016-2916-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baaki T.K., Baharum M.R., Akashah F.W. Critical success factors of medical waste management implementation in healthcare facilities in Nigeria: a case study. J Des Built Environ. 2017;17(1):18–35. [Google Scholar]
- 86.Etim M.A., Academe S., Emenike P., Omole D. Application of multi-criteria decision approach in the assessment of medical waste management systems in Nigeria. Sustainability. 2021;13(19) [Google Scholar]
- 87.Longe E.O., Williams A. A preliminary study of medical waste management in Lagos metropolis, Nigeria. Iran J Environ Health Sci Eng. 2006;3(2):133–139. [Google Scholar]
- 88.Olanrewaju O.O. Assesment of medical waste management in two public health facilites within akure metropolis, Ondo state, Nigeria. Int. J. Res. Stud. Sci. Eng. Tech. 2019;6(5):17–29. [Google Scholar]
- 89.Oruonye E.D., Ahmed A.Y. Covid-19 and challenges of management of infectious medical waste in Nigeria: a case of taraba state. Int J Wine Res. 2020;10(3):1–5. [Google Scholar]
- 90.Makhura R.R., Matlala S.F., Kekana M.P. Medical waste disposal at A hospital i?n mpumalanga province, South Africa: implications for training of healthcare professionals. S Afr Med J. 2016;106(11):1096–1102. doi: 10.7196/SAMJ.2016.v106i11.10689. [DOI] [PubMed] [Google Scholar]
- 91.Motlatla M., Maluleke T.X. Assessment of knowledge about healthcare risk waste management at a tertiary hospital in the northern cape province, South Africa. Int J Environ Res Publ Health. 2021;18(2):449. doi: 10.3390/ijerph18020449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Olaifa A., Govender R.D., Ross A.J. Knowledge, attitudes and practices of healthcare workers about healthcare waste management at A district hospital in Kwazulu-natal. S Afr Fam Pract. 2018;60(5):137–145. [Google Scholar]
- 93.Olaniyi F.C., Ogola J.S., Tshitangano T.G. Efficiency of health care risk waste management in rural healthcare facilities of South Africa: an assessment of selected facilities in vhembe district, Limpopo province. Int J Environ Res Publ Health. 2019;16(12):2199. doi: 10.3390/ijerph16122199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Udofia E.A., Fobil J.N., Gulis G. Solid medical waste management in Africa. Afr J Environ Sci Technol. 2015;9(3):244–254. [Google Scholar]
- 95.Mmereki D., Baldwin A., Li B., Liu M. Healthcare waste management in Botswana: storage, collection, treatment and disposal system. J Mater Cycles Waste Manag. 2017;19(1):351–365. [Google Scholar]
- 96.Basak S.R., Mita A.F., Ekra N.J., Alam M.J.B. A study on hospital waste management of Sylhet city in Bangladesh. Int. J. Eng. Appl. Sci. Technol. 2019;4:36–40. [Google Scholar]
- 97.Hassan M.M., Ahmed S.A., Rahman K.A., Biswas T.K. Pattern of medical waste management: existing scenario in dhaka city, Bangladesh. BMC Publ Health. 2008;8(1):36. doi: 10.1186/1471-2458-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rahman M., Sarker P., Sarker N. Existing scenario of healthcare waste management in noakhali, Bangladesh. Bangladesh J. Environ. Res. 2020;11:60–71. [Google Scholar]
- 99.Reza S.M.S., Akter K.S. Finding an optimum technology for medical waste management at upazila & rural level in Bangladesh. J. Environ. Treat. Tech. 2018;6(1):1–7. [Google Scholar]
- 100.Sarker M.F.R., Debnath R., Rahman A.S., Howlader L.B., Sarker Z.J., Rahman M.S. Medical waste management practices in a selected secondary healthcare facility. J Bangladesh Coll Phys Surg. 2020;38(4):160–165. [Google Scholar]
- 101.Gilbert O.O., Magu D., Sagwe D.N. Risks associated with compliance in medical waste practices among health workers at Kenyatta national hospital. J. Health. Med. Nurs. 2020;5(1):1–9. [Google Scholar]
- 102.Maina J.W. Knowledge, attitude and practice of staff on segregation of hospital waste: a case study of a tertiary private hospital in Kenya. Eur Sci J. 2018;14:401–417. [Google Scholar]
- 103.Njue P.M., Cheboi K.S., Oiye S. Adherence to healthcare waste management guidelines among nurses and waste handlers in thika sub-county-Kenya. Ethiopian. J Health Sci. 2015;25(4):295–304. doi: 10.4314/ejhs.v25i4.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Adu R.O., Gyasi S.F., Essumang D.K., Otabil K.B. Medical waste-sorting and management practices in five hospitals in Ghana. J. Environ. Publ. Health. 2020;2020 doi: 10.1155/2020/2934296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Agyekum N.K., Ansah E.W. Medical waste management practices at healthcare facilities in cape coast metropolis. Adv. J. Soc. Sci. 2022;10(1):63–74. [Google Scholar]
- 106.Odonkor S.T., Mahami T. Healthcare waste management in Ghanaian hospitals: associated public health and environmental challenges. Waste Manag Res. 2020;38(8):831–839. doi: 10.1177/0734242X20914748. [DOI] [PubMed] [Google Scholar]
- 107.Wiafe S., Nooni I.K., Nlasia M.S., Diaba S.K., Fianko S.K. Assessing clinical solid waste management strategies in sunyani municipality, Ghana–evidence from three healthcare facilities. Int. J. Environ. Pollut. Res. 2015;3(3):32–52. [Google Scholar]
- 108.Assemu D.M., Tafere T.E., Gelaw Y.M., Bantie G.M. Healthcare waste management practice and associated factors among private and public hospitals of bahir dar city administration. J. Environ. Publ. Health. 2020;2020 doi: 10.1155/2020/7837564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Debalkie D., Kumie A. Healthcare waste management: the current issue in menellik II referral hospital, Ethiopia. Curr World Environ. 2017;12(1):42. [Google Scholar]
- 110.Tesfahun E., Kumie A., Beyene A. Developing models for the prediction of hospital healthcare waste generation rate. Waste Manag Res. 2016;34(1):75–80. doi: 10.1177/0734242X15607422. [DOI] [PubMed] [Google Scholar]
- 111.Chisholm J.M., Zamani R., Negm A.M., Said N., Abdel Daiem M.M., Dibaj M., Akrami M. Sustainable waste management of medical waste in african developing countries: a narrative review. Waste Manag Res: J. Int. Solid Wastes. Publ. Cleansing. Assoc. ISWA. 2021;39(9):1149–1163. doi: 10.1177/0734242X211029175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Eryılmaz H., Demiraslan K.O. Türkiye tibbi atik envanteri ve değerlendirilmesi. Adıyaman Üniversitesi Mühendislik Bilimleri Dergisi. 2020;7(13):89–103. [Google Scholar]
- 113.Ökten H.E., Corum A., Demir H.H. A comparative economic analysis for medical waste treatment options. Environ Protect Eng. 2015;41(3):137–145. [Google Scholar]
- 114.Üçüncü O., Yazici E. Hospital waste management in trabzon. Sigma. 2009;27:49–59. [Google Scholar]
- 115.Akbolat M., Dede C., Isik O., Saglam H. Medical waste management practices in Turkey: a case study in sakarya. Pakistan J Med Sci. 2011;27:892–895. [Google Scholar]
- 116.Alagöz A.Z., Kocasoy G. Determination of the best appropriate management methods for the health-care wastes in Istanbul. Waste Manag. 2008;28(7):1227–1235. doi: 10.1016/j.wasman.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 117.Birpınar M.E., Bilgili M.S., Erdoğan T. Medical waste management in Turkey: a case study of Istanbul. Waste Manag. 2009;29(1):445–448. doi: 10.1016/j.wasman.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 118.Cıplak N., Barton J.R. A system dynamics approach for healthcare waste management: a case study in Istanbul metropolitan city, Turkey. Waste Manag Res. 2012;30(6):576–586. doi: 10.1177/0734242X12443405. [DOI] [PubMed] [Google Scholar]
- 119.Çetinkaya A.Y., Kuzu S.L., Demir A. Medical waste management in a mid-populated Turkish city and development of medical waste prediction model. Environ Dev Sustain. 2020;22(7):6233–6244. [Google Scholar]
- 120.Eker H.H., Bilgili M.S., Sekman E., Top S. Evaluation of the regulation changes in medical waste management in Turkey. Waste Manag Res. 2010;28(11):1034–1038. doi: 10.1177/0734242X10366158. [DOI] [PubMed] [Google Scholar]
- 121.Eren E., Tuzkaya U.R. Occupational health and safety-oriented medical waste management: a case study of Istanbul. Waste Manag Res. 2019;37(9):876–884. doi: 10.1177/0734242X19857802. [DOI] [PubMed] [Google Scholar]
- 122.Gören N S., Demir G., Yaman C., Yildiz A. Medical waste management by geographical region in Turkey. J Residuals Sci Technol. 2011;8(3):109–115. [Google Scholar]
- 123.Sevindi S., ve Özçifçi A. Tıbbi atık yönetimi : aksaray İli Örneği. V. Uluslararası Aksaray Sempozyumu Dergisi. 2020;1(1):258–270. [Google Scholar]
- 124.Uysal F., Tınmaz E. Medical waste management in trachea region of Turkey: suggested remedial action. Waste Manag Res. 2004;22(5):403–407. doi: 10.1177/0734242X04045690. [DOI] [PubMed] [Google Scholar]
- 125.Özkan A. Evaluation of healthcare waste treatment/disposal alternatives by using multi-criteria decision-making techniques. Waste Manag Res. 2013;31(2):141–149. doi: 10.1177/0734242X12471578. [DOI] [PubMed] [Google Scholar]
- 126.Budak A., Ustundag A. Reverse logistics optimisation for waste collection and disposal in health institutions: the case of Turkey. Int J Logist Res Appl. 2017;20(4):322–341. [Google Scholar]
- 127.Pruss-Üstün A., Rapiti E., Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;6(48):482–490. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 128.Wei Y., Cui M., Ye Z., Guo Q. Environmental challenges from the increasing medical waste since SARS outbreak. J Clean Prod. 2021;291 doi: 10.1016/j.jclepro.2020.125246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zroychikov N.A., Fadeev S.A., Bezruky P.P. Development of an environmentally safe process for medical waste disposal based on pyrolysis. Therm Eng. 2018;65(11):833–840. [Google Scholar]
- 130.Jindal A.K., Gupta A., Grewal V.S., Mahen A. Biomedical waste disposal: a systems analysis. Med J Armed Forces India. 2013;69(4):351–356. doi: 10.1016/j.mjafi.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Narayanamoorthy S., Annapoorani V., Kang D., Baleanu D., Jeon J., Kureethara J.V., Ramya L. A novel assessment of bio-medical waste disposal methods using integrating weighting approach and hesitant fuzzy MOOSRA. J Clean Prod. 2020;275 [Google Scholar]
- 132.Padmanabhan K.K., Barik D. Energy from toxic organic waste for heat and power generation. Woodhead Publishing; 2019. Health hazards of medical waste and its disposal; pp. 99–118. [Google Scholar]
- 133.Behera B.C. Challenges in handling COVID-19 waste and its management mechanism: a review. Environ Nanotechnol Monit Manag. 2021;15 doi: 10.1016/j.enmm.2021.100432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chen C., Chen J., Fang R., Ye F., Yang Z., Wang Z., Shi F., Tan W. What medical waste management system may cope with COVID-19 pandemic: lessons from wuhan. Resources. Conserv Recycl. 2021;170 doi: 10.1016/j.resconrec.2021.105600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Maalouf A., Maalouf H. Impact of COVID-19 pandemic on medical waste management in Lebanon. Waste Manag Res. 2021;39(1_suppl):45–55. doi: 10.1177/0734242X211003970. [DOI] [PubMed] [Google Scholar]
- 136.Mihai F.C. Assessment of COVID-19 waste flows during the emergency state in Romania and related public health and environmental concerns. Int J Environ Res Publ Health. 2021;17:5439. doi: 10.3390/ijerph17155439. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sangkham S. Face mask and medical waste disposal during the novel COVID-19 pandemic in asia. Case Stud. Chem. Environ. Eng. 2020;2 doi: 10.1016/j.cscee.2020.100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Saxena P., Pradhan I.P., Kumar D. Redefining bio medical waste management during COVID-19 in India: a way forward. Mater Today Proc. 2021;60:849-858 doi: 10.1016/j.matpr.2021.09.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yoon C.W., Kim M.J., Park Y.S., Jeon T.W., Lee M.Y. A review of medical waste management systems in the Republic of Korea for hospital and medical waste generated from the COVID-19 pandemic. Sustainability. 2022;14(6):3678. [Google Scholar]
- 140.Joneghani N.M., Zarrinpoor N., Eghtesadifard M. A mathematical model for designing a Network of sustainable medical waste management under uncertainty. Comput Ind Eng. 2022 [Google Scholar]
- 141.Ghoushchi S.J., Bonab S.R., Ghiaci A.M., Haseli G., Tomaskova H., Hajiaghaei-Keshteli M. Landfill site selection for medical waste using an i?ntegrated SWARA-WASPAS framework based on spherical fuzzy set. Sustainability. 2021;13(24) [Google Scholar]
- 142.Maldonado-Macías A., Alvarado A., García J.L., Balderrama C.O. Intuitionistic fuzzy TOPSIS for ergonomic compatibility evaluation of advanced manufacturing technology. Int J Adv Manuf Technol. 2014;70(9–12):2283–2292. [Google Scholar]
- 143.Dammak F., Baccour L., Alimi A.M. A comparative analysis for multi-attribute decision making methods: TOPSIS, AHP, VIKOR using intuitionistic fuzzy sets. Fuzzy Syst Conf. 2015:1–5. [Google Scholar]
- 144.Büyüközkan G., Göçer F. Uncertainty modelling in knowledge engineering and decision making: proceedings of the 12th international FLINS conference. 2016. Evaluation of government websites using intuitionistic fuzzy AHP and TOPSIS; pp. 930–935. [Google Scholar]
- 145.Büyüközkan G., Güleryüz S. A new integrated intuitionistic fuzzy group decision making approach for product development partner selection. Comput Ind Eng. 2016;102:383–395. [Google Scholar]
- 146.Karasan A., Erdogan M., Ilbahar E. Prioritization of production strategies of a manufacturing plant by using an integrated intuitionistic fuzzy AHP & TOPSIS approach. J Enterprise Inf Manag. 2018;31(4):510–528. [Google Scholar]
- 147.Tooranloo H.S., Ayatollah A.S., Iranpour A. A model for supplier evaluation and selection based on integrated interval-valued intuitionistic fuzzy AHP-TOPSIS approach. Int J Math Oper Res. 2018;13(3):401–417. [Google Scholar]
- 148.Adar T., Emeç Ş., Delice E.K., Akkaya G. An integrated IF-AHP and IF-TOPSIS method for neuroimaging techniques selection. Turkish J. Fuzzy Sys. 2019;10(1):14–38. [Google Scholar]
- 149.Doğan O., Deveci M., Canıtez F., Kahraman C. A corridor selection for locating autonomous vehicles using an interval-valued intuitionistic fuzzy AHP and TOPSIS method. Soft Comput. 2019;24:8937–8953. [Google Scholar]
- 150.Kumar A., Anbanandam R. Location selection of multimodal freight terminal under STEEP sustainability. Res. Transport. Bus. Manag. 2020 [Google Scholar]
- 151.Choudhary A., De A., Ahmed K., Shankar R. An integrated fuzzy intuitionistic sustainability assessment framework for manufacturing supply chain: a study of UK based firms. Ann Oper Res. 2021:1–44. [Google Scholar]
- 152.Demir E., Koca G. International conference on intelligent and fuzzy systems. Springer; Cham: 2020. Green supplier selection using intuitionistic fuzzy AHP and TOPSIS methods: a case study from the paper mills; pp. 666–673. [Google Scholar]
- 153.Kabadayi N. Fuzzy hybrid FMEA for risk assessment in service industry: an integrated intuitionistic fuzzy AHP and TOPSIS approach. Advancements in fuzzy reliability theory. IGI Global. 2021:43–75. [Google Scholar]
- 154.Zadeh L. Fuzzy sets. Inf Control. 1965;8(3):338–353. [Google Scholar]
- 155.Behret H. Group decision making with i?ntuitionistic fuzzy preference relations. Knowl Base Syst. 2014;70:33–43. [Google Scholar]
- 156.Xu Z., Liao H. Intuitionistic fuzzy analytic hierarchy process. IEEE Trans Fuzzy Syst. 2014;22(4):749–761. [Google Scholar]
- 157.Abdullah L., Najib L. Sustainable energy planning decision using the intuitionistic fuzzy analytic hierarchy process: choosing energy technology in Malaysia. Int J Sustain Energy. 2016;35(4):360–377. [Google Scholar]
- 158.Boran F.E., Genç S., Kurt M., Akay D. A multi-criteria intuitionistic fuzzy group decision making for supplier selection with TOPSIS method. Expert Syst Appl. 2009;36(8):11363–11368. [Google Scholar]
- 159.Karande P., Zavadskas E., Chakraborty S. A study on the ranking performance of some MCDM methods for i?ndustrial robot selection problems. Int J Ind Eng Comput. 2016;7(3):399–422. [Google Scholar]
- 160.Butler J., Jia J., Dyer J. Simulation techniques for the sensitivity analysis of multi- criteria decision models. Eur J Oper Res. 1997;103(3):531–546. [Google Scholar]
- 161.Tabrizi J.S., Rezapour R., Saadati M., Seifi S., Amini B., Varmazyar F. Medical waste management in community health centers. Iran J Public Health. 2018;47(2):286. [PMC free article] [PubMed] [Google Scholar]
- 162.Janagi R., Shah J., Maheshwari D. Scenario of management of medical waste in US and UK: A Review. J. Global Trends Pharmaceut. Sci. 2015;6(1):2328–2339. [Google Scholar]
- 163.Acharya D.B., Singh M. Minerva Press; New Delhi: 2000. The book of hospital waste management. [Google Scholar]
- 164.Johannessen L.M., Dijkman M., Bartone C., Hanrahan D., Boyer G., Chandra C. The International Bank for Reconstruction and Development/The World Bank; Washington: 2000. Healthcare waste management guidance note. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.