Abstract
Background
Although social distancing is necessary to decrease COVID-19 dissemination, it might also be associated with suicidal ideation. Therefore, we analyzed the impact of social distancing and loneliness in suicidal ideation.
Methods
We performed two waves of a snowball sample, web-based survey in Brazil (W1: from May 6th to June 6th, 2020; W2: from June 6th to July 6th, 2020). We assessed whether risk factors related to social relationships (loneliness, living alone, not leaving home, and the number of days practicing social distancing) at W1 were associated with suicidal ideation at W1 and W2 using multiple regression models. Analyses were adjusted for sociodemographic, mental health, and lifestyle variables.
Results
A total of 1,674 (18-75 years old; 86.5% females) were included in our longitudinal sample. Living alone (OR: 1.16; 95%CI = 1.03 - 1.30; p=0.015), number of days practicing social distancing (OR: 1.002; 95%CI = 1.000 - 1.004; p=0.027), and loneliness (OR: 1.49; 95%CI = 1.32 - 1.68; p<0.001) were associated with suicidal ideation in the cross-sectional analysis of W1. Only loneliness (OR= 2.12; 95%CI = 1.06 - 4.24; p = 0.033) remained significant as a risk factor to suicidal ideation in the longitudinal analysis between both waves.
Limitation
Snowball, convenience sample design limits outcome estimates. Assessments were not objectively performed.
Conclusion
Loneliness was consistently associated with the incidence of suicidal ideation, while other variables, such as living alone, not leaving home, and the number of days practicing social distancing, were not. Measures to overcome loneliness are therefore necessary to reduce suicidal ideation during pandemics.
Keywords: Suicidal ideation, Loneliness, Social distancing, COVID-19
1. Introduction
The Coronavirus Disease 2019 (COVID-19) outbreak was sudden and unexpected worldwide (Moreno et al., 2020). Since December 2019, when the first case was reported, it has swept across the world (Galea et al., 2020). This has brought unprecedented efforts to institute “social distancing”, resulting in changes in behavioral patterns and restrictions of daily activities (Galea et al., 2020). While these steps can mitigate the spread of this disease, they might have immediate and long-term consequences for mental health and well-being (Galea et al., 2020). Social distancing and lockdown, along with unpredictability and uncertainty, are risk factors to mental health issues, since they might lead to social isolation and loneliness (Moreno et al., 2020, Moutier, 2020).
Objective social isolation and loneliness are distinct. The former is outwardly visible to an onlooker, inferred by the lack of social proximity and engagement with others, even though the individuals themselves may not feel alone (Cacioppo and Cacioppo, 2018, McClelland et al., 2020). Loneliness is a subjective psychological state identified through introspection, in which an individual may feel alone even within a crowd (McClelland et al., 2020). Loneliness is a painful emotional state caused by a discrepancy between a person's desired meaningful social relationships, and the perceived present relationships (Lee et al., 2021, Mann et al., 2017, Wang et al., 2017). Evidence demonstrates that measures of social isolation (such as living alone) or loneliness could both be major risks for premature mortality and suicide (Cerel et al., 2019, Fazel and Runeson, 2020, McClelland et al., 2020, Moutier, 2020, Naghavi, 2019, Turecki et al., 2019, World Health Organization 2014).
A US Centers for Disease Control and Prevention (CDC) survey (Czeisler et al., 2020) released in August 2020 found that approximately twice as many respondents reported serious considerations of suicide in the previous 30 days than did adults in the United States in 2018 (Lipari and Park-Lee, 2019), regarding the prior year (10.7% versus 4.3%). Suicides are likely to have increased in the 1918 influenza pandemic and the 2003 SARS epidemic as well (Brooks et al., 2020, Gunnell et al., 2020). Social distancing might lead to social isolation and increase the risk of suicide. In fact, quarantine-related social isolation was a prominent factor associated with suicide during emerging viral disease outbreaks before the COVID-19 pandemic (Leaune et al., 2020). However, insufficient studies explored the association of suicidal ideation with objective and subjective measures of social relationships during the COVID-19 pandemic. Recognizing whether and how the pandemic increases suicide risk can help designing suicide prevention strategies (Gunnell et al., 2020).
1.1. Aims of the study
The present study aims to analyze whether subjective (such as loneliness) and objective (such as social distancing, living alone, and staying only indoors) measures of social relationships are risk factors for suicidal ideation in the COVID-19 pandemic considering a one-month follow-up. We also tested whether sociodemographic, lifestyle and pandemic-related variables were associated with suicidal ideation. Based on previous findings, we hypothesized that measures of social relationships would be associated with suicidal ideation in both the cross-sectional and longitudinal analyses. Finally, we hypothesized that previously known risk factors for suicidal ideation (eg, depression) would be observed, especially factors that could worsen during the pandemic, such as economic factors (unemployment and financial crisis) and population with increased stress burden (health professionals).
2. Methods
2.1. Setting, participants, and design
The present study is part of a larger cohort project, composed of three temporal waves (0, 1, and 6 months) that aimed to investigate the impact of the COVID-19 pandemic on mental health in the Brazilian population at different stages of the pandemic. The cohort used online questionnaires as the method of data collection, due to the need of complying with recommendations of social distancing. For inclusion in the baseline cohort, participants needed to be at least 18 years old, live in Brazil at the time of data collection, and have access to the internet. For inclusion in the second wave of data collection, participants needed to provide their email address at the end of the baseline questionnaire and agree to receive an email with the specific questionnaires regarding that wave. All online questionnaires were provided to eligible participants using an online platform (Survey Monkey) (Survey Monkey, n.d.), and the baseline questionnaire was advertised through social media (Facebook, Instagram, and Whatsapp) to reach participants. The advertisement explicitly stated that the survey was anonymous.
This investigation is based on the first 2 waves of data collection of this cohort. The Wave 1 (W1) questionnaire was administered between May 6th and June 6th, 2020. The Wave 2 (W2) data collection was performed between June 6th and July 6th, 2020, in which participants who agreed to receive the questionnaire of the second wave received an email one month after the completion of the baseline questionnaire. Considering that our study started approximately 2 months after the confirmation of the first case of COVID-19 in Brazil (Ministério da Saúde, n.d.), our analyzes refer to an early stage of the pandemic.
The study was approved by the local research ethics committee All participants signed the informed consent before answering the online questionnaires. The second wave questionnaire was only sent to those who agreed to write down their email address at the end of the baseline questionnaire. After completion of each questionnaire, contact information for suicide prevention services and mental health support centers located in Brazil were provided to participants.
This study is in accordance with the STROBE guidelines (von Elm et al., 2007). Table S1 in the supplemental material presents the STROBE checklist.
2.2. Measures
2.2.1. Survey instruments
The online questionnaires for data collection included validated scales, such as the 9-item Patient Health Questionnaire (PHQ-9) (Santos et al., 2013), the Generalized Anxiety Disorder-7 (GAD-7) (Moreno et al., 2016a), the Alcohol Use Disorders Identification Test-Concise (AUDIT-C) (Bradley et al., 2003, Bush et al., 1998, Meneses-Gaya et al., 2010), and the Revised UCLA Loneliness Scale (R-UCLA) (Hughes et al., 2004). In addition, the questionnaires covered sociodemographic variables, the COVID-19 pandemic and social distancing measures, alcohol and substance misuse, suicidal ideation, adverse life experiences, lifestyle variables, among other clinical variables. Both a Portuguese (original versions) and a translated English version of the questions used in this study were provided in the supplemental material (see Method S1).
2.2.2. Suicidal Ideation
Participants were classified as having suicidal ideation if they answered “yes” to the following question: “Over the past month, have you had any desire or thoughts about killing yourself?”.
2.2.3. Subjective measure of social relationship
Loneliness was measured with the 3-item short form of R-UCLA (Hughes et al., 2004). The scale asks “How often do you feel you lack companionship?”, “How often do you feel left out?”, and “How often do you feel isolated from others?”. Response options for each item are “hardly ever or never”, “some of the time”, or “often” (equating to scores of 1,2, and 3, respectively). Total scores range from 3 to 9 and higher scores indicate greater loneliness (Hughes et al., 2004), with scores ≥ 6 indicating important loneliness (Steptoe et al., 2013). We used Cronbach's α and McDonald's ω to test internal reliability (Lucke, 2005, Raykov, 1997).
2.2.4. Objective measures of social relationship
Social distancing was defined in accordance with the Centers for Disease Control and Prevention (CDC) and includes measures such as staying away from agglomerations or groups of people and keeping a distance (at least 2 meters) from others whenever possible (Centers for Disease Control and Prevention, 2020). We calculate the time spent practicing such measures with the question: "How many days have you been practicing social distancing due to the COVID-19 outbreak?".
We also asked the following questions to evaluate social isolation: "How many people have been living under the same roof as you since the COVID-19 outbreak began? (Number of people including you)" and "After the outbreak of COVID-19 in your country, how often have you left your house? (Number of days/week)". For the first question, we analyzed whether the participants lived alone or not. For the second question, we analyzed whether the participants left home at least once a week or not.
2.2.5. Mental Health
Depressive symptoms were measured with the PHQ-9 (Kroenke et al., 2001). A score equal to or greater than 9 is considered a positive screening result for depression in the Brazilian population (Santos et al., 2013). Anxiety symptoms were measured using the GAD-7 (Moreno et al., 2016b). A positive indicator of signs and symptoms of anxiety disorders is considered to be a value equal to or greater than 10. The AUDIT-C was used to evaluate alcohol use (Bush et al., 1998). In men, a score of 4 or more is considered positive; in women, a score of 3 or more is considered positive. The questions about cocaine/crack use and benzodiazepines were based on the ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) instrument (Group and WHO ASSIST Working Group, 2002), asking about use over the previous 30 days.
2.2.6. Statistical analysis
Data analysis was performed using SPSS V21.0. Descriptive statistics were reported in terms of mean and standard deviation (Mean(SD)), median and interquartile range (Md[1st-3rd IQR]), or absolute and relative frequencies. We estimated Cronbach's α (assuming tau-equivalence) and McDonald's ω (not assuming tau-equivalence) to test the internal reliability of instruments not previously published in Brazilian Portuguese. Values >0.7 and >0.9 are considered of acceptable and excellent reliability (i.e. sum scores reliably measure a given construct) (Nunnally et al., 1994).
All statistical estimates were performed using survey weight. This procedure applies iterative post-stratification to match population margins to the survey sample proportions, which can approximate the demographic characteristics of the sample to the Brazilian population. We weighted our sample using Brazilian population margins regarding sex at birth, age groups, the region of residency, race/ethnicity, and household income according to the last Brazilian census (Instituto Brasileiro de Geografia e Estatística, 2010). Survey weight was trimmed to 20. Survey weight and scale reliability were run using R (R Core Team 2020) version 4.0.3 using the packages survey (Lumley, 2020) (rake function) and semTools (Jorgensen et al., 2020) (reliability function) respectively.
2.2.7. Cross-sectional analyses
Initially, cross-sectional analyses were conducted on a sample of 8,104 participants who were included at baseline. Multiple Poisson regression analyses were performed to assess the sole effect of social isolation and loneliness factors on suicidal ideation at baseline with adjustments for potential confounders. We selected confounders based on existing studies (Turecki et al., 2019) and theoretical assumptions (Gunnell et al., 2020, Wasserman et al., 2020). Associations between social factors and suicidal ideation may be confounded by age, gender, sexual orientation, marital status, income, geographical area, education, healthcare professional, unemployment, financial crisis during the pandemic, quality of family relationships, quality of friend relationships, religion, meditation, sleep quality, physical activity, childhood trauma, previous suicide attempt, family history of suicide, depressive symptoms (PHQ-9), anxiety symptoms (GAD-7), being at severe risk for alcohol abuse (AUDIT-C), cocaine/crack use, and benzodiazepines use.
Before multiple Poisson regression, we calculated univariate Poisson regression, prevalence ratios (PR), and confidence intervals (95%CI) for each possible confounding. Any variable in the univariate model that was significant at p<0.1 was entered in multiple Poisson regression analyses.
2.2.8. Longitudinal analyses
After the cross-sectional analyses, data analysis was conducted on a longitudinal subsample, comprising 1,674 individuals who completed both first and second waves of data collection (0 and 1 month).
The participants were divided into four groups: 1) Incidents (participants who had no suicidal ideation in W1 and had in W2); 2) Remitted (participants who had suicidal ideation in the W1 and did not have it in W2; 3) Absent (who did not have suicidal ideation in any wave); 4) Persistent (who had suicidal ideation in both waves). We used the chi-square with the adjusted residual test for categorical variables and Kruskal-Wallis with the Dunn's test for quantitative variables to analyze social relationship variables between these four groups.
Multinomial logistic regression analyses were then performed with 4 groups (according to the presence of suicidal ideation in the two waves) as outcome. The independent variables were the same as in the cross-sectional analyses except for cocaine/crack users due to the small number of participants with this condition, that is, we used just the variables from W1 to predict our outcome (W2). We calculated the odds ratio (OR) and confidence intervals (95%CI) for each possible confounding.
3. Results
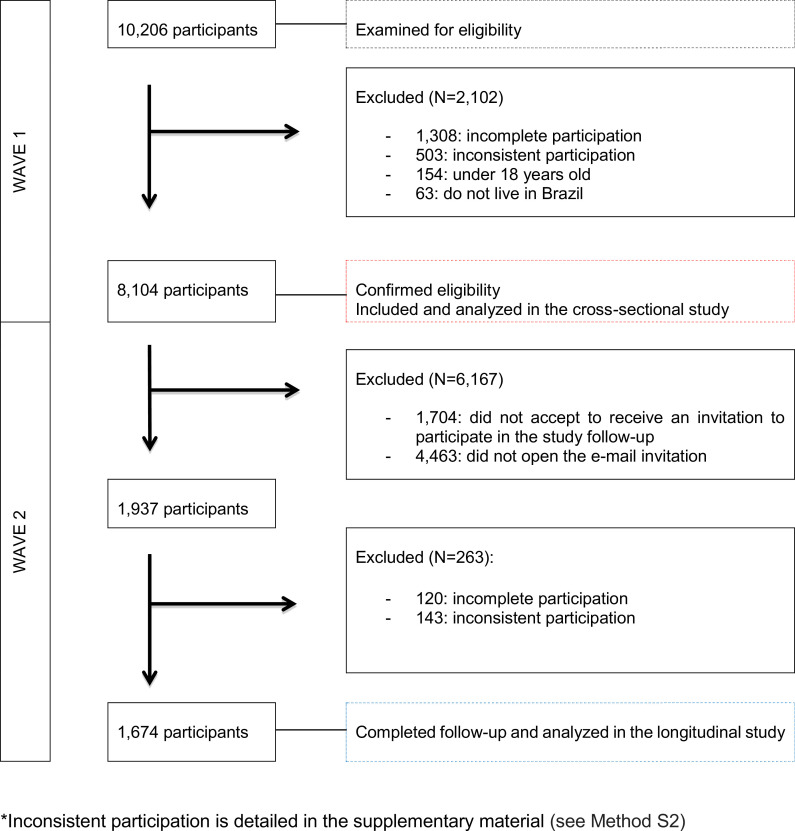
Fig. 1 shows the flowchart of the participants' inclusion process.
Fig. 1.
Flowchart of participants selection.
In the sample included in the longitudinal study, the mean age was 38.6 (14.1) years and 86.5% were females. However, our weighted sample was very close to being representative of the Brazilian population, according to data from the last national census (Instituto Brasileiro de Geografia e Estatística, 2010). Table 1 presents the demographic and personal characteristics of respondents in the cross-sectional and longitudinal study. The rate of suicidal ideation in W1 was 22.6% and in W2, 20.3% (p=0.005). Table S2 in the supplemental material presents the variation in the rates of mental health symptoms and loneliness between W1 and W2.
Table 1.
Demographic and personal characteristics of participants
| Variable | Cross-sectional study (n=8,104) | Longitudinal study* (n=1,674) | ||
|---|---|---|---|---|
| n (%) | Weighted sample (%) | n (%) | Weighted sample (%) | |
| Age | ||||
| 18 – 30 years | 3026 (37.3) | 30.6 | 662 (39.5) | 32.2 |
| 30 – 39 years | 2559 (31.6) | 24.2 | 532 (31.8) | 25.7 |
| 40 – 49 years | 1332 (16.4) | 18.0 | 248 (14.8) | 16.1 |
| 50 – 59 years | 822 (10.1) | 15.4 | 159 (9.5) | 14.9 |
| ≥ 60 years | 365 (4.5) | 11.8 | 73 (4.4) | 11.0 |
| Sex | ||||
| Female | 6791 (83.8) | 56.1 | 1448 (86.5) | 61.1 |
| Male | 1313 (16.2) | 43.9 | 226 (13.5) | 38.9 |
| Sexual orientation | ||||
| Heterosexual | 6816 (84.1) | 77.7 | 1398 (83.5) | 77.7 |
| No Heterosexual | 1288 (15,9) | 22.3 | 276 (16.5) | 22.3 |
| Marital status | ||||
| No partner | 3655 (45.1) | 55.8 | 793 (47.4) | 62.3 |
| With partner | 4449 (54.9) | 44.2 | 881 (52.6) | 37.7 |
| Living alone | 807 (10.0) | 15.3 | 175 (10.5) | 18.5 |
| Leaving home | 6792 (83.8) | 83.2 | 1377 (82.3) | 87.3 |
| Education | ||||
| Elementary/Middle/High School | 1326 (16.4) | 32.6 | 206 (12.3) | 21.0 |
| Undergraduate | 3705 (45.7) | 46.4 | 772 (46.1) | 50.9 |
| Postgraduate | 3073 (37.9) | 21.0 | 696 (41.6) | 28.1 |
| * Data from the baseline | ||||
| Table 1. (Continued) | ||||
| Variable | Cross-sectional study (n=8,104) | Longitudinal study* (n=1,674) | ||
| n (%) | Weighted sample (%) | n (%) | Weighted sample (%) | |
| Income | ||||
| A/B | 2830 (34.9) | 9.3 | 654 (39.1) | 12.7 |
| C | 1694 (20.9) | 7.8 | 333 (19.9) | 9.2 |
| D/E | 3580 (44.2) | 82.9 | 687 (41.0) | 78.1 |
| Region | ||||
| North | 500 (6.2) | 8.4 | 73 (4.4) | 7.4 |
| Northeast | 2008 (24.8) | 29.1 | 324 (19.4) | 26.6 |
| Midwest | 843 (10.4) | 7.8 | 133 (7.9) | 8.9 |
| Southeast | 2430 (30.0) | 37.8 | 568 (33.9) | 36.9 |
| South | 2323 (28.7) | 17.0 | 576 (34.4) | 20.2 |
| Color | ||||
| White | 4253 (52.5) | 50.1 | 959 (57.3) | 48.4 |
| Not White | 3851 (47.5) | 49.9 | 715 (42.7) | 51.6 |
| Unemployed | 1322 (16.3) | 33.7 | 274 (16.4) | 32.0 |
| Healthcare professional | 2448 (30.2) | 19.5 | 517 (30.9) | 21.3 |
| * Data from the baseline | ||||
3.1. Cross-sectional analyses in Wave 1
R-UCLA presented acceptable to good reliability (α=0.861; ω=0.791). The multiple Poisson regression analysis of W1 showed that living alone (OR=1.16; 95%CI = 1.03-1.30; p=0.015), number of days practicing social distancing (OR=1.002; 95%CI = 1.000-1.004; p=0.027), and loneliness (OR=1.49; 95%CI = 1.32-1.68; p<0.001) were associated with suicidal ideation. This analysis was adjusted for all confounding variables mentioned in the methods as they were significantly associated with suicidal ideation in the univariate Poisson analysis (Table S3 - supplementary material).
Table 2.
Multiple Poisson regression analysis to assess the isolated effect of social isolation factors on suicidal ideation in Wave 1
| Variables | Prevalence of SI (%) | Crude PR (CI 95%) | Adjusteda PR (CI 95%) | p |
|---|---|---|---|---|
| Leaving home | ||||
| Yes | 19.2% | 1.04 (0.91 – 1.18) | 0.99 (0.88 – 1.13) | 0.927 |
| No | 19.7% | 1.00 | 1.00 | |
| Living alone | ||||
| Yes | 21.1% | 1.13 (1.00 – 1.28) | 1.16 (1.03 – 1.30) | 0.015 |
| No | 18.9% | 1.00 | 1.00 | |
| Social distancing (time) |
– | 1.000 (1.000 - 1.001) | 1.002 (1.000 – 1.004) | 0.027 |
| R- UCLA Positive | ||||
| Yes | 27.1% | 3.06 (2.69 – 3.47) | 1.49 (1.32 - 1.68) | <0.001 |
| No | 8.7% | 1.00 | 1.00 |
adjusted for age, gender, sexual orientation, marital status, income, geographical area, education, healthcare professional, unemployment, financial crisis during the pandemic, quality of family relationships, quality of friend relationships, religion, meditation, sleep quality, physical activity, childhood trauma, previous suicide attempt, family history of suicide, GAD-7, PHQ-9, cocaine / crack use, benzodiazepines use and AUDIT-C. Abbreviations: SI, Suicidal Ideation; PR, Prevalence Ratio; CI, Confidence Interval; AUDIT-C, Alcohol Use Disorders Identification Test - Concise; GAD-7, Generalized Anxiety Disorder 7-item; PHQ-9, Patient Health Questionnaire 9-item; R-UCLA, three-item short form of the Revised University of California, Los Angeles Loneliness Scale.
3.2. Longitudinal analyses
Table 3 shows the comparison of the isolation variables between the four suicidal ideation groups.
Table 3.
Association of social isolation / loneliness between suicidal ideation groups
| Variables | No SI(n=1,227; 73.3%) | Remitted (n=108; 6.4%) | Incidents(n=70; 4.2%) | Persistents(n=270; 16.1%) | P |
|---|---|---|---|---|---|
| Leaving home - n(%) | 1,035 (84.4)a | 83 (76.9) | 52 (74.3) | 213 (78.9) | 0.012 |
| Living alone – n(%) | 203 (16.5)b | 20 (18.5) | 5 (7.1)b | 81 (30.0)a | <0.001 |
| Social distancing (yes) – n(%) | 1,179 (96.1) | 106 (99.1) | 66 (94.3) | 259 (96.3) | 0.366 |
| Social distancing time (days) – median (P25 – P75) | 52 (44 – 60)1 | 55 (50 – 60)1,2 | 51,4 (60 – 61)1,2 | 60 (49 – 63)2 | <0.001 |
| R-UCLA positive > 6 – n(%) | 670 (54.6)b | 58 (53.7)b | 55 (78.6)a | 248 (91.9)a | <0.001 |
positive association by adjusted residual test to 5% significance
negative association by adjusted residual test to 5% significance;
equal numbers do not differ by Dunn's test at 5% significance. Abbreviations: SI, Suicidal Ideation; R-UCLA, three-item short form of the Revised University of California, Los Angeles Loneliness Scale.
equal numbers do not differ by Dunn's test at 5% significance. Abbreviations: SI, Suicidal Ideation; R-UCLA, three-item short form of the Revised University of California, Los Angeles Loneliness Scale.
After adjustment for all covariates, loneliness was directly associated (OR= 2.12; 95%CI = 1.06-4.24; p=0.033) with the incidence of suicidal ideation between W1 and W2.
Table 4.
Multiple Multinomial Logistic Regression Analysis to assess the adjusted effect of isolation factors on suicidal ideation groups between W1 and W2 (longitudinal).
| Variables | No SI | Remitted | Incidents | Persistents | |||||
|---|---|---|---|---|---|---|---|---|---|
| OR (IC 95%) | P* | OR (IC 95%) | P* | OR (IC 95%) | P* | ||||
| Leaving home | 1.00 | 0.66 (0.37-1.18) | 0.160 | 0.54 (0.29-1.02) | 0.057 | 0.64 (0.39-1.05) | 0.078 | ||
| Living alone | 1.00 | 3.02 (1.56-5.85) | 0.001 | 0.65 (0.24-1.78) | 0.400 | 2.52 (1.48-4.31) | 0.001 | ||
| Social distancing time (days) | 1.00 | 1.01 (0.99-1.02) | 0.321 | 1.00 (0.99-1.02) | 0.874 | 1.01 (1.00-1.02) | 0.020 | ||
| R-UCLA positive | 1.00 | 0.31 (0,18-0,54) | <0.001 | 2.12 (1.06-4.24) | 0.033 | 3.95 (2.25-6.96) | <0.001 | ||
Centers of Control Disease and Prevention, n.d. Risk and Protective Factors [WWW Document]. Suicide Prevention. URL https://www.cdc.gov/suicide/factors (accessed 2.9.21).
adjusted for age, gender, sexual orientation, marital status, income, geographical area, education, profession, unemployment, financial crisis during the pandemic, quality of family relationships, quality of friend relationships, religion, meditation, sleep quality, physical activity, childhood trauma, previous suicide attempt, family history of suicide, GAD-7, PHQ-9, benzodiazepines use and AUDIT-C.
Among the adjustment covariables, female gender (OR= 2.76; 95%CI = 1.33-5.75; p = 0.007), depression (OR= 4.61; 95%CI = 1.66-12.80; p=0.003), previous suicide attempt (OR= 2.70; 95%CI = 1.39-5.25; p=0.003), and being a health professional (OR= 2.00; 95%CI = 1.06-3.79; p=0.033) were also directly associated with the incidence of suicidal ideation. However, participants at severe risk for alcohol abuse (OR= 0.37; 95%CI = 0.18-0.78; p=0.009), users of benzodiazepine (OR= 0.47; 95%CI = 0.24-0.93; p=0.030) and being unemployed (OR= 0.43; 95%CI = 0.20-0.91; p=0.028) were inversely associated. There was no association between age and the incidence of suicidal ideation (Table S4 - supplemental material).
4. Discussion
This is the first longitudinal study to analyze the impact of objective and subjective social relationship measures on suicidal ideation during the COVID-19 pandemic. Despite the cross-sectional analyses showing that living alone, number of days practicing social distancing, and feeling of loneliness were associated with suicidal ideation; only feeling of loneliness remained a predictor of suicidal ideation in the longitudinal analyses, even after adjustment for multiple confounding variables. The loneliness rate was high in our sample, with 61.6% of participants scoring above the cutoff point.
Contrary to our initial hypothesis, objective measures of social relationships were not associated with an increased risk of suicidal ideation in a one-month follow-up. This result is similar to a cross-sectional study (Bryan et al., 2020) conducted from March 18 to April 4, 2020, that evaluated a representative sample of 10,625 U.S. adults. To understand these findings, we can make a comparison with other situations in which physical distance is imposed. The specific condition of physical isolation (being in isolation or segregation cells) of life in prison intensifies suicidal risk (Calati et al., 2019). However, having greater social support can be a protective factor for suicidal ideation in a prison population even with other risk factors present, such as major depressive disorder (Richie et al., 2019). During the pandemic, social distancing measures may not mean a distance in social relations because it is possible to stay connected in non-physical ways, via text, phone, or videoconferencing. Several authors have highlighted the importance of increasing communication with friends, family members, and loved ones (Fiorillo and Gorwood, 2020, Thorp, 2020). In this sense, a longitudinal study assessed a nationwide sample of 1,545 American adults and showed that participants felt more social support during the initial phase of the COVID-19 pandemic than they did before it (Luchetti et al., 2020).
Addressing loneliness is more complex and nuanced than simply increasing social connection (Lim et al., 2020). Since the number of friends or social interactions is not predictive of loneliness, increasing opportunities for social interaction and increasing social support can address social isolation more than loneliness (Masi et al., 2011). Our finding that loneliness is associated with suicidal ideation is consistent with a cross-sectional study (Jorgensen et al., 2020) that analyzed a representative sample of 1,013 U.S. adults on April 9-10, 2020. In this study, loneliness was elevated, with 43% of respondents scoring above published cutoffs, and was strongly associated with depression and suicidal ideation. Before the pandemic, both the objective condition of being alone (e.g. living alone) and the subjective feeling of being alone (i.e. loneliness) were associated with suicidal outcomes. However, the subjective feeling of loneliness had a major impact on both suicide ideation and suicide attempts (Calati et al., 2019). A meta-analysis of 31 studies indicated a 57% likelihood increase of suicidal ideation for elderly participants with poor social relationships. The functional (subjective) measures of social relationships (e.g. loneliness), however, were more predictive than structural (objective) measures (e.g. social isolation) (Chang et al., 2017).
The relationship between loneliness and suicidal ideation is supported by the interpersonal theory of suicide. According to the theory, suicidal ideation can be induced by the simultaneous presence of two interpersonal constructs — thwarted belongingness and perceived burdensomeness (i.e. the perception to represent a burden for others) (Joiner, 2007). Thwarted Belongingness includes loneliness and the absence of reciprocal care (Van Orden et al., 2010). Chu and colleagues conducted meta-analyses with 122 distinct published and unpublished samples and the findings supported the interpersonal theory: the interaction between thwarted belongingness and perceived burdensomeness was significantly associated with suicidal ideation (Chu et al., 2017).
Loneliness led to social, mental, and physical health problems before the Covid-19 pandemic (Jorgensen et al., 2020) and with the possible increase during the pandemic (McGinty et al., 2020), measures are needed to overcome loneliness. A meta-analysis with 50 studies of interventions to reduce loneliness shows that the most successful interventions addressed maladaptive social cognition by cognitive behavioral therapy (Masi et al., 2011). In older people, loneliness can create serious problems that could also not be alleviated with social support only (Chen et al., 2014); however, there are promising technological interventions (for example, digital applications (apps), online social networks, and social robots) that can be effective in improving emotional support, in addition to social support. These technologies are appropriate for measures of social distancing during pandemics (Pu et al., 2019).
To deal with loneliness it is also important to know the possible associated factors, because some of these factors, such as social anhedonia, can be an obstacle to treatment. Social anhedonia is characterized by social disinterest and a lack of pleasure from social contact, indicating a deficit in the need to belong (Brown et al., 2007). Tan and colleagues conducted a cross-sectional online survey with 824 undergraduate students to investigate the association between social anhedonia, loneliness, and social functioning. Both social anhedonia and loneliness were negatively correlated with social functioning and mediation analyses revealed that loneliness fully mediated the relationship between social anhedonia and overall social functioning. According to the authors, individuals who are high in social anhedonia have an innate tendency to withdraw from social interactions, which potentially reduces the opportunity for them to build or gain subjectively meaningful social networks (Tan et al., 2020). Future studies are also needed to assess how interventions in social anhedonia could impact loneliness, social functioning, and suicidal ideation.
A meta-analysis of 15 observational case-control studies (from 1965 to 2016) showed an association between anhedonia and suicidal ideation, independently of depression (Ducasse et al., 2018). Besides, other studies have shown the association between anhedonia and suicidal ideation in medical students (Loas et al., 2019) and physicians (Loas et al., 2018). Loas and colleagues found that in physicians, anhedonia can be associated with suicidal ideation, but it also functions as a mediator in the relationship between suicidal ideation and perceived burdensomeness or thwarted belongingness, supporting the interpersonal theory of suicide for this population of health professionals (Loas et al., 2018).
Being a health professional, previous history of suicide attempts, depression, and female sex were directly associated with the incidence of suicidal ideation between W1 and W2. Special attention deserves to be given to health professionals during epidemics and pandemics (Brooks et al., 2020; Gunnell et al., 2020). During the COVID-19 outbreak, a study analyzed data from the baseline assessment (May 5 – July 23, 2020) of a cohort of 5,450 Spanish hospital workers and they found a thirty-day prevalence of 3.5% for active ideation, plans, or attempts (Mortier et al., 2021). This suggests that suicidal thoughts and behaviors among hospital workers during the COVID-19 outbreak are at least three times higher than in the general Spanish population before the COVID-19 outbreak (Mortier et al., 2021). Health professionals working in hospitals should receive regular clinical screening for depression, anxiety, and suicidality by mental health workers (Xiang et al., 2020).
Previous suicide attempts and mental illness, such as depression, are known risk factors for suicide (Centers of Controle Disease and Prevention, 2021). Although we do not have other studies to compare in the COVID-19 pandemic scenario, it is important to highlight that one of the main adverse consequences of the COVID-19 pandemic is loneliness (Holmes et al., 2020) that in turn is associated with depression and suicide attempts across the lifespan. Females have also been found to have a generally higher risk of developing psychological issues during the COVID-19 pandemic period (Wang et al., 2020). Data of 34,778 individuals from the University College London COVID-19 Social Study, collected between March 21st and April 20th, 2020, suggests self-harm and thoughts of suicide were higher among women (Iob et al., 2020). Besides that, a cross-sectional study assessed 10,067 individuals during the COVID-19 pandemic (April 1-10, 2020) in Bangladesh and showed that being female is one of the risk factors for suicidal ideation (Mamun et al., 2021).
Being unemployed, at serious risk of alcohol abuse, and use of benzodiazepines were protective factors. Of note, these results are within a multiple regression framework where the effects of alcohol, benzodiazepines, and unemployment are conditioned to the effects of other variables in the model, such as loneliness, depression, anxiety, occupation, and education. Therefore, after adjusting for symptoms and socioeconomic variables, being unemployed in a pandemic situation may indicate that a subject was not exposed to work-specific stressors that could lead to suicide ideation, such as burnout. Besides, some jobs increase the possibility of contagion and some people may have felt protected by less exposure. At the same time, alcohol use and benzodiazepines use at the early stages of the pandemic may have exerted therapeutic effects and subsequently reducing the probability of self-reporting suicide ideation, especially considering the estimated regression model. Nonetheless, these variables need to be investigated with proper study design and as the main predictor to avoid Table 2 fallacy (Lederer et al., 2019).
Our cross-sectional findings indicate that in the first wave collection time there was a greater difficulty for the participants in dealing with social distancing and living alone. In fact, the rate of suicidal ideation decreased from 22.6% to 20.3% between the two waves, which may show a better adaptation to risk factors. Despite the decrease, these numbers represent a significant increase (approximately 5 times higher) about 3.8% of a previous study of the prevalence of suicidal ideation in the Brazilian population in 2013 (Carpena et al., 2019).
This study has several strengths that are worth discussing. First, the study has a longitudinal design that allows a better understanding of the cause and effect relationship between predictors and outcome. Second, our national sample recruited individuals covering all 27 federative units in Brazil and the weighting of the sample allowed the demographic characteristics to be close to the Brazilian demographic census. Third, we had a sample size that allowed us to analyze a wide range of variables and thus we corrected our findings for several confounding factors. Fourth, this is one of the first studies to assess the impacts of the pandemic on mental health in low- and middle-income countries (LMIC).
Our study also has some limitations. First, we followed social distancing recommendations and did a self-report survey online, but, as with any survey of this type, there may be variations in the way some questions are interpreted by participants. Second, our weighted sample has demographic characteristics very close to the Brazilian demographic census but it is not fully compatible and the last Brazilian census was made a decade ago (2010). Therefore, we need to be cautious when interpreting the rates as a representative prevalence of the Brazilian population. Third, the outcome of this study is a complex and delicate question and participants with suicidal ideation may choose not to answer due to the sensitivity of the topic. Conversely, it is possible that the population with these symptoms would be more willing to respond because of their interest in the subject. Fourth, our cross-sectional findings should also be viewed with caution due to the possibility of reverse causality. Finally, we had a significant loss of participants between the two waves of evaluation and this may have happened for several reasons, such as worsening mental health status, suicide in the interval of evaluations, loss of interest in following the study, among others. Despite the limitations, this study provides valuable information about the impact of social relationships on suicidal ideation during the early stage of the COVID-19 pandemic. Since the evolution of the COVID-19 pandemic is still unpredictable and mental health problems are likely to persist even after its complete control, our results can help guide the development of psychological interventions to minimize the effects of the pandemic on suicide.
In summary, loneliness was consistently associated with the incidence of suicidal ideation in a one-month follow-up during the initial stage of the COVID-19 pandemic, while objective social relationship variables related to social isolation, such as living alone, not leaving home, and the number of days practicing social distancing, were not. Therefore, interventions that address the subjective feeling of loneliness will be necessary to reduce suicidal ideation during pandemics.
CRediT authorship contribution statement
Thyago Antonelli-Salgado: Conceptualization, Data curtion, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing, Writing – original draft. Gabriela Massaro Carneiro Monteiro: Conceptualization, Data curtion, Methodology, Visualization, Writing – review & editing. Grasiela Marcon: Conceptualization, Data curtion, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing. Thiago Henrique Roza: Conceptualization, Data curtion, Investigation, Methodology, Validation, Visualization, Writing – review & editing. Aline Zimerman: Conceptualization, Data curtion, Investigation, Methodology, Validation, Visualization, Writing – review & editing. Maurício Scopel Hoffmann: Conceptualization, Data curtion, Investigation, Methodology, Validation, Visualization, Writing – review & editing. Bo Cao: Conceptualization, Methodology, Visualization, Writing – review & editing. Simone Hauck: Visualization, Writing – review & editing. André Russowsky Brunoni: Conceptualization, Data curtion, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing, Writing – original draft. Ives Cavalcante Passos: Conceptualization, Data curtion, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing, Writing – original draft.
Declaration of Competing Interest
All authors has no conflict to declare.
Acknowledgments
MSH is supported by the US National Institute of Mental Health (Grant No. R01MH120482) under a post-doctoral research fellowship at Universidade Federal do Rio Grande do Sul and by the UK Academy of Medical Sciences (Newton International Fellowship NIF\R1\181942). ARB receives scholarships and support from São Paulo Research State Foundation (FAPESP 18/10861-7, 19/06009-7), the Brazilian National Council of Scientific Development (CNPq-1B), University of São Paulo Medical School (FMUSP), the UK Academy of Medical Sciences (Newton Advanced Fellowship), and the International Health Cohort Consortium (IHCC). ICP is CNPq (Brazilian National Council for Scientific and Technological Development) research fellow and supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil and by FIPE (Fundo de Incentivo à Pesquisa e Eventos) from Hospital de Clínicas de Porto Alegre, Brazil.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.04.044.
Appendix. Supplementary materials
References
- Bradley K.A., Bush K.R., Epler A.J., Dobie D.J., Davis T.M., Sporleder J.L., Maynard C., Burman M.L., Kivlahan D.R. Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT) Arch. Internal Med. 2003 doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown L.H., Silvia P.J., Myin-Germeys I., Kwapil T.R. When the need to belong goes wrong: the expression of social anhedonia and social anxiety in daily life. Psychol. Sci. 2007;18:778–782. doi: 10.1111/j.1467-9280.2007.01978.x. [DOI] [PubMed] [Google Scholar]
- Bryan C.J., Bryan A.O., Baker J.C. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. Suicide Life Threat. Behav. 2020;50:1223–1229. doi: 10.1111/sltb.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K., Kivlahan D.R., McDonell M.B., Fihn S.D., Bradley K.A. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP) Arch. Intern. Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. Alcohol Use Disorders Identification Test. [DOI] [PubMed] [Google Scholar]
- Cacioppo J.T., Cacioppo S. The growing problem of loneliness. Lancet. 2018;391:426. doi: 10.1016/S0140-6736(18)30142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calati R., Ferrari C., Brittner M., Oasi O., Olié E., Carvalho A.F., Courtet P. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J. Affect. Disord. 2019;245:653–667. doi: 10.1016/j.jad.2018.11.022. [DOI] [PubMed] [Google Scholar]
- Carpena M.X., Martins-Silva T., Costa F.S., Darley R., Loret de Mola C. Contextual risk factors of depression and suicidal thoughts in Brazilian adults: a multilevel analysis. Braz J Psychiatry. 2019;41:433–436. doi: 10.1590/1516-4446-2018-0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . CDC; 2020. Social Distancing, Quarantine, and Isolation [WWW Document].https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html URL. accessed 4.11.20. [Google Scholar]
- Centers of Controle Disease and Prevention . 2021. Risk and Protective Factors [WWW Document]. Suicide Prevention.https://www.cdc.gov/suicide/factors URL. accessed 2.9.21. [Google Scholar]
- Cerel J., Brown M.M., Maple M., Singleton M., van de Venne J., Moore M., Flaherty C. How many people are exposed to suicide? Not six. Suicide Life Threat. Behav. 2019;49:529–534. doi: 10.1111/sltb.12450. [DOI] [PubMed] [Google Scholar]
- Chang Q., Chan C.H., Yip P.S.F. A meta-analytic review on social relationships and suicidal ideation among older adults. Soc. Sci. Med. 2017;191:65–76. doi: 10.1016/j.socscimed.2017.09.003. [DOI] [PubMed] [Google Scholar]
- Chen Y., Hicks A., While A.E. Loneliness and social support of older people in China: a systematic literature review. Health Soc. Care Community. 2014;22:113–123. doi: 10.1111/hsc.12051. [DOI] [PubMed] [Google Scholar]
- Chu C., Buchman-Schmitt J.M., Stanley I.H., Hom M.A., Tucker R.P., Hagan C.R., Rogers M.L., Podlogar M.C., Chiurliza B., Ringer F.B., Michaels M.S., Patros C.H.G., Joiner T.E. The interpersonal theory of suicide: a systematic review and meta-analysis of a decade of cross-national research. Psychol. Bull. 2017;143:1313–1345. doi: 10.1037/bul0000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducasse D., Loas G., Dassa D., Gramaglia C., Zeppegno P., Guillaume S., Olié E., Courtet P. Anhedonia is associated with suicidal ideation independently of depression: a meta-analysis. Depress. Anxiety. 2018;35:382–392. doi: 10.1002/da.22709. [DOI] [PubMed] [Google Scholar]
- Fazel S., Runeson B. Suicide. N. Engl. J. Med. 2020;382:266–274. doi: 10.1056/NEJMra1902944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63:e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing. JAMA Internal Med. 2020 doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Group, W.A.W., WHO ASSIST Working Group . 2002. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. [DOI] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J., COVID-19 Suicide Prevention Research Collaboration Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys. Res. Aging. 2004 doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística, IBGE; 2010. Sinopse do Censo Demográfico: 2010. [Google Scholar]
- Iob E., Steptoe A., Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry. 2020;217:543–546. doi: 10.1192/bjp.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner T. Harvard University Press; 2007. Why People Die by Suicide. [Google Scholar]
- Jorgensen, T.D., Pornprasertmanit, S., Schoemann A M Rosseel, 2020. SemTools: useful tools for structural equation modeling.
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leaune E., Samuel M., Oh H., Poulet E., Brunelin J. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: A systematic rapid review. Prev. Med. 2020;141 doi: 10.1016/j.ypmed.2020.106264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lederer D.J., Bell S.C., Branson R.D., Chalmers J.D., Marshall R., Maslove D.M., Ost D.E., Punjabi N.M., Schatz M., Smyth A.R., Stewart P.W., Suissa S., Adjei A.A., Akdis C.A., Azoulay É., Bakker J., Ballas Z.K., Bardin P.G., Barreiro E., Bellomo R., Bernstein J.A., Brusasco V., Buchman T.G., Chokroverty S., Collop N.A., Crapo J.D., Fitzgerald D.A., Hale L., Hart N., Herth F.J., Iwashyna T.J., Jenkins G., Kolb M., Marks G.B., Mazzone P., Moorman J.R., Murphy T.M., Noah T.L., Reynolds P., Riemann D., Russell R.E., Sheikh A., Sotgiu G., Swenson E.R., Szczesniak R., Szymusiak R., Teboul J.-L., Vincent J.-L. Control of confounding and reporting of results in causal inference studies. guidance for authors from editors of respiratory, sleep, and critical care journals . Ann. Am. Thorac. Soc. 2019;16:22–28. doi: 10.1513/AnnalsATS.201808-564PS. [DOI] [PubMed] [Google Scholar]
- Lee S.L., Pearce E., Ajnakina O., Johnson S., Lewis G., Mann F., Pitman A., Solmi F., Sommerlad A., Steptoe A., Tymoszuk U., Lewis G. The association between loneliness and depressive symptoms among adults aged 50 years and older: a 12-year population-based cohort study. Lancet Psychiatry. 2021 doi: 10.1016/s2215-0366(20)30383-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim M.H., Eres R., Vasan S. Understanding loneliness in the twenty-first century: an update on correlates, risk factors, and potential solutions. Soc. Psychiatry Psychiatr. Epidemiol. 2020;55:793–810. doi: 10.1007/s00127-020-01889-7. [DOI] [PubMed] [Google Scholar]
- Lipari, R.N., Park-Lee, E., 2019. Key substance use and mental health indicators in the United States: results from the 2018 national survey on drug use and health. substance abuse and mental health services administration. Published. [PubMed]
- Loas G., Lefebvre G., Rotsaert M., Englert Y. Relationships between anhedonia, suicidal ideation and suicide attempts in a large sample of physicians. PLoS One. 2018;13 doi: 10.1371/journal.pone.0193619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loas G., Solibieda A., Rotsaert M., Englert Y. Suicidal ideations among medical students: the role of anhedonia and type D personality. PLoS One. 2019;14 doi: 10.1371/journal.pone.0217841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., Sutin A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020;75:897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucke J.F. The α and the ω of congeneric test theory: An extension of reliability and internal consistency to heterogeneous tests. Appl. Psychol. Meas. 2005;29:65–81. [Google Scholar]
- Lumley, T., 2020. Survey: analysis of complex survey samples.
- Mamun M.A., Sakib N., Gozal D., Bhuiyan A.I., Hossain S., Bodrud-Doza M., Al Mamun F., Hosen I., Safiq M.B., Abdullah A.H., Sarker M.A., Rayhan I., Sikder M.T., Muhit M., Lin C.-Y., Griffiths M.D., Pakpour A.H. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J. Affect. Disord. 2021;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann F., Bone J.K., Lloyd-Evans B., Frerichs J., Pinfold V., Ma R., Wang J., Johnson S. A life less lonely: the state of the art in interventions to reduce loneliness in people with mental health problems. Soc. Psychiatry Psychiatr. Epidemiol. 2017;52:627–638. doi: 10.1007/s00127-017-1392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi C.M., Chen H.-Y., Hawkley L.C., Cacioppo J.T. A meta-analysis of interventions to reduce loneliness. Pers. Soc. Psychol. Rev. 2011;15:219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland H., Evans J.J., Nowland R., Ferguson E., O'Connor R.C. Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta-analysis of prospective studies. J. Affect. Disord. 2020;274:880–896. doi: 10.1016/j.jad.2020.05.004. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meneses-Gaya C., Zuardi A.W., Loureiro S.R., Hallak J.E.C., Trzesniak C., de Azevedo Marques J.M., Machado-de-Sousa J.P., Chagas M.H.N., Souza R.M., Crippa J.A.S. Is the full version of the AUDIT really necessary? Study of the validity and internal construct of its abbreviated versions. Alcohol. Clin. Exp. Res. 2010;34:1417–1424. doi: 10.1111/j.1530-0277.2010.01225.x. [DOI] [PubMed] [Google Scholar]
- Ministério da Saúde, n.d. Painel Coronavírus [WWW Document]. Coronavírus Brasil. URL https://covid.saude.gov.br/ (accessed 1.20.21). 2021.
- Moreno A.L., DeSousa D.A., Lisbôa Ana Maria Frota, Manfro G.G., Salum G.A., Koller S.H., Osório F.L., Crippa J.A.S. Factor structure, reliability, and item parameters of the Brazilian-Portuguese version of the GAD-7 questionnaire. Temas em Psicologia. 2016 doi: 10.9788/tp2016.1-25. [DOI] [Google Scholar]
- Moreno A.L., DeSousa D.A., Souza A.M.F.L.P., Manfro G.G., Salum G.A., Koller S.H., Osório F.de L., Crippa J.A.de S. Factor structure, reliability, and item parameters of the brazilian-portuguese version of the GAD-7 questionnaire. Temas Psicol. 2016;24:367–376. [Google Scholar]
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., Cannon M., Correll C.U., Byrne L., Carr S., Chen E.Y.H., Gorwood P., Johnson S., Kärkkäinen H., Krystal J.H., Lee J., Lieberman J., López-Jaramillo C., Männikkö M., Phillips M.R., Uchida H., Vieta E., Vita A., Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortier P., Vilagut G., Ferrer M., Serra C., de Dios Molina J., López-Fresneña N., Puig T., Pelayo-Terán J.M., Pijoan J.I., Emparanza J.I., Espuga M., Plana N., González-Pinto A., Ortí-Lucas R.M., de Salázar A.M., Rius C., Aragonès E., Del Cura-González I., Aragón-Peña A., Campos M., Parellada M., Pérez-Zapata A., Forjaz M.J., Sanz F., Haro J.M., Vieta E., Pérez-Solà V., Kessler R.C., Bruffaerts R., Alonso J., MINDCOVID Working Group Thirty-day suicidal thoughts and behaviors among hospital workers during the first wave of the Spain COVID-19 outbreak. Depress. Anxiety. 2021 doi: 10.1002/da.23129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moutier C. Suicide prevention in the COVID-19 era: transforming threat into opportunity. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.3746. [DOI] [PubMed] [Google Scholar]
- Naghavi M., Global Burden of Disease Self-Harm Collaborators Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the global burden of disease study 2016. BMJ. 2019;364:l94. doi: 10.1136/bmj.l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally J., Jum N., Bernstein I.H., Bernstein I. McGraw-Hill Companies,Incorporated; 1994. Psychometric Theory. [Google Scholar]
- Pu L., Moyle W., Jones C., Todorovic M. The effectiveness of social robots for older adults: a systematic review and meta-analysis of randomized controlled studies. Gerontologist. 2019;59:e37–e51. doi: 10.1093/geront/gny046. [DOI] [PubMed] [Google Scholar]
- Raykov T. Scale reliability, cronbach's coefficient alpha, and violations of essential tau-equivalence with fixed congeneric components. Multivar. Behav. Res. 1997;32:329–353. doi: 10.1207/s15327906mbr3204_2. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2020. A language and environment for statistical computing.
- Richie F.J., Bonner J., Wittenborn A., Weinstock L.M., Zlotnick C., Johnson J.E. Social support and suicidal ideation among prisoners with major depressive disorder. Arch. Suicide Res. 2019:1–8. doi: 10.1080/13811118.2019.1649773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos I.S., Tavares B.F., Munhoz T.N., de Almeida L.S.P., da Silva N.T.B., Tams B.D., Patella A.M., Matijasevich A. Sensibilidade e especificidade do patient health questionnaire-9 (PHQ-9) entre adultos da população geral. Cadernos Saúde Pública. 2013 doi: 10.1590/s0102-311x2013001200006. [DOI] [PubMed] [Google Scholar]
- Steptoe A., Shankar A., Demakakos P., Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. U. S. A. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Survey Monkey 2021 [WWW Document], n.d. . SurveyMonkey Inc. URL pt.surveymonkey.com.
- Tan M., Shallis A., Barkus E. Social anhedonia and social functioning: loneliness as a mediator. Psych J. 2020;9:280–289. doi: 10.1002/pchj.344. [DOI] [PubMed] [Google Scholar]
- Thorp H.H. Time to pull together. Science. 2020;367:1282. doi: 10.1126/science.abb7518. [DOI] [PubMed] [Google Scholar]
- Turecki G., Brent D.A., Gunnell D., O'Connor R.C., Oquendo M.A., Pirkis J., Stanley B.H. Suicide and suicide risk. Nat. Rev. Dis. Primers. 2019;5:74. doi: 10.1038/s41572-019-0121-0. [DOI] [PubMed] [Google Scholar]
- Van Orden K.A., Witte T.K., Cukrowicz K.C. 2010. The interpersonal theory of suicide. Psychological. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P., Initiative STROBE. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann. Intern. Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Lloyd-Evans B., Giacco D., Forsyth R., Nebo C., Mann F., Johnson S. Social isolation in mental health: a conceptual and methodological review. Soc. Psychiatry Psychiatr. Epidemiol. 2017;52:1451–1461. doi: 10.1007/s00127-017-1446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman D., Iosue M., Wuestefeld A., Carli V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatry. 2020;19:294–306. doi: 10.1002/wps.20801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2014. Preventing Suicide: a Global Imperative. [Google Scholar]
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.