Abstract
Background
: The impact of the coronavirus disease 2019 (COVID-19) on the mental health of the US population is unclear. This study drew on two nationally representative samples to compare the prevalence rate of anxiety in the U.S. before and during the 2020 COVID-19 pandemic.
Methods
: The Generalized Anxiety Disorder-2 (GAD-2) screening tool was used to detect the proportion of US adults screening positive for high levels of anxiety symptoms. Anxiety symptoms was assessed in 2019 using the National Health Interview Survey (NHIS; N = 30,915) and during the pandemic using biweekly surveys collected as part of the Understanding America Study (UAS; N=8,022 Obs.=121,768) between March and December 2020.
Results
: The proportion of participants with high levels of anxiety symptoms increased significantly from 8.1% (95% CI[7.7, 8.5]) in 2019 to 21.4% (95% CI[19.9, 22.9]) at the beginning of April, 2020. The prevalence then declined to 11.4% (95% CI[10.3, 12.5]) in May and remained 3% above 2019 levels until December 2020. This pattern of increasing anxiety between 2019 and April 2020 followed by a rapid decrease in anxiety was identified across all demographic characteristics examined.
Limitations
: The NHIS and UAS samples differ in their sampling and mode of administration which may bias comparisons between samples.
Conclusions
: Anxiety symptoms increased markedly during the onset of the COVID-19 pandemic and reduced quickly as stay-at-home orders were lifted. These findings highlight the importance of providing mental health supports during future lockdowns and suggest that resilience in mental health may have been a key population-level response to the demands of the pandemic.
Keywords: COVID-19, Coronavirus infection, Mental health, anxiety, Longitudinal research, Nationally representative study
Introduction
As of March 2021, the coronavirus disease 2019 (COVID‐19) pandemic has led to almost 30 million confirmed cases of the virus and 535,000 deaths in the U.S. (OWID, 2021). Mandatory stay-at-home orders and physical distancing policies launched to curtail the virus spread have profoundly disrupted daily life. Nations across the globe have been faced with job losses, economic uncertainty, and the social isolation of citizens (Altig et al., 2020; Robinson & Daly, 2020). For these reasons, it has been widely predicted by experts and the media that the pandemic may have severe and long-lasting mental health effects (Holmes et al., 2020; O'Connor et al., 2020).
However, to date, there is relatively little direct evidence in support of this idea. A high prevalence of anxiety, depression, and post-traumatic disorder has been repeatedly reported over the course of the pandemic in studies relying largely on convenience samples or without comparable pre-pandemic assessments (Vindegaard et al., 2020). Due to the lack of large-scale nationally representative studies with data before and during the pandemic it is unclear whether the prevalence of psychiatric conditions has increased throughout the pandemic. Three multi-wave probability-based general population studies have shown that psychological distress and depression increased as the pandemic emerged in the U.S. (Daly et al., 2021b, Ettman et al., 2020, McGinty et al., 2020). A fourth study found that the proportion of adults re reporting high levels of anxiety or depressive symptoms increased over three-fold between 2019 and April-May 2020 in the U.S. (Twenge & Joiner, 2020).
While these studies have shown that substantial numbers of U.S. adults reported worsening mental health in the initial weeks of the pandemic, the longer-term effects as the pandemic progressed remain unclear. The above increase in anxiety and depressive symptoms occurred while unprecedented restrictions on travel were introduced, schools and universities were closed, and mandatory stay-at-home orders were being issued in most states (Tolbert et al., 2020), but less is known about mental health as restrictions were eased after the initial period of the pandemic.
In this study, we therefore examine the prevalence of anxiety symptoms in two US probability-based nationally representative samples over the course of 2020 (i.e. March - December 2020) compared to 2019 pre-pandemic data, in order to chart the longitudinal profile of population level anxiety during the 2020 COVID pandemic.
Methods
Sample
The National Heath Interview Survey (NHIS) is an annual, cross-sectional, in-person survey administered by the National Center for Health Statistics (NCHS) within the Centers for Disease Control and Prevention (CDC). The NHIS uses a stratified cluster probability design to obtain a nationally representative sample of noninstitutionalized civilians. NHIS data is collected continuously throughout the year and the sample is designed to produce nationally representative samples for each quarter. The NHIS is a key source of up-to-date information on health trends in the United States and the 2019 sample includes 31,997 adults. We excluded 3.4% of observations with missing anxiety or covariate data and the sample size for the current study was 30,915.
The Understanding American Study (UAS) is a national probability-based sample of US adults recruited via address-based sampling from the U.S. Postal Service Computerized Delivery Sequence file (Alattar et al., 2018). The UAS is a longitudinal online study and eligible participants without internet access are provided with internet-enabled tablets to ensure sample representativeness. Of a total of 8,815 panel members 8,131 provided data as part of the UAS COVID-19 study. From March 10, 2020 to December 31, 2020 UAS participants were invited to participate in 20 biweekly surveys and participants submitted approximately 15 surveys on average over this period (total responses = 124,685). In this study we excluded 109 participants and 2,899 observations (2.3% of total responses) due to missing anxiety or covariate data leaving a sample size of 8,022 adults and 121,768 responses for the current study.
The NHIS and UAS samples were broadly comparable on age, gender, and race/ethnicity, as shown in Table S1. However, the UAS included a larger portion of participants with a college degree and the NHIS sample included a larger portion of adults with household income levels ≥ $50,000 and ‘Other’ race/ethnicity participants. This study involved secondary analysis of the NIHS and UAS anonymized microdata files which did not require institutional approval from the Maynooth University Social Research Ethics Sub-Committee.
Measures
Demographic characteristics
Participants reported their age (grouped into 18-39, 40-59, and 60+ years), sex (male, female), race/ethnicity (White, Hispanic, Black, Asian, other race/ethnicity), education (college degree, no degree) and household income levels (low income = $0-$49,999, high income = $50,000+ per annum).
Anxiety
Participants completed the validated Generalized Anxiety Disorder (GAD-2) screening measure for assessing anxiety in the general population (Donker et al., 2011). The GAD-2 items ask how often in the past 2 weeks participants have been bothered by core anxiety symptoms: “feeling nervous, anxious, or on edge” and “not being able to stop or control worrying”. Both items were rated on a scale with response options not at all = 0, several days = 1, more than half of days = 2, and nearly every day = 3. Response to both items were summed to give a score from 0-6 with scores ≥ 3 classed as above the validated threshold for detecting probable cases of GAD (sensitivity = .86, specificity = .83) (Donker et al., 2011). A recent diagnostic meta-analysis has shown that the GAD-2 cut-off of ≥ 3 optimally balances sensitivity (0.76) and specificity (0.81) for detecting GAD (Plummer et al., 2016).
Analytical strategy
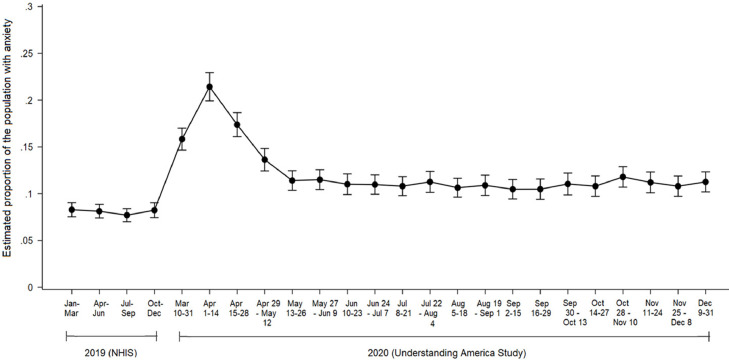
We first compared the prevalence of anxiety in the NHIS in each quarter of 2019 and at each of 20 time-points in the UAS. Specifically, we estimated the weighted percentage of the sample with anxiety with 95% confidence intervals for the overall sample for each time-period. Our initial analyses indicated that anxiety levels were highly stable and did not change significantly from May to December 2020 (see Figure 1 ). For this reason, we focused our in-depth analyses of changes in anxiety levels on the UAS survey waves at the pandemic onset (i.e. March – May, 2020) and six months later in December 2020. Logistic regression analysis followed by the margins post-estimation command was used to estimate changes in the prevalence of anxiety from 2019 levels over the course of the pandemic.
Figure 1.
Proportion of U.S. adults with anxiety in 2019 and throughout the COVID-19 pandemic in 2020.
Note: Estimates from 2019 are derived from the National Health Interview Survey (NHIS) (N = 30,915) and 2020 estimates are derived from the Understanding America Study (N = 8,022, observations = 121,768).
In the NHIS and UAS survey sampling weights were applied to adjust for the differential probabilities of selection into the survey and to align the sample with the distribution of demographic characteristics in the US civilian population. A comprehensive account of the weighting methodologies can be found in Bramlett et al. (2020) and Angrisani et al. (2019).
Results
The proportion of adults experiencing anxiety in the U.S. was stable throughout 2019 (min. = 7.7%, max. = 8.3%) and then increased from an average of 8.1% (95% CI[7.7, 8.5]) in 2019 to 15.8% (95% CI[14.6, 17.0]) in March 2020 and rose to 21.4% (95% CI[19.9, 22.9]) in the first half of April (see Table 1 and Figure 1). Anxiety levels then declined significantly to 11.4% (95% CI[10.3, 12.5]) in May (13-26) and remained at this level until December 2020, as can be seen in Figure 1.
Table 1.
Comparisons of the prevalence of anxiety in 2019 and at six time-points during the COVID-19 pandemic from March 10th to December 31st 2020.
| Date / Year | Jan - Dec 2019 | Mar 10-31, 2020 | Apr 1-14, 2020 | Apr 15-28, 2020 | Apr 29-May 12 2020 | May 13-26, 2020 | Dec 9-31, 2021 |
|---|---|---|---|---|---|---|---|
| N | 30,915 | 6,813 | 5,392 | 6,199 | 6,301 | 6,239 | 5,840 |
| % [95% CI] | % [95% CI] | % [95% CI] | % [95% CI] | % [95% CI] | % [95% CI] | % [95% CI] | |
| Adults ≥ 18 y | 8.1 [7.7, 8.5] | 15.8⁎⁎⁎ [14.6, 17.0] | 21.4⁎⁎⁎ [19.9, 22.9] | 17.4⁎⁎⁎ [16.1, 18.7] | 13.6⁎⁎⁎ [12.5, 14.8] | 11.4⁎⁎⁎ [10.3, 12.5] | 11.3⁎⁎⁎ [10.1, 12.4] |
| Age group, y | |||||||
| 18 – 39 | 9.1 [8.5, 9.8] | 20.8⁎⁎⁎ [18.5, 23.2] | 25.3⁎⁎⁎ [22.4, 28.1] | 21.4⁎⁎⁎ [18.9, 23.8] | 16.9⁎⁎⁎ [14.7, 19.2] | 13.9⁎⁎⁎ [11.8, 16.0] | 15.3⁎⁎⁎ [13.0, 17.6] |
| 40 – 59 | 8.4 [7.7, 9.0] | 15.9⁎⁎⁎ [13.9, 17.9] | 23.5⁎⁎⁎ [20.9. 26.1] | 18.5⁎⁎⁎ [16.3, 20.8] | 14.8⁎⁎⁎ [12.8, 16.9] | 12.5⁎⁎⁎ [10.5, 14.4] | 11.0⁎⁎ [9.2, 12.8] |
| 60+ | 6.4 [5.8, 6.9] | 9.4⁎⁎⁎ [7.8. 10.9] | 14.3⁎⁎⁎ [12.2, 16.4] | 11.1⁎⁎⁎ [9.3, 12.9] | 8.2* [6.7, 9.7] | 7.2 [5.8, 8.7] | 6.7 [5.3, 8.1] |
| Male | 5.8 [5.3, 6.3] | 11.9⁎⁎⁎ [10.3, 13.5] | 17.2⁎⁎⁎ [15.1, 19.3] | 14.2⁎⁎⁎ [12.4. 16.1] | 11.1⁎⁎⁎ [9.5, 12.8] | 8.4⁎⁎⁎ [6.9, 9.8] | 8.1⁎⁎ [6.7, 9.6] |
| Female | 10.2 [9.6, 10.8] | 19.5⁎⁎⁎ [17.8, 21.3] | 25.4⁎⁎⁎ [23.2, 27.6] | 20.3⁎⁎⁎ [18.5, 22.2] | 16.0⁎⁎⁎ [14.3, 17.6] | 14.3⁎⁎⁎ [12.6, 15.9] | 14.2⁎⁎⁎ [12.6, 15.9] |
| Hispanic | 7.1 [6.1, 8.0] | 17.3⁎⁎⁎ [13.6, 20.9] | 24.4⁎⁎⁎ [19.4, 29.4] | 19.0⁎⁎⁎ [14.9, 23.0] | 14.4⁎⁎⁎ [10.8, 17.9] | 12.6⁎⁎⁎ [9.1, 16.2] | 9.6 [6.5, 12.7] |
| Black | 7.3 [6.2, 8.4] | 11.7⁎⁎ [8.4, 15.0] | 14.4⁎⁎⁎ [10.3, 18.4] | 13.6⁎⁎⁎ [9.9, 17.3] | 9.8 [6.7, 13.0] | 8.7 [5.7, 11.7] | 7.4 [4.4, 10.3] |
| Other race/ethnicity | 5.7 [4.5, 6.8] | 12.4⁎⁎⁎ [7.9, 16.9] | 15.2⁎⁎⁎ [9.5, 21.0] | 11.7⁎⁎ [7.4, 16.1] | 12.6⁎⁎⁎ [8.0, 17.2] | 9.8* [5.5, 14.0] | 11.1⁎⁎ [6.4, 15.7] |
| White | 8.8 [8.3, 9.3] | 16.5⁎⁎⁎ [15.1, 17.9] | 22.5⁎⁎⁎ [20.8, 24.2] | 18.2⁎⁎⁎ [16.6, 19.7] | 14.2⁎⁎⁎ [12.9, 15.6] | 11.7⁎⁎⁎ [10.5, 13.0] | 12.4⁎⁎⁎ [11, 13.7] |
| No college degree | 9.3 [8.8, 9.7] | 16.9⁎⁎⁎ [15.3, 18.4] | 22.2⁎⁎⁎ [20.2, 24.2] | 18.3⁎⁎⁎ [16.6, 20.0] | 14.4⁎⁎⁎ [12.9, 15.9] | 11.2⁎⁎ [9.8, 12.6] | 12.4⁎⁎⁎ [11.0, 13.9] |
| College degree | 5.2 [4.8, 5.7] | 13.8⁎⁎⁎ [12.0, 15.6] | 20.0⁎⁎⁎ [17.6, 22.3] | 15.6⁎⁎⁎ [13.5, 17.6] | 12.1⁎⁎⁎ [10.4, 13.9] | 11.8⁎⁎⁎ [10.0, 13.6] | 9.1⁎⁎⁎ [7.5, 10.8] |
| Low income (<$50,000) | 12.0 [11.4, 12.7] | 19.1⁎⁎⁎ [17.2, 21.1] | 23.9⁎⁎⁎ [21.4, 26.3] | 20.5⁎⁎⁎ [18.3, 22.6] | 17.5⁎⁎⁎ [15.5, 19.5] | 15.2⁎⁎ [13.3, 17.1] | 14.2⁎⁎ [12.4, 16.0] |
| High income (≥$50,000) | 5.7 [5.2, 6.1] | 13.1⁎⁎⁎ [11.7, 14.5] | 19.4⁎⁎⁎ [17.5, 21.4] | 14.9⁎⁎⁎ [13.3, 16.5] | 10.5⁎⁎⁎ [9.1, 11.8] | 8.3⁎⁎⁎ [7.1, 9.6] | 8.2⁎⁎⁎ [6.9, 9.4] |
Note: Those with a GAD-2 score of 3 or greater screened positive for anxiety. The prevalence of anxiety in the 2019 National Health Interview Survey (NHIS) is contrasted with anxiety prevalence rates across six waves from the Understanding America Study (UAS). Significance levels are estimated using logistic regression analysis.
p < .05.
p < .01.
p < .001.
Statistically significant increases in the prevalence of anxiety between 2019 and April 1-14, 2020 were identified across all population subgroups examined, as shown in Table 1. Anxiety levels increased most sharply over this period in young adults aged 18-39 (16.1% increase, 95% CI[13.2, 19.1], p <.001), Hispanic participants (17.3%, 95% CI[12.2, 22.4], p <.001), and females (15.2%, 95% CI[13.0, 17.5], p <.001). In contrast, the smallest increases in anxiety were found amongst older adults aged 60+ (7.9%, 95% CI[5.7, 10.1], p <.001) and Black participants (7.1%, 95% CI[2.9, 11.4], p <.01).
The sharp decline in the prevalence of anxiety between April 1-14 and May 13-26 was statistically significant in the overall sample (10% decrease, 95% CI[8.4, 11.6], p <.001) and for each population subgroup examined with the exception of ‘Other race/ethnicity’ participants (see Table S2), potentially reflecting the small size of this group. The prevalence of anxiety remained 3.2% (95% CI[2.0, 4.4], p <.001) above 2019 levels in December 2020. At this time, the prevalence of anxiety was significantly above 2019 levels for all population subgroups with the exception of older adults, Black, and Hispanic participants. Older adults and Back participants showed close to complete recovery to pre-pandemic anxiety levels, as shown in Table 1.
Discussion
This study aimed to track how reports of anxiety symptoms changed from pre-pandemic levels throughout the COVID-19 pandemic in 2020. Drawing on two nationally representative probability-based samples we showed that U.S. adults were almost three times more likely to report high levels of anxiety symptoms at the beginning of the COVID-19 pandemic compared to a year earlier. In line with prior research (Daly et al., 2021a) the sharpest increases in anxiety were found in young adults and women, groups that were disproportionally impacted by business closures at the onset of the pandemic (ILO, 2020).
However, anxiety levels recovered quickly in the weeks following the initiation of stay-at-home orders, and plateaued after lockdown restrictions were lifted in most states in May, 2020 (Tolbert et al., 2020). Decreases in anxiety were almost universally observed across demographic groups, a trend that corroborates emerging evidence from the U.K indicating that the deterioration in mental health in April 2020 (Daly et al., 2021a) was followed by stabilization and recovery in the months immediately afterwards (Daly and Robinson, 2020a). Two additional large-scale studies of U.K. adults have also shown that anxiety levels declined following the pandemic onset (Fancourt et al., 2020, O'Connor et al., 2020).
It is feasible that this decline occurred because the initial sharp rise in anxiety like symptoms was part of a functional and adaptive response to a major stressful and sizeable threat to society (Bateson et al., 2011). In line with this explanation, people likely adapted to the perceived threat posed by the pandemic and there is evidence that people were less fearful of the virus as knowledge about its transmission and effects was communicated (Daly and Robinson, 2020b), which in turn may explain why anxiety like symptoms then decreased across the course of 2020.
Despite this large-scale recovery, anxiety levels did not return to their pre-pandemic baseline level for most groups. In the general population the prevalence of high levels of anxiety remained over 3 percentage points above 2019 levels from May to December 2020. The anxiety levels of young adults were persistently elevated above 2019 levels suggesting that this group may have been particularly vulnerable to longer-term pandemic effects. This may reflect an enduring impact of the psychosocial consequences of the pandemic over this period. However, it is also possible that differences in the mode of administration or sampling strategies between the NHIS and UAS could partly explain this difference. Distinguishing between these possibilities will now be important. Further, given high levels of anxiety were observed in a range of countries at the onset of the pandemic (Vindegaard et al., 2020; Winkler et al., 2020) testing whether anxiety symptoms declined in a similar fashion in other nations and the role of the COVID-19 situation in shaping trajectories of anxiety will now be crucial.
Strengths of the current study include the use of two large-scale probability-based surveys of U.S. adults and the examination of longitudinal changes in anxiety levels during the COVID-19 pandemic. However, it is important to note that the NHIS and UAS samples differ in their sampling and mode of administration which may bias comparisons between samples. Further, while the GAD-2 is well-validated for detecting high levels of anxiety, longer scales would shed light on the robustness of the national trends identified in this study.
Taken together our findings suggest that while the pandemic may have induced substantial increases in anxiety like symptoms, these increases were largely transient. This conclusion is consistent with the findings of a recent review and meta-analysis examining anxiety symptoms before vs. during the pandemic (Robinson et al., 2021). While prolonged major fluctuations in mental health may not have occurred, it remains possible that a small but enduring effect of the pandemic could have persisted in the population. Therefore, it will be important to ensure that community mental health treatment services are accessible, particularly for young people who are already at high risk of developing mental health difficulties (Auerbach et al., 2018) and may be experiencing significant anxiety symptoms for the first time.
Author Contribution Statement
Dr Daly had access to the data used in the study and takes responsibility for accuracy of the data analysis. MD & ER designed the research, MD analyzed data, & MD and ER performed research and wrote the paper.
Funding Statement
This research received no specific grant from any funding agency, commercial or not-for-profit sector.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration of competing interest
None. ER has previously received funding from Unilever and the American Beverage Association for unrelated research
Acknowledgements
The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. The collection of the UAS COVID-19 tracking data is supported in part by the Bill & Melinda Gates Foundation and by grant U01AG054580 from the National Institute on Aging. We are also grateful to the Centers for Disease Control and Prevention's (CDC) National Center for Health Statistics (NCHS) for their management of the National Health Interview Survey (NHIS) and making the data available. However, these organizations bear no responsibility for the analysis or interpretation of the data.
References
- Alattar L., Messel M., Rogofsky D. An introduction to the Understanding America Study Internet panel. Soc. Secur. Bull. 2018;78:13–28. [Google Scholar]
- Altig D., Baker S., Barrero J.M., Bloom N., Bunn P., Chen S., Thwaites G. Economic uncertainty before and during the COVID-19 pandemic. J. Public Econ. 2020;191 doi: 10.1016/j.jpubeco.2020.104274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angrisani M., Kapteyn A., Meijer E., Saw H.-W. University of Southern California, Center for Economic and Social Research; 2019. Sampling and weighting the Understanding America Study. Working Paper No. 2019-004Retrieved from. [DOI] [Google Scholar]
- Auerbach R.P., Mortier P., Bruffaerts R., Alonso J., Benjet C., Cuijpers P., Kessler R.C. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018;127:623–638. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateson M., Brilot B., Nettle D. Anxiety: an evolutionary approach. Can. J. Psychiatry. 2011;56:707–715. doi: 10.1177/070674371105601202. [DOI] [PubMed] [Google Scholar]
- Bramlett M.D., Dahlhamer J.M., Bose J., Blumberg S.J. New procedures for nonresponse adjustments to the 2019 National Health Interview Survey sampling weights. Centers for Disease Control and Prevention. 2020 Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2019/nonresponse-report-508.pdf. [Google Scholar]
- Daly M., Sutin A.R., Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: Evidence from the UK Household Longitudinal Study. Psychol. Med. 2021 doi: 10.1017/S0033291720004432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Sutin A.R., Robinson E. Depression reported by US adults in 2017-2018 and March and April 2020. J. Affect. Disord. 2021;278:131–135. doi: 10.1016/j.jad.2020.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research. 2020 doi: 10.1016/j.jpsychires.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E, Sutin A, R, Jones A, Daly M. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic. medRXiv. 2021 doi: 10.1101/2021.03.04.21252921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Longitudinal changes in psychological distress in the UK from 2019 to September 2020 during the COVID-19 pandemic: Evidence from a large nationally representative study. PsyArXiv. 2020 doi: 10.31234/osf.io/mjg72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donker T, van Straten A, Marks I, Cuijpers P. Quick and easy self-rating of Generalized Anxiety Disorder: validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI. Psychiatry Research. 2011;58:58–64. doi: 10.1016/j.psychres.2011.01.016. [DOI] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. -e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiat. 2020 doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I., Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiat. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., Robb K.A. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2020 doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic meta-analysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Robinson E., Daly M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the US: Longitudinal evidence from the Understanding America Study. Br. J. Health. Psychol. 2020 doi: 10.1111/bjhp.12493. [DOI] [PubMed] [Google Scholar]
- Our World in Data (OWID) (2021). United States: What is the daily number of confirmed cases?. Retrieved from https://ourworldindata.org/coronavirus/country/united-states?country=~USA.
- Tolbert, J., Kates, J. Levitt, L. (2020). Lifting social distancing measures in America: state actions and metrics. Retrieved from https://www.kff.org/coronavirus-policy-watch/lifting-social-distancing-measures-in-america-state-actions-metrics/.
- Twenge J.M., Joiner T.E. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety. 2020;37(10):954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immu. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler P., Formanek T., Mlada K., Kagstrom A., Mohrova Z., Mohr P., Csemy L. Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol. Psychiatr. Sci. 2020;29:E173. doi: 10.1017/S2045796020000888. [DOI] [PMC free article] [PubMed] [Google Scholar]