Abstract
Background
The coronavirus (COVID-19) pandemic presents an unprecedented crisis with potential negative mental health impacts.
Methods
This study used data collected via Youper, a mental health app, from February through July 2020. Youper users (N = 157,213) in the United States self-reported positive and negative emotions and anxiety and depression symptoms during the pandemic. We examined emotions and symptoms before (pre), during (acute), and after (sustained) COVID-related stay-at-home orders.
Results
For changes in frequency of reported acute emotions, from the pre to acute periods, anxiety increased while tiredness, calmness, happiness, and optimism decreased. From the acute to sustained periods, sadness, depression, and gratitude increased. Anxiety, stress, and tiredness decreased. Between the pre and sustained periods, sadness and depression increased, as did happiness and calmness. Anxiety and stress decreased. Among symptom measures, anxiety increased initially, from the pre to the acute periods, but later returned to baseline.
Limitations
The study sample was primarily comprised of young people and women. The app does not collect racial or ethnicity data. These factors may limit generalizability. Sample size was also not consistent for all data collected.
Conclusions
The present study suggests that although there were initial negative impacts on emotions and mental health symptoms in the first few weeks, many Americans demonstrated resilience over the following months. The impact of the pandemic on mental health may not be as severe as predicted, although future work is necessary to understand longitudinal effects as the pandemic continues.
Keywords: pandemic, mental health, depression, anxiety
When faced with stressful events, people often experience marked shifts in emotional states (e.g., Marco et al., 1999; van Eck et al., 1998). Natural disasters, pandemics, and terrorist attacks are life stressors that can increase symptoms of anxiety and depression and acute negative emotion states. Evidence from prior national and global disasters supports this notion. The September 11th terrorist attacks led to increases in symptoms of post-traumatic stress disorder, depression, and global distress (Brackbill et al., 2009; Silver et al., 2002). However, some work also highlighted resilience in college students and more general populations after the attacks (Matt & Vázquez, 2008; Bonanno et al., 2007). Hurricane Katrina similarly resulted in increased anxiety and trauma-related symptoms (Galea et al., 2007). In early stages of virus spread during the H1N1 pandemic (i.e., April 2009), when concerns about infection were high, data has demonstrated that amongst a large, representative sample of Dutch adults, anxiety levels were high, but declined fairly rapidly (Bults et al., 2011). The aforementioned studies demonstrate that time-limited global disasters may be associated with poor acute or long-term emotional health, although effects may be time-limited, and many people may show resilience.
While prior studies have been helpful in understanding potential responses to pandemics, coronavirus 2019 (COVID-19) has presented an enormous, long-term, global crisis. Importantly, the COVID-19 pandemic has differed from other disasters in duration; the pandemic has been prolonged and uncertain, where most past disasters have had discrete end points. Its immense health, social, economic, and educational implications worldwide are likely to have a significant impact on emotions as people manage pandemic-related concerns alongside isolation and occupational and academic shifts (Pfefferbaum & North, 2020). To date, there is evidence that the COVID-19 pandemic may be associated with greater anxiety and depression in the general population, among healthcare workers, and among those who have contracted the virus (da Silva et al., 2020; Ettman et al., 2020; Pappa et al., 2020).
Although early evidence suggests that the pandemic has been detrimental to mental health, responses to trauma and loss exposure can be quite variable, even within homogeneous subgroups of the population (Silver & Wortman, 1980; Wortman & Silver, 1989, 2001). For example, it is common to observe resilience in the face of stressful or traumatic events (Garcia & Rimé, 2019; Pfefferbaum & North, 2020). While the extant literature surrounding the impact of the COVID-19 pandemic has been helpful to date, studies have been limited in several ways. Studies have been regional (e.g., in parts of Asia, at the epicenter of the pandemic; Qiu et al., 2020; Wang et al., 2020), focused on unique parts of the population (e.g., healthcare workers; Pappa et al., 2020) and have rarely included more than a few time points (Kwong et al., 2020; Wang et al., 2020). Furthermore, while some samples have been large or moderately sized (e.g., Kwong et al., 2020; Qiu et al., 2020), few have included tens of thousands of individuals, limiting the capacity to understand trends in the broader population. Finally, extant studies have generally collected data during a restricted time period, making it difficult to understand change in emotion over many months. The pandemic's impact on mental health warrants study in a large sample of the general population over a broad time period to fully understand the widespread and dynamic effects and to identify sensitive periods in which mental health care or digital interventions are needed.
The Present Study
This study examined effects of the COVID-19 pandemic on mental health among 157,213 users of a publicly available mental health application called Youper AI. We extracted Youper data from February 2 through July 6, 2020. We examined users' reports of (1) positive and negative acute emotions and (2) self-reported symptoms of anxiety and depression. We hypothesized that acute negative emotions (i.e., momentary reports of emotional states, including anxiety and sadness) would increase, and acute positive emotions (i.e., momentary reports of emotional states, including happiness and gratitude) would decrease during initial stages of the pandemic. We also hypothesized initial increases in symptoms of anxiety and depression. Finally, based on prior research showing resilience during stressors (e.g., Bonanno et al., 2007; Bults et al., 2011; Matt & Vázquez, 2008), we hypothesized that after an initial worsening of emotions and symptoms, during later months of the pandemic, people would show improvements in emotions and symptoms. We conducted exploratory analyses to assess whether change in acute emotions and symptoms differed by age, gender, and occupational status.
Method
Participants
The study sample included users of Youper, a mental health application, who were located in the United States. Youper is an app that provides brief cognitive and behavioral interventions. Users can complete mood ratings, use mindfulness meditations, and engage with various cognitive behavioral techniques such as cognitive restructuring and behavioral activation. All app users who had at least one interaction with Youper and who did not opt out of research were included (N = 157,213). Upon signing up for the app, all users reported gender, age, and occupation. Acute emotions were available for the full sample. A smaller proportion of users, who signed up for the Youper app, reported demographics, including (49.70%). A subset of users, who signed up and paid for Youper, reported symptoms of anxiety and/or depression (3.40%; N = 5,326). Participants were between 13 and 100 years old (M = 24.32 years, SD = 9.55 years). The sample included women (83.91%), men (12.81%) and non-binary individuals (3.28%). The application does not collect racial or ethnicity data. See Table 1 for full demographics.
Table 1.
Demographics.
| Demographic | N | % |
|---|---|---|
| Gender | ||
| Female | 63,893 | 83.91 |
| Male | 9,753 | 12.81 |
| Nonbinary | 2,496 | 3.28 |
| Age | ||
| Adolescents (13-18) | 23,615 | 30.24 |
| Late Adolescents (19-22) | 17,027 | 21.80 |
| Young Adults (23-30) | 21,910 | 28.05 |
| Adults (31-40) | 10,232 | 13.10 |
| Older Adults (41-100) | 5,319 | 6.81 |
| Occupation | ||
| Employed Full Time | 24,357 | 15.49 |
| Freelancer/Work Part Time | 5,056 | 3.22 |
| Student Full Time | 22,200 | 14.12 |
| Work and Attend School | 11,552 | 7.35 |
| !Unemployed | 13,869 | 8.82 |
Data Collection Procedures
Data were collected via Youper. Users voluntarily downloaded the app from either Google Play or Apple stores. Users agreed to Youper's privacy policy, which specifies that anonymized data can be used for scientific research. Users had the option to opt out of research in the app settings. As far as ethical considerations, the first authors’ IRB (University of California, Los Angeles) or institutions (Medical University of Vienna; Graz University of Technology) were consulted and did not require IRB approval for the study, given that this was a secondary analysis of de-identified data. Users can engage with Youper repeatedly, but to avoid confounding intervention effects, we only included each user's first interaction with Youper.
Measures
Acute negative and positive emotions were self-reported. At initiation of the app, users were prompted to select their current emotion from a list of 25 options. We analyzed the 9 emotions that were most frequently reported by users (i.e., anxiety, sadness, depression, stress/overwhelm, tiredness, calmness, happiness, optimism, gratitude). We selected the emotions for analysis by reviewing frequency of responses to each of the 25 possible emotions during the study time period. We then ordered emotions based on their frequency and selected the 9 most commonly reported emotions.
Depressive symptoms were measured using an eight-item version of the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001) which assesses symptom frequency in the past two weeks on a four point scale from 0 (not at all) to 3 (nearly every day). The PHQ-9 item (i.e., item 9) that typically addresses suicide ideation, was removed in the version of the measure used by the app due to the fact that collecting suicide data would necessitate a greater level of intervention for people endorsing suicide ideation, which is not possible given the number of app users. Anxiety symptoms were assessed using the seven-item General Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006) questionnaire, which measures frequency of anxiety symptoms over the past two weeks on a four point scale from 0 (not at all) to 3 (nearly every day).
Analyses
Analyses were performed in Stata 14 (StataCorp, 2015). Analyses of fluctuations in reports of emotion across participants during the pandemic used the following time delineations: pre, acute, and sustained. The acute period was the two weeks prior to and three weeks after a stay-at-home order was instituted in the state of residence identified for each user. The dates for the state-specific stay at home orders were obtained from a publicly available website (National Academy for State Health Policy, 2020). The mean stay-at-home order date across all states was March 26, 2020. The pre period was defined as the time between February 2, 2020 (i.e., first day in dataset) and the start of the acute period (M = March 12, 2020). The sustained period was defined as the end of the acute period (M = April 16, 2020) to July 6, 2020 (i.e., last day in dataset).
To calculate predicted probabilities, odds ratios, and respective confidence intervals for fluctuations in reports of acute emotion, we conducted logistic regressions with presence or absence of each acute emotion as the outcome and time (pre, acute, sustained) as the predictor. To conduct pairwise comparisons of the three time periods, we used dummy and backward difference coding to establish the contrasts for the categorical “period” variable. We fit two models per emotion to cover all period pairs. Because we used only users’ first interaction with the app, we did not correct for multiple interactions per user. We used linear regression to calculate the coefficient estimates for the influence of time period on depression and anxiety symptoms. We established the contrasts between the time periods as described above.
To test moderating effects of age, gender, and occupational status, we extended regression models by including an intercept for the moderating variable and an interaction term with the period variable. We performed F-tests of the interaction terms for the linear regression models of depression and anxiety and χ2 tests for the logistic regression models of each acute emotion. Significant interactions (p < .05) were followed by tests of simple effects. To minimize type-1 error, we limited our simple effects tests to the examination of changes in frequency of reported emotions or symptoms from the pre to acute periods and the acute to sustained periods. For moderation analyses, participant age was binned into five categories: 13-18 (Adolescents; n = 23,615); 19-22 (Late Adolescents; n = 17,027); 23-30 (Young Adults; n = 21,910); 31-40 (Adults; n = 10,232); 41- 100 (Older Adults; n = 5,319). Occupation included five categories: full-time employed (n = 24,357), freelance or part-time work (n = 5,056), full-time student (n = 22,200), unemployed (n = 13,869), or work and attend school (n = 11,552).
Results
Acute Negative Emotions
Effect of pandemic
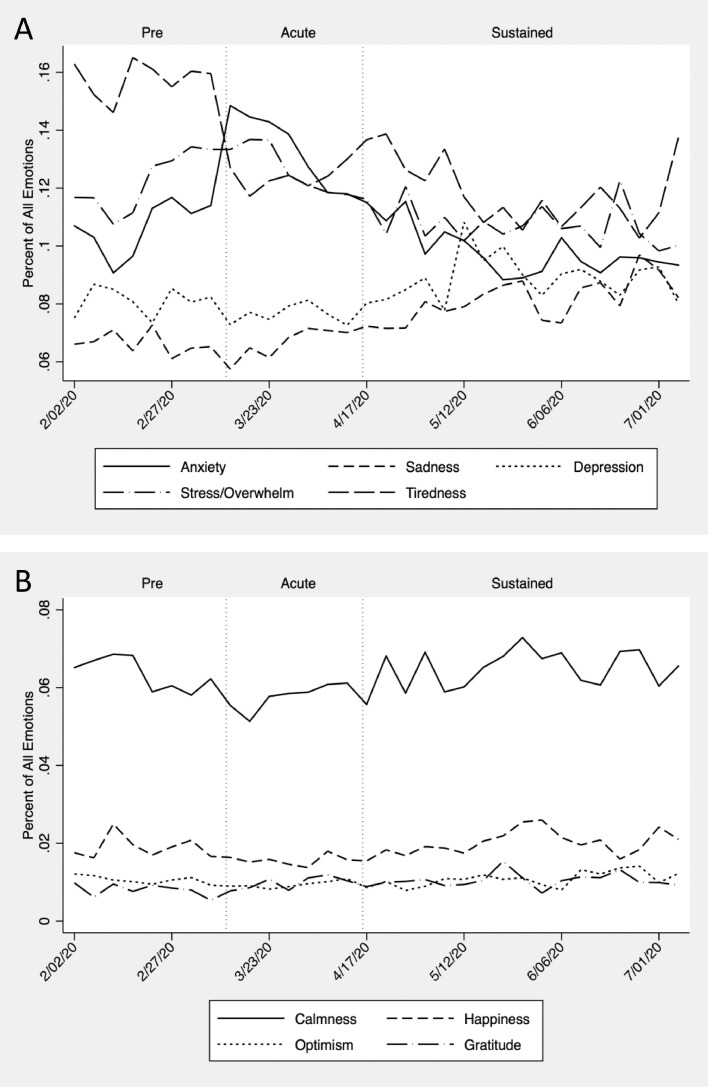
See Table 2 and Figure 1 for results. From the pre to acute periods, the odds of users reporting anxiety statistically significantly increased by 26% (p < .001) whereas tiredness significantly decreased by 24% (p < .001). No other emotions showed statistically significant changes in frequency during this period. From acute to sustained, the odds of users reporting anxiety and stress/overwhelm significantly decreased by 25% (p < .001) and 16% (p < .001) respectively, whereas the odds of users reporting sadness and depression increased by 18% (p < .001) and 13% (p < .001) respectively. From pre to sustained, odds of reporting anxiety decreased by 5% (p < .01). The odds of users reporting stress/overwhelm and tiredness were also significantly reduced compared to the pre period by 13% (p < .001) and 25% (p < .001) respectively, whereas the odds of users reporting sadness and depression remained significantly elevated, by 21% (p < .001) and 9% (p < .001) respectively, compared to pre.
Table 2.
Changes in Acute Emotions Across Pandemic Time Periods.
| Pre (N = 49,831) | Acute (N = 51,094) |
Sustained (N = 56,307) |
Pre v. Acute | Pre v. Sustained | Acute v. Sustained | |
|---|---|---|---|---|---|---|
| Predicted Probability | Odds Ratio [95% CI] | |||||
| Negative & Somatic Emotions | ||||||
| Anxiety | .108 | .132 | .103 | 1.26 [1.21, 1.30] | .95 [.91, .98] | .75 [.73, .78] |
| Sadness | .066 | .067 | .079 | 1.02 [.97, 1.07] | 1.21 [1.15, 1.26] | 1.18 [1.13, 1.24] |
| Depression | .080 | .078 | .087 | .97 [.92, 1.01] | 1.09 [1.04, 1.13] | 1.13 [1.08, 1.18] |
| Stress/Overwhelm | .123 | .127 | .109 | 1.04 [1.00, 1.08] | .87 [.84, .91] | .84 [.81, .87] |
| Tiredness | .158 | .124 | .123 | .76 [.73, .79] | .75 [.72, .77] | .98 [.95, 1.02] |
| Positive Emotions | ||||||
| Calmness | .063 | .058 | .064 | .93 [.88, .98] | 1.02 [.98, 1.08] | 1.10 [1.05, 1.16] |
| Happiness | .019 | .015 | .019 | .80 [.73, .88] | 1.02 [.93, 1.11] | 1.27 [1.15, 1.39] |
| Optimism | .011 | .009 | .010 | .87 [.77, .98] | .98 [.87, 1.10] | 1.13 [1.00, 1.28] |
| Gratitude | .008 | .009 | .010 | 1.12 [.99, 1.28] | 1.25 [1.10, 1.42] | 1.11 [.99, 1.26] |
Note. Statistically significant odds ratios are in bold. Pre included data collected prior to the acute period. Acute was defined as two weeks prior to and three weeks following the start of a stay-at-home order in a given state. Sustained included all data collected following the acute period.
Figure 1.
Changes in Acute (A) Negative Emotions and (B) Positive Emotions During the Pandemic
Note. Positive and negative emotions during the pre, acute and sustained time periods of the pandemic from first interactions of Youper app users. Displayed timelines are given in percent of all reported emotions and are seven-day rolling averages.
Differences by age, gender, and occupation
For anxiety, the Gender by Time interaction was significant χ2 (4, N = 76,142) = 9.28; p = .05. Tests of simple effects showed that women had a significant increase in anxiety from the pre to acute periods (b = .02, p < .01) and a significant decrease from the acute to sustained periods (b = -.03, p < .01) whereas men and non-binary app users did not (ps > .05). For stress/overwhelm, the Gender by Time interaction was also significant χ2 (4, N = 76,142) = 12.38; p = .02. Tests of simple effects showed that women and nonbinary app users had a significant decrease in stress/overwhelm from the acute to sustained periods (b women = -.02, p < .01; b nonbinary = -.04, p = .02) whereas men did not (p > .05). No other interaction effects were statistically significant (ps > .05).
Acute Positive Emotions
Effect of pandemic
From the pre to acute pandemic periods, the odds of users reporting calmness, happiness, and optimism decreased significantly by 7% (p < .01), 20% (p < .001), and 13% (p < .05) respectively. From acute to sustained, odds of reporting calmness and happiness increased significantly by 10% (p < .001) and 27% (p < .001) respectively. Finally, from pre to sustained, odds of reporting gratitude significantly increased by 25% (p < .001). All other positive emotions were not significantly different between pre and sustained periods, suggesting a return to baseline. See Table 2 for detailed results.
Differences by age, gender, and occupation
For optimism, the Occupation by Time interaction was significant χ2 (4, N = 77,034) = 20.66; p = .01. Tests of simple effects showed that optimism decreased significantly in frequency from the pre to acute period among users who were working full-time (b = -.01, p < .01), but not for any other occupation group (ps > .05). No other simple effects were significant for optimism. No other demographic by Time interaction effects were found (ps > .05).
Mood and Anxiety Symptoms
Effect of pandemic
Anxiety symptoms significantly increased between pre and acute periods with a very small effect size (Cohen's d = .12). No other significant effects of Time on anxiety and depression symptoms emerged. See Table 3 for full results and statistics.
Table 3.
Changes in Symptom Measures Over Time.
| Measure | Pre | Acute | Sustained | Pre v. Acute | Pre v. Sustained | Acute v. Sustained |
|---|---|---|---|---|---|---|
| Mean (SD) | Coefficient [95% CI] Cohen's D | |||||
| GAD-7a | 11.92 (5.07) | 12.52 (4.95) | 12.08 (5.12) | .59 [.24, .95] .12 | .16 [-.16, .49] .03 | -.44 [-.76, -.11] .09 |
| PHQ-9b | 14.20 (5.96) | 14.48 (5.72) | 14.12 (5.77) | .28 [-.13, .69] .05 | -.07 [-.45, .31] .01 | -.35 [-.74, .03] .06 |
Note. Abbreviations: GAD-7 = General Anxiety Disorder-7. PHQ-9 = Patient Health Questionnaire-9. Statistically significant pairwise comparisons are bolded. Pre included data collected prior to the acute period. Acute was defined as two weeks prior to and three weeks following the start of a stay-at-home order in a given state. Sustained included all data collected following the acute period.
Competing Interests: Andrea Niles, Jose Hamilton Vargas, Diego Dotta Couto, and Thiago Marafon are employees of Youper and are shareholders in the company
For the GAD-7, sample size varied by pandemic period. In the pre period, N = 1,562. In the acute period, N = 1,600. In the sustained period, N = 2,164.
Sample size also varied by pandemic period for the PHQ-9. In the pre period, N = 1,611. In the acute period, N = 1,517. In the sustained period, N = 2,068.
Differences by age, gender, and occupation
Demographic characteristics did not significantly interact with Time to predict anxiety or depression symptoms (ps > .05).
Discussion
The present study examined changes in prevalence of reported emotions and symptom measures of anxiety and depression as well as life domains and demographic variables associated with these changes in the United States over the first five months of the COVID-19 pandemic.
Results demonstrated that early in the pandemic, both acute reports and symptoms of anxiety increased, but returned to baseline weeks later. As the pandemic continued over months, sadness and depression increased, whereas feelings of stress and tiredness decreased. In terms of positive emotions, calmness, happiness and optimism declined initially, although calmness and happiness increased weeks later. Interestingly, results also showed an increase in gratitude over the time period examined.
Analyses of demographic differences showed that women drove both an initial increase and subsequent decrease in anxiety compared to other genders. It is possible that the increase was due to greater responsibilities around childcare during school closures, especially among working mothers (Power, 2020). It may be that over time, women had greater support from partners, family, friends, or other parents (e.g., forming learning pods), in managing novel demands at home and in school, contributing to decreased anxiety. The same changes over time may explain the decrease in stress reported by women. Demographic analyses also demonstrated that full-time employees drove declines in optimism. This could be due to concerns about financial instability or losing full-time work. This also may relate to more pessimistic viewpoints driven by workplace closures, many of which extended many months beyond lockdown measures (e.g., companies announcing closures until summer of 2021).
The pandemic has undeniably posed challenges around the world and especially in the United States, where cases continue to rise in new virus hot spots (Centers for Disease Control and Prevention, 2020). In accordance, our data suggest that many Americans initially experienced a greater frequency of anxiety and anxiety symptoms (albeit with small effect sizes), as well as greater instances of sadness that emerged as the pandemic persisted. However, consistent with prior studies (e.g., Bults et al., 2011), frequency of reports of anxiety returned to its baseline weeks later, as did happiness (which initially declined). Furthermore, despite increases in reports of sadness and acute depression, people did not show increases in their reports of depressive symptoms. Taken together, these findings suggest that people find ways to cope with life-changing negative circumstances. Findings are also consistent with the fact that habituation to or reductions in anxiety are common in cases of prolonged exposure (Nacasch et al., 2010).
There is some evidence for positive impacts of the pandemic on emotions like increased reports of gratitude as well as decreased reports of stress and tiredness. Possible explanations for mood improvements may be fewer burdens at work and school, less time away from home and commuting (Clark et al., 2020), more social connection inside the home (Cohen & Wills, 1985), and gratitude for basic needs being met during a chaotic period (Tay & Diener, 2011). Therefore, it is possible that the pandemic offered some people an opportunity to refocus on priorities (e.g., family, security).
Overall, these results demonstrate that the negative impact of the pandemic on mental health may be smaller than health experts predicted. Furthermore, although we did not measure resilience directly, results suggest that some Americans demonstrated resilience in that they reported positive emotions and reduced mental health symptoms with greater frequency. These results provide mostly divergent evidence from prior work, which has pointed to negative mental health effects (e.g., da Silva et al., 2020; Xiong et al., 2020), although a recent study showed that some individuals have had adaptive responses (Park et al., 2020). Our findings may differ from prior work for several reasons. First, Youper users who voluntarily sought mental health support may be a more resilient subset of the population. Second, populations most affected by the pandemic (e.g., the elderly, first responders, healthcare workers; Armitage & Nellums, 2020; Pappa et al., 2020; Stogner et al., 2020) may not have been well represented in this sample given that many in the sample were teenagers, and therefore, likely students, who may not have been exposed to the same pandemic-related risks as adults in the workforce. Third, given that the majority of our sample were age 30 or younger, it is possible that participants underestimated pandemic-related risks, engaged in pre-pandemic behaviors, and in turn, did not experience expected levels of worsening mental health. Fourth, our methodology was different from prior studies. Emotions and symptoms were assessed continuously from prior to when the pandemic spread to months after the initial spread, and the data collection methods were the same across all time points with no specific reference to a stated goal of understanding the impact of COVID-19 on mental health. Prior studies collected data explicitly for the purpose of assessing the pandemic's impact on mental health (e.g., Ettman et al., 2020; Lei et al., 2020; Mazza et al., 2020). This may have led to demand characteristics where participants reported distress due to perceptions that the researchers were expecting to find evidence of worsening mental health.
This study had several strengths, including a very large sample of app users in the United States. The sample included participants from a variety of age, gender, and occupational groups. The study also sampled throughout the pandemic, allowing for continual assessment of pandemic effects from February through July of 2020, and made no explicit reference to the pandemic, meaning that results are unlikely to be impacted by demand characteristics. Additionally, the present study used both acute and symptom measures of mood states, allowing for more highly sensitive assessment of momentary shifts in emotion. The study also had some limitations. Sample size was not consistent for all data collected. Specifically, some individuals who provided emotion data did not provide demographic information, and therefore a smaller sample was used in moderation analyses. Furthermore, far fewer users provided symptom data, yielding a smaller subset of the sample for analyses of validated mental health measures. Thus, symptom analyses may not be as generalizable to the population as emotion analyses. The sample also comprised people who used a mental health app. Therefore, a treatment- or intervention-seeking sample may not be representative of the population. However, given that this sample is likely at risk for psychopathology, emotional shifts should be more extreme than a population sample, making the small effects observed here even more surprising. The sample was also primarily young and female, which limits generalizability of results. Another limitation is that we did not have racial data and were unable to assess emotional changes in racial groups disproportionately impacted by the pandemic. Additionally, we did not have data about whether participants in the study sample became infected with the virus, which could be associated with poorer mental health outcomes. Finally, these data do not include recent months of the pandemic, in which cases have increased, which may be associated with worsening mood.
This study demonstrated that emotional responses to the pandemic have been complex, variable over time, in some cases longer lasting, and in others, more fleeting. Despite concerns that the COVID-19 pandemic has led to a mental health crisis, this study suggests that the first five months of the pandemic have resulted in temporary emotional shifts with limited evidence of lasting effects. Our results are notable from a policy perspective. Specifically, many suggested that adhering to pandemic safety measures (i.e., social distancing, quarantining) may be associated with marked reductions in mental health. While the pandemic has undoubtedly posed a burden to Americans, our results point to the notion that even in the context of managing stay-at-home orders and their aftermath, Americans may be poised to adapt. Therefore, it is possible that broader policies that implore Americans to engage in safe behavior during the pandemic may not be deleterious to long-term mental health outcomes. In sum, despite some negative impacts on acute mood states, people appear to have found ways to cope that protect against deleterious long-term impacts on mental health. However, as the number of cases continues to grow and the pandemic surges around the world, it is possible that more mental health effects may emerge. Thus, continued research is essential to understand the longitudinal impact.
Funding
David Garcia has been funded by the Vienna Science and Technology Fund (WWTF) through project VRG16-005. Andrea Niles, Jose Hamilton Vargas, Diego Dotta Couto, and Thiago Marafon are employees of Youper and are shareholders in the company.
Competing Interests: Andrea Niles, Jose Hamilton Vargas, Diego Dotta Couto, and Thiago Marafon are employees of Youper and are shareholders in the company.
References
- Armitage R., Nellums L.B. COVID-19 and the consequences of isolating the elderly. The Lancet Public Health. 2020;5(5) doi: 10.1016/S2468-2667(20)30061-X. e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Galea S., Bucciarelli A., Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology. 2007;75(5):671–682. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- Brackbill R.M., Hadler J.L., DiGrande L., Eckenga C.C., Farfel M.R., Friedman S., Perlman S.E., Stellman S.D., Walker D.J., Wu D., Yu S., Thorpe L.E. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the world trade center terrorist attack. JAMA. 2009;302(5):502–516. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- Bults M., Beaujean D.J., de Zwart O., Kok G., van Empelen P., van Steenbergen J.E., Richardus J.H., Voeten H.A. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health. 2011;11(2):2–15. doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Trends in number of COVID-19 cases in the US reported to CDC, by state/territory. Retrieved from https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases on October 29, 2020.
- Clark B., Chatterjee K., Martin A., Davis A. How commuting affects subjective wellbeing. Transportation. 2020;47(6):2777–2805. doi: 10.1007/s11116-019-09983-9. [DOI] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- da Silva M.L., Rocha R.S.B., Buheji M., Jahrami H., Cunha K.da C. A systematic review of the prevalence of anxiety symptoms during coronavirus epidemics. Journal of Health Psychology. 2020:1–11. doi: 10.1177/1359105320951620. [DOI] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Brewin C.R., Gruber M., Jones R.T., King D.W., King L.A., McNally R.J., Ursano R.J., Petukhova M., Kessler R.C. Exposure to hurricane-related stressors and mental illness after hurricane Katrina. Archives of General Psychiatry. 2007;64(12):1427. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia D., Rimé B. Collective emotions and social resilience in the digital traces after a terrorist attack. Psychological Science. 2019;30(4):617–628. doi: 10.1177/0956797619831964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwong A.S.F., Pearson R.M., Adams M.J., Northstone K., Tilling K., Smith D., Fawns-Ritchie C., Bould H., Warne N., Zammit S., Gunnell D.J., Moran P., Micali N., Reichenberg A., Hickman M., Rai D., Haworth S., Campbell A., Altschul D., …, Timpson N.J. Mental health during the COVID-19 pandemic in two longitudinal UK population cohorts. MedRxiv. 2020 doi: 10.1101/2020.06.16.20133116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Medical Science Monitor : International Medical Journal of Experimental and Clinical Research. 2020;26 doi: 10.12659/MSM.924609. e924609-1-e924609-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marco C.A., Neale J.M., Schwartz J.E., Shiffman S., Stone A.A. Coping with daily events and short-term mood changes: An unexpected failure to observe effects of coping. Journal of Consulting and Clinical Psychology. 1999;67(5):755–764. doi: 10.1037//0022-006x.67.5.755. [DOI] [PubMed] [Google Scholar]
- Matt G.E., Vázquez C. Anxiety, depressed mood, self-esteem, and traumatic stress symptoms among distant witnesses of the 9/11 terrorist attacks: Transitory responses and psychological resilience. The Spanish Journal of Psychology. 2008;11(2):503–515. [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nacasch N., Foa E.B., Huppert J.D., Tzur D., Fostick L., Dinstein Y., Polliack M., Zohar J. Prolonged exposure therapy for combat- and terror-related posttraumatic stress disorder: A randomized control comparison with treatment as usual. The Journal of Clinical Psychiatry. 2010;72(9):1174–1180. doi: 10.4088/JCP.09m05682blu. [DOI] [PubMed] [Google Scholar]
- National Academy for State Health Policy https://www.nashp.org/governors-prioritize-health-for-all/
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park A., Velez C.V., Kannan K., Chorpita B.F. Stress, functioning, and coping during the COVID-19 pandemic: Results from an online convenience sample. The Behavior Therapist. 2020;43(6):210–216. [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the COVID-19 pandemic. New England Journal of Medicine. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy. 2020;16(1):67–73. doi: 10.1080/15487733.2020.1776561. [DOI] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver R.C., Holman E.A., McIntosh D.N., Poulin M., Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA. 2002;288(10):1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- Silver R.C., Wortman C.B. Human Helplessness: Theory and Applications. Academic Press; 1980. Coping with undesirable life events; pp. 279–340. [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata statistical software: Release 14. StataCorp LP.
- Stogner J., Miller B.L., McLean K. Police stress, mental health, and resiliency during the COVID-19 pandemic. American Journal of Criminal Justice. 2020;45(4):718–730. doi: 10.1007/s12103-020-09548-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay L., Diener E. Needs and subjective well-being around the world. Journal of Personality and Social Psychology. 2011;101(2):354–365. doi: 10.1037/a0023779. [DOI] [PubMed] [Google Scholar]
- van Eck M., Nicolson N.A., Berkhof J. Effects of stressful daily events on mood states: relationship to global perceived stress. Journal of Personality and Social Psychology. 1998;75(6):1572–1585. doi: 10.1037/0022-3514.75.6.1572. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortman C.B., Silver R.C. The myths of coping with loss. Journal of Consulting and Clinical Psychology. 1989;57(3):349–357. doi: 10.1037/0022-006X.57.3.349. [DOI] [PubMed] [Google Scholar]
- Wortman C.B., Silver R.C. Handbook of bereavement research: Consequences, coping, and care. American Psychological Association; 2001. The myths of coping with loss revisited; pp. 405–429. [DOI] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]