Abstract
Background
Pregnant women are emotionally vulnerable and have suffered great psychological impacts. Following the coronavirus disease 2019 (COVID-19) outbreak, a study was undertaken of the prevalence of, and factors contributing to, symptoms of anxiety and depression among pregnant women in Shenzhen, China.
Methods
A cross-sectional study on pregnant women was conducted from September to December 2020 in Shenzhen, using a random-recruit method. The General Anxiety Disorder (GAD-7) and Patient Health Questionnaire (PHQ-9) surveys were used to evaluate symptoms of anxiety and depression. A multivariate logistic regression model was developed to explore factors potentially associated with symptoms of anxiety and depression during pregnancy.
Results
A total of 3,434 pregnant women aged 15 to 59 years were enrolled. Symptoms of anxiety and depression were present in 9.8% and 6.9%, respectively. Logistic regression analysis using a stepwise procedure revealed that an increased risk of symptoms of anxiety and depression was associated with unmarried/divorced/widowed, unemployed, received professional psychological counseling, family dysfunction, the first trimester of pregnancy, pregnancy complications and vaginal bleeding, unplanned pregnancy, decline in household income and disputes between partners caused by the COVID-19 pandemic, consumption of alcoholic drinks by women and their partners, smoking, lack of exercise and sedentary lifestyle. Women with education from junior high school through college were less likely to experience symptoms of prenatal depression.
Conclusions
Our study revealed factors associated with psychological symptoms among pregnant women in the post-COVID-19-pandemic era. These results should help to update guidance for psychological interventions for pregnant women during the period of COVID-19.
Keywords: Depression, Anxiety, Pregnancy, Covid-19
1. Introduction
An outbreak of pneumonia of unknown cause began in December 2019, in Wuhan, Hubei Province, China (Wang et al., 2020), which caused intense scrutiny not only within China but also worldwide. The common symptoms of COVID-19 include fever, cough, shortness of breath, nasal tampon, pharyngalgia, myalgia, fatigue, headache and expectoration (Ding et al., 2020). The pathogen was identified as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of 5 January 2021, there have been over 83 million reported cases and over 1.8 million deaths globally since the start of the pandemic according to a world health organization (WHO) report (https://www.who.int/publications/m/item/weekly-epidemiological-update—5-january-2021).
It is well known that COVID-19 is highly infectious and potentially fatal (Colizzi et al., 2020), which can cause panic and anxiety in a population (Maunder et al., 2003). A few empirical studies related to this pandemic have reported a higher prevalence of mental health problems such as depression, anxiety, and post‐traumatic stress symptoms in women compared to men (Thapa et al., 2020). Pregnant women, as an especially sensitive group, have to face economic pressures and physiological changes, and there is little doubt that their mental health will also be affected (Bjelica et al., 2018), and perinatal mental disorders can be associated with short- and long-term risks for the physical and psychological health of themselves and their children (Dunkel Schetter and Tanner, 2012; Kendig et al., 2017; Kotabagi et al., 2020). Nevertheless, after the COVID-19 outbreak, researchers have been more concerned about postpartum psychological effects (Hui et al., 2020; Liang et al., 2020; Pariente et al., 2020), and all of the above studies show that pregnant women reported more depressive symptoms in the postpartum period following the alert announcement regarding coronavirus infection. The prevalence of the symptoms of anxiety and depression in Canadian pregnant women were reported to be 57% and 37%, respectively, with The Edinburgh Postpartum Depression Scale (EPDS) and The PROMIS Anxiety Adult 7-item serve as assessment tools (Lebel et al., 2020). A study in Turkey used EPDS and The Beck Anxiety Inventory (BAI) found that 35.4% of pregnant women were suffering from prenatal depression (Durankuş and Aksu, 2020). And scholars in Qatar announced that prenatal anxiety and depression were experienced by 34.4% and 39.2% of pregnant women, respectively, applied the Patient Health Questionnaire Anxiety-Depression Scale (PHQ-ADS) (Farrell et al., 2020). In Beijing, China, the symptoms of anxiety and depression in pregnant women were reported to be only 6.8% and 5.3%, respectively, when used PHQ-9 and GAD-7 to evaluate the depression and anxiety symptoms of pregnant women (Zhou et al., 2020).The risk factors for such adverse psychological conditions can include worrying about lack of prenatal care, strained relationships, social isolation (Lebel et al., 2020), poor sleep (Lin et al., 2020), and changes in exercise routines (Gildner et al., 2020).
Prior studies have specifically focused on pregnancies in the first (Tang et al., 2019), second (Li et al., 2019) or third (Yu et al., 2020) trimesters, but very few have considered all pregnant women, especially after the COVID-19 pandemic. Research that we conducted early in the COVID-19 pandemic was limited by non-random sampling and small sample size (Lin et al., 2020). Moreover, a Swedish study suggested that these considerations will be of paramount importance to public health in the post-COVID-19-pandemic era (Macassa and Tomaselli, 2020). However, no researchers have discussed adverse effects on the mental state of pregnant women and factors that affect their psychological state in the post-COVID-19-pandemic era in China. Since Shenzhen is one of the most economically developed cities in mainland China, with large movements of people, women who live in Shenzhen seemed more likely to be at risk and representative of the prevalence of anxiety and depression during pregnancy. Thus, we explored the occurrence of prenatal anxiety and depression and investigated contributory factors throughout pregnancy among women in Shenzhen City, China in the post-COVID-19-pandemic era. Specifically, the purposes of our study included: (1) describing the levels of anxiety and depression symptoms among pregnant women in the post-pandemic era of COVID-19, (2) investigating the contributory factors of anxiety and depression symptoms.
2. Methods
2.1. Study design and participants
We carried out a cross-sectional survey in Shenzhen City from September 15 to December 15, 2020. A full description of the objectives, contents, procedures, associated benefits, and risks of the present study was provided at the beginning of the electronic questionnaire. Pregnant women who had established perinatal health records in Shenzhen District Maternity and Child Healthcare Hospitals and gave consent to participate were involved in this study, whereas those with psychotic disorders such as schizophrenia, mania, or serious substance dependence and pregnant women who refused to participate were excluded. Specially trained investigators, including doctors and nurses, screened pregnant women who met the inclusion and exclusion criteria and then filled out the electronic questionnaire anonymously.
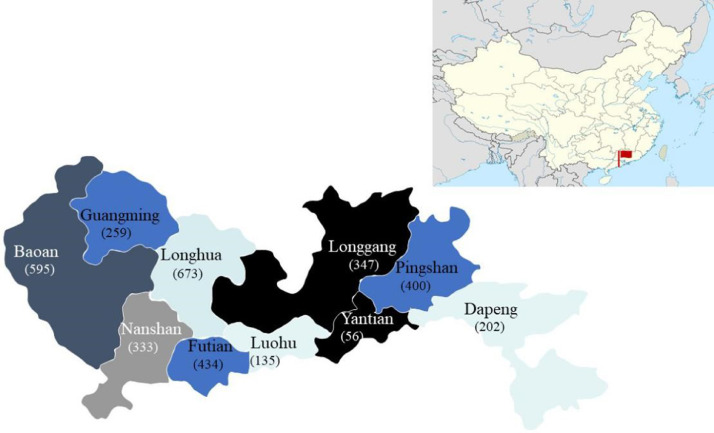
A total of 3437 women had established perinatal health records in Shenzhen District Maternity and Child Healthcare Hospitals and gave consent to participate were enrolled in the present study using a random recruitment method. Those who completed the questionnaire in less than 100 s were excluded, leaving 3434 women in the study. Sample recruitment began in September 2020 and ended in December 2020 (see Fig. 1 for details).
Fig. 1.
Geographic distribution of participants in Shenzhen City, China. The map of China and the inset showing the distribution of participants from ten districts in Shenzhen were obtained from online sources (https://www.wikiwand.com/ and https://wenku.baidu.com/, respectively). Sample sizes are shown below the names of each region.
This study was a cross-sectional survey approved by the Ethics Committee of Shenzhen Maternity and Child Healthcare Hospital, and conducted in Shenzhen, a city of over 20 million residents in southwestern China.
2.2. Measurements
2.2.1. Socio-demographic characteristics and family care
The socio-demographic characteristics included age, medical insurance, education level, partner's educational level, working status after pregnancy, partner's working status, marital status, marriage age, living status, psychological counseling before pregnancy and level of family care. The assessment of family care used the Family Adaptation Partnership Growth and Resolve index (APGAR) (Smilkstein et al., 1982).
2.2.2. Obstetric characteristics
The obstetric characteristics consisted of gestation weeks (first, second, third trimester), parity (1, 2, ≥3), number of spontaneous abortions (0, 1, 2, ≥3), vaginal bleeding and pregnancy complications (including gestational hypertension, gestational diabetes, intrahepatic cholestasis and cervical disease), pregnancy planning (planned conception, unplanned pregnancy, artificial impregnation), expected mode of delivery (not considered, vaginal delivery, cesarean delivery).
2.2.3. Characteristics related to COVID-19
To investigate the impacts of the COVID-19 pandemic on pregnant women, we also collected variables as follows: the duration of isolation at home (day), frequency of handwashing after going out, changes in intimacy between partners, household income and regular prenatal examinations.
2.2.4. Lifestyle characteristics
Lifestyle characteristics comprised body mass index (BMI), smoking and drinking of a pregnant woman and her partner, exercise and sitting time per day. Individual BMI was calculated before pregnancy and adhered to the Chinese classification of underweight (BMI <18.5 kg/m2), normal weight (BMI of 18.5–23.9 kg/m2), overweight (BMI of 24–27.9 kg/m2) and obese (BMI ≥28 kg/m2). Smoking was defined as an average of one cigarette a day in recent years. Drinking was defined as drinking alcohol once a week on average. Exercise was defined as having engaged in walking, yoga or other physical activities more than three times during the past week. The above definitions were used in previous research (Yu et al., 2020). Sitting time (hours) per day was categorized into several levels (≤1, 1–3, ≥3–5, ≥5–10, ≥10).
2.2.5. Assessment of maternal anxiety and depression
2.2.5.1. Prenatal anxiety
Prenatal anxiety was assessed by the General Anxiety Disorder 7-item (GAD-7) questionnaire with a 7-question scale, with each item scored on a 4-point scale ranging from 0 to 3. The total score ranges from 0 to 21; higher scores represent more severe anxiety symptoms. A previous study suggested that the GAD-7 questionnaire is reliable and valid for pregnant Chinese women (Tong et al., 2016). In this study, a GAD-7 score of ≥7 indicated maternal anxiety.
2.2.5.2. Prenatal depression
Prenatal depression was assessed by the Patient Health Questionnaire 9-item (PHQ-9) survey, which considers the applicability, reliability and validity of prenatal studies in China and the educational level of the participants (Zhang et al., 2013). PHQ-9 consists of 9 items with a 3-point scale ranging from 0 (none), 1 (a few days), 2 (more than half the days) and 3 (almost every day). The total score is from 0 to 27, and participants were considered to have depressive symptoms if their score was 10 or higher.
2.3. Statistical analyses
Data collection and analyses were performed in SPSS V.25.0. In the present study, some continuous variables, including age, BMI before pregnancy, family care score (APGAR), prenatal anxiety score and prenatal depression score, were converted into categorical variables. Then the Chi-square test or Fisher's exact test was used to analyze the relationship between the collected variables and prenatal adverse psychological symptoms (anxiety, depression). Variables with P ≤ 0.1 in the univariate analysis were taken as independent variables and brought into the multivariate logistic regression model with a stepwise procedure. Odds ratios (OR) and 95% confident intervals (CI) were calculated. Two-tailed tests with P values less than 0.05 were considered statistically significant. The variance inflation factor (VIF) was used to evaluate collinearity between independent variables.
3. Results
3.1. Participant characteristics
We received 3437 completed questionnaires in total; three respondents who completed the questionnaire in less than 100 s were excluded. All participants were aged 15–59 years (28.97±4.57). Most of them (83.2%) had medical insurance. Undergraduate (27.3%) and college (27.2%) degrees were held by the majority of pregnant women and their partners. Numerous pregnant women worked during pregnancy (61.5%), and the vast majority of their partners worked (95.8%). Among our participants, 92.8% were married, with the largest proportion (34.1%) having lasted 3–10 years. A majority (67.5%) of couples chose to live separately. Regarding family care, over half of the pregnant women had a high level of family care (58.5%), as shown in Table 1 .
Table 1.
Characteristics of pregnant women and chi-square analysis.
| Variables | Total | Depression | P | Anxiety | P | ||
|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | ||||
| Age (years) | <0.001 | 0.002 | |||||
| ≤19 | 32 (0.9) | 27 (84.4) | 5 (15.6) | 23 (71.9) | 9 (28.1) | ||
| 20–24 | 520 (15.1) | 459 (88.3) | 61 (11.7) | 459 (88.3) | 61 (11.7) | ||
| 25–29 | 1371 (39.9) | 1280 (93.4) | 91 (6.6) | 1238 (90.3) | 133 (9.7) | ||
| 30–34 | 1115 (32.5) | 1053 (94.4) | 62 (5.6) | 1022 (91.7) | 93 (8.3) | ||
| ≥35 | 396 (11.5) | 377 (95.2) | 19 (4.8) | 355 (89.6) | 41 (10.4) | ||
| Medical insurance | <0.001 | 0.005 | |||||
| Yes | 2857 (83.2) | 2680 (93.8) | 177 (6.2) | 2595 (90.8) | 262 (9.2) | ||
| No | 577 (16.8) | 516 (89.4) | 61 (10.6) | 502 (87.0) | 75 (13.0) | ||
| Educational level | 0.013 | 0.167 | |||||
| Master degree and above | 147 (4.3) | 133 (90.5) | 14 (9.5) | 125 (85.0) | 22 (15.0) | ||
| Undergraduate | 937 (27.3) | 867 (27.1) | 70 (7.5) | 840 (89.6) | 97 (10.4) | ||
| College degree | 933 (27.2) | 885 (94.9) | 48 (5.1) | 853 (91.4) | 80 (8.6) | ||
| High school degree | 713 (20.8) | 658 (92.3) | 55 (7.7) | 647 (90.7) | 66 (9.3) | ||
| Junior high school diploma | 687 (20.0) | 640 (93.2) | 47 (6.8) | 618 (90.0) | 69 (10.0) | ||
| Primary school or below | 17 (0.5) | 13 (76.5) | 4 (23.5) | 14 (82.4) | 3 (17.6) | ||
| Partner’ education level | 0.057 | 0.351 | |||||
| Master degree and above | 208 (6.1) | 195 (93.8) | 13 (6.3) | 185 (88.9) | 23 (11.1) | ||
| Undergraduate | 1020 (29.7) | 941 (92.3) | 79 (7.7) | 907 (88.9) | 113 (11.1) | ||
| College degree | 862 (25.1) | 812 (94.2) | 50 (5.8) | 793 (92.0) | 69 (8.0) | ||
| High school degree | 711 (20.7) | 673 (94.7) | 38 (5.3) | 643 (90.4) | 68 (9.6) | ||
| Junior high school diploma | 616 (17.9) | 560 (90.9) | 56 (9.1) | 554 (89.9) | 62 (10.1) | ||
| Primary school or below | 17 (0.5) | 15 (88.2) | 2 (11.8) | 15 (88.2) | 2 (11.8) | ||
| Working status after pregnancy | 0.003 | 0.002 | |||||
| Employed | 2112 (61.5) | 1987 (94.1) | 125 (5.9) | 1931 (91.4) | 181 (8.6) | ||
| Unemployed | 1322 (38.5) | 1209 (91.5) | 113 (8.5) | 1166 (88.2) | 156 (11.8) | ||
| Partner’ working status | 0.178 | 0.049 | |||||
| Employed | 3290 (95.8) | 3066 (93.2) | 224 (6.8) | 2974 (90.4) | 316 (9.6) | ||
| Unemployed | 144 (4.2) | 130 (90.3) | 14 (9.7) | 123 (85.4) | 21 (14.6) | ||
| Marital status | <0.001 | <0.001 | |||||
| Married | 3188 (92.8) | 2988 (93.7) | 200 (6.3) | 2897 (90.9) | 291 (9.1) | ||
| Unmarried/divorced/widowed | 246 (7.2) | 208 (84.6) | 38 (15.4) | 200 (81.3) | 46 (18.7) | ||
| Marriage length | 0.001 | 0.131 | |||||
| ≥10 years | 228 (6.6) | 218 (95.6) | 10 (4.4) | 210 (92.1) | 18 (7.9) | ||
| 3–10 years | 1170 (34.1) | 1113 (95.1) | 57 (4.9) | 1071 (91.5) | 99 (8.5) | ||
| 1–3 years | 986 (28.7) | 906 (91.9) | 80 (8.1) | 879 (89.1) | 107 (10.9) | ||
| <1 year | 1050 (30.6) | 959 (91.3) | 91 (8.7) | 937 (89.2) | 113 (10.8) | ||
| Residential status | 0.601 | 0.762 | |||||
| Lives alone | 2317 (67.5) | 2153 (92.9) | 164 (7.1) | 2084 (89.9) | 233 (10.1) | ||
| Live with in-laws | 858 (25.0) | 798 (93.0) | 60 (7.0) | 777 (90.6) | 81 (9.4) | ||
| Live with Parents | 259 (7.5) | 245 (94.6) | 14 (5.4) | 236 (91.1) | 23 (8.9) | ||
| Professional psychological counseling before pregnancy | 0.074 | <0.001 | |||||
| Not received | 3187 (92.8) | 2973 (93.3) | 214 (6.7) | 2906 (91.2) | 281 (8.8) | ||
| Received | 247 (7.2) | 223 (90.3) | 24 (9.7) | 191 (77.3) | 56 (22.7) | ||
| Gestation age | <0.001 | 0.189 | |||||
| First trimester | 1144 (33.3) | 1033 (90.3) | 111 (9.7) | 1017 (88.9) | 127 (11.1) | ||
| Second trimester | 1151 (33.5) | 1086 (94.4) | 65 (5.6) | 1043 (90.6) | 108 (9.4) | ||
| Last trimester | 1139 (33.2) | 1077 (94.6) | 62 (5.4) | 1037 (91.0) | 102 (9.0) | ||
| Parity | 0.085 | 0.367 | |||||
| One | 1870 (54.5) | 1724 (92.2) | 146 (7.8) | 1679 (89.8) | 191 (10.2) | ||
| Two | 1296 (37.7) | 1219 (94.1) | 77 (5.9) | 1180 (91.0) | 116 (9.0) | ||
| Three and above | 268 (7.8) | 253 (94.4) | 15 (5.6) | 238 (88.8) | 30 (11.2) | ||
| Number of abortions | 0.156 | 0.873 | |||||
| Zero | 2559 (74.5) | 2383 (93.1) | 176 (6.9) | 2308 (90.2) | 251 (9.8) | ||
| One | 614 (17.9) | 574 (93.5) | 40 (6.5) | 557 (90.7) | 57 (9.3) | ||
| Two | 187 (5.4) | 175 (93.6) | 12 (6.4) | 166 (88.8) | 21 (11.2) | ||
| Three and above | 74 (2.2) | 64 (86.5) | 10 (13.5) | 66 (89.2) | 8 (10.8) | ||
| Vaginal bleeding | 0.396 | 0.003 | |||||
| No | 2589 (75.4) | 2415 (93.3) | 174 (6.7) | 2357 (91.0) | 232 (9.0) | ||
| Yes | 845 (24.6) | 781 (92.4) | 64 (7.6) | 740 (87.6) | 105 (12.4) | ||
| Pregnancy complications | <0.001 | 0.002 | |||||
| No | 2651 (77.2) | 2496 (94.2) | 155 (5.8) | 2414 (91.1) | 237 (8.9) | ||
| Yes | 783 (22.8) | 700 (89.4) | 83 (10.6) | 683 (87.2) | 100 (12.8) | ||
| Pregnancy intentions | <0.001 | 0.001 | |||||
| Plan conception | 1829 (53.3) | 1733 (94.8) | 96 (5.2) | 1681 (91.9) | 148 (8.1) | ||
| Unplanned pregnancy | 1493 (43.5) | 1357 (90.9) | 136 (9.1) | 1313 (87.9) | 180 (12.1) | ||
| Artificial impregnation | 112 (3.3) | 106 (94.6) | 6 (5.4) | 103 (92.0) | 9 (8.0) | ||
| Expected mode of delivery | 0.006 | <0.001 | |||||
| Out of consideration | 759 (22.1) | 687 (90.5) | 72 (9.5) | 661 (87.1) | 98 (12.9) | ||
| Vaginal delivery | 2349 (68.4) | 2206 (93.9) | 143 (6.1) | 2152 (91.6) | 197 (8.4) | ||
| Cesarean delivery | 326 (9.5) | 303 (92.9) | 23 (7.1) | 284 (87.1) | 42 (12.9) | ||
| Duration of isolation at home (day) after COVID-19 | 0.749 | 0.765 | |||||
| ≥14 | 3050 (88.8) | 2837 (93.0) | 213 (7.0) | 2752 (90.2) | 298 (9.8) | ||
| 7–13 | 131 (3.8) | 121 (92.4) | 10 (7.6) | 115 (87.8) | 16 (12.2) | ||
| 4–7 | 75 (2.2) | 69 (92.0) | 6 (8.0) | 69 (92.0) | 6 (8.0) | ||
| ≤3 | 178 (5.2) | 169 (94.9) | 9 (5.1) | 161 (90.4) | 17 (9.6) | ||
| Frequency of handwashing after going out after COVID-19 | 0.017 | 0.057 | |||||
| Every time | 2686 (78.2) | 2513 (93.6) | 173 (6.4) | 2433 (90.6) | 253 (9.4) | ||
| Most of the time | 512 (14.9) | 473 (92.4) | 39 (7.6) | 460 (89.8) | 52 (10.2) | ||
| Occasionally | 216 (6.3) | 194 (89.8) | 22 (10.2) | 189 (87.5) | 27 (12.5) | ||
| Scarcely | 20 (0.6) | 16 (80.0) | 4 (20.0) | 15 (75.0) | 5 (25.0) | ||
| Intimacy with partners after COVID-19 | <0.001 | <0.001 | |||||
| Essentially unchanged | 2601 (75.7) | 2428 (93.3) | 173 (6.7) | 2364 (90.9) | 237 (9.1) | ||
| Strained | 77 (2.2) | 59 (76.6) | 18 (23.4) | 57 (74.0) | 20 (26.0) | ||
| More intimate | 756 (22.0) | 709 (93.8) | 47 (6.2) | 676 (89.4) | 80 (10.6) | ||
| Impact on household income after COVID-19 | 0.002 | <0.001 | |||||
| Essentially unchanged | 1835 (53.4) | 1732 (94.4) | 103 (5.6) | 1691 (92.2) | 144 (7.8) | ||
| Increased | 65 (1.9) | 63 (96.9) | 2 (3.1) | 58 (89.2) | 7 (10.8) | ||
| Decreased 20–50% | 1195 (34.8) | 1095 (91.6) | 100 (8.4) | 1057 (88.5) | 138 (11.5) | ||
| Decrease 50% and above | 339 (9.9) | 306 (90.3) | 33 (9.7) | 291 (85.8) | 48 (14.2) | ||
| Regular prenatal examination | 0.006 | 0.274 | |||||
| Yes | 3104 (90.4) | 2901 (93.5) | 203 (6.5) | 2805 (90.4) | 299 (9.6) | ||
| No | 330 (9.6) | 295 (89.4) | 35 (10.6) | 292 (88.5) | 38 (11.5) | ||
| BMI before pregnancy | 0.212 | 0.472 | |||||
| 18.5–23.9 | 2139 (63.3) | 1992 (93.1) | 147 (6.9) | 1933 (90.4) | 206 (9.6) | ||
| <18.5 | 519 (15.4) | 478 (92.1) | 41 (7.9) | 463 (89.2) | 56 (10.8) | ||
| 24–27.9 | 425 (12.6) | 404 (95.1) | 21 (4.9) | 389 (91.5) | 36 (8.5) | ||
| ≥28 | 294 (8.7) | 269 (91.5) | 25 (8.5) | 260 (88.4) | 34 (11.6) | ||
| Smoking habits | <0.001a | <0.001 | |||||
| No | 3372 (98.2) | 3148 (93.4) | 224 (6.6) | 3051 (90.5) | 321 (9.5) | ||
| Yes | 62 (1.8) | 48 (77.4) | 14 (22.6) | 46 (74.2) | 16 (25.8) | ||
| Her partner’ smoking habits | 0.008 | 0.086 | |||||
| No | 2125 (61.9) | 1997 (94.0) | 128 (6.0) | 1931 (90.9) | 194 (9.1) | ||
| Yes | 1309 (38.1) | 1199 (91.6) | 110 (8.4) | 1166 (89.1) | 143 (10.9) | ||
| Drinking habits | 0.005 | <0.001 | |||||
| No | 3262 (95.0) | 3045 (93.3) | 217 (6.7) | 2961 (90.8) | 301 (9.2) | ||
| Yes | 172 (5.0) | 151 (87.8) | 21 (12.2) | 136 (79.1) | 36 (20.9) | ||
| Her partner’ drinking habits | <0.001 | 0.003 | |||||
| No | 2486 (72.4) | 2339 (94.1) | 147 (5.9) | 2265 (91.1) | 221 (8.9) | ||
| Yes | 948 (27.6) | 857 (90.4) | 91 (9.6) | 832 (87.8) | 116 (12.2) | ||
| Exercise | 0.001 | 0.639 | |||||
| Yes | 975 (28.4) | 929 (95.3) | 46 (4.7) | 883 (90.6) | 92 (9.4) | ||
| No | 2459 (71.6) | 2267 (92.2) | 192 (7.8) | 2214 (90.0) | 245 (10.0) | ||
| Sitting time per day (hour) | <0.001 | 0.005 | |||||
| ≤1 | 473 (13.8) | 442 (93.4) | 31 (6.6) | 430 (90.9) | 43 (9.1) | ||
| 1–3 | 1090 (31.7) | 1039 (95.3) | 51 (4.7) | 1009 (92.6) | 81 (7.4) | ||
| 3–5 | 840 (24.5) | 782 (93.1) | 58 (6.9) | 753 (89.6) | 87 (10.4) | ||
| 5–10 | 849 (24.7) | 774 (91.2) | 75 (8.8) | 748 (88.1) | 101 (11.9) | ||
| ≥10 | 182 (5.3) | 159 (87.4) | 23 (12.6) | 157 (86.3) | 25 (13.7) | ||
a:Calibration chi-square test.
Regarding the different gestation age groups, 33.3%, 33.5% and 33.2% of the participants were in the first, second and third trimesters, respectively. Of these, 54.5% belonged to primiparas and more than half (74.5%) of pregnant women had no abortion history. Most of the pregnant women expressed no experience of vaginal bleeding (75.4%) or pregnancy complications (77.2%). Over half (53.3%) the pregnancies were planned. The most common expected method of birth was vaginal delivery (68.4%), as shown in Table 1.
After the COVID-19 pandemic, most pregnant women reported self-isolating at home for 14 days (88.8%). Among the participants, 78.2% always washed or disinfected their hands after going out. There were small changes in intimacy with partners in 75.7%, and in household income in 53.4%, of the participants. Also, the vast majority (90.4%) had regular prenatal examinations, as shown in Table 1.
BMI before pregnancy was normal for 63.3% of pregnant women. A large proportion of pregnant women did not smoke (98.2%) or drink alcoholic beverages (95.0%), while 61.9% and 72.4% of their partners were smoking and drinking, respectively. A majority of participants (71.6%) reported no exercise, and the largest proportion (31.7%) of pregnant women sat continuously from 1 to 3 h per day, as shown in Table 1.
3.2. Prevalence and factors contributing to maternal anxiety and depression
In this study, 9.8% of pregnant women experienced anxiety during pregnancy. In the multivariate logistic regression model, expected vaginal delivery was inversely associated with maternal anxiety (OR 0.721, 95%CI 0.549–0.948). However, participants with a marital status of unmarried/divorced/widowed had a higher risk of anxiety than married women (OR 1.752, 95%CI 1.212–2.534). Individuals who had received professional psychological counseling before pregnancy were more likely to develop anxiety (OR 3.581, 95%CI 2.538–5.051). Pregnant women with moderate or severe dysfunction in family care have an increased likelihood of experiencing prenatal anxiety (OR 2.374, 95%CI 1.806–3.122, and OR 2.795, 95%CI 2.030–3.848, respectively). Also, histories of vaginal bleeding (OR 1.483, 95%CI 1.146–1.920) and pregnancy complications (OR 1.426, 95%CI 1.097–1.852) triggered anxiety in pregnant women. After the outbreak of COVID-19, pregnant women and their partners experienced more strife (OR 2.838, 95%CI 1.594–5.052) and their household income decreased by 20–50% (OR 1.393, 95% 1.076–1.805) and 50% or above (OR 1.498, 95% 1.034–2.170). Both factors increased the risk of prenatal anxiety. Moreover, pregnant women who regularly consumed alcoholic beverages were almost two times more likely to experience anxiety than those who did not (OR 1.961, 95%CI 1.294–2.970). In addition, sitting continuously for 5–10 h (OR 1.882, 95%CI 1.260–2.810) and ≥10 h per day (OR 2.128, 95%CI 1.223–3.701) actively raised the risk of prenatal anxiety. The VIF in the multiple-mental models was less than 2. A VIF of less than 10 indicates that multi-collinearity may not affect the estimates, as shown in Table 2 .
Table 2.
Logistic regression model of anxiety symptoms in pregnant women.
| Variables | β | Wald | P Value | OR (95%CI) | VIF |
|---|---|---|---|---|---|
| Marital status | 1.058 | ||||
| Married | Ref. | ||||
| Unmarried/divorced/widowed | 0.561 | 8.889 | 0.003 | 1.752 (1.212–2.534) | |
| Professional psychological counseling before pregnancy | 1.050 | ||||
| Not received | Ref. | ||||
| Received | 1.276 | 52.801 | <0.001 | 3.581 (2.538–5.051) | |
| Level of family care | 1.120 | ||||
| Barrier free | Ref. | ||||
| Moderately dysfunctional | 0.865 | 38.316 | <0.001 | 2.374 (1.806–3.122) | |
| Severe dysfunctional | 1.028 | 39.643 | <0.001 | 2.795 (2.030–3.848) | |
| Vaginal bleeding | 1.028 | ||||
| No | Ref. | ||||
| Yes | 0.394 | 8.964 | 0.003 | 1.483 (1.146–1.920) | |
| Pregnancy complications | 1.025 | ||||
| No | Ref. | ||||
| Yes | 0.355 | 7.042 | 0.008 | 1.426 (1.097–1.852) | |
| Expected mode of delivery | 1.050 | ||||
| Out of consideration | Ref. | ||||
| Vaginal delivery | −0.327 | 5.508 | 0.019 | 0.721 (0.549–0.948) | |
| Cesarean delivery | 0.064 | 00.097 | 0.756 | 1.067 (0.710–1.601) | |
| Intimacy with partners after COVID-19 | 1.090 | ||||
| Essentially unchanged | Ref. | ||||
| Strained | 1.043 | 12.568 | <0.001 | 2.838 (1.594–5.052) | |
| More intimate | 0.250 | 2.988 | 0.084 | 1.285 (0.967–1.706) | |
| Impact on household income after COVID-19 | 1.075 | ||||
| Essentially unchanged | Ref. | ||||
| Increased | 0.198 | 0.214 | 0.644 | 1.219 (0.527–2.820) | |
| Decreased 20–50% | 0.332 | 6.309 | 0.012 | 1.393 (1.076–1.805) | |
| Decrease 50% and above | 0.404 | 4..562 | 0.033 | 1.498 (1.034–2.170) | |
| Drinking habits | 1.027 | ||||
| No | Ref. | ||||
| Yes | 0.673 | 10.091 | 0.001 | 1.961 (1.294–2.970) | |
| Sitting time per day(hour) | 1.090 | ||||
| ≤1 | Ref. | ||||
| 1–3 | 0.021 | 0.010 | 0.921 | 1.021 (0.680–1.532) | |
| 3–5 | 0.369 | 3.139 | 0.076 | 1.446 (0.962–2.175) | |
| 5–10 | 0.632 | 9.552 | 0.002 | 1.882 (1.260–2.810) | |
| ≥10 | 0.755 | 7.147 | 0.008 | 2.128 (1.223–3.701) |
VIF: Variance inflation factor.
Adjusted for age, educational level, medical insurance, working status, partner's working status, marital status, professional psychological counseling before pregnancy, family care, gestation age, vaginal bleeding, pregnancy complications, pregnancy planning, expected mode of delivery, frequency of handwashing after going out after COVID-19, intimacy with partners after COVID-19, impact on household income after COVID-19, smoking habit, partner smoking habits, drinking habits, partner drinking habits, sitting time.
The prevalence of depressive symptoms was found to be 6.9%. In the multivariate model, we found that college degree, high school degree and junior high school diploma were inversely associated with prenatal depression (OR 0.327, 95%CI 0.–188–0.737; OR 0.499, 95%CI 0.250–0.998; OR 0.499, 95%CI 0.250–0.998). These findings were similar to those for prenatal anxiety with the following factors increasing the risk of prenatal depression: unmarried/divorced/widowed marital status (OR 1.582, 95%CI 1.007–2.486), having received professional psychological counseling before pregnancy (OR 1.673, 95%CI 1.025–2.732), moderate (OR 2.353, 95%CI 1.702–3.252) or severe (OR 2.543, 95%CI 1.720–3.760) dysfunction in family care, pregnancy complications (OR 1.793, 95%CI 1.330–2.418), strained relationships with partners (OR 3.808, 95%CI 2.063-7.028), reduction in household income of 20–50% after the COVID-19 pandemic (OR 1.490, 95%CI 1.090–2.038), and sitting time per day of 5–10 h (OR 1.701,95%CI 1.051–2.755) or ≥10 h (OR 2.113, 95%CI 1.139–3.921). Moreover, unemployed women were 1.4 times more likely than employed women to develop depression (OR 1.422, 95%CI 1.048–1.930). Regarding gestation, women in their first trimester of pregnancy had a higher risk of depression than in their last trimester (OR 1.951, 95%CI 1.373–2.772). In terms of pregnancy planning, unplanned pregnancies significantly increased the possibility of depression (OR 1.609, 95%CI 1.190–2.175). Smoking in pregnant women and alcoholic beverage consumption by their partners were also found to be risk factors (OR 2.451,95%CI 1.248–4.815; OR 1.497, 95%CI 1.116–2.008). Moreover, lack of exercise was positively related to prenatal depression (OR 1.615, 95%CI 1.128–2.313). The VIF in the multiple-mental models was less than 2. A VIF less than 10 indicates that the multi-collinearity may not affect the estimations, as shown in (Table 3 ).
Table 3.
Logistic regression model of depressive symptoms in pregnant women.
| Variables | β | Wald | P Value | OR (95%CI) | VIF |
|---|---|---|---|---|---|
| Education level | 1.603 | ||||
| Master degree and above | Ref. | ||||
| Undergraduate | −0.324 | 0.968 | 0.325 | 0.723 (0.379–1.379) | |
| College degree | −0.989 | 8.042 | 0.005 | 0.372 (0.188–0.737) | |
| High school degree | −0.695 | 3.864 | 0.049 | 0.499 (0.250–0.998) | |
| Junior high school diploma | −1.073 | 8.474 | 0.004 | 0.342 (0.166–0.704) | |
| Primary school or below | 0.338 | 0.229 | 0.632 | 1.402 (0.351–5.601) | |
| Working status after pregnancy | 1.207 | ||||
| Employed | Ref. | ||||
| Unemployed | 0.352 | 5.121 | 0.024 | 1.422 (1.048–1.930) | |
| Marital status | |||||
| Married | Ref. | 1.135 | |||
| Unmarried/divorced/widowed | 0.459 | 3.965 | 0.046 | 1.582 (1.007–2.486) | |
| Professional psychological counseling before pregnancy | 1.095 | ||||
| Not received | Ref. | ||||
| Received | 0.515 | 4.231 | 0.040 | 1.673 (1.025–2.732) | |
| Level of family care | 1.186 | ||||
| Barrier free | Ref. | ||||
| Moderately dysfunctional | 0.856 | 26.829 | <0.001 | 2.353 (1.702–3.252) | |
| Severe dysfunctional | 0.933 | 21.863 | <0.001 | 2.543 (1.720–3.760) | |
| Gestation age | 1.133 | ||||
| First trimester | 0.668 | 13.895 | <0.001 | 1.951 (1.373–2.772) | |
| Second trimester | 0.014 | 0.005 | 0.943 | 1.014 (0.697–1.475) | |
| Last trimester | Ref. | ||||
| Pregnancy complications | 1.030 | ||||
| No | Ref. | ||||
| Yes | 0.584 | 14.677 | <0.001 | 1.793 (1.330–2.418) | |
| Pregnancy planning | 1.124 | ||||
| Planned conception | Ref. | ||||
| Unplanned pregnancy | 0.475 | 9.545 | 0.002 | 1.609 (1.190–2.175) | |
| Artificial impregnation | −0.065 | 0.021 | 0.885 | 0.937 (0.389–2.257) | |
| Intimacy with partners after COVID-19 | 1.107 | ||||
| Essentially unchanged | Ref. | ||||
| Strained | 1.337 | 18.281 | <0.001 | 3.808 (2.063–7.028) | |
| More intimate | 0.101 | 0.310 | 0.577 | 1.106 (0.776–1.577) | |
| Impact on household income after COVID-19 | 1.211 | ||||
| Essentially unchanged | Ref. | ||||
| Increased | −0.915 | 1.499 | 0.221 | 0.401 (0.093–1.732) | |
| Decreased 20–50% | 0.399 | 6.236 | 0.013 | 1.490 (1.090–2.038) | |
| Decrease 50% and above | 0.375 | 2.540 | 0.111 | 1.455 (0.917–2.309) | |
| Smoking habits | 1.047 | ||||
| No | Ref. | ||||
| Yes | 0.897 | 6.772 | 0.009 | 2.451 (1.248–4.815) | |
| Her partner’ drinking habits | 1.048 | ||||
| No | Ref. | ||||
| Yes | 0.404 | 7.266 | 0.007 | 1.497 (1.116–2.008) | |
| Exercise | 1.084 | ||||
| Yes | Ref. | ||||
| No | 0.479 | 6.847 | 0.009 | 1.615 (1.128–2.313) | |
| Sitting time per day(hour) | 1.192 | ||||
| ≤1 | Ref. | ||||
| 1–3 | −0.117 | 0.218 | 0.641 | 0.890 (0.545–1.452) | |
| 3–5 | 0.209 | 0.682 | 0.409 | 1.232 (0.751–2.021) | |
| 5–10 | 0.531 | 4.668 | 0.031 | 1.701 (1.051–2.755) | |
| ≥10 | 0.748 | 5.630 | 0.018 | 2.113 (1.139–3.921) |
VIF: Variance inflation factor.
Adjusted for age, educational level, medical insurance, working status, marital status, marriage age, professional psychological counseling before pregnancy, family care, gestation age, parity, number of abortions, pregnancy complications, pregnancy planning, expected mode of delivery, frequency of handwashing after going out after COVID-19, intimacy with partners after COVID-19, impact on household income after COVID-19, prenatal examination after COVID-19, smoking habits, drinking habits, partner drinking habits, exercise, sitting time.
4. Discussion
In this study, 9.8% of participants experienced symptoms of anxiety, which was lower than in our recent study (13.4%) used consistent screening tools (GAD-7) and conducted at the peak of the COVID-19 pandemic in Shenzhen City, China (Lin et al., 2020), suggesting that the prevalence of anxious pregnant women has decreased as the number of COVID-19 cases has visibly declined under strict control by the Chinese government. When compared with the case proportions reported in Canada (Lebel et al., 2020) (57.0%) and Qatar (Farrell et al., 2020) (34.4%) after the COVID-19 outbreak, the prevalence of anxiety symptoms in this study is much lower. The differences can be explained by different measurement tool adopted, cultural differences between the countries, and the relatively lower number of COVID-19 cases in China. Meanwhile, the prevalence of anxiety symptoms in our study was similar to that reported in a prior study (11.1%) (Ma et al., 2019) in Shanghai assessed by Self-Rating Anxiety Scale (SAS) before the COVID-19 outbreak, which further suggests that there was a limited influence of the pandemic on pregnant women when the COVID-19 situation became stable.
In terms of prenatal depression, we found a prevalence of 6.9% in pregnant women. The prevalence of depression in pregnant women in Turkey was 35.4% (Durankuş and Aksu, 2020), while in Canada it was 37% (Lebel et al., 2020) and in America it was 36.4% (Liu et al., 2021). The prevalence of prenatal depression worldwide was much higher than in China, suggesting that cultural, economic and regional differences play an essential role in this issue. However, the present finding was slightly lower than in our previous research that was carried out after the COVID-19 outbreak (Lin et al., 2020), which found the prevalence of prenatal depression to be 9.1% in pregnant women based on the PHQ-9 scale cut-off of 10. The combined results from these two studies indicate that depression in pregnant women fell as the number of COVID-19 cases decreased. In addition, the prevalence of depression reported in the present study was similar to other results in China (5.19% assessed by the self-rating depression scale (SDS) (Tang et al., 2019), 9.2% assessed by PHQ-9 (Yu et al., 2020)) obtained before the COVID-19 outbreak.
In general, depression and anxiety are highly comorbid (Kessler et al., 2003), and the contributory factors were found to be similar in this study. Pregnant women with abnormal marital status (unmarried/divorced/widowed) were more likely to experience prenatal anxiety and depression, inconsistent with previous studies (Fadzil et al., 2013). Interestingly, we found that pregnant women who had never received professional psychological counseling before pregnancy were at higher risk of anxiety and depression, indicating that previous psychological conditions could harm women after pregnancy. According to similar research, Chinese women are more family-oriented in contrast to western women, and family care is therefore especially important for pregnant women (Hu et al., 2019). In other words, lack of family care was found to be another factor closely associated with increased risk of prenatal symptoms of anxiety and depression in this study, which is consistent with a previous study conducted in Chengdu City, China (Hu et al., 2019). It is worth noting that pregnant women with education levels from junior high school to college were less likely to experience symptoms of prenatal depression in our study, whereas a cohort study in Japan reported that less education was associated with a higher prevalence of postpartum depressive symptoms (Matsumura et al., 2019), probably because the subjects were a postpartum population and cultures are different in the two countries. We found that prenatal depression was related to working status during pregnancy. Unemployment leads pregnant women to not only face economic pressure and social alienation, but concern about whether they can continue to work in the future (Bödecs et al., 2013; Tang et al., 2019).
In terms of obstetric characteristics, physiological changes during pregnancy often bring malaise to pregnant women. We found that complications during pregnancy significantly increased the risk of anxiety and depressive symptoms in pregnant women. In turn, antenatal depressive symptoms were associated prospectively with self-reports of perinatal complications in Ethiopia (Bitew et al., 2017). Similarly, pregnant women who experienced vaginal bleeding were more anxious than those who did not in our study, consistent with previous work (Ding et al., 2015) in Anhui Province, China. However, previous studies have suggested that pregnant women in the third trimester were more likely to worry about their baby's health and delivery and were considered to be at increased risk for depression (Bisetegn et al., 2016; Setse et al., 2009; Yu et al., 2020). In contrast, we found that pregnant women in the first trimester of pregnancy are likely to experience symptoms of depression, probably due to emotional responses to pregnancy. One study has suggested that depression during the third trimester might be caused by intermittent negative emotions that occur during the first trimester (Records and Rice, 2007). A relationship between unintended pregnancy and postpartum depressive symptoms has been confirmed in multiple studies (Leathers and Kelley, 2000; Najman et al., 1991), while here we revealed that unplanned pregnancy may also lead to prenatal depression, in line with previous findings in the Netherlands (van de Loo et al., 2018). In addition, labor pain is a subjective interaction between multiple physiological and psychological factors, the stress of which can result in feelings of diminished self-worth and self-confidence, and lead to self-aversion (Guittier et al., 2014). Labor pain reduces women's happiness, strength, courage and feelings of meaning and purpose during childbirth (Taghizdeh et al., 2017), while cesarean section, as a major obstetric operation, may lead to many major and minor short-term and long-term complications (da Silva Charvalho et al., 2019). Our investigation found that women who expected to give birth vaginally had reduced anxiety. There seem to be two primary explanations for this result: firstly, pregnant women hope to reduce any negative impacts of the operation on the child's health; and secondly, maternal complications are higher in cesarean sections compared with vaginal delivery (Sharma and Dhakal, 2018).
The COVID-19 pandemic has greatly impacted people's lives, especially those of pregnant women. Increasingly, assessment and management of depression and anxiety during pregnancy consider interpersonal relationships with partners (Glazier et al., 2004). In the present study, estrangement of pregnant women from their partners following the COVID-19 pandemic increased anxiety and symptoms of depression in pregnant women. Many people chose to self-isolate at home to reduce the spread of the coronavirus, and in those cases pregnant women spent more time with their intimate partners. However, during pregnancy, these women become more sensitive and they needed more care from family members, especially their partner. A previous study have shown that partner violence, especially emotional abuse, can lead to unhealthy emotions and even adverse birth outcomes for pregnant women (Yu et al., 2018). Social distancing and isolation at home after the COVID-19 pandemic has greatly impacted human health, causing sudden lifestyle changes with accompanying social and economic consequences (Di Renzo et al., 2020). Our results showed that pregnant women who suffered a reduction of 20–50% or over 50% in household income were likely to experience symptoms of prenatal anxiety and depression. Similarly, a reduction in household income of 20–50% greatly increased the risk of depressive symptoms. Therefore the economic fallout and increased unemployment caused by the COVID-19 crisis may explain why anxiety and depression increased in pregnant women (Ng et al., 2004).
Regarding lifestyle, previous studies have reported that smoking during pregnancy was harmful to offspring, increasing the likelihood of pre-term birth (Shah and Bracken, 2000), low birth weight (Tyrrell et al., 2012), and childhood psychological problems (Taylor et al., 2017). Interestingly, we also found that pregnant women who smoked were at higher risk of depression, while women who consumed alcoholic beverages were more likely to experience anxiety. Pregnancy is a stressful event that alters women's hormonal balance (Kendig et al., 2017), and thus pregnant women might tend to respond to their uncomfortable feelings by smoking and drinking. At the same time, our results showed that a partner's alcohol use increased depression in pregnant women, supporting the suggestion that alcohol abuse by a partner correlates with women's mental health (Davis et al., 2017). On the other hand, we proposed that depressive symptoms were more likely to occur in pregnant women who had little exercise, inconsistent with prior findings (Tang et al., 2019; Yu et al., 2020). Exercise affects neurotransmitters in the brain, including dopamine and serotonin that affect mood and behaviors (Greenwood and Fleshner, 2011), which may explain why pregnant women with physical training were more likely to control their negative emotions. Likewise, pregnant women who sat for more than 5 h per day were found to be at higher risk of anxiety and depression in the present study.
5. Strengths and limitations
This study represents the first investigation of prenatal mental health and risk factors among women throughout pregnancy after the COVID-19 pandemic. The participants were representative of the entire population of Shenzhen City. However, the present study did not investigate symptoms of anxiety and depression and their contributory factors in pregnant women before the COVID-19 pandemic, and so lacked a regional control. There were options in the questionnaire that needed to be filled out by participants recalling the situations of the last week, month or year, meaning that there was recall bias. However, the present study selected measurement tools with certain reliability and validity to minimize this problem. Additionally, after screening pregnant women for depression and anxiety symptoms, no further diagnosis and intervention was performed. Further research may explore the differences in the symptoms of anxiety and depression between pregnant women and the general population after the COVID-19 pandemic.
6. Conclusions
Our study shows that symptoms of anxiety and of depression in Shenzhen, China in post-pandemic era of COVID-19 were exhibited by 9.8% and 6.9%, respectively, of participants. Therefore, there has been relatively little effect of COVID-19 on anxiety and depression in pregnant women living through the post-pandemic era. Some of the sociodemographic characteristics, obstetric characteristics and lifestyles of individuals were shown to have a negative impact on pregnant women. Therefore, identification of strategies and taking measures to assist pregnant women exposed to risk factors seems to be essential. The results reported here can help professionals to identify high-risk pregnant women and offer effective advice for their families seeking to obtain improved living conditions, and further provide public health administration screening tools for adverse psychological events in pregnant women.
Authorship contribution statement
All authors have made substantial contributions to this study in the various sections described below. FW, WL, PL, and MZ originated the study, conceptualization, design, supervised implementation. FW, SH, CC, QL, WH and CZ acquired the data. FW, WL, YW, and QC interpreted the data and performed statistical analysis. FW wrote the draft of the manuscript. All authors contributed to the critical revision of the manuscript and gave their final approval for the manuscript to be published.
Funding
This research received support from the Shenzhen Science and Technology Innovation Committee (Grant number: JCYJ20170307091451207) and China Maternal and Child Health Association (Project number: 21). The funder did not involve in any part of the study process, from design to submit the article for publication.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors thank all the participants for their time and efforts.
References
- Bisetegn T.A., Mihretie G., Muche T. Prevalence and Predictors of Depression among Pregnant Women in Debretabor Town, Northwest Ethiopia. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0161108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitew T., Hanlon C., Kebede E., Honikman S., Fekadu A. Antenatal depressive symptoms and perinatal complications: a prospective study in rural Ethiopia. BMC Psychiatry. 2017;17:301. doi: 10.1186/s12888-017-1462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelica A., Cetkovic N., Trninic-Pjevic A., Mladenovic-Segedi L. The phenomenon of pregnancy - a psychological view. Ginekol. Pol. 2018;89:102–106. doi: 10.5603/GP.a2018.0017. [DOI] [PubMed] [Google Scholar]
- Bödecs T., Szilágyi E., Cholnoky P., Sándor J., Gonda X., Rihmer Z., Horváth B. Prevalence and psychosocial background of anxiety and depression emerging during the first trimester of pregnancy: data from a Hungarian population-based sample. Psychiatr. Danub. 2013;25:352–358. [PubMed] [Google Scholar]
- Colizzi M., Bortoletto R., Silvestri M., Mondini F., Puttini E., Cainelli C., Gaudino R., Ruggeri M., Zoccante L. Medically unexplained symptoms in the times of COVID-19 pandemic: a case-report. Brain, behavior, & immunity - health. 2020;5 doi: 10.1016/j.bbih.2020.100073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva Charvalho P., Hansson Bittár M., Vladic Stjernholm Y. Indications for increase in caesarean delivery. Reprod. Health. 2019;16:72. doi: 10.1186/s12978-019-0723-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis E.C., Rotheram-Borus M.J., Weichle T.W., Rezai R., Tomlinson M. Patterns of Alcohol Abuse, Depression, and Intimate Partner Violence Among Township Mothers in South Africa Over 5 Years. AIDS Behav. 2017;21:174–182. doi: 10.1007/s10461-017-1927-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attinà A., Cinelli G., Leggeri C., Caparello G., Barrea L., Scerbo F., Esposito E., De Lorenzo A. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J. Transl. Med. 2020;18:229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Q., Lu P., Fan Y., Xia Y., Liu M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan. China. J. med. virol. 2020;92:1549–1555. doi: 10.1002/jmv.25781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding X., Mao L., Ge X., Xu S., Pan W., Yan S., Huang K., Tao F. [Course and risk factors of maternal pregnancy-related anxiety across pregnancy in Ma’ anshan city] Wei Sheng Yan Jiu. 2015;44:371–375. [PubMed] [Google Scholar]
- Dunkel Schetter C., Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin. Psych. 2012;25:141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durankuş F., Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the. Int. Soc. Perinatal Obstet. 2020:1–7. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- Fadzil A., Balakrishnan K., Razali R., Sidi H., Malapan T., Japaraj R.P., Midin M., Nik Jaafar N.R., Das S., Manaf M.R. Risk factors for depression and anxiety among pregnant women in Hospital Tuanku Bainun, Ipoh, Malaysia. Asia-Pacific psychiatry: official journal of the Pacific Rim College of Psychiatrists. 2013;5(1):7–13. doi: 10.1111/appy.12036. Suppl. [DOI] [PubMed] [Google Scholar]
- Farrell T., Reagu S., Mohan S., Elmidany R., Qaddoura F., Ahmed E.E., Corbett G., Lindow S., Abuyaqoub S.M., Alabdulla M.A. The impact of the COVID-19 pandemic on the perinatal mental health of women. J. Perinat. Med. 2020;48:971–976. doi: 10.1515/jpm-2020-0415. [DOI] [PubMed] [Google Scholar]
- Gildner T.E., Laugier E.J., Thayer Z.M. Exercise routine change is associated with prenatal depression scores during the COVID-19 pandemic among pregnant women across the United States. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0243188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazier R.H., Elgar F.J., Goel V., Holzapfel S. Stress, social support, and emotional distress in a community sample of pregnant women. J. Psychosom. Obstet. Gynaecol. 2004;25:247–255. doi: 10.1080/01674820400024406. [DOI] [PubMed] [Google Scholar]
- Greenwood B.N., Fleshner M. Exercise, stress resistance, and central serotonergic systems. Exerc. Sport. Sci. Rev. 2011;39:140–149. doi: 10.1097/JES.0b013e31821f7e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guittier M.J., Cedraschi C., Jamei N., Boulvain M., Guillemin F. Impact of mode of delivery on the birth experience in first-time mothers: a qualitative study. BMC Pregnancy Childbirth. 2014;14:254. doi: 10.1186/1471-2393-14-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Wang Y., Wen S., Guo X., Xu L., Chen B., Chen P., Xu X., Wang Y. Association between social and family support and antenatal depression: a hospital-based study in Chengdu. China. BMC pregnancy and childbirth. 2019;19:420. doi: 10.1186/s12884-019-2510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui P.W., Ma G., Seto M.T.Y., Cheung K.W. Effect of COVID-19 on delivery plans and postnatal depression scores of pregnant women. Hong Kong medical journal = Xianggang yi xue za zhi. 2020 doi: 10.12809/hkmj208774. [DOI] [PubMed] [Google Scholar]
- Kendig S., Keats J.P., Hoffman M.C., Kay L.B., Miller E.S., Moore Simas T.A., Frieder A., Hackley B., Indman P., Raines C., Semenuk K., Wisner K.L., Lemieux L.A. Consensus Bundle on Maternal Mental Health: perinatal Depression and Anxiety. Obstet. Gynecol. 2017;129:422–430. doi: 10.1097/AOG.0000000000001902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K.R., Rush A.J., Walters E.E., Wang P.S. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kotabagi P., Fortune L., Essien S., Nauta M., Yoong W. Anxiety and depression levels among pregnant women with COVID-19. Acta. Obstet. Gynecol. Scand. 2020;99:953–954. doi: 10.1111/aogs.13928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leathers S.J., Kelley M.A. Unintended pregnancy and depressive symptoms among first-time mothers and fathers. Am. J. Orthopsych. 2000;70:523–531. doi: 10.1037/h0087671. [DOI] [PubMed] [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect Disord. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., Guo N., Jiang H., Eldadah M., Zhuang W. Social support and second trimester depression. Midwifery. 2019;69:158–162. doi: 10.1016/j.midw.2018.11.012. [DOI] [PubMed] [Google Scholar]
- Liang P., Wang Y., Shi S., Liu Y., Xiong R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: a cross-sectional study. BMC Psychiatry. 2020;20:557. doi: 10.1186/s12888-020-02969-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin W., Wu B., Chen B., Lai G., Huang S., Li S., Liu K., Zhong C., Huang W., Yuan S., Wang Y. Sleep Conditions Associate with Anxiety and Depression Symptoms among Pregnant Women during the Epidemic of COVID-19 in Shenzhen. J. Affect Disord. 2020 doi: 10.1016/j.jad.2020.11.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Erdei C., Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psych. Res. 2021;295 doi: 10.1016/j.psychres.2020.113552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X., Wang Y., Hu H., Tao X.G., Zhang Y., Shi H. The impact of resilience on prenatal anxiety and depression among pregnant women in Shanghai. J. Affect Disord. 2019;250:57–64. doi: 10.1016/j.jad.2019.02.058. [DOI] [PubMed] [Google Scholar]
- Macassa G., Tomaselli G. Rethinking developed nations’ health systems through a social sustainability perspective in the light of the COVID-19 pandemic. A viewpoint. J. Public Health Res. 2020;9:1834. doi: 10.4081/jphr.2020.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumura K., Hamazaki K., Tsuchida A., Kasamatsu H., Inadera H. Education level and risk of postpartum depression: results from the Japan Environment and Children’s Study (JECS) BMC Psychiatry. 2019;19:419. doi: 10.1186/s12888-019-2401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- Najman J.M., Morrison J., Williams G., Andersen M., Keeping J.D. The mental health of women 6 months after they give birth to an unwanted baby: a longitudinal study. Soc. Sci. Med. 1991;32:241–247. doi: 10.1016/0277-9536(91)90100-q. (1982) [DOI] [PubMed] [Google Scholar]
- Ng J., Sham A., Tang P.L., Fung S.J.T.B.J.o.M. SARS: pregnant women’s fears and perceptions. Br J. Midwifery. 2004;12:698–702. [Google Scholar]
- Pariente G., Wissotzky Broder O., Sheiner E., Lanxner Battat T., Mazor E., Yaniv Salem S., Kosef T., Wainstock T. Risk for probable post-partum depression among women during the COVID-19 pandemic. Arch Womens Ment. Health. 2020:1–7. doi: 10.1007/s00737-020-01075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Records K., Rice M. Psychosocial correlates of depression symptoms during the third trimester of pregnancy. J. obst., Gynecologic. Neonatal nursing: JOGNN. 2007;36:231–242. doi: 10.1111/j.1552-6909.2007.00140.x. [DOI] [PubMed] [Google Scholar]
- Setse R., Grogan R., Pham L., Cooper L.A., Strobino D., Powe N.R., Nicholson W. Longitudinal study of depressive symptoms and health-related quality of life during pregnancy and after delivery: the Health Status in Pregnancy (HIP) study. Matern. Child Health J. 2009;13:577–587. doi: 10.1007/s10995-008-0392-7. [DOI] [PubMed] [Google Scholar]
- Shah N.R., Bracken M.B. A systematic review and meta-analysis of prospective studies on the association between maternal cigarette smoking and preterm delivery. Am. J. Obstet. Gynecol. 2000;182:465–472. doi: 10.1016/s0002-9378(00)70240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S., Dhakal I. Cesarean vs Vaginal Delivery: an Institutional Experience. JNMA J. Nepal Med. Assoc. 2018;56:535–539. [PMC free article] [PubMed] [Google Scholar]
- Smilkstein G., Ashworth C., Montano D. Validity and reliability of the family APGAR as a test of family function. J. Fam. Pract. 1982;15:303–311. [PubMed] [Google Scholar]
- Taghizdeh Z., Ebadi A., Dehghani M., Gharacheh M., Yadollahi P. A time for psycho-spiritual transcendence: the experiences of Iranian women of pain during childbirth. Women and birth: J. Australian College of Midwives. 2017;30:491–496. doi: 10.1016/j.wombi.2017.04.010. [DOI] [PubMed] [Google Scholar]
- Tang X., Lu Z., Hu D., Zhong X. Influencing factors for prenatal Stress, anxiety and depression in early pregnancy among women in Chongqing. China. J. affective disorders. 2019;253:292–302. doi: 10.1016/j.jad.2019.05.003. [DOI] [PubMed] [Google Scholar]
- Taylor A.E., Carslake D., de Mola C.L., Rydell M., Nilsen T.I.L., Bjørngaard J.H., Horta B.L., Pearson R., Rai D., Galanti M.R., Barros F.C., Romundstad P.R., Davey Smith G., Munafò M.R. Maternal Smoking in Pregnancy and Offspring Depression: a cross cohort and negative control study. Sci. Rep. 2017;7:12579. doi: 10.1038/s41598-017-11836-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapa S.B., Mainali A., Schwank S.E., Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta. Obstet. Gynecol. Scand. 2020;99:817–818. doi: 10.1111/aogs.13894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong X., An D., McGonigal A., Park S.P., Zhou D. Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 2016;120:31–36. doi: 10.1016/j.eplepsyres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- Tyrrell J., Huikari V., Christie J.T., Cavadino A., Bakker R., Brion M.J., Geller F., Paternoster L., Myhre R., Potter C., Johnson P.C., Ebrahim S., Feenstra B., Hartikainen A.L., Hattersley A.T., Hofman A., Kaakinen M., Lowe L.P., Magnus P., McConnachie A., Melbye M., Ng J.W., Nohr E.A., Power C., Ring S.M., Sebert S.P., Sengpiel V., Taal H.R., Watt G.C., Sattar N., Relton C.L., Jacobsson B., Frayling T.M., Sørensen T.I., Murray J.C., Lawlor D.A., Pennell C.E., Jaddoe V.W., Hypponen E., Lowe W.L., Jr., Jarvelin M.R., Davey Smith G., Freathy R.M. Genetic variation in the 15q25 nicotinic acetylcholine receptor gene cluster (CHRNA5-CHRNA3-CHRNB4) interacts with maternal self-reported smoking status during pregnancy to influence birth weight. Hum. Mol. Genet. 2012;21:5344–5358. doi: 10.1093/hmg/dds372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Loo K.F.E., Vlenterie R., Nikkels S.J., Merkus P., Roukema J., Verhaak C.M., Roeleveld N., van Gelder M. Depression and anxiety during pregnancy: the influence of maternal characteristics. Birth. 2018;45:478–489. doi: 10.1111/birt.12343. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Jiang X., Bao W., Xu G., Yang R., Shen M. Association of intimate partner violence during pregnancy, prenatal depression, and adverse birth outcomes in Wuhan. China. BMC pregnancy and childbirth. 2018;18:469. doi: 10.1186/s12884-018-2113-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., Zhu X., Xu H., Hu Z., Zhou W., Zheng B., Yin S. Prevalence of depression symptoms and its influencing factors among pregnant women in late pregnancy in urban areas of Hengyang City, Hunan Province, China: a cross-sectional study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-038511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.L., Liang W., Chen Z.M., Zhang H.M., Zhang J.H., Weng X.Q., Yang S.C., Zhang L., Shen L.J., Zhang Y.L. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia-Pacific psychiatry: official journal of the Pacific Rim College of Psychiatrists. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- Zhou Y., Shi H., Liu Z., Peng S., Wang R., Qi L., Li Z., Yang J., Ren Y., Song X., Zeng L., Qian W., Zhang X. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl Psychiatry. 2020;10:319. doi: 10.1038/s41398-020-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]