Abstract
To determine whether the past half-year of COVID-19-related lockdowns, stay-at-home orders, and social isolation were associated with changes in high-risk alcohol use, a total of 5,931 individuals completed the Alcohol Use Disorders Identification Test (AUDIT) at one of six time points from April through September 2020. Over the 6-month period, hazardous alcohol use and likely dependence increased month-by-month for those under lockdowns compared to those not under restrictions. This increase in harmful alcohol use and related behaviors is likely to have prolonged adverse psychosocial, interpersonal, occupational, and health impacts as the world attempts to recover from the pandemic crisis.
Keywords: Alcohol dependence, COVID-19, Lockdowns
1. Introduction
The rapid emergence of the COVID-19 pandemic has led to an extraordinary social and economic upheaval throughout the world. Beginning in March 2020, in an attempt to contain the spread of the novel coronavirus, local governments throughout the United States initiated orders for individuals to stay at home and shelter-in-place. With the vast majority of the nation staying home and many businesses closing for extended periods—or even permanently, tens of millions of workers found themselves losing their primary jobs within the first few months of the pandemic. Added to the financial uncertainty posed by job loss and expiring unemployment benefits, many people have also experienced the emotional strains of prolonged social isolation, loneliness, depression, and even suicidal ideation as stay-at-home restrictions were extended or re-initiated to curb surging infection rates (Killgore et al., 2020a, 2020b, 2020c). Under such situations, individuals often resort to increased alcohol intake to cope with emotional stress and chronic uncertainty (Esterwood and Saeed, 2020). Emerging data suggest that alcohol use began to increase in the summer months of 2020 as it became clear that the pandemic was likely to continue into the fall months (Pollard et al., 2020). Here, we sought to determine the effects of continued lockdown/stay-at-home orders on potentially hazardous alcohol use and dependence during the first six months of the COVID-19 pandemic in the U.S.
2. Methods
Between April and September 2020, we collected 5,931 cross-sectional responses to the Alcohol Use Disorders Identification Test (AUDIT) (Babor et al., 2001), divided across six data collections taken approximately one month apart (i.e., April 9–10, 2020, n = 929; May 11–14, 2020, n = 944; June 10–13, 2020, n = 1009; July 14–18, 2020, n = 1035; August 11–12, 2020, n = 998; September 10–11, 2020, n = 1016). Using an online survey, AUDIT data were collected from English speaking individuals (18–84 years old) across all 50 U.S. states, proportional to each state's population. Table 1 provides a breakdown of demographic data for each monthly administration. Participants were recruited via the Amazon Mechanical Turn (MTurk) online crowdsourcing platform (Litman et al., 2017). It has been reported that the MTurk platform typically has upwards of 250,000 workers available in the U.S. and has considerable turnover in new participants, allowing an effective tool for recruiting naïve participants for certain types of survey research (Robinson et al., 2019). Individuals registered on the MTurk platform were sent an email message indicating that they might be eligible to complete an online survey about attitudes related to COVID-19. Participants were only permitted to enroll and enter the study if they passed a simple screener for 6th grade English reading comprehension. To minimize dependence between samples across monthly administrations, participants were not allowed to enroll in the study if they had already participated in earlier administrations of the survey for four of the six data collections. All participants provided written informed consent and the protocol was approved by the Institutional Review Board of the University of Arizona.
Table 1.
Sample demographics by data collection month.
| Study Month | |||||||
|---|---|---|---|---|---|---|---|
| April | May | June | July | Aug | Sep | Total | |
| N | 929 | 944 | 1009 | 1035 | 998 | 1016 | 5931 |
| Age yrs. (M, SD) | 36.4 (12.3) | 36.0 (12.1) | 35.3 (11.8) | 35.7 (12.1) | 36.6 (12.2) | 37.4 (12.0) | 36.3 (12.1) |
| Sex (% Female) | 55.4 | 54.8 | 52.5 | 53.8 | 50.0 | 55.9 | 53.7 |
| Primary Job Loss due to COVID-19 (% yes) | 16.7 | 21.4 | 22.4 | 18.4 | 25.8 | 25.9 | 21.8 |
| Ethnicity (%) | |||||||
| White | 76.5 | 73.6 | 73.8 | 72.9 | 74.1 | 77.0 | 74.7 |
| Black/African American | 9.6 | 10.0 | 9.0 | 10.6 | 10.1 | 9.4 | 9.8 |
| Hispanic/Latino | 4.4 | 7.5 | 5.3 | 5.5 | 6.5 | 4.2 | 5.6 |
| Asian | 6.8 | 6.0 | 7.2 | 7.0 | 6.8 | 5.4 | 6.5 |
| Native American/Native Alaskan | 0.5 | 1.1 | 1.9 | 1.4 | 0.7 | 1.5 | 1.2 |
| Native Hawaiian/Pacific Islander | 0.1 | 0.3 | 0.2 | 0.3 | 0.2 | 0.4 | 0.3 |
| Other | 2.0 | 1.3 | 1.7 | 1.8 | 1.1 | 2.0 | 1.7 |
| Prefer not to answer | 0.0 | 0.2 | 0.9 | 0.5 | 0.4 | 0.2 | 0.4 |
| Household Income (%) | |||||||
| ≤$10K | 4.8 | 5.0 | 6.8 | 6.0 | 4.8 | 4.2 | 5.3 |
| $10K-$25K | 10.7 | 12.1 | 10.6 | 11.5 | 9.7 | 10.8 | 10.9 |
| $25K-$50K | 26.6 | 25.6 | 23.1 | 27.0 | 28.0 | 26.7 | 26.1 |
| $50K-$75K | 23.3 | 21.0 | 21.8 | 23.1 | 22.2 | 23.8 | 22.6 |
| $75K-$100K | 17.3 | 16.8 | 17.0 | 13.4 | 17.0 | 17.1 | 16.4 |
| $100K-150K | 11.9 | 12.1 | 12.8 | 12.7 | 11.1 | 10.9 | 11.9 |
| $150K-$200K | 3.6 | 4.0 | 5.0 | 4.2 | 4.2 | 3.3 | 4.0 |
| >$200K | 1.8 | 3.5 | 2.9 | 2.1 | 2.9 | 3.1 | 2.7 |
The AUDIT is a brief 10-item questionnaire with scores ranging from 0 to 40, that focuses on hazardous alcohol consumption (Babor et al., 2001). The items assess the frequency and quantity of alcohol consumed, behaviors associated with dependence, and harm resulting from alcohol use. While many cutoff scores have been proposed, a total score of 8 or above is often considered evidence of hazardous or harmful use of alcohol, 15 or above is widely accepted as suggestive of probable alcohol dependence that should be appropriately followed up with brief counselling and continued monitoring, while a score of 20 or higher is indicative of severe alcohol dependence that necessitates a referral for diagnostic evaluation and professional treatment (Babor et al., 2001). Here, our outcome variables included the mean AUDIT score, as well as the percentage of respondents who scored at or above each cutoff point (harmful use ≥ 8, probable dependence ≥ 15, and severe dependence ≥ 20). The independent variables included month of assessment (April, May, June, July, August, September 2020), and current lockdown/stay-at-home status (i.e., “currently on a stay-at-home, shelter-in-place, or lockdown order,” or otherwise “currently sheltering-in-place”). The proportion of each sample reporting they were under stay-at-home/lockdown generally declined over the half-year, but fluctuated significantly across months due to dynamic changes in local COVID-19 infection rates and government-imposed restrictions (April=93.3%, May=78.7%, June=44.2%, July=76.0%, August=42.1%, September=34.5%). Mean AUDIT data were analyzed with a 2 (lockdown status) x 6 (month) between-groups analysis of covariance (ANCOVA), controlling for age, sex, and primary job loss due to the COVID-19 pandemic. Furthermore, the percentage of respondents scoring above each of the three cutoff scores was compared across months, and across months by lockdown status using chi-square contingency table analyses.
3. Results
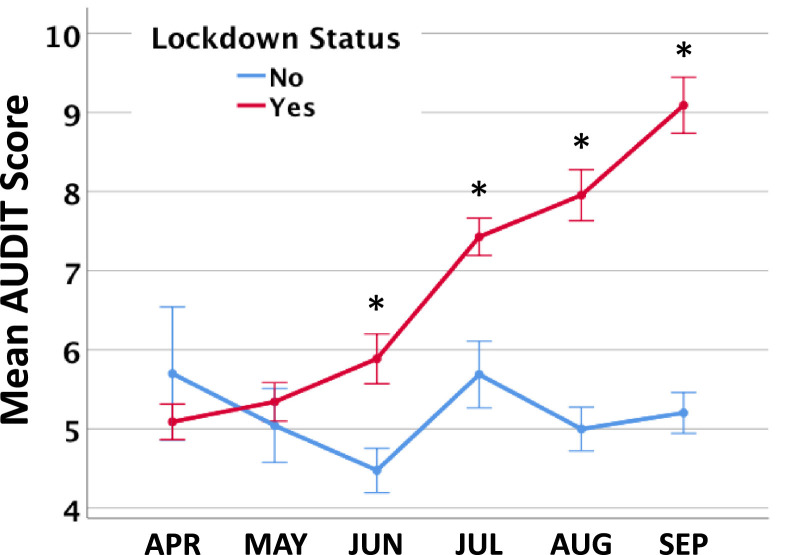
Over the six data collections there was a significant interaction between month and lockdown status on mean AUDIT scores (F 5,5916=9.04, p<.000001, ηp 2=0.008). Covariates of age (F 1,5916=37.34, p<.000001, ηp 2=0.006), sex (F 5,5916=98.46, p<.000001, ηp 2=0.016), and primary job loss (F 5,5916=238.97, p<.000001, ηp 2=0.039) accounted for significant variance, with job loss yielding by far the greatest effect size. Simple effects analyses revealed that AUDIT scores increased month-by-month for those under lockdown (F 5,3605=25.32, p<.000001), but not for those reporting no such restrictions (F 5,2308=1.74, p=.122). Bonferroni corrected post-hoc comparisons at each month revealed significantly greater AUDIT scores for those under lockdown during June (p=.001), July (p=.0003), August (p<.000001), and September (p<.00001) (see Fig. 1 ).
Fig. 1.
Estimated marginal mean scores on the Alcohol Use Disorders Identification Test (AUDIT) over the six months of the 2020 COVID-19 pandemic lockdown period. The figure shows an interaction between lockdown status and month (p < .000001). Simple effects analyses revealed a significant increase in month-by-month AUDIT scores for those reporting being under lockdown (red, p < .000001), but no significant difference across months for those not under lockdown (blue, p = .122). Post-hoc comparisons show significantly greater AUDIT scores for those under lockdown than not (*p ≤ 0.001, Bonferroni corrected).
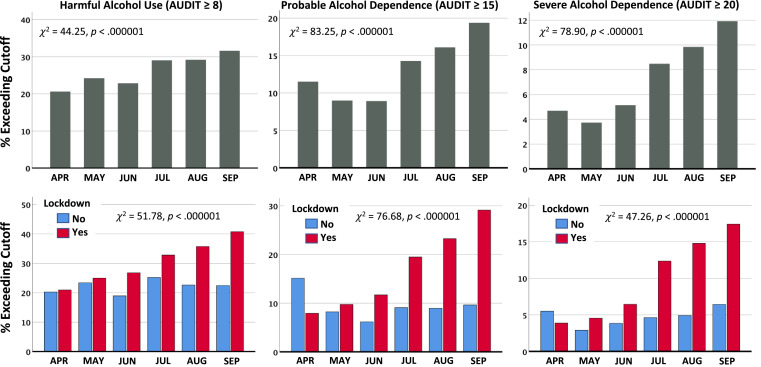
We also examined the percentage of participants at each month scoring above the three AUDIT severity cutoffs. Contingency table analyses showed that for the lowest threshold (harmful alcohol use >8), there was a significant increase across months in the proportion of individuals meeting the criterion cutoff (χ2(5)=44.26, p<.000001), but this differed by lockdown status (χ2(1)=51.78, p<.000001), with those remaining at home showing dramatically increasing rates over the 6-month period compared to those not under restrictions. Percentages (adjusted for covariates described above) for those under lockdown increased from 21.0% in April to 40.7% in September, but were essentially unchanged for those not under restrictions (see Fig. 2 ). For the intermediate threshold (probable alcohol dependence ≥15), there was a significant upward trend across months (χ2(5)=83.25, p<.000001), which differed by lockdown status (χ2(1)=76.68, p<.000001). Adjusted percentages for those under lockdown increased from 7.9% meeting criteria in April to 29.1% meeting this criterion by September (Fig. 2). Finally, for the most stringent cutoff (severe alcohol dependence ≥20), the overall prevalence increased over the six month period for the sample as a whole (χ2(5)=78.90, p<.000001). This finding differed by lockdown status (χ2(1)=47.26, p<.000001). Adjusted percentages for those under lockdown increased from 3.9% in April to 17.4% by September, but were essentially unchanged for those not under restrictions (Fig. 2).
Fig. 2.
The percentage of participants exceeding established cutoffs on the Alcohol Use Disorders Identification Test (AUDIT), adjusted for age, sex, and job loss. Left: Results for harmful alcohol use (AUDIT scores ≥ 8); Middle: Results for probable alcohol dependence (AUDIT scores ≥ 15); Right: Results for severe alcohol dependence (AUDIT scores ≥ 20). Top Row: Trends for the sample as a whole (n = 5931). Bottom Row: Effects of lockdown (red) versus no lockdown (blue).
4. Discussion
The dramatic increases in harmful alcohol consumption we observed over the first six months of the COVID-19 pandemic are concerning. First, greater alcohol consumption was associated with younger age, male sex, and primary job loss due to COVID-19, with by far the greatest influence produced by losing a job during the pandemic. Second, the greatest increase in high-risk drinking over the course of the pandemic occurred predominantly among individuals who were under lockdowns or stay-at-home restrictions, meaning that they were confined to their homes in close proximity to other family members who were doing the same. As the pandemic continues, many families are experiencing increased stress as they are now responsible for ensuring that children stay actively involved in online educational activities, while still managing work-from-home responsibilities and general housework. Many individuals are also coping with the stresses of job losses and other economic hardships, social isolation, disrupted routines, and the general uncertainties and anxieties surrounding the virus itself. When harmful levels of alcohol use are added to this situation, there is an increased potential for aggressive behavior, domestic violence, child abuse, and/or neglect (Foran and O'Leary, 2008). Third, a large proportion of those under lockdowns/stay-at-home restrictions are working from home. Workers who would never consider consuming alcohol at the office are now free to drink to excess during work hours while at home, potentially leading to reduced motivation, poor judgment, increased errors, or presenteeism. In other words, intoxicated employees working from home may appear occupied as they check email and sit through online meetings, but may contribute very little of tangible value to their work. Prolonged presenteeism due to alcohol use while working from home could erode the long-term career potential of many individuals or even jeopardize the continued viability of the entities that employ them. Finally, there are grave concerns over the long-term health implications of the rising level of alcohol dependence, which has been associated with elevated rates of injuries, liver disease, cancer, somatic problems, psychiatric conditions, and all-cause mortality (Holst et al., 2017).
While our data, and that of others (Pollard et al., 2020; Szajnoga et al., 2020), suggest that the severity of alcohol misuse has increased over the course of the COVID-19 pandemic, other studies have pointed to declines in alcohol use during quarantine (Chodkiewicz et al., 2020; Sallie et al., 2020). However, those studies only reported data during the months of April (Chodkiewicz et al., 2020) or May 2020 (Sallie et al., 2020), which represents a time early in the pandemic when we also found the lowest alcohol scores on the AUDIT (see Fig. 1, Fig. 2). Our study now extends the available data across the first six months of the COVID-19 pandemic, providing a much broader understanding of the trajectory of harmful alcohol use during lockdowns. It is also important to acknowledge that these data are cross-sectional and we did not follow individuals longitudinally. Consequently, these findings only point to changes in population prevalence over time as the pandemic unfolds, not the effects of prolonged lockdowns on individual-level changes over time. These data strongly argue for the need for longitudinal studies to further inform appropriate policies for lockdowns. Nonetheless, our findings suggest that the rapidly increasing population prevalence of harmful alcohol use and dependence is likely to become a prominent physical and psychiatric health concern if these trends continue. As our nation and the world work tirelessly to recover from the COVID-19 pandemic, the escalating rates of alcohol problems are likely to hamper the speed and effectiveness of this recovery.
Author statement
William Killgore: Conceptualization, Formal analysis, Resources, Data Curation, Writing-Original Draft, Review & Editing, Supervision, Funding Acquisition. Sara Cloonan: Investigation, Writing-Review & Editing. Emily Taylor: Project Administration, Writing-Review & Editing. Daniel Lucas: Writing-Review & Editing. Natalie Dailey: Conceptualization, Writing-Review & Editing.
Funding
None.
Declaration of Competing Interest
None.
References
- Babor T.F., de la Fuente J.R., Saunders J., Grant M. 2nd ed. World Health Organization; 2001. The Alcohol Use Disorders Indetification Test: Guidelines for Use in Primary Care. [Google Scholar]
- Chodkiewicz J., Talarowska M., Miniszewska J., Nawrocka N., Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int. J. Environ. Res. Public Health. 2020;(13):17. doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esterwood E., Saeed S.A. Past epidemics, natural disasters, COVID19, and mental health: learning from history as we deal with the present and prepare for the future. Psychiatr. Q. 2020 doi: 10.1007/s11126-020-09808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foran H.M., O’Leary K.D. Alcohol and intimate partner violence: a meta-analytic review. Clin. Psychol. Rev. 2008;28(7):1222–1234. doi: 10.1016/j.cpr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Holst C., Tolstrup J.S., Sorensen H.J., Becker U. Alcohol dependence and risk of somatic diseases and mortality: a cohort study in 19 002 men and women attending alcohol treatment. Addiction. 2017;112(8):1358–1366. doi: 10.1111/add.13799. [DOI] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Allbright M.C., Dailey N.S. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Lucas D.A., Dailey N.S. Loneliness during the first half-year of COVID-19 Lockdowns. Psychiatry Res. 2020;294 doi: 10.1016/j.psychres.2020.113551. [DOI] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Miller M.A., Dailey N.S. Three months of loneliness during the COVID-19 lockdown. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litman L., Robinson J., Abberbock T. TurkPrime.com: a versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav. Res. Methods. 2017;49(2):433–442. doi: 10.3758/s13428-016-0727-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D., Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J., Rosenzweig C., Moss A.J., Litman L. Tapped out or barely tapped? Recommendations for how to harness the vast and largely unused potential of the Mechanical Turk participant pool. PLoS ONE. 2019;14(12) doi: 10.1371/journal.pone.0226394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallie S.N., Ritou V., Bowden-Jones H., Voon V. Assessing international alcohol consumption patterns during isolation from the COVID-19 pandemic using an online survey: highlighting negative emotionality mechanisms. BMJ Open. 2020;10(11) doi: 10.1136/bmjopen-2020-044276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szajnoga D., Klimek-Tulwin M., Piekut A. COVID-19 lockdown leads to changes in alcohol consumption patterns. Results from the Polish national survey. J. Addict. Dis. 2020:1–12. doi: 10.1080/10550887.2020.1848247. [DOI] [PubMed] [Google Scholar]