Abstract
This study sought to examine if mental health issues, namely depression and anxiety symptoms, and loneliness were experienced differently according to various demographic groups during the COVID-19 pandemic (i.e., a societal stressor). An online survey, comprising demographic questions and questionnaires on depression, anxiety and loneliness symptoms, was distributed in Canada during the height of social distancing restrictions during the COVID-19 pandemic. Respondents (N=661) from lower income households experienced greater anxiety, depression and loneliness. Specifically, loneliness was greater in those with an annual income <$50,000/yr versus higher income brackets. Younger females (18-29yr) displayed greater anxiety, depressive symptoms and loneliness than their male counterparts; this difference did not exist among the other age groups (30-64yr, >65yr). Moreover, loneliness scores increased with increasing depression and anxiety symptom severity category. The relationship between loneliness and depression symptoms was moderated by gender, such that females experienced higher depressive symptoms when encountering greater loneliness. These data identify younger females, individuals with lower income, and those living alone as experiencing greater loneliness and mental health challenges during the height of the pandemic in Canada. We highlight the strong relationship between loneliness, depression and anxiety, and emphasize increased vulnerability among certain cohorts.
Keywords: Anxiety, Depression, Gender, Income, Young adults, Living arrangements
1. Introduction
Loneliness is a potent risk factor for developing a number of health conditions, such as coronary heart disease and stroke (Valtorta et al., 2016), and is associated with a 26%-50% increased risk in mortality (Holt-Lunstad et al., 2015, 2010). Moreover, while loneliness is a subjective state that can be felt even in the presence of others (Cacioppo and Cacioppo, 2018), the effects are no different than objective measures of social isolation (Holt-Lunstad et al., 2015). In fact, the impacts of loneliness on health are similar to well-established risk factors such as smoking, hypertension and obesity (Holt-Lunstad and Smith, 2016). In terms of mental health, loneliness and social isolation are not just strongly correlated with depression (Pitman et al., 2018), but can increase vulnerability to developing future depressive episodes (Cruwys et al., 2013; Cacioppo et al., 2010). Taken together, loneliness has been a significant and growing concern for a number of years (Cacioppo and Cacioppo, 2018); however, it is now being more widely recognized as a critical public health issue with the arrival and continued impact of the COVID-19 pandemic (Killgore et al., 2020).
In March of 2020, the governments of a number of countries started to implement rather expansive social restriction measures to reduce the spread of the COVID-19 virus. Such restrictions represented an intense stressor that has negatively impacted social connectedness (Bricker, 2020) and mental health in the general population (Findlay and Arim, 2020). While it might have been anticipated that older adults would be at particularly high-risk to the negative psychological impacts of COVID-19 (Meng et al., 2020), emerging data indicate the opposite. It appears to be disproportionately impacting the mental health of younger populations (Statistics Canada, 2020) and their perceived loneliness (Bricker, 2020; Luchetti et al., 2020). Emerging data indicate that 69% of young Canadians (aged 18-24) reported experiencing loneliness due to the physical distancing measures imposed during COVID-19, compared to 54% of the general population (Bricker, 2020). Data from the United Kingdom, Austria and Spain, indicate that both a younger age and female gender are identified risk factors for loneliness during COVID-19 (González-Sanguino et al., 2020; Li and Wang, 2020; Pieh et al., 2020).
Youth and young adulthood represents a period of increased vulnerability for the emergence of mental health disorders (Patten, 2017). According to the 2012 Canadian Community Health Survey-Mental Health, 15-24-year-olds have the highest rates of anxiety and mood disorders compared to all other age groups (Statistics Canada, 2012), which is comparable with European and American data. Critically, it appears that mental health concerns (and concurrent decrease in mental well-being) have increased most dramatically among those aged 15-24 during COVID-19 compared to reports obtained in 2018 in Canada (Findlay and Arim, 2020; Statistics Canada, 2012). Similarly, the prevalence of anxiety, distress and post-traumatic stress disorder (PTSD) symptomatology linked to COVID-19 was found to be greater among transitional aged youth/young adults relative to older individuals in Italian and Spanish populations (Casagrande et al., 2020; Odriozola-González et al., 2020).
What has emerged from data in other countries, is that beyond age and gender, the negative effects of COVID-19 on mental health are disproportionately impacting disadvantaged groups (Mishra et al., 2020; Pieh et al., 2020). However, North American data on the effects of COVID-19 among specific groups are limited (Williamson et al., 2020). The current study aimed to fill these gaps, by examining the influence of gender, age, living arrangements, income and depression and anxiety symptoms, on subjective ratings of loneliness among Canadians during the height of the COVID-19 pandemic. We hypothesized that ratings of loneliness would be highest in young adult females, individuals living alone, and those in low-income households. Moreover, we predicted higher scores of depressive and anxiety symptoms in young females, and a positive relationship between loneliness and depression and anxiety scores. Specifically, we expected a moderating role of gender in these relationships, with a stronger link in females. This study centered on examining groups at potentially increased risk of negative mental health impacts of the COVID-19 pandemic; such information is a critical first-step to informing targeted supports/services and policies for disadvantaged groups during and after this pandemic.
2. Methods
2.1. Procedure
The survey was developed and distributed using the Research Electronic Data Capture (REDCap; Harris et al., 2009). The survey link was distributed across Canada by the researchers’ personal and professional networks via email/social media (e.g. Facebook, Twitter, Royal Ottawa Mental Health Centre [ROMHC] communications team). Individuals able to consent to participating in research in Canada, and who were able to read and understand English, were invited to participate. All respondents were assured anonymity. The survey was launched on April 27, 2020 and closed July 17, 2020. Data were only included when COVID-19-related restrictions were extensive; i.e. when schools/daycares were closed (except for essential workers), as were other public venues such as bars, restaurants and movie theaters. Social gatherings were restricted to essential services, and physical distancing and strict social gathering limits were imposed (<15 people in Canada, except British Columbia where gatherings were not as restrictive [<50]). Restriction measures were determined based on government communications. The survey took ~15-20min to complete. This research was approved by the Research Ethics Board (REB) of the ROMHC (REB#2020006).
2.2. Measures
2.2.1. Demographics
Demographic and socioeconomic questions included age, sex at birth, gender identity, annual household income level (<$25,000; $25,000-50,000; $50,000-100,000; $100,000-200,000; >$200,000), education level (high school diploma; college diploma; some post-secondary education; Bachelor's; Master's; Doctorate/PhD) and living arrangement (with roommates; with parents; alone; with partner/spouse; with family [combination of partner/spouse, children, parents]). Questions related to physical and mental health were also collected, including the presence of any current psychological/psychiatric disorders (yes/no).
Age was considered as a continuous variable in some models. However, in order to examine the effects of loneliness specifically among young adults (in line with our hypotheses), age categories were created. Initially, these included four age groups: (1) 18-29, (2) 30-44, (3) 45-64 and (4) 65+ years. However, in our final analyses, individuals in the 30-44 and 45-64-year-old groups were collapsed as their mean loneliness scores (M=8.91, SE=.34 and M=8.60, SE=.33, respectively) did not differ (p=1.00).
2.2.2. Depressive symptoms
To assess depression symptoms, the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) was administered; this is a 9-item questionnaire that measures symptoms of depression on a 4-point Likert scale (range: 0-3). Total PHG-9 scores were summed (Cronbach's α=.89). Categories were also assessed as indices of depression symptom severity, as reported previously (0-4: none/minimal symptoms; 5-9: mild symptoms; 10-14: moderate symptoms; 15-19: moderate-severe symptoms, and 20-27: severe symptoms; Kroenke et al., 2001). In the current study, the moderate-severe and severe symptom categories were collapsed (referred to as “severe”) due small number of respondents that fell into the latter category (N=28).
2.2.3. Anxiety symptoms
Anxiety symptoms were examined using the Generalized Anxiety Scale (GAD-7; Spitzer et al., 2006), a 7-item questionnaire, with items being on a 4-point Likert scale (range: 0-3). Total GAD-7 scores were summed (Cronbach's α=.91). Categories of anxiety severity included: no symptoms (scores=0-4), mild (scores=5-9), moderate (scores=10-14) and severe symptoms (scores=15-21), in keeping with the original symptom category boundaries proposed by Spitzer and colleagues (2006).
2.2.4. Loneliness symptoms
The 8-item UCLA Loneliness Scale (ULS-8; Russell, 1996) was administered, on which items are rated on a 4-point Likert scale (range: 0-3). Higher scores (range: 0-24) indicate more frequent and intense feelings of loneliness (Cronbach's α=.81).
2.3. Data cleaning/quality control
Incomplete surveys (>10% of required questions unanswered; n=4), were removed from the final dataset. Missing questionnaire values (PHQ9, GAD-7, ULS-8) were imputed by calculating average values of participants’ responses on the remaining questions, restricted to only one imputed value per questionnaire (PHQ-9: n=5; GAD-7, n=4; ULS-8, n=0). Participants with >2 missing values per questionnaire were excluded (n=0). Data quality (i.e., to ensure that participants did not respond randomly) was assessed using 15 quality control checks for consistency in participants’ responses (i.e., degree of similarity between comparable questions; if responses on such questions were opposite, these were flagged). Two individuals were removed from the dataset (failed >4 quality controls); the final sample consisted of n=661 respondents.
2.4. Statistics
Statistical analyses were performed using SPSS for Windows 24.0 (SPSS, Chicago, Illinois, USA). Pearson product moment correlations were conducted between age and total loneliness, depression and anxiety scores; Spearman's Rho was used to correlate these variables to income categories. Correlations of r=.00-.29 were considered weak, r=.30-.59 were moderate, and r=.60-1.0 were strong. The influence of annual household income categories, depression (PHQ-9) and anxiety (GAD-7) symptom categories on loneliness (ULS-8) ratings was assessed using one-way analysis of variance (ANOVA) tests. A one-way analysis of covariance (ANCOVA) was conducted to examine loneliness according to living arrangement categories, with age as a covariate (as it was expected that living arrangements would be confounded by age). A two-way ANOVA was used to assess the influence of both gender and age categories (18-29 years, 30-64 years, 65+ years) on loneliness, depressive and anxiety ratings. Additionally, two-way ANCOVAs were conducted when examining total loneliness symptoms, total depression and total anxiety symptoms as a function of gender and age categories with household income category included as a covariate as it was related to each of these outcome variables. Follow-up comparisons were Bonferroni-corrected t-tests for significant (p<.05) outcomes. We were interested in examining how gender identities differed on variables of interest, however, given the small sample in categories other than male/female, this was not possible. Individuals who did not identify as male/female (N=9) were not included in models where gender was an independent variable. To examine the moderating role of gender in the relationship between loneliness with depression and anxiety scores, PROCESS (model 1) was used (Hayes, 2012). Moderation analyses were also re-analyzed with age as a covariate and results remained identical (data not shown). Significant findings were considered at p< .05.
3. Results
3.1. Participants
Table 1 includes detailed demographic data of all respondents (n=661).
Table 1.
Participant demographic and socioeconomic information (Ns and Percentages).
| Demographics | Population (n) | Percentage (%) | |
|---|---|---|---|
| Age categories (yr) | 18 – 29 | 157 | 23.8 |
| 30 – 64 | 434 | 65.7 | |
| 65+ | 69 | 10.4 | |
| Gender | Female | 511 | 77.3 |
| Male | 140 | 21.2 | |
| Non-binary | 3 | 0.5 | |
| Gender fluid | 1 | 0.2 | |
| Gender queer | 1 | 0.2 | |
| Two-spirit | 1 | 0.2 | |
| Other | 3 | 0.5 | |
| Annual household income (CDN) | <$25, 000 | 38 | 5.8 |
| $25,000 - $50, 000 | 77 | 11.7 | |
| $50, 000 – $100, 000 | 207 | 31.5 | |
| $100,000 - $200, 000 | 206 | 31.3 | |
| >$200, 000 | 75 | 11.4 | |
| Prefer not to say | 55 | 8.3 | |
| Education (highest level completed) | Bachelor's Degree | 215 | 32.5 |
| Master's Degree | 139 | 21.0 | |
| Doctorate Degree | 93 | 14.1 | |
| College diploma | 94 | 14.2 | |
| Some Post-Secondary | 63 | 9.5 | |
| High school | 47 | 7.1 | |
| Other | 10 | 1.5 | |
| Living arrangement | Partner & children/parents | 254 | 38.5 |
| Partner/spouse | 194 | 27.4 | |
| Alone | 108 | 16.4 | |
| Parents only | 62 | 9.4 | |
| Roommates | 31 | 4.7 | |
| Other | 10 | 1.5 | |
| Current mental health disorder | No | 269 | 71.0 |
| Yes | 163 | 24.7 | |
| Do not know | 25 | 3.8 |
3.2. Correlations
Total loneliness (ULS-8) scores were positively and moderately related to GAD-7-indexed anxiety (r=.50, n=661), and had a strong positive association with PHQ-9-indexed depression symptoms (r=.61, n=661). Loneliness was negatively, albeit weakly, associated with age (r=.-23, n=660) and income categories (rho=.-21, n=603). Age was also weakly correlated with income categories (rho=.24, n=603), GAD-7 (r=-.28, n=660) and PHQ-9 (r=-.27, n=660) scores. Finally, income categories weakly correlated with GAD-7 (rho=-.18, n=603) and PHQ-9 scores (rho=-.27, n=603). All correlations were p<.001.
3.3. Severity of anxiety and depression and loneliness differences
In sum, 43.0% of respondents (n=284) reported no/minimal depression symptoms, 31.2% (n=206) had mild symptoms, 13.8% (n=91) reported symptoms reflecting moderate depression, and 12.1% (n=80) were considered to have severe depression symptoms. Just over half (52.4%, n=346) reported no anxiety symptoms, 28.4% (n=188) had mild anxiety symptoms, 11.4% (n=75) had moderate symptoms, and 7.7% (n=51) reported symptoms consistent with severe anxiety.
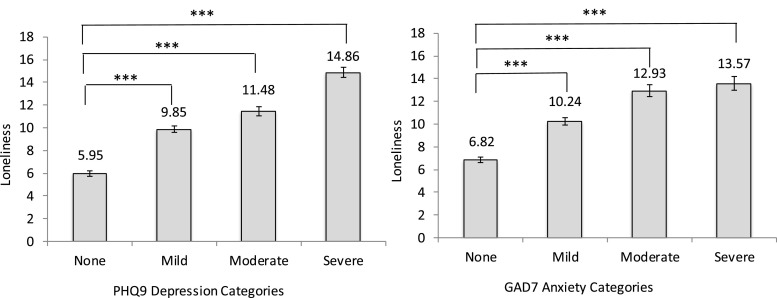
One-way ANOVAs yielded a main effect of depression and anxiety symptom categories on loneliness scores ([F(3,657)=125.06, p<.001, η 2 =.36] and [F(3,656)=71.91, p<.001, η 2 =.25], respectively). Individuals with no/minimal depression symptoms had lower loneliness scores from those with mild, moderate and severe depression symptom profiles (ps<.001; Fig. 1 A). Additionally, loneliness scores increased with each increase in depression severity category (ps<.01). Similarly, respondents with no anxiety symptoms had lower loneliness scores than those with mild, moderate, and severe anxiety symptoms (ps< .001; Fig. 1 B). Loneliness scores also increased with each increase in anxiety severity category (ps<.001). Finally, individuals who reported a current mental health disorder had higher loneliness scores (n=163; M=11.20, SEM=0.43) compared to those without a mental health disorder (n=469; 8.03, SEM=0.21) [t(244.64)=-6.67, p<.001].
Fig. 1.
ULS-8 loneliness scores according to PHQ-9 depression and GAD-7 anxiety categories (mean ± standard error presented), ***p<.001.
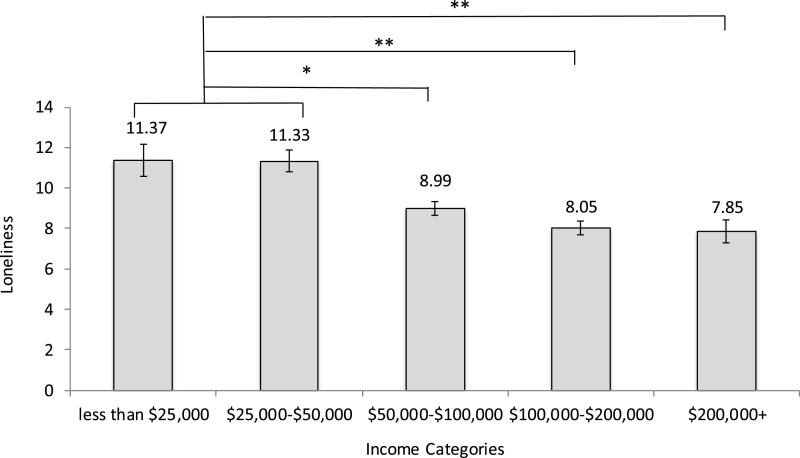
3.4. Loneliness differences according to income and living arrangements
Loneliness differed according to household annual income [F(4,598)=9.87, p<.001, η 2 =.06; Fig. 2 ]. Respondents who reported an income <$25,000, experienced greater loneliness compared to those in other categories (ps<.05), except those making $25,000-$50,000 (p=1.00). Similarly, those earning $25,000-$50,000 experienced greater loneliness than those in the higher income categories (ps<.003). Respondents making >$50,000 did not differ from each other on loneliness scores (ps=.49-1.0).
Fig. 2.
ULS-8 loneliness scores according to income categories (mean ± standard error presented), *p<05, **p<.01.
The ANCOVA (controlling for age) revealed that loneliness scores also differed according to living arrangement [F(4,642)=12.22, p<.001, η 2 =.07]. Respondents living with a parent(s) reported greater loneliness (M=11.23, SEM=0.66) compared to those living with a partner/spouse (M=7.78, SEM=0.35, p<.001) and those living with a number of family members (including partner/spouse and children/parents; M=8.61, SEM=0.30 p=.003). Respondents who lived alone (M=11.15, SEM=0.46) also reported greater loneliness than those living with a partner/spouse and a number of family members (ps<.001). Those living with roommates (M=8.74, SEM=0.89) did not differ on loneliness scores compared to any groups (ps=.19-1.0).
3.5. Loneliness and mental health differences according to gender and age categories
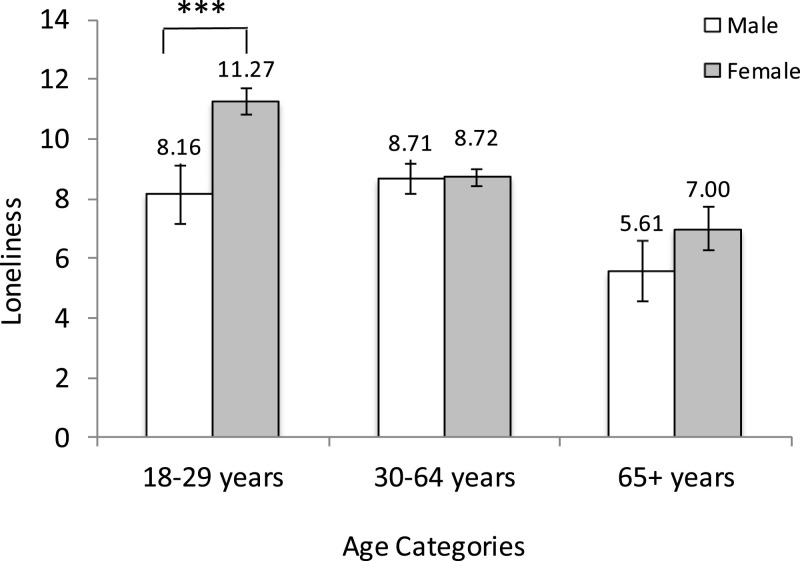
Loneliness scores differed significantly according to gender [F(1,650)=6.85, p=.009, η 2 =.01] and age categories [F(2,650)=9.15, p<.001, η 2 = .03)]; further, a gender × age category interaction existed [F(2,650)=3.44, p=.03, η 2 =.01]. Simple effects comprising this interaction revealed that females reported significantly higher loneliness than males, but only among the 18-29-year-olds (p=.003). There were no gender differences in loneliness scores among individuals aged 30-64yr (p=.98) or >65yr (p=.26; Fig. 3 ). As income was significantly related to loneliness, it was added as a covariate; the gender × age interaction was strengthened [F(2,587)=5.98, p=.003, η 2 =.02].
Fig. 3.
ULS-8 loneliness scores according to gender and age categories (mean ± standard error reported), ***p< .001.
Depression scores significantly differed according to gender [F(1,644)=11.55, p=.001, η 2 =.02] and age categories [F(2,644)=9.71, p< .001, η 2 =.03)]; further, a gender × age category interaction existed [F(2,644)=5.21, p=.006, η 2 =.02]. Simple effects comprising this interaction revealed that females hadsignificantly higher depression scores than males, but only among the 18-29-year-olds (p<.001). There were no gender differences in depression scores among individuals aged 30-64yr (p=.18) or those aged >65yr (p =.64). Moreover, as income category was related to depression scores, it was added as a covariate; the gender × age category interaction effect was strengthened [F(2,587)=6.90, p=.001, η 2 =.02].
Similarly, anxiety scores significantly differed according to gender [F(1,644)=7.39, p=.007, η 2 = .01] and age categories [F(2,644)=10.54, p<.001, η 2 =.03)]; further, a gender × age category interaction existed [F(2,644)=3.34, p=.04, η 2 = .01]. Simple effects comprising this interaction revealed that females had significantly higher anxiety scores than males, but, again, only among the 18-29-year-olds (p=.001). There were no gender differences in anxiety scores among individuals aged 30-64yr (p=.47) or >65yr (p=.53). Moreover, as income also related to anxiety scores, it was added as a covariate; again, the gender × age interaction effect was strengthened [F(2,587)=5.10, p=.006, η 2 =.02].
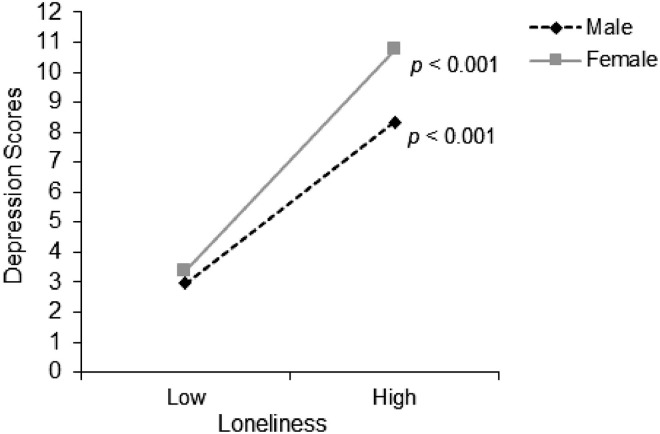
3.6. Loneliness in relation to depression and anxiety symptoms moderated by gender
A moderation analysis was conducted to examine whether the relationship between loneliness and depression scores was moderated by gender. The overall model was significant (R2=.39, [F(3,647)=4.95, p<.001]), and a significant interaction existed between gender and loneliness in relation to depression scores [R2change=.01, F(1,647)=5.79, p=.02]. As shown in Fig. 4 , the relationship between loneliness and depression was stronger for females (B=.74, p<.001), but also existed in males (B=.54, p<.001). The moderating role of gender was also examined in the relation between loneliness and anxiety, but, was not significant [R2change=.003, F(1,647)=2.20, p=.14].
Fig. 4.
The moderating role of gender in the relationship between ULS-8-indexed loneliness and PHQ-9-indexed depression scores.
4. Discussion
The current findings are among the first to show that individuals from lower income households, individuals living alone or with their parents, and young females, in particular, experienced higher anxiety and depression scores, and greater loneliness during the peak of the COVID-19 restrictions in Canada. In fact, loneliness was significantly higher for those with an annual income <$50,000/year compared with an income category of >$50,000/year. Thus, while economic inequalities have been tied to mental health prior to COVID-19 (Cairney and Streiner, 2010; Reiss, 2013), this pandemic appears to be exacerbating these effects. Prior to COVID-19, loneliness affected up to a half of adults, and has been discussed as the “great equalizer”, in that it does not necessarily target any one group, with socio-demographic factors such as sex, ethnicity, income and education not being all that protective (Cacioppo and Cacioppo, 2018; Polack, 2018). Our findings are consistent with recent reports showing that the negative impacts of the COVID-19 pandemic on health and wellness are disproportionately affecting disadvantaged groups (Mishra et al., 2020; Pieh et al., 2020). This includes ethnic minorities (Kapilashrami and Bhui, 2020) and individuals in low income brackets (Pieh et al., 2020; Tull et al., 2020). Due to the rather homogenous ethnic make-up of our sample (83.8% White), we could not adequately assess the contribution of ethnicity on measures of wellbeing, though this is certainly a critical consideration in future.
As expected, and in-line with other studies during the pandemic (Li and Wang, 2020), respondents in the current study who reported living alone had higher levels of loneliness than those living with other family members and/or with a spouse. Unexpectedly, individuals living with their parents displayed similarly high levels of loneliness as those living alone. While age was included as a covariate, it is expected that respondents in our younger cohort (18-29-year-olds) would be most likely to live with their parents. Individuals in this age group might represent a cohort most inclined to move out on their own (i.e., unsettled in their current situation) and/or could include a student population who moved back to live with their parents during the pandemic, away from their friends/peers (and, potentially school and jobs). Since relationships with friends and peers play such an important role at this age (Mundt and Zakletskaia, 2014), the potential removal of these supports during the pandemic could have been a significant contributing factor to the detriment of mental health among this younger cohort. Granted, this is speculative as we did not directly ask about the change in living situation during the pandemic.
During COVID-19, we found that a younger age is related to higher loneliness, depression and anxiety symptoms. While extensive literature exists regarding loneliness among older adults (Courtin and Knapp, 2017), loneliness might actually be a larger problem in younger adults, as feelings of loneliness can stabilize or decline with increased age (Beam and Kim, 2020). In fact, prior to COVID-19, a study in the United States of 20,000 individuals identified Generation X (18-22-year-olds) as the ‘loneliness cohort’ (Polack, 2018). Certainly, the COVID-19 pandemic has brought loneliness to the forefront, and data are showing that older age groups are less likely to feel lonely or develop psychiatric disorders during the COVID-19 pandemic; this may also be because young individuals’ educational, economic and social lives are more disrupted by this public health crisis (Cao et al., 2020). Emerging reports in Canada also show that the pandemic has resulted in greater increases in loneliness among 18-24-year-olds compared to the general population (Bricker, 2020). Similarly, the greatest declines in mental health during the pandemic have been reported among those aged 15-24 years (Findlay and Arim, 2020), which is consistent with our findings showing highest depression and anxiety symptoms in younger age groups.
Depression, anxiety and loneliness in the current study were tied not only to a younger age, but also to the female gender. We found an interaction between age groups and gender such that young (18-29-year-old) females had significantly elevated loneliness scores, and depression and anxiety symptoms than same-aged males. These effects were not found among the other age groups. Prior to COVID-19, gender differences in loneliness were either not found or were inconsistent (Heinrich and Gullone, 2006; Rokach, 2018), with a recent meta-analysis showing similar mean levels of loneliness in males and females across the lifespan (Maes et al., 2019). However, the finding that younger females - in particular - are more likely to experience increased depression and anxiety symptoms during COVID-19 is consistent with trends prior to its onset (Findlay and Arim, 2020; Hellemans et al., 2019); the pandemic might be exacerbating these differences. This could, in part, be due to intense isolation associated with this pandemic/societal stressor as females generally report a greater reliance on social cohesion/support than males during times of stress (Taylor et al., 2000), thus, increased isolation could result in greater wellbeing decreases in younger females. Indeed, before COVID-19, young females were found to be at higher risk of mental health concerns, including depression, anxiety and suicide attempts (Findlay, 2017; Gardner et al., 2019; Hellemans et al., 2019; McQuaid et al., 2019; Woods et al., 2020). Adolescence and early adulthood are critical periods both in terms of neurodevelopment, and in the concomitant development of mental health problems (Jaworska and MacQueen, 2015; Patten, 2017), during which time risk factors, such as stressors, may differentially affect females (Ferro et al., 2015).
In-line with a recent report during the pandemic (Killgore et al., 2020), we found a strong positive relationship between loneliness and depression, which were linked in a dose-related fashion. This relationship also emerged between anxiety severity and loneliness. While the loneliness-anxiety link is less established, it has been shown in an older adult sample (Domènech-Abella et al., 2019), whereas in young adults research has typically focused on social anxiety and loneliness. Thus, the current data extend earlier work showing a dose-related relationship between loneliness and more general anxiety symptom measures, including among young adults. Under circumstances not related to COVID-19, psychosocial factors such as social connections influence mental health (Cruwys et al., 2014; Haslam et al., 2015; Lamblin et al., 2017). In this regard, psychosocial functioning and experiencing stressors are strongly associated with depression among youth/young adults (Findlay, 2017; Vrshek-Schallhorn et al., 2015).
When considering the association between loneliness and mental health according to gender, we found a moderated relation. Although present in both genders, the relationship between loneliness and depression was stronger for females. This is in-line with a non-COVID-19-related study among college students showing that loneliness scores served as a longitudinal predictor for increased depressive symptoms for females but not males (Liu et al., 2020); although, in the current study, the relation also existed in males. Gender did not moderate the loneliness-anxiety relationship, which is inconsistent with prior research in African American college students (Chang, 2018). Nevertheless, our findings collectively show that higher loneliness is tied to greater depressive and anxiety outcomes in both males and females (despite being stronger in females).
Several limitations to the current work should be acknowledged. First, the study was cross-sectional, obfuscating causal or directional conclusions. As such, we cannot comment on how these findings were impacted or changed due to the COVID-19 pandemic directly (though we compared/framed our results in the context of available pre-pandemic data). Second, the study comprised a convenience sample, thus, the sample is not ethnically representative. Similarly, our sample included more females (77.3%) than males (21.2%); this is problematic for analyses considering males according to age groups as it resulted in relatively small samples sizes of males in the young adult and older adult categories. For this reason, the gender by age categroy interactions should be interpreted cautiously. Moreover, very few individuals identified as a gender other than male/female, thus, this variable could not be meaningfully explored. Also related to the representativeness of these data, this sample was highly educated, with >67% having completed a university degree, and representing higher income households (62.5% earned >$50,000/year). Thus, it is important to recognize that this does not reflect a generalizable Canadian sample, and that the lower end of the socioeconomic (SES) spectrum is not adequately reflected by these data. Despite a relative underrepresentation of low SES individuals, this sample was nevertheless large enough to observe a significant effect of SES (income-indexed) on loneliness. Further, this was an on-line study, available through the use of a computer or smart phone. Certainly, there are inequality issues related to access to technology (Harris et al., 2017), and individuals without access to on-line technologies during the COVID-19 pandemic might be particularly prone to loneliness. Finally, some effect sizes were small, suggesting that other factors than those identified are also important in understanding loneliness.
Despite the above limitations, the current study suggests that young adult females appear to be most susceptible to the impacts of COVID-19 (i.e., a salient and persistent stressor) on depressive and anxiety symptoms. Critically, loneliness might, in part, be responsible as it was strongly linked to depression scores. Further, these data demonstrate just how strong the loneliness-depression link is, revealing a dose-related increase in loneliness for each increase in depressive severity category. More novel, this was also shown for anxiety symptoms and loneliness. These data shed light on the inequalities associated with the pandemic on mental well-being in a Canadian adult cohort revealing that low socio-economic households can experience higher depression, anxiety and loneliness scores during the pandemic.
Author statement
R.M. aided in conceptualizing the study, conducted the analyses, and wrote the manuscript. A.A. conducted data collection, aided up in cleaning-up the data, and aided in editing the manuscript. S.M.L.C. aided in conceptualizing the study, in cleaning-up the data, and in interpreting the results. She also aided with manuscript writing and editing. N.J. conceptualized the study, oversaw the collection and clean-up of the data, and aided in analyses and interpretation of the results. She also aided in revising/editing the manuscript.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
References
- Beam C.R., Kim A.J. Psychological sequelae of social isolation and loneliness might be a larger problem in young adults than older adults. Psychol.Trauma Theory, Res. Pract. Policy. 2020 doi: 10.1037/tra0000774. Epub ahead of print]10/1037/tra0000774. [DOI] [PubMed] [Google Scholar]
- Bricker D. Ipsos; 2020. Majority (54%) of Canadians Say Physical Distancing has Left Them Feeling Lonely or Isolated. [Google Scholar]
- Cacioppo J.T., Cacioppo S. The growing problem of loneliness. Lancet. 2018;391:426. doi: 10.1016/S0140-6736(18)30142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C., Thisted R.A. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the chicago health, aging, and social relations study. Psychol. Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairney J., Streiner D.L. University of Toronto Press; 2010. Mental disorder in Canada: an Epidemiological Perspective, Mental Disorder in Canada: an Epidemiological Perspective. [DOI] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020:287. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang E.C. Relationship between loneliness and symptoms of anxiety and depression in African American men and women: evidence for gender as a moderator. Pers. Individ. Dif. 2018;120:138–143. doi: 10.1016/j.paid.2017.08.035. [DOI] [Google Scholar]
- Courtin E., Knapp M. Social isolation, loneliness and health in old age: a scoping review. Heal. Soc. Care Community. 2017;5:799–812. doi: 10.1111/hsc.12311. [DOI] [PubMed] [Google Scholar]
- Cruwys T., Dingle G.A., Haslam C., Haslam S.A., Jetten J., Morton T.A. Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Soc. Sci. Med. 2013;98:179–186. doi: 10.1016/j.socscimed.2013.09.013. [DOI] [PubMed] [Google Scholar]
- Cruwys T., Haslam S.A., Dingle G.A., Haslam C., Jetten J. Depression and social identity. Personal. Soc. Psychol. Rev. 2014;18:215–238. doi: 10.1177/1088868314523839. [DOI] [PubMed] [Google Scholar]
- Domènech-Abella J., Mundó J., Haro J.M., Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA) J. Affect. Disord. 2019;246:82–88. doi: 10.1016/j.jad.2018.12.043. [DOI] [PubMed] [Google Scholar]
- Ferro M.A., Gorter J.W., Boyle M.H. Trajectories of depressive symptoms in Canadian emerging adults. Am. J. Public Health. 2015;105:2322–2327. doi: 10.2105/AJPH.2015.302817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findlay L. Depression and suicidal ideation among Canadians aged 15 to 24. Heal. Rep. Stat. Canada. 2017:2020. Retrieved September 10. [PubMed] [Google Scholar]
- Findlay L., Arim R. StatCan COVID-19: Data to Insights for a Better Canada Canadians Report Lower Self-Perceived Mental Health during the COVID-19 Pandemic. 2020:2020. doi: 10.25318/82-003-x202000400003-eng. Retrieved September 10. [DOI] [PubMed] [Google Scholar]
- Gardner W., Pajer K., Cloutier P., Zemek R., Currie L., Hatcher S., Colman I., Bell D., Gray C., Cappelli M., Duque D.R., Lima I. Changing rates of self-harm and mental disorders by sex in youths presenting to Ontario emergency departments: repeated cross-sectional study. Can. J. Psychiatry. 2019;64:789–797. doi: 10.1177/0706743719854070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.040. EPub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris C., Straker L., Pollock C.A. Socioeconomic related 'digital divide' exists in how, not if, young people use computers. PLoS One. 2017;31(3) doi: 10.1371/journal.pone.0175011. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam C., Cruwys T., Haslam S.A., Jetten J. Encyclopedia of Geropsychology. Springer Singapore; Singapore: 2015. Social connectedness and health; pp. 1–10. [DOI] [Google Scholar]
- Hayes A.F. Manuscr. Submitt. Publ; 2012. PROCESS: a Versatile Computational Tool for Observed Variable Moderation, Mediation, and Conditional Process Modeling. [Google Scholar]
- Heinrich L.M., Gullone E. The clinical significance of loneliness: a literature review. Clin. Psychol. Rev. 2006;25:695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Hellemans K.G.C., Wilcox J., Nino J.N., Young M., McQuaid R.J. Cannabis use, anxiety, and perceptions of risk among Canadian undergraduates: the moderating role of gender. Can. J. Addict. 2019;10:22–29. doi: 10.1097/CXA.0000000000000059. [DOI] [Google Scholar]
- Holt-Lunstad J., Smith T.B. Loneliness and social isolation as risk factors for CVD: implications for evidence-based patient care and scientific inquiry. Heart. 2016;106:987–989. doi: 10.1136/heartjnl-2015-309242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010 doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaworska N., MacQueen G. Adolescence as a unique developmental period. J. Psychiatry Neurosci. 2015;40:291–293. doi: 10.1503/jpn.150268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapilashrami A., Bhui K. Mental health and COVID-19: is the virus racist? Br. J. Psychiatry. 2020:1–3. doi: 10.1192/bjp.2020.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113117. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamblin M., Murawski C., Whittle S., Fornito A. Social connectedness, mental health and the adolescent brain. Neurosci. Biobehav. Rev. 2017;80:57–68. doi: 10.1016/j.neubiorev.2017.05.010. [DOI] [PubMed] [Google Scholar]
- Li L.Z., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Zhang M., Yang Q., Yu B. Gender differences in the influence of social isolation and loneliness on depressive symptoms in college students: a longitudinal study. Soc. Psychiatry Psychiatr. Epidemiol. 2020;55:251–257. doi: 10.1007/s00127-019-01726-6. [DOI] [PubMed] [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., Sutin A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020 doi: 10.1037/amp0000690. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes M., Qualter P., Vanhalst J., Van den Noortgate W., Goossens L. Gender differences in loneliness across the lifespan: a meta-analysis. Eur. J. Pers. 2019;33:642–654. doi: 10.1002/per.2220. [DOI] [Google Scholar]
- McQuaid, R.J., Gabrys, R.L., McInnis, O.A., Anisman, H., Matheson, K., 2019. Understanding the relation between early-life adversity and depression symptoms: the moderating role of sex and an interleukin-1β gene variant. Front. Psychiatry 10. DOI: 10.3389/fpsyt.2019.00151. [DOI] [PMC free article] [PubMed]
- Meng H., Xu Y., Dai J., Zhang Y., Liu B., Yang H. Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.112983. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra S., Kwong J.C., Chan A.K., Baral S.D. Understanding heterogeneity to inform the public health response to COVID-19 in Canada. CMAJ. 2020 doi: 10.1503/cmaj.201112. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt M.P., Zakletskaia L.I. That's what friends are for: Adolescent peer social status, health-related quality of life and healthcare costs. Appl. Health Econ. Health Policy. 2014;12:191–201. doi: 10.1007/s40258-014-0084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten S.B. Age of onset of mental disorders. Can. J. Psychiatry. 2017;64:235–236. doi: 10.1177/0706743716685043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitman A., Mann F., Johnson S. The Lancet Psychiatry; 2018. Advancing our Understanding of Loneliness and Mental Health Problems in Young People. [DOI] [PubMed] [Google Scholar]
- Polack, E., 2018. New Cigna study reveals loneliness at epidemic levels in America. Accessed September 10, 2020.
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc. Sci. Med. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Rokach A. The effect of gender and culture on loneliness: a mini review. Emerg. Sci. J. 2018;2:59–64. doi: 10.28991/esj-2018-01128. [DOI] [Google Scholar]
- Russell D.W. UCLA loneliness scale (Version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Statistics Canada . 2020. Canadians’ Mental Health during the COVID-19 Pandemic. Ottawa, ON. [Google Scholar]
- Statistics Canada, 2012. Table 105-1101 - Mental Health Profile, Canadian Community Health Survey - Mental Health (CCHS), by Age Group and Sex, Canada and Provinces, Occasional [WWW Document]. CANSIM.
- Taylor S.E., Klein L.C., Lewis B.P., Gruenewald T.L., Gurung R.A.R., Updegraff J.A. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol. 2000;107:411–429. doi: 10.1037/0033-295X.107.3.411. Rev. [DOI] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with Stay-at-Home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtorta N.K., Kanaan M., Gilbody S., Ronzi S., Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrshek-Schallhorn S., Stroud C.B., Mineka S., Hammen C., Zinbarg R.E., Wolitzky-Taylor K., Craske M.G. Chronic and episodic interpersonal stress as statistically unique predictors of depression in two samples of emerging adults. J. Abnorm. Psychol. 2015;124:918–932. doi: 10.1037/abn0000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson, E., Walker, A.J., Bhaskaran, K.J., Bacon, S., Bates, C., Morton, C.E., Curtis, H.J., Mehrkar, A., Evans, D., Inglesby, P., Cockburn, J., Mcdonald, H.I., MacKenna, B., Tomlinson, L., Douglas, I.J., Rentsch, C.T., Mathur, R., Wong, A., Grieve, R., Harrison, D., Forbes, H., Schultze, A., Croker, R.T., Parry, J., Hester, F., Harper, S., Perera, R., Evans, S., Smeeth, L., Goldacre, B., 2020. COVID-19/SARS-CoV-2 news from preprints; OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. medRxiv. DOI: 10.1101/2020.05.06.20092999.
- Woods R., McInnis O., Bedard M., Asokumar A., Santoni S., Anisman H., Matheson K., McQuaid R.J. Social support and unsupportive interactions in relation to depressive symptoms: Implication of gender and the BDNF polymorphism. Soc. Neurosci. 2020;15:64–73. doi: 10.1080/17470919.2019.1650826. [DOI] [PubMed] [Google Scholar]