Abstract
Background
The outbreak of COVID-19 has forced parents to deal with a challenging crisis, which may have increased their stress levels, negatively affecting their parenting and putting their infants at risk of abuse.
Objective
To examine the contribution of the pandemic to parenting stress, exploring differences in parenting stress among new parents before and during the crisis, the role of background and personal variables, and the possibility that the study phase moderated the associations of gender and personal resources with parenting stress.
Method
Israeli parents (n = 1591) whose first child was 3–12 months old were recruited twice through social media: in 2019, before the spread of COVID-19 (n = 985); and in March 2020, during the pandemic (n = 606).
Results
Sociodemographic variables, perception of the childbirth as traumatic, lower meaning in life, higher search for meaning, less marital satisfaction, and study phase all contributed to greater parenting stress. In addition, the association between gender and stress was moderated by study phase, with fathers reporting a greater increase in stress during the pandemic. Moreover, only during the pandemic did fathers report higher parenting stress than mothers.
Conclusions
The findings highlight the vulnerability of new parents of young infants to parenting stress during the crisis, and the special attention which should be paid to fathers. They indicate the value of strengthening meaning in life and preserving good marital relationships as resources that help to cope with the heightened parenting stress at this time.
Keywords: COVID-19, Israel, Parenting stress, Fathers, Mothers, Meaning in life, Marital satisfaction
1. Introduction
The negative effects of parenting stress on the kind of parenting provided, as well as on infant outcomes, has been well documented (Abidin, 1990; Le, Fredman, & Feinberg, 2017; Vondra & Belsky, 1993). More specifically, positive associations have been found between parenting stress and the tendency for child maltreatment (Rodriguez & Green, 1997; Rodriguez & Richardson, 2007; Tiwari, Self-Brown, Lai, McCarty, & Carruth, 2018), emotional regulation difficulties among children (Bradley & Corwyn, 2007), behavioral problems (Crnic, Gaze, & Hoffman, 2005) such as internalizing (anxiety\depression, withdrawal) and externalizing (aggression, delinquency) problem behavior (Liu & Wang, 2015), conduct problems during their adolescence years (Deater‐Deckard, Wang, Chen, & Bell, 2012), and increased risk of child psychopathology (Deater-Deckard, 1998). The adverse effects of parenting stress reported in routine times may be accentuated by external events, such as the current COVID-19 pandemic (Brown, Doom, Lechuga-Peña, Watamura, & Koppels, 2020; Griffith, 2020; Lawson, Piel, & Simon, 2020). Indeed, the crisis has forced families across the world to cope with the psychological implications, including heightened stress, which may negatively impact parenting and consequently put infants’ well-being at greater risk.
1.1. COVID-19 and its effect on stress and mental health
December 2019 officially marks the beginning of what was later labeled the COVID-19 pandemic, the rapid worldwide spread of a virus that has taken millions of lives. The threatening nature of the outbreak has led to an unprecedented global crisis, with countries imposing stringent public health measures to prevent infection, the most extreme being a total lockdown. The continuous newscasts about the spread of COVID-19 arouse fear of the unknown, which in turn raises anxiety levels in healthy individuals, as well as those with preexisting mental health conditions (Shigemura, Ursano, Morganstein, Kurosawa, & Benedek, 2020). The large-scale outbreak of the highly infectious disease has been associated with psychological distress and symptoms of mental illness (Bao, Sun, Meng, Shi, & Lu, 2020). Moreover, the outbreak of the pandemic may heighten the levels of stress for parents, due to various aspects, such as school closures and its economic impact (Cluver et al., 2020).
Studies that have already been published on the potential impact of COVID-19 on mental health suggest that the characteristics of the current situation, including unpredictability, uncertainty, the seriousness of the disease, misinformation, and social isolation, contribute to stress and mental morbidity (Choi, Hui, & Wan, 2020; Gao et al., 2020; Taubman – Ben-Ari, Chasson, Abu-Sharkia, & Weiss, 2020; Wang et al., 2020; Zandifar & Badrfam, 2020). The economic threat of the pandemic has also been shown to lead to lower well-being and higher levels of fear and panic behavior (Shigemura et al., 2020).
Although the literature relating to the current situation is limited, much can be learned from the effect of previous crises on mental health (Kang et al., 2020; Taylor, 2019). When isolation has been imposed as a protective measure in circumstances other than a pandemic, such as terrorist attacks, it has been associated with an increase in mental distress (Fagan, Galea, Ahern, Bonner, & Vlahov, 2003). One of the more vulnerable populations is that of parents (Taubman – Ben-Ari and Ben-Yaakov, 2020), due to increased parenting stress and a lower capacity for tolerance (Cluver et al., 2020). Studies have already found a relationship between COVID-19–related stress and anxiety and adverse maternal and neonatal outcomes (Rashidi Fakari & Simbar, 2020). Thus, whereas the current situation is generally stressful, it is important to relate separately to the unique group of new parents, who are additionally subject to the stress of adjusting to their new role.
1.2. Parenting stress and COVID-19
Since the transition to parenthood is usually perceived to be a natural developmental stage in the human life course (e.g., Erikson, 1963), it may be experienced by most parents as a predictable and positive event. Nevertheless, it involves numerous changes in the lives of the parents, including the need to care for the health and well-being of a helpless infant. The emotional response to these challenges may be manifested as parenting stress, defined as the aversive psychological reaction to the demands of being a parent (Deater-Deckard, 1998). Although it is a natural outcome of the transition to parenthood and the need to adapt quickly to caring for a child (Epifanio, Genna, De Luca, Roccella, & La Grutta, 2015), parenting stress may adversely affect a variety of domains, such as parents’ well-being (Nomaguchi & Milkie, 2017), relationship quality (Berryhill, Soloski, Durtschi, & Adams, 2016), and the parent-child relationship (McQuillan & Bates, 2017). Among the factors that have been associated with the level of parenting stress are the infant’s temperament and behavior (McQuillan & Bates, 2017), the parent's personality and physical and mental health (Huizink et al., 2017; Leigh & Milgrom, 2008), and social structures, background variables, and culture (e.g., socioeconomic status, social class, race, ethnicity, gender; Nomaguchi & Milkie, 2017). According to Abidin (1995), parenting stress may be related to the parent, the child, or the parent-child interaction, and is thus expressed in one or more of the following categories: parental distress, a perception of the child as difficult, and/or a dysfunctional relationship with the child.
Alongside the normal potential to experience parenting stress following the transition to parenthood, new parents are now subject to additional anxieties aroused by the COVID-19 pandemic. As we had data on parenting stress that was collected during the first half of 2019, we decided to collect similar data in April 2020, when COVID-19 was a part of the new Israeli reality, with the whole country in lockdown. At this time in Israel, people were allowed to go no more than 100 m from their home unless absolutely necessary, all non-essential workplaces were closed, all educational institutions ceased to operate, public transportation was restricted, and the international airport was closed. We were thus able to compare parenting stress before and during the pandemic among mothers and fathers whose first-born child was no more than 12 months old.
Prime, Wade, & Browne, 2020 suggest examining the impact of the pandemic by drawing on the family stress model (Conger & Elder, 1994). Originally developed during the Great Farm Crisis of the 1980s, the model holds that when caregivers are faced with increased levels of stress, their mental and emotional resources are drained, making the task of positive leadership in the family highly challenging. This leads to an overreliance on less effective parenting approaches (e.g., harshness or coerciveness), or in the present context, to elevated levels of parenting stress (i.e., higher parental distress, a greater perception of the child as difficult, and/or a more dysfunctional relationship with the child). Prime, Wade, & Browne, 2020 note that in the current situation, severe financial stressors are common, and are coupled with stressors related to both the biomedical and social consequences of COVID-19, including threats to the health of oneself and/or loved ones, reductions in social support outside the home, and changes in work roles and/or routines. Parents have the added burden of meeting all the social and developmental needs of their children due to the closure of childcare centers. This may lead to an acute level of stress that raises serious concerns, as it may be damaging both to the caregivers themselves and to their relationship with the child (Chemtob et al., 2010).
The literature is unclear as to whether mothers and fathers experience different levels of anxiety and stress in the transition to parenthood. Whereas some studies did not find any gender differences (Epifanio et al., 2015), others found that mothers reported higher levels of anxiety and parenting stress than fathers (Hildingsson & Thomas, 2014; Lu, 2006; Matvienko-Sikar, Murphy, & Murphy, 2018).
1.3. Personal resources
Empirical evidence shows that personal resources play an important role in the way people cope with stress (Biggs, Brough, & Drummond, 2017; Lazarus & Folkman, 1984). Moreover, studies indicate that coping strategies for handling stress aroused by difficult life circumstances in general appear to operate in much the same way with respect to reducing parenting stress (Deater-Deckard, 2004). For example, parents of children with disabilities, who tend to exhibit high levels of parenting stress (Cushner-Weinstein et al., 2008; Hussain & Juyal, 2007), have been able to cope with the challenge with the help of personal resources, including positive emotions, active coping, meaning-making strategy (Graungaard, Andersen, & Skov, 2011), optimism, and social support (Peer & Hillman, 2014).
Deater-Deckard (2004) explains that successful coping emerges from a broad and diverse repertoire of strategies used to reduce or eliminate the negative consequences of the stresses of parenting. The more strategies parents have at their disposal, and the more able they are to apply them efficiently and appropriately, the more likely it is that they will cope successfully. Among the personal attributes that have been found to aid in coping are attitudes about the self, others, and the world, and internal and external resources such as intelligence, optimism, social capital, and support from others (Deater-Deckard, 2004).
In the current study, we examined the contribution to the level of parenting stress of the internal resource of meaning in life and the external resource of marital satisfaction.
Meaning in life refers to a person’s entire network of associations, beliefs, goals, conclusions, and perceptions regarding a particular domain (Morse & Steger, 2019), and consists of two dimensions: presence of meaning, and search for meaning (Steger, Frazier, Oishi, & Kaler, 2006). Presence of meaning captures the idea that people have a generally positive set of associations and beliefs, whereas search for meaning relates to their efforts to obtain greater, or qualitatively deeper, meaning than they already experience (Morse & Steger, 2019). Perceiving one’s life to be meaningful is fundamental to well-being and positive mental health in general (Steger, 2012), and to parenting in particular (e.g., Nelson, Kushlev, English, Dunn, & Lyubomirsky, 2013; Nomaguchi & Milkie, 2003; Palkovitz, 2002). In contrast, search for meaning is often linked to undesirable outcomes such as depression (Steger et al., 2006; Steger, Oishi, & Kashdan, 2009), and negatively associated with well-being (Cohen & Cairns, 2012; Park, Park, & Peterson, 2010).
Marital satisfaction, that is, the quality of the relationship that is typically the most significant long-term commitment people take upon themselves in adult life, has comprehensive effects on the individual’s well-being (Proulx, Helms, & Buehler, 2007), life satisfaction, stress levels, and depression (Holt-Lunstad, Birmingham, & Jones, 2008). As the quality of the marital relationship is dynamic, it is likely to change over time, particularly in the wake of childbirth (Keizer & Schenk, 2012), and consequently to impact parenting (Ulbricht et al., 2013). A crisis, particularly one of the magnitude of the COVID-19 pandemic, may pose threats to the marital dyad, with harmful consequences for the parents’ mental health and the child’s well-being (Prime, Wade, & Browne, 2020). In other words, parents’ ability to engage in effective coping, including good communication and mutual problem-solving, in the face of stressful events is crucial for protecting not only the marriage, but the whole family system (Merz, Meuwly, Randall, & Bodenmann, 2014).
1.4. Background variables
In addition to these resources, we explored the role of background variables, including features of the birth and sociodemographic characteristics, which have been found to affect well-being and may therefore contribute to parenting stress. Women who had undergone instrumental delivery, for example, not only described the birth as significantly more distressing and themselves as being more at risk of injury (Rowlands & Redshaw, 2012), but also reported higher somatization and obsessive-compulsive, depressive, and anxiety symptoms than women who had undergone other obstetric procedures (Chen et al., 2017; Clout & Brown, 2015; Dekel et al., 2019). Moreover, rapid labor was found to be directly related to maternal parenting stress at 9 months of infant age (Matvienko-Sikar et al., 2018).
Another relevant characteristic of the birth is its perception as traumatic, which has been significantly and negatively associated with women’s well-being, relationships with their partner and the baby (Ayers, Eagle, & Waring, 2006), and self-identity (Fenech & Thomson, 2014), and positively associated with high levels of depression and anxiety (Dikmen-Yildiz, Ayers, & Phillips, 2017).
Sociodemographic variables may also affect the level of parenting stress. Studies have shown, for instance, that older mothers report more stress than younger mothers (Östberg & Hagekull, 2000), and that parenting stress is higher among parents who have fewer socioeconomic resources (Deater-Deckard, 2004).
1.5. The current study
The current study compared the parenting stress of new parents during the COVID-19 pandemic with the level of stress reported in the previous year, relating to both mothers and fathers. In addition, it investigated the role in parenting stress of a number of personal resources and background variables. In view of the literature, the following hypotheses were formulated.
-
1
New parents will report higher parenting stress during the COVID-19 pandemic than in the preceding period.
-
2
The lower the parents’ perceptions of presence of meaning in life and marital satisfaction, and the higher their search for meaning, the greater parenting stress they will report.
Given the lack of previous research on which to rely, the following questions were examined exploratively:
-
1
Are there differences in parenting stress between mothers and fathers?
-
2
Are circumstances of the birth (type of delivery, perception of the birth as traumatic) related to parenting stress?
-
3
What is the unique and combined contribution of the study variables to new parents’ parenting stress?
-
4
Is the association between gender, meaning in life and marital satisfaction, on the one hand, and parenting stress, on the other, moderated by phase of the study (before or during the pandemic)?
2. Method
2.1. Study design
Following approval of the study protocol by the university's Institutional Review Board, convenience samples of Israeli parents of infants 3–12 months old were recruited in two phases: from August 2018 to May 2019 (for a large-scale research project on new parents); and from April 8 to 13, 2020, in the midst of the COVID-19 pandemic. In both phases, a request to participate was posted on social media groups for parents and was directed specifically at parents whose first child was no more than 12 months old. A link to an electronic version of the questionnaire was provided. The opening page ensured the anonymity and confidentiality of the information and explained that the parent could cease to participate at any stage should they wish to do so. Furthermore, the parents were informed that if they felt any distress during or after completing the questionnaire, they could call or email the researchers, whose contact details were supplied.
2.2. Sampling frame
Participants were considered eligible for the study if they were first-time parents of infants 3–12 months old and indicated that they could complete questionnaires in Hebrew. Response rate was 75 % for both samples, i.e., three-quarters of the parents who opened the questionnaire completed it. The final sample consisted of 1591 parents: 985 (285 fathers and 700 mothers) in the year prior to the pandemic (Phase 1); and 606 parents (137 fathers and 469 mothers) during the pandemic (Phase 2).
2.3. Measures
Parenting Stress Index–Short Form (PSI-SF; Abidin, 1995) was used to measure parenting stress. The scale contains 36-items that assess stress on three dimensions: parenting distress (e.g., "Since I have had a child I can't do things that I love to do"); parent-child dysfunctional interactions (e.g., "Usually I feel that my child does not like me and does not want to be near me"); and perception of the child as a difficult (e.g., "There are several things my child does that bother me very much"). Responses were indicated on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree). A high reliability (Cronbach’s alpha .95) has been found across diverse populations for a total score based on the responses to all three subscales (Reitman, Currier, & Stickle, 2002). In the current sample, Cronbach’s alpha was .92. A total score was therefore calculated for each participant by averaging their responses to all items, with higher scores indicating a higher level of parenting stress.
Meaning in Life Questionnaire (MLQ; Steger et al., 2006), a 10-item instrument, was used to assess meaning in life on two dimensions: presence of meaning (5 items; e.g., “My life has a clear sense of purpose”); and search for meaning (5 items; e.g., “I am searching for meaning in my life”). Responses were indicated on a 7-point scale from 1 (absolutely untrue) to 7 (absolutely true). Cronbach’s alpha for the original questionnaire was .88 for presence of meaning and .90 for search for meaning. In the current study, Cronbach’s alpha was .82 for presence of meaning and .89 for search for meaning. Each participant was assigned a score for each dimension equal to the mean of their responses to the relevant items, with higher scores indicating a higher level of that dimension of meaning in life.
Relationship Assessment Scale (RAS; Hendrick, 1988) was used to measure marital satisfaction. The instrument contains 7 items (e.g., "How well does your partner meet your needs?"), with responses marked on a 7-point Likert scale from 1 (strongly disagree) to 7 (strongly agree). Cronbach’s alpha of .86 is reported for the original scale (Hendrick, 1988), and was .89 in the present study. A total score was calculated for each participant by averaging their responses to all items, with higher scores indicating greater satisfaction with the marital relationship.
A sociodemographic questionnaire was used to tap the parents’ background characteristics: age (continuous), education (1= elementary; 2= high school; 3= post high school; 4= academic), physical health (1= poor ; 2= average ; 3= good ; 4= very good), economic status (1= below average; 2= average; 3= above average), marital status (1= single; 2= married; 3= in a couple relationship without marriage; 4= Separated / Divorced), at-risk pregnancy (0 = Low-risk pregnancy; 1 = High-risk pregnancy), type of birth (1= vaginal; 2= C-section; 3= Forceps/Vacuum), and perception of the birth as traumatic (0 = Nontraumatic birth; 1 = Traumatic birth). Parents also indicated the age of their infant (continuous).
2.4. Data analysis
Analyses were conducted using SPSS (ver. 24). First, t-tests were computed to examine differences in the study variables between the two phases. Next, Pearson correlations were computed between the study and background variables and parenting stress. In the third stage of analysis, a six-step hierarchical regression was performed to examine the contribution of the independent variables to parenting stress. In Step 1, the background variables were entered; in Step 2, birth and child characteristics; in Step 3, the internal resources of presence and search for meaning; in Step 4, the external resource of marital satisfaction; in Step 5, study phase; and in Step 6, the interactions between study phase and parent’s gender, internal, and external resources. Finally, PROCESS analysis (Hayes, 2017) was used to identify indirect effects and learn whether the study phase moderated the associations between gender, meaning in life, and marital satisfaction on the one hand, and parenting stress on the other.
3. Results
3.1. Characteristic of study participants
As can be seen from Table 1 , the final sample consisted of 1591 parents. Parent's age ranged from 19 to 50 (M = 30.31, SD = 4.47), and mean infant age was approximately 7 months (M = 7.05, SD = 2.77). Most of the participants (98.5 %) were married or in a spousal relationship; 70 % had an academic degree, and most of the rest had a high school or post-high school diploma; 29.1 % defined their income as average, 30.6 % as above average, and 40.3 % as below average; and 56.7 % defined their health status as very good, 35.1 % as good, and the rest (8.2 %) as poor. In terms of characteristics of the birth, 64.6 % of the parents reported a vaginal birth, 23.3 % a Cesarean section, and the rest (12.1 %) a vacuum extraction. An at-risk pregnancy was indicated by 26.4 % of the parents, and 29.3 % reported experiencing the birth as traumatic.
Table 1.
Background Characteristics of the Participants (n = 1591) in the Whole Sample and by Study Phase.
| Phase 1 (N = 985) |
Phase 2 (N = 606) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | M | SD | t | |
| Parent's age (years) | 30.31 | 4.47 | 29.63 | 4.52 | 31.42 | 4.14 | −8.06*** | |
| Infant's age (months) | 7.05 | 2.77 | 6.84 | 2.84 | 7.40 | 2.61 | −3.97*** | |
| Education | 4.54 | 1.35 | 4.39 | 1.41 | 4.79 | 1.20 | −6.04*** | |
| Physical health | 4.47 | .70 | 4.43 | .74 | 4.53 | .64 | −2.86*** | |
| Economic status | 2.12 | .70 | 2.19 | .64 | 2.07 | .73 | 3.32*** | |
| N | (%) | N | % | N | % | ᵡ2 | ||
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 422 | 26.5 | 285 | 28.9 | 137 | 22.6 | ||
| Female | 1169 | 73.5 | 700 | 71.1 | 469 | 77.4 | ||
| Family status | 7.96 | |||||||
| Single | 9 | 0.6 | 3 | 0.3 | 6 | 1 | ||
| Married | 1413 | 88.8 | 887 | 90.1 | 526 | 86.8 | ||
| In a marital relationship without marriage | 155 | 9.7 | 89 | 9 | 66 | 10.9 | ||
| Separated / Divorce | 14 | 0.9 | 6 | 0.6 | 8 | 1.3 | ||
| At-risk pregnancy | 3.97* | |||||||
| Low-risk pregnancy | 1171 | 73.6 | 742 | 75.3 | 429 | 70.8 | ||
| High-risk pregnancy | 420 | 26.4 | 243 | 24.7 | 177 | 29.2 | ||
| Type of delivery | 9.47* | |||||||
| Vaginal | 1028 | 64.6 | 653 | 66.3 | 375 | 61.9 | ||
| C-section | 345 | 21.7 | 192 | 19.5 | 153 | 25.3 | ||
| Forceps / Vacuum | 218 | 13.7 | 140 | 85.8 | 78 | 12.8 | ||
| Experience of birth | .03 | |||||||
| Nontraumatic birth | 1125 | 70.7 | 695 | 70.6 | 430 | 71 | ||
| Traumatic birth | 466 | 29.3 | 290 | 29.4 | 176 | 29 |
p < .05.
p < .001.
A series of t-tests, performed to examine differences in background variables between the samples (Table 1), indicated that parents in Phase 2 were somewhat older, had a slightly older infant, slightly higher level of education, slightly better physical health, and slightly lower economic status than those in Phase 1. All these variables were controlled for in the regression analysis described below.
3.2. Differences between study variables before and during the COVID-19 pandemic
The means and standard deviations of the study variables by study phase, along with the results of the t-tests, appear in Table 2 . As Table 2 shows, parents reported significantly higher parenting stress, during the pandemic than previously, as predicted in Hypothesis 1. Higher search for meaning in life and marital satisfaction were also reported during the crisis.
Table 2.
Means, Standard Deviations, and t-tests for the Study Variables by Study Phase.
| Phase 1 (n = 985) |
Phase 2 (n = 606) |
||||
|---|---|---|---|---|---|
| M | SD | M | SD | t | |
| Parenting stress | 2.05 | 0.52 | 2.12 | 0.56 | 2.05** |
| Presence of meaning | 5.29 | 1.10 | 5.19 | 1.10 | 1.77 |
| Search for meaning | 4.44 | 1.47 | 4.62 | 1.35 | 2.43** |
| Marital satisfaction | 5.64 | 1.11 | 5.77 | 1.00 | 2.34* |
p < .05.
p< .01.
3.3. Associations between study variables and parenting stress
The results of the Pearson correlations are presented in Table 3 . As can be seen from Table 3, higher level of education and lower physical health were significantly associated with higher parenting stress. In reply to the first research question, fathers reported on higher levels of parenting stress than mothers at phase 2. Finally, in confirmation of Hypothesis 2, lower presence of meaning in life and marital satisfaction, and higher search for meaning were related to higher parenting stress.
Table 3.
Pearson Correlations between Sociodemographic Variables, Personal Resources, and Parenting Stress in the Whole Sample and by Study Phase.
| Variable | Parenting Stress |
||
|---|---|---|---|
| Whole sample (n = 1591) | Phase 1 (n = 985) | Phase 2 (n = 606) | |
| Gendera | −.04 | .03 | −.16*** |
| Age | .01 | −.01 | .09 |
| Education | .06 | .08 | −.05 |
| Physical health | −.24*** | −.26*** | −.23*** |
| Economic status | −.05 | −.06 | −.01 |
| High-risk pregnancyb | .03 | .02 | .05 |
| Vaginal birthc | .08 | .04 | .11 |
| Traumatic birthd | .13*** | .15*** | .11 |
| Infant age | .02 | .02 | .01 |
| Presence of meaning | −.34*** | −.33*** | −.34*** |
| Search for meaning | .14*** | .12*** | .17*** |
| Marital satisfaction | −.33*** | −.37*** | −.28*** |
Note.
0 = Men, 1 = Women.
0 = Low-risk pregnancy, 1 = High-risk pregnancy.
0 = Vaginal birth, 1 = Non-vaginal birth.
0 = Nontraumatic birth, 1 = Traumatic birth.
p<.001.
3.4. Contribution of the study variables to parenting stress
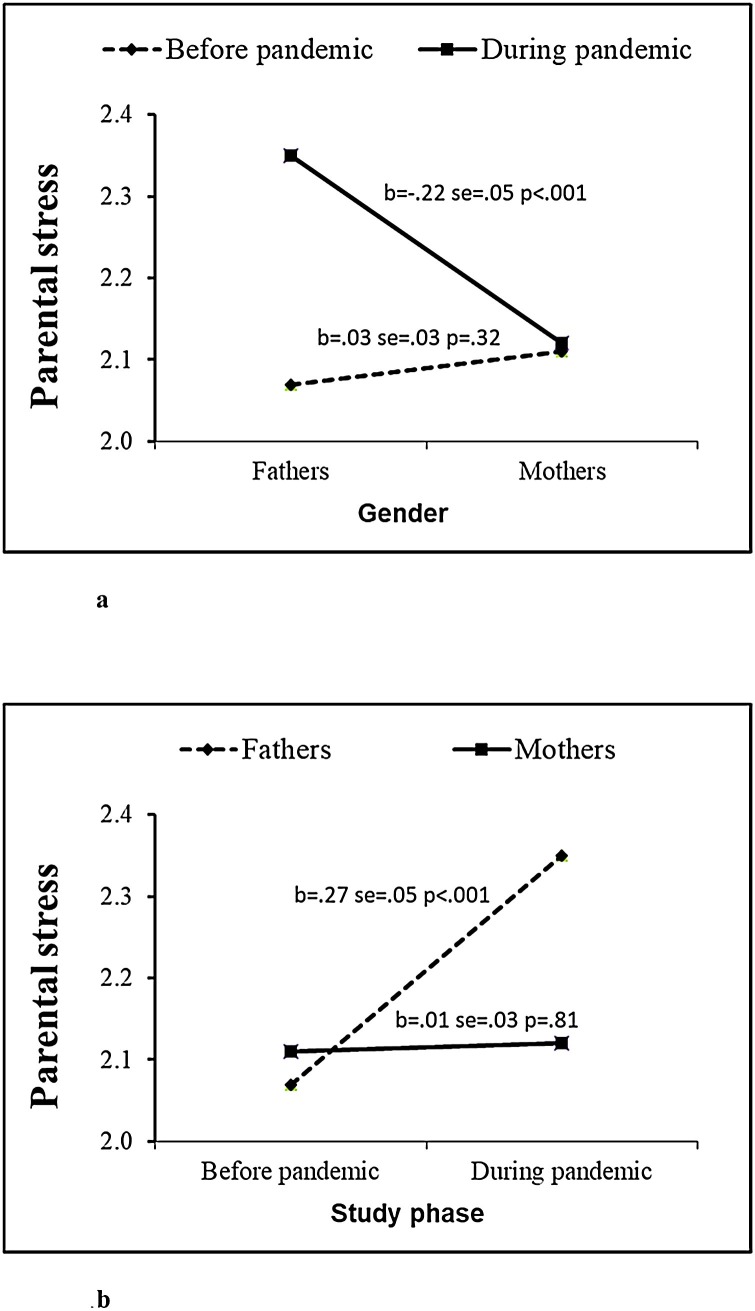
The regression analysis for parenting stress (Table 4 ) revealed that the study variables explained 24.2 % of the variance. The background characteristics in Step 1 contributed a significant 6 % to the explained variance, with higher level of education and lower physical health associated with higher parenting stress. The birth and child characteristics in Step 2 contributed a further 1.5 % to the explained variance, so that parents who perceived the childbirth as more traumatic reported higher parenting stress. The two dimensions of meaning in life in Step 3 added 9.7 % to the explanation of the variance, with both lower presence of meaning and higher search for meaning associated with higher parenting stress. Marital satisfaction in Step 4 accounted for a further 5.5 % of the explained variance, so that lower marital satisfaction was related to higher parenting stress. Study phase in Step 5 contributed an additional 0.5 % to the explained variance, with parents reporting higher stress during the pandemic than prior to it. Finally, only the interaction between gender and study phase in Step 6 was significant, adding another 1 % to the explained variance. Analysis of the source of the interaction (Hayes, 2017), shown in Fig. 1 a,b, revealed that whereas parenting stress was significantly higher among fathers than among mothers during the pandemic (b = −.22, se = .05, p < .001), this gender difference was not found before COVID-19 (b = .03, se = .03, p = .32). In other words, the study phase moderated the association between gender and parenting stress. Interestingly, gender was also found to moderate the association between phase and parenting stress: parenting stress was significantly higher during the pandemic than it was before COVID-19 among fathers (b = .27, se = .05, p < .001), but no such difference was found for mothers (b = .01, se = .03, p = .81).
Table 4.
Hierarchical Regression Coefficients (Beta Weights) for Parenting Stress.
| Parenting stress |
|||
|---|---|---|---|
| ß | t | ΔR2 | |
| Step 1: Background variables | .060*** | ||
| Gendera | −.03 | 1.31 | |
| Parent age | −.02 | 0.69 | |
| Education | .07 | 2.32* | |
| Physical health | −.24 | 8.91*** | |
| Economic status | −.03 | 1.09 | |
| Step 2: Birth and child characteristics | .015*** | ||
| High-risk pregnancyb | .01 | 0.44 | |
| Vaginal birthc | .02 | 0.74 | |
| Traumatic birthd | .12 | 4.30*** | |
| Infant age | .02 | .76 | |
| Step 3: Internal resources | .097*** | ||
| Presence of meaning | −.29 | 11.21*** | |
| Search for meaning | .13 | 5.05*** | |
| Step 4: External Resource | .055*** | ||
| Marital satisfaction | −.25 | 9.76*** | |
| Step 5: Phase | .005* | ||
| Study phasee | .08 | 2.83** | |
| Step 6: Interactions | .010** | ||
| Marital satisfaction X Study phase | .03 | 1.04 | |
| Presence of meaning X Study phase | −.01 | 0.42 | |
| Search for meaning X Study phase | .04 | 1.36 | |
| Gender X Study phase | −.36 | 3.51*** | |
| R2 | 24.2 | ||
| F (17, 1346) | 24.89*** | ||
Note.
0 = Men, 1 = Women.
0 = Low-risk pregnancy, 1 = High-risk pregnancy.
0 = Vaginal birth, 1 = Non-vaginal birth.
0 = Nontraumatic birth, 1 = Traumatic birth.
0 = Phase 1, 1 = Phase 2.
p < .05.
p < .01.
p<.001.
Fig. 1.
a) Effect of the Interaction between Gender and Study Phase on Parenting Stress. b) Effect of the Interaction between Study Phase and Gender on Parenting Stress.
4. Discussion
Research is already showing the negative effects of COVID-19 on global stress, distress, and anxiety (e.g., Bao et al., 2020; Brooks et al., 2020). In addition, recent studies indicate that new parents may experience heightened stress and burnout in the face of the pandemic (Brown, Doom, Lechuga-Peña, Watamura, & Koppels, 2020; Griffith, 2020; Lawson, Piel, & Simon, 2020). This study sought to contribute to this growing body of knowledge by examining the impact of the current crisis on parenting stress in the transition to parenthood, comparing the experience of new parents during the pandemic with that of new parents before the outbreak of the virus.
As predicted, parents reported significantly, though mildly, higher parenting stress during the pandemic than in the period preceding it. Although the difference was significant, it was not as substantial as we expected. A deeper examination revealed that this finding was true for fathers but not for mothers. Thus, whereas fathers reported significantly higher parenting stress during the pandemic than in the year before the outbreak of COVID-19, this difference was not significant for mothers, who displayed a similar level of parenting stress before and during the pandemic. The finding of generally heightened stress is in line with previous studies indicating the negative consequences of crisis events on parenting (Conger & Elder, 1994). However, to the best of our knowledge, this is the first study to show differences in parenting stress before and during the spread of COVID-19, thereby shedding light on the potential ramifications of the current crisis for new parenthood, especially among men. The results suggest that the difficult circumstances of this period, which include lack of clarity, social and physical isolation, economic concerns, and health issues, also have implications for the parenting stress of new parents, who are facing this significant change in their lives in the shadow of a threatening and unstable reality.
Similar to the results of previous studies (Epifanio et al., 2015), gender did not contribute directly to parenting stress in the sample as a whole. Unlike other studies, however, mothers did not report higher levels of anxiety and parenting stress than fathers (Hildingsson & Thomas, 2014). On the contrary, in the current study, the associations between gender and parenting stress were different in the two study phases, so that whereas no gender differences were apparent in the period which preceded the crisis, fathers reported higher parenting stress than mothers during the pandemic. The explanation may lie in the change in routine imposed by the lockdown. While most mothers in Israel take three to six months of maternity leave and are therefore accustomed to intensive childcare, fathers usually return to work immediately after the birth. As they spend less time at home, they are less involved in the daily care of the infant. Thus, when fathers were forced to stay home, the intense and unfamiliar interaction with the infant may have aroused cognitive and emotional discomfort and raised stress levels.
Importantly, the parents in Phase 2 of the study reported a higher level of both search for meaning and marital satisfaction. The increase in search for meaning might be interpreted as an attempt to make sense of the pandemic. On the other hand, the higher marital satisfaction might be attributed to the fact that the many challenges of this period triggered the activation of personal resources (Lazarus & Folkman, 1984), including the marital relationship, particularly at a time when both partners were at home due to the lockdown. In other words, exposure to the difficulty that characterizes the transition to parenthood specifically during a general crisis may have made parents more appreciative of their marital resources.
In addition, two parental background variables were found to be related to parenting stress: high level of education and poorer physical health. Previous findings regarding the relationship between education and parenting stress are inconsistent (e.g., Hildingsson & Thomas, 2014; Moh & Magiati, 2012). However, a number of factors may explain why more educated parents are apt to experience greater stress. These include the higher likelihood of a conflict between personal career development and the burden of raising a child (Schieman, Glavin, & Milkie, 2009), and greater difficulty adapting to the parental role (Nomaguchi & Brown, 2011).
The association between poorer health and higher parenting stress is consistent with previous studies (Murphy, Marelich, Armistead, Herbeck, & Payne, 2010; Silver, Bauman, Camacho, & Hudis, 2003). It is logical to assume that parents with health issues will find it more physically and mentally difficult to perform the tasks demanded by their parenting role, causing them to experience greater stress.
The perception of childbirth as traumatic was also associated with higher parenting stress. This is in line with previous studies (Lobel & DeLuca, 2007; Suttora, Spinelli, & Monzani, 2014), and may reflect the fact that the memory of a traumatic experience during childbirth may cause a parent to feel threatened and saddened, consequently making them less mentally available for parenting tasks. This, in turn, may lead to heightened levels of stress.
In addition, the findings highlight the contribution of personal resources to coping with parenting stress. As predicted, and in line with previous studies, presence of meaning was associated with a lower level of parenting stress, whereas search for meaning was associated with higher stress (Steger et al., 2006, 2009). The transition to parenthood is characterized by a multitude of changes in the parent’s life as they adapt to their new role. Parents who feel that their life has a clear and positive meaning may experience these changes as less threatening and as coinciding with their life purpose. In contrast, new parents who sense a lack of meaning in life, that is, those who may be searching for meaning, may feel more overwhelmed and insecure, thereby leading to a higher experience of stress. Previous studies have also shown that search for meaning is linked to negative psychological outcomes, including depression (Steger et al., 2006, 2009), and lower well-being (Cohen & Cairns, 2012; Park et al., 2010).
The finding that higher marital satisfaction was associated with lower parenting stress is similarly consistent with previous findings (Brown, Whiting et al., 2020; Holt-Lunstad et al., 2008). It may be assumed that parents who feel that their relationship with their partner is positive and supportive will experience parenting as less stressful despite the challenges that characterize the first year of parenthood.
This study has a number of limitations that should be noted. First, our aim was to compare parenting stress during the COVID-19 pandemic with the stress reported in a prior period, examining parents at the same stage of parenthood. Although this was the best option for investigating the effect of the crisis, it is obvious that the two samples were not identical. Longitudinal studies following the same participants at various stages of the pandemic and once it is over might shed additional light on its effect on parenting stress and its trajectory over time. Secondly, the study was based on samples recruited only through social networks, and as such tend to include more educated women (see also Jang & Vorderstrasse, 2019), which may limit its generalizability, as they cannot be considered representative. In addition, more women than men agreed to participate in the study, and all of the parents were Israeli. Thirdly, it relies exclusively on self-report measures, which are susceptible to biases, including the shared variance bias. Moreover, in the current study, we did not examine dyads of mothers and fathers from the same family. Further studies might attempt to examine the parental and psychological aspects of the crisis in a sample containing an equal number of mothers and fathers, also those from the same couple dyads if possible, as well as in a more diverse population of parents in terms of culture, sociodemographic variables, and so on, and consider parents with physical health issues and traumatic birth experiences. They may also attempt to corroborate self-reports by cross-validating reports from dyads of spouses.
Despite these limitations, the study contributes to our understanding of the implications of the pandemic for new parents, revealing that the external crisis affected parenting stress in general, and that fathers were particularly vulnerable. Importantly, the finding that parenting stress was higher during the pandemic was affirmed above and beyond all other variables, indicating that the current circumstances are taking a direct toll on new parents, adding to the challenges already inherent in this life transition. Moreover, the results highlight the important role of personal resources in reducing parenting stress, during both routine and crisis times. The study therefore suggests the heightened need for professional interventions for new parents, both mothers and fathers, in an especially stressful period. Such interventions should seek to enhance parents’ resources, including their sense of meaning in life and the quality of their marital relationship, and encourage them to make use of them. In addition, they can offer an opportunity for parents to share their experiences and concerns, and can provide them with information and guidance on emotional and practical coping, as well as on the special challenges of new parenting in the shadow of the pandemic. Moreover, not only research, but also future intervention need to focus on parents with physical health issues and traumatic birth experiences, as these factors were significantly associated with increased level of parenting stress.
References
- Abidin R.R. Pediatric Psychology Press; Charlottesville, VA: 1990. Parenting stress index-short form. [Google Scholar]
- Abidin R.R. Pediatric Psychology Press; 1995. The parenting stress index short form. [DOI] [PubMed] [Google Scholar]
- Ayers S., Eagle A., Waring H. The effects of postnatal PTSD on women and their relationships: A qualitative study. Psychology, Health & Medicine. 2006;11(4):389–398. doi: 10.1080/13548500600708409. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: Address mental health care to empower society. The Lancet. 2020;22(395):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berryhill M.B., Soloski K.L., Durtschi J.A., Adams R.R. Family process: Early child emotionality, parenting stress, and couple relationship quality. Personal Relationships. 2016;23(1):23–41. doi: 10.1111/pere.12109. [DOI] [Google Scholar]
- Biggs A., Brough P., Drummond S. In: The handbook of stress and health. Cooper C., Quick J.C., editors. John Wiley; 2017. Lazarus and Folkman’s psychological stress and coping theory; pp. 349–364. [Google Scholar]
- Bradley R.H., Corwyn R.F. Externalizing problems in fifth grade: Relations with productive activity, maternal sensitivity, and harsh parenting from infancy through middle childhood. Developmental Psychology. 2007;43:1390–1401. doi: 10.1037/0012-1649.43.6.1390. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S.M., Doom J.R., Lechuga-Peña S., Watamura S.E., Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect. 2020;110(Part 2) doi: 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown M., Whiting J., Kahumoku‐Fessler E., Witting A.B., Jensen J. A dyadic model of stress, coping, and marital satisfaction among parents of children with autism. Family Relations. 2020;69(1):138–150. doi: 10.1111/fare.12375. [DOI] [Google Scholar]
- Chemtob C.M., Nomura Y., Rajendran K., Yehuda R., Schwartz D., Abramovitz R. Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior. Child Development. 2010;81(4):1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H.H., Lai J.C.Y., Hwang S.J., Huang N., Chou Y.J., Chien L.Y. Understanding the relationship between cesarean birth and stress, anxiety, and depression after childbirth: A nationwide cohort study. Birth. 2017;44(4):369–376. doi: 10.1111/birt.12295. [DOI] [PubMed] [Google Scholar]
- Choi E.P.H., Hui B.P.H., Wan E.Y.F. Depression and anxiety in Hong Kong during COVID-19. International Journal of Environmental Research and Public Health. 2020;17(10):3740. doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clout D., Brown R. Sociodemographic, pregnancy, obstetric, and postnatal predictors of postpartum stress, anxiety and depression in new mothers. Journal of Affective Disorders. 2015;188:60–67. doi: 10.1016/j.jad.2015.08.054. [DOI] [PubMed] [Google Scholar]
- Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S.…McDonald K. Parenting in a time of COVID-19. The Lancet. 2020;395(10231):e64. doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen K., Cairns D. Is searching for meaning in life associated with reduced subjective well-being? Confirmation and possible moderators. Journal of Happiness Studies. 2012;13(2):313–331. doi: 10.1007/s10902-011-9265-7. [DOI] [Google Scholar]
- Conger R.D., Elder G.H. Jr., editors. Families in troubled times: Adapting to change in rural America. Aldine de Gruyter; 1994. [Google Scholar]
- Crnic K.A., Gaze C., Hoffman C. Cumulative parenting stress across the preschool period: Relations to maternal parenting and child behaviour at age 5. Infant and Child Development. 2005;14(2):117–132. [Google Scholar]
- Cushner-Weinstein S., Dassoulas K., Salpekar J.A., Henderson S.E., Pearl P.L., Gaillard W.D., Weinstein S.L. Parenting stress and childhood epilepsy: The impact of depression, learning, and seizure-related factors. Epilepsy & Behavior. 2008;13(1):109–114. doi: 10.1016/j.yebeh.2008.03.010. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice. 1998;5(3):314–332. doi: 10.1111/j.1468-2850.1998.tb00152.x. [DOI] [Google Scholar]
- Deater-Deckard K. Yale University Press; 2004. Parenting stress. [Google Scholar]
- Deater‐Deckard K., Wang Z., Chen N., Bell M.A. Maternal executive function, harsh parenting, and child conduct problems. Journal of Child Psychology and Psychiatry. 2012;53(10):1084–1091. doi: 10.1111/j.1469-7610.2012.02582.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekel S., Ein-Dor T., Berman Z., Barsoumian I.S., Agarwal S., Pitman R.K. Delivery mode is associated with maternal mental health following childbirth. Archives of Women’s Mental Health. 2019;22(6):817–824. doi: 10.1007/s00737-019-00968-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dikmen-Yildiz P., Ayers S., Phillips L. Factors associated with post-traumatic stress symptoms (PTSS) 4–6 weeks and 6 months after birth: A longitudinal population-based study. Journal of Affective Disorders. 2017;221:238–245. doi: 10.1016/j.jad.2017.06.049. [DOI] [PubMed] [Google Scholar]
- Epifanio M.S., Genna V., De Luca C., Roccella M., La Grutta S. Paternal and maternal transition to parenthood: The risk of postpartum depression and parenting stress. Pediatric Reports. 2015;7(2):5872. doi: 10.4081/pr.2015.5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erikson E.H. 2nd ed. Norton; New York: 1963. Childhood and society. [Google Scholar]
- Fagan J., Galea S., Ahern J., Bonner S., Vlahov D. Relationship of self-reported asthma severity and urgent health care utilization to psychological sequelae of the September 11, 2001 terrorist attacks on the World Trade Center among New York City area residents. Psychosomatic Medicine. 2003;65(6):993–996. doi: 10.1097/01.psy.0000097334.48556.5f. [DOI] [PubMed] [Google Scholar]
- Fenech G., Thomson G. Tormented by ghosts from their past’: A meta-synthesis to explore the psychosocial implications of a traumatic birth on maternal well-being. Midwifery. 2014;30(2):185–193. doi: 10.1016/j.midw.2013.12.004. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S.…Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graungaard A.H., Andersen J.S., Skov L. When resources get sparse: A longitudinal, qualitative study of emotions, coping and resource-creation when parenting a young child with severe disabilities. Health. 2011;15(2):115–136. doi: 10.1177/1363459309360794. [DOI] [PubMed] [Google Scholar]
- Griffith A.K. Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence. 2020:1–7. doi: 10.1007/s10896-020-00172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Guilford; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hendrick S.S. A generic measure of relationship satisfaction. Journal of Marriage and the Family. 1988;50(1):93–98. doi: 10.2307/352430. [DOI] [Google Scholar]
- Hildingsson I., Thomas J. Parental stress in mothers and fathers one year after birth. Journal of Reproductive and Infant Psychology. 2014;32(1):41–56. doi: 10.1080/02646838.2013.840882. [DOI] [Google Scholar]
- Holt-Lunstad J., Birmingham W., Jones B.Q. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Annals of Behavioral Medicine. 2008;35:239–244. doi: 10.1007/s12160-008-9018-y. [DOI] [PubMed] [Google Scholar]
- Huizink A.C., Menting B., De Moor M.H.M., Verhage M.L., Kunseler F.C., Schuenge C., Oosterman M. From prenatal anxiety to parenting stress: A longitudinal study. Archives of Women’s Mental Health. 2017;20(5):663–672. doi: 10.1007/s00737-017-0746-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain A., Juyal I. Stress appraisal and coping strategies among parents of physically challenged individuals. Journal of the Indian Academy of Applied Psychology. 2007;33(2):179–182. [Google Scholar]
- Jang M., Vorderstrasse A. Socioeconomic status and racial or ethnic differences in participation: Web-based survey. JMIR Research Protocols. 2019;8(4) doi: 10.2196/11865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X.…Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry. 2020;7(3):E14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keizer R., Schenk N. Becoming a parent and relationship satisfaction: A longitudinal dyadic perspective. Journal of Marriage and Family. 2012;74(4):759–773. doi: 10.1111/j.1741-3737.2012.00991.x. [DOI] [Google Scholar]
- Lawson M., Piel M.H., Simon M. Child maltreatment during the CoViD-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse & Neglect. 2020;110(part 2) doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R.S., Folkman S. Springer; 1984. Stress, appraisal, and coping. [Google Scholar]
- Le Y., Fredman S.J., Feinberg M.E. Parenting stress mediates the association between negative affectivity and harsh parenting: A longitudinal dyadic analysis. Journal of Family Psychology. 2017;31(6):679. doi: 10.1037/fam0000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh B., Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. 2008;8:24. doi: 10.1186/1471-244X-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Wang M. Parenting stress and children’s problem behavior in China: The mediating role of parental psychological aggression. Journal of Family Psychology. 2015;29(1):20–28. doi: 10.1037/fam0000047. [DOI] [PubMed] [Google Scholar]
- Lobel M., DeLuca R.S. Psychosocial sequelae of cesarean delivery: Review and analysis of their causes and implications. Social Science & Medicine. 2007;64(11):2272–2284. doi: 10.1016/j.socscimed.2007.02.028. [DOI] [PubMed] [Google Scholar]
- Lu L. The transition to parenthood: Stress, resources, and gender differences in a Chinese society. Journal of Community Psychology. 2006;34(4):471–488. doi: 10.1002/jcop.20110. [DOI] [Google Scholar]
- Matvienko-Sikar K., Murphy G., Murphy M. The role of prenatal, obstetric, and post-partum factors in the parenting stress of mothers and fathers of 9-month old infants. Journal of Psychosomatic Obstetrics & Gynecology. 2018;39(1):47–55. doi: 10.1080/0167482X.2017.1286641. [DOI] [PubMed] [Google Scholar]
- McQuillan M.E., Bates J.E. In: Parental stress and early child development: Adaptive and maladaptive outcomes. Deater-Deckard K., Panneton R., editors. Springer; 2017. Parental stress and child temperament; pp. 75–106. [Google Scholar]
- Merz C.A., Meuwly N., Randall A.K., Bodenmann G. Engaging in dyadic coping: Buffering the impact of everyday stress on prospective relationship satisfaction. Family Science. 2014;5(1):30–37. doi: 10.1080/19424620.2014.927385. [DOI] [Google Scholar]
- Moh T.A., Magiati I. Factors associated with parental stress and satisfaction during the process of diagnosis of children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2012;6(1):293–303. doi: 10.1016/j.rasd.2011.05.011. [DOI] [Google Scholar]
- Morse J.L., Steger M.F. In: Pathways and barriers to the transition to parenthood – Existential concerns regarding fertility, pregnancy, and early parenthood. Taubman – Ben-Ari O., editor. Springer; 2019. Giving birth to meaning: Understanding parenthood through the psychology of meaning in life. [Google Scholar]
- Murphy D.A., Marelich W.D., Armistead L., Herbeck D.M., Payne D.L. Anxiety/stress among mothers living with HIV: Effects on parenting skills and child outcomes. AIDS Care. 2010;22(12):1449–1458. doi: 10.1080/09540121.2010.487085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson S.K., Kushlev K., English T., Dunn E.W., Lyubomirsky S. In defense of parenthood: Children are associated with more joy than misery. Psychological Science. 2013;24(1):3–10. doi: 10.1177/0956797612447798. [DOI] [PubMed] [Google Scholar]
- Nomaguchi K.M., Brown S.L. Parental strains and rewards among mothers: The role of education. Journal of Marriage and Family. 2011;73(3):621–636. doi: 10.1111/j.1741-3737.2011.00835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomaguchi K.M., Milkie M.A. Costs and rewards of children: The effects of becoming a parent on adults’ lives. Journal of Marriage and Family. 2003;65(2):356–374. doi: 10.1111/j.1741-3737.2003.00356.x. [DOI] [Google Scholar]
- Nomaguchi K., Milkie M.A. In: Parental stress and early child development: Adaptive and maladaptive outcomes. Deater-Deckard K., Panneton R., editors. Springer; 2017. Sociological perspectives on parenting stress: How social structure and culture shape parental strain and the well-being of parents and children; pp. 47–73. [Google Scholar]
- Östberg M., Hagekull B. A structural modeling approach to the understanding of parenting stress. Journal of Clinical Child Psychology. 2000;29(4):615–625. doi: 10.1207/S15374424JCCP2904_13. [DOI] [PubMed] [Google Scholar]
- Palkovitz R. In: Handbook of father involvement: Multidisciplinary perspectives. Tamis-LeMonda C.S., Cabrera N., editors. Lawrence Erlbaum; 2002. Involved fathering and child development: Advancing our understanding of good fathering; pp. 119–140. [Google Scholar]
- Park N., Park M., Peterson C. When is the search for meaning related to life satisfaction? Applied Psychology: Health and Well‐Being. 2010;2(1):1–13. doi: 10.1111/j.1758-0854.2009.01024.x. [DOI] [Google Scholar]
- Peer J.W., Hillman S.B. Stress and resilience for parents of children with intellectual and developmental disabilities: A review of key factors and recommendations for practitioners. Journal of Policy and Practice in Intellectual Disabilities. 2014;11(2):92–98. doi: 10.1111/jppi.12072. [DOI] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Proulx C.M., Helms H.M., Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage & Family. 2007;69(3):576–593. doi: 10.1111/j.1741-3737.2007.00393.x. [DOI] [Google Scholar]
- Rashidi Fakari F., Simbar M. Coronavirus pandemic and worries during pregnancy; A letter to the editor. Archives of Academic Emergency Medicine. 2020;8(1):e21. doi: 10.22037/aaem.v8i1.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitman D., Currier R.O., Stickle T.R. A critical evaluation of the Parenting Stress Index—Short Form (PSI-SF) in a Head Start population. Journal of Clinical Child and Adolescent Psychology. 2002;31(3):384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Rodriguez C.M., Green A.J. Parenting stress and anger expression as predictors of child abuse potential. Child abuse & neglect. 1997;21(4):367–377. doi: 10.1016/s0145-2134(96)00177-9. [DOI] [PubMed] [Google Scholar]
- Rodriguez C.M., Richardson M.J. Stress and anger as contextual factors and preexisting cognitive schemas: Predicting parental child maltreatment risk. Child Maltreatment. 2007;12:325–337. doi: 10.1177/1077559507305993. [DOI] [PubMed] [Google Scholar]
- Rowlands I.J., Redshaw M. Mode of birth and women’s psychological and physical wellbeing in the postnatal period. BMC Pregnancy and Childbirth. 2012;12:138. doi: 10.1186/1471-2393-12-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieman S., Glavin P., Milkie M.A. When work interferes with life: Work-nonwork interference and the influence of work-related demands and resources. American Sociological Review. 2009;74(6):966–988. doi: 10.1177/000312240907400606. [DOI] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences. 2020;74(4):281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver E.J., Bauman L.J., Camacho S., Hudis J. Factors associated with psychological distress in urban mothers with late-stage HIV/AIDS. AIDS and Behavior. 2003;7(4):421–431. doi: 10.1023/b:aibe.0000004734.21864.25. [DOI] [PubMed] [Google Scholar]
- Steger M.F. In: The human quest for meaning. 2nd ed. Wong P.T.P., editor. Routledge; 2012. Experiencing meaning in life: Optimal functioning at the nexus of spirituality, psychopathology, and well-being; pp. 165–184. [Google Scholar]
- Steger M.F., Frazier P., Oishi S., Kaler M. The meaning in life questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology. 2006;53(1):80–93. doi: 10.1037/0022-0167.53.1.80. [DOI] [Google Scholar]
- Steger M.F., Oishi S., Kashdan T.B. Meaning in life across the life span: Levels and correlates of meaning in life from emerging adulthood to older adulthood. Journal of Positive Psychology. 2009;4(1):43–52. doi: 10.1080/17439760802303127. [DOI] [Google Scholar]
- Suttora C., Spinelli M., Monzani D. From prematurity to parenting stress: The mediating role of perinatal post-traumatic stress disorder. European Journal of Developmental Psychology. 2014;11(4):478–493. doi: 10.1080/17405629.2013.859574. [DOI] [Google Scholar]
- Taubman – Ben-Ari O., Ben-Yaakov O. American Journal of Orthopsychiatry. 2020. Distress and apprehension among new parents during the COVID-19 Pandemic: The contribution of personal resources; pp. 810–816. 90(6) [DOI] [PubMed] [Google Scholar]
- Taubman – Ben-Ari O., Chasson M., Abu-Sharkia S., Weiss E. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. Journal of Reproductive and Infant Psychology. 2020;38(3):340–348. doi: 10.1080/02646838.2020.1786037. [DOI] [PubMed] [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; Newcastle upon Tyne, UK: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. ISBN 1527541185. [Google Scholar]
- Tiwari A., Self-Brown S., Lai B.S., McCarty C., Carruth L. Effects of an evidence-based parenting program on biobehavioral stress among at-risk mothers for child maltreatment: A pilot study. Social Work in Health Care. 2018;57(3):137–163. doi: 10.1080/00981389.2017.1371096. [DOI] [PubMed] [Google Scholar]
- Ulbricht J.A., Ganiban J.M., Button T.M.M., Feinberg M., Reiss D., Neiderhiser J.M. Marital adjustment as a moderator for genetic and environmental influences on parenting. Journal of Family Psychology. 2013;27(1):42–52. doi: 10.1037/a0031481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vondra J., Belsky J. In: Parenting: An ecological perspective. Luster T., Okagaki L., editors. Lawrence Erlbaum Associates; Hillsdale, NJ: 1993. Developmental origins of parenting: Personality and relationship factors; pp. 1–33. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]