Abstract
Due to the spread of COVID 2019, the Italian government imposed a lockdown on the national territory. Initially, citizens were required to stay at home and not to mix with others outside of their household (Phase 1); eventually, some of these restrictions were lifted (Phase 2). To investigate the impact of lockdown on emotional and binge eating, an online survey was conducted to compare measures of self-reported physical (BMI), psychological (Alexithymia), affective (anxiety, stress, and depression) and social (income, workload) state during Phase 1 and Phase 2. Data from 365 Italian residents showed that increased emotional eating was predicted by higher depression, anxiety, quality of personal relationships, and quality of life, while the increase of bingeing was predicted by higher stress. Moreover, we showed that higher alexithymia scores were associated by increased emotional eating and higher BMI scores were associated with both increased emotional eating and binge eating. Finally, we found that from Phase 1 to Phase 2 binge and emotional eating decreased. These data provide evidence of the negative effects of isolation and lockdown on emotional wellbeing, and, relatedly, on eating behaviour.
Keywords: COVID-19 pandemic, Lockdown, Binge eating, Emotional eating, Negative emotions, BMI
1. Introduction
After China, Italy was the first country in which the COronaVIrus Disease 2019 (COVID-19) pandemic rapidly spread. As a consequence, the Italian government was the first country in Europe to impose a total lockdown in the entire national territory to reduce the spread of infections. From the March 10, 2020 citizens were required to socially isolate themselves and were not allowed to leave their homes except for documented reasons (such as serious health reasons or to shop for necessities). Non-essential activities (e.g. schools, universities, gyms, restaurants, commercial activities, companies, and industries selling or producing non-essential goods) were moved on-line or closed, so most people either worked from home or stopped working (“Cities deserted, families separated and social life on hold in Italy's first day of lockdown,” 2020; “Conte annuncia l'inasprimento delle misure: ‘Italia zona protetta,’” 2020). This dramatic and extraordinary situation was extended until the 4th of May. From that day on, some of the restrictions were lifted: people were allowed to leave their houses once more to visit families and to do physical activity, and some non-essential activities as well as some public parks and gardens re-opened. In the media, these two periods of time have been called respectively Phase 1 and Phase 2 of the lockdown (“Europe is in a new phase of reopening, but it's hardly a return to normal,” 2020; “Fase 2: prove di normalità, runner e bici nei parchi, primi funerali,” 2020).
Even though these restrictions were required to prevent people from being infected, the prolonged lockdown, social isolation, uncertainty, and the potential negative consequences in the near future triggered a variety of psychological problems: for example, results from a survey during COVID-19 epidemic including more than 50.000 Chinese respondents showed that almost 35% of the participants experienced psychological distress (Qiu et al., 2020), while a similar survey on the Italian population during Phase 1 of the lockdown, which collected more than 18,000 answers, reported that 37% of the participants experienced post-traumatic stress symptoms, and around the 20% encountered depression, anxiety or high perceived stress (Rossi et al., 2020). The incidence found in Italy was in line with other studies as confirmed by a meta-analysis published in July 2020 (Salari et al., 2020). In general, the prevalence of stress was 29.6% (5 studies, 9074 participants), the prevalence of anxiety was 31.9% (17 studies, 63,439 participants) and that of depression was 33.7% (14 studies, 44,531 participants) (Salari et al., 2020).
The combination of stress, anxiety, and depression due to this unprecedented situation had an impact also on the eating behaviours. Indeed, the sudden start of the lockdown triggered panic buying and stockpiling of food and daily supplies, as a coping mechanism in reaction to the uncertainty of the duration of the pandemic and to the stress of the incessant news of rising numbers of infected individuals and deaths (Baker et al., 2020; Sim, Chua, Vieta, & Fernandez, 2020). Panic buying and stockpiling lead to a supply shock (Baldwin 2020, but see Benker, 2020 for resilience aspects that some stockpiling represents), quickly emptying supermarkets shelves, and to the temporary unavailability of some food products, which in turn created a more stressful situation (Barua, 2020; Di Renzo, Gualtieri, Pivari, et al., 2020). This scenario, combined with the changes in eating habits and routines, such as a higher percentage of meals cooked and consumed at home (such as pizza and pasta; International Food Council Information, 2020; Statista, 2020a, b), affected individual behaviours: many of them reported having eaten more during the lockdown and having had overall more unhealthy eating habits, such as consuming comfort foods (Robinson et al., 2020; Scarmozzino & Visioli, 2020). Crucially, some of them attributed these changes to higher anxiety (Ammar et al., 2020; Scarmozzino & Visioli, 2020; Scharmer et al., 2020).
Dysfunctional eating habits, such as binge eating and emotional eating have been shown to be predicted by both stress (Freeman & Gil, 2004; Lattimore, 2001; Levine & Marcus, 1997; Michels et al., 2012; Talbot, Maguen, Epel, Metzler, & Neylan, 2013; van Strien, Herman, Anschutz, Engels, & de Weerth, 2012; Wallis & Hetherington, 2004) and negative emotions, such as anxiety and depression (Goossens, Braet, Vlierberghe, & Mels, 2009; Nguyen-Rodriguez, Unger, & Spruijt-Metz, 2009; Rosenbaum & White, 2015; Schulz & Laessle, 2010). Binge eating consists of ingesting a large amount of food in a short amount of time, combined with a sense of lack of control during the episode (American Psychiatric Association, 2013), while emotional eating consists of excessive eating in response to arousal states such as anger, fear, and anxiety (van Strien, Frijters, Bergers, & Defares, 1986). Two factors, in particular, seem to play a primary role in mediating the relationship among stress, anxiety, depression, and dysfunctional eating: body weight status, and the subjects’ ability to correctly perceive and interpret their emotional sensations, distinguishing them from their physical ones, a condition called alexithymia (Sifneos, 1973). Previous literature has shown that people who have overweight are particularly at risk for emotional eating during negative emotional states (Geliebter & Aversa, 2003), and that high trait anxiety is associated with food intake for people living with obesity, but not their lean counterparts (Schneider, Appelhans, Whited, Oleski, & Pagoto, 2010). The relationship between stress and emotional eating has also been shown to be modulated by Body Mass Index (BMI; Nguyen-Rodriguez, Chou, Unger, & Spruijt-Metz, 2008; Tchanturia et al., 2012; Torres & Nowson, 2007). Additionally, alexithymia has been related to higher levels of obesity, emotional eating, and more in general to impulsivity and negative affect (Casagrande, Boncompagni, Forte, Guarino, & Favieri, 2019; Pink, Lee, Price, & Williams, 2019). It has been suggested that higher alexithymia reduces the ability to identify emotional states and to distinguish them from internal signals of hunger and satiety, therefore leading individuals to regulate their emotions through food intake (Pink et al., 2019; Tan & Chow, 2014), increasing their BMI (Casagrande et al., 2019; Tan & Chow, 2014; Taylor, Parker, Bagby, & Bourke, 1996).
Given the literature reviewed so far, the present study aimed at investigating, through an online survey, how COVID-19 lockdown affected emotional eating and binge eating in the Italian residents. In particular, we wanted to analyze the effect of the level of anxiety, stress, and depression on eating habits. Particular attention was given to the social features that characterized the quality of life during the lockdown, such as the changes in workload and type of occupation, the level of social isolation, and the quality of home residency. Moreover, we intended to investigate how these aspects interact with personal characteristics such as BMI and level of alexithymia. Crucially, unlike other studies that focused only on Phase 1 of the lockdown and its effect on individual well-being, we aimed at testing how the difference in the restrictions during Phase 1 and Phase 2 of the lockdown differently affected eating behaviour, to better understand the implication of the lockdown rigidity and provide some tools to guide future lockdown policies. We hypothesized that emotional distress and poor quality of life during lockdown would lead to increased self-reported emotional eating and more frequent binge eating. Furthermore, we expected that the lockdown restrictions would impact more individuals with higher BMI and higher levels of alexithymia. Moreover, we hypothesized that the partial lift of the restrictions during Phase 2 of the lockdown would allow individuals to better cope with negative emotions and therefore to reduce emotional eating and binge eating, compared to Phase 1. To investigate stressors and eating behaviors in the two Phases of the lockdown, we administered the online survey during the second week of Phase 2, and we asked participants to respond to questions about their experiences during the two Phases, i.e. Phase 1, i.e. recalling their experience from the 10th of March until the 3rd of May, and Phase 2, from the 4th of May until the day the questionnaire was filled in.
2. Materials and methods
2.1. Participants
The anonymous online Survey (hosted by Qualtrics XM Platform) was shared via social media from the 14th of May to the May 19, 2020, targeting Italian residents and Italian speakers 18 or more years old. Participants were invited to complete a survey on the changes in eating behaviours during the lockdown. There was no compensation for participating in the study. The study protocol was approved by the Ethics Committee of the University of Padova and was conducted in accordance with the Declaration of Helsinki. All respondents read the written consent form and explicitly agreed to participate before starting the survey.
A total of 635 participants started the survey. From this sample, we excluded 194 participants because they did not complete the survey, 7 because of missed information (five because of missed information about gender), five because of pregnancy, two because they reported having been infected by COVID- 19, and 23 because they spent part or all of the lockdown outside the Italian territory. Moreover, 35 participants were excluded from the main analyses because they reported currently having or having had an eating disorder in the past; we report in the supplementary results the analyses run separately on this sample.
2.2. Measures
The online survey was divided into three parts. In the first part, participants answered questions regarding socio-demographic information (age, gender, education, family income, body weight and height, pregnancy, presence of pathologies, type of occupation before the lockdown, presence of eating disorders or history of eating disorders, COVID-19 infection) and filled in the Toronto Alexithymia Scale (TAS-20; Bressi et al., 1996). The second and the third parts included questions and questionnaires that referred respectively to the first and second Phases of the lockdown. They included questions regarding the present home residence (dimensions of the house, presence of an external space such as a garden or a balcony), the number of people living with the participant (including the type and the quality of the relationships), the Type of Occupation (TO; home working or not-working, desk job, public-facing job, a job in contact with COVID patients), and how occupation changed from the previous Phase (not working anymore, working less, working more or no changes). Also, both parts included the 7-Item Binge-Eating Disorder Screener (BEDS-7, Herman et al., 2016), the subsection of the Dutch Eating Behaviour Questionnaire investigating Emotional Eating (DEBQ; Dakanalis et al., 2013), the Patient Health Questionnaire (PHQ-2; Kroenke, Spitzer, & Williams, 2003), investigating depressive symptoms, the Generalized Anxiety Disorder scale (GAD-2; Kroenke, Spitzer, Williams, Monahan, & Löwe, 2007), and the Perceived Stress Scale (PSS-10; Mondo, Sechi, & Cabras, 2019).
2.3. Questionnaires
The TAS-20 is a self-report scale measuring the general level of alexithymia. Each item is scored from 1 (strongly disagree) to 5 (strongly agree), for a total score of 100. The cut-off for alexithymia is 61 (Bressi et al., 1996). To assess the presence of binge eating during each Phase, we included the 7-Item Binge-Eating Disorder Screener (BEDS-7). Only if participants answered “yes” to the first question, inquiring into having experienced episodes characterized by eating an amount of food definitely larger than most people would eat in the same period of time, and to the second question, describing a sense of lack of control over eating during these episodes, the other 5 questions, which inquired into the features of the binging episodes (as per the description of the binge eating disorder in the DSM-5; American Psychiatric Association, 2013), were presented. The total score ranged from 0 to 5: if one of the first two questions was answered negatively or none of the 5 criteria was selected, the score was 0; if both the first two questions were answered positively, the score was equal to the number of criteria met (Shankman et al., 2018). The DEBQ is a self-report questionnaire that contains 33 items, rated on a 5-point Likert scale (from “never” to “very often”; Dakanalis et al., 2013). In this study, we administered only the “emotional eating” subscale which included 13 items (e.g., “Do you have a desire to eat when you are irritated?“). The PHQ-2 is a two-item screening tool inquiring about the frequency of depressed mood and anhedonia over the previous two weeks. Each item is scored from 0, “not at all”, to 3, “nearly every day”. A PHQ-2 ≥ 3 showed a sensitivity of 83% for major depression (Kroenke et al., 2003). The GAD-2 scale is represented by the first 2 items of the GAD-7 and it describes core anxiety symptoms. Each item is scored from 0, “not at all”, to 3, “nearly every day”, and total scores range from 0 to 6; 3 is considered the cut-off for anxiety disorder (Kroenke et al., 2007). The PSS-10 is a ten-item scale that evaluates thoughts and feelings related to stressful events that occurred one month before. It has six negatively- and four positively-stated items rated on a 5-point Likert scale ranging from 0, “never”, to 4, “very often”. Higher scores indicate higher levels of perceived stress (Mondo et al., 2019). Differing from the validated procedure, for the specific purposes of this study, the DEBQ, the BEDS-7, the PHQ-2, the GAD-2, and the PSS-10 were repeated twice to collect participants’ experiences in the two phases: once to record their current experience and once asking them to recollect their experience one week prior.
2.3.1. Indices
To simplify statistical analyses, we combined some measures into indexes. We computed the BMI dividing the body weight by the square of the body height (World Health Organization, 2018), as a measure of body weight status. We defined Quality of Life (QL) as a measure that combines the quantity and quality of the personal space at home and the family income. It was computed as the standard deviation from the population mean of m2 available per person in the house, to which a unit was added per each number of accesses to an external space (such as a balcony, a garden, or a courtyard), and one more unit was added if the family income was greater than 36.000 euro. We defined Quality of the Relationships (QR) as a measure that combines the quality of the relationships and the relationship type (e.g. parents, partner, friends) that each respondent experienced with the people they were living with. Participants rated how good the relationship with each cohabitant was: 3 “not good all”, −1 “okay”, 1 “quite good”, 3 “very good”. This score was then multiplied by a coefficient depending on the relationship type: 1 for partners, by 0.85 for parents, 0.70 for siblings, 0.55 for friends, 0.4 for relatives, 0.25 for housemates. The relationships scores of multiple cohabitants were then averaged per each respondent. Respondents who were living alone were given a score of 0, equal to having neutral relationships. The Workload (WL) was computed to measure the workload in each Phase, from not employed to working full time, and was rated from 0 to 2. The Changes in Workload (CW) is the measure of how much the workload changed compared to before the lockdown, and it was rated from −1.5 to 0.5, with 0 indicating no change in workload.
2.4. Statistical analyses
Analyses were designed to test our predefined hypotheses that the lockdown rigidity would influence emotional and social well-being and to investigate the effect of these cumulative factors on eating habits. Data were cleaned and analyzed using the software R (Team, 2017). All continuous variables were centered and scaled, and participants who deviated more than 4 standard deviations from the mean of any continuous predictor were removed from the sample (N = 5). The final sample was constituted of 365 participants, having excluded any participant with a current or past eating disorder. A second database that included only participants who had or had had a self-reported eating disorder (N = 35) was created, to conduct separate additional analyses (reported in the supplementary results).
Descriptive analyses on the experimental measures were run using t-tests (stats package; R Core Team, 2017). The DEBQ emotional eating and BEDS-7 scales were investigated through two separate linear mixed models (LMMs) with the same predictors. LMMs were computed using the “lmer” function (lme4 package, Bates, Mächler, Bolker, & Walker, 2015) and explored using the Anova function type 3 of the car package (Fox, Weisberg, & Price, 2019). Predictors consisted of four categories: the lockdown Phase (first or second), personal traits that did not vary with the lockdown, and emotional states and social variables during the two Phases of the lockdown. Personal traits included participants’ BMI and TAS scores. Emotional variables included the GAD, PHQ, and PSS questionnaires scores. Social variables included the aggregated variables QL, QR, OC, WL, and TO. To explore the interaction between personal, emotional, and social characteristics in influencing emotional eating and bingeing in the two Phases of the lockdown, each of these categories was put in interaction with the other categories. To avoid overly complicated and uninterpretable models, interactions between items of the same category were not computed, and only second-level interactions were entered into the models. A random intercept for participant ID was added to account for within-subject measures, and two further intercepts for sex and age were included in the initial models:
~ Phase * (BMI + TAS-20) + Phase * (GAD + PSS + PHQ) + Phase * (QL + QR + WL + CW + TO) + (BMI + TAS-20) * (GAD + PSS + PHQ) + (BMI + TAS-20) * (QL + QR + WL + CW + TO) + (GAD + PSS + PHQ) * (QL + QR + WL + CW + TO) + (1|ID) + (1|Gender) + (1|Age)
To ensure that each random intercept and each personal trait, emotional states, and social predictor measure improved the models' fit, one factor at a time was removed from the model, and the resulting model was compared with the initial one on the basis of the AIC criterion (Bolker et al., 2009), using the “anova” function (lmerTest package, Kuznetsova, Brockhoff, & Christensen, 2017). The random intercept for participant ID was always kept in the models to ensure the correct computation of within-subject measures. Factors that did not significantly improve the model's fit were removed, starting with the ones with the highest p value (indicating the lowest chance that the factor improved the model's fit) and repeating the procedure until all the factors included in the models significantly improved their fit. Post-hoc tests of interactions that included categorical factors were corrected using Benjamini & Hochberg's False Discovery Rate method (Benjamini & Hochberg, 1995), and interactions including continuous factors were analyzed according to Aiken & West's method (Aiken, West, & Reno, 1991). The same procedures were used in the supplementary analysis run on the eating disorders dataset.
3. Results
3.1. Sample characteristics
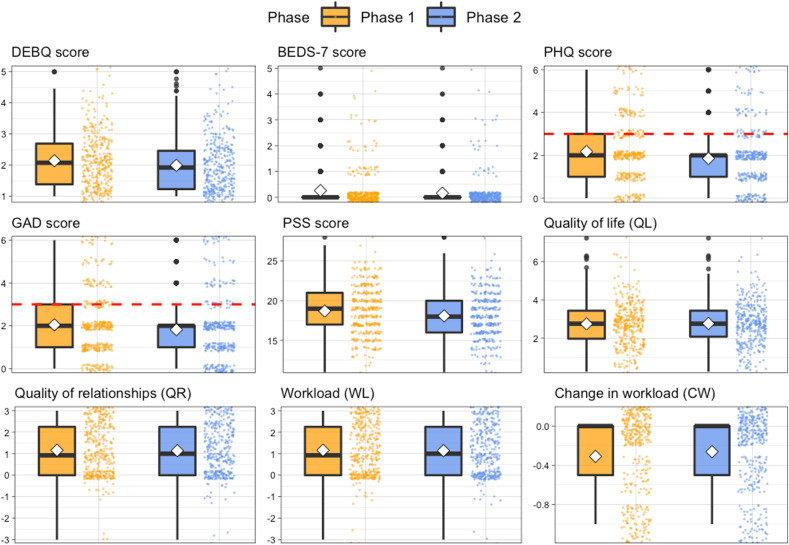
The main sample (n = 365) included only respondents who declared not having a current or past eating disorder. See Table 1 for the mean and standard deviations of demographic and psychological characteristics. Fifty-five participants reported that, before the lockdown, they had a part-time job, 166 that they had a full-time job, 106 reported to be students, and 39 that they were not employed (retired or unemployed). During the lockdown, the type of occupation slightly changed between Phase 1 and 2: in Phase 1, 280 respondents were home working or not working, 50 were employed at a desk job and not working from home, 23 were employed in public-facing jobs and 12 had jobs which put them in contact with COVID patients; in Phase 2, 221 were home working or not working, 96 were employed at a desk job and not working from home, 39 were employed in public-facing jobs and 9 had jobs that put them in contact with COVID patients. For the variables measured in the two Phases, we compared the mean, SD, and cut-off for each Phase; see Table 1 and Fig. 1 for these descriptive results. We then compared our data on emotional eating with the normative data from Dakanalis et al. (2013); (see Table 1) throught t.tests and found that emotional eating was significantly higher than normative data in Phase 1 [t (1282) = 7.85, p < 0.001] but not in Phase 2 [t (1282) = −0.58, p = 0.562]. We also compared the prevalence of binge eating in our data with the normative data (Kessler et al., 2013; see Table 1) and found a significantly higher prevalence of binge eating both in Phase 1 [χ2 (1) = 17.25, p < 0.001] and in Phase 2 [χ2 (1) = 12.67, p < 0.001].
Table 1.
Mean and SD (Standard Deviation) of demographic and psychological variables of the main sample without participants reporting any current or past eating disorder. For PHQ and GAD, the percentages of participants above the cut-off for each Phase are reported.
| Sample | N = 365 | |||
|---|---|---|---|---|
| Gender | 267 women (73.1%) | |||
| Age | mean = 35.09, SD = 13.59 (18–74 years) | |||
| BMI | mean = 23.08, SD = 3.81 (15.05–37.50) | |||
| TAS-20 | mean = 46.21, SD = 11.70 (0–100) | |||
| Phase 1 | Phase 2 | Phase comparisons | ||
| Mean (SD) | Mean (SD) | |||
| DBEQ, Emotional eating+ | 2.14 (0.87) | 1.99 (0.86) | t (364) = 6.49, p < 0.001 | |
|
BEDS-7 % with an episode of binge eating*+ |
0.26 (0.73) | 0.16 (0.63) | t (364) = 3.59, p < 0.001 | |
| 3.01% * | 2.46%* | |||
|
PHQ % above cut-off |
2.18 (1.51) | 1.86 (1.43) | t (364) = 5.86, p < 0.001 | |
| 32% | 22% | |||
|
GAD % above cut-off |
2.04 (1.51) | 1.82 (1.52) | t (364) = 3.97, p < 0.001 | |
| 27% | 20% | |||
| PSS | 18.70 (3.04) | 18.09 (2.89) | t (364) = 3.99, p < 0.001 | |
| QL | 2.74 (1.13) | 2.76 (1.10) | t (364) = −1.51, p = 0.13 | |
| QR | 1.16 (1.20) | 1.14 (1.70) | t (364) = 1.07, p = 0.28 | |
| WL | 1.12 (0.90) | 1.24 (0.82) | t (364) = −5.19, p < 0.001 | |
| CW | −0.31 (0.42) | −0.26 (0.38) | t (364) = −3.97, p < 0.001 | |
Note: BMI = body mass index; TAS-20 = 20 items Toronto Alexithymia Scale; QL = Quality of Life; QR = Quality of the Relationships; WL = Workload; CW = Changes in Workload; * percentage of individuals who had an episode of binge eating, who meet the first two criteria of DSM-V for binge eating disorders, during Phase 1 or Phase 2. +Normative data: mean of emotional eating of 2.00 (sd = 0.84) in a sample of 919 Italian respondents (517 women and 473 men, aged 20–63 M = 34.9, SD = 8.0; Dakanalis et al., 2013); 0.2% of prevalence in Italy in the normal population according to the World Health Organization (WHO) (World Mental Health Surveys; Kessler et al., 2013).
Fig. 1.
Distribution of the questionnaire data during Phase 1 and Phase 2 of the lockdown. The boxplots depict the median and quartile ranges of the distribution; the white diamonds indicate the mean.
3.2. Emotional eating during Phase 1 and Phase 2
The final model investigating the DEBQ emotional eating scale included Phase, BMI, TAS, GAD, PHQ, QL, and QR as predictors, and ID and gender as random intercepts (initial AIC = 1245.4, final AIC = 1215.2, p = 0.10).
~ Phase * (BMI + TAS-20) + Phase * (GAD + PHQ) + Phase * (QL + QR) + (BMI + TAS-20) * (GAD + PHQ) + (BMI + TAS-20) * (QL + QR) + (GAD + PHQ) * (QL + QR) + (1|ID) + (1|Gender)
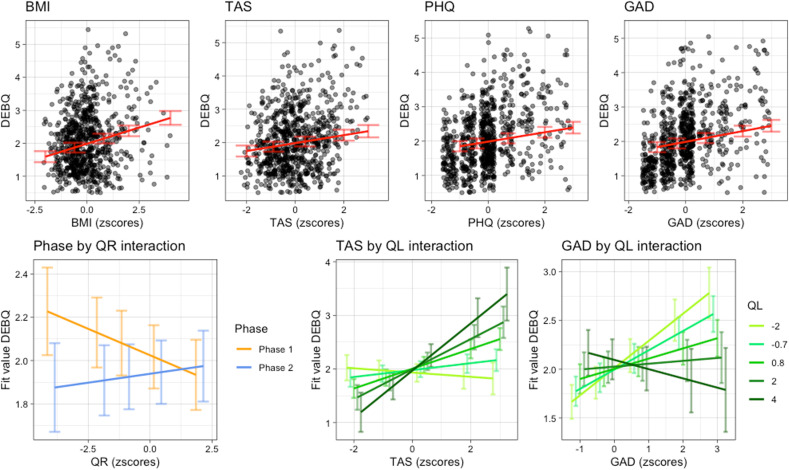
Conditional R2 was equal to 0.88, and marginal R2 was equal to 0.24. Results showed a main effect of Phase [χ2 (1) = 15.53, p < 0.001], illustrating a higher emotional eating during Phase 1 (mean = 2.14, SD = 0.87) than during Phase 2 (mean = 1.99, SD = 0.86). Moreover, higher emotional eating was found among individuals with a higher BMI [χ2 (1) = 23.60, p < 0.001], higher alexithymia score [TAS-20; χ2 (1) = 7.91, p = 0.005], higher anxiety [GAD; χ2 (1) = 20.83, p < 0.001], and higher depressive symptoms [PHQ; χ2 (1) = 21.25, p < 0.001; see Fig. 3]. The model showed a significant Phase by QR interaction [χ2 (1) = 7.34, p = 0.007]. Post-hoc tests found that QR did not predict emotional eating in Phase 1 [t (579) = −1.38, p = 0.17] nor in Phase 2 [t (595) = 0.46, p = 0.65]; however, while in all participants emotional eating was higher in Phase 1 than Phase 2, this difference was bigger among participants with low QR [t (391) = 2.98, p = 0.003] than in participants with a high QR [t (371) = 2.29, p = 0.022]. There was also a significant TAS-20 by QL interaction [χ2 (1) = 4.70, p = 0.030]. Post-hoc showed that among individuals with higher QL, higher alexithymic scores predicted higher emotional eating [t (482) = 3.88, p < 0.001], while alexithymic scores did not have significant effects in individuals with low QL [t (480) = 0.84, p = 0.40]. High and low alexithymic scores did not predict differences in emotional eating depending on the QL [t (552) = 1.79, p = 0.07 and t (523) = −1.23, p = 0.22, respectively]. Finally, there was a significant QL by anxiety interaction [χ2 (1) = 4.26, p = 0.039]. Post-hoc tests showed that QL did not predict emotional eating in individuals with low [t (712) = 1.58, p = 0.11] or high [t (699) = −0.98, p = 0.33] anxiety, but that higher anxiety significantly predicted emotional eating both in individuals with low QL [t (608) = 5.03, p < 0.001] and high QL [t (565) = 1.99, p = 0.047], with a stronger effect among individuals with low QL. All main and interaction effects are depicted in Fig. 2 .
Fig. 3.
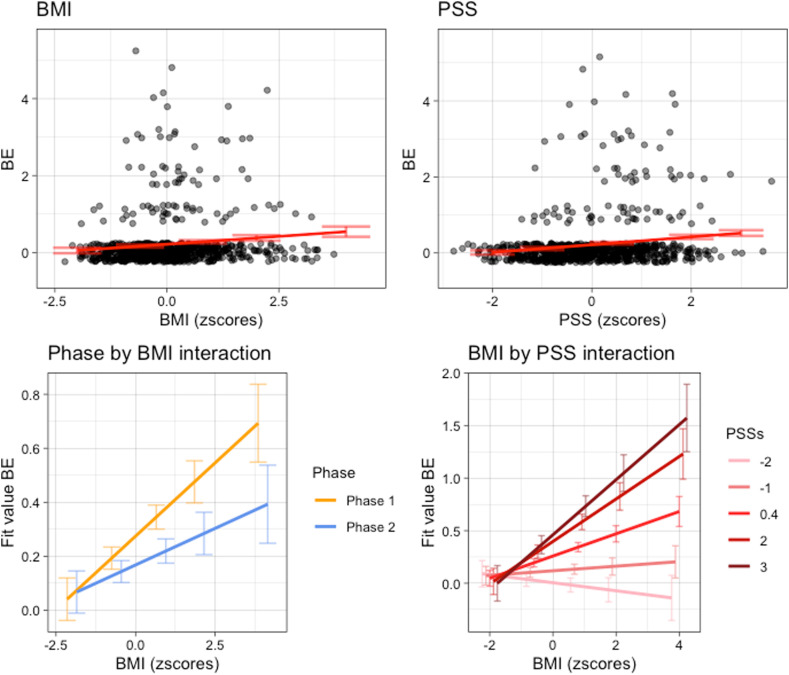
Main and interaction effects between predictors of binge eating. In the first row, the main effects, with data distribution as black dots and fit lines in red. In the second row, fit lines of the interaction effects. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Main and interaction effects between predictors of emotional eating. In the first row, the main effects, with data distribution as black dots and fit lines in red. In the second row, fit lines of the interaction effects. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3.3. Binge eating during Phase 1 and Phase 2
The final model investigating binge eating included Phase, BMI, and PSS as predictors, and ID as random intercept (initial AIC = 1298, final AIC = 1246, p = 0.18).
| ~ Phase × BMI + Phase × PSS + BMI × PSS + (1|ID) |
Conditional R2 was equal to 0.71, and marginal R2 was equal to 0.05. Results showed a main effect of Phase [χ2 (1) = 9.02, p = 0.003], indicating higher binge eating in Phase 1 (mean = 0.26, SD = 0.73) than Phase 2 (mean = 0.16, SD = 0.63), a main effect of BMI [χ2 (1) = 9.67, p = 0.002], indicating higher binge eating among individuals with a higher BMI, and a main effect of PSS [χ2 (1) = 17.87, p < 0.001], indicating higher binge eating in individuals who reported a higher level of stress. There was also a Phase by BMI significant interaction [χ2 (1) = 3.91, p = 0.048]. Post-hoc test showed that higher BMI significantly predicted a higher binge eating in Phase 1 [t (499) = 3.11, p = 0.002], but not in Phase 2 [t (496) = 1.56, p = 0.12; see Fig. 2]. Finally, we found a BMI by stress interaction [χ2 (1) = 7.10, p = 0.008]. Post-hoc tests showed that higher stress lead to a higher binge eating score among individuals with a higher BMI [t (687) = 4.90, p < 0.001], but not among individuals with a lower BMI [t (653) = 1.53, p = 0.13], and that BMI only predicted higher binge eating among individuals with a higher stress score [t (604) = 3.99, p < 0.001], and not among individuals with a lower stress score [t (593) = 1.20, p = 0.23].
4. Discussion
The present study was designed to investigate how the negative emotions raised by the lockdown and the social features that characterized the quality of life during lockdown interacted with individual characteristics to affect the eating behaviour during the lockdown. Our main hypothesis, that emotional distress and poor quality of life during lockdown would lead to increased self-reported emotional eating and more frequent binge eating was confirmed. Indeed increased emotional eating was significantly predicted by higher level of anxiety, depression, and, partially, by Quality of Life and Quality of the Relationships. Moreover, increased binge eating was predicted by higher stress. Our second hypothesis, that the lockdown restrictions would impact more individuals with higher BMI and higher levels of alexithymia, was also confirmed as we showed that higher alexithymia scores were associated by increased emotional eating and higher BMI scores were associated with both increased emotional eating and binge eating. Finally, in line with our third hypothesis, we showed that emotional eating and binge eating decreased significantly in Phase 2 compared to Phase 1.
In line with the literature, we found that emotional eating significantly increased with a higher level of negative emotions, i.e. anxiety (Nguyen-Rodriguez et al., 2009), and depression (Goossens et al., 2009), with higher BMI (Geliebter & Aversa, 2003) and with a higher level of alexithymia (Pink et al., 2019). Moreover, we found that anxiety significantly interacts with the Quality of Life, which was an index of the quantity and quality of the personal space at home and the family income: higher levels of anxiety had stronger effects in those individuals who reported having lower QL. This suggests that lower quality or smaller personal space, the absence of access to external space, or a lower family income made individuals more vulnerable to the negative consequences of anxiety. In developing countries, socioeconomic disadvantage has been strongly correlated with a higher propensity toward obesity (Sobal & Stunkard, 1989; Spinosa, Christiansen, Dickson, Lorenzetti, & Hardman, 2019), in particular, low socioeconomic status seems to affect BMI through increased psychological distress and emotional eating (Spinosa et al., 2019). Additionally, we found a significant effect on emotional eating of the Quality of the Relationships concerning the Phase: individuals who reported a lower QR presented higher emotional eating during Phase 1 as compared to Phase 2. Unsupportive social interactions have been proved to be associated with emotional eating in healthy participants and are considered an effective coping resource to deal with the effects of stressful events (Raspopow, Matheson, Abizaid, & Anisman, 2013). Accordingly, in our data, negatively perceived social interactions influenced emotional eating especially during Phase 1, which was characterized by a higher level of negative emotions. Finally, emotional eating was predicted by the significant interaction between alexithymia and Quality of Life. Unexpectedly, and in contrast with previous explained results, we found that, among individuals with higher QL, higher alexithymic scores predicted higher emotional eating. One possible explanation is that high availability of resources, among which there is probably high availability of good quality food, leads alexithymic individuals, which present difficulties in identifying, describing, and expressing their emotions as well as in recognizing or experiencing emotional bodily responses as emotional feeling states (Lane et al., 1997), to try regulating their bodily emotional responses through eating. It is worth noting that our Quality of Life index was computed based on both income and the space available during the lockdown. Future research should specifically address the effects of each of these factors separately.
The analysis of binge eating revealed that, in line with previous literature (Palmisano, Innamorati, & Vanderlinden, 2016; Torres & Nowson, 2007), higher stress led to higher binge eating score among individuals with a higher BMI, and that BMI predicted higher binge eating among individuals with a higher stress score. A recent meta-analysis reported that living a stressful experience is a risk factor for developing obesity and binge eating disorder (Palmisano et al., 2016). Our data strongly support this association and highlight the necessity for further investigations on the possibility that isolation and lockdown would become a key factor for the development of an eating disorder, in particular in vulnerable individuals (Brown et al., 2020; Fernández-Aranda et al., 2020; Fernández‐Aranda et al., 2020). On the other side, our results on binge eating showed that the final model, that unexpectedly did not include most of the initial factors, explained only a small percentage of the variance, in contrast with the results on emotional eating. This indicates that factors that were not investigated in the study may be involved in binge eating. As binge eating is a clinical disorder, this result may indicate the role of deeper psychological factors, such as trauma, attachment patterns, and significant relationships with caregivers, in the development of an eating disorder (Dominy, Johnson, & Koch, 2000; Harrington, Crowther, Henrickson, & Mickelson, 2006; Maxwell, Tasca, Ritchie, Balfour, & Bissada, 2013; Pace, Cacioppo, & Schimmenti, 2012; Ward, Ramsay, & Treasure, 2000).
Importantly, we found that the partial lift of the restrictions during Phase 2 of the lockdown influenced emotional and binge eating. This result suggests that the loosening of some restrictions helped people to better deal with lockdown. On a more general note, we found that the mean of emotional eating during the lockdown was significanlty higher during Phase 1 compared to the normative data collected in the Italian population (Dakanalis et al., 2013), while our data pointed towards a more consistent increase in the percentage of individuals who presented at least one episode of binge eating during both phases of lockdown compared to the prevalence in Italy in the normal population (Kessler et al., 2013; see Table 1). To our knowledge, this is one of the few reports (see Al-Musharaf, 2020) of emotional eating and binge eating on individuals without eating disorders during the lockdown and, even though more investigations and additional data are needed for comparisons, these data suggest that the negative feelings that individuals had to face during the lockdown may have increased dysfunctional eating behaviour. This is in line with a previous report showing that lockdown leads to an unhealthy pattern of food consumption (e.g. consuming unhealthy food, eating out of control, snacking between meals) and that these changes were exhibited in people from different continents (Ammar et al., 2020; Di Renzo, Gualtieri, Cinelli, et al., 2020; Pietrobelli et al., 2020; Robinson et al., 2020).
As additional analyses, we applied the same models for emotional eating and binge eating on the group of participants that had been excluded from the main analyses because they had reported currently having or having had an eating disorder in the past (see Supplementary Results). Interestingly, even though none of the predictors were linked to binge eating, for emotional eating we found significant predictors that differed from the ones influencing healthy participants. In particular, while alexithymia did not influence emotional eating, stress, in interaction with Quality of Life, was associated with it, and anxiety and depression have only a marginal role. This result indicates that the two groups are indeed samples from different populations that responded differently to stressful situations such as lockdown. However, since it was outside the aim of the present study, this sample was quite small and this analysis must be considered with caution.
This study presents some limitations. First, we relied on social networks to recruit participants, which could have introduced some bias in our sample as it excluded those people that are not on social networks or that could not use personal computers or smartphones. Second, we used an online survey which was based on self-report questionnaires. This aspect could have been particularly problematic for the binge eating questionnaire which was adapted from the structured interview of DSM; however, this procedure was imposed by the exceptionality of the moment and the lockdown restrictions. Third, there was an uneven number of males and female participants; we however tried to account for this issue by including gender as a random factor in the initial models. For the same reason, we also include age in the initial models. Fourth, our sample could be considered small for an online survey; however, we would like to point out that the survey was kept available only for six days to be still able to collect reliable answers related to Phase 1 but at the same time to have people already felt the effects of Phase 2. Five, while our experimental design allowed us to collect information from the same participants for the two phases of the lockdown, it should be noted that data is not acquired longitudinally, but rather participants were asked to recall at the beginning of Phase 2 how they felt a week earlier (during Phase 1). This limitation needs to be carefully considered in particular for the validated instruments (DEBQ, BEDS-7, GAD-2. PSS-10, PHQ-2) that were used following a different procedure from the validated one.
In conclusion, our study shows evidence of the negative effects of isolation and lockdown on eating behaviour in the Italian population. Even though these restrictions were needed to prevent the spread of the pandemic, these and previous observations act as warnings that careful monitoring and nutritional as well as health recommendations are important to mitigate the impact of negative effects of possible future lockdowns. Future policies during lockdown should also take into consideration the emotional toll on individual well-being and should include measures of psychological support. Future studies should consider whether the effects of these two months' lockdown caused long-term consequences on eating behaviour.
Acknowledgment
C.C. was supported by a grant from MIUR (Dipartimenti di Eccellenza DM May 11, 2017 n. 262) to the Department of General Psychology. S.A.O. was supported by the Swiss National Science Foundation (grant PP00P1_170506/1 to Silvio Ionta). We thank Prof. Bruno Osimo for the English revision of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.appet.2021.105122.
Author contributions
M.A., C.C, S.A.O development of the study concept and the study design; C.C, M.A., S.A.O. data collection; S.A.O and C.C data analysis under the supervision of M.A.; S.A.O. and C.C data interpretation and manuscript writing; M.A., C.G., and S.I. review and editing; M.A. and C.G. supervision and project administration. All authors approved the final version of the manuscript.
Conflicts of interest
Authors reported no conflict of interest.
Ethical statement
The study protocol was approved by the Ethics Committee of the University of Padova (Reference n°: 3628) and was conducted in accordance with the Declaration of Helsinki. All respondents read the written consent form and explicitly agreed to participate before starting the survey.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Aiken L.S., West S.G., Reno R.R. Sage; 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- Al-Musharaf S. Prevalence and predictors of emotional eating among healthy young Saudi women during the COVID-19 pandemic. Nutrients. 2020;12(10):2923. doi: 10.3390/nu12102923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. American Psychiatric Association; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders DSM-5. [Google Scholar]
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S.R., Farrokhnia R.A., Meyer S., Pagel M., Yannelis C., Pontiff J. How does household spending respond to an epidemic? Consumption during the 2020 COVID-19 pandemic. The Review of Asset Pricing Studies. 2020;10(4):834–862. [Google Scholar]
- Barua S. Understanding coronanomics: The economic implications of the coronavirus (COVID-19) pandemic. SSRN Electronic Journal. 2020 doi: 10.2139/ssrn.3566477. [DOI] [Google Scholar]
- Bates D., Mächler M., Bolker B., Walker S. Fitting linear mixed-effects models using {lme4} Journal of Statistical Software. 2015;67(1):1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Benjamini Y., Hochberg Y. Controlling the False Discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B. 1995;57(1):289–300. https://www.jstor.org/stable/2346101 [Google Scholar]
- Benker B. Appetite; 2020. Stockpiling as resilience: Defending and contextualising extra food procurement during lockdown. 104981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolker B.M., Brooks M.E., Clark C.J., Geange S.W., Poulsen J.R., Stevens M.H.H., et al. Generalized linear mixed models: A practical guide for ecology and evolution. Trends in Ecology & Evolution. 2009;24(3):127–135. doi: 10.1016/j.tree.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Bressi C., Taylor G., Parker J., Bressi S., Brambilla V., Aguglia E., et al. Cross validation of the factor structure of the 20-item Toronto alexithymia scale: An Italian multicenter study. Journal of Psychosomatic Research. 1996;41(6):551–559. doi: 10.1016/s0022-3999(96)00228-0. [DOI] [PubMed] [Google Scholar]
- Brown S., Opitz M.-C., Peebles A.I., Sharpe H., Duffy F., Newman E. A qualitative exploration of the impact of COVID-19 on individuals with eating disorders in the UK. Appetite. 2020;156 doi: 10.1016/j.appet.2020.104977. 104977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Boncompagni I., Forte G., Guarino A., Favieri F. Emotion and overeating behavior: Effects of alexithymia and emotional regulation on overweight and obesity. Eating and weight disorders-Studies on anorexia. Bulimia and Obesity. 2019;1–13 doi: 10.1007/s40519-019-00767-9. [DOI] [PubMed] [Google Scholar]
- Cities deserted Families separated and social life on hold in Italy's first day of lockdown. 2020. https://edition.cnn.com/2020/03/10/europe/italy-coronavirus-quarantine-europe-intl/index.html Retrieved November 6, 2020, from CNN website:
- Conte annuncia l’inasprimento delle misure “Italia zona protetta.”. 2020. https://www.ansa.it/sito/notizie/cronaca/2020/03/09/borrelli-salgono-a-7985-i-malati-1598-rispetto-a-ieri.-_dd169084-d4a9-4391-9d1c-2d9f42bace3f.html
- Dakanalis A., Zanetti M.A., Clerici M., Madeddu F., Riva G., Caccialanza R. Italian version of the Dutch Eating Behavior Questionnaire. Psychometric proprieties and measurement invariance across sex, BMI-status and age. Appetite. 2013;71:187–195. doi: 10.1016/j.appet.2013.08.010. [DOI] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Cinelli G., Bigioni G., Soldati L., Attinà A., et al. Psychological aspects and eating habits during COVID-19 home confinement: Results of EHLC-COVID-19 Italian Online Survey. Nutrients. 2020;12(7):2152. doi: 10.3390/nu12072152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attinà A., Cinelli G., et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. Journal of Translational Medicine. 2020;18(1):229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominy N.L., Johnson W.B., Koch C. Perception of parental acceptance in women with binge eating disorder. Journal of Psychology. 2000;134(1):23–36. doi: 10.1080/00223980009600846. [DOI] [PubMed] [Google Scholar]
- Europe is in a new phase of reopening But it's hardly a return to normal. 2020. https://edition.cnn.com/2020/05/04/europe/europe-coronavirus-reopening-lockdown-intl/index.html
- Fase 2 Prove di normalità, runner e bici nei parchi, primi funerali. 2020. https://www.ansa.it/sito/notizie/cronaca/2020/05/04/fase-2-milano-e-roma-piu-auto-in-giro-_9f7f5a07-49c4-4dd8-930c-0d6d32ab3c1b.html
- Fernández‐Aranda F., Casas M., Claes L., Bryan D.C., Favaro A., Granero R., et al. COVID‐19 and implications for eating disorders. European Eating Disorders Review. 2020;28(3):239. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J., Weisberg S., Price B. carData: Companion to applied regression data sets. 2019. https://cran.r-project.org/package=carData
- Freeman L.M.Y., Gil K.M. Daily stress, coping, and dietary restraint in binge eating. International Journal of Eating Disorders. 2004;36(2):204–212. doi: 10.1002/eat.20012. [DOI] [PubMed] [Google Scholar]
- Geliebter A., Aversa A. Emotional eating in overweight, normal weight, and underweight individuals. Eating Behaviors. 2003;3(4):341–347. doi: 10.1016/s1471-0153(02)00100-9. [DOI] [PubMed] [Google Scholar]
- Goossens L., Braet C., Vlierberghe L. Van, Mels S. Loss of control over eating in overweight youngsters: The role of anxiety, depression and emotional eating. European Eating Disorders Review. 2009;17(1):68–78. doi: 10.1002/erv.892. [DOI] [PubMed] [Google Scholar]
- Harrington E.F., Crowther J.H., Henrickson H.C.P., Mickelson K.D. The relationships among trauma, stress, ethnicity, and binge eating. Cultural Diversity and Ethnic Minority Psychology. 2006;12(2):212–229. doi: 10.1037/1099-9809.12.2.212. [DOI] [PubMed] [Google Scholar]
- Herman B.K., Deal L.S., DiBenedetti D.B., Nelson L., Fehnel S.E., Brown T.M. Development of the 7-item binge-eating disorder screener (BEDS-7) The Primary Care Companion for CNS Disorders. 2016;18(2) doi: 10.4088/PCC.15m01896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Food Council Information 2020 food and health survey. 2020. https://foodinsight.org/2020-food-and-health-survey/
- Kessler R.C., Berglund P.A., Chiu W.T., Deitz A.C., Hudson J.I., Shahly V., et al. The prevalence and correlates of binge eating disorder in the World health organization World mental health surveys. Biological Psychiatry. 2013;73(9):904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Monahan P.O., Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Kuznetsova A., Brockhoff P.B., Christensen R.H.B. lmerTest package: Tests in linear mixed effects models. Journal of Statistical Software. 2017;82(13) doi: 10.18637/jss.v082.i13. [DOI] [Google Scholar]
- Lattimore P.J. Stress-induced eating: An alternative method for inducing ego-threatening stress. Appetite. 2001;36(2):187–188. doi: 10.1006/appe.2000.0387. [DOI] [PubMed] [Google Scholar]
- Levine M.D., Marcus M.D. Eating behavior following stress in women with and without bulimic symptoms | SpringerLink. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 1997;19(2):132–138. doi: 10.1007/BF02883330. [DOI] [PubMed] [Google Scholar]
- Maxwell H., Tasca G., Ritchie K., Balfour L., Bissada H. Change in attachment insecurity is related to improved outcomes 1-year post group therapy in women with binge eating disorder. Psychotherapy. 2013;51(1):57–65. doi: 10.1037/a0031100. [DOI] [PubMed] [Google Scholar]
- Michels N., Sioen I., Braet C., Eiben G., Hebestreit A., Huybrechts I., et al. Stress, emotional eating behaviour and dietary patterns in children. Appetite. 2012;59(3):762–769. doi: 10.1016/j.appet.2012.08.010. [DOI] [PubMed] [Google Scholar]
- Mondo M., Sechi C., Cabras C. Psychometric evaluation of three versions of the Italian perceived stress scale. Current Psychology. 2019;1–9 [Google Scholar]
- Nguyen-Rodriguez S.T., Chou C.-P., Unger J.B., Spruijt-Metz D. BMI as a moderator of perceived stress and emotional eating in adolescents. Eating Behaviors. 2008;9(2):238–246. doi: 10.1016/j.eatbeh.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Rodriguez S.T., Unger J.B., Spruijt-Metz D. Psychological determinants of emotional eating in adolescence. Eating Disorders. 2009;17(3):211–224. doi: 10.1080/10640260902848543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace U., Cacioppo M., Schimmenti A. The moderating role of father's care on the onset of binge eating symptoms among female late adolescents with insecure attachment. Child Psychiatry and Human Development. 2012;43(2):282–292. doi: 10.1007/s10578-011-0269-7. [DOI] [PubMed] [Google Scholar]
- Palmisano G.L., Innamorati M., Vanderlinden J. Life adverse experiences in relation with obesity and binge eating disorder: A systematic review. Journal of Behavioral Addictions. 2016;5(1):11–31. doi: 10.1556/2006.5.2016.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., et al. Obesity; 2020. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in verona, Italy: A longitudinal study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pink A.E., Lee M., Price M., Williams C. A serial mediation model of the relationship between alexithymia and BMI: The role of negative affect, negative urgency and emotional eating. Appetite. 2019;133:270–278. doi: 10.1016/j.appet.2018.11.014. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raspopow K., Matheson K., Abizaid A., Anisman H. Unsupportive social interactions influence emotional eating behaviors. The role of coping styles as mediators. Appetite. 2013;62:143–149. doi: 10.1016/j.appet.2012.11.031. [DOI] [PubMed] [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., et al. Appetite; 2020. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. 104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum D.L., White K.S. The relation of anxiety, depression, and stress to binge eating behavior. Journal of Health Psychology. 2015;20(6):887–898. doi: 10.1177/1359105315580212. [DOI] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmozzino F., Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9(5):675. doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharmer C., Martinez K., Gorrell S., Reilly E.E., Donahue J.M., Anderson D.A. Eating disorder pathology and compulsive exercise during the COVID‐19 public health emergency: Examining risk associated with COVID‐19 anxiety and intolerance of uncertainty. International Journal of Eating Disorders. 2020;53(12):2049–2054. doi: 10.1002/eat.23395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider K.L., Appelhans B.M., Whited M.C., Oleski J., Pagoto S.L. Trait anxiety, but not trait anger, predisposes obese individuals to emotional eating. Appetite. 2010;55(3):701–706. doi: 10.1016/j.appet.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz S., Laessle R.G. Associations of negative affect and eating behaviour in obese women with and without binge eating disorder. Eating and Weight Disorders - Studies on Anorexia. Bulimia and Obesity. 2010;15(4):e287–e293. doi: 10.1007/BF03325311. [DOI] [PubMed] [Google Scholar]
- Shankman S.A., Funkhouser C.J., Klein D.N., Davila J., Lerner D., Hee D. Reliability and validity of severity dimensions of psychopathology assessed using the Structured Clinical Interview for DSM‐5 (SCID) International Journal of Methods in Psychiatric Research. 2018;27(1) doi: 10.1002/mpr.1590. e1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sifneos P.E. The prevalence of ‘alexithymic’ characteristics in psychosomatic patients. Psychotherapy and Psychosomatics. 1973;22(2–6):255–262. doi: 10.1159/000286529. [DOI] [PubMed] [Google Scholar]
- Sim K., Chua H.C., Vieta E., Fernandez G. The anatomy of panic buying related to the current COVID-19 pandemic. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.113015. 113015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobal J., Stunkard A.J. Socioeconomic status and obesity: A review of the literature. Psychological Bulletin. 1989;105(2):260. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- Spinosa J., Christiansen P., Dickson J.M., Lorenzetti V., Hardman C.A. From socioeconomic disadvantage to obesity: The mediating role of psychological distress and emotional eating. Obesity. 2019;27(4):559–564. doi: 10.1002/oby.22402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statista Percentage growth in sales of food products during the coronavirus (COVID-19) outbreak in Italy between February and March 2020, by category. 2020. https://www.statista.com/statistics/1109965/best-selling-food-products-during-coronavirus-italy/
- Statista Sales value growth of fresh food products during the coronavirus (COVID-19) outbreak in Italy in 2020. 2020. https://www.statista.com/statistics/1111159/fresh-food-products-during-the-coronavirus-outbreak-italy/
- van Strien T., Frijters J., Bergers G.P.a., Defares P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International journal of eating disorders. 1986;5(2):295–315. doi: 10.1002/1098-108X(198602)5:2<295. AID-EAT2260050209>3.0.CO;2-T. [DOI] [Google Scholar]
- van Strien T., Herman C.P., Anschutz D.J., Engels R.C.M.E., de Weerth C. Moderation of distress-induced eating by emotional eating scores. Appetite. 2012;58(1):277–284. doi: 10.1016/j.appet.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Talbot L.S., Maguen S., Epel E.S., Metzler T.J., Neylan T.C. Posttraumatic stress disorder is associated with emotional eating. Journal of Traumatic Stress. 2013;26(4):521–525. doi: 10.1002/jts.21824. [DOI] [PubMed] [Google Scholar]
- Tan C.C., Chow C.M. Stress and emotional eating: The mediating role of eating dysregulation. Personality and Individual Differences. 2014;66:1–4. doi: 10.1016/j.paid.2014.02.033. [DOI] [Google Scholar]
- Taylor G.J., Parker J.D.A., Bagby R.M., Bourke M.P. Relationships between alexithymia and psychological characteristics associated with eating disorders. Journal of Psychosomatic Research. 1996;41(6):561–568. doi: 10.1016/s0022-3999(96)00224-3. [DOI] [PubMed] [Google Scholar]
- Tchanturia K., Davies H., Roberts M., Harrison A., Nakazato M., Schmidt U., et al. Poor cognitive flexibility in eating disorders: Examining the evidence using the Wisconsin card sorting task. PloS One. 2012;7(1) doi: 10.1371/journal.pone.0028331. e28331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team R.C. R: A language and environment for statistical computing. 2017. http://www.r-project.org/ 3.4.3.
- Torres S.J., Nowson C.A. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11):887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Wallis D.J., Hetherington M.M. Stress and eating: The effects of ego-threat and cognitive demand on food intake in restrained and emotional eaters. Appetite. 2004;43(1):39–46. doi: 10.1016/j.appet.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Ward A., Ramsay R., Treasure J. Attachment research in eating disorders. British Journal of Medical Psychology. 2000;73(Pt 1):35–51. doi: 10.1348/000711200160282. [DOI] [PubMed] [Google Scholar]
- World Health Organization Obesity and overweight, Key facts. 2018. http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.