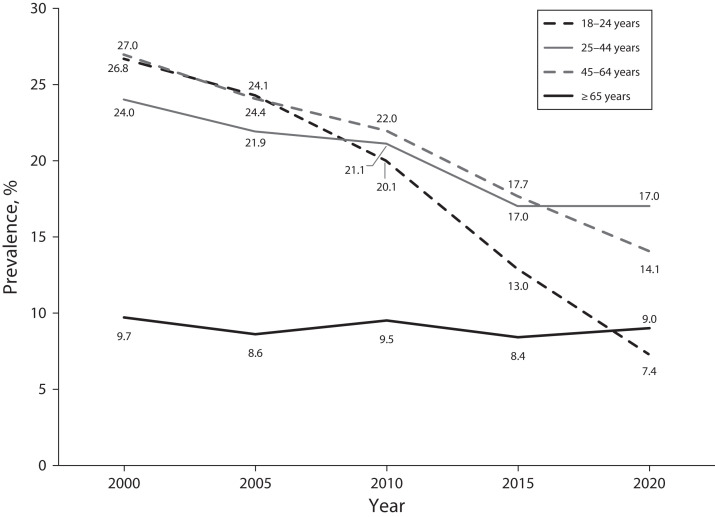
The number of adults aged 65 years and older is expected to more than double worldwide over the next several decades, and for the first time in recorded history, older adults will outnumber children (https://bit.ly/3D4p0im). Despite these unprecedented population shifts, older adults are significantly underrepresented in biomedical research, especially in the field of nicotine and tobacco science (https://bit.ly/3shUSuI). This focus on younger cohorts has obscured the reality that combustible tobacco use (i.e., smoking) has remained virtually unchanged for older adults for nearly two decades in the United States (Figure 1).
FIGURE 1—
Current Cigarette Smoking Among Adults Aged 18 Years and Older, by Age: United States, 2000–2020
Note. The National Health Interview Survey (NHIS) defines current cigarette smokers, represented in the figure, as those who had smoked 100 or more cigarettes in their lifetime and, at the time of the interview, smoked every day or some days.
Source. Data are from the NHIS and are published in Morbidity and Mortality Weekly Reports for each year represented (https://bit.ly/3MT3nWE).
Meanwhile, smoking prevalences among youths and young adults in the United States are at the lowest levels ever recorded. One explanation for these differences in prevalence trajectories could be that, since at least 2005, quit rates among older smokers have remained stagnant (https://bit.ly/3Nax XeF).1 Aligning with this observation is evidence suggesting that traditional tobacco control policies (i.e., pricing, smoke-free policies, information campaigns, bans on advertising, health warning labels, cessation treatments) are not affecting older smokers the same as younger cohorts, as represented in an analysis of smoking behavior in Europe between 2004 and 2013 (https://bit.ly/3VVs2y2). Additionally, older smokers may have less knowledge of quitlines or other local smoking cessation services2,3 and more misconceptions about the relative harms of nicotine and combustible tobacco.2 Older adults are also less likely to use noncombustible nicotine products (https://bit.ly/3z3iZAY).
The lack of attention paid to older smokers does not match the incredible burden of disease and death that this population carries. Tobacco-related disease is age-related disease as evidenced by older smokers incurring 12 times greater health care expenses than middle-aged smokers (https://bit.ly/3eXhLR8).4 As noted by the American Cancer Society, cancers associated with smoking are most often diagnosed after the age of 65 years and include lung, kidney, bladder, and stomach cancer (https://bit.ly/3F7gtxB). Although most people start smoking in the early part of their life, most suffering and deaths associated with tobacco use occur far later. Unfortunately, older adult smokers are not represented in the most basic methodological details of nicotine and tobacco research. For example, in other fields of study, “older adults” are often defined as those who are 65 years and older and may be further delineated as the young old (65–74 years), middle old (75–84 years), and old old (≥ 85 years).5 However, research on tobacco use does not adhere to this definition, with studies defining “older adults” across a wide range of ages (e.g., 25 years or older; https://bit.ly/3TIjwAr). Beyond this, many studies explicitly exclude anyone older than 65 years from participation (https://bit.ly/3VP032T). These inconsistencies in definitions and study inclusion criteria can confound what we know about tobacco use among older adults.
Adding to these disparities is the reality that older smokers face a range of socially and medically complex challenges. In the United States, older smokers are more likely to be American Indian/Alaska Native, Black, or multiracial; to have less than a high school education; and to earn less than $25 000 a year (https://bit.ly/3TpJzfP). The intersection of age and race is notable, particularly when examining smoking cessation behaviors. Older Black men are less likely to stop smoking as they age than are older White men despite starting smoking later in life.6 Older Black smokers are also disproportionately excluded from lung cancer screening guidelines despite this population facing a higher risk of lung cancer.7 Older adults in the United States are less likely to use the Internet for health-related information seeking,8 which may heighten inequalities in health information access. Compounding these health equity issues are the multitude of comorbid health conditions associated with tobacco smoking, that could increase the likelihood of age-related psychosocial and physical health conditions such as chronic pain, dementia, and social isolation or loneliness.
One rarely discussed option for addressing the health of aging smokers is harm reduction. The topic of tobacco harm reduction has become a lightning rod for disagreement because of ongoing concerns that novel nicotine products such as electronic cigarettes (e-cigarettes) could damage the health of nonsmokers, including youths. Although efforts to prevent the uptake of tobacco and nicotine use among young people are critical, they should not supersede a focus on the lives of older smokers. Prioritizing dependence prevention over harm reduction is not ethically justified.9 Like harm reduction approaches for other substance use disorders and geriatric patients facing chronic health conditions, such as obesity, tobacco harm reduction philosophy respects the autonomy and health goals of older adults who might be ambiguous about smoking cessation. Such smokers could benefit from learning that reducing the number of cigarettes smoked can significantly lower their mortality risk (https://bit.ly/3guzMqj) or that the predominant cause of cancer is combustible tobacco, not nicotine.
Although previous research indicates that the public largely does not have a good understanding of harm reduction as it relates to nicotine products (https://bit.ly/3TH4MSV), emerging ethical frameworks cautiously support the adoption of noncombustible nicotine products, such as electronic cigarettes, as a harm reduction alternative to smoking.10 Clinicians working with older adults should consider emphasizing the differential risks associated with smoking compared with noncombustible products (https://bit.ly/3Sr6KFe). Messages can support the cessation of all nicotine and tobacco products while simultaneously providing education about differential product risk and adhering to principles of informed consent and consumer autonomy (https://bit.ly/3Sr6KFe). Furthermore, clinicians working with older adults may wish to develop graphical risk messaging, as people are more likely to accurately perceive tobacco product risk and to share that information with others when risk messaging is graphics-based as opposed to text-based (https://bit.ly/3f2pqgS).
Future work should explore whether this type of risk messaging is effective for older adult smokers. Likewise, clinicians and others providing cessation support to older adults should tailor their messaging to this population, with attention to acknowledging behavioral stage, beliefs about the harms of smoking and benefits of quitting, supporting motivation and self-efficacy, and ensuring adequate and timely social support.11 Clinicians and research teams should be reminded that older adult smokers want to quit smoking and can still experience benefits from cessation (https://bit.ly/3TOgEll).11,12
Efforts to rectify the age-related disparities we have described are imperative and must include strategic approaches for educating and motivating older smokers to reduce or stop their use of smoked tobacco. Older adults are not a homogenous group, and intervention efforts must consider social and environmental factors contributing to their health behaviors. Unfortunately, funding opportunities and public health interventions are rarely tailored to older adults, leaving a significant gap in what we understand about the older smoker’s experience or what interventions best help older adults. Key research gaps include the degree of nicotine dependence among older smokers and its relationship with quitting smoking. In addition, operational definitions used to define smoking history such as the 30 or more pack-years used in lung cancer screening eligibility7 should be evaluated to better understand whether such definitions are perpetuating health inequalities among Black and other minority older adult smokers. Finally, understanding the efficacy and effectiveness of noncombustible nicotine products, such as e-cigarettes, and how they might aid older adults’ smoking cessation attempts is warranted. Certainly, there are challenges to adopting a harm reduction framework, and continued surveillance of the long-term effects of e-cigarettes and other noncombustible tobacco products among older adults is needed.
Older smokers deserve to know that it is never too late to improve their health and that quitting smoking can add years to their lives regardless of age (https://bit.ly/3guzMqj). Future research efforts focused on developing novel, age-tailored interventions are critical for public health, including efforts to address smoking among older people historically marginalized because of age, race, education level, and income. Otherwise, the status quo will continue, and the suffering and early death of millions of older adult smokers will persist.
CONFLICTS OF INTEREST
During the past 36 months, B. A. Kleykamp has received compensation for full-time work from the US Food and Drug Administration–supported public–private partnership ACTTION (https://www.acttion.org) and the American Society of Addiction Medicine (ASAM). B. A. Kleykamp is also the owner of BAK and Associates, a research consulting and science writing firm. Contracts include work for nonprofits, ASAM, the ECRI Institute, the health technology assessment company Hayes, Inc./Symplr, the real-world evidence company STATinMED, the government contractor Palladian Associates, and the health care consulting company PinneyAssociates. The work for PinneyAssociates was completed in 2021 and focused on regulatory submissions related to psychedelic drugs. None of this work was funded by the nicotine or tobacco industries. B. A. Kleykamp has also received honorarium payments totaling US $700 for articles published in Filter (https://filtermag.org/about-the-influence-foundation) and PBS Next Avenue (https://www.nextavenue.org/about-us). J. A. Kulak has no conflicts of interest to declare.
REFERENCES
- 1.Isenberg JY, Quiñones AR, Slatore CG, Bryson WC, Thielke SM. Trends in cigarette smoking and cessation among Medicare managed care recipients, 2005–2012. Addict Behav. 2016;58:155–160. doi: 10.1016/j.addbeh.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 2.Kulak JA, LaValley S. Cigarette use and smoking beliefs among older Americans: findings from a nationally representative survey. J Addict Dis. 2018;37(1–2):46–54. doi: 10.1080/10550887.2018.1521255. [DOI] [PubMed] [Google Scholar]
- 3.Kerr S, Watson H, Tolson D, Lough M, Brown M. Smoking after the age of 65 years: a qualitative exploration of older current and former smokers’ views on smoking, stopping smoking, and smoking cessation resources and services. Health Soc Care Community. 2006;14(6):572–582. doi: 10.1111/j.1365-2524.2006.00659.x. [DOI] [PubMed] [Google Scholar]
- 4.Maciosek MV, Xu X, Butani AL, Pechacek TF. Smoking-attributable medical expenditures by age, sex, and smoking status estimated using a relative risk approach. Prev Med. 2015;77:162–167. doi: 10.1016/j.ypmed.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma M, Branscum PW. Introduction to Community and Public Health. 2nd ed. Hoboken, NJ: Wiley; 2020. [Google Scholar]
- 6.Holford TR, Levy DT, Meza R. Comparison of smoking history patterns among African American and White cohorts in the United States born 1890 to 1990. Nicotine Tob Res. 2016;18(suppl 1):S16–S29. doi: 10.1093/ntr/ntv274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li CC, Matthews AK, Rywant MM, Hallgren E, Shah RC. Racial disparities in eligibility for low-dose computed tomography lung cancer screening among older adults with a history of smoking. Cancer Causes Control. 2019;30(3):235–240. doi: 10.1007/s10552-018-1092-2. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs W, Amuta AO, Jeon KC. Health information seeking in the digital age: An analysis of health information seeking behavior among US adults. Cogent Soc Sci. 2017;3(1):1302785. doi: 10.1080/23311886.2017.1302785. [DOI] [Google Scholar]
- 9.Magalhaes M. Vaping restrictions: is priority to the young justified? Nicotine Tob Res. 2021;23(1):32–35. doi: 10.1093/ntr/ntaa175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franck C, Filion KB, Kimmelman J, Grad R, Eisenberg MJ. Ethical considerations of e-cigarette use for tobacco harm reduction. Respir Res. 2016;17(1):53. doi: 10.1186/s12931-016-0370-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rimer BK, Orleans CT, Fleisher L, et al. Does tailoring matter? The impact of a tailored guide on ratings and short-term smoking-related outcomes for older smokers. Health Educ Res. 1994;9(1):69–84. doi: 10.1093/her/9.1.69. [DOI] [PubMed] [Google Scholar]
- 12.Avila JC, Berg CJ, Robinson J, Ahluwalia JS. Short and long-term cigarette and tobacco abstinence among daily and non-daily older smokers. Nicotine Tob Res. 2022 doi: 10.1093/ntr/ntac116. [DOI] [PMC free article] [PubMed] [Google Scholar]