Abstract
The COVID-19 pandemic has brought not only the risk of infection but also unbearable mental health difficulties with the concern of educational loss among students. This study explored the adverse impact of the COVID-19 outbreak on Bangladeshi students’ mental health and detected potential influencing factors related to post-traumatic stress symptoms (PTSS) and depressive symptoms. Convenience sampling was applied to collect data via online survey from 3997 college and university students between 29th May and 22nd July 2020. PHQ-9 and IES scales were used to assess depressive symptoms and PTSS, respectively. Of all participants, 52.87% had depressive symptoms and 40.91% had PTSS. Severe educational disruption was a risk factor for depressive symptoms (AOR = 1.68; 95% CI: 1.37–2.06) and PTSS (AOR = 1.86; 95% CI: 1.51–2.29). COVID-19 like symptoms including fever, cough, breathing difficulty and fatigue showed a stronger association with higher IES and PHQ-9 scores than other symptoms (e.g., diarrhea, sore throat) (p ≤ 0.01). Fear of infection and death by COVID-19 were risk factors for PTSS and depressive symptoms (p ≤ 0.01). Recreational activity and regular physical exercise emerged as the most protective factors for depressive symptoms and PTSS. The mental health of students is significantly affected in this pandemic suggesting the need for adequate psychological support.
Keywords: COVID-19, Post-traumatic stress symptoms, Depressive symptoms, Students, Mental health, Bangladesh
1. Introduction
Amid an epidemic, the number of individuals whose mental wellbeing is affected tends to be more prominent than the number of individuals influenced by the disease (Reardon, 2015). Currently, the world is devastated by the COVID-19 pandemic. As of 14th December of 2020, there were 70 461,926 confirmed cases leading to 1,599,704 deaths globally (World Health Organization, 2020a). At the same time in Bangladesh, the number of confirmed cases were approximately 490,533 alongside 7,045 deaths (World Health Organization, 2020b). It is well known that stressful events can take a toll on mental wellbeing and can result in conditions such as posttraumatic stress disorder (PTSD) and depression (Kopala-Sibley et al., 2016, Schwartz et al., 2019). The social and economic crisis caused by COVID-19 became so overwhelming and resulted in distress, affective symptoms, post-traumatic stress disorder, and a variety of other negative consequences for young population (Bolton, O'Ryan, Udwin, Boyle, & Yule, 2000). A 2.5–3 fold increase in depression prevalence among university students has been reported in Greece during this COVID-19 pandemic (Kaparounaki et al., 2020).
Stress, anxiety, loneliness and depressive symptoms of university students in Switzerland got worse during COVID-19 outbreak in comparison to pre-COVID period (Elmer, Mepham, & Stadtfeld, 2020). Another study conducted on Spanish university students showed that, 50.3% of the respondents were impacted by the outbreak from moderate to severe level (Odriozola-González, Planchuelo-Gómez, Irurtia, & de Luis-García, 2020). And a study in Italy provided the evidence that confinement due to COVID-19 could have greater impact on students rather than other classes of people in the population (Marelli et al., 2020). In a Chinese study conducted of college students found that final year students, students who lived in the hardest hit areas and who felt incredibly terrified had higher risk for developing PTSD and/depression (Tang et al., 2020). To the best of our knowledge, there is a scarcity of studies in Bangladesh assessing PTSS and its associated factors among students during COVID-19 which indicates a gap in evidence and informed knowledge.
As for Bangladesh, the students were the first group of people to fall under any intervention against COVID-19, then office workers and others. On-campus activities were called off since 18th March 2020 that was followed by a strict lockdown since 26th March 2020 to contain the viral spread. A recent study in Bangladesh during COVID-19 pandemic revealed that college and university students are facing mental health difficulties which includes anxiety (33.3%), depression (46.92%) and event specific distress (69.31%) (Khan et al., 2020). A prior study during COVID-19 in Bangladesh showed that students who engaged themselves in supplementary classes and who were lagging behind in terms of academic activities were anxious and depressed, respectively (Islam et al. 2020) and physical exercise and recreational activities appeared as protective factors for mental health difficulties in previous studies during the COVID-19 pandemic (Islam et al., 2020, Khan et al., 2020). Moreover, longer duration of home-stay may increase anxiety and depression (Sultana et al., 2020b) which warrants the need for exploration of mental health among students who had to confine themselves at home during this pandemic.
Bangladesh has scarcity of evidence on mental health difficulties like post-traumatic stress symptoms and relevant influencing factors during the COVID-19 among students. This study was aimed to explore post-traumatic stress symptoms (PTSS) and depressive symptoms among college and university students in Bangladesh during the COVID-19 outbreak. The present study will add to the existing limited evidence and support researchers in designing and implementing effective psychosocial interventions to deal with mental health difficulties for students when confined at home.
2. Methods
2.1. Participants
Being a college or university student, staying in home for at least 7 days and had been residing in Bangladesh during the outbreak were considered for the eligibility to participate in this study. All confirmed cases of COVID-19 patients were excluded from the study. Participants were from all 8 divisions in Bangladesh.
2.2. Study design & procedure
This cross-sectional study was conducted through an online survey. Convenient sampling technique was used for collecting data. The study was conducted following the Checklist for Reporting Results of Internet ESurveys (CHERRIES) guidelines (Eysenbach, 2004).
This voluntary survey was completed by college and university students from 29th May 2020 to 22nd July 2020. An online questionnaire was developed and disseminated by trained research assistants for data collection via social media (e.g. Facebook). All research assistants were trained by the experts according to the study objectives before starting final data collection. The questionnaire was in native language, Bengali. It was first drafted in Bengali, then translation-back translation process took place from Bengali to English, done by bilingual experts to check the consistencies. An information sheet describing the aim and process, right to refuse their participation from the study was presented on the first page of the survey along with an electronic consent form with it. The questionnaire had sections on sociodemographic information, suspected COVID-19 symptoms, activities during home-stay, COVID-19 related social stressors (CRSS), PHQ-9 scale and Impact of event scale (IES) to assess depressive symptoms and post-traumatic stress symptoms, respectively. A total of 4011 respondents participated in the survey and 3997 respondents were taken for final analysis after discarding incomplete submissions. No financial incentive was provided to the participants and anonymity was maintained to ensure the confidentiality and reliability of data. This study was conducted online in full compliance with the provisions of the Declaration of Helsinki regarding research on human participants. Ethical clearance certificate (Ref No: BBEC, JU/M 2020/COVID-19/(8)1) for this study was obtained from the Institutional Review Board (IRB), “Biosafety, Biosecurity & Ethical Committee” of the Jahangirnagar University.
2.3. Measures
2.3.1. Socio-demographics
Socio-demographic information of the students was obtained through both open and closed ended questions involving their age, gender, religion, educational attainment, study field, current residence, marital status and number of family members.
2.3.2. Suspected COVID-19 symptoms
Suspected COVID-19 symptoms were obtained through questions including concerned symptoms to be answered in “Yes” or “No” options. Concerned physical symptoms were chosen on the basis of closeness towards the symptoms of COVID-19 such as fever, difficulty breathing, dry cough and other symptoms like fatigue, diarrhea and sore throat. The students were also asked if they perceived the symptoms they had as COVID-19 infection.
2.3.3. Activities during home stay and COVID-19 related social stressors (CRSS)
Student activities during this pandemic and COVID-19 related social stressors they perceived to be psychologically uncomfortable were obtained using a checklist for each section. Home-staying activity checklist had options such as online social networking, recreational activity (e.g. watching entertainment shows, playing online and offline games, etc.), physical exercise, educational activity and a scope to mention any other activities apart from the ones mentioned above. CRSS checklist had options such as prolonged homestay, financial uncertainty, disease uncertainty, inadequate food supply, fear of infection, fear of death by COVID-19 and excessive exposure to the news of outbreak and death on media. Additionally, students were also asked to rate how much their study was disrupted in this situation from slight to severe.
2.3.4. Patient health questionnaire (PHQ-9)
Bengali validated version of patient health questionnaire (PHQ-9) (Chowdhury, Ghosh, & Sanyal, 2004), a nine-item depression module which corresponds to DSM-IV Diagnostic Criteria of major depressive symptoms was used in this study to assess depressive symptoms in the participants (Kroenke, Spitzer, & Williams, 2001). Respondents answered on a 4-point Likert scale ranging from “0 = not at all” to “3 = nearly every day” and two weeks recall period was used to measure depression. Total score ranges from 0 to 27 where higher score indicates higher level of depression. Example items include “I feel down, depressed, or hopeless”; “I face trouble falling or staying asleep, or sleeping too much”. The five cut-off points were used for the categorization of depressive symptoms as: i) ‘0–4’ for ‘normal’; ii) ‘5–9’ for ‘mild depressive symptoms’; iii) ‘10–14’ for ‘moderate depressive symptoms’; iv) ‘15–19’ for ‘moderately severe depressive symptoms’; and finally, v) ‘20 or higher’ for ‘severely severe depressive symptoms’. A cut off score ≥ 10 was used to record depressive symptoms in the participants (Anjum, Hossain, Sikder, Uddin, & Rahim, 2019). This scale was previously used and found to have good reliability in Bangladeshi context (Anjum et al., 2019, Hossain et al., 2019). In the present study, the Cronbach's alpha was 0.84.
2.3.5. Impact of event scale
With a focus on the previous two weeks, the post-traumatic stress symptoms (PTSS) were assessed using the Impact of Event scale (IES) (Horowitz, Wilner, & Alvarez, 1979) which is often a broadly utilized substantial and solid scale and gives for a low-cost brief self-report estimation to identify PTSD (Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). The IES contains 15 items that are distributed across two subscales, which assess intrusion (7 items) and avoidance (8 items). The frequency of each item is rated on a 4-point scale: 0 (not at all), 1 (rarely), 3 (sometimes), or 5 (often). The highest possible total score on the IES is 75. Example items include ‘I had trouble falling asleep or staying asleep, because of pictures or thoughts about it that came into my mind’ (intrusion) and 'I stayed away from reminders of it' (avoidance). A cut-off score ≥ 27 was set to denote “PTSS positive”. This cut off score showed 91% sensitivity and 72% specificity with 80% correction rate to detect PTSD (Coffey, Gudmundsdottir, Beck, Palyo, & Miller, 2006). This scale was previously used in China during COVID-19 outbreak (Zhang & Ma, 2020), in Singapore during SARS outbreak (Tham et al., 2005). In this study the Cronbach's alpha was high 0.87.
2.4. Statistical analysis
Descriptive analysis was performed to obtain the characteristics of the participants. Both bivariate and multivariate logistic regression was performed to predict the odds of potential risk factors associated with PTSS and depressive symptoms. Dependent variables were binary in nature and multicollinearity was checked before proceeding with analysis. All examined variables except PTSS were conducted as co-variates for PTSS with respect to performing adjusted estimates. Again, all examined variables except depressive symptoms were performed as co-variates for depressive symptoms to perform adjusted estimates. The estimates of the strengths of associations were demonstrated by Odds ratio (OR and adjusted odds ratio (AOR) with 95% confidence interval (CI). P-value < 0.05 was considered as significant. The STATA version 14.1 (StataCorp LP, College Station, TX, USA) was used to carry out all statistical analysis.
3. Results
3.1. Demographics
Responses came from 3997 students (age range: 15–37 years, with a mean of 21.96 ± 2.56 years) from all 8 divisions of Bangladesh. Respondents were aged mostly 20 to 24 year (70.18%), male (61.10%), unmarried (92.27%), lived in a family of 5 to 7 members (47.16%) and resided in Dhaka division (46.63%) during the outbreak. More than half of the students (53.49%) were from science discipline. Female respondents were 48% more likely to experience depressive symptoms (AOR = 1.48; 95% CI: 1.30–1.70) and 38% more likely to have PTSS (AOR = 1.38; 95% CI: 1.20–1.58). Being unmarried (AOR = 1.30; 95% CI: 1.01–1.68) and living in a family consisting of more than 7 members (AOR = 1.29; 95% CI: 1.04–1.59) were significantly associated with higher odds of depressive symptoms. However, respondents residing outside Dhaka division had lower likelihood to be affected by both depressive symptoms and PTSS. (Table 1 )
Table 1.
Depressive symptoms, PTSS and demographic characteristics students.
| Variables | N (n = 3997) | Depressive symptoms§ |
PTSS§§ |
||
|---|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | ||
| Age (years) | |||||
| ≤19 | 630 (15.76%) | Ref. | Ref. | Ref. | Ref. |
| 20–24 | 2805 (70.18%) | 0.89 (0.75–1.06) | 0.85 (0.66–1.08) | 1.01 (0.85–1.20) | 0.95 (0.74–1.21) |
| ≥25 | 562 (14.06%) | 0.89 (0.71–1.12) | 0.93 (0.69–1.25) | 0.99 (0.79–1.25) | 0.98 (0.73–1.32) |
| Gender | |||||
| Male | 2442 (61.10%) | Ref. | Ref. | Ref. | Ref. |
| Female | 1555 (38.90%) | 1.47** (1.29–1.67) | 1.48** (1.30–1.70) | 1.40** (1.23–1.60) | 1.38**(1.20–1.58) |
| Institute | |||||
| College | 647 (16.19%) | Ref. | Ref. | Ref. | Ref. |
| University | 3350 (83.81%) | 1.00 (0.84–1.18) | 1.02 (0.81–1.30) | 1.09 (0.91–1.29) | 1.03 (0.81–1.31) |
| Study field | |||||
| Science | 2138 (53.49%) | Ref. | Ref. | Ref. | Ref. |
| Business | 987 (24.69%) | 1.93** (1.66–2.26) | 1.82** (1.55–2.13) | 1.81**(1.56–2.11) | 1.68**(1.43–1.97) |
| Arts | 521 (13.03%) | 2.06**(1.69–2.51) | 2.01**(1.64–2.46) | 1.75**(1.44–2.13) | 1.68**(1.38–2.05) |
| Social science | 351 (8.78%) | 2.23**(1.76–2.81) | 2.24**(1.76–2.85) | 1.43**(1.14–1.80) | 1.38**(1.09–1.74) |
| Marital status | |||||
| Unmarried | 3688 (92.27%) | 0.98 (0.77–1.23) | 1.30* (1.01–1.68) | 0.83 (0.66–1.05) | 1.05 (0.81–1.35) |
| Married | 309 (7.73%) | Ref. | Ref. | Ref. | Ref. |
| Number of family members | |||||
| <5 | 1622 (40.58%) | Ref. | Ref. | Ref. | Ref. |
| 5–7 | 1885 (47.16%) | 0.99 (0.86–1.13) | 0.98 (0.86–1.13) | 0.93 (0.81–1.06) | 0.92 (0.80–1.06) |
| >7 | 490 (12.26%) | 1.23* (1.01–1.51) | 1.29* (1.04–1.59) | 1.01 (0.83–1.24) | 1.02 (0.83–1.26) |
| Division | |||||
| Dhaka | 1864 (46.63%) | Ref. | Ref. | Ref. | Ref. |
| Chittagong | 883 (22.09%) | 0.66** (0.56–0.77) | 0.70** (0.59–0.83) | 0.69** (0.59–0.81) | 0.75** (0.63–0.88) |
| Barisal | 159 (3.98%) | 1.39 (0.99–1.96) | 1.41 (0.99–2.00) | 1.23 (0.89–1.70) | 1.24 (0.89–1.71) |
| Mymensingh | 235 (5.88%) | 0.62** (0.47–0.81) | 0.58** (0.44–0.78) | 0.64** (0.49–0.85) | 0.66** (0.49–0.88) |
| Khulna | 224 (5.60%) | 0.74* (0.56–0.98) | 0.86 (0.64–1.14) | 0.52** (0.39–0.70) | 0.59** (0.44–0.80) |
| Rajshahi | 204 (5.10%) | 0.60** (0.45–0.80) | 0.68* (0.50–0.92) | 0.64** (0.48–0.87) | 0.72* (0.53–0.98) |
| Rangpur | 97 (2.43%) | 0.83 (0.55–1.25) | 0.97 (0.64–1.48) | 0.57** (0.37–0.87) | 0.66 (0.42–1.02) |
| Sylhet | 331 (8.28%) | 0.47** (0.37–0.60) | 0.53** (0.41–0.68) | 0.48** (0.37–0.62) | 0.54** (0.42–0.70) |
Abbreviations: OR = Odds ratio; AOR = Adjusted odds ratio; CI = Confidence interval.
P-value < 0.05.
P-value < 0.01.
Depressive symptoms was defined as individuals who scored ≥ 10.
PTSS was defined as individuals who scored ≥ 27.
3.2. Illness & suspected COVID-19 symptoms and their association with depressive symptoms and PTSS
Only 5.43% of the respondents reported to have serious illness or health conditions. However, respondents reported to experience suspected COVID-19 symptoms such as fever (21.97%), sore throat (11.28%), difficulty breathing (5.45%), dry cough (14.24%), fatigue (17.56%) etc. during their home-stay. Respondents having serious illness were 52% more likely to be experience depressive symptoms (AOR = 1.52; 95% CI:1.12–2.06). They had significant association with PTSS as well (OR = 1.35; 95% CI: 1.03–1.78). Respondents having trouble breathing were about two-fold more likely to experience depressive symptoms (AOR = 1.84; 95% CI: 1.33–2.54). Other symptoms experiences were also significantly associated with depressive symptoms or PTSS or both. Additionally, respondents perceiving these symptoms as COVID-19 had higher odds to be affected by depressive symptoms (OR = 1.48; 95% CI: 1.23–1.77) and PTSS (OR = 1.40; 95% CI: 1.18; 95% CI: 1.18–1.68). (Table 2 )
Table 2.
Association of serious illness and experience of suspected COVID-19 symptoms with depressive symptoms and PTSS.
| Variables | N (n = 3997) | Depressive symptoms§ |
PTSS§§ |
||
|---|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | ||
| Serious Illness€ | |||||
| Yes | 217 (5.43%) | 1.94** (1.45–2.59) | 1.52** (1.12–2.06) | 1.35* (1.03–1.78) | 1.18 (0.88–1.56) |
| No | 3780 (94.57%) | Ref. | Ref. | Ref. | Ref. |
| Suspected COVID-19 symptoms | |||||
| Fever | |||||
| Yes | 878 (21.97%) | 1.26** (1.09–1.47) | 0.92 (0.77–1.09) | 1.32** (1.14–1.54) | 1.16 (0.97–1.38) |
| No | 3119 (78.03%) | Ref. | Ref. | Ref. | Ref. |
| Sore throat | |||||
| Yes | 451 (11.28%) | 1.63** (1.33–2.00) | 1.21 (0.97–1.53) | 1.23* (1.01–1.50) | 0.98 (0.78–1.22) |
| No | 3546 (88.72%) | Ref. | Ref. | Ref. | Ref. |
| Difficulty breathing | |||||
| Yes | 218 (5.45%) | 2.51** (1.85–3.42) | 1.84** (1.33–2.54) | 1.60** (1.21–2.10) | 1.31 (0.98–1.76) |
| No | 3779 (94.55%) | Ref. | Ref. | Ref. | Ref. |
| Cough | |||||
| Yes | 569 (14.24%) | 1.55** (1.29–1.86) | 1.24* (1.01–1.52) | 1.26** (1.05–1.50) | 1.04 (0.85–1.27) |
| No | 3428 (85.76%) | Ref. | Ref. | Ref. | Ref. |
| Fatigue | |||||
| Yes | 702 (17.56%) | 1.79** (1.51–2.12) | 1.49** (1.24–1.80) | 1.30** (1.10–1.53) | 1.11 (0.93–1.34) |
| No | 3295 (82.44%) | Ref. | Ref. | Ref. | Ref. |
| Diarrhea | |||||
| Yes | 232 (5.80%) | 1.98** (1.49–2.62) | 1.52** (1.13–2.05) | 1.30 (1.00–1.70) | 1.07 (0.95–1.45) |
| No | 3765 (82.44%) | Ref. | Ref. | Ref. | Ref. |
| Perceived these symptoms as COVID-19 | |||||
| Yes | 585 (14.64%) | 1.48** (1.23–1.77) | 0.97 (0.78–1.21) | 1.40** (1.18–1.68) | 1.17 (0.81–1.42) |
| No | 3412 (85.36%) | Ref. | Ref. | Ref. | Ref. |
Abbreviations: OR = Odds ratio; AOR = Adjusted odds ratio; CI = Confidence interval.
P-value < 0.05.
P-value < 0.01.
Depressive symptoms was defined as individuals who scored ≥ 10.
PTSS was defined as individuals who scored ≥ 27.
Included asthma, diabetes, CVD, etc.
3.3. Home-staying activities and their association with depressive symptoms and PTSS
During home-stay, respondents were involved in various activities such as online social networking (77.43%), recreational activities (45.21%), physical exercises (33.07%), educational activities (57.54%) etc. Respondents who engaged themselves in recreational activities were 21% less likely to experience depressive symptoms (AOR = 0.79; 95% CI: 0.70–0.91). They were also 13% less likely to have PTSS (AOR = 0.87; 95% CI: 0.76–0.99). Similarly, respondents engaged in physical exercises had lower likelihood of being affected by depressive symptoms (AOR = 0.79; 95% CI: 0.68–0.91) and PTSS (AOR = 0.82; 95% CI: 0.71–0.95). However, being involved in educational activities had shown the opposite effect. (Table 3 )
Table 3.
Association of home-staying activities with depressive symptoms and PTSS.
| Variables | N (n = 3997) | Depressive symptoms§ |
PTSS§§ |
||
|---|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | ||
| Online social networking | |||||
| Yes | 3095 (77.43%) | 1.10 (0.94–1.27) | 1.14 (0.97–1.33) | 1.16 (0.99–1.35) | 1.18* (1.01–1.38) |
| No | 902 (22.57%) | Ref. | Ref. | Ref. | Ref. |
| Recreational activities† | |||||
| Yes | 1807 (45.21%) | 0.80** (0.70–0.90) | 0.79** (0.70–0.91) | 0.88 (0.78–1.00) | 0.87* (0.76–0.99) |
| No | 2190 (54.79%) | Ref. | Ref. | Ref. | Ref. |
| Regular Physical exercises | |||||
| Yes | 1322 (33.07%) | 0.79** (0.69–0.90) | 0.79** (0.68–0.91) | 0.84** (0.74–0.97) | 0.82** (0.71–0.95) |
| No | 2675 (66.93%) | Ref. | Ref. | Ref. | Ref. |
| Educational activities¥ | |||||
| Yes | 2300 (57.54%) | 1.18** (1.04–1.34) | 1.19** (1.05–1.35) | 1.29** (1.14–1.47) | 1.31** (1.15–1.49) |
| No | 1697 (42.46%) | Ref. | Ref. | Ref. | Ref. |
| Household chores | |||||
| Yes | 2231 (55.82%) | 1.04 (0.92–1.18) | 1.09 (0.96–1.24) | 1.01 (0.89–1.15) | 1.03 (0.90–1.18) |
| No | 1766 (44.18%) | Ref. | Ref. | Ref. | Ref. |
| Others activities†† | |||||
| Yes | 158 (4.58%) | 0.61** (0.45–0.82) | 0.63** (0.46–0.85) | 0.98 (0.72–1.33) | 1.04 (0.77–1.41) |
| No | 3814 (95.42%) | Ref. | Ref. | Ref. | Ref. |
Abbreviations: OR = Odds ratio; AOR = Adjusted odds ratio; CI = Confidence interval.
P-value < 0.05.
P-value < 0.01.
Depressive symptoms was defined as individuals who scored ≥ 10.
PTSS was defined as individuals who scored ≥ 27.
Educational activities included online class, exams, assignments, thesis.
Recreational activities included TV series, movie, gaming, painting.
Other activities included business, skill development, freelancing etc.
3.4. CRSS, home-stay duration and educational loss and their association with depressive symptoms and PTSS
The majority of the respondents reported financial uncertainty (77.43%) as psychologically stressing. Other reported stressors are prolonged home-stay (68.33%), fear of COVID-19 infection (50.96%), fear of death by COVID-19 (29.32%), inadequate food supply (18.81%), exposure to COVID-19 news (30.77%), etc. Furthermore, almost 60% of the respondents were home-staying for more than 3 months and more than half of the respondents reported to experience moderate to severe educational loss. Respondents reporting financial uncertainty (OR = 1.19; 95% CI:1.05–1.35) and inadequate food supply (OR = 1.31; 95% CI:1.11–1.53) had higher odds for depressive symptoms. Fear of COVID-19 infection was significantly associated with both depressive symptoms and PTSS with higher odds. However, respondents reporting fear of death by COVID-19 were about two times more likely to be affected by depressive symptoms (AOR = 1.86 ;95% CI:1.59–2.17) and PTSS (AOR = 1.96; 95% CI: 1.68–2.29). Respondents those were in home-stay for more than 3 months were also more likely to experience depressive symptoms (OR = 1.16; 95% CI: 1.03–1.31) and PTSS (OR = 1.14; 95% CI: 1.01–1.30). Furthermore, educational loss, from moderate to severe level, was also significantly associated with higher odds of depressive symptoms and PTSS. (Table 4 )
Table 4.
COVID-19 related social stressors (CRSS), duration of home-stay and educational loss.
| Variables | N (n = 3997) | Depressive symptoms§ |
PTSS§§ |
||
|---|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | ||
| Financial uncertainty | |||||
| Yes | 1729 (77.43%) | 1.19** (1.05–1.35) | 1.13 (0.98–1.29) | 1.05 (0.92–1.19) | 0.99 (0.86–1.14) |
| No | 2268 (56.74%) | Ref. | Ref. | Ref. | Ref. |
| Fear of COVID-19 infection | |||||
| Yes | 2037 (50.96%) | 1.18** (1.04–1.34) | 1.04 (0.90–1.19) | 1.55** (1.36–1.76) | 1.39** (1.21–1.61) |
| No | 1960 (49.04%) | Ref. | Ref. | Ref. | Ref. |
| Fear of death (by COVID-19) | |||||
| Yes | 1172 (29.32%) | 1.90** (1.65–2.18) | 1.86** (1.59–2.17) | 2.12** (1.85–2.44) | 1.96** (1.68–2.29) |
| No | 2825 (70.68%) | Ref. | Ref. | Ref. | Ref. |
| Inadequate food supply | |||||
| Yes | 752 (18.81%) | 1.31** (1.11–1.53) | 1.22* (1.02–1.46) | 0.97 (0.82–1.14) | 0.89 (0.74–1.07) |
| No | 3245 (81.19%) | Ref. | Ref. | Ref. | Ref. |
| Disease related uncertainty | |||||
| Yes | 1471 (36.80%) | 1.03 (0.90–1.17) | 0.89 (0.77–1.03) | 1.09 (0.96–1.25) | 0.95 (0.82–1.10) |
| No | 2526 (63.20%) | Ref. | Ref. | Ref. | Ref. |
| Exposure to COVID-19 news on media | |||||
| Yes | 1230 (30.77%) | 1.13 (0.99–1.30) | 0.97 (0.83–1.13) | 1.13 (0.98–1.29) | 0.96 (0.82–1.13) |
| No | 2767 (69.23%) | Ref. | Ref. | Ref. | Ref. |
| Duration of home stay | |||||
| <3 months | 1660 (41.53%) | Ref. | Ref. | Ref. | Ref. |
| >3 months | 2337 (58.47%) | 1.16* (1.03–1.31) | 1.12 (0.99–1.28) | 1.14* (1.01–1.30) | 1.09 (0.96–1.25) |
| Educational Disruption | |||||
| I don’t know | 664 (16.61%) | Ref. | Ref. | Ref. | Ref. |
| Slightly | 555 (13.89%) | 1.05 (0.84–1.32) | 1.06 (0.85–1.34) | 1.15 (0.91–1.45) | 1.14 (0.89–1.44) |
| Moderately | 1243 (31.10%) | 1.19 (0.98–1.43) | 1.26* (1.03–1.52) | 1.40** (1.15–1.71) | 1.41** (1.15–1.72) |
| Severely | 1030 (25.77%) | 1.70** (1.39–2.07) | 1.68** (1.37–2.06) | 1.93** (1.57–2.36) | 1.86** (1.51–2.29) |
| Didn’t hamper | 505 (12.63%) | 1.08 (0.86–1.06) | 1.11 (0.88–1.40) | 0.91 (0.71–1.16) | 0.93 (0.72–1.19) |
Abbreviations: OR = Odds ratio; AOR = Adjusted odds ratio; CI = Confidence interval.
P-value < 0.05.
P-value < 0.01.
Depressive symptoms was defined as individuals who scored ≥ 10.
PTSS was defined as individuals who scored ≥ 27.
4. Discussion
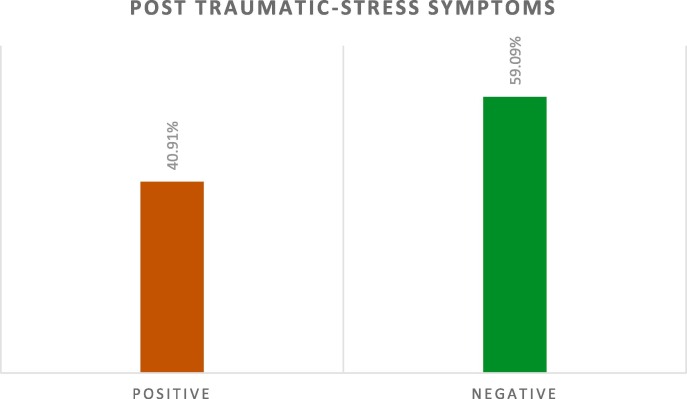
Our findings highlight major psychological challenges faced by college and university students in Bangladesh. Nearly 40.91% of the respondents suffered from PTSS (Fig. 1 ), which is higher than (2.7%) reported in China after one month of COVID-19 outbreak among students (Tang et al., 2020). However, this estimate is much lower than 96.2% among patients during hospital admission with COVID-19 infection (Bo et al., 2020). This higher prevalence of PTSS among students may be attributable to the fact that media led to the exposure to mass trauma (Neria & Sullivan, 2011). In addition to that, losing loved one/family members (Keyes et al. 2014), being a friend or family member of a health-care personnel or a person infected with COVID-19 (Jiang et al. 2020) may be the reason for the elevated prevalence of PTSS among students. However, those are speculative and so it warrants further research in student sample during COVID-19 in Bangladesh.
Fig. 1.
Prevalence of PTSS among participants.
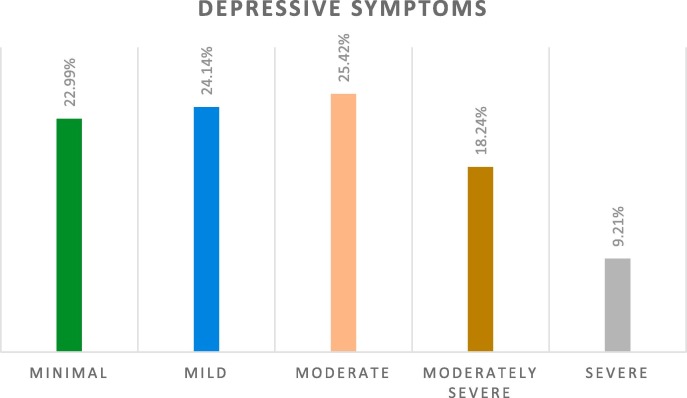
The prevalence estimate of depressive symptoms in the present study is 52.87% (Fig. 2 ). However, recent reports from China (Tang et al., 2020) and Greece (Kaparounaki et al., 2020) showed 9% and 74.3% depression, respectively. This discrepancy may be attributable to different socioeconomic status and developed health care system. However, a recent study showed that uncertainty about the health care system capacity affected mental health (Banna et al., 2020). Concurrently, unmarried individuals were 30% more likely to suffer from depressive symptoms (Table 1) which is in line with a previous study indicating greater psychological impact among singles compared to married population (Rodríguez-Rey, Garrido-Hernansaiz, & Collado, 2020).
Fig. 2.
Distribution of participants by depressive symptoms.
Corresponding to the previous studies, our study showed that being female was associated with a higher risk of developing PTSS and depressive symptoms (González-Sanguino et al., 2020). A recent study during the COVID-19 pandemic revealed violence against women increased during lockdown from 4.4% to 14.8% which was significantly associated with mental health problems like depression (Sediri et al. 2020). This might be a prominent reason for elevated depression and PTSS among women in the present study. In addition to that, women are more financially vulnerable than men during this COVID-19 pandemic and financial loss may increase the likelihood of developing PTSS and depression (Boyraz and Legros, 2020, Sultana et al., 2020a). Apparently, students participating in this study were mostly healthy. Only 5.43% reported to have serious illness like asthma, diabetes, etc. As expected, students with serious health conditions were 52% and 35% more likely to experience depressive symptoms and PTSS (Table 2). This might possibly be the result of being knowledgeable to the fact that people with underlying health conditions are at greater risk of COVID-19 infection (Centers for DIsease Control and Prevention (CDC), 2020). The study indicates lower likelihood of depressive symptoms and PTSS among students those were residing in other divisions apart from Dhaka during lockdown. As of 17th Aug, Dhaka division had the highest attack rate (4147/1,000,000) and other 7 divisions had lower attack rate (410/1,000,000 in Mymensingh division) compared to Dhaka (World Health Organization, 2020c). The lower number of confirmed cases might be the reason for lower likelihood of mental health difficulties in other divisions except from Dhaka. However, it’s worth noting that longer home stay increased the risk for depressive symptoms and PTSS (Table 4). This finding corresponds to a previous study indicating longer confinement is associated with poorer mental condition (Brooks et al., 2020).
Almost two third (70.77%) of the participants reported they experienced educational disruptions had higher odds for PTSS and depressive symptoms (Table 4). This finding indicates that the educational loss due to the institutional shut down has significantly affected students’ mental health. Though online education was introduced to fill the loss but rural and underprivileged individuals without devices, internet or high-speed broadband connection were still in stress for not being able to attend online class. A recent suicide pact has been reported which was related to unresolved arguments about the online schooling (Mamun, Chandrima, & Griffiths, 2020). Additionally, respondents who involved themselves in educational activities (i.e., online class, exams, assignments, thesis) were 31% and 19% more likely to experience PTSS and depressive symptoms, respectively (Table 3). Uncertainty about academic advancement might act as a stressor for students (Roy et al., 2020). Longitudinal research and qualitative explorations are needed in order to understand the mechanisms behind this finding.
Another noteworthy finding was about students experiencing suspected COVID-19 symptoms such as fever, dry cough, sore throat, difficulty breathing and fatigue had higher likelihood of having PTSS and depressive symptoms (Khan et al., 2020). It encourages the adopting of a fast COVID 19 diagnostic strategy with widespread access to mitigate the psychological effect and psychiatric symptoms (Wang et al., 2020). Most importantly, due to the resemblance of these symptoms with COVID-19, about 14.64% of the students perceived that they were infected with COVID-19 and produced higher level of PTSS and depressive symptoms among them. This finding corresponds to previous study conducted on Bangladeshi students indicating increased depression and event specific distress associated with perceiving flu-like symptoms as COVID-19 (Khan et al., 2020). This finding indicates the importance of adding psychological intervention with treatment for who experience suspected symptoms during any outbreak. Regarding the variables related to psychological impact, we have found recreational activities and physical exercise helped students to cope up with the situation by indicating lower level of PTSS and depressive symptoms (Table 3). Recreational activities can provide rest by rendering less stress throughout the pandemic. Furthermore, physical activity is able to decease psychological morbidities by ameliorating sleep quality (Ji et al., 2017). The study also figures strong association of fear of COVID-19 infection and fear of death by COVID-19 with PTSS and depressive symptoms (Khan et al., 2020) which indicates that PTSS can occur when fear is not regulated appropriately (Rau, DeCola, & Fanselow, 2005). About 19% and 77.43% of the students reported to have inadequate food supply and financial uncertainty that were significantly associated with depressive symptoms. It is no surprise considering extended confinement and social isolation that is exhausting limited resources available. As students are receptive to mobile applications (Do et al., 2018), health personnel should consider ensuring online psychological care through smartphone. Furthermore, adaptation of healthy lifestyles like doing physical exercise regularly is highly recommended to prevent depression and PTSS.
4.1. Strength and limitation
To the best of our knowledge, this study is reporting novel findings for the first time on PTSS and depressive symptoms among Bangladeshi students during COVID-19 mandatory home confinement. This study assessed the effect of educational disruption and suspected COVID-19 symptoms on mental health among students during COVID-19 which might assist in suitable policy implementation for students.
The present study has some limitations that should be noted whilst interpreting the findings. Firstly, the self-reported data from the study are subjected to social desirability bias and reporting bias. As internet access was a requirement to participate in this study, it is definite that the study could not include respondents from lower socio-economic subgroup who do not have access to the internet. Thirdly, convenience sampling technique is limited by selection bias. Although respondents were from all 8 divisions, responses were not equally distributed in all 8 division. It was possible that the most concerned individuals were more likely to participate in the study. Finally, the cross-sectional design of the study limited the ability to draw any causality which emphasize the need for future longitudinal study. Large-scale studies with both qualitative and quantitative methods should be conducted to further explore these issues. Notwithstanding these limitations, we believe that the study provides an important early look at the mental health of students during COVID-19 outbreak.
5. Conclusion
The results of this study provide the first nationwide data about PTSS and depressive symptoms among Bangladeshi students, suggesting the need for adequate psychological support. The factors that predicted higher impact were being female, having suspected COVID-19 symptoms, fear of infection and death by COVID-19, longer duration of home-stay and educational disruptions. While physical exercise and recreational activities emerged as the protective factors against depressive symptoms and PTSS. A key public health implication is that the findings of this research could help identify students who are particularly vulnerable to mental health issues so that health authorities can provide effective psychological support around the world to cope with this situation mentally at such difficult times.
Funding
Self-funded.
Ethics and consent to participate
Ethical standards were maintained to the highest possible extent whilst the study was conducted. Ethical clearance certificate (Ref No: BBEC, JU/M 2020/COVID-19/(8)1) for this study was obtained from the Institutional Review Board (IRB), “Biosafety, Biosecurity & Ethical Committee” of the Jahangirnagar University. Furthermore, all participants read, understood a consent form and agreed to participate in the study.
CRediT authorship contribution statement
Mst. Sadia Sultana: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft, Writing - review & editing, Validation. Abid Hasan Khan: Conceptualization, Investigation, Formal analysis, Data curation, Writing - original draft, Validation. Sahadat Hossain: Conceptualization, Supervision, Writing - review & editing, Validation. Adnan Ansar: Writing - review & editing. Md Tajuddin Sikder: Writing - review & editing, Validation. M. Tasdik Hasan: Writing - review & editing, Validation.
Declaration of Competing Interest
The authors declare that they have no complicit of interest.
Acknowledgements
The authors would like to express the most profound gratitude to the respondents who participated in this study voluntarily and spontaneously. Furthermore, the authors highly appreciate the contribution of Md. Tanzirul Alam, Tauhidul Islam, Md. Shahjahan, Md. Arifur Rahman, Md. Sabbir Mia, Rakebul Hasan, Md. Fazle Rabby, Sadia Yasmin, Mahjabeen Siddique, Jannatul Ferdous Tora, Anik Dutta, A. K. M. Sadikur Rahman Siam, Mohuya Jannat Masuma, Md. Rahmatullah, Md. Kamruzzaman, Nasim Chowdhuri, Hazera Sultana, Md. Asifur Rahaman, Md. Rakibul Alam Sorkar Rabby, Bishakha Mutsuddy, Mst. Jemi Khatun, Rebeka Sultana, Maksuda Akter Tane, Md. Momshad Reza during data collection periods.
References
- Anjum A., Hossain S., Sikder T., Uddin M.E., Rahim D.A. Investigating the prevalence of and factors associated with depressive symptoms among urban and semi-urban school adolescents in Bangladesh: A pilot study. International Health. 2019 doi: 10.1093/inthealth/ihz092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banna M.H.A., Sayeed A., Kundu S., Christopher E., Hasan M.T., Begum M.R.…Khan M.S.I. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: A nationwide cross-sectional study. International Journal of Environmental Research. 2020;1–12 doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T.…Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychological Medicine. 2020;1–2 doi: 10.1017/s0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton D., O'Ryan D., Udwin O., Boyle S., Yule W. The long-term psychological effects of a disaster experienced in adolescence: II: General psychopathology. Journal of Child Psychology and Psychiatry. 2000;41(4):513–523. [PubMed] [Google Scholar]
- Boyraz G., Legros D.N. Coronavirus Disease (COVID-19) and Traumatic Stress: Probable risk factors and correlates of posttraumatic stress disorder. Journal of Loss and Trauma. 2020;25:503–522. doi: 10.1080/15325024.2020.1763556. [DOI] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England) 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for DIsease Control and Prevention (CDC). (2020). Coronavirus Disease 2019 (COVID-19) Retrieved 2020, Aug 20, from https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html.
- Chowdhury A.N., Ghosh S., Sanyal D. Bengali adaptation of brief patient health questionnaire for screening depression at primary care. Journal of the Indian Medical Association. 2004;102(10):544–547. [PubMed] [Google Scholar]
- Coffey S.F., Gudmundsdottir B., Beck J.G., Palyo S.A., Miller L. Screening for PTSD in motor vehicle accident survivors using the PSS-SR and IES. Journal of Traumatic Stress. 2006;19(1):119–128. doi: 10.1002/jts.20106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do T.T.T., Le M.D., Van Nguyen T., Tran B.X., Le H.T., Nguyen H.D.…Zhang M.W.B. Receptiveness and preferences of health-related smartphone applications among Vietnamese youth and young adults. BMC Public Health. 2018;18(1):764. doi: 10.1186/s12889-018-5641-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. Students under lockdown: Comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One. 2020;15(7):e0236337. doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) Journal of Medical Internet Research. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hossain S., Anjum A., Uddin M.E., Rahman M.A., Hossain M.F. Impacts of socio-cultural environment and lifestyle factors on the psychological health of university students in Bangladesh: A longitudinal study. Journal of Affective Disorders. 2019;256:393–403. doi: 10.1016/j.jad.2019.06.001. [DOI] [PubMed] [Google Scholar]
- Islam M.A., Barna S.D., Raihan H., Khan M.N.A., Hossain M.T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PLoS One. 2020;15:e0238162. doi: 10.1371/journal.pone.0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, H.-J, Nan, J, Lv, Z.-Y, &, Yang, J. (2020). Psychological impacts of the COVID-19 epidemic on Chinese people: Exposure, post-traumatic stress symptom, and emotion regulation 13,252–259 doi:10.4103/1995-7645.281614.
- Ji X.W., Chan C.H., Lau B.H., Chan J.S., Chan C.L., Chung K.F. The interrelationship between sleep and depression: A secondary analysis of a randomized controlled trial on mind-body-spirit intervention. Sleep Medicine. 2017;29:41–46. doi: 10.1016/j.sleep.2016.08.025. [DOI] [PubMed] [Google Scholar]
- Kaparounaki C.K., Patsali M.E., Mousa D.V., Papadopoulou E.V.K., Papadopoulou K.K.K., Fountoulakis K.N. University students' mental health amidst the COVID-19 quarantine in Greece. Psychiatry Research. 2020;290:113111. doi: 10.1016/j.psychres.2020.113111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Pratt C., Galea S., McLaughlin K.A., Koenen K.C., Shear M.K. The burden of loss: Unexpected death of a loved one and psychiatric disorders across the life course in a national study. American Journal of Psychiatry. 2014;171:864–871. doi: 10.1176/appi.ajp.2014.13081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A.H., Sultana M.S., Hossain S., Hasan M.T., Ahmed H.U., Sikder T. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. Journal of Affective Disorders. 2020 doi: 10.1016/j.jad.2020.07.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopala-Sibley D.C., Danzig A.P., Kotov R., Bromet E.J., Carlson G.A., Olino T.M.…Klein D.N. Negative emotionality and its facets moderate the effects of exposure to Hurricane Sandy on children's postdisaster depression and anxiety symptoms. Journal of Abnormal Psychology. 2016;125(4):471–481. doi: 10.1037/abn0000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Chandrima R.M., Griffiths M.D. Mother and son suicide pact due to COVID-19-related online learning issues in Bangladesh: An unusual case report. International Journal of Mental Health and Addiction. 2020;1–4 doi: 10.1007/s11469-020-00362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marelli S., Castelnuovo A., Somma A., Castronovo V., Mombelli S., Bottoni D.…Ferini-Strambi L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology. 2020 doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y., Sullivan G.M. Understanding the mental health effects of indirect exposure to mass trauma through the media. JAMA. 2011;306(12):1374–1375. doi: 10.1001/jama.2011.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Research. 2020;290:113108. doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rau V., DeCola J.P., Fanselow M.S. Stress-induced enhancement of fear learning: An animal model of posttraumatic stress disorder. Neuroscience & Biobehavioral Reviews. 2005;29(8):1207–1223. doi: 10.1016/j.neubiorev.2005.04.010. [DOI] [PubMed] [Google Scholar]
- Reardon S. Ebola's mental-health wounds linger in Africa. Nature. 2015;519(7541):13–14. doi: 10.1038/519013a. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Rey R., Garrido-Hernansaiz H., Collado S. Psychological Impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.01540. 1540–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum B.O., Foa E.B., Riggs D.S., Murdock T., Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5(3):455–475. doi: 10.1002/jts.2490050309. [DOI] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102083. 102083–102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz R.M., Rasul R., Gargano L.M., Lieberman-Cribbin W., Brackbill R.M., Taioli E. Examining associations between hurricane sandy exposure and posttraumatic stress disorder by community of residence. Journal of Traumatic Stress. 2019;32(5):677–687. doi: 10.1002/jts.22445. [DOI] [PubMed] [Google Scholar]
- Sediri S., Zgueb Y., Ouanes S., Ouali U., Bourgou S., Jomli R., Nacef F. Women’s mental health: acute impact of COVID-19 pandemic on domestic violence. Archives of Women's Mental Health. 2020 doi: 10.1007/s00737-020-01082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultana M.S., Khan A.H., Hossain S., Ansar A., Sikder M.T., Hasan M.T. Anxiety, depressive symptoms, sleep patterns & associated factors among Bangladeshi wage earners during the COVID-19 pandemic: A cross-sectional study. PsyArXiv. 2020 doi: 10.1080/13548506.2022.2083642. https://psyarxiv.com/289uf/ [DOI] [PubMed] [Google Scholar]
- Sultana M.S., Khan A.H., Hossain S., Islam T., Hasan M.T., Ahmed A.U., Khan J.A.M. The association between financial hardship and mental health difficulties among adult wage earners during the COVID-19 pandemic in Bangladesh: Findings from a cross-sectional analysis. PsyArXiv. 2020 doi: 10.3389/fpsyt.2021.635884. https://psyarxiv.com/q3ehv/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C.…Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of affective disorders. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tham K., Tan Y., Loh O., Tan W., Ong M., Tang H. Psychological morbidity among emergency department doctors and nurses after the SARS Outbreak. Hong Kong Journal of Emergency Medicine. 2005;12(4):215–223. doi: 10.1177/102490790501200404. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020a). Coronavirus disease (COVID-19) Retrieved 18 Dec, 2020, from file:///C:/Users/Suhi/Downloads/wou-14december2020.pdf.
- World Health Organization. (2020b). Morbidity Mortality Weekly Update Retrieved 18 Dec, 2020, from https://www.who.int/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who_covid-19-update_42_20201214.pdf?sfvrsn=9272a233_7.
- World Health Organization. (2020c). COVID-19 Retrieved 17 Aug, 2020, from https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/.
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. International Journal of Environmental Research and Public Health. 2020;17(7) doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]