Abstract
Mobile health (mHealth) applications have become an important tool to support public health, especially in times of increased health awareness in the midst of the COVID-19 pandemic. However, there is still uncertainty about what factors determine successful mHealth services from the users’ perspective. Based on the results of a systematic literature review, a qualitative content analysis of available apps and semi-structured user and expert interviews, we derive a structural model with antecedents on user attitudes towards mHealth and user satisfaction with the mHealth application. These variables determine users’ intention to continue using the application and their intention to recommend it to others. For verification, we tested the model with a sample of 249 German mHealth users from the “MyFitnessPal” community using structural equation modelling and found that all derived path relations have significant coefficients.
Keywords: Mobile health, mHealth adoption, Structural equation modelling, Empirical research, Continuance intention, Public health
1. Introduction
Digitalization and the associated growth of efficient information and communication technology (ICT) are shaping modern society. In particular, the use of mobile communication technologies, such as smartphones and wearables, continues to increase (Larios Hernández, 2019; Wirtz, Birkmeyer, & Langer, 2019). This development also influences the health sector, especially through the use of mHealth applications (Mobile Health Apps). mHealth is a collective term for the use of mobile devices in private medical care. Building on the definition of mHealth by Tomlinson, Rotheram-Borus, Swartz, and Tsai (2013) and Van Heerden, Tomlinson, and Swartz (2012) we define mHealth services as services that improve personal healthcare through the use of mobile technologies. With this in mind, we consider the acceptance of mHealth services as the willingness of individuals to adopt mHealth technologies and applications.
The most common application of mHealth is the use of mobile devices for preventive health services such as fitness and nutrition, and mobile-based telehealth approaches to connect users and health professionals (Tomlinson et al., 2013; Van Heerden et al., 2012). Despite the personal benefits, the use of mHealth applications is also considered to have merit for society as it improves public health (Agarwal et al., 2016). Moreover, mHealth is an emerging field that has the potential to make the healthcare system more efficient, increase patient satisfaction and reduce healthcare costs (Hussain et al., 2018). In this context, the World Health Organization (WHO) concludes “mHealth has the potential to transform the face of health service delivery across the globe” (World Health Organization, 2011). Furthermore, the WHO points out that mHealth is now part of everyday life for many citizens and is therefore of great importance for public health worldwide (World Health Organization, 2018). The benefits of using mHealth technologies are manifold in concrete terms: to name but a few, mHealth-allows for the cost-effective generation of detailed long-term data on the health status of individuals as well as a larger number of people. Fitness data can be compared from mobile devices or wearables, and information exchange between all parties can take place anytime and anywhere. In remote areas, for example, mHealth enables more people to access health services. Patients can share their health-related parameters in real time and as often as necessary with the doctor or institution in charge. This allows for more efficient staff planning on the one hand and cost savings on the other. In addition, more efficient management of chronic health issues can be achieved through the introduction of remote monitoring and consultation. In view of the global situation the world is facing these days due to the coronavirus pandemic, many companies, governments, and citizen movements have launched mHealth initiatives to inform and help the population cope with the crisis.
Even though the benefits are obvious, there are still several questions about the diffusion of mHealth technologies in society. In the academic literature, there are calls for more research on mHealth as a still developing research field (Baulch, Watkins, & Tariq, 2018; Huang, Dong, & Wu, 2018). Specifically, scholars and companies see a particular need for research to investigate the determinants of mHealth success (Baldwin, Singh, Sittig, & Giardina, 2017; Marwah & Mittal, 2017; Stewart, 2018).
Even though many conceptual studies claim theoretical connections, there are still few empirical studies in this field, despite the request that " future researches are supposed to conduct deeper analysis" from the perspectives of different user groups and incorporate new path relations (Zhao, Ni, & Zhou, 2018, p. 346). With this in mind, we derive the following research questions: Is there a theory-based structural model that explains the success of mHealth apps? Do the derived hypotheses stand up to analytical testing based on a sample of mHealth users? And more specifically: What are the drivers for a positive attitude of users towards the respective apps and which factors determine user satisfaction regarding mHealth apps? And as a result of this impact relationship: What determines the decisive success factors for a continuous use of mHealth apps and a corresponding positive Word-of-Mouth (WoM)?
2. Literature overview
This literature review only provides insights into current and empirical studies in the field that are related to the stated research objective. Within the quantitative empirical literature on mHealth, a total of 18 studies were identified by searching relevant databases such as EBSCO, ScienceDirect, ResearchGate and Google Scholar. Regarding the empirical multivariate quantitative research on mHealth, it can first be noted that almost all contributions have exclusively taken up established models of acceptance and information systems research. In particular, models of technology acceptance such as the Technology Acceptance Model (TAM) or the Unified Theory of Acceptance and Use of Technology (UTAUT) as well as models of success factors of information systems such as the DeLone and McLean IS Success Model are used. Only two contributions follow the Theory of Reasoned Action, two other contributions are based on previous research results without theoretical reference.
The TAM is a common starting point for analyzing the acceptance of new technologies because of its clearly structured specification and its simplicity (Legris, Ingham, & Collerette, 2003; Venkatesh & Davis, 2000). However, the parsimonious nature of the TAM has also been the source of criticism and has led researchers to adapt it depending on the context of the study and based on relevant factors (Nysveen, Pedersen, & Thorbjørnsen, 2005; Venkatesh & Davis, 2000). Therefore, the TAM has often been extended to include other aspects and to adapt the model according to the context. Eventually, this has contributed to the development of a Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh, Morris, Davis, & Davis, 2003). Table 1 provides an overview of the empirical-quantitative mHealth literature relevant to this study.
Table 1.
Empirical Studies on mHealth.
| Author(s) | Central Question | Theory | Empirical review | Core results |
|---|---|---|---|---|
| Akter et al. (2010) | Which factors influence the service quality of mHealth? | D&M- Modell |
|
The quality of service has a strong positive effect on the satisfaction, continuance intentions and quality of life of mHealth. |
| Akter et al. (2011) | What influence does the trust in consumer confidence and continuity intention of mHealth? | TRA |
|
Trustworthiness is a second order reflective construct, the influence on the continuity intention of mHealth. |
| Akter, D’Ambra et al. (2013) | What influence does the mHealth service quality have on the continuity intention, the satisfaction and the life quality? | Previous Research |
|
The quality of service has both direct and indirect effects on the continuance intention and on the quality of life. In this context, satisfaction has a mediating effect. |
| Cho et al. (2015) | Which Relationship exists between body perception the perceived usefulness of dietetic and fitness apps and the behavioral intention to use these apps? | TAM |
|
The appearance, the fitness orientation and the own fitness evaluation influence the perceived usefulness of diet and fitness apps. |
| Cho et al. (2014) | What influence do cognitive factors have on the use of health apps? | Previous Research |
|
Health awareness has an impact on health app usage. |
| Deng (2013) | Which determinants determine the user adoption of mHealth? | TAM; HBM |
|
Perceived benefits, perceived barriers and cues to use positively influence the mHealth attitude of users |
| Dwivedi et al. (2016) | What explains intrinsic and extrinsic adoption behavior for mhealth services, considering user preferences and intercultural differences? | UTAUT, UTAUT2 |
|
The results suggest that the UTAUT model partially explains the pattern behavior with respect to mHealth applications. In addition, specific determinants such as cognitive, affective and conative or behavioral play an important role. |
| Guo et al. (2016) | What effects have security concerns and personalization on the acceptance of mHealth? | Previous Research |
|
Perceived personalization and privacy concerns are positively and negatively associated with behavioral intent. |
| Hoque and Sorwar (2017) | How is the acceptance of mHealth among older users? | UTAUT |
|
Expectations of performance, expectations of effort, social influence, fear of technology and resistance to change all have an impact on the behavioral intention to accept mHealth services. |
| Hossain (2016) | How can a success model for the validation of mHealth be developed? | D&M- Modell |
|
The intention to continue depends on perceived value and user satisfaction. The quality of medical advice and interaction quality have a positive effect on perceived value and user satisfaction. The Continuance intention positively influences the quality of health life. |
| Hung and Jen (2012) | Which determinants determine the adoption of mHealth? | TAM |
|
Perceived usefulness and attitude influence the behavioral intention of adopting mHealth. The determinants of attitude towards mHealth differ according to age: young adults have a stronger intention of adopting mHealth. |
| Nisha, Iqbal, Rifat, and Idrish (2015) | Which critical factors influence the intention to use mHealth? | UTAUT |
|
Effort expectation, facilitating conditions, information quality and trust influence the behavioral intention. |
| Okazaki, Castañeda, Sanz, and Henseler (2013) | What factors influence the adoption of Japanese doctors for mHealth use in diabetics? | D&M- Modell |
|
Net benefit and perceived value influence the usage intention. The influence of overall quality and net benefits on the usage intention is significantly strengthened by self-efficacy and compatibility |
| Sezgin, Özkan-Yildirim, and Yildirim (2018) | How is the perception by physicians regarding the use of mobile health applications? | TAM |
|
Effort Expectancy, Mobile Anxiety, Perceived Service Availability and Technical Training and Support have influence on the behavioral intention. |
| Shareef, Kumar, and Kumar (2014) | Which determinants influence the mHealth adaptation of diabetes patients? | TAM |
|
Perceived benefits, perceived usability, perceived reliability, perceived security and privacy influence the attitude towards the mHealth adaptation of patients. |
| Vervier, Valdez, and Ziefle (2019) | Which determinants have an influence on the attitude towards mHealth? | Previous Research |
|
Health consciousness has a positive influence on the attitude towards mHealth. Privacy Concerns have no influence on the attitude towards mHealth. |
| Wu, Wang, and Lin (2007) | Which factors influence the acceptance of mHealth by medical professionals? | TAM |
|
Compatibility, perceived usefulness and perceived usability influence behavioral intention. MHS self-efficacy has a strong influence on the behavioral intention. |
| Zhang, Guo, Lai, Guo, and Li (2014) | What role do gender-specific differences play a role in the adoption of mHealth? | TRA |
|
Facilitating conditions, attitude and subjective norm influence the mHealth adoption Men show a higher level of mHealth adoption than women. |
Considering the set objective, one of the most relevant studies examining the key determinants of individual attitude and behavioral intention is Zhao et al. (2018). Their meta-analysis of 35 empirical studies offers a comprehensive framework regarding the adoption of individual mobile health services. The constructs perceived usefulness, perceived ease of use, perceived vulnerability and perceived severity have all been found to have significant impact on mHealth users’ attitude. Perceived usefulness, perceived ease of use, subjective norm, trust, perceived risk, and attitude also significantly influence behavioral intention. The study finds also that “the core model of technology acceptance theories, TAM is demonstrated to be supportable and robust” (Zhao et al., 2018, p. 348). This study that is based on various empirical articles still calls for further investigation of different perspectives as well as new path relations.
One aspect that is not investigated in the Zhao et al. study is the importance of patient satisfaction as major indicator in measuring the effects of quality or overall service performance (Akter, D’Ambra, Ray, & Hani, 2013). Hence, the concept of satisfaction is also central to the mHealth literature (Akter, D’Ambra et al., 2013; Chaniotakis & Lymperopoulos, 2009; Cianflone et al., 2018; Hossain, 2016). Hossain (2016) sees user satisfaction as a prerequisite for the intention of users to continuously use mHealth applications. A similar argumentation can also be found in Akter, Ray, and D’Ambra (2013).
Furthermore, user satisfaction is also of great importance for word-of-mouth recommendation. Palka, Pousttchi, and Wiedemann (2009) for example argue that satisfaction plays a critical role in studies of word of mouth behavior as it affects individual motivations to recommend services. With regard to our research focus Nelson (2017) states that the mHealth App MyFitnessPal has grown significantly without paid marketing because users were very satisfied and recommended it accordingly (Nelson, 2017). In another study, Lee (Lee, 2009) found a positive influence of attitude on user satisfaction. The qualitative-empirical study of Butt and Aftab (Butt & Aftab, 2013) also showed a positive influence of attitude on satisfaction.
In the scientific literature there are only few studies which take health-specific factors into account. A study by Deng (2013) investigates the influence of perceived disease threat on attitude. Within a health status, perceived disease threat has been suggested to positively affect user attitude toward health-related application (Deng, 2013). In addition, the study of Cho, Park, and Lee (2014) investigates the importance of health consciousness. They argue that people who are more health conscious are more likely to have healthy habits - spending more time on healthy activities but also actively gathering health information from a variety of sources while avoiding potentially unhealthy situations. (Cho et al., 2014).
Another study by Guo, Zhang, and Sun (2016) focuses on the personalization of mHealth. They highlight the importance of personalization as the provision of appropriate health services for specific health conditions and diseases to consumers via mobile devices (Guo et al., 2016). Besides, Guo et al. (2016) and Mohr, Schueller, Montague, Burns, and Rashidi (2014) mention that the content of information should be tailored to fit the user’s needs and capabilities by altering language or providing examples that are more likely to be relevant to the user (Mohr et al., 2014).
The study by Wang and Chen (2016) investigates the influence between interaction quality and satisfaction. Their results show that the quality of interaction significantly influences user satisfaction (Wang & Chen, 2016). Similar results are reported in the study by Akter, D’Ambra, and Ray (2010). In a different study by Tang, Abraham, Stamp, and Greaves (2015) the authors mention the importance of the mobile app design. In this respect, Tang et al. (2015) demand that designers should also consider the importance of user interface design as it determines the functionality, and consequently, the usability of an e-health weight loss app (Tang et al., 2015). Additionally, the study by Lee and Chuang (2009) shows display formats, colors, and graphs versus tables and how these factors affect customer satisfaction (Lee & Chuang, 2009). Moorhead et al. (2013) mention the importance of Social media networks as a changing the nature and speed of health care interaction between individuals and health organizations. Furthermore the general public, patients, and health professionals are using social media to communicate about health issues (Moorhead et al., 2013).
Other recent studies provide important insights for the model development but focus on different aspects: Liu, Ngai, and Ju (2019) investigate the influence of individuals’ different motivation incentives on their intentions to use mHealth services by testing interdependencies from motivation theory. Dwivedi, Shareef, Simintiras, Lal, and Weerakkody (2016) compare different model theories such as the TAM and the UTAUT in the field of mHealth and also examine cultural dominance on user behavior. Accordingly, the starting point for the model development of this research project was the factors and impact relations of the TAM and the UTAUT. Recent studies show that there is still a theoretical debate about the most reliable model designs and the respective interdependencies to explain the drivers of technology acceptance (Dwivedi et al., 2017; Dwivedi, Rana, Jeyaraj, Clement, & Williams, 2019; Dwivedi, Rana, Tamilmani, & Raman, 2020).
In summary, despite some empirical studies, there are few articles that examine the importance of user satisfaction with mHealth apps. Furthermore, there are also only few studies that analyze health-specific determinants (such as health awareness and disease threat) on user attitudes. This is surprising, as the success of mHealth apps can be characterized by attitude and satisfaction with the app features.
3. Methodology
For the identification and selection of relevant mHealth success factors and the corresponding model derivation, a mixed methods research approach was used, thus combining quantitative and qualitative research approaches (Brannen, 2005; Greene, Caracelli, & Graham, 1989; Tashakkori & Creswell, 2007; Venkatesh, Brown, & Bala, 2013). In our study we follow the concept of a developmental approach defined in line with the work of Irma Becerra-Fernandez (2001), Ho, Ang, and Straub (2003) and Grimsley and Meehan (2007) as follows: the “qualitative study was used to develop constructs and hypotheses and a quantitative study was conducted to test the hypotheses” (Venkatesh et al., 2013, p. 26). The object of the study is not to test a “well-established theoretical perspective” (Venkatesh et al., 2013, p. 36), but to investigate the specific interactions in the mHealth app context. Against this background, epistemologically we follow a pragmatic approach: “a pragmatic approach is based on abduction reasoning that moves back and forth between induction and deduction” (Venkatesh et al., 2013, p. 37). Regarding the design strategy, we follow a sequential approach by first using qualitative data and then performing a test to examine the qualitative data.
The model development is based on three steps of qualitative research: 1. A literature-based identification of determinants and corresponding impact relations on relevant success factors, 2. A qualitative content analysis of available apps, 3. Semi-structured expert interviews with experts and mHealth app-users.
Regarding the first step, initial findings are already presented in the literature review. Furthermore, explanatory models and factors from the literature were identified and compared. In the second step, we conducted a qualitative content analysis according to Mayring (2004) by comparing the top ten mHealth apps on the market in terms of features, functions, services offered and related content. Based on the first two steps, we identified a relevant set of mHealth factors. In the third step, interviews were conducted with eleven intensive users of mHealth apps. These individuals use the apps several times a day over a longer period. They have extensive knowledge and can evaluate the features and functions of the apps more accurately and meaningfully than casual users. Intensive users of health apps were identified based on their posts or contributions in the community of the respective mHealth app. They were then contacted by personal message and invited to an interview. In this way, 11 intensive users could be reached who agreed to participate in an interview. An interview guide was first designed for the interviews. The topic of the study was first explained to the intensive users to further check the relevance of the topic of the study in advance. Regarding the relevance of the topic of the study, the intensive users generally confirmed the relevance of the topic of the study for them as users of mHealth apps. Furthermore, the intensive users were asked about their average daily usage time of the mHealth app to ensure that they are indeed intensive users. The daily usage time of the intensive users was between 25 and 35 min, which corresponds to an average usage time of 28 min daily. Thus, it could be confirmed that the interviewed users are indeed intensive users.
In order to subsequently match the constructs of the research model derived from the theory, the relevant literature and the qualitative content analysis with the experiences of the intensive users, the relevance of the individual exogenous success factors was discussed with regard to their effect on user satisfaction and the users' attitude towards mHealth. First, the intensive users were asked about their understanding of the individual constructs of the success factors in order to compare them with the scientific definition from the literature. In case of an unclear understanding of the terms, the intensive users were informed about the corresponding definition of the unclear success factor. Furthermore, the intensive users were asked about the practical significance of the success factors. For this purpose, they were asked to rate the individual success factors as relevant or not relevant for use in practice. For this purpose, the users were first asked about the practical relevance of the information technology success factors.
Finally, to validate the identified set, we conducted semi-structured expert interviews with nine academics researching in the field and seven practitioners from the digital and mobile industry. In doing so, we used established interview methods, an iterative process of multi-stage rounds of enquiry that leads to more comprehensive results and more relevant data than using traditional interview methods (Okoli & Pawlowski, 2004).
4. Theoretical background and hypotheses development
The following section presents the derivation of the conceptual model and the associated hypotheses. Building on the findings from the literature and the insights from the expert interviews, a comprehensive theoretical explanatory model is designed that presents and conceptualizes relevant determinants of mHealth success. In line with the principles of a pragmatic multi-method approach, the context of mHealth required that a specific model be derived based on qualitative methodology.
There are two basic approaches to user behavior in information systems research: The user attitude approach and the user satisfaction approach (Wixom & Todd, 2005). Both components are important approaches and are interrelated.
The original TAM by Davis, Bagozzi, and Warshaw (1989) assumes that a positive user attitude is the key determinant of actual usage. What exogenous factors influence users' attitudes towards mHealth? In this regard, Hung and Jen (2012) state that: “Users of Mobile Health Management Systems adopt the system voluntarily, and their attitudes are important” (Hung & Jen, 2012). In terms of the original TAM, there are two drivers that shape attitudes, perceived usefulness and perceived ease of use that are in turn influenced by other factors, what is also true in the mHealth context (Zhao et al., 2018). Considering previous research in the area, however, with regard to mHealth applications, attitudes are also influenced by positive or negative health-specific factors such as perceived disease threat or health awareness (Cho et al., 2014; Deng, 2013). In addition to the basic technology-related determinants of perceived usefulness and perceived ease of use, it can therefore be argued that health-specific factors (health awareness and disease threat) influence the general attitude of users towards the use of mHealth apps. Accordingly, it can be concluded that user attitudes in this context cannot be derived exclusively from the provided mHealth app, but rather from the user's basic attitude towards their own health.
While the TAM assumes that user attitudes are fundamentally shaped by technology, we now separate technology-related attitudes and use the term attitude to describe only general mHealth-related attitudes. Technology and specific app-related attitudes can also be investigated by examining satisfaction with the specific app and its characteristics. This differentiation is the result of the survey of users and experts in the field of mHealth and enables a clear delimitation. However, this differentiation deviates from the understanding of the original TAM, which uses the term user attitude to refer in particular to the attitude towards the specific technology.
From the results of the survey of users and experts, a distinction can now be made between the two basic factors of general mHealth attitude and technology or app satisfaction. As already mentioned, two important factors that shape the basic attitude are health awareness and disease threat (Deng, 2013). These two factors were considered particularly relevant by both the experts and the users.
Despite the differentiation, it can be assumed that the user's mHealth attitude also influences user satisfaction (Butt & Aftab, 2013; Lee, 2009; Sun, Tsai, Finger, Chen, & Yeh, 2008). This can be explained by the fact that people who attribute a significant role to health and thus have a positive attitude to mHealth are also generally more satisfied with a health-related app.
Satisfaction with a specific health app is in turn determined by various factors. Several factors were presented in the interviews. In particular, the users confirmed the importance of personalization, interaction, the user interface (app design) and the social networking component.
While the intention to use an application can be considered as an initial step towards success of an mHealth app provider, we consider a more sustainable usage to be the eventual goal, which is why the construct continuous intention to use is the more important construct (Bhattacherjee, 2001; Bhattacherjee & Premkumar, 2004). In addition, (Hossain, 2016) and Akter, Ray et al. (2013) see satisfaction as a necessary prerequisite for the intention of users to use mHealth applications continuously (continuance intention to use). Thus, this impact relation should be included in the conceptual model.
Sun, Wang, Guo, and Peng (2013) argue that mHealth service providers should carry out certain promotion strategies to obtain early adopters and then expand the consumer scale through the social influence (e.g., word of mouth). Accordingly, the word of mouth, along with the continuance intention to use, is another endogenous factor for the success of mHealth applications. WoM describes the intention to share opinions about the products and services people consume (Gupta & Harris, 2010; Lee, Shi, Cheung, Lim, & Sia, 2011) and to research the companies that sell them. Hence, the conceptual model comprises the endogenous constructs of attitude, satisfaction, and continuance intention to use as well as word of mouth. The intention of customers to continue using the app and their intention to recommend it (WoM) were confirmed by experts as fundamental success factors for mHealth apps.
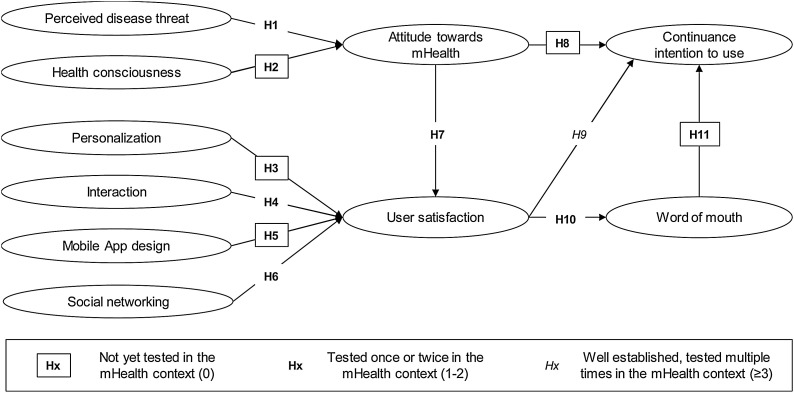
Fig. 1 below illustrates the model, which is explained in more detail in the following sections. The model graphically represents the degree of establishment of relationships to provide an immediate understanding of which paths have already been empirically investigated and which have not.
Fig. 1.
mHealth Model.
4.1. Perceived disease threat
At the beginning, we deduce and conceptualize the first health-specific factor perceived disease threat. The perceived health threat has its theoretical origin in the Health-Belief-Model (Rosenstock, Strecher, & Becker, 2013). In principle, the perceived health threat consists of the factor subjective vulnerability to a disease and the perceived severity level of a disease (Tarkang & Zotor, 2015). In contrast, Deng (2013) understands the perceived disease threat as a threat which includes perceived susceptibility and severity, which refers to one's subjective perception of the risk of contracting a health condition and the seriousness of contracting an ailment or of leaving it untreated. According to his Health-Belief-Model, the stronger the perceived disease threat, the easier it would be for a person to take health-related actions. Furthermore, Deng (2013) argues that within a health setting the perceived disease threat is suggested to positively affect user attitude towards health-related applications. Based on these explanations, it can be anticipated that the exogenous health-specific success construct of the perceived disease threat has a positive influence on the attitude of the user towards mHealth. Consequently, the exogenous health-specific success construct, the perceived disease threat, is to be included in the study model. Therefore, the following hypothesis is postulated:
H1
The perceived health threat positively influences the user's attitude towards mHealth.
4.2. Health consciousness
The second health-specific exogenous mHealth success factor is health consciousness. In contrast to the exogenous mHealth success factor perceived disease threat, health consciousness does not focus on the threat of a possible illness, but on self-motivation (Cho et al., 2014). It can therefore be assumed that users with a high health consciousness spend more time searching for health-specific information than users with a comparatively low health consciousness (Cho, Lee, Kim, & Park, 2015). In this context Cho et al. (2014) state: “People with higher levels of health consciousness are more likely to have healthy habits, spend more time on exercise and healthy activities, actively gather health information from various sources, and avoid unhealthy situations” (Cho et al., 2014, p. 2). Regarding our study, it therefore seems reasonable to include health consciousness in the research model. The following hypothesis should be formulated for the study:
H2
Health consciousness positively influences the user's attitude towards mHealth.
4.3. Personalization
Personalization possibility of the mHealth App was identified as the first mobile-specific exogenous factor. With regard to the definition of the exogenous success construct personalization, the definition of Fan and Poole (2006) can be used. Fan and Poole (2006) define personalization as: „a process that changes the functionality, interface, information access and content, or distinctiveness of a system to increase its personal relevance to an individual or a category of individuals “(Fan & Poole, 2006). As each mHealth user has different individual needs, the possibility of adjusting the mHealth service to the individual preferences and needs of the users is a critical success factor of mHealth. In this context, Mohr et al. (2014) cite the following example for a personalization of an mHealth application: “the content of information may be tailored to fit the user’s needs and capabilities by altering language or providing examples that are more likely to be relevant to the user “(Mohr et al., 2014). In addition, Guo et al. (2016), in their quantitative-empirical study, highlight the importance of personalization for adjusting the mHealth application to the specific needs and requirements of mHealth users: “in the mHealth context, personalization can thus be defined as the provision of appropriate health services for specific health conditions and diseases to consumers via mobile devices” (Guo et al., 2016). With regard to the cause effect relationship between personalization and user satisfaction, there are indications in the literature that suggest a positive influence of personalization on user satisfaction. Park (2014), for example, states: “personalization increases satisfaction” (Park, 2014). Accordingly, the exogenous success construct of personalization represents a relevant and significant influencing factor for user satisfaction of mHealth applications. Against this background, personalization is to be included in our research model. Therefore, the following hypothesis is formulated:
H3
Personalization positively influences the user satisfaction of mHealth services.
4.4. Interaction
Similarly to personalization, previous research has proposed interaction as a second relevant mobile-specific factor in the context of mHealth. Wang and Chen (2016) understand interaction as the interactive relationship with service providers, including the most used positioning and navigating functions (Wang & Chen, 2016). Thus, interaction describes the possibility of the app to interact with the user or to give feedback. This includes in particular prompt input and the corresponding feedback. The feedback can range from a simple confirmation by a vibration of the smartphone to animated effects on the display but also reminder messages on the home screen, e.g. in case of longer inactivity, are part of the interactive elements. In this way, interaction is the ability of a technology to use a bidirectional way of communication providing a virtual “personal trainer” who takes care of users (Dicianno et al., 2015). Thus, most m-Health services are highly interactive, enabling a meaningful collaboration of the parties, and thus being crucial for user satisfaction (Hossain, 2016; Wang & Chen, 2016). Due to the meaningful interaction between the mHealth app and the user an influence of the exogenous construct of interaction on user satisfaction can be anticipated. Therefore, the inclusion of interaction in the conceptual model is recommended. Based on this execution, the following hypothesis can be postulated:
H4
Interaction positively influences the user satisfaction of mHealth.
4.5. Mobile app design
Mobile app design or interface design is the appealing, comprehensible, and logical design of the user interface. Mobile app design is omnipresent at any time of use. Therefore, it is of particular importance for the user that the app is appealing, comprehensible and logically structured. In the mHealth literature Tang et al. (2015) emphasize the importance of mobile app design and provide recommendations for the designers of health tips and especially for the design of mHealth applications. Designers should consider the importance of user interface design as it determines the functionality, and consequently, usability of mHealth applications (Tang et al., 2015). Furthermore, Lee and Chuang (2009) mention the importance of mobile app design for user satisfaction with mobile devices: “an interface is often the first point of contact. It is therefore important that a good image is presented, as users will form their impressions based on this initial information. Numerous studies have assessed such factors as display formats, colors, and graphs versus tables and how these factors affect customer satisfaction” (Lee & Chuang, 2009). The explanations have shown that the design represents an important mobile-specific success factor for mHealth. In particular, the ubiquitous and inevitable nature of mobile app design recommends the inclusion of the exogenous success construct of mobile app design in the research model. The explanations have shown that a professionally designed mobile app design can have a positive influence on user satisfaction. Therefore, the following hypothesis should be formulated for the research model:
H5
A well-perceived mobile app design positively influences mHealth user satisfaction.
4.6. Social networking
The construct of social networking is understood as giving users the opportunity to establish contacts and networks with other users. For this purpose, requests for friendship can be sent and events can be shared with other members. Some mHealth apps allow users to post results and information on social media networks such as Facebook or Instagram. In addition, social networking enables the user to interact with other users on health-specific topics via mobile devices. Regarding the importance of social networking for improving health, Luxton, McCann, Bush, Mishkind, and Reger (2011) argue that: “social support is a frequently targeted area in clinical practice and social networking via the Internet is recognised for its potential to provide new opportunities for social engagement and connection. […] several empirical studies have demonstrated the benefits of social networking sites for mental health and well-being […] and smartphones increase opportunities for social networking by making social media sites more accessible” (Luxton et al., 2011). Hence, social networking can be seen as a motivating factor for the user to use the mHealth app more intensively and thus lead to more satisfaction (Borrelli & Ritterband, 2015; Luxton et al., 2011). The following hypothesis should therefore be formulated for the study model:
H6
Social networking positively influences the user satisfaction of mHealth.
4.7. Attitude towards mHealth
The factor user attitude towards mHealth is based on the technology acceptance model (Davis et al., 1989). Attitude refers to an individual's positive or negative feelings towards something (Deng, 2013). Hence, the user attitude towards mHealth refers to a user's positive or negative feelings about mHealth applications. In respect of mHealth applications, these feelings are caused or influenced positively or negatively by health-specific factors such as perceived disease threat or health consciousness (Deng, 2013; Park, 2014).
The literature contains numerous studies that examine the influence of user attitude on user satisfaction. In a qualitative-empirical study Lee (2009) showed a direct, positive influence of attitude on satisfaction (Lee, 2009). The qualitative-empirical study of Butt and Aftab (2013) also showed a positive influence of attitude on satisfaction (Butt & Aftab, 2013). Overall, attitude describes psychological tendencies expressed through positive or negative evaluations. Hence, attitude is an effective predictor of user satisfaction (Lee, 2009). Therefore, the user attitude towards mHealth is to be included in the research model. For this purpose, the following hypothesis is formulated:
H7
A positive attitude towards mHealth increases the satisfaction of mHealth users.
Furthermore, a positive influence on the user behavior towards mHealth Apps can also be assumed by a positive attitude towards mHealth (Deng, 2013; Hung & Jen, 2012). Research on user attitudes towards information technologies has established continuance intention to use as a relevant measure of success. With regard to the significance of user attitudes for continuance intention to use, Bhattacherjee and Premkumar (2004) state that attitudes are immediate antecedents of continuance intention (Bhattacherjee & Premkumar, 2004). On the basis of these explanations, it can be anticipated that positive user attitudes towards mHealth will not only have a positive influence on user satisfaction but will also have a positive influence on the mHealth user’s continuance intention to use mHealth. Therefore, the following hypothesis should be formulated for the research model:
H8
A positive attitude towards mHealth will increase the continuation intention to use mHealth.
4.8. User satisfaction
In this investigation, user satisfaction is assumed to be the key factor for mHealth success. In the context of mHealth, the quantitative empirical studies of Akter et al. (2010), Akter, D’Ambra et al. (2013), Akter, Ray et al. (2013) and Hossain (2016) take up the endogenous construct of user satisfaction to measure mHealth success. In all these investigations, the theoretical leading concept is the IS Success Model by DeLone and McLean (1992), which theoretically justifies the construct of user satisfaction. Hossain (2016) attributes great importance to satisfaction and cites it as the following: „STF [Satisfaction] is one of the two most dominating research streams in IS and is defined as “the extent to which users believe the IS available to them meets their information requirements […]. However, over the period, the definition of STF encompasses more perspectives (than “information” only) including users’ evaluation of their overall experience with the system” (Hossain, 2016). Accordingly, user satisfaction is a decisive factor for mHealth success. Hossain (2016) sees user satisfaction as a prerequisite for the intention of users to continuously use mHealth applications. A similar argumentation can also be found in Akter, Ray et al. (2013). To this end, Akter, Ray et al. (2013) cite the following regarding the relationship between satisfaction and continuance intention to use of mHealth: “satisfaction leads to continuance intentions […]. Satisfactory experiences with a behavior are a key condition to continuance intentions as they increase one’s tendency to repeat the same course of action again and again. In the IS context, electronic service consumption offers a good illustration of the close relationship between satisfaction and continuance intentions” (Akter, Ray et al., 2013). Regarding the relationship between user satisfaction and continuance intention to use mHealth, the following hypothesis should be postulated:
H9
The user satisfaction of mHealth positively influences the continuance intention to use mHealth.
The literature contains numerous studies that empirically substantiate the importance of user satisfaction for word of mouth. In this context, Palka et al. (2009) argue: “satisfaction plays a critical role in studies of WOM [word of mouth] behavior as it affects individual motivations to recommend products or services “(Palka et al., 2009). Thus, the explanations have shown that both a positive influence on the continuance intention to use mHealth and a positive influence on the word of mouth of mHealth users can be anticipated from user satisfaction. Regarding the relationship between user satisfaction and the word of mouth of mHealth users, the following hypothesis should be postulated:
H10
The user satisfaction of mHealth positively influences the word of mouth of mHealth users.
4.9. Continuance intention to use
The continuance intention to use represents another endogenous construct for mHealth success. In the relevant mHealth literature, several quantitative empirical studies use continuance intention to use to measure the success of mHealth. For example, Akter et al. (2010), Akter, D'Ambra, and Ray (2011), Akter, Ray et al. (2013) and Hossain (2016) use continuance intention to use as an endogenous construct for measuring mHealth success. In principle, continuance intention to use describes the willingness of a user to use mHealth applications in the future. In the context of mHealth, Akter et al. (2010) define continuance intention to use as: “behavioral patterns reflecting continued use of a particular IS [information system]. It is also defined as a usage stage when IS use transcends conscious behavior and becomes part of normal routine activity” (Akter et al., 2010). Accordingly, the continuance intention to use can be described as a central construct of mHealth success, since it describes the sustainable use of the mHealth App by the user. With regard to the importance of continuance intention to use for the success of an information system, Bhattacherjee (2001) states: “long-term viability of an IS and its eventual success depend on its continued use rather than first-time use” (Bhattacherjee, 2001). Thus, it can be assumed that users’ continuance intention to use mHealth also has a positive effect on their word of mouth. With regard to the cause effect relationship between the continuance intention to use and word of mouth, Li and Liu (2011) state that continuance intention to use an IS is always regarded as a dimension of loyalty in IS domain. If IS users intend to continue using mobile services, it means they have perceived that they have received great value in their e-service encounters. They are motivated to use mobile services again and may promote these mobile services to others by WoM behavior. On the basis of these explanations, it can be anticipated that the continuance intention to use has a positive influence on the word of mouth of mHealth users. Therefore, this impact relationship should be included in the research model. The following hypothesis should be postulated for this purpose:
H11
The continuance intention to use mHealth positively influences the word of mouth of mHealth users.
4.10. Word of mouth
As the last endogenous factor for the research model, word of mouth has been identified. The word-of-mouth intention describes a user’s intention to recommend the mHealth app to other persons, e.g. family members, friends or acquaintances, or to advise against its use. The diffusion of an innovation and its establishment on the market depends on various factors, which is researched intensively in respective literature on innovation diffusion. The spreading of service innovations such as mobile health applications is often expensive and difficult due to specific customer cohort. Therefore, WoM has such an importance concerning the successful introduction of health innovations. The peer recommendation of new services plays a pivotal role as few other communication channels are available. In the scientific literature, user satisfaction is regarded as a prerequisite for a user to recommend an mHealth application (Palka et al., 2009). In addition, the scientific literature also attributes great importance to users’ continuance intention to use for their word of mouth. As an example of the importance of a user's word of mouth in attracting new users, Nelson (2017) states that the mHealth application MyFitnessPal grew to over 100 million users without paid marketing because people who used it were very satisfied and recommended it (Nelson, 2017).
The rapid growth of online communication through social media, websites, blogs, etc., has increased academic interest in word of mouth (WoM), as it influences both businesses and consumers and has become one of the most influential information sources for decision-making. And yet word of mouth is one of the oldest ways of conveying information (Dellarocas, 2003), and it has been defined in many ways. One of the earliest definitions was put forward by Katz and Lazarsfeld (1966), who described it as the exchanging of marketing information between consumers in such a way that it plays a fundamental role in shaping their behavior and in changing attitudes toward products and services. Other authors (e.g., Arndt, 1967) have suggested that WoM is a person-to-person communication tool, between a communicator and a receiver, who perceives the information received about a brand, product, or service as non-commercial. WoM is widely regarded as one of the most influential factors affecting consumer behavior and consequently one of the most important information sources in consumers’ buying decisions and intended behavior (Lee & Youn, 2009). Users generally trust other consumers more than sellers. As a result, WOM can influence many receivers and is viewed as a consumer-dominated marketing channel in which the senders are independent of the market, which lends them credibility (Brown, Broderick, & Lee, 2007).
Hence, it can be assumed that the user's word of mouth is a decisive factor for mHealth success. Thus, mHealth users’ word of mouth should be included in the research model as the final construct for mHealth success.
5. Empirical examination
5.1. Method and data
In the following, we examine the hypotheses of the research model. Thereby, the latent variables of this study were measured using multiple item scales that have been successfully tested in previous research (see Table 4). In respect to research models with latent variables and their complex interrelations, structural equation modeling has been considered an adequate method to achieve suitable results in the field of IS research (Chin, Peterson, & Brown, 2014; Hair, Hult, Ringle, & Sarstedt, 2017).
Table 4.
Items.
| Factor | Indicators | ITK-corr. | Factor load. | Cronb. A | Expl. var. | Factors extr. | Items elimin. | References |
|---|---|---|---|---|---|---|---|---|
| Perceived disease threat | I find that I can fall ill easier than others. | 0.712 | 0.724 | 0.823 | 65,661 % | 1 | 3 | Deng (2013) |
| I find that I have to put more effort into keeping good health/fitness than others. | 0.726 | 0.738 | ||||||
| I am afraid that my health may deteriorate with age. | 0.688 | 0.702 | ||||||
| I think that the mHealth app can help me to prevent future diseases. | 0.498 | 0.462 | ||||||
| Health consciousness | I take much effort to keep a good level of fitness. | 0.865 | 0.926 | 0.930 | 82,802 % | 1 | 2 | , Cho et al. (2015) |
| It is important to me to have good fitness. | 0.848 | 0.916 | ||||||
| Physical fitness is very important in my life. | 0.883 | 0.937 | ||||||
| All in all, I have a great health consciousness. | 0.759 | 0.858 | ||||||
| Personalization | The mHealth app offers me the possibility to configure the app according to my personal preferences (e.g. deactivation of pop-up messages). | 0.750 | 0.855 | 0.919 | 82,224 % | 1 | 2 | Guo et al. (2016) |
| I have no effort to customize the mHealth app to my needs. | 0.835 | 0.912, | ||||||
| The mHealth app is tailored to my needs. | 0.846 | 0.922 | ||||||
| I think that the mHealth-app is configured according to my wishes and my individual needs. | 0.872 | 0.937 | ||||||
| Interaction | For me, the mHealth app is like an interactive "personal trainer" who supports me. | 0.547 | 0.725 | 0.843 | 68,748 % | 1 | 2 | Lee, Moon, Kim, and Yi (2015) |
| The mHealth app offers interactive interfaces with communication functions (e.g. symbols, pictures or videos). | 0.592 | 0.763 | ||||||
| When I interact with the mHealth app, I can get feedback immediately. | 0.781 | 0.899 | ||||||
| All in all, I think mHealth app is very interactive | 0.812 | 0.914 | ||||||
| Mobile app design | The interface of the mHealth app is professionally designed. | 0.796 | 0.889 | 0.892 | 75,768 % | 1 | 2 | Guo et al. (2016) |
| The interface of the mHealth app is appealing. | 0.769 | 0.874 | ||||||
| The contents (e.g. the text) of the mHealth app are easy to read. | 0.723 | 0.843 | ||||||
| The mHealth app is logically structured and designed. | 0.770 | 0.875 | ||||||
| Social networking | The mHealth app allows me to share with other users. | 0.900 | 0.944 | 0.967 | 91,195 % | 1 | 2 | Pesamaa, Shoham, Khan, & Muhammad (2015) |
| The app allows me to share content with others. | 0.938 | 0.966 | ||||||
| The app allows me to make friends with other users. | 0.904 | 0.946 | ||||||
| All in all, the app allows me to network with others. | 0.934 | 0.963 | ||||||
| Attitude towards mHealth | Using a health app is a good idea for my personal health/fitness management. | 0.854 | 0.927 | 0.923 | 82,284 % | 1 | 2 | Deng (2013) |
| Using a mobile health application is a wise idea for my personal health/fitness management. | 0.878 | 0.939 | ||||||
| I find the use of a health app valuable for my personal health/fitness management. | 0.862 | 0.929 | ||||||
| All in all, I have a positive attitude towards health apps. | 0.719 | 0.830 | ||||||
| User satisfaction | The use of the mHealth app gives me pleasure. | 0.706 | 0.819 | 0.924 | 82,858 % | 1 | 2 | Akter et al. (2010), |
| I am satisfied with the functions of the mHealth app. | 0.871 | 0.935 | ||||||
| I am satisfied with the range of services offered by the mHealth app. | 0.870 | 0.939 | ||||||
| All in all, I am satisfied with the mHealth-app. | 0.883 | 0.943 | ||||||
| Word of mouth | I would recommend the mHealth app to my friends or acquaintances. | 0.714 | 0.844 | 0.924 | 77,149 % | 1 | 2 | Shaikh and Karjaluoto (2016) |
| I share my experiences with the mHealth app. | 0.706 | 0.828 | ||||||
| I would recommend the mHealth app for healthcare. | 0.785 | 0.889 | ||||||
| All in all, I think I would recommend the mHealth app to my friends | 0.887 | 0.947 | ||||||
| Continuance Intention to use | It is very likely that I will continue to use the mHealth app in the future. | 0.714 | 0.844 | 0.924 | 77,149 % | 1 | 2 | Akter (2013) |
| I am willing to continue using the mHealth app in the future. | 0.706 | 0.828 | ||||||
| I would recommend the mHealth app for healthcare. | 0.785 | 0.889 | ||||||
| All in all, I think I would recommend the mHealth app to my friends | 0.887 | 0.947 |
We used the internet community forum of one of the largest mHealth apps "MyFitnessPal", as it has been proven to have a high activity of user exchange and offers access to active mHealth users. MyFitnessPal is the second most successful mHealth app worldwide after Fitbit. It has 19 million active monthly users (Verto, 2018) and was acquired by the large American sports equipment company Under Amour in 2015. We posted a link of our survey on the forum and offered an incentive to participate in the survey: Amazon vouchers were raffled among all participants. Data collection in the “MyFitnessPal” community extended from mid-April to the end of August 2018, during which 263 fully completed questionnaires were collected.
These questionnaires were then checked for possible outliers, since for a better multivariate normal distribution in scientific literature the elimination of outliers within the sample based on Mahalanobis distances is recommended. By calculating the Mahalanobis distances eleven outliers could be identified which had to be excluded from further analysis. On closer inspection of the eliminated questionnaires, it was found that they had a noticeably short completion time compared to other questionnaires, so that it could be assumed that these participants were only interested in taking part in the competition.
After all a return of 249 valid and completed questionnaires could be achieved. In terms of methodological requirements, Chin and Newsted (1999) demand a sample larger than 200 to obtain statistically robust results (Chin & Newsted, 1999), which is the case in this research.
Since there is no database available for the specific mHealth app "MyFitnessPal" that lists all users of the app, this study must work with a partial survey or a sample selection. For this purpose, the sample selection for this investigation is determined by a random, multi-stage cluster selection. To avoid the risk of sample bias (“Selection Bias” or “Sampling Bias”), the characteristics of the sample are compared with the characteristics of the population.
The introductory first part of the online questionnaire contains questions about the individual characteristics of the respondents. For this purpose, age and gender were asked in detail. In addition, the participants were asked about their usage intensity of the mobile Internet and the mHealth app.
Regarding the distribution of the genders, it can be stated that 70.6 percent of the respondents were women and 29.4 percent men. In principle, this distribution is not unusual for mHealth apps, since they, like other health prevention measures, are used by women more than average. This distribution also almost coincides with other surveys on demography conducted by “MyFitnessPal”. In the survey by Verto (2018), the gender distribution was 74 percent women to 26 percent men.
A Chi-square homogeneity test was performed to support representativeness. The Chi-square homogeneity test yielded a value of 0.399 with degrees of freedom of 1, which is far below the 90 % quantile, which has a value of 2.71. It can therefore be stated that there is no statistically significant difference between the sample of this survey and the population of all "MyFitnessPal" users. Thus, the sample of this survey can be considered representative with regard to the gender distribution.
This can be compared to a convenience sample (Bhattacherjee, 2012, p. 69), a standard methodological approach in comparable cases (Burns & Bush, 2014; Christensen, Johnson, & Turner, 2014). Representativeness is almost impossible to achieve due to the problem of defining and finding data on the total population of mHealth users. To the best of our knowledge there is no other data on users available and thus it is difficult to test representativeness any further.
Regarding the intensity of use of the mHealth app, we asked how many hours per week the app “MyFitnessPal” is used. The results of the descriptive statistics show that 19.8 percent of the respondents use the app less than one hour per week. Most users, namely 52.8 percent, use the mHealth app for one to two hours per week. An intensity of use of three to five hours per week is shown by 21.8 percent of the respondents. The mHealth app "MyFitnessPal" is used for more than five hours a week by 5.6 percent of respondents.
Considering the characteristics of the app it can be anticipated that – despite the wide range of mHealth apps available, many users of mHealth apps have chosen “MyFitnessPal”, which unlike Fitbit is not preinstalled on new smartphones. With regard to the research questions of this study, the community of the mHealth app “MyFitnessPal” was considered an appropriate setting for the survey.
Our study uses a 7-point Likert scale ranging from “1” strongly disagree to “7” strongly agree.
The descriptive statistics show that only 2.4 % of respondents are younger than 18 years. 19.7 % are between the age of 18 years and 24 years. Furthermore, 40.2 % are between the age of 25 years and 34 years and 20.5 % are between the age of 35 years and 44 years and 11.2 % are between the age of 45 years and 54 years and only 6.0 % are older than 55 years. Only 2.4 % of respondents use mobile Internet less than 1 h per week. Furthermore, 21.3 % use mobile Internet between 2 and 4 h per week, 28.5 % use mobile Internet between 5 and 10 h per week and 47.8 % of respondents use mobile Internet more than 10 h per week.
With regard to validity and reliability of the results, we tested for systematic biases during and after the data collection as recommended by methodical literature (e.g. Chang, van Witteloostuijn, & Eden, 2010; Groves, 2004; MacKenzie, Podsakoff, & Jarvis, 2005; Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Due to the application of the specific study design regarding method and sampling, we focus on two potential biases: the nonresponse bias and common method bias. The non-response bias may occur due to a lack of information of the population’s non-responding test persons (Ruxton, 2006). In this context, we used an established approach that compares the earliest-responding survey participants with the latest-responding participants. The former are supposed to represent the responding and the latter the non-responding participants (Armstrong & Overton, 1977). In terms of the respective non-response bias test, it is assumed that the latest-responding participants are most similar to the non-respondents (Kanuk & Berenson, 1975). Therefore, we evaluated a potential existence of non-response bias by comparing early and late respondents. Thus, we conducted a Mann–Whitney-U-Test (Mann & Whitney, 1947; Ruxton, 2006). As a result, it could be shown that only slightly under 10 % of the indicators of the study showed a significant difference between the early respondents and the late respondents at the 5 % significance level. Thus, a significant influence of a non-response bias can be ruled out.
The second check for bias refers to the issue of common method. For the validation of data reliability, the potential influence of a common method bias was therefore analyzed. This type of bias does not relate to the data itself, but primarily to the survey method used. In this regard, Podsakoff and Organ (1986) explain that distortions may occur when the indicators of the exogenous and endogenous construct are assessed simultaneously by one and the same source/person: “Because both measures come from the same source, defect in that source contaminates both measures presumably in the same fashion and in the same direction” (Podsakoff & Organ, 1986, p. 533). Against this background, the calculated correlations between the exogenous and endogenous constructs may not be based on their actual relationship, but on the methodology, they share i.e., on the common method.
In addition to the precautionary measures taken to prevent distortions in terms of a common method bias, a statistical test was carried out for the subsequent verification of such a bias effect. In this context, the Harman Single-Factor Test (Harman, 1965, 1976) is a method in empirical research in which all indicators contained in the research model are examined as part of an exploratory factor analysis. In general, the result of this test indicates the rejection of a common-method bias if, and only if, several factors are extracted rather than a single factor, which explains much of the covariance between the variables (Chang et al., 2010). The evaluation of the test for the present study suggests that the existence of a common-method bias cannot be demonstrated since none of the extracted factors account for over 50 % of the total variance. Consequently, the distortion may be discarded in the sense of a common method bias.
6. Results
In the following, we present the results of our analysis. First, we can assume that the analysis of the individual measurement models shows reliable and valid indicators. Table 2 shows the inter-item correlations, which we used for our exploratory factor analysis for all exogenous success factors.
Table 2.
Inter-Item Correlations.
 |
Extraction method: Main axis factor analysis.
Rotation method: Varimax with Kaiser normalization.
Kaiser-Meyer-Olkin criterion: 0.892.
Cumulative variance of factors: 79.0.90 %.
The grey shadow indicates that the factor loadings of the individual items load most strongly on the corresponding construct.
Moreover, all constructs show acceptable levels as presented in Table 3 . After verifying the measurement models, we tested the discriminant validity by using the Fornell–Larcker criterion. The Fornell–Larcker criterion states that discriminant validity can be assumed if the average variance extracted of a construct is higher than any squared correlation with another construct (Fornell & Larcker, 1981). All exogenous factors satisfy the Fornell–Larcker criterion as stated in Table 3.
Table 3.
Fornell-Larcker.
 |
The grey numbers indicate that they are larger than all the numbers below them.
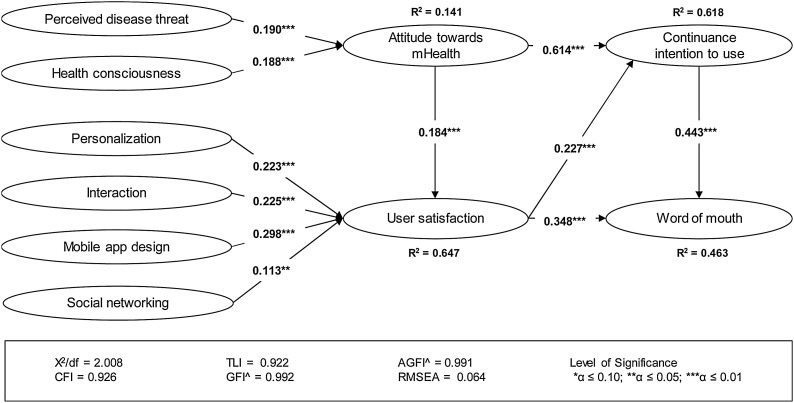
In addition, the results of the research model show an adequate fit with regard to the global quality levels, since the fit indices (CFI, GFI ^, AGFI ^, TLI and RMSEA) correspond with the values which are recommended in the scientific literature. More precisely, all values (CFI = 0.926; GFI^ = 0.992; TLI = 0.922; AGFI^ = 0.991) are above 0.9 which is the recommended value in the scientific literature (Bagozzi & Yi, 2012; Bollen & Curran, 2006; Hu & Bentler, 1999). Additionally, the RMSEA with a value of 0.064 is clearly below the critical criterion of 0.1 which is recommended by Hu and Bentler (1999). In addition, the entire research model is statistically significant and the antecedents proposed together explain more than 0,647 % (R² = 0.647) of the central endogenous variable user satisfaction of mHealth, which is regarded as a nearly substantial result according to methodological research (Chin, 1998).
Besides the global quality levels, we have examined the structural relationships of the structural model. Ten of eleven path relationships show high statistical significance. One path relationship (social networking and user satisfaction) shows moderate statistical significance. To sum up, the health-specific factors (perceived disease threat and health consciousness) have a substantial positive influence on user’s attitude towards mHealth. In addition, user’s attitude towards mHealth has a high positive influence on user satisfaction and continuance intention to use. Furthermore, the four mobile-specific factors (personalization, interaction, mobile app design and social networking) have a significant positive influence on user satisfaction. Regarding the success factors of mHealth our results show potent relationships between the endogenous factors. Especially user satisfaction has a significantly high positive influence on continuance intention to use and word of mouth. Ultimately, it can be said that also continuance intention to use has a significantly high positive influence on word of mouth. In the following, Fig. 2 shows the above-described results.
Fig. 2.
Research Results.
7. Discussion
This study investigates from the user perspective the interdependencies of the factors that determine mHealth acceptance in order to provide useful implications for research and practice. The qualitatively derived structural model is designed based on findings from the scientific literature, a qualitative content analysis of available mHealth applications, but mainly on user and expert interviews. In summary, the structural model shows that all eleven proposed hypotheses are supported, and the exogenous and endogenous factors show significant positive correlations.
The first identified core factor for mHealth success is the user's general mHealth attitude, which we define as a general feeling towards mHealth rather than a feeling towards the specific mHealth app. The studies by Cho et al. (2014) and Park (2014) related the two factors of health threat and health consciousness to a user's attitude. As far as we know, the present study is the first to empirically investigate the extent to which the combination of the two factors determine a general mHealth attitude.
Satisfaction was identified as the second core factor for mHealth success. Despite the differences in the models, this central position of the satisfaction factor is in line with studies by Hossain (2016), Cianflone et al. (2018) and Akter, D’Ambra et al. (2013). The general mHealth attitude component significantly shapes satisfaction with the app. Additional to users mHealth attitude, mobile-specific exogenous factors play a noteworthy role in the user satisfaction of mHealth apps. The design of the mobile app has a strong positive significant influence on user satisfaction. This is not surprising, as the user interface is what defines the product for users. Therefore, it is important for the user that the app is well designed and intuitive. This result is in line with the findings in the banking sector of Lee and Chuang (2009). Moreover, the interaction of the app has a strong positive impact on user satisfaction. This finding is in line with the results of research on mobile apps of Wang and Chen (2016).
In contrast to app design, interaction and personalization, social networking shows only a moderately significant influence on user satisfaction. Social networking enables the user to communicate with other users about health-related topics via mobile devices. In the age of social media, it is not surprising that social networking has a significant positive impact on user satisfaction. The comparatively low influence of the determinant social networking shows that users attach less importance to this aspect.
Regarding the endogenous success factors of mHealth, our results show that user satisfaction has a strong positive influence on Continuance Intention to Use. This result is in line with the findings of Akter, Ray et al. (2013). It can be concluded that satisfied users will continue to use the mHealth app. Furthermore, satisfied users will engage in positive word of mouth.
7.1. Theoretical contributions
The derived model differs fundamentally from conventional model theories such as the TAM, the UTAUT or the IS-Success Model. The most obvious difference lies in the definition of the construct mHealth attitude. The present study describes the construct attitude towards mHealth as a rather general mHealth-related attitude and is not referring to the attitude towards the specific app. The original TAM by Davis et al. (1989) assumes that a positive user attitude is the central determinant of actual use. In terms of the original TAM, there are two drivers that shape attitudes, perceived usefulness, and perceived ease of use, which in turn are influenced by other factors. These determinants have also been found relevant in the mHealth literature (Zhao et al., 2018).
However, in addition to these basic technology-related determinants, health-specific factors can also be expected to influence users' overall attitudes toward using mHealth apps (Cho et al., 2014; Deng, 2013). Accordingly, user attitudes cannot be derived exclusively from the mHealth app provided, but additionally from the user's basic attitude toward his or her own health. As a result, in addition to the technology-related aspects (usefulness and ease of use), one could simply include the health-consciousness-related factors. However, such an approach would overlap with examining the construct of satisfaction with the app and the potential influence of different characteristics.
While the TAM assumes that users’ attitudes are fundamentally shaped by the specific technology, we now separate technology-related attitudes and use the term attitude only for basic mHealth-related attitudes. Technology- and app-related attitudes are examined by examining satisfaction and its determinants. This differentiation is the result of the survey of users and experts in the field of mHealth and allows a clear distinction. However, this differentiation deviates from the understanding of the original TAM, which uses the term user attitude to mean, in particular, the attitude toward the specific technology.
Against this background, the model consisting of the two central units attitude and satisfaction is clearly distinguishable from conventional model theories. This approach is a fundamental contribution that also stands up to empirical scrutiny. However, the coefficient of determination for our conceptualization of the construct user attitude shows that it is less clearly shaped by its two determinants than the construct satisfaction by its four determinants.
7.2. Implications for practice
The derived model is also important in practical applications, as it explains empirically tested relationships that can also be the basis for business decisions. The four endogenous variables (user attitude, satisfaction, continuance intention to use, WoM) can be important success factors for the introduction and operation of health applications. Knowing the drivers of these success factors helps companies allocate their resources accordingly.
In the context of the model, the construct user attitude is determined by fundamental health factors. However, it is evident that a comparatively low R2 suggests further determinants. For companies, basic health factors such as health awareness and a high sensitivity to threats cannot be directly influenced. However, it can be deduced from this that changes in perception, for example as a result of a pandemic, certainly influence the success of mHealth offerings.
Unlike basic health awareness, satisfaction can certainly be changed by working on the given determinants. The model shows, for example, that the social media factor is less relevant for user satisfaction than the factors personalization, interaction, and design. Looking at the comparatively high R2 of the satisfaction construct, it can be concluded that the four exogenous factors strongly explain user satisfaction.
In addition to the study's interesting results from a business perspective, the study creates a general understanding of the relationships between mHealth acceptance and success. Especially in times of the global SARS-CoV 2 or COVID-19 pandemic, mHealth applications have gained a special importance. They are seen as one of the solutions for better early indication. At the same time, different countries have been working separately on public health apps, noting that one of the challenges is public acceptance for their use. Against this background, identifying the key drivers of mHealth apps, as achieved in this study, is of particular importance.
As an interim conclusion, mHealth practitioners should consider the confirmed antecedents of personalization, interaction, mobile app design, and social networking as a whole to assess the achievement of user satisfaction, because user satisfaction leads to continued intent to use and word of mouth.
7.3. Limitations and future research direction
Despite the careful conceptual and methodological design of the study, it also comes with some limitations. First, we only surveyed German mHealth users of a specific mHealth community in our study. This entails a possible selection bias. Future research should therefore extend the study to other communities, countries, cultural backgrounds, and nationalities. Second, because our study examines only a specific period, we encourage researchers to conduct multiyear and replication studies to approach generalization of our findings. Third, future research should focus on other mHealth services such as wearables or smartwatches. In addition, future research should also address privacy and data security in the mHealth context. There is serious criticism of the use of personal data for a central assessment of citizens, which also plays an important role in the context of mHealth, as mHealth applications allow detailed citizen profiles to be created based on location-based data (Langer, 2020; Kurtz, Wirtz, & Langer, 2021). Despite these specific limitations, the literature still lacks research on other factors that determine mHealth adoption, such as privacy concerns, opaque mHealth business models, and location-based services. Future studies should address these concerns. Furthermore, the model only considers direct effects between factors but does not examine possible moderating effects. Future research should address possible boundary conditions for the relationships.
8. Conclusions
Based on a multimethod approach and with reference to findings from previous research, an analysis of actual mHealth offerings and, not least, extensive interviews with users and experts, the present study has developed a structural model that in many respects does not correspond to conventional theory.
This difference is due to the attempt to view attitude as a fundamental health attitude and not as a product-related attitude. This is the only way to clearly differentiate the construct of satisfaction, which deals with the product and its features.
In terms of theory, the present study thus provides a conceptual framework that requires further theoretical elaboration and empirical testing. Yet, the derived structural model has already withstood a first empirical test based on a survey of German mHealth app users. The specific context as well as broad limitations of the study provide a rough framework for future research.
CRediT authorship contribution statement
Steven Birkmeyer: Conceptualization, Methodology, Writing - original draft, Project administration. Bernd W. Wirtz: Supervision. Paul F. Langer: Resources, Writing - review & editing.
Biographies
Dr. Steven Birkmeyer is a researcher at the German University of Administrative Sciences Speyer, Germany. He is especially interested in marketing and mobile health services.
Professor Dr. Bernd W. Wirtz holds the Chair for Information and Communication Management at the German University of Administrative Sciences Speyer. Recently, he published studies on electronic procurement in public administration and the acceptance of electronic health cards in Germany. Furthermore his research interests include social media, e-business and e-government. His textbooks deal with electronic business, business model management and media- and internet management.
Mr. Paul F. Langer is a research associate and PhD candidate at the Chair for Information and Communication Management at the German University of Administrative Sciences Speyer, Germany. His main research interests are innovation diffusion, platform economics and cloud computing.
References
- Agarwal S., LeFevre A.E., Lee J., L’Engle K., Mehl G., Sinha C., Labrique A. Guidelines for reporting of health interventions using mobile phones: Mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ (Clinical Research Edition) 2016;352:i1174. doi: 10.1136/bmj.i1174. [DOI] [PubMed] [Google Scholar]
- Akter S., D’Ambra J., Ray P. Service quality of mHealth platforms: Development and validation of a hierarchical model using PLS. Electronic Markets. 2010;20(3-4):209–227. doi: 10.1007/s12525-010-0043-x. [DOI] [Google Scholar]
- Akter S., D'Ambra J., Ray P. Trustworthiness in mHealth information services: An assessment of a hierarchical model with mediating and moderating effects using partial least squares (PLS) Journal of the American Society for Information Science and Technology. 2011;62(1):100–116. [Google Scholar]
- Akter S., D'Ambra J., Ray P. Development and validation of an instrument to measure user perceived service quality of mHealth. Information and Management. 2013;50(4):181–195. [Google Scholar]
- Akter S., D’Ambra J., Ray P., Hani U. Modelling the impact of mHealth service quality on satisfaction, continuance and quality of life. Behaviour & Information Technology. 2013;32(12):1225–1241. doi: 10.1080/0144929X.2012.745606. [DOI] [Google Scholar]
- Akter S., Ray P., D’Ambra J. Continuance of mHealth services at the bottom of the pyramid: The roles of service quality and trust. Electronic Markets. 2013;23(1):29–47. doi: 10.1007/s12525-012-0091-5. [DOI] [Google Scholar]
- Armstrong J.S., Overton T.S. Estimating nonresponse bias in mail surveys. Journal of Marketing Research. 1977;14(3):396–402. doi: 10.1177/002224377701400320. [DOI] [Google Scholar]
- Arndt J. Role of product-related conversations in the diffusion of a new product. Journal of Marketing Research. 1967;4(3):291–295. doi: 10.1177/002224376700400308. [DOI] [Google Scholar]
- Bagozzi R.P., Yi Y. Specification, evaluation, and interpretation of structural equation models. Journal of the Academy of Marketing Science. 2012;40(1):8–34. doi: 10.1007/s11747-011-0278-x. [DOI] [Google Scholar]
- Baldwin J.L., Singh H., Sittig D.F., Giardina T.D. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other. Healthcare (Amsterdam, Netherlands) 2017;5(3):81–85. doi: 10.1016/j.hjdsi.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baulch E., Watkins J., Tariq A. Mobile communication in Asia. mHealth innovation in Asia: Grassroots challenges and practical interventions. Springer Netherlands; Dordrecht: 2018. Introduction: Social and cultural futures—The everyday use and shifting discourse of mHealth; pp. 1–6. [DOI] [Google Scholar]
- Bhattacherjee A. Understanding information systems continuance: An expectation-confirmation model. MIS Quarterly. 2001;25(3):351–370. doi: 10.2307/3250921. [DOI] [Google Scholar]
- Bhattacherjee A. 2nd ed. CreateSpace Independent Publishing; Tampa: 2012. Social science research. [Google Scholar]
- Bhattacherjee A., Premkumar G. Understanding changes in belief and attitude toward information technology usage: A theoretical model and longitudinal test. MIS Quarterly. 2004;28(2):229–254. doi: 10.2307/25148634. [DOI] [Google Scholar]
- Bollen K.A., Curran P.J. Wiley-Interscience; Hoboken, N.J: 2006. Latent curve models: A structural equation perspective. Wiley series in probability and statistics.http://site.ebrary.com/lib/alltitles/docDetail.action?docID=10300097 Retrieved from. [Google Scholar]
- Borrelli B., Ritterband L.M. Special issue on eHealth and mHealth: Challenges and future directions for assessment, treatment, and dissemination. Health Psychology. 2015;34S:1205–1208. doi: 10.1037/hea0000323. [DOI] [PubMed] [Google Scholar]
- Brannen J. 2005. Mixed methods research: A discussion paper. [Google Scholar]
- Brown J., Broderick A.J., Lee N. Word of mouth communication within online communities: Conceptualizing the online social network. Journal of Interactive Marketing. 2007;21(3):2–20. doi: 10.1002/dir.20082. [DOI] [Google Scholar]
- Burns A.C., Bush R.F. 7th ed. Pearson; Boston: 2014. Marketing research. [Google Scholar]
- Butt M., Aftab M. Incorporating attitude towards Halal banking in an integrated service quality, satisfaction, trust and loyalty model in online Islamic banking context. International Journal of Bank Marketing. 2013;31(1):6–23. doi: 10.1108/02652321311292029. [DOI] [Google Scholar]
- Chang S.‑J., van Witteloostuijn A., Eden L. From the Editors: Common method variance in international business research. Journal of International Business Studies. 2010;41(2):178–184. doi: 10.1057/jibs.2009.88. [DOI] [Google Scholar]
- Chaniotakis I.E., Lymperopoulos C. Service quality effect on satisfaction and word of mouth in the health care industry. Managing Service Quality. 2009;19(2):229–242. doi: 10.1108/09604520910943206. [DOI] [Google Scholar]
- Chin W.W. In: Modern methods for business research. Marcoulides G., editor. Lawrence Erlbaum Associates; New York: 1998. The partial least squares approach to structural equation modeling; pp. 295–336. [Google Scholar]
- Chin W.W., Newsted P.R. In: Statistical strategies for small sample research. Hoyle R.H., editor. CA: Sage Publications; Thousand Oaks: 1999. Structural equation modeling analysis with small samples using partial least squares; pp. 307–341. [Google Scholar]
- Chin W.W., Peterson R.A., Brown S.P. Structural equation modeling in marketing: Some practical reminders. The Journal of Marketing Theory and Practice. 2014;16(4):287–298. doi: 10.2753/MTP1069-6679160402. [DOI] [Google Scholar]
- Cho J., Lee H.E., Kim S.J., Park D. Effects of body image on college students’ attitudes toward diet/fitness apps on smartphones. Cyberpsychology, Behavior and Social Networking. 2015;18(1):41–45. doi: 10.1089/cyber.2014.0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho J., Park D., Lee H.E. Cognitive factors of using health apps: Systematic analysis of relationships among health consciousness, health information orientation, eHealth literacy, and health app use efficacy. Journal of Medical Internet Research. 2014;16(5):e125. doi: 10.2196/jmir.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen L.B., Johnson B., Turner L.A. twelfth edition. Pearson; Boston: 2014. Research methods, design, and analysis. [Google Scholar]
- Cianflone D., Omboni S., Alessa T., Abdi S., Hawley M.S., de Witte L. Mobile apps to support the self-management of hypertension: Systematic review of effectiveness, usability, and user satisfaction. JMIR MHealth and UHealth. 2018;6(7) doi: 10.2196/10723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis F.D., Bagozzi R.P., Warshaw P.R. User acceptance of computer technology: A comparison of two theoretical models. Management Science. 1989;35(8):982–1003. doi: 10.1287/mnsc.35.8.982. [DOI] [Google Scholar]
- Dellarocas C. The digitization of word of mouth: Promise and challenges of online feedback mechanisms. Management Science. 2003;49(10):1407–1424. doi: 10.1287/mnsc.49.10.1407.17308. [DOI] [Google Scholar]
- DeLone W.H., McLean E.R. Information systems success: The quest for the dependent variable. Information Systems Frontiers. 1992;3(1):60–95. doi: 10.1287/isre.3.1.60. [DOI] [Google Scholar]
- Deng Z. Understanding public users’ adoption of mobile health service. International Journal of Mobile Communications. 2013;11(4):351. doi: 10.1504/IJMC.2013.055748. [DOI] [Google Scholar]
- Dicianno B.E., Parmanto B., Fairman A.D., Crytzer T.M., Yu D.X., Pramana G.…Petrazzi A.A. Perspectives on the evolution of mobile (mHealth) technologies and application to rehabilitation. Physical Therapy. 2015;95(3):397–405. doi: 10.2522/ptj.20130534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwivedi Y.K., Rana N.P., Janssen M., Lal B., Williams M.D., Clement M. An empirical validation of a unified model of electronic government adoption (UMEGA) Government Information Quarterly. 2017;34(2):211–230. [Google Scholar]
- Dwivedi Y.K., Rana N.P., Jeyaraj A., Clement M., Williams M.D. Re-examining the unified theory of acceptance and use of technology (UTAUT): Towards a revised theoretical model. Information Systems Frontiers. 2019;21(3):719–734. [Google Scholar]
- Dwivedi Y.K., Rana N.P., Tamilmani K., Raman R. A meta-analysis based modified unified theory of acceptance and use of technology (meta-UTAUT): A review of emerging literature. Current Opinion in Psychology. 2020;36:13–18. doi: 10.1016/j.copsyc.2020.03.008. [DOI] [PubMed] [Google Scholar]
- Dwivedi Y.K., Shareef M.A., Simintiras A.C., Lal B., Weerakkody V. A generalised adoption model for services: A cross-country comparison of mobile health (m-health) Government Information Quarterly. 2016;33(1):174–187. doi: 10.1016/j.giq.2015.06.003. [DOI] [Google Scholar]
- Fan H., Poole M.S. What is personalization?: Perspectives on the design and implementation of personalization in information systems. Journal of Organizational Computing and Electronic Commerce. 2006;16(3-4):179–202. doi: 10.1080/10919392.2006.9681199. [DOI] [Google Scholar]
- Fornell C., Larcker D.F. Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research. 1981;18(1):39–50. doi: 10.2307/3151312. [DOI] [Google Scholar]
- Greene J.C., Caracelli V.J., Graham W.F. Toward a conceptual framework for mixed-method evaluation designs. Educational Evaluation and Policy Analysis. 1989;11(3):255–274. [Google Scholar]
- Grimsley M., Meehan A. e-Government information systems: Evaluation-led design for public value and client trust. European Journal of Information Systems. 2007;16(2):134–148. [Google Scholar]
- Groves R.M. John Wiley & Sons; 2004. Survey errors and survey costs. [Google Scholar]
- Guo X., Zhang X., Sun Y. The privacy–personalization paradox in mHealth services acceptance of different age groups. Electronic Commerce Research and Applications. 2016;16:55–65. doi: 10.1016/j.elerap.2015.11.001. [DOI] [Google Scholar]
- Gupta P., Harris J. How e-WOM recommendations influence product consideration and quality of choice: A motivation to process information perspective. Journal of Business Research. 2010;63(9-10):1041–1049. doi: 10.1016/j.jbusres.2009.01.015. [DOI] [Google Scholar]
- Hair J.F., Hult G.T.M., Ringle C.M., Sarstedt M. second edition. SAGE; Los Angeles, London, New Delhi, Singapore, Washington DC, Melbourne: 2017. A primer on partial least squares structural equation modeling (PLS-SEM) [Google Scholar]
- Harman G.H. The inference to the best explanation. The Philosophical Review. 1965;74(1):88–95. doi: 10.2307/2183532. [DOI] [Google Scholar]
- Harman H.H. University of Chicago Press; 1976. Modern factor analysis. [Google Scholar]
- Ho V.T., Ang S., Straub D. When subordinates become IT contractors: Persistent managerial expectations in IT outsourcing. Information Systems Research. 2003;14(1):66–86. [Google Scholar]
- Hoque R., Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. International Journal of Medical Informatics. 2017;101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002. [DOI] [PubMed] [Google Scholar]
- Hossain M. Assessing m-Health success in Bangladesh. Journal of Enterprise Information Management. 2016;29(5):774–796. doi: 10.1108/JEIM-02-2014-0013. [DOI] [Google Scholar]
- Hu L., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huang X., Dong K., Wu J. In: Chen H., Fang Q., Zeng D., Wu J., editors. Vol. 10983. Springer International Publishing; Cham: 2018. Evolution of research on smart health: A bibliometrics analysis; pp. 351–358. (Lecture notes in computer science. Smart health). [DOI] [Google Scholar]
- Hung M.‑C., Jen W.‑Y. The adoption of mobile health management services: An empirical study. Journal of Medical Systems. 2012;36(3):1381–1388. doi: 10.1007/s10916-010-9600-2. [DOI] [PubMed] [Google Scholar]
- Hussain M., Zaidan A.A., Zidan B.B., Iqbal S., Ahmed M.M., Albahri O.S., Albahri A.S. Conceptual framework for the security of mobile health applications on Android platform. Telematics and Informatics. 2018;35(5):1335–1354. doi: 10.1016/j.tele.2018.03.005. [DOI] [Google Scholar]
- Irma Becerra-Fernandez R.S. Organizational knowledge management: A contingency perspective. Journal of Management Information Systems. 2001;18(1):23–55. [Google Scholar]
- Kanuk L., Berenson C. Mail surveys and response rates: A literature review. Journal of Marketing Research. 1975;12(4):440–453. doi: 10.2307/3151093. [DOI] [Google Scholar]
- Katz E., Lazarsfeld P.F. Transaction publishers.; 1966. Personal Influence, the part played by people in the flow of mass communications. [Google Scholar]
- Kurtz O.T., Wirtz B.W., Langer P.F. An empirical analysis of location-based mobile advertising—Determinants, success factors, and moderating effects. Journal of Interactive Marketing. 2021;54:69–85. doi: 10.1016/j.intmar.2020.08.001. [DOI] [Google Scholar]
- Langer P.F. Lessons from China-The Formation of a Social Credit System: Profiling, Reputation Scoring, Social Engineering. The 21st Annual International Conference on Digital Government Research. 2020:164–174. doi: 10.1145/3396956.3396962. [DOI] [Google Scholar]
- Larios Hernández G.J. In: Palgrave pivot. Reverse entrepreneurship in Latin America: Internationalization from emerging markets to developed economies. Reyes-Mercado P., Larios Hernández G.J., editors. Palgrave Macmillan; Cham: 2019. Wearable technology: Shaping market opportunities through innovation, learning, and networking; pp. 29–44. [DOI] [Google Scholar]
- Lee T.H. A structural model to examine how destination image, attitude, and motivation affect the future behavior of tourists. Leisure Sciences. 2009;31(3):215–236. doi: 10.1080/01490400902837787. [DOI] [Google Scholar]
- Lee K., Chuang N. Understanding factors affecting trust in and satisfaction with mobile banking in Korea: A modified DeLone and McLean’s model perspective. Interacting with Computers. 2009;21(5-6):385–392. doi: 10.1016/j.intcom.2009.06.004. [DOI] [Google Scholar]
- Lee M., Youn S. Electronic word of mouth (eWOM) How eWOM platforms influence consumer product judgement. International Journal of Advertising. 2009;28(3):473–499. [Google Scholar]
- Lee M.K.O., Shi N., Cheung C.M.K., Lim K.H., Sia C.L. Consumer’s decision to shop online: The moderating role of positive informational social influence. Information & Management. 2011;48(6):185–191. [Google Scholar]
- Lee D., Moon J., Kim Y., Yi M. Antecedents and consequences of mobile phone usability: Linking simplicity and interactivity to satisfaction, trust, and brand loyalty. Information & Management. 2015;52(3):295–304. [Google Scholar]
- Legris P., Ingham J., Collerette P. Why do people use information technology? A critical review of the technology acceptance model. Information & Management. 2003;40(3):191–204. doi: 10.1016/S0378-7206(01)00143-4. [DOI] [Google Scholar]
- Li H., Liu Y. Post adoption behaviour of e-service users: An empirical study on chinese online travel service users. ECIS 2011 Proceedings. 2011:56. [Google Scholar]
- Liu F., Ngai E., Ju X. Understanding mobile health service use: An investigation of routine and emergency use intentions. International Journal of Information Management. 2019;45:107–117. doi: 10.1016/j.ijinfomgt.2018.09.004. [DOI] [Google Scholar]
- Luxton D.D., McCann R.A., Bush N.E., Mishkind M.C., Reger G. 2011. mHealth for mental health: Integrating smartphone technology in behavioral healthcare.https://pdfs.semanticscholar.org/66e5/d4bab20d0f8ed4c2299c8ec2e940aa09d03b.pdf Retrieved from. [Google Scholar]
- MacKenzie S.B., Podsakoff P.M., Jarvis C.B. The problem of measurement model misspecification in behavioral and organizational research and some recommended solutions. The Journal of Applied Psychology. 2005;90(4):710–730. doi: 10.1037/0021-9010.90.4.710. [DOI] [PubMed] [Google Scholar]
- Mann H.B., Whitney D.R. On a test of whether one of two random variables is stochastically larger than the other. The Annals of Mathematical Statistics. 1947:50–60. [Google Scholar]
- Marwah S., Mittal P. M-health for maternal health- bridging the gaps!! International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2017;7(1):1–4. doi: 10.18203/2320-1770.ijrcog20175822. [DOI] [Google Scholar]
- Mayring P. Vol. 1. 2004. Qualitative content analysis; pp. 159–176. (A companion to qualitative research). (2004) [Google Scholar]
- Mohr D.C., Schueller S.M., Montague E., Burns M.N., Rashidi P. The behavioral intervention technology model: An integrated conceptual and technological framework for eHealth and mHealth interventions. Journal of Medical Internet Research. 2014;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorhead S.A., Hazlett D.E., Harrison L., Carroll J.K., Irwin A., Hoving C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. Journal of Medical Internet Research. 2013;15(4):e85. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson T.‑N. 1 edition. Berrett-Koehler Publishers; Oakland, CA: 2017. The transformational consumer: Fuel a lifelong love affair with your customers by helping them get healthier, wealthier and wiser. [Google Scholar]
- Nisha N., Iqbal M., Rifat A., Idrish S. Mobile health services. International Journal of Asian Business and Information Management. 2015;6(1):1–17. [Google Scholar]
- Nysveen H., Pedersen P.E., Thorbjørnsen H. Explaining intention to use mobile chat services: Moderating effects of gender. The Journal of Consumer Marketing. 2005;22(5):247–256. doi: 10.1108/07363760510611671. [DOI] [Google Scholar]
- Okazaki S., Castañeda J., Sanz S., Henseler J. Physicians' appraisal of mobile health monitoring. Service Industries Journal. 2013;33(13/14):1326–1344. [Google Scholar]
- Okoli C., Pawlowski S.D. The Delphi method as a research tool: An example, design considerations and applications. Information & Management. 2004;42(1):15–29. [Google Scholar]
- Palka W., Pousttchi K., Wiedemann D.G. Mobile word-of-mouth – A grounded theory of mobile viral marketing. Journal of Information Technology. 2009;24(2):172–185. doi: 10.1057/jit.2008.37. [DOI] [Google Scholar]
- Park J.‑H. The effects of personalization on user continuance in social networking sites. Information Processing & Management. 2014;50(3):462–475. doi: 10.1016/j.ipm.2014.02.002. [DOI] [Google Scholar]
- Pesämaa O., Shoham A., Khan M., Muhammad I. The impact of social networking and learning orientation on performance. Journal of Global Marketing. 2015;28(2):113–131. [Google Scholar]
- Podsakoff P.M., Organ D.W. Self-reports in organizational research: Problems and prospects. Journal of Management. 1986;12(4):531–544. doi: 10.1177/014920638601200408. [DOI] [Google Scholar]
- Podsakoff P.M., MacKenzie S.B., Lee J.‑Y., Podsakoff N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. The Journal of Applied Psychology. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Rosenstock I.M., Strecher V.J., Becker M.H. In: Preventing aids: Theories and methods of behavioral interventions. DiClemente R.J., Peterson J.L., editors. Springer; New York: 2013. The health belief model and HIV risk behavior change; pp. 5–24. [DOI] [Google Scholar]
- Ruxton G.D. The unequal variance t-test is an underused alternative to Student’s t-test and the Mann–Whitney U test. Behavioral Ecology. 2006;17(4):688–690. doi: 10.1093/beheco/ark016. [DOI] [Google Scholar]
- Sezgin E., Özkan-Yildirim S., Yildirim S. Understanding the perception towards using mHealth applications in practice. Information Development. 2018;34(2):182–200. [Google Scholar]
- Shaikh A., Karjaluoto H. Mobile Banking Services Continuous Usage -- Case Study of Finland. Proceedings of the 49th Annual Hawaii International Conference on System Sciences; Piscataway, NJ; 2016. 5-8 January 2016, Kauai, Hawaii, T.X. Bui und R.H. Sprague (Hrsg.) [Google Scholar]
- Shareef M., Kumar V., Kumar U. Predicting mobile health adoption behaviour: A demand side perspective. Journal of Customer Behaviour. 2014;13(3):187–205. [Google Scholar]
- Stewart R. 2018. Identifying barriers that affect patients access to their patient portals and MHealth applications.https://dc.uthsc.edu/cgi/viewcontent.cgi?article=1054&context=hiimappliedresearch Retrieved from. [Google Scholar]
- Sun P.‑C., Tsai R., Finger G., Chen Y.‑Y., Yeh D. What drives a successful e-Learning? An empirical investigation of the critical factors influencing learner satisfaction. Computers & Education. 2008;50(4):1183–1202. doi: 10.1016/j.compedu.2006.11.007. [DOI] [Google Scholar]
- Sun Y., Wang N., Guo X., Peng Z. Understanding the acceptance of mobile health services : A comparison and integration of alternative models. Journal of Electronic Commerce Research. 2013;14(2):183–200. [Google Scholar]
- Tang J., Abraham C., Stamp E., Greaves C. How can weight-loss app designers’ best engage and support users? A qualitative investigation. British Journal of Health Psychology. 2015;20(1):151–171. doi: 10.1111/bjhp.12114. [DOI] [PubMed] [Google Scholar]
- Tarkang E.E., Zotor F.B. Application of the health belief model (HBM) in HIV prevention: A literature review. Central African Journal of Public Health. 2015;1(1):1–8. doi: 10.11648/j.cajph.20150101.11. [DOI] [Google Scholar]
- Tashakkori A., Creswell J.W. Sage Publications; 2007. The new era of mixed methods. [Google Scholar]
- Tomlinson M., Rotheram-Borus M.J., Swartz L., Tsai A.C. Scaling up mHealth: where is the evidence? PLoS Medicine. 2013;10(2) doi: 10.1371/journal.pmed.1001382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Heerden A., Tomlinson M., Swartz L. Point of care in your pocket: A research agenda for the field of m-health. Bulletin of the World Health Organization. 2012;90:393–394. doi: 10.2471/BLT.11.099788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh V., Davis F.D. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Management Science. 2000;46(2):186–204. doi: 10.1287/mnsc.46.2.186.11926. [DOI] [Google Scholar]
- Venkatesh V., Brown S.A., Bala H. Bridging the qualitative-quantitative divide: Guidelines for conducting mixed methods research in information systems. MIS Quarterly. 2013:21–54. [Google Scholar]
- Venkatesh V., Morris M.G., Davis G.B., Davis F.D. User acceptance of information technology: Toward a unified view. MIS Quarterly. 2003:425–478. doi: 10.2307/30036540. [DOI] [Google Scholar]
- Verto . 2018. Verto index: Health and fitness app.https://vertoanalytics.com/verto-index-health-fitness/ Retrieved from. [Google Scholar]
- Vervier L., Valdez A., Ziefle M. “Attitude”- mHealth Apps and Users’ Insights: An Empirical Approach to Understand the Antecedents of Attitudes towards mHealth Applications. Proceedings of the 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health. 2019 [Google Scholar]
- Wang W.‑T., Chen W.‑Y., editors. Assessing the effects of mobile service quality on customer satisfaction and the continued usage intention of mobile service: A study of non-gaming mobile apps: Cross-cultural design. Springer International Publishing; 2016. [Google Scholar]
- Wirtz B.W., Birkmeyer S., Langer P.F. International review of administrative sciences. Advance online publication; 2019. Citizens and mobile government: An empirical analysis of the antecedents and consequences of mobile government usage. [DOI] [Google Scholar]
- Wixom B.H., Todd P.A. A theoretical integration of user satisfaction and technology acceptance. Information Systems Research. 2005;16(1):85–102. http://www.jstor.org/stable/23015766 Retrieved from. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2011. Mhealth: Second global survey on eHealth.http://gbv.eblib.com/patron/FullRecord.aspx?p=851142 Retrieved from. [Google Scholar]
- World Health Organization . 2018. mHealth: Use of appropriate digital technologies for public health.http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_20-en.pdf Retrieved from. [Google Scholar]
- Wu J.-H., Wang S.-C., Lin L.-M. Mobile computing acceptance factors in the healthcare industry: a structural equation model. International Journal of Medical Informatics. 2007;76(1):66–77. doi: 10.1016/j.ijmedinf.2006.06.006. [DOI] [PubMed] [Google Scholar]
- Zhao Y., Ni Q., Zhou R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. International Journal of Information Management. 2018;43:342–350. doi: 10.1016/j.ijinfomgt.2017.08.006. [DOI] [Google Scholar]
- Zhang X., Guo X., Lai K., Guo F., Li C. Understanding gender differences in m-health adoption: a modified theory of reasoned action model. Telemedicine journal and e-health: the official journal of the American Telemedicine Association. 2014;20(1):39–46. doi: 10.1089/tmj.2013.0092. [DOI] [PubMed] [Google Scholar]