Abstract
The coronavirus disease (COVID-19) has dramatically altered daily activities including eating and physical activity behaviors, which in turn may be related to eating pathology. Those who care for children (henceforth caregivers) may face the brunt of these changes, but little research has examined the consequences of COVID-19 on eating pathology in caregivers. A community sample of caregivers (N = 140) completed a cross-sectional online survey assessing demographics, stress and concern about weight gain before/during COVID-19, disordered eating (Eating Disorder Examination Questionnaire-Short Form), and emotional eating (Emotional Eating Scale-Revised). Significant positive relationships emerged between stress and concern about weight gain before/during COVID-19 and disordered eating, emotional eating-depression, emotional eating-anger/anxiety, and emotional eating-boredom. Stress and concern about weight gain during, but not before, COVID-19 positively predicted variance in disordered eating and emotional eating. Stress was associated with lower emotional eating-boredom when concern about weight gain during COVID-19 was low. Stress was associated with lower emotional eating-depression when concern about weight gain before COVID-19 was low, but when high, stress was associated with higher emotional eating-depression. Stress and concern about weight gain before/during COVID-19 may be relevant to worsened disordered eating and emotional eating in caregivers, a neglected population in the literature. Targeting concern about weight gain may weaken the relationship between stress and emotional eating-depression and emotional eating-boredom among caregivers in the context of the COVID-19 pandemic.
Keywords: Coronavirus, COVID-19, Disordered eating, Emotional eating, Stress, Concern about weight gain, Caregivers
1. Introduction
Following the emergence and spread of the coronavirus disease (COVID-19), public health policies were adopted to mitigate its impact on global health. These policies (e.g., public school and childcare closures, travel restrictions) immediately impacted routines of caregivers responsible for young children. Many parents and guardians (henceforth caregivers) faced unemployment, financial uncertainty, food insecurity, increased childcare needs, and myriad other stressors related to COVID-19 (Fontanesi et al., 2020; Patrick et al., 2020). Not surprisingly, changes also emerged for both eating behaviors and physical activity during COVID-19 (Martínez-de-Quel, Suárez-Iglesias, López-Flores, & Pérez, 2021; Tison et al., 2020). These dramatic alterations in daily routine, especially those around eating behaviors, may exacerbate disordered eating (DE) at both clinical and non-clinical levels.
For example, individuals with anorexia nervosa and bulimia nervosa reported worsened binge eating (Phillipou et al., 2020), compensatory exercise (Castellini et al., 2020), drive for physical activity, and shape and weight concerns (Schlegl, Maier, Meule, & Voderholzer, 2020) during COVID-19. Populations with non-clinical DE may also be at risk for worsened outcomes during COVID-19 such as skipping meals and fasting (Khubchandani, Kandiah, & Saiki, 2020), overeating (Owen, Tran, Hammarberg, Kirkman, & Fisher, 2020), and binge eating (Phillipou et al., 2020). COVID-19 may also present new barriers to DE treatment such as difficulty monitoring clients with severe pathology and increased burden on family members involved in eating disorder care (Fernandez-Aranda et al., 2020). Initial findings suggest that some adults with eating pathology experienced a loss of or decreased quality of therapeutic support during the pandemic (Vullier et al., 2021). Thus, it is important for research to examine correlates of DE during COVID-19 to add information on potential treatement targets.
Two such correlates may be stress and concern about weight gain, both of which may be heightened during COVID-19. Indeed, COVID-19 has drastically changed daily routines including stressful alterations in eating behaviors and mealtimes, limited ability to exercise due to gym closures, and increased childcare responsibilities. Furthermore, altered eating behaviors and physical activity may provoke higher concern about weight gain during COVID-19. Because COVID-19 has introduced novel challenges that may uniquely impact stress and concern about weight gain, research is needed to map their relationships with DE in caregivers. Adults in multiple countries reported more instances of eating out of control, snacks between meals, and number of main meals each day during their lockdown periods (Ammar et al., 2020). The little data that targets caregiver experiences show higher odds of overeating and a more severe impact on daily living during lockdown for caregivers (Owens et al., 2020). Of note, this same study identified that in addition to caregivers, those living alone, without a partner, those worried about COVID-19 contraction, and those self-reporting adverse impacts of the pandemic also displayed higher odds of maladaptive eating behaviors and negative consequences on daily living (Owens et al., 2020). Thus, the impacts of the COVID-19 pandemic on eating behaviors cut across diverse groups of people, including caregivers. Taken together, stress and concern about weight gain during COVID-19 may introduce added challenges to those presenting DE symptoms, and may be exacerbated for caregivers who face the brunt of these challenges.
Another eating phenotype potentially impacted by stress and concern about weight gain is emotional eating (EE). EE, or the urge to eat in response to negative emotions in the absence of hunger (Arnow, Kenardy, & Agras, 1995), is positively associated with DE attitudes, cognitions, and behaviors across diverse symptom presentations (Barnhart, Braden, & Jordan, 2020; Barnhart, Braden, & Price, 2021; Braden, Musher-Eizenman, Watford, & Emley, 2018; Duarte & Pinto-Gouveia, 2015; Fischer et al., 2007; Ricca et al., 2012). Furthermore, EE is positively related to stress (Oliver, Wardle, & Gibson, 2000), concern about weight gain (Belcher et al., 2011), and appears to be elevated during COVID-19 (Elmacioğlu, Emiroğ; Al-Musharaf, 2020); however, no research to date has explored relationships among these constructs with specific EE types like EE-depression, EE-anger/anxiety, and EE-boredom as outcomes (Arnow et al., 1995; Koball, Meers, Storfer-Isser, Domoff, & Musher-Eizenman, 2012). Examining such emotional states may be especially relevant in a sample of caregivers, as previous findings indicate parents have experienced increased negative affect (Janssen et al., 2020), generally worsened mental health outcomes (Patrick et al., 2020), and even thoughts of death or self-harm since the declaration of COVID-19 as a global pandemic (Crasta, Daks, & Rogge, 2020). Importantly, each of these aversive emotional states may be heightened during COVID-19, revealing a unique opportunity for research to better discern the role of the pandemic on these specific types of EE and DE. To add information to the eating pathology literature on this underrepresented population, one aim of the present study was to describe correlates of these variables in caregivers within the context of the COVID-19 pandemic.
1.1. The present study
To this end, the present study had three exploratory study aims: 1) examine bivariate relationships between stress, concern about weight gain before/during COVID-19, and eating pathology (i.e., DE and EE); 2) examine if stress and concern about weight gain before/during COVID-19 predict variance in eating pathology; and 3) examine if concern about weight gain before/during COVID-19 moderates (e.g., strengthens/weakens) relationships between stress and eating pathology.
2. Methods
2.1. Participants
Participants self-reported caring for at least one child (ages 2–17) and were recruited during the first wave of the COVID-19 (July 2020–September 2020) pandemic. Participants were recruited from snowball sampling and social media advertisements. Sixteen participants were excluded due to not being a legal guardian (n = 12) or failing attention checks (n = 4) embedded into the online survey. The final sample consisted of 140 caregivers: age 39.77 (SD = 6.85) years, mostly female (88.6%), White (88.4%), overweight (BMI = 29.10, SD = 6.80), and middle to upper-middle class (82.2%). Caregivers reported having 1–5 children in the home (M = 1.99, SD = 0.88).
2.2. Measures
2.2.1. Demographics
Participants self-reported their age, sex, race, income, and height and weight (i.e., BMI) at the time of completing the online survey.
2.2.2. Stress
Stress was self-reported using the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983). Ten items assessed the extent to which participants perceived their lives to be unpredictable, uncontrollable, and overloaded. Stress was self-reported on a five-point Likert scale (0 = Never, 4 = Very Often) for the past month. Previous research demonstrated adequate reliability and predictive and construct validity (Cohen et al., 1983). An example item is “In the last month, how often have you been upset because of something that happened unexpectedly?” Higher scores indicated greater stress.
2.2.3. Concern about weight gain
Participants answered two questions on a five-point likert scale (1 = Strongly Disagree, 5 = Strongly Agree): “Before the coronavirus pandemic, I was concerned I would gain weight” and “During the coronavirus pandemic, I am concerned about gaining weight.” Higher scores indicated greater concern about weight gain before/during COVID-19.
2.2.4. Disordered eating
DE was self-reported using the Eating Disorder Examination Questionnaire-Short Form (EDE-QS; Gideon et al., 2016). Twelve items assessed DE attitudes, cognitions, and behaviors such as dietary restraint, weight and shape concerns, binge eating, and compensatory behaviors, which were summed to calculate DE. Participants self-reported symptom prevalence over the previous 7-days on a 4-point Likert scale (0 days, 1–2 days, 3–5 days, or 6–7 days). Previous research has demonstrated adequate reliability and validity of this measure (Gideon et al., 2016). An example of an item is “In the past 7 days, has thinking about food, eating or calories made it very difficult to concentrate on things you are interested in (such as working, following a conversation or reading).” Higher scores indicated greater DE.
2.2.5. Emotional eating
Participants self-reported EE using twelve items from the Emotional Eating Scale-Revised (EES-R; Koball et al., 2012) assessing urges to eat in response to negative emotions. Participants self-reported EE on a continuous scale from 0 to 100 (0 = No desire to eat, 100 = An overwhelming urge to eat), with responses divided by 20 to overlap with existing research (Koball et al., 2012). Items reflected subscales of EE-depression, EE-anger/anxiety, and EE-boredom. Items were preceded with the phrase “Please indicate the extent to which the following feelings lead you to feel an urge to eat by choosing the appropriate response.” Examples for the emotions in each subscale are “discouraged” (e.g., EE-depression), “irritated” (e.g., EE-anger/anxiety), and “bored” (e.g., EE-boredom). Previous research has demonstrated reliability and validity of the EES-R (Koball et al., 2012). Higher scores indicated greater EE.
2.3. Procedure
Research questions, variables, and present analyses were pre-registered; (see https://osf.io/t7zy3, hypothesis/research question 5); Institutional Review Board approval was received prior to data collection; data were collected online in Qualtrics; and informed consent was given prior to study completion. After completion, participants were entered into a raffle for a chance to win one of two $20 Amazon gift cards.
2.4. Analytic plan
Descriptive statistics, internal consistency reliability, and bivariate correlations were calculated (Table 1 ). Missingness, outliers, and assumptions of multiple regression including homoscedasticity, normality, and linearity were examined. Next, four multiple regressions were conducted to examine stress and concern about weight gain before/during COVID as predictors of DE and EE-depression, EE-anger/anxiety, and EE-boredom. Finally, model 1 moderation analyses with BMI and sex entered as covariates were examined (Hayes, 2018) in PROCESS macro in SPSS 27 to determine if the interactions of stress and concern about weight gain before/during COVID-19 were related to DE, EE-depression, EE-anger/anxiety, and EE-boredom. Due to the exploratory nature of this study, interaction effects p ≤ .10 were probed for exploratory conditional moderation effects (Hayes, 2018). Two moderation models were examined per dependent variable, eight moderation analyses in total.
Table 1.
Descriptive statistics, internal consistency reliability, and bivariate correlations across primary study variables.
| Mean | SD | Min. | Max. | Range | Kurtosis (se) | Skew (se) | Alpha | 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. EDEQ-SF | 8.40 | 7.11 | 0.00 | 28.00 | 28.00 | -.17 (.48) | .71 (.22) | .89 | – | |||||
| 2. EES-D | 1.95 | 1.18 | 0.00 | 4.46 | 4.46 | -.78 (.50) | -.03 (.25) | .84 | .54** | – | ||||
| 3. EES-AA | 1.74 | 1.19 | 0.00 | 4.58 | 4.58 | -.43 (.50) | -.48 (.25) | .84 | .38** | .71** | – | |||
| 4. EES-B | 2.90 | 1.40 | 0.00 | 5.00 | 5.00 | −1.09 (.50) | -.30 (.25) | – | .46** | .68** | .57** | – | ||
| 5. PSS | 18.53 | 6.61 | 2.00 | 33.00 | 31.00 | -.69 (.43) | -.16 (.22) | .88 | .50** | .49** | .37** | .37** | – | |
| 6. B-COVID | 3.45 | 1.10 | 1.00 | 5.00 | 4.00 | -.87 (.47) | -.26 (.24) | – | .46** | .43** | .18 | .33** | .22* | – |
| 7. D-COVID | 3.67 | 1.67 | 1.00 | 5.00 | 4.00 | −1.03 (.47) | -.43 (.24) | – | .52** | .51** | .31** | .38** | .22* | .57** |
Notes. *p < .05. **p < .01. SD = standard deviation. Min. = Minimum. Max. = Maximum. (se) = standard error. EDEQ-SF = Eating Disorder Examination Questionnaire-Short Form. EES-D = Emotional Eating-Depression. EES-AA = Emotional Eating-Anxiety/Anger. EES-B = Emotional Eating-Boredom. PSS=Perceived Stress Scale. B-COVID=Concern About Weight Gain Before COVID-19. D-COVID=Concern About Weight Gain During COVID-19. Single items were used to assess EES-B, B-COVID, and D-COVID; thus, internal consistency reliability statistics were not calculated.
3. Results
3.1. Preliminary results
Little's test did not reveal systematic differences between individuals with missing data and those with complete data on any of the measured variables (X 2 = 234.36, p = .964); thus, data were assumed to be Missing Completely At Random. Descriptive statistics, internal consistency, and bivariate correlations are presented in Table 1. Collinearity diagnostics revealed tolerance and variance inflation factors within acceptable ranges (tolerance < 0.20; variance inflation factors < 2) across all models.
3.2. Study aim 1: Examine bivariate relationships between stress and concern about weight gain before/during COVID-19 and eating pathology
Stress was significantly positively related (ps < .01) to DE, EE-depression, EE-anger/anxiety, and EE-boredom. Concern about weight gain before COVID-19 was significantly positively related (ps < .01) to DE, EE-depression, and EE-boredom, but unrelated to EE-anger/anxiety. Finally, concern about weight gain during COVID-19 was significantly positively related (ps < .01) to DE, EE-depression, EE-anger/anxiety, and EE-boredom. See Table 1 for more information.
3.3. Study aim 2: Examine if stress and concern about weight gain before/during COVID-19 predict variance in eating pathology
Stress and concern about weight gain during COVID-19 were significant positive predictors of DE (stress, β = 0.37, p < .001; concern about weight gain during COVID-19, β = 0.32, p < .01), EE-depression (stress, β = 0.39, p < .001; concern about weight gain during COVID-19, β = 0.25, p < .01), EE-anger/anxiety (stress, β = 0.32, p < .01; concern about weight gain during COVID-19, β = 0.26, p < .05), and EE-boredom (stress, β = 0.29, p < .01; concern about weight gain during COVID-19, β = 0.26, p < .05). Concern about weight gain before COVID-19 did not emerge as a significant predictor (ps > .05) across outcome variables. See Table 2 for more information.
Table 2.
Multiple regression analyses of factors predicting eating pathology.
| B | SEB | β | t | p | |
|---|---|---|---|---|---|
| DE | |||||
| Constant | −10.20 | 2.32 | – | −4.40 | .00*** |
| PSS | .38 | .09 | .37 | 4.46 | .00*** |
| B-COVID | 1.20 | .63 | .18 | 1.90 | .06 |
| D-COVID | 1.99 | .59 | .32 | 3.36 | .00** |
| EE-Depression | |||||
| Constant | −1.23 | .41 | – | −3.01 | .00** |
| PSS | .07 | .02 | .39 | 4.67 | .00*** |
| B-COVID | .14 | .11 | .13 | 1.30 | .20 |
| D-COVID | .36 | .10 | .25 | 3.53 | .00** |
| EE-Anger/Anxiety | |||||
| Constant | -.11 | .47 | – | -.23 | .82 |
| PSS | .06 | .02 | .32 | 3.22 | .00** |
| B-COVID | -.05 | .13 | -.05 | -.39 | .70 |
| D-COVID | .26 | .12 | .26 | 2.19 | .03* |
| EE-Boredom | |||||
| Constant | -.02 | .58 | – | -.04 | .97 |
| PSS | .06 | .02 | .29 | 2.97 | .00** |
| B-COVID | .15 | .15 | .12 | 1.00 | .32 |
| D-COVID | .33 | .14 | .26 | 2.26 | .03* |
Notes. *p < .05. **p < .01. ***p < .001. DE = Disordered Eating. EE = Emotional Eating. PSS=Perceived Stress Scale. B-COVID=Concern About Weight Gain Before COVID-19. D-COVID=Concern About Weight Gain During COVID-19.
3.4. Study aim 3: Examine if concern about weight gain before/during COVID-19 moderates relationships between stress and eating pathology
3.4.1. Disordered eating
The overall models assessing stress and concern about weight gain before (R 2 = 0.46, p < .001) and during (R 2 = 0.48, p < .001) COVID-19 contributed significant variance in DE. However, no significant interaction nor conditional moderation effects were observed between stress and concern about weight gain before/during COVID-19 in relation to DE (see Table 3 ).
Table 3.
Concern about weight gain before/during COVID-19 as moderators of relationships between stress and eating pathology.
| b | se | t | p | LLCI | ULCI | |
|---|---|---|---|---|---|---|
| DE | ||||||
| PSS | .39 | .09 | 4.50 | 00*** | .22 | .56 |
| B-COVID | 1.72 | .57 | 3.00 | .00** | .58 | 2.86 |
| PSS * B-COVID | -.05 | .08 | -.70 | .48 | -.21 | .10 |
| CV: Sex | 1.02 | 1.83 | .56 | .58 | −2.62 | 4.65 |
| CV: BMI | .33 | .09 | 3.77 | .00*** | .16 | .51 |
| DE | ||||||
| PSS | .36 | .08 | 4.33 | .00*** | .20 | .53 |
| D-COVID | 1.98 | .52 | 3.78 | .00*** | .94 | 3.02 |
| PSS * D-COVID | -.03 | .07 | -.43 | .67 | -.17 | .11 |
| CV: Sex | .06 | 1.75 | .03 | .97 | −3.41 | 3.53 |
| CV: BMI | .32 | .09 | 3.65 | .00*** | .14 | .49 |
| EE-Depression | ||||||
| PSS | .07 | .02 | 4.44 | .00*** | .04 | .10 |
| B-COVID | .35 | .10 | 3.42 | .00** | .15 | .55 |
| PSS * B-COVID | -.02 | .01 | −1.77 | .08† | -.05 | .00 |
| CV: Sex | -.14 | .34 | -.43 | .67 | -.82 | .53 |
| CV: BMI | .02 | .02 | 1.22 | .23 | -.01 | .05 |
| ECME | ||||||
| −1 SD | .09 | .02 | 4.25 | .00*** | .05 | .14 |
| Average B-COVID | .07 | .02 | 4.44 | .00*** | .04 | .10 |
| +1 SD | .04 | .02 | 2.05 | .04* | .00 | .08 |
| EE-Depression | ||||||
| PSS | .07 | .01 | 4.56 | .00*** | .04 | .09 |
| D-COVID | .45 | .09 | 4.96 | .00*** | .27 | .63 |
| PSS * D-COVID | -.01 | .01 | -.50 | .62 | -.03 | .02 |
| CV: Sex | -.34 | .32 | −1.08 | .28 | -.98 | .29 |
| CV: BMI | .01 | .02 | .72 | .47 | -.02 | .04 |
| EE-Anger/Anxiety | ||||||
| PSS | .06 | .02 | 3.29 | .00** | .02 | .10 |
| B-COVID | .08 | .12 | .71 | .48 | -.15 | .32 |
| PSS * B-COVID | -.01 | .02 | -.80 | .43 | -.04 | .02 |
| CV: Sex | -.04 | .39 | -.11 | .91 | -.81 | .73 |
| CV: BMI | .01 | .02 | .31 | .75 | -.03 | .04 |
| EE-Anger/Anxiety | ||||||
| PSS | .05 | .02 | 2.87 | .01* | .02 | .09 |
| D-COVID | .26 | .11 | 2.31 | .02* | .04 | .48 |
| PSS * D-COVID | -.02 | .01 | −1.36 | .18 | -.05 | .01 |
| CV: Sex | -.12 | .37 | -.33 | .74 | -.86 | .62 |
| CV: BMI | -.00 | .02 | -.11 | .91 | -.04 | .03 |
| EE-Boredom | ||||||
| PSS | .06 | .02 | 2.83 | .01* | .02 | .09 |
| B-COVID | .19 | .13 | 1.50 | .14 | -.06 | .45 |
| PSS * B-COVID | -.03 | .02 | −1.57 | .12 | -.06 | .01 |
| CV: Sex | -.46 | .41 | −1.11 | .27 | −1.28 | .36 |
| CV: BMI | .07 | .02 | 3.52 | .00** | .03 | .11 |
| EE-Boredom | ||||||
| PSS | .05 | .02 | 2.82 | .01* | .02 | .09 |
| D-COVID | .30 | .12 | 2.49 | .01* | .06 | .54 |
| PSS * D-COVID | -.03 | .02 | −1.70 | .09† | -.06 | .00 |
| CV: Sex | -.60 | .40 | −1.50 | .14 | −1.39 | .19 |
| CV: BMI | .06 | .02 | 3.11 | .00** | .02 | .10 |
| ECME | ||||||
| −1 SD | .09 | .03 | 3.17 | .00** | .03 | .14 |
| Average D-COVID | .05 | .02 | 2.82 | .01* | .02 | .09 |
| +1 SD | .02 | .03 | .81 | .42 | -.03 | .07 |
Notes. *p < .05. **p < .01. ***p < .001. † = exploratory conditional moderation effects reported for p ≤ .10. se = standard error. LLCI = Lower Level Confidence Interval. ULCI = Upper Level Confidence Interval. ECME = Exploratory Conditional Moderation Effects. DE = Disordered Eating. EE = Emotional Eating. PSS=Perceived Stress Scale. B-COVID=Concern About Weight Gain Before COVID-19. D-COVID=Concern About Weight Gain During COVID-19.
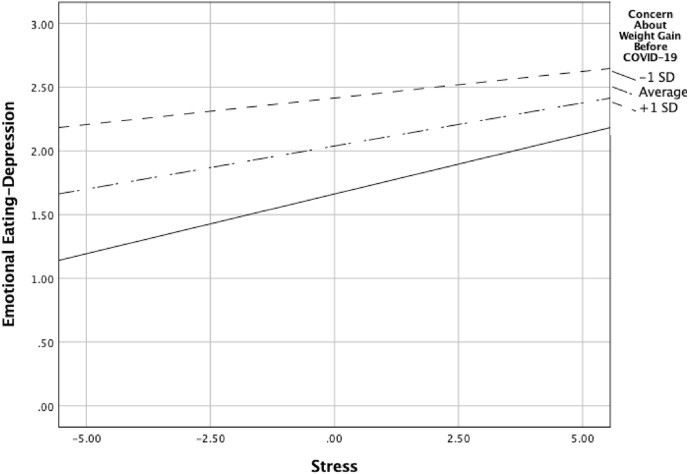
3.4.2. Emotional eating-depression
The overall models assessing stress and concern about weight gain before (R 2 = 0.39, p < .001) and during (R 2 = 0.46, p < .001) COVID-19 contributed significant variance in EE-depression. Interaction effects between stress and concern about weight gain during COVID-19 on EE-depression were not significant (b = -.01, p = .62); however, the interaction of stress and concern about weight gain before COVID-19 on EE-depression (b = -.02, p = .08) was probed for exploratory conditional moderation effects due to p ≤ .10 (Hayes, 2018). Significant exploratory conditional moderation effects were observed such that lower (−1 SD below average; b = 0.09, p < .001), average (b = 0.07, p < .001), and higher (+1 SD above average; b = 0.04, p = .04) concern about weight gain before COVID-19 interacted with stress in relation to EE-depression. More specifically, stress was associated with lower EE-depression when concern about weight gain before COVID-19 was lower, but as concern about weight gain before COVID-19 increased (+1 SD above average), stress was associated with higher EE-depression (see Fig. 2). Conditional moderation effects with concern about weight gain before COVID-19 remained significant with the inclusion of BMI (b = 0.02, p = .23) and sex (b = -.14, p = .67) covariates.
Fig. 2.
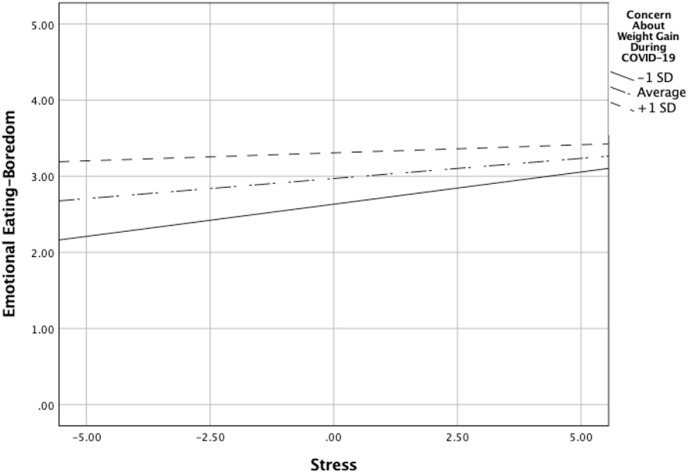
Moderation of stress and emotional eating-boredom by concern about weight gain during COVID-19.
3.4.3. Emotional eating-anger/anxiety
The overall models assessing stress and concern about weight gain before (R 2 = 0.16, p = .02) and during (R 2 = 0.20, p < .005) COVID-19 contributed significant variance in EE-anger/anxiety. However, no significant interaction nor exploratory conditional moderation effects were observed between stress and concern about weight gain before/during COVID-19 in relation to EE-anger/anxiety (see Table 3).
3.4.4. Emotional eating-boredom
The overall models assessing stress and concern about weight gain before (R 2 = 0.33, p < .001) and during (R 2 = 0.36, p < .001) COVID-19 contributed significant variance in EE-boredom. Interaction effects across stress and concern about weight gain before COVID-19 on EE-boredom were not significant (b = -.03, p = .12); however, the interaction of stress and concern about weight gain during COVID-19 on EE-boredom (b = -.03, p = .09) was probed for exploratory conditional moderation effects due to p ≤ .10 (Hayes, 2018). Significant exploratory conditional moderation effects were observed such that lower (−1 SD below average; b = 0.08, p < .005) and average (b = 0.05, p = .01) concern about weight gain during COVID-19 significantly interacted with stress in relation to EE-boredom. More specifically, stress was associated with lower EE-boredom when concern about weight gain during COVID-19 was average and below average (see Fig. 1 ). Conditional moderation effects with concern about weight gain during COVID-19 remained significant with the inclusion of BMI (b = 0.06, p < .005) and sex (b = -.60, p = .14) covariates.
Fig. 1.
Moderation of stress and emotional eating-depression by concern about weight gain before COVID-19.
4. Discussion
To address the first study aim, we examined bivariate relationships between stress and concern about weight gain before/during COVID-19 and eating pathology among caregivers. Moderate positive relationships between stress and eating pathology were observed among caregivers, consistent with growing research mapping positive relationships between stress and eating pathology during the COVID-19 pandemic across diverse populations (Al-Musharaf, 2020; Elmacioğlu, Emiroğlu, Ülker, Kircali, & Oruç, 2020; Khubchandani et al., 2020; Owen et al., 2020). While concern about weight gain before/during COVID-19 was significantly positively related with DE, EE-depression, and EE-boredom, differential relationships emerged for EE-anger/anxiety. More specifically, concern about weight gain before COVID-19 was unrelated to EE-anger/anxiety but concern about weight gain during COVID-19 was positively related to EE-anger/anxiety. These findings echo research documenting the deleterious impact of COVID-19 on broad EE behavior (Elmacioğlu et al., 2020; Al-Musharaf, 2020) and build on these findings to suggest that some EE types such as the urge to eat in response to anger/anxiety may overlap with concern about weight gain during, but not before, the pandemic. Importantly, findings from the present work provide initial evidence for negative EE types to overlap with negative psychological correlates relevant to the COVID-19 pandemic among caregivers.
While we did not measure the eating pathology of caregivers' children, these data may inform previous research showing that caregivers' eating pathology may influence the development and maintenance of eating pathology in their children (see Agras, Hammer, & McNicholas, 1999; Allen, Gibson, McLean, Davis, & Byrne, 2014; Patel, Wheatcroft, Park, & Stein, 2002; Reba-Harreleson et al., 2010; Waugh & Bulik, 1999). For example, one study suggested that family exposure to stress, alongside maternal current or past eating disorder diagnosis, were risk factors for significantly higher eating disorder and emotional eating symptoms among children (Allen et al., 2014). Findings from the present study add to this literature, suggesting that stress and concern about weight gain before/during COVID-19 were meaningful positive correlates of eating pathology in caregivers, and therefore these variables may be relevant to researchers and clinicians interested in the potential transmission of eating pathology from caregivers to children. Furthermore, considering the fact that caregivers and their children may be under increased contact due to COVID-19 global shutdowns, the potential transmission of eating pathology may be pronounced due, in part, to increased opportunities for children to observe and model their caregivers’ eating pathology.
To address the second study aim, four multiple regressions examined if stress and concern about weight gain before/during COVID-19 predicted variance in eating pathology among caregivers. Results revealed that stress and concern about weight gain during, but not before, COVID-19 positively predicted variance in eating pathology among caregivers. These data parallel previous research that points to COVID-19 in relation to worsened eating pathology (Khubchandani et al., 2020; Owen et al., 2020) and highlight specific psychological stressors such as stress and concern about weight gain that may be associated with DE and EE among caregivers. Importantly, findings that distinguish concern about weight gain during COVID-19 as a positive predictor of variance in eating pathology among caregivers build on the idea that caregivers may face the brunt of changes caused by the pandemic and thus may experience inflated concern about weight gain and eating pathology during the pandemic. Importantly, due to the cross-sectional nature of the present findings, temporal order of variables cannot be discerned; nonetheless, findings add to research in this area and suggest that caregivers may be an important population to further explore in relation to eating pathology and the COVID-19 pandemic.
To address the third study aim, moderation analyses examined if relationships between stress and eating pathology were moderated by concern of weight gain before/during COVID-19. Overall, moderation effects were negligible with the exception of EE-depression and EE-boredom models. More specifically, the association between stress and EE-depression was weakened when concern about weight gain before COVID-19 was lower, but when concern about weight gain before COVID-19 was higher, the association between stress and EE-depression was strengthened. Thus, higher levels of concern about weight before COVID-19 in tandem with self-reported stress was more strongly associated with EE-depression in caregivers. Furthermore, the association between stress and EE-boredom was weakened when concern about weight gain during COVID-19 was lower. Thus, lower levels of concern about weight during COVID-19 in tandem with self-reported stress was less strongly associated with EE-boredom in caregivers. Together, exploratory findings provide preliminary evidence for the interaction of stress and concern about weight gain in relation to depression and boredom EE among caregivers within the context of the COVID-19 pandemic.
Because the COVID-19 pandemic is in its second wave and will undoubtedly continue to exert negative effects for some time, including global shutdowns, findings from the present study may aid in the mitigation of some types of EE, such as EE-boredom, which are associated with higher desire for snacking (Moynihan et al., 2015), food consumption (Abramson & Stinson, 1977), and calorie and fat consumption (Moynihan et al., 2015), all of which may be related to poor health outcomes (e.g., overweight/obesity; but see Braden et al., 2018). Indeed, to the understanding of the authors, no research to date has mapped negative psychological correlates of negative EE types in relation to the COVID-19 pandemic among caregivers. This is important because the EE literature contends that specific types of emotions, particularly negative emotions, exert unique effects on eating behaviors (Macht, 2008), and thus the present work adds more detailed information to the budding COVID-19 literature that maps relationships with negative EE behaviors more broadly (Elmacioğlu et al., 2020; Al-Musharaf, 2020). Despite these strengths, conditional moderation effects should be interpreted with caution because of the exploratory, non-significant nature of the interaction effects, as well as several important limitations and future directions.
4.1. Limitations and future directions
First, the cross-sectional nature of the present study prevents attributions of causality between study variables. Longitudinal methods comparing these variables across time (e.g., weeks, months, years) would offer meaningful insights such as whether concern about weight gain precedes DE or EE, or how rates of COVID-19 infection impact stress and eating behaviors among caregivers. Second, measurements of DE and EE were non-clinical in nature. Non-significant findings, such as those observed for moderation effects between stress and concern about weight gain before/during COVID-19 in relation to DE, could then be attributable to overall low levels of DE among caregivers. Third, though the sample was large enough (N = 140) to adequately power analyses for the exploratory research aims, a larger sample would have been able to detect smaller effects in DE and EE. Fourth, the reliance on self-report measures may limit the accuracy of these findings. To combat this, future research could use laboratory or ecological momentary assessment research designs to provide important information about the causal nature of these variables and how these variables unfold in the real world, both of which would increase the accuracy of findings. Fifth, the present study did not include a comparison sample, nor did it include caregiver-specific variables of stress that could further distinguish these findings from clinical and community populations. Future research would be well suited to examine caregiver-specific stressors in relation to eating pathology to add detail about the caregiving experience that contributes to outcomes. For example, future research should discern if increased schooling and feeding responsibilities, decreased time for self-care, disruption in routines, or other stressors played a role in self-reported stress, concern about weight gain, DE, and EE. A better understanding of which stressors were most salient in COVID-19-related stress may offer important information to researchers and clinicians alike. Relatedly, future research assessing for existing coping skills to manage stress may add useful information upon which researchers and clinicians can build on existing strengths to manage the negative impacts of stress on caregivers' eating pathology. Even more, though these findings do extend stress and concern about weight gain as relevant variables in relation to caregivers eating pathology, including a comparison sample would further aid in quantifying these effects and their generalizability to the eating and weight disorders literature. Finally, other variables outside of the caregiving experience such as time in quarantine social isolation, concern about contracting COVID, remote work, and interpersonal conflict (e.g., divorce), to name a few, could add more information about caregiver stress and subsequent effects on their eating pathology. It is important for future research to be exhaustive in capturing these variables to add more complete information on the role of stress and concern about weight gain on caregivers’ eating pathology.
5. Conclusions
The COVID-19 pandemic has resulted in over 3 million deaths and profoundly disrupted typical daily routines surrounding childcare, eating behaviors, and physical activity. It may be the case that caregivers face the brunt of these changes in daily routines, which may be related to the development and maintenance of eating pathology in caregivers. Findings from the present study suggest that stress and concern about weight gain before/during COVID-19 may be important, positive correlates of eating pathology in caregivers. Furthermore, stress and concern about weight gain during, but not before, COVID-19 emerged as positive predictors of eating pathology among caregivers. Exploratory moderation models introduce the potential for concern about weight gain before/during COVID-19 to influence relationships between stress and EE-depression and EE-boredom in caregivers. Findings suggest that the COVID-19 pandemic may confer deleterious effects in the context of stress and concern about weight gain on eating pathology among caregivers, which furthers the notion that caregivers may be vulnerable to eating pathology during the pandemic.
Ethical statement
This research was conducted in accordance with standard ethical and human research guidelines, and the rights of participants were protected. The manuscript contains original research that is not currently published or under review elsewhere. Amy K. Jordan and Wesley R. Barnhart are co-first authors for this manuscript. Each author has contributed significantly to the work and accept full responsibility for all aspects of the work. Upon request, original data will be provided for review. There are no conflicts of interest to disclose. Correspondence should be addressed to Amy K. Jordan, Department of Psychology, 822 East Merry Avenue, Bowling Green, OH 43403. E-mail: akjorda@bgsu.edu, and Wesley R. Barnhart, Department of Psychology, 822 East Merry Avenue, Bowling Green, OH 43403. E-mail: wrbarnh@bgsu.edu.
Funding acknowledgement
No funding supported the present research.
Declaration of competing interest
There are no conflicts of interest to disclose among authors.
References
- Abramson E.E., Stinson S.G. Boredom and eating in obese and non-obese individuals. Addictive Behaviors. 1977;2(4):181–185. doi: 10.1016/0306-4603(77)90015-6. [DOI] [PubMed] [Google Scholar]
- Agras W.S., Hammer L.D., McNicholas F. A prospective study of the influence of eating-disordered mothers on their children. International Journal of Eating Disorders. 1999;25:252–262. doi: 10.1002/(sici)1098-108x(199904)25:3<253::aid-eat2>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Al-Musharaf S. Prevalence and predictors of emotional eating among healthy young Saudi women during the COVID-19 pandemic. Nutrients. 2020;12(10):2923. doi: 10.3390/nu12102923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen K.L., Gibson L.Y., McLean N.J., Davis E.A., Byrne S.M. Maternal and family factors and child eating pathology: Risk and protective relationships. Journal of Eating Disorders. 2014;2:11. doi: 10.1186/2050-2974-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Hoekelmann A. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnow B., Kenardy J., Agras W.S. The emotional eating scale: The development of a measure to assess coping with negative affect by eating. International Journal of Eating Disorders. 1995;18(1):79–90. doi: 10.1002/1098-108x(199507)18:1<79::aid-eat2260180109>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Barnhart W.R., Braden A.L., Jordan A.K. Negative and positive emotional eating uniquely interact with ease of activation, intensity, and duration of emotional reactivity to predict increased binge eating. Appetite. 2020;151:104688. doi: 10.1016/j.appet.2020.104688. [DOI] [PubMed] [Google Scholar]
- Barnhart W.R., Braden A.L., Price E. Emotion regulation difficulties interact with negative, not positive, emotional eating to strengthen relationships with disordered eating: An exploratory study. Appetite. 2021;158:105038. doi: 10.1016/j.appet.2020.105038. [DOI] [PubMed] [Google Scholar]
- Belcher B.R., Nguyen-Rodriguez S.T., McClain A.D., Hsu Y.W., Unger J.B., Spruijt-Metz D. The influence of worries on emotional eating, weight concerns, and body mass index in Latina female youth. Journal of Adolescent Health. 2011;48(5):487–492. doi: 10.1016/j.jadohealth.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braden A., Musher-Eizenman D., Watford T., Emley E. Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite. 2018;125:410–417. doi: 10.1016/j.appet.2018.02.022. [DOI] [PubMed] [Google Scholar]
- Castellini G., Cassioli E., Rossi E., Innocenti M., Gironi V., Sanfilippo G., Ricca V. The impact of COVID‐19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. International Journal of Eating Disorders. 2020:1–8. doi: 10.1002/eat.23368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Crasta D., Daks J.S., Rogge R.D. Modeling suicide risk among parents during the COVID-19 pandemic: Psychological inflexibility exacerbates the impact of COVID-19 stressors on interpersonal risk factors for suicide. Journal of contextual behavioral science. 2020;18:117–127. doi: 10.1016/j.jcbs.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte C., Pinto-Gouveia J. Returning to emotional eating: The emotional eating scale psychometric properties and associations with body image flexibility and binge eating. Eating and weight disorders - Studies on anorexia. Bulimia and Obesity. 2015;20:497–504. doi: 10.1007/s40519-015-0186-z. [DOI] [PubMed] [Google Scholar]
- Elmacioğlu F., Emiroğlu E., Ülker M.T., Kircali B.Ö., Oruç S. Evaluation of nutritional behavior related to Covid-19. Public Health Nutrition. 2020:1–20. doi: 10.1017/S1368980020004140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández‐Aranda F., Casas M., Claes L., Bryan D.C., Favaro A., Granero R., Menchón J.M. COVID‐19 and implications for eating disorders. European Eating Disorders Review. 2020;28(3):239. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer S., Chen E., Katterman S., Roerhig M., Bochierri-Ricciardi L., Munoz D., le Grange D. Emotional eating in a morbidly obese bariatric surgery-seeking population. Obesity Surgery. 2007;17(6):778–784. doi: 10.1007/s11695-007-9143-x. [DOI] [PubMed] [Google Scholar]
- Fontanesi L., Marchetti D., Mazza C., Di Giandomenico S., Roma P., Verrocchio M.C. Psychological trauma: Theory, research, practice, and policy. 2020. The effect of the COVID-19 lockdown on parents: A call to adopt urgent measures. [DOI] [PubMed] [Google Scholar]
- Gideon N., Hawkes N., Mond J., Saunders R., Techanturia K., Serpell L. Development and psychometric validation of the EDE-QS, a 12 item short form of the eating disorder examination questionnaire (EDE-Q) PloS One. 2016;11(5) doi: 10.1371/journal.pone.0152744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. 2nd ed. The Guilford Press; New York: 2018. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Janssen L.H., Kullberg M.L.J., Verkuil B., van Zwieten N., Wever M.C., van Houtum L.A., Elzinga B.M. Does the COVID-19 pandemic impact parents' and adolescents' well-being? An EMA-study on daily affect and parenting. PloS One. 2020;15(10) doi: 10.1371/journal.pone.0240962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani J., Kandiah J., Saiki D. The COVID-19 pandemic, stress, and eating practices in the United States. European Journal of Investigation in Health, Psychology and Education. 2020;10(4):950–956. doi: 10.3390/ejihpe10040067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koball A.M., Meers M.R., Storfer-Isser A., Domoff S.E., Musher-Eizenman D.R. Eating when bored: Revision of the emotional eating scale with a focus on boredom. Health Psychology. 2012;31(4):521–524. doi: 10.1037/a0025893. [DOI] [PubMed] [Google Scholar]
- Macht M. How emotions affect eating: A five-way model. Appetite. 2008;50(1):1–11. doi: 10.1016/j.appet.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Martínez-de-Quel Ó., Suárez-Iglesias D., López-Flores M., Pérez C.A. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite. 2021;158:105019. doi: 10.1016/j.appet.2020.105019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moynihan A.B., van Tilburg W.A.P., Igou E.R., Wisman A., Donnelly A.E., Mulcaire J.B. Eaten up by boredom: Consuming food to escape awareness of the bored self. Frontiers in Psychology. 2015;6:369. doi: 10.3389/fpsyg.2015.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver G., Wardle J., Gibson E.L. Stress and food choice: A laboratory study. Psychosomatic Medicine. 2000;62(6):853–865. doi: 10.1097/00006842-200011000-00016. [DOI] [PubMed] [Google Scholar]
- Owen A.J., Tran T., Hammarberg K., Kirkman M., Fisher J.R.W. Poor appetite and overeating reported by adults in Australia during the COVID-19 pandemic: A population-based study. Public Health Nutrition. 2020:1–20. doi: 10.1017/S1368980020003833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P., Wheatcroft R., Park R.J., Stein A. The children of mothers with eating disorders. Clinical Child and Family Psychology Review. 2002;5(1):1–19. doi: 10.1023/a:1014524207660. [DOI] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., Davis M.M. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E., et al. Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reba-Harreleson L., Von Holle A., Hamer R.M., Torgersen L., Reichborn-Kjennerud T., Bulik C.M. Patterns of maternal feeding and child eating associated with eating disorders in the Norwegian mother and child cohort study (MoBe) Eating Behaviors. 2010;11:54–61. doi: 10.1016/j.eatbeh.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricca V., Castellini G., Fioravanti G., Lo Sauro C., Rotella F., Ravaldi C., et al. Emotional eating in anorexia nervosa and bulimia nervosa. Comprehensive Psychiatry. 2012;53:245–251. doi: 10.1016/j.comppsych.2011.04.062. [DOI] [PubMed] [Google Scholar]
- Schlegl S., Maier J., Meule A., Voderholzer U. Eating disorders in times of the COVID‐19 pandemic—results from an online survey of patients with anorexia nervosa. International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tison G.H., Avram R., Kuhar P., Abreau S., Marcus G.M., Pletcher M.J., et al. Worldwide effect of COVID-19 on physical activity: A descriptive study. Annals of Internal Medicine. 2020;173(9):767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuillier L., May L., Greville-Harris M., Surman R., Moseley R.L. The impact of the COVID-19 pandemic on individuals with eating disorders: The role of emotion regulation and exploration of online treatment experiences. Journal of eating disorders. 2021;9(1):1–18. doi: 10.1186/s40337-020-00362-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waugh E., Bulik C.M. Offspring of women with eating disorders. International Journal of Eating Disorders. 1999;25:123–133. doi: 10.1002/(sici)1098-108x(199903)25:2<123::aid-eat1>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]