Abstract
Increases in longevity combined with a policy emphasis on caring for older people in their own homes could have widened or narrowed the survival gap between care home and community-dwelling resident older people. Knowledge of pre-COVID-19 trends in this gap is needed to assess the longer-term impacts of the pandemic. We provide evidence for England on recent trends in 1, 2 and 3-year mortality amongst care home residents aged 65+ compared with similar community-dwelling residents. We use the Clinical Practice Research Datalink, a nationally representative primary care database. For each of the ten years from 2006 to 2015, care home and community-dwelling residents aged 65+ were identified and matched in the ratio 1:3, according to age, gender, area deprivation and region. Cox survival analyses were used to estimate mortality risks for care home residents in comparison with similar community-dwelling people, adjusting for age, gender, area deprivation and region. The study sample consisted of ten overlapping cohorts averaging 5495 care home residents per cohort. Adjusted mortality risks increased over the study period for care home residents while decreasing slightly for matched community-dwelling residents. The relative risks (RRs) of mortality associated with care home residence were higher for younger ages and shorter follow-up periods, in all years. Over the decade, the RRs increased, most at younger ages and for shorter follow-up periods (e.g. for the age group 65–74 years, 1-year average RR increased by 61% from 5.4 to 8.8, while for those aged 85–94 years and over, 3-year RR increased by 22% from 1.3 to 1.6). Thus the survival gap between older care home and community-dwelling residents has been widening, especially at younger ages. In due course, it will be possible to establish to what extent the COVID-19 pandemic has resulted in further growth in this gap.
Keywords: Long-term care, Older people, Ageing, Survival gap, Care home, Community-dwelling
1. Introduction
The COVID-19 pandemic has brought increased interest in mortality in residential long-term care facilities (care homes) (Comas-Herrera et al., 2020; Morciano et al., 2020). Survival rates among older people living in care homes tend to be lower than for their counterparts living in the community, because care home residents are generally in poorer health than community-dwelling people of similar ages (Shah et al., 2010; Falconer and O'Neil, 2007; Castora-Binkley et al., 2014; Gaugler et al., 2007). For some years, health and social care policy has emphasised enabling older people to live in their own homes (Colombo et al., 2011; European Commission, 2015; DHSC, 2020; Foundations, 2015; Humphries et al., 2016; Katz, 2011). Older people who enter care homes are therefore tending to enter them at older ages, and at increased levels of frailty than previously (Humphries et al., 2016; Katz, 2011; Matthews et al., 2016; Sund Levander et al., 2016). At the same time, life expectancy at older ages continues to increase (Kontis et al., 2017; Bennett et al., 2015). These trends could result in increasing or reducing disparities between the survival of older care home residents and those who remain living in their own homes. Evidence of the effect of COVID-19 (Comas-Herrera et al., 2020) suggests that the pandemic is likely to be widening mortality differentials between care home and community-dwelling residents because of the difficulty of infection control in communal facilities. There is no official UK analysis of trends in mortality in care homes so we do not know from official statistics whether this widening represents an acceleration or a reversal of previous trends, nor how such trends varied by age, gender, socio-economic characteristics and so forth.
Only a small number of previous studies have addressed recent trends in mortality for older people living in care homes (literature search details are given in Appendix Table 1) and none has done so recently for England. A study in Sweden comparing 5-year survival after admission for two cohorts of older nursing home residents in 2000 and 2007, found an increase in their age and frailty at admission, and a shortening of the survival time after their admission (Sund Levander et al., 2016). Another Swedish study compared time from care home admission to death for older people between 2006 and 2012, finding a significant decrease in survival time, the most dramatic change being an increase in the proportion of people who died shortly after moving to an institution (Schon et al., 2016). An older study for England and Wales showed an increase in the relative risk of mortality associated with residence in a ‘communal establishment’ (for older people most ‘communal establishments’ are care homes) using mortality data over 5-year periods for the years 1981–5, 1991–5, and 2001–5 (Grundy, 2011). One study in England and Wales used The Health Improvement Network (THIN), a primary care database, to provide 1-year survival estimates (2009–2010) for care home and community-dwelling residents. It concluded that mortality was at that time higher in care homes than amongst community-dwelling residents but the higher mortality associated with care home residence was attenuated with increasing age (Shah et al., 2013). The study provided no evidence on trends in the mortality of care home and community residents.
Some studies for England have considered predictors of length of stay in care homes, which is closely related to mortality. However, they did not examine trends in length of stay and were limited to publicly funded residents (Steventon and Roberts, 2012) typically with high frailty and low socioeconomic profile, or to data from a single care home provider (Forder and Fernandez, 2011).
Thus studies of recent trends in the survival gap between older care home residents and similar community-dwelling people are lacking for the UK and its constituent countries. Our objective is to provide evidence for England on trends over a recent, pre-COVID-19, ten-year period in survival of older care home residents compared with their counterparts living in their own homes, taking account of differences in their age, gender, region and area deprivation levels. Establishing such trends is important for an understanding of the impact of COVID-19 on the care home sector and is of more general relevance to health and social care policy.
2. Data and methods
2.1. Study population
Data come from the February 2018 version of the Clinical Practice Research Datalink GOLD (CPRD). CPRD is a primary care database of anonymised electronic medical records from participating primary care General Practices (GPs) in the UK (Herrett et al., 2015). Participation is voluntary and dependent on the record-keeping software used by the practice. Over 98% of the UK population are registered with a GP and patients from participating practices are automatically included in CPRD unless they opt out individually. CPRD labels patients as “acceptable” for research if their data allows a continuous follow-up and satisfies a series of validity checks. For practices, an up-to-standard date is provided at which their data is continuous high-quality data fit for use in research. In 2013, CPRD patients with acceptable data quality represented nearly 7% of the UK population and were representative of the UK population in terms of age, gender and ethnicity (Herrett et al., 2015). Our study population is CPRD patients aged 65 and over identified as resident in care homes and a matched comparator group of similar community-dwelling patients. We construct and analyse separately 10 overlapping cohorts of patients who were aged 65 years and over, and living in England at the start of each year from 2006 to 2015. Linkage with Office for National Statistics (ONS) data provides dates of death of cohort members and their small area level Index of Multiple Deprivation (ONS, 2015; Smith et al., 2015).
2.2. Distinguishing care home and community residence
There are several variables in CPRD which indicate that a patient is likely to be a resident in a care home, although not all are recorded for every patient. We adapted a method previously used with the (similar) THIN database (Shah et al., 2010) to classify patients as care home or community residents. We used patient Read codes (Chisholm, 1990) and other available information in CPRD to form three groups of markers of likely long-term care home residence (and excluding settings providing lower levels of support such as sheltered/supported housing): explicit mention of residence or admission to a care home (which we call ‘R’ markers); visits/consultations in a care home (‘V’ markers); and death/past residence in a care home (‘P’ markers). Appendix Table A2 provides further details of the R, V and P markers. Unlike Shah et al. (2010), we were not able to establish for every year we use, whether a patient's postcode (English postcodes cover about 15 properties on average) included a care home. In our study, care home residence was therefore assigned where at least one of the following conditions held: (a) one or more R markers of care home residence before the start of the year; (b) two or more V markers separated by at least six weeks; (c) a V marker before year start and a subsequent P marker; or (d) having a V indicator before year start and the patient's household consisted of at least 4 people aged 65 and over. Condition (a) follows closely Shah et al. (2010). Conditions (b) to (d) are similar to the alternatives to condition (a) used by those authors except that as we are unable to use whether the postcode includes a care home, we are more stringent in terms of evidence available directly from CPRD, for example requiring at least two markers in each condition. We added the six-week requirement in (b) to avoid temporary care home residence: in England publicly-funded temporary reablement care services may occur in care homes for a maximum of six weeks (SCIE, 2020). Similar to Shah et al. (2010), we defined an ‘undetermined’ group of patients having some of the R, V or P indicators but not satisfying any of conditions (a) to (d), and an ‘excluded’ category of patients with none of the care home residency markers but living in households with 3 older people. Community-dwelling patients were those not classified as care home residents, undetermined or excluded. Our approach was to adopt a relatively tight definition of care home residence because the impact on the comparison of community and care home residents of mistakenly including some care home residents in the relatively large number of community-dwelling residents is likely to be less than wrongly including some community residents in the small care home sample. However we undertake a sensitivity analysis in which we move from the undetermined to the care home category patients who lived in households with at least 4 older people where at least 30% of older people were aged 85 and over and at most 20% of the older people in the household were aged 65–74 (the higher the proportion of the 4+ older household members who are aged over 85, the greater is the likelihood that the household is a care home).
2.3. Analysis sample
The sample was restricted as follows. We included only patients for whom data quality was ‘acceptable’, the general practice data quality was ‘up-to-standard’ (Herrett et al., 2015) and the practice had consented to record linkage with ONS data. Patients had to be known to be alive (according to CPRD and ONS mortality data), aged 65+, living in England and not transferred out of the practice at the start of the relevant year (2006–2015). Additionally we excluded patients for whom gender, region, and quintile of the Index of Multiple Deprivation for their residence area could not be established. Finally, to allow follow-up periods of up to three years, for statistical analysis we limited the sample for each cohort to those practices where the last data collection date was at least three years after 1st January of the cohort's starting year.
Table A3 in the Appendix shows the number of eligible practices and patients before and after the three-year follow-up requirement and, amongst the latter, the percentage assigned to each residence category. The number of practices and patients before requiring the three-year follow-up decreased over time due to falling numbers of practices available in CPRD GOLD. As a consequence, the reduction resulting from the three-year follow-up requirement increased over time. However, each year's sample of patients was demographically representative of the English population aged 65 or older. Comparing the age composition of the sample with three-year follow-up in Table A3 with ONS mid-year population estimates (ONS, 2019) showed only small differences (e.g. the largest difference was for the percentage of women who were aged 65–74 in 2012 which was 50.2% according to ONS and in our sample was 48.6%; the median (IQR) absolute difference is 0.3 (0.2,0.7)). Differences in gender composition were negligible: median (IQR) absolute difference is 0.1 (0.1,0.2). The percentage of residents with undetermined residence fell over time while the percentages assigned to care home and community residence both increased. Comparing the residency split with figures for England from the most recent (March 27, 2011) population Census indicates that the percentage of our (1 January) 2011 sample identified as living in a care home is about 50% of that found by the Census, and is closest at younger ages (53.3% among those aged 65–74, falling to 46.4% amongst the 85+ age group) and very similar for men and women for the 65+ age group as a whole. Despite these differences in the percentages identified as care home residents, their broad regional pattern showed similarities with the Census with the percentages being lowest in London and highest in the South (excluding London) (Appendix Table A4). Importantly, the age and gender composition of our 2011 sample of care home residents was close to that found for England in the 2011 Census (Appendix Table A4). Its composition by region was also similar although it had a notably higher proportion of care home residents from the South and a lower proportion from the North. This is attributable partly to the restriction of our sample to practices with a 3-year follow-up. In our sensitivity analysis using a less restrictive identification of care home residents, the percentage of the 2011 sample identified as living in a care home is much closer to that found by the Census (3.0% compared with 3.2%) while the age and gender composition and the variation in proportions of care home residents by region are again consistent with the 2011 Census. In contrast with the main analysis the percentage of patients identified as care home residents fell over time. This is because the increase in the proportion (and number) of patients identified as care home residents was most marked in the earlier cohorts where for the main analysis the numbers in the undetermined category were largest (Appendix Table A3).
2.4. Matching care home and community-dwelling residents
To control for differences in the demographic and socioeconomic/geographic composition of care home and community residents we constructed a matched sample of community-dwelling residents. For each year and care home resident, we randomly selected as controls three community-dwelling patients having, at year start (1st January): the same age in years (sequentially allowing for a difference of up to two years in age), gender, region, and quintile of area deprivation. For this purpose Health Authority regions for England available in CPRD, were aggregated into North, Midlands/East, London, and South. Care home residents for whom three matches were not found in a given year were excluded from that year's cohort.
2.5. Statistical methods
We used survival analysis techniques tailored to the right-censoring of survival data; survival times were right-censored during the follow-up period if patients were alive or transferred out of the practice before the end of that period. We estimated mortality hazard rate ratios (HRs) for care home versus community residence using non-parametric Cox proportional hazards models (one per cohort), adjusted for age, gender, quintile of deprivation (providing a check on the matching process) and region at year start. Age was measured in years. The reference group was aged 65, female, from the South of England, and in the central quintile of deprivation. Their baseline survival/mortality was obtained using the Kaplan-Meier product-limit estimate. The assumption of proportionality of hazards was tested by adding time-dependent covariates to the Cox models. Interaction terms were also tested for statistical significance. We explored the effect of also adjusting for length of time before year start of the first record of care home residence as indicated by the earliest R or V marker.
From the main analysis Cox models, adjusted risks of 1-, 2-, 3-year mortality for care home and community residents, and the relative risk associated with care home residence, were calculated separately for each cohort, age group and gender; see Symons and Moore (2002) for standard formulae.
All computations were performed using Stata Release 14.2 (StataCorp, 2015).
3. Results
3.1. Sample composition
Table 1 presents the numbers in the matched samples of care home and community residents at the start of each year and the percentages of them who had died or had been transferred out of the practice and so were lost to follow-up after 1, 2, and 3 years. Care home mortality was higher than mortality amongst the matched community residents and rose over the period whereas community mortality fell. Transfers out increased over the period for both groups.
Table 1.
Sample size (at year start) and 1, 2, 3-Year mortality and transfers out rates by residence type.
| Care home residents |
Community-dwelling residents |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | N | 1-year |
2-year |
3-year |
N | 1-year |
2-year |
3-year |
||||||
| Died | Transferred out | Died | Transferred out | Died | Transferred out | Died | Transferred out | Died | Transferred out | Died | Transferred out | |||
| 2006 | 6699 | 22.7% | 4.2% | 39.4% | 7.3% | 52.1% | 9.6% | 20,097 | 9.1% | 5.2% | 17.6% | 9.6% | 24.8% | 13.2% |
| 2007 | 7043 | 23.3% | 4.5% | 40.4% | 7.6% | 52.1% | 9.3% | 21,129 | 9.7% | 5.2% | 18.0% | 9.5% | 24.8% | 13.4% |
| 2008 | 6862 | 23.3% | 4.6% | 39.2% | 7.1% | 51.9% | 8.9% | 20,586 | 9.8% | 5.1% | 17.7% | 9.7% | 24.3% | 13.6% |
| 2009 | 6550 | 21.8% | 4.2% | 38.7% | 6.8% | 50.7% | 8.5% | 19,650 | 9.2% | 5.4% | 17.1% | 9.9% | 23.7% | 13.6% |
| 2010 | 6393 | 22.7% | 3.8% | 38.2% | 6.2% | 51.9% | 8.0% | 19,179 | 9.3% | 5.3% | 16.9% | 10.0% | 23.3% | 14.1% |
| 2011 | 6208 | 21.5% | 4.1% | 39.6% | 6.8% | 53.4% | 9.5% | 18,624 | 9.1% | 5.3% | 16.8% | 9.7% | 23.6% | 14.0% |
| 2012 | 5539 | 23.4% | 4.0% | 40.3% | 7.6% | 53.0% | 10.1% | 16,617 | 9.2% | 5.6% | 17.4% | 10.5% | 23.2% | 14.9% |
| 2013 | 4021 | 24.1% | 5.8% | 41.3% | 9.6% | 55.5% | 12.3% | 12,063 | 8.8% | 6.0% | 15.8% | 10.8% | 22.0% | 14.8% |
| 2014 | 2927 | 25.1% | 6.4% | 45.3% | 10.5% | 57.6% | 15.5% | 8781 | 7.8% | 6.0% | 15.1% | 10.8% | 21.0% | 14.9% |
| 2015 | 2713 | 30.0% | 7.6% | 46.8% | 15.4% | 56.9% | 17.0% | 8139 | 8.2% | 5.5% | 15.2% | 10.2% | 21.4% | 14.0% |
Note: CPRD patients aged 65+, living in England and known to be alive at the start of relevant calendar year.
Table A5, Table A6, Table A7 show the composition of each cohort in the matched sample in terms of age, gender, deprivation and region. The proportions of the cohort in the youngest (65–74) and oldest (85+) age groups have both increased over time, while the proportion in the middle age group (75–84) has fallen. Similar trends are observed in the ONS mid-year population estimates for England as a whole (ONS, 2019). The trend in age composition is found for both men and women, although in every cohort women in care homes are older than men e.g. in 2015 64% of female care home residents were aged 85+ and 9% were aged 65–74; corresponding figures for males were 42% and 23%. The proportion who are female has fallen over time – from 76% in 2006 to 70% in 2015. The matched cohorts are less likely than the general population to live in areas in the two most deprived quintiles or in the North of England and this has become more so over time. This reflects the fact that the number of practices without a 3-year follow-up increased in these areas and more of them had to be excluded. For this reason, we adjust the yearly survival models for region and area deprivation.
3.2. Comparison of care home and community mortality
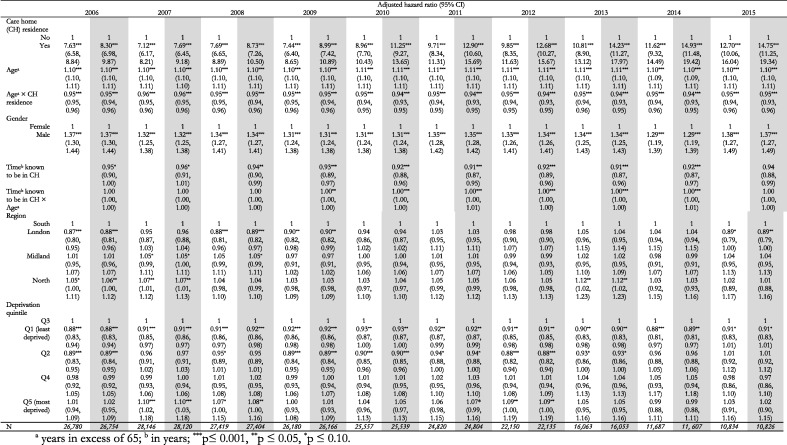
None of the time-varying covariates was statistically significant. The assumption of proportionality of the hazards was thus not rejected. Only the interaction term between age and care home residence was statistically significant. It was therefore retained in the Cox proportional hazard models which are reported in Appendix Table A8. As we would expect, mortality risk increases with age (p ≤ 0.001) and is higher for males than females (p ≤ 0.001). Adjusting for age, gender, region and deprivation quintile, care home residents have a higher mortality risk than the community-dwelling counterparts (p ≤ 0.001), although this differential diminishes as age increases. The size and statistical significance of mortality hazard ratios for region and deprivation quintile are variable but in general mortality risk is higher in the North and in more deprived areas.
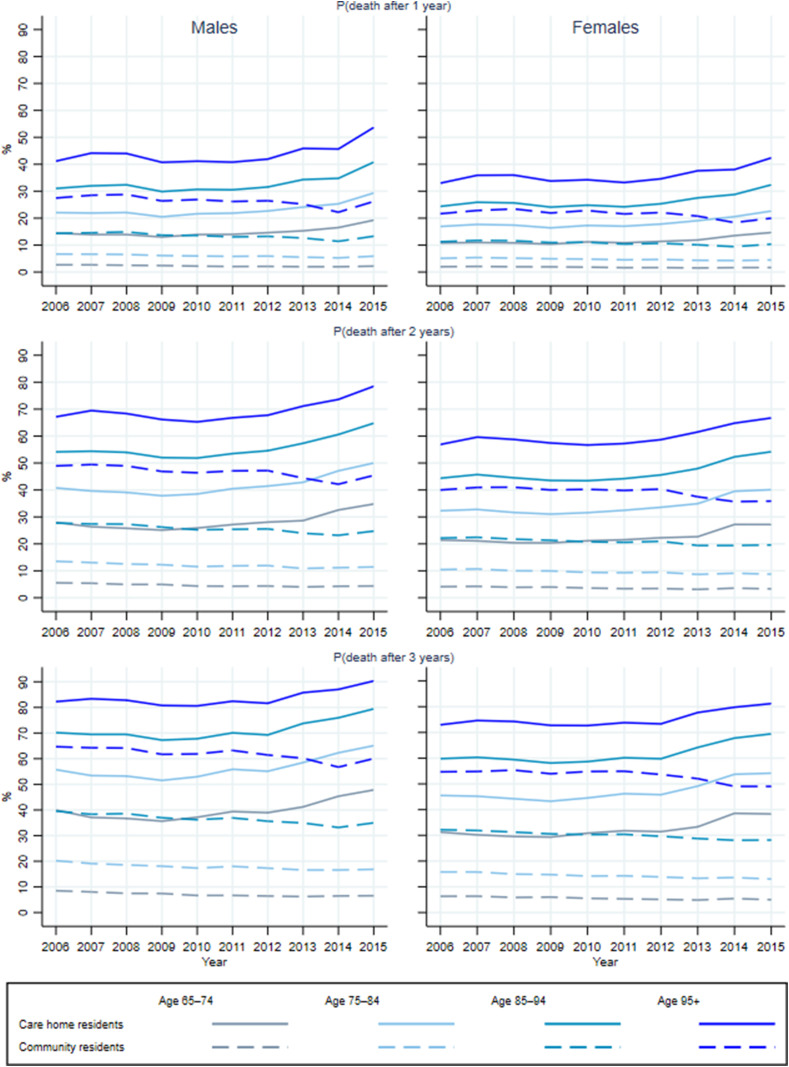
The extent to which mortality risk is higher amongst care home residents has increased over time. This is illustrated in Fig. 1 which presents gender-specific 1, 2 and 3-year adjusted mortality risks for care home residents (solid lines) and matched community-dwelling people (dashed lines), by age group and year. The adjusted mortality risks for care home residents increased over time, especially since 2012. Between 2006 and 2015, the highest proportional increases were in 1-year mortality risk for care home residents aged 65–74: 33.5% increase for males, from 14.4% to 19.3%, and 35.7% for females, from 10.8% to 14.7%. Amongst care home residents, the lowest proportional increases were in 3-year mortality risk for ages 95 or older: 9.8% increase in risk for males, from 82.3% to 90.3%, and 11.3% for females, from 73.0% to 81.2%. The proportional increase in mortality risk of care home residents between 2006 and 2015 was higher for females than for males. There was a general decrease in mortality risk for their counterparts in the community which was proportionally greater for males than females, consistent with trends in life expectancy for the general population (Kontis et al., 2017; Bennett et al., 2015).
Fig. 1.
Trends in 1, 2 and 3-year mortality risk by residence type, age group, gender and cohort.
Note: Average probabilities of death computed within gender and age group from Cox proportional hazard models of mortality adjusted for region and area deprivation quintile at year start. Solid lines represent care home residents, dashed lines represent community residents.
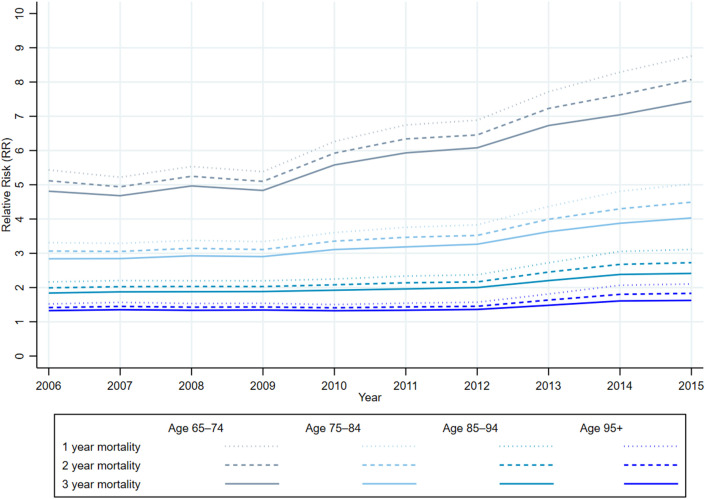
The widening of the mortality risk differential is illustrated in Fig. 2 which plots the adjusted relative risks (RRs) of 1, 2 and 3-year mortality associated with care home residence. Between 2006 and 2015, RRs increased especially for younger ages and shorter follow-up periods. The greatest change in RR over the decade was for ages 65–74 in 1-year mortality (3.3 increase in average RR and 61.2% proportional increase), and the lowest change was for 3-year mortality at ages 95 and over (0.3 and 22.5% respectively). There were practically no differences in RR by gender (the interaction term between gender and care home residence was not significant in any of the yearly Cox models). Relative mortality risks were smaller at older ages and when using longer follow-up periods in all years.
Fig. 2.
Trends in 1, 2 and 3-year adjusted relative mortality risk of care home vs community residence by age group and year.
Note: Average relative risks within age group computed from the Cox proportional hazard model as the ratio of the average mortality risk for care home residents to the average mortality risk for community residents within age group, adjusted for gender, region and area deprivation quintile at year start.
Adjusting also for the length of time before year start since the first record of care home residence produced no major change in hazard rate ratios (HRs) associated with care home residence, age and gender, or in their trends over time (Appendix Table A8). The HRs associated with care home residence were higher for shorter periods of known previous residence in a care home, and changed little over time.
The less restrictive identification of care home residents resulted in lower hazard ratios associated with care home residence than those in the main analysis, especially in the early years (Appendix Table A9). These hazard ratios increased faster over time than for the main analysis but similarly the increase was most pronounced at younger ages and for shorter follow-up periods. This sensitivity analysis thus confirms the existence of an increase over time in the adjusted relative risk of mortality for care home residents which if anything may be underestimated in the main analysis.
4. Discussion
This study provides for the first time evidence on trends in the survival gap between older (aged 65+) care home residents and similar (in terms of age group, gender, region and area deprivation) community-dwelling people in England over a ten year period prior to the start of the COVID-19 pandemic. It thus provides a baseline against which trends post-COVID-19 can be compared. Using a multi-cohort observational study design and taking account of age, gender, region, and area deprivation, we detected, between 2006 and 2015, an increase in the mortality risk of older care home residents (especially after 2011 and being higher for females), combined with a slight decrease in mortality for their counterparts not living in care homes. As a result, we found a rising trend in the relative risk of mortality associated with care home residence, which was greater at younger ages, for shorter rather than longer follow-up periods and for shorter known periods of care home residence. The greatest change in the RR associated with care home residence over the decade was for ages 65–74 in 1-year mortality (an increase of 61% from 5.4 to 8.8); the lowest changes were for 3-year mortality at the oldest ages 95 and over (from 1.3 to 1.6 or 22%). Our findings indicate that older care home residents in England have not enjoyed the same increases in longevity as similar community-dwelling older people. This would be consistent with postponement of care home entry until greater health deterioration has occurred. That the largest differentials are at younger ages and for shorter follow-up periods suggests that care home residence at younger ages may be increasingly confined to those in poorest health and closest to death. We tested the effect of additionally adjusting for the length of time before year start since the first record of care home residence, and we detected no major change in trends in mortality hazard rate ratios (care home vs community) associated with age or gender. Mortality hazard rate ratios associated with known shorter care home residency were higher than those associated with known longer residency although did not change much over time (Appendix Table A8).
One-year survival estimates from Shah et al. (2013) were consistent with ours for 2008–2009. The detected decrease in survival of care home residents is consistent with Swedish and Belgian studies (Sund Levander et al., 2016; Schon et al., 2016; Poulain et al., 2020) and with an increase in dependency/frailty levels for care home residents in the US (Katz, 2011) and in England (Matthews et al., 2016). The greater increase in relative risk of mortality associated with care home residence for shorter follow-up periods is compatible with an increase in short-term mortality as has been reported in Sweden between 2006 and 2012 (Schon, 2016) and in Belgium between 1991-1993 and 2010–2012 for older people in collective households (Poulain et al., 2020).
The strengths of this study are the use of ten consecutive (relatively large) cohorts of older care home residents; and the study of trends in their survival in comparison with community-dwelling people with similar demographic and socio-economic characteristics. We showed the validity of our residence identification and resulting yearly cohorts through a generally favourable demographic comparison with the limited available official statistics on the age and gender composition of the older care home population. Sensitivity analysis using a less restrictive identification of care home residents strongly supported the main finding of an increase in relative mortality risk associated with care home residence. The use of recent and representative data, like the primary care data in this study, is fundamental, given the continuously changing nature of health and social care policies, services, and users.
The lack of an unambiguous marker of care home residence in CPRD is a limitation and may be the cause of our under-identification of care home residents in 2011 when compared with the Population Census. Additionally, we cannot rule out some bias in our cohorts in dimensions against which we have not been able to validate the sample due to practice and patient selection (limited by their participation in CPRD) and any differential recording of care home residence across practices. The socio-economic variables used in the matching of care home to community residents were constrained by those available in CPRD so that we could not include some socio-economic factors known to be associated with care home residence such as marital status, availability of informal carers, housing tenure and education (Grundy and Jitlal, 2007; Matthews et al., 2016). Future research would benefit from an improvement in recording of care home residence in CPRD and ideally from an annual census of care home residents as exists currently in Scotland (PHS, 2020).
In many countries, health and social care policy has emphasised enabling older people to live in their own homes (e.g. Colombo et al., 2011; European Commission, 2015; DHSC, 2020; Humphries et al., 2016). Over recent years older care home residents have tended to be older and with higher disability and poorer health (Humphries et al., 2016; Katz, 2011; Matthews et al., 2016; Sund Levander et al., 2016) resulting in an increase in their mortality. In combination with the increase in longevity of the general population in those countries, an increasing trend in mortality for care home residents relative to mortality for community-dwelling residents is likely to occur not only in England but in many other countries.
The policy and practice implications of higher absolute and relative mortality amongst care home residents depend in part on the underlying determinants of this trend. Some of the implications concern policies and practice within care homes. Increasing mortality rates imply higher rates of turnover with business consequences for care home owners/managers, and practice implications for the support of staff and residents in such an environment. If higher mortality rates are the result of people entering care homes in poorer health, perhaps partly because of changing admission criteria for publicly-funded residents (Commission on Funding Care and Support, 2011b), there are implications for the nature of care and support of this increasingly frail population with an enhanced need for appropriate end-of-life care in care homes. At a time (pre-COVID-19) when mortality rates for the general population have been falling, the question of whether, and how, the opposite trend in care homes can be stemmed has become especially poignant since the advent of the COVID-19 pandemic.
Understanding trends in mortality rates in care homes is also relevant for national policies on funding care and support for older people. In England proposals for reform have sought to address perceived injustices when residents have to deplete their savings to pay for care. Appraisal of reforms such as a lifetime cap on how much individuals are required to contribute to their care costs needs better data than currently exist on lengths of stay in care homes (Commission on Funding Care and Support, 2011a; Idriss et al., 2020). If associated with delayed care home entry, increased mortality in care homes suggests falling lengths of stay in care homes with implications for both the costs and benefits of such reforms both now and in the future.
We did not set out to examine trends in the causes of mortality amongst older care home residents, such as changing health profiles, and this is an obvious topic for future research which will be especially important in disentangling the impact of COVID-19 on mortality in care homes compared with the community from other trends. The evidence presented here provides a baseline as well as being useful to inform health and social care policy and practice in areas such as those discussed above.
Funding
This study was funded by the Economic and Social Research Council (ESRC) through the Business and Local Government Data Research Centre (grant number ES/L011859/1). RH was also supported by the ESRC Research Centre on Micro-Social Change (grant number RES-518-28-5001). MM was also supported by the National Institute for Health Research (NIHR) Applied Research Collaboration for Greater Manchester. The funders had no involvement in study design, data collection, interpretation of data, writing or decision to submit for publication. All responsibility for data analysis, interpretation and any errors rests with the authors.
Ethics
Access to CPRD data is subject to protocol approval by an Independent Scientific Advisory Committee (ISAC https://www.gov.uk/government/groups/independent-scientificadvisory-committee-for-mhra-database-research) and onward data sharing is not allowed. Our ISAC approved study protocol had reference number 17_157RAR.
Credit author statement
Ferran Espuny Pujol: Conceptualization, Data Curation, Formal analysis, Methodology, Software, Visualization, Writing - Original Draft, Writing - Review & Editing. Ruth Hancock: Conceptualization, Funding acquisition, Methodology, Project administration, Software, Supervision, Visualization, Writing - Original Draft, Writing - Review & Editing. Marcello Morciano: Conceptualization, Funding acquisition, Methodology, Software, Visualization, Writing - Original Draft, Writing - Review & Editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.113883.
Appendix Contributions.
Table A1.
Details of the search for trends in survival of older care home residents using Ovid MEDLINE® (1946 to November 20, 2020) and Embase (1974 to 2020 November 20): step number, search performed at each step, and number of results obtained.
| Step | Search | Results |
|---|---|---|
| 1 | exp mortality/ or exp survival/ | 2425473 |
| 2 | ("length of stay" or death* or dying or mortality or survival).ab,kw,ti. | 5456428 |
| 3 | 1 or 2 | 6016058 |
| 4 | (old or older or elder or "65 and above" or "65 and over").ab,kw,ti. | 3560782 |
| 5 | ("care home" or "care homes" or "nursing home" or "nursing homes" or "residential home" or "residential homes" or "residential institution" or "residential institutions").ab,kw,ti. | 81444 |
| 6 | 3 and 4 and 5 | 5620 |
| 7 | remove duplicates from 6 | 3653 |
| 8 | 7 and 2005:2020.(sa_year). | 2923 |
| 9 | (trend* or chang*).ab,kw,ti. | 7942367 |
| 10 | 9 and 10 | 587 |
Notes: We used Ovid to search Embase and MEDLINE for articles published from January 01, 2005, to November 20, 2020, with no language restrictions, related to recent trends in survival or length of stay for older people living in care homes. We subsequently excluded duplicates and reviews (67), non-mortality articles (further 363), those focused on specific causes of mortality (further 122) or unrelated to care home residents (further 13); the remaining 22 articles considered relevant are summarised in the main text, none was found addressing trends in all-cause mortality of older care home residents.
Table A2.
CPRD codes used to identify care home residence. Read codes used in the detection of care home residence/admission (R), visit/consultation taking place in a care home (V), and to detect past care home residence happened or at death (P).
| Medical code | Read code | Read term | Type |
|---|---|---|---|
| 27425 | 13F5.00 | Part III accommodation | R |
| 36096 | 13F5.11 | Part 3 accommodation | R |
| 27360 | 13F5100 | Part III accommodation arranged | R |
| 66122 | 13F5111 | Part 3 accommodation arranged | R |
| 21280 | 13F5200 | Resident in part III accommodation | R |
| 13360 | 13F6.00 | Nursing/other home | R |
| 13359 | 13F6100 | Lives in a nursing home | R |
| 27968 | 13F7.00 | Residential institution | R |
| 15840 | 13F7100 | Lives in a welfare home | R |
| 11419 | 13F7200 | Lives in an old people’s home | R |
| 24956 | 13FK.00 | Lives in a residential home | R |
| 52249 | 13FQ.00 | Lives on council site | R |
| 59548 | 13FT.00 | Lives in an old people’s home | R |
| 68005 | 13FV.00 | Lives in a welfare home | R |
| 49681 | 13FX.00 | Lives in care home | R |
| 102493 | 8Ht..00 | Admission to nursing home | R |
| 108525 | 9kw..00 | Care home enhanced services administration | R |
| 107443 | 9NFW000 | Care home visit for initial patient assessment | R |
| 107602 | 9NFW100 | Care home visit for follow-up patient review | R |
| 24816 | Z177C00 | Residential care | R |
| 53140 | Z177D00 | Local authority residential care | R |
| 24828 | Z177F00 | Nursing home care | R |
| 42191 | ZLG3.00 | Discharge to residential home | R |
| 48549 | ZLG3100 | Discharge to private residential home | R |
| 69028 | ZLG3200 | Discharge to part III residential home | R |
| 10993 | ZLG4.00 | Discharge to nursing home | R |
| 43915 | ZLG4100 | Discharge to private nursing home | R |
| 54948 | ZLG5200 | Discharge to part III accommodation | R |
| 13562 | ZV70317 | [V]Old age home admission medical | R |
| 93998 | 9b0i.00 | Residential home visit note | V |
| 73083 | 9b0Y.00 | Nursing home visit note | V |
| 73321 | 9b1P.00 | Nursing home | V |
| 17782 | 9N16.00 | Seen in institution | V |
| 50792 | 9N1F.11 | Seen in Part 3 accommodation | V |
| 7101 | 9N1F.12 | Seen in old people’s home February 2009 | V |
| 7653 | 9N1G.00 | Seen in nursing home | V |
| 35279 | 9N1H.00 | Seen in Elderly Mentally Infirm home | V |
| 101003 | 9NFR.00 | Home visit request by residential institution | V |
| 107757 | 9NFW.00 | Care home visit | V |
| 39311 | 9492 | Patient died in part 3 accom. | P |
| 6991 | 9493 | Patient died in nursing home | P |
| 26812 | 9494 | Patient died in resid.inst.NOS | P |
| 98758 | 13Zo.00 | Previously lived in care home | P |
| 101078 | 949D.00 | Patient died in care home | P |
Notes: Shah et al. (2010) used the subset of Care Home Residence codes “13F5. - 13F72, 13FK., 13FT., 13FV., 13FX.”. Read Term misspelling errors found in CPRD were corrected in this table. Codes indicating residence in sheltered accommodation or supported homes were not considered as care home residence codes.
Table A3.
Numbers of practices and older patients before and after requiring a 3-year follow-up and within the latter percentages of patients in each residence group (CH=care home, Com.=community, Undet.=undetermined, Excl.=excluded) for the main and sensitivity analyses.
| Cohort start year | All practices |
Practices with 3-year follow-up |
Patients’ Residence (practices with 3-year follow-up) |
Alternative identification of care home residents used in sensitivity analysis (practices with 3-year follow-up) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
N Practices |
N Patients |
N Practices |
N Patients |
% Com. |
% CH |
% Undet. |
% Excl. |
% Com. |
% CH |
% Undet. |
% Excl. |
|
| 2006 | 350 | 486,230 | 342 | 476,855 | 92.8 | 1.4 | 5.2 | 0.6 | 92.8 | 3.7 | 2.9 | 0.6 |
| 2007 | 353 | 493,463 | 339 | 475,045 | 93.2 | 1.5 | 4.8 | 0.6 | 93.2 | 3.6 | 2.7 | 0.6 |
| 2008 | 361 | 505,784 | 332 | 466,922 | 93.5 | 1.5 | 4.4 | 0.6 | 93.5 | 3.5 | 2.4 | 0.6 |
| 2009 | 356 | 507,500 | 315 | 449,165 | 93.9 | 1.5 | 4.1 | 0.6 | 93.9 | 3.2 | 2.3 | 0.6 |
| 2010 | 353 | 511,704 | 298 | 437,485 | 94.3 | 1.5 | 3.7 | 0.6 | 94.3 | 3.0 | 2.1 | 0.6 |
| 2011 | 339 | 498,799 | 267 | 397,888 | 94.4 | 1.6 | 3.4 | 0.6 | 94.4 | 3.0 | 2.0 | 0.6 |
| 2012 | 326 | 488,668 | 215 | 330,630 | 94.6 | 1.7 | 3.2 | 0.6 | 94.6 | 2.9 | 1.9 | 0.6 |
| 2013 | 311 | 481,975 | 151 | 239,594 | 95.1 | 1.7 | 2.6 | 0.6 | 95.1 | 2.7 | 1.6 | 0.6 |
| 2014 | 277 | 439,411 | 111 | 166,851 | 95.9 | 1.8 | 1.8 | 0.5 | 95.9 | 2.4 | 1.2 | 0.5 |
| 2015 | 224 | 361,491 | 86 | 133,182 | 96.2 | 2.1 | 1.2 | 0.5 | 96.2 | 2.5 | 0.8 | 0.5 |
Note: The Main analysis (and adjusting additionally for the time known in care home) use the identification with results in the middle of the table, while Sensitivity Analysis (less restrictive identification of care home residents) uses the identification reported at the right of the table.
Table A4.
Care home residence rates (%) and composition of care home residents by age and gender, England 2011: Census and CPRD sample before matching (practices with 3-year follow-up) for the main and sensitivity analysis.
| Age | Female | Male | Region | |||||||
| 65–74 |
75–84 |
85+ |
65+ |
65+ |
65+ |
South |
London |
Midlands |
North |
|
| % |
||||||||||
| Care home residency rates | ||||||||||
| Census | 0.6 | 2.8 | 13.7 | 3.2 | 4.2 | 1.9 | 3.4 | 2.5 | 3.0 | 3.3 |
| CPRD sample | 0.3 | 1.4 | 6.4 | 1.6 | 2.1 | 0.9 | 1.7 | 1.3 | 1.6 | 1.5 |
| CPRD sensitivity | 0.5 | 2.8 | 12.5 | 3.0 | 4.0 | 1.8 | 3.5 | 2.1 | 2.7 | 2.8 |
| Composition of care home residents | ||||||||||
| Census | 10.5 | 30.3 | 59.2 | 100.0 | 73.6 | 26.4 | 31.6 | 8.2 | 30.0 | 30.2 |
| CPRD sample | 11.1 | 30.7 | 58.2 | 100.0 | 73.9 | 26.1 | 47.4 | 10.3 | 23.6 | 18.8 |
| CPRD sensitivity | 9.1 | 31.4 | 59.5 | 100.0 | 73.9 | 26.1 | 52.6 | 8.9 | 20.7 | 17.8 |
Note: The CPRD samples are used for building the matched cohorts used in the Main analysis (and adjusting additionally for the time known in care home), while the “CPRD sensitivity” sample is used for building the matched cohorts in the Sensitivity Analysis #2 (less restrictive identification of care home residents).
Table A5.
CPRD matched care home residents with 3-year follow-up by age and gender.
| Cohort start year | N | Age |
Female |
Males by Age |
Females by Age |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 65–74 |
75–84 |
85+ |
65–74 |
75–84 |
85+ |
65–74 |
75–84 |
85+ |
|||
| % | |||||||||||
| 2006 | 6,701 | 9.9 | 34.6 | 55.4 | 76.1 | 18.2 | 42.0 | 39.6 | 7.3 | 32.3 | 60.4 |
| 2007 | 7,043 | 10.2 | 33.4 | 56.4 | 76.1 | 18.3 | 39.5 | 42.2 | 7.6 | 31.5 | 60.9 |
| 2008 | 6,863 | 10.4 | 33.1 | 56.5 | 75.7 | 18.8 | 41.8 | 39.3 | 7.6 | 30.3 | 62.0 |
| 2009 | 6,553 | 10.7 | 32.5 | 56.7 | 75.5 | 20.5 | 39.1 | 40.2 | 7.5 | 30.4 | 62.1 |
| 2010 | 6,393 | 11.1 | 31.9 | 57.0 | 75.1 | 21.7 | 38.5 | 39.8 | 7.6 | 29.7 | 62.7 |
| 2011 | 6,209 | 11.2 | 30.9 | 57.9 | 73.8 | 21.4 | 36.1 | 42.4 | 7.5 | 29.0 | 63.4 |
| 2012 | 5,542 | 10.7 | 29.6 | 59.7 | 74.1 | 20.9 | 34.3 | 44.6 | 7.1 | 28.0 | 64.9 |
| 2013 | 4,024 | 11.4 | 29.4 | 59.0 | 73.9 | 20.9 | 34.3 | 44.5 | 8.1 | 27.7 | 64.2 |
| 2014 | 2,931 | 12.7 | 29.2 | 58.0 | 71.9 | 23.1 | 33.4 | 43.0 | 8.6 | 27.5 | 63.9 |
| 2015 | 2,714 | 13.5 | 29.0 | 57.4 | 69.6 | 23.3 | 35.0 | 41.6 | 9.3 | 26.4 | 64.4 |
Table A6.
CPRD matched care home residents with 3-year follow-up by quintile of 2015 Index of Multiple Deprivation.
| Cohort start year | % in each quintile of 2015 Index of Multiple Deprivation |
||||
|---|---|---|---|---|---|
| Q1 (least deprived) | Q2 | Q3 | Q4 | Q5 (most deprived) | |
| 2006 | 19.5 | 21.5 | 23.5 | 19.6 | 16.0 |
| 2007 | 19.6 | 21.6 | 25.2 | 18.9 | 14.7 |
| 2008 | 20.2 | 21.3 | 26.5 | 18.1 | 13.9 |
| 2009 | 19.9 | 22.2 | 25.7 | 18.4 | 13.8 |
| 2010 | 20.1 | 21.2 | 27.1 | 18.8 | 12.8 |
| 2011 | 19.8 | 22.7 | 27.9 | 17.2 | 12.5 |
| 2012 | 17.2 | 25.8 | 26.6 | 18.3 | 12.1 |
| 2013 | 17.1 | 21.7 | 29.7 | 19.4 | 12.1 |
| 2014 | 20.2 | 19.5 | 35.0 | 13.3 | 12.1 |
| 2015 | 21.6 | 21.3 | 32.8 | 12.5 | 11.8 |
Table A7.
CPRD matched care home residents with 3-year follow-up by Region.
| Cohort start year | % in each Region |
|||
|---|---|---|---|---|
| South | London | Midlands and East | North | |
| 2006 | 44.9 | 9.0 | 20.5 | 25.6 |
| 2007 | 45.2 | 7.9 | 21.9 | 25.0 |
| 2008 | 45.9 | 8.6 | 20.8 | 24.7 |
| 2009 | 45.6 | 8.1 | 22.4 | 24.0 |
| 2010 | 47.4 | 9.8 | 22.8 | 20.0 |
| 2011 | 47.4 | 10.3 | 23.6 | 18.7 |
| 2012 | 51.0 | 9.4 | 23.8 | 15.8 |
| 2013 | 52.0 | 12.5 | 21.9 | 13.6 |
| 2014 | 47.1 | 15.4 | 26.1 | 11.4 |
| 2015 | 52.0 | 12.0 | 28.3 | 7.7 |
Table A8.
Cox Proportional Hazard Rate ratio estimates for predictors of mortality: main models (unshaded) and models including covariates for known time in a care home (shaded).
Table A9.
Cox Proportional Hazard Rate ratio estimates for predictors of mortality: sensitivity analysis using a less restrictive identification of care home residence.
| Adjusted hazard ratio (95% CI) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
| Care home (CH) residence | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 4.92∗∗∗ (4.43, 5.45) | 5.16∗∗∗ (4.65, 5.72) | 6.31∗∗∗ (5.66, 7.03) | 6.83∗∗∗ (6.10, 7.64) | 7.71∗∗∗ (6.87, 8.65) | 9.16∗∗∗ (8.11, 10.35) | 9.73∗∗∗ (8.50, 11.14) | 12.43∗∗∗ (10.55, 14.64) | 12.56∗∗∗ (10.32, 15.29) | 11.76∗∗∗ (9.54, 14.50) |
| Agea | 1.10∗∗∗ (1.10, 1.11) | 1.10∗∗∗ (1.10, 1.10) | 1.11∗∗∗ (1.10, 1.11) | 1.11∗∗∗ (1.10, 1.11) | 1.11∗∗∗ (1.10, 1.11) | 1.11∗∗∗ (1.11, 1.11) | 1.11∗∗∗ (1.10, 1.11) | 1.11∗∗∗ (1.10, 1.11) | 1.10∗∗∗ (1.09, 1.11) | 1.10∗∗∗ (1.09, 1.10) |
| Agea × CH residence | 0.96∗∗∗ (0.96, 0.97) | 0.96∗∗∗ (0.96, 0.97) | 0.96∗∗∗ (0.95, 0.96) | 0.95∗∗∗ (0.95, 0.96) | 0.95∗∗∗ (0.95, 0.96) | 0.95∗∗∗ (0.94, 0.95) | 0.95∗∗∗ (0.94, 0.95) | 0.94∗∗∗ (0.94, 0.95) | 0.95∗∗∗ (0.94, 0.96) | 0.95∗∗∗ (0.94, 0.96) |
| Gender | ||||||||||
| Female | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Male | 1.35∗∗∗ (1.31, 1.39) | 1.30∗∗∗ (1.26, 1.35) | 1.33∗∗∗ (1.28, 1.37) | 1.32∗∗∗ (1.28, 1.37) | 1.32∗∗∗ (1.27, 1.37) | 1.31∗∗∗ (1.26, 1.37) | 1.35∗∗∗ (1.29, 1.41) | 1.36∗∗∗ (1.29, 1.43) | 1.31∗∗∗ (1.23, 1.40) | 1.38∗∗∗ (1.28, 1.48) |
| Region | ||||||||||
| South | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| London | 1.05 (0.99, 1.11) | 1.11∗∗∗ (1.05, 1.18) | 1.00 (0.94, 1.06) | 1.08∗∗ (1.01, 1.14) | 1.01 (0.95, 1.08) | 1.06∗ (0.99, 1.12) | 0.99 (0.92, 1.06) | 1.07∗ (0.99, 1.17) | 1.01 (0.92, 1.11) | 0.90∗ (0.80, 1.01) |
| Midland | 1.05∗∗∗ (1.01, 1.09) | 1.04∗ (1.00, 1.08) | 1.03 (0.99, 1.07) | 1.00 (0.96, 1.04) | 1.00 (0.96, 1.05) | 1.04∗ (0.99, 1.08) | 1.02 (0.98, 1.07) | 1.02 (0.96, 1.08) | 0.99 (0.92, 1.06) | 1.04 (0.96, 1.13) |
| North | 1.17∗∗∗ (1.12, 1.21) | 1.16∗∗∗ (1.12, 1.21) | 1.10∗∗∗ (1.06, 1.14) | 1.09∗∗∗ (1.04, 1.13) | 1.09∗∗∗ (1.05, 1.14) | 1.07∗∗∗ (1.02, 1.12) | 1.13∗∗∗ (1.06, 1.19) | 1.17∗∗∗ (1.08, 1.26) | 1.06 (0.96, 1.18) | 1.09 (0.96, 1.25) |
| Deprivation quintile | ||||||||||
| Q3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q1 (least deprived) | 0.93∗∗∗ (0.89, 0.97) | 0.94∗∗∗ (0.90, 0.99) | 0.92∗∗∗ (0.88, 0.96) | 0.91∗∗∗ (0.87, 0.95) | 0.94∗∗ (0.90, 0.99) | 0.91∗∗∗ (0.87, 0.96) | 0.93∗∗ (0.88, 0.98) | 0.91∗∗∗ (0.85, 0.98) | 0.88∗∗∗ (0.81, 0.95) | 0.91∗∗ (0.83, 1.00) |
| Q2 | 0.96∗∗ (0.92, 1.00) | 0.98 (0.94, 1.02) | 0.96∗ (0.92, 1.01) | 0.95∗∗ (0.90, 0.99) | 0.96∗ (0.92, 1.00) | 0.94∗∗∗ (0.89, 0.98) | 0.95∗ (0.90, 1.00) | 1.02 (0.96, 1.09) | 0.99 (0.92, 1.08) | 1.07 (0.97, 1.17) |
| Q4 | 1.01 (0.96, 1.06) | 1.03 (0.99, 1.08) | 1.01 (0.96, 1.06) | 1.02 (0.97, 1.07) | 1.03 (0.97, 1.08) | 0.98 (0.93, 1.04) | 0.99 (0.93, 1.05) | 1.00 (0.93, 1.07) | 1.09 (0.98, 1.21) | 0.99 (0.88, 1.11) |
| Q5 (most deprived) |
1.07∗∗∗ (1.02, 1.13) |
1.13∗∗∗ (1.08, 1.19) |
1.06∗∗ (1.01, 1.12) |
1.02 (0.96, 1.08) |
1.07∗∗ (1.01, 1.13) |
1.06∗ (1.00, 1.12) |
1.06∗ (0.99, 1.13) |
1.09∗∗ (1.00, 1.18) |
1.06 (0.96, 1.18) |
1.01 (0.90, 1.14) |
| N | 66,079 | 65,047 | 62,100 | 55,729 | 51,525 | 46,134 | 37,475 | 25,095 | 15,178 | 12,333 |
a years in excess of 65; ∗∗∗p≤ 0.001, ∗∗p ≤ 0.05, ∗p ≤ 0.10.
Appendix B. Supplementary data
The following are the Supplementary data to this article:
References
- Bennett J.E., Li G., Foreman K., et al. The future of life expectancy and life expectancy inequalities in England and Wales: bayesian spatiotemporal forecasting. Lancet. 2015;386(9989):163–170. doi: 10.1016/S0140-6736(15)60296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castora-Binkley M., Meng H., Hyer K. Predictors of long-term nursing home placement under competing risk: evidence from the health and retirement study. J. Am. Geriatr. Soc. 2014;62(5):913–918. doi: 10.1111/jgs.12781. [DOI] [PubMed] [Google Scholar]
- Chisholm J. The Read clinical classification. Br. Med. J. 1990;300(6732):1092. doi: 10.1136/bmj.300.6732.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas Herrera A., Zalakain J., Litwin C., et al. Mortality associated with covid-19 outbreaks in care homes: early international evidence. 2020. https://ltccovid.org/wp-content/uploads/2020/06/Mortality-associated-with-COVID-among-people-who-use-long-term-care-26-June-1.pdf Article in LTC-covid.org International Long-term Care Policy Network, CPEC-LSE, 26 June 2020.
- Commission on Funding Care and Support . 2011. Fairer Care Funding.https://webarchive.nationalarchives.gov.uk/20120713201059/http://www.dilnotcommission.dh.gov.uk/files/2011/07/Fairer-Care-Funding-Report.pdf [Google Scholar]
- Commission on Funding Care and Support . 2011. Fairer Care Funding Volume II.https://webarchive.nationalarchives.gov.uk/20120803155708/https://www.wp.dh.gov.uk/carecommission/files/2011/07/Volume-II-Evidence-and-Analysis1.pdf [Google Scholar]
- DHSC . Department of Health and Social Care; London: 2020. Care and Support Statutory Guidance Updated 24 June 2020.https://www.gov.uk/government/publications/care-act-statutory-guidance/care-and-support-statutory-guidance [Google Scholar]
- European Commission . Social Investment in Europe. A Study of National Policies. European Union Publications; 2015. Directorate-general for employment, social affairs and inclusion. [Google Scholar]
- Falconer M., O'Neill D. Profiling disability within nursing homes: a census-based approach. Age Ageing. 2007;36(2):209–213. doi: 10.1093/ageing/afl185. [DOI] [PubMed] [Google Scholar]
- Forder J., Fernandez J.-L. Length of stay in care homes. 2011. http://eprints.lse.ac.uk/33895/1/dp2769.pdf Report commissioned by Bupa Care Services. Personal Social Services Research Unit Discussion paper 2769. Canterbury: PSSRU.
- Foundations Linking disabled facilities grants to social care data. Freedom Inf. Surv. Glossop: Astra PS Limited. 2015 http://foundationsweb.s3.amazonaws.com/4210/foundations-dfg-foi-report-nov-2015.pdf [Google Scholar]
- Gaugler J.E., Duval S., Anderson K.A., Kane R.L. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy E. Household transitions and subsequent mortality among older people in England and Wales: trends over three decades. J. Epidemiol. Community. 2011;65(4):353–359. doi: 10.1136/jech.2009.089383. [DOI] [PubMed] [Google Scholar]
- Grundy E., Jitlal M. Socio-demographic variations in moves to institutional care 1991–2001: a record linkage study from England and Wales. Age Ageing. 2007;36(4):424–430. doi: 10.1093/ageing/afm067. [DOI] [PubMed] [Google Scholar]
- Herrett E., Gallagher A.M., Bhaskaran K., et al. Data resource profile: clinical practive research datalink (CPRD) Int. J. Epidemiol. 2015;44(3):827–836. doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphries R., Thorlby R., Holder H., et al. The King's Fund; 2016. Social Care for Older People: Home Truths London. [Google Scholar]
- Idriss O., Tallack C., Shembavnekar N., et al. 2021. Social care funding gap.https://www.health.org.uk/news-and-comment/charts-and-infographics/REAL-social-care-funding-gap The Health Foundation. [Google Scholar]
- Katz P.R. An international perspective on long term care: focus on nursing homes. J. Am. Med. Dir. Assoc. 2011;12(7):487–492 e1. doi: 10.1016/j.jamda.2011.01.017. [DOI] [PubMed] [Google Scholar]
- Kontis V., Bennett J.E., Mathers C.D., et al. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389:1323–1335. doi: 10.1016/S0140-6736(16)32381-9. 10076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews F.E., Bennett H., Wittenberg R., et al. Who lives where and does it matter? Changes in the health profiles of older people living in long term care and the community over two decades in a high income country. PloS One. 2016;11(9) doi: 10.1371/journal.pone.0161705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morciano M., Stokes J., Kontopantelis E., et al. medRxiv. Cold Spring Harbor Laboratory Press; 2020. Excess mortality for care home residents during the first 23 weeks of the COVID-19 pandemic in England: a national cohort study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ONS . Office for National Statistics; Cardiff: 2015. Mortality statistics: metadata. [Google Scholar]
- ONS Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2019. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/latest Office for National Statistics.
- PHS . Public Health Scotland; 2020. Care Home Census for Adults in Scotland, Statistics for 2009 – 2019.https://beta.isdscotland.org/find-publications-and-data/health-and-social-care/social-and-community-care/care-home-census-for-adults-in-scotland/ [Google Scholar]
- Poulain M., Dal L., Hern A. Trends in living arrangements and their impact on the mortality of older adults. Demogr. Res. 2020;43(15):401–430. doi: 10.4054/DemRes.2020.43.15. [DOI] [Google Scholar]
- Schon P., Lagergren M., Kareholt I. Rapid decrease in length of stay in institutional care for older people in Sweden between 2006 and 2012: results from a population-based study. Health Soc. Care Community. 2016;24(5):631–638. doi: 10.1111/hsc.12237. [DOI] [PubMed] [Google Scholar]
- SCIE . Social Care Institute for Excellence; 2020. Role and Principles of Reablement.https://www.scie.org.uk/reablement/what-is/principles-of-reablement [Google Scholar]
- Shah S.M., Carey I.M., Harris T., et al. Identifying the clinical characteristics of older people living in care homes using a novel approach in a primary care database. Age Ageing. 2010;39(5):617–623. doi: 10.1093/ageing/afq086. [DOI] [PubMed] [Google Scholar]
- Shah S.M., Carey I.M., Harris T., et al. Mortality in older care home residents in England and Wales. Age Ageing. 2013;42(2):209–215. doi: 10.1093/ageing/afs174. [DOI] [PubMed] [Google Scholar]
- Smith T., Noble M., Noble S., et al. Department for Communities and Local Government; London: 2015. The English Indices of Deprivation 2015.https://www.gov.uk/government/publications/english-indices-of-deprivation-2015-technical-report Technical report. [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2015. Stata Statistical Software: Release 14. 2015. [Google Scholar]
- Steventon A., Roberts A. Estimating length of stay in publicly-funded residential and nursing care homes: a retrospective analysis using linked administrative data sets. BMC Health Serv. Res. 2012;12:377. doi: 10.1186/1472-6963-12-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sund Levander M., Milberg A., Rodhe N., et al. Differences in predictors of 5-year survival over a 10-year period in two cohorts of elderly nursing home residents in Sweden. Scand. J. Caring Sci. 2016;30(4):714–720. doi: 10.1111/scs.12284. 2016. [DOI] [PubMed] [Google Scholar]
- Symons M.J., Moore D.T. Hazard rate ratio and prospective epidemiological studies. J. Clin. Epidemiol. 2002;55(9):893–899. doi: 10.1016/s0895-4356(02)00443-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.