Abstract
Objective:
Stressful conditions within disadvantaged neighborhoods may shape unhealthy alcohol use and related harms. Yet, associations between neighborhood disadvantage and more severe unhealthy alcohol use are underexplored, particularly for subpopulations. Among national Veterans Health Administration (VA) patients (2013–2017), we assessed associations between neighborhood disadvantage and multiple alcohol-related outcomes and examined moderation by sociodemographic factors.
Method:
Electronic health record data were extracted for VA patients with a routine Alcohol Use Disorders Identification Test–Consumption (AUDIT-C) screen. Patient addresses were linked by census block group to the Area Deprivation Index (ADI), dichotomized at the 85th percentile, and examined in quintiles for sensitivity analyses. Using modified Poisson generalized estimating equations models, we estimated associations between neighborhood disadvantage and five outcomes: unhealthy alcohol use (AUDIT-C ≥ 5), any past-year heavy episodic drinking (HED), severe unhealthy alcohol use (AUDIT-C ≥ 8), alcohol use disorder (AUD) diagnosis, and alcohol-specific conditions diagnoses. Moderation by gender, race/ethnicity, and rurality was tested using multiplicative interaction.
Results:
Among 6,381,033 patients, residence in a highly disadvantaged neighborhood (ADI ≥ 85th percentile) was associated with a higher likelihood of unhealthy alcohol use (prevalence ratio [PR] = 1.06, 95% CI [1.05, 1.07]), severe unhealthy alcohol use (PR = 1.14, 95% CI [1.12, 1.15]), HED (PR = 1.04, 95% CI [1.03, 1.05]), AUD (PR = 1.14, 95% CI [1.13, 1.15]), and alcohol-specific conditions (PR = 1.21, 95% CI [1.18, 1.24]). Associations were larger for Black and American Indian/Alaska Native patients compared with White patients and for urban compared with rural patients. There was mixed evidence of moderation by gender.
Conclusions:
Neighborhood disadvantage may play a role in unhealthy alcohol use in VA patients, particularly those of marginalized racialized groups and those residing in urban areas.
Unhealthy alcohol use is a serious and increasing public health concern (Spillane et al., 2020). It is the third leading preventable cause of death in the United States (Mokdad et al., 2018) and is responsible for 1 in 10 deaths among working-age adults (Stahre et al., 2014). The spectrum of unhealthy alcohol use ranges from drinking above national recommended limits and heavy episodic drinking (HED) to meeting diagnostic criteria for alcohol use disorder (AUD; Grant et al., 2017). These patterns are associated with a range of acute consequences such as injuries, chronic conditions (Room et al., 2005), poorer mental health (Jané-Llopis & Matytsina, 2006), worse social and economic outcomes (Kendler et al., 2017), and harm to others (Karriker-Jaffe et al., 2018). Of note, the prevalence of reported unhealthy alcohol use (Dawson et al., 2015; Grant et al., 2017) and mortality from alcohol-specific conditions has increased across nearly all sociodemographic groups— contributing to startling overall increases in midlife mortality (Case & Deaton, 2017; Spillane et al., 2020; Woolf et al., 2018). Given these patterns, additional research is needed to investigate varied factors—including stressful socioeconomic conditions—that may influence unhealthy alcohol use.
The proportion of persons residing in neighborhoods with concentrated neighborhood disadvantage in the United States increased during the 2007–2009 Great Recession and has remained at those levels (Kneebone & Holmes, 2016). This has implications for well-being, in that disadvantaged neighborhoods may expose residents to disproportionate stressors within built and social environments (e.g., more limited access to essential services, violence) above and beyond individual experiences of poverty (Diez Roux & Mair, 2010). Chronic stress and psychological distress (Petteway et al., 2019), social norms (Cohen et al., 2000), and alcohol availability (Bryden et al., 2012) are interrelated mechanisms that may link neighborhood disadvantage and patterns of unhealthy alcohol use. Neighborhood disadvantage is associated with biological markers indicative of chronic stress (Ribeiro et al., 2018) and has been linked to increased psychological distress (Boardman et al., 2001). Concentrated disadvantage could erode the ability of communities to realize common values, creating more violent and psychologically distressing environments (Joshi et al., 2017) that could shape unhealthy alcohol use (Cambron et al., 2017). Beyond stress and psychological distress–related mechanisms, neighborhood disadvantage is associated with more permissive social norms around drinking (Ahern et al., 2008) and higher alcohol retail density (Berke et al., 2010), which could work synergistically (Ahern et al., 2015).
A growing number of studies have examined the role of neighborhood context in patterns of unhealthy alcohol use and alcohol-related outcomes with mixed findings (Jackson et al., 2014; Karriker-Jaffe, 2011; Mair et al., 2019). This is likely attributable to varying definitions of neighborhoods (Duncan & Kawachi, 2018), differing neighborhood disadvantage measures, alcohol-related outcomes studied (e.g., frequency vs. quantity vs. problems; Karriker-Jaffe, 2011; Kendler et al., 2014), and the timing of the life course in which neighborhood conditions are assessed (Barr, 2018). Studies that examine moderation by individual sociodemographic characteristics may help explain heterogeneous findings and inform targeted interventions (Karriker-Jaffe et al., 2012).
Associations between neighborhood disadvantage and unhealthy alcohol use are complex and likely depend on the characteristics of both places and individuals (Karriker-Jaffe et al., 2012). In particular, rurality, gender, and race/ethnicity may play salient moderating roles in the relationship between neighborhood disadvantage and unhealthy alcohol use. As observed for other behavioral health outcomes (Rudolph et al., 2014), neighborhood disadvantage and unhealthy alcohol use may have a more pronounced relationship in more urban areas because of distinct characteristics of social and built environments in disadvantaged urban neighborhoods (e.g., safety and policing concerns). In studies examining moderation by gender identity (or those using sex as a proxy for gender identity), associations between neighborhood disadvantage and unhealthy alcohol use among men have tended to be larger, potentially because of gendered social norms around drinking (Karriker-Jaffe et al., 2012); however, women may be more adversely affected by the stress of neighborhood disadvantage (Barrington et al., 2014). Neighborhood disadvantage may also be more strongly associated with unhealthy alcohol use for marginalized racialized groups (Chauhan et al., 2016; Jones-Webb et al., 1997; Karriker-Jaffe et al., 2012), potentially because of the compounding of disadvantages faced by people with multiple marginalized identities.
Electronic health record (EHR) data increasingly facilitate social epidemiologic (Schinasi et al., 2018) and health care disparities research (Glass & Williams, 2018). These data may be particularly valuable for studies of populations with stigmatized health conditions, such as AUD (Glass et al., 2014; Keyes et al., 2010), where broad-scale research recruitment may be particularly challenging (Casey et al., 2016). The Veterans Health Administration (VA) serves more than 9 million patients at 138 medical centers and more than 900 clinics and is the largest integrated health care system in the United States. VA patients tend to be from more disadvantaged groups (Nelson et al., 2007), and AUD prevalence among VA outpatients is higher than the prevalence among veterans in the general population (Hoggatt et al., 2021). The VA is a leader in implementing universal, population-based alcohol screening annually with a three-item instrument, the Alcohol Use Disorders Identification Test–Consumption (AUDIT-C), which enables measurement of several patterns of unhealthy alcohol use (Bradley et al., 2007). We used VA EHR data to examine associations between neighborhood disadvantage, measured with a composite index at the census block group level, and multiple patterns of unhealthy alcohol use, which have not previously been examined in a single study. Because the role of neighborhood disadvantage on unhealthy alcohol use may vary across populations, and given the sample size afforded by the EHR data, we also assessed whether associations identified differed by gender, race/ethnicity, and rurality.
Method
Data sources
Data for the present study included VA EHR data linked to the Area Deprivation Index (ADI), a composite measure of neighborhood socioeconomic status (SES). VA EHR data were extracted from the VA’s Corporate Data Warehouse (CDW)—a national VA data repository that contains sociodemographic, clinical, enrollment, pharmacy, and utilization data, including geocoded patient residential addresses—for a parent study that included all patients 18 years and older who had an outpatient appointment October 1, 2009, to July 31, 2017, and one or more documented routine alcohol screens (AUDIT-Cs). Patient residential addresses from enrollment data in the CDW are geocoded annually for operations, budgeting, and research use by the VA Planning Systems Support Group using ArcGIS for Server software and the most extensive commercially available address location database.
Study population
Patients from the parent study were included in the present study if they had a last documented alcohol screen (AUDIT-C) between 2013 and 2017 because geocoded data are more accurate in those years, given transitions in geocoding technology and vendors and less stringent address matching standards in prior years (U.S. Department of Veterans Affairs, 2016). Patients also had to have a reliably geocoded residential address and live in a census block group with sufficient population size or count of housing units to be matched to a valid ADI. Of the 6,525,332 patients with a last documented alcohol screen between 2013 and 2017, 134,464 (2%) were excluded because they did not have a reliably geocoded residential address, and 9,835 (0.2%) were excluded because they did not live in a census block with a sufficient population to generate a valid ADI. The final analytic sample for the present study included 6,381,033 patients with geocoded data linked to a census block group who had a last AUDIT-C screen between 2013 and 2017. The present study was approved by the VA Puget Sound Institutional Review Board and the University of Washington and University of Pittsburgh Institutional Review Boards.
Independent variable: Neighborhood disadvantage Area Deprivation Index
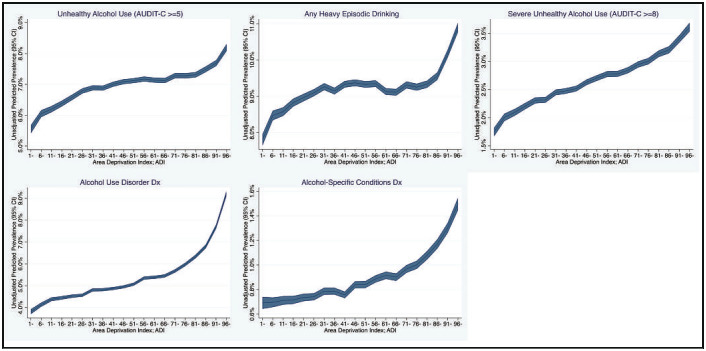
Neighborhood disadvantage has long been used to indicate the lived experience of social hardship, capturing interrelated community-level conditions of poverty, inadequate housing, and poor employment quality (Gordon, 2003). The ADI is a composite measure of neighborhood SES based on the widely used Singh Deprivation Index methodology, in which census indicators theoretically related to SES and health disparities were selected, and factor analysis and principal components analysis were used to construct a composite index (Singh, 2003). The ADI was developed and made publicly available by researchers at the University of Wisconsin (Kind & Buckingham, 2018) and is based on 17 domains of SES (Supplemental Figure 1) derived from the U.S. Census Bureau’s American Community Survey (ACS) 5-year estimates at the census block group level. (Supplemental material appears as an online-only addendum to the article on the journal’s website.) Census block groups are the smallest available geographic unit of analysis, typically ranging from 600 to 3,000 individuals, and likely capture individual-level exposure to neighborhood disadvantage more adequately than larger census units (Duncan & Kawachi, 2018). Patients were linked by their census block group Federal Information Processing Series code to an ADI percentile based on a national ranking and the year of their AUDIT-C screen (2013–2014 linked to ADI based on 2009–2013 ACS estimates; 2015–2017 linked to ADI based on 2011–2015 ACS estimates). Given that preliminary descriptive analyses (Figure 1) and previous national analyses found a nonlinear relationship between ADI and health outcomes (Durfey et al., 2019; Hu et al., 2018; Kind et al., 2014)—with a marked increase among individuals residing in the top 15th percentile of neighborhood disadvantage nationally—a binary measure of ADI was used to compare patients living in less disadvantaged versus highly disadvantaged (≥85th percentile) neighborhoods and test for moderation. For sensitivity analyses, we also categorized ADI percentiles into quintiles.
Figure 1.
Unadjusted predicted prevalence and 95% confidence interval (CI) of outcomes across increments of Area Deprivation Index. AUDIT-C = Alcohol Use Disorders Identification Test-Consumption; Dx = diagnosis.
Outcomes
We used the AUDIT-C screening information on alcohol consumption and diagnostic data on AUDs and alcohol-attributable conditions to assess multiple patterns of unhealthy alcohol use as outcomes because patterns of unhealthy alcohol use vary in prevalence across the population and differ in their associations with acute and chronic risk factors (Rehm et al., 2017). The AUDIT-C is a short, three-item validated screen for unhealthy alcohol use. Its items assess the quantity and frequency of average consumption and the frequency of HED in the past year. Each item is scored from 0 to 4 points and summed (total score ranges from 0 to 12), with scores of 8 or higher indicating a high likelihood of AUD (Rubinsky et al., 2010). Study outcomes included (a) unhealthy alcohol use (AUDIT-C ≥ 5), in line with VA’s performance measure requiring follow-up counseling in this group (Lapham et al., 2012); (b) severe unhealthy alcohol use (AUDIT-C ≥ 8); (c) any HED (responding greater than “never” to AUDIT-C Question #3, “How often did you have 6 or more drinks on one occasion?”); (d) AUD measured based on ICD-9-CM and ICD-10-CM codes for alcohol abuse and dependence, excluding in remission, documented up to a year before the AUDIT-C screen; and (e) alcohol-specific conditions based on ICD-9-CM and ICD-10-CM codes documented up to a year before the AUDIT-C screen. Alcohol-specific conditions included conditions wholly attributable to alcohol use (Centers for Disease Control and Prevention [CDC], 2013), such as alcoholic liver disease, alcoholic myopathy, and alcohol-induced chronic pancreatitis.
Covariates
We adjusted for sets of predefined covariates hypothesized as confounders or precision variables. The year of the AUDIT-C screen was included to adjust for any changes in VA’s screening for unhealthy alcohol use over time. Sociodemographic measures were extracted for patients at the time of the AUDIT-C screen. They included age in groups, race/ethnicity, marital status, gender, rurality, and two proxy indicators of individual SES recorded in the EHR. Race/ethnicity—a proxy for experiences of discrimination and marginalization associated with selection into disadvantaged neighborhoods—was self-reported (Sohn et al., 2006) and categorized as non-Hispanic Black, non-Hispanic White, Hispanic, non-Hispanic Asian/Pacific Islander (API), non-Hispanic American Indian/Alaska Native (AI/AN), non-Hispanic multiple races, and non-Hispanic other/unknown. Marital status was defined using five categories (divorced/separated, married, never married/single, widowed, unknown/missing). Sex (a proxy for gender) is documented in the EHR as male or female.
Based on the census tract, patients were assigned to one of four 2010 Rural-Urban Commuting Areas rurality classifications, capturing population density and linkage to larger urban centers. Although VA EHR data do not have reliable measures of income and education, we used two proxy indicators for individual-level SES. These include VA copay status and financial hardship. Copay status was ascertained using a four-category variable based on VA copay requirements (VA copay required due to means, no copay required due to disability, no copay required due to means/other, and not assigned; Williams et al., 2012). Financial hardship was measured using a binary variable based on diagnosis codes and stop codes in the prior 2 years indicative of housing instability, homelessness, or economic hardship (Blosnich et al., 2017). Because comorbidities including physical and mental conditions could be downstream of both unhealthy alcohol use and neighborhood disadvantage and raise potential for collider bias, we did not adjust for this.
Statistical analyses
First, we examined the data’s nested structure and performed analyses to understand the distribution of ADI percentile values in relation to prevalence of outcomes. Next, we described the sociodemographic and health characteristics of the sample and outcomes, overall and across the binary and categorical measures of neighborhood disadvantage. For inferential analyses, we used modified Poisson (log-linear models with robust standard errors) generalized estimating equations (GEE) models with an exchangeable covariance structure to estimate prevalence ratios [PRs] and 95% confidence intervals [CIs]. Modified Poisson models are commonly used to estimate PRs for non-rare binary outcomes (Greenland, 2004; Zou, 2004), are more conservative than alternatives, and perform better in cases of model misspecification (Chen et al., 2018). We selected a GEE approach over a multilevel model approach to analyze correlated data because we were interested in estimating marginal population average rather than neighborhood-specific effects (i.e., conditional on random effects; Hubbard et al., 2010).
Modified Poisson models were fit using GEE with models clustered on census tract to optimize the estimation of standard errors (Bottomley et al., 2016) and were adjusted for year, state of residence, and sociodemographic characteristics. To test for multiplicative interaction suggestive of moderation (VanderWeele & Knol, 2014), an interaction term was fit between the binary measure of neighborhood disadvantage and each potential categorical moderator (gender, race/ethnicity, and rurality) in separate models. We presented stratified findings for models with evidence of moderation at alpha level .05. To illustrate the magnitude of differences in alcohol outcomes across categories of ADI, recommended marginal standardization techniques (Muller & MacLehose, 2014) were used to estimate predicted probabilities and 95% CIs. Given that p values may be sensitive because of the very large data set, we focused presentation of findings on association estimates and predicted probabilities. We used Stata 15.1 (StataCorp LLC, College Station, TX) for all analyses.
Results
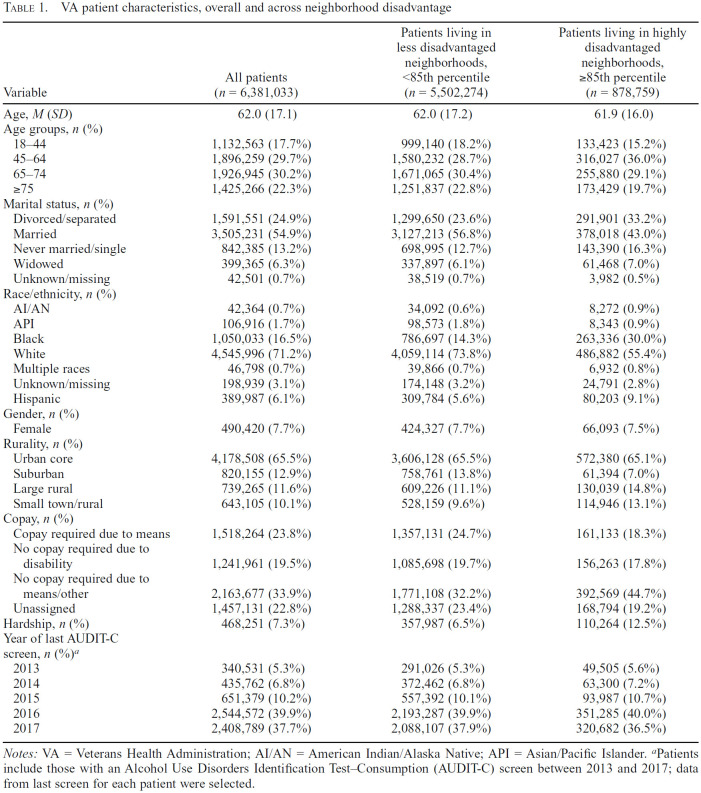
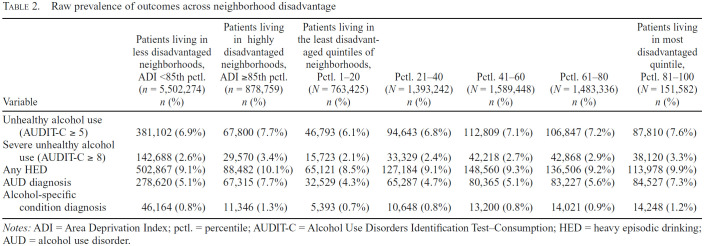
A lower proportion of patients residing in highly disadvantaged neighborhoods (n = 878,759) compared with those in less disadvantaged neighborhoods (n = 5,502,274) were non-Hispanic White, and a lower proportion were married. A higher proportion of patients residing in highly disadvantaged neighborhoods compared with those in less disadvantaged neighborhoods lived in rural areas, and a higher proportion had no copay (Table 1). Similar patterns were found comparing categories of neighborhood disadvantage (Supplemental Table 1). The raw prevalence of all outcomes was descriptively higher among those living in highly disadvantaged versus less disadvantaged neighborhoods, and similar patterns were observed across categories of neighborhood disadvantage (Table 2). When examining the unadjusted predicted prevalence of outcomes across categories of ADI in 5-percentile increments, we found that unadjusted predicted prevalences were more pronounced for patients residing in highly disadvantaged neighborhoods (Figure 1).
Table 1.
VA patient characteristics, overall and across neighborhood disadvantage
| Variable | All patients (n = 6,381,033) | Patients living in less disadvantaged neighborhoods, <85th percentile (n = 5,502,274) | Patients living in highly disadvantaged neighborhoods, ≥85th percentile (n = 878,759) |
|---|---|---|---|
| Age, M (SD) | 62.0 (17.1) | 62.0 (17.2) | 61.9 (16.0) |
| Age groups, n (%) | |||
| 18-44 | 1,132,563 (17.7%) | 999,140 (18.2%) | 133,423 (15.2%) |
| 45-64 | 1,896,259 (29.7%) | 1,580,232 (28.7%) | 316,027 (36.0%) |
| 65-74 | 1,926,945 (30.2%) | 1,671,065 (30.4%) | 255,880 (29.1%) |
| ≥75 | 1,425,266 (22.3%) | 1,251,837 (22.8%) | 173,429 (19.7%) |
| Marital status, n (%) | |||
| Divorced/separated | 1,591,551 (24.9%) | 1,299,650 (23.6%) | 291,901 (33.2%) |
| Married | 3,505,231 (54.9%) | 3,127,213 (56.8%) | 378,018 (43.0%) |
| Never married/single | 842,385 (13.2%) | 698,995 (12.7%) | 143,390 (16.3%) |
| Widowed | 399,365 (6.3%) | 337,897 (6.1%) | 61,468 (7.0%) |
| Unknown/missing | 42,501 (0.7%) | 38,519 (0.7%) | 3,982 (0.5%) |
| Race/ethnicity, n (%) | |||
| AI/AN | 42,364 (0.7%) | 34,092 (0.6%) | 8,272 (0.9%) |
| API | 106,916 (1.7%) | 98,573 (1.8%) | 8,343 (0.9%) |
| Black | 1,050,033 (16.5%) | 786,697 (14.3%) | 263,336 (30.0%) |
| White | 4,545,996 (71.2%) | 4,059,114(73.8%) | 486,882 (55.4%) |
| Multiple races | 46,798 (0.7%) | 39,866 (0.7%) | 6,932 (0.8%) |
| Unknown/missing | 198,939 (3.1%) | 174,148 (3.2%) | 24,791 (2.8%) |
| Hispanic | 389,987 (6.1%) | 309,784 (5.6%) | 80,203 (9.1%) |
| Gender, n (%) | |||
| Female | 490,420 (7.7%) | 424,327 (7.7%) | 66,093 (7.5%) |
| Rurality, n (%) | |||
| Urban core | 4,178,508 (65.5%) | 3,606,128 (65.5%) | 572,380 (65.1%) |
| Suburban | 820,155 (12.9%) | 758,761 (13.8%) | 61,394 (7.0%) |
| Large rural | 739,265 (11.6%) | 609,226 (11.1%) | 130,039 (14.8%) |
| Small town/rural | 643,105 (10.1%) | 528,159 (9.6%) | 114,946 (13.1%) |
| Copay, n (%) | |||
| Copay required due to means | 1,518,264 (23.8%) | 1,357,131 (24.7%) | 161,133 (18.3%) |
| No copay required due to disability | 1,241,961 (19.5%) | 1,085,698 (19.7%) | 156,263 (17.8%) |
| No copay required due to means/other | 2,163,677 (33.9%) | 1,771,108 (32.2%) | 392,569 (44.7%) |
| Unassigned | 1,457,131 (22.8%) | 1,288,337 (23.4%) | 168,794(19.2%) |
| Hardship, n (%) | 468,251 (7.3%) | 357,987 (6.5%) | 110,264(12.5%) |
| Year of last AUDIT-C screen, n (%)a | |||
| 2013 | 340,531 (5.3%) | 291,026 (5.3%) | 49,505 (5.6%) |
| 2014 | 435,762 (6.8%) | 372,462 (6.8%) | 63,300 (7.2%) |
| 2015 | 651,379 (10.2%) | 557,392 (10.1%) | 93,987 (10.7%) |
| 2016 | 2,544,572 (39.9%) | 2,193,287 (39.9%) | 351,285 (40.0%) |
| 2017 | 2,408,789 (37.7%) | 2,088,107 (37.9%) | 320,682 (36.5%) |
Notes: VA = Veterans Health Administration; AI/AN = American Indian/Alaska Native; API = Asian/Pacific Islander.
Patients include those with an Alcohol Use Disorders Identification Test–Consumption (AUDIT-C) screen between 2013 and 2017; data from last screen for each patient were selected.
Table 2.
Raw prevalence of outcomes across neighborhood disadvantage
| Variable | Patients living in less disadvantaged neighborhoods, ADI <85th pctl. (n = 5,502,274) n (%) | Patients living in highly disadvantaged neighborhoods, ADIs ≥85th pctl. (n = 878,759) n (%) | Patients living in the least disadvantaged quintiles of neighborhoods, Pctl. 1-20 (N =763,425) n (%) | Pctl. 21-40 (N = 1,393,242) n (%) | Pctl. 41-60 (N = 1,589,448) n (%) | Pctl. 61-80 (N = 1,483,336) n (%) | Patients living in most disadvantaged quintile, Pctl. 81-100 (N = 151,582) n (%) |
|---|---|---|---|---|---|---|---|
| Unhealthy alcohol use (AUDIT-C ≥ 5) | 381,102 (6.9%) | 67,800 (7.7%) | 46,793 (6.1%) | 94,643 (6.8%) | 112,809 (7.1%) | 106,847 (7.2%) | 87,810(7.6%) |
| Severe unhealthy alcohol use (AUDIT-C ≥ 8) | 142,688 (2.6%) | 29,570 (3.4%) | 15,723 (2.1%) | 33,329 (2.4%) | 42,218 (2.7%) | 42,868 (2.9%) | 38,120 (3.3%) |
| Any HED | 502,867 (9.1%) | 88,482 (10.1%) | 65,121 (8.5%) | 127,184 (9.1%) | 148,560 (9.3%) | 136,506 (9.2%) | 113,978(9.9%) |
| AUD diagnosis | 278,620 (5.1%) | 67,315 (7.7%) | 32,529 (4.3%) | 65,287 (4.7%) | 80,365 (5.1%) | 83,227 (5.6%) | 84,527 (7.3%) |
| Alcohol-specific condition diagnosis | 46,164 (0.8%) | 11,346 (1.3%) | 5,393 (0.7%) | 10,648 (0.8%) | 13,200 (0.8%) | 14,021 (0.9%) | 14,248(1.2%) |
Notes: ADI = Area Deprivation Index; pctl. = percentile; AUDIT-C = Alcohol Use Disorders Identification Test–Consumption; HED = heavy episodic drinking; AUD = alcohol use disorder.
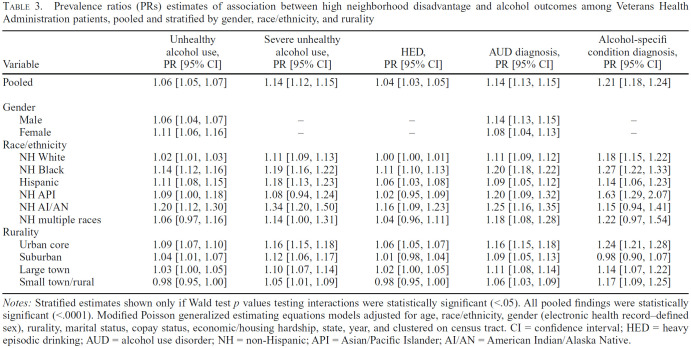
In adjusted models, we observed that those living in highly disadvantaged neighborhoods had a significantly higher likelihood of unhealthy alcohol use (PR = 1.04, 95% CI [1.03, 1.05]), severe unhealthy alcohol use (PR = 1.12, 95% CI [1.11, 1.13]), HED (PR = 1.04, 95% CI [1.02, 1.04]), AUD (PR = 1.12, 95% CI [1.11, 1.13]), and alcohol-specific conditions (PR = 1.18, 95% CI [1.15, 1.20]) than did those living in less disadvantaged neighborhoods (Table 3).
Table 3.
Prevalence ratios (PRs) estimates of association between high neighborhood disadvantage and alcohol outcomes among Veterans Health Administration patients, pooled and stratified by gender, race/ethnicity, and rurality
| Variable | Unhealthy alcohol use, PR [95% CI] | Severe unhealthy alcohol use, PR [95% CI] | HED, PR [95% CI] | AUD diagnosis, PR [95% CI] | Alcohol-specifi condition diagnosis, PR [95% CI] |
|---|---|---|---|---|---|
| Pooled | 1.06 [1.05, 1.07] | 1.14 [1.12, 1.15] | 1.04 [1.03, 1.05] | 1.14 [1.13, 1.15] | 1.21 [1.18, 1.24] |
| Gender | |||||
| Male | 1.06 [1.04, 1.07] | - | - | 1.14 [1.13, 1.15] | - |
| Female | 1.11 [1.06, 1.16] | - | - | 1.08 [1.04, 1.13] | - |
| Race/ethnicity | |||||
| NH White | 1.02 [1.01, 1.03] | 1.11 [1.09, 1.13] | 1.00 [1.00, 1.01] | 1.11 [1.09, 1.12] | 1.18 [1.15, 1.22] |
| NH Black | 1.14 [1.12, 1.16] | 1.19 [1.16, 1.22] | 1.11 [1.10, 1.13] | 1.20 [1.18, 1.22] | 1.27 [1.22, 1.33] |
| Hispanic | 1.11 [1.08, 1.15] | 1.18 [1.13, 1.23] | 1.06 [1.03, 1.08] | 1.09 [1.05, 1.12] | 1.14 [1.06, 1.23] |
| NH API | 1.09 [1.00, 1.18] | 1.08 [0.94, 1.24] | 1.02 [0.95, 1.09] | 1.20 [1.09, 1.32] | 1.63 [1.29, 2.07] |
| NH AI/AN | 1.20 [1.12, 1.30] | 1.34 [1.20, 1.50] | 1.16 [1.09, 1.23] | 1.25 [1.16, 1.35] | 1.15 [0.94, 1.41] |
| NH multiple races | 1.06 [0.97, 1.16] | 1.14 [1.00, 1.31] | 1.04 [0.96, 1.11] | 1.18 [1.08, 1.28] | 1.22 [0.97, 1.54] |
| Rurality | |||||
| Urban core | 1.09 [1.07, 1.10] | 1.16 [1.15, 1.18] | 1.06 [1.05, 1.07] | 1.16 [1.15, 1.18] | 1.24 [1.21, 1.28] |
| Suburban | 1.04 [1.01, 1.07] | 1.12 [1.06, 1.17] | 1.01 [0.98, 1.04] | 1.09 [1.05, 1.13] | 0.98 [0.90, 1.07] |
| Large town | 1.03 [1.00, 1.05] | 1.10 [1.07, 1.14] | 1.02 [1.00, 1.05] | 1.11 [1.08, 1.14] | 1.14 [1.07, 1.22] |
| Small town/rural | 0.98 [0.95, 1.00] | 1.05 [1.01, 1.09] | 0.98 [0.95, 1.00] | 1.06 [1.03, 1.09] | 1.17 [1.09, 1.25] |
Notes: Stratified estimates shown only if Wald test p values testing interactions were statistically significant (<.05). All pooled findings were statistically significant (<.0001). Modified Poisson generalized estimating equations models adjusted for age, race/ethnicity, gender (electronic health record–defined sex), rurality, marital status, copay status, economic/housing hardship, state, year, and clustered on census tract. CI = confidence interval; HED = heavy episodic drinking; AUD = alcohol use disorder; NH = non-Hispanic; API = Asian/Pacific Islander; AI/AN = American Indian/Alaska Native.
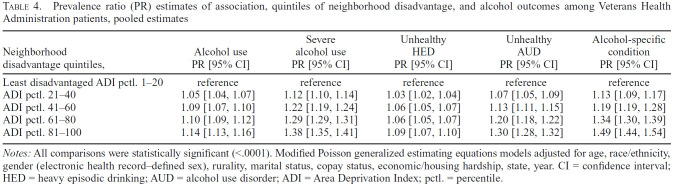
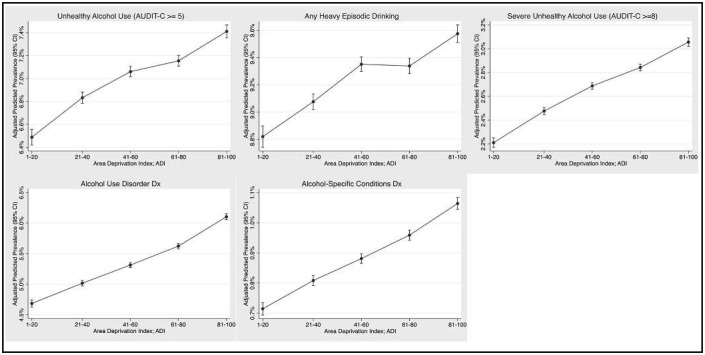
In sensitivity analyses in which neighborhood disadvantage was modeled in categories, we observed consistent patterns, whereby higher PRs of outcomes were observed with increasing categories of disadvantage compared with patients in the least disadvantaged category (Table 4). Specifically, compared with patients in neighborhoods with the lowest quintile of ADI (least disadvantaged), we identified that patients in the highest quintile of ADI (most disadvantaged) had a significantly higher likelihood of unhealthy alcohol use (PR = 1.14, 95% CI [1.13, 1.16]), severe unhealthy alcohol use (PR = 1.38, 95% CI [1.35, 1.41]), HED (PR = 1.09, 95% CI [1.07, 1.10]), AUD (PR = 1.30, 95% CI [1.28, 1.32]), and alcohol-specific conditions (PR = 1.49, 95% CI [1.44, 1.54]). Adjusted predicted prevalences and corresponding 95% CIs from these models are shown in Figure 2 to illustrate the magnitude of differences across ADI.
Table 4.
Prevalence ratio (PR) estimates of association, quintiles of neighborhood disadvantage, and alcohol outcomes among Veterans Health Administration patients, pooled estimates
| Neighborhood disadvantage quintiles, | Alcohol use PR [95% CI] | Severe alcohol use PR [95% CI] | Unhealthy HED PR [95% CI] | Unhealthy AUD PR [95% CI] | Alcohol-specific condition PR [95% CI] |
|---|---|---|---|---|---|
| Least disadvantaged ADI pctl. 1-20 | reference | reference | reference | reference | reference |
| ADI pctl. 21-40 | 1.05 [1.04, 1.07] | 1.12 [1.10, 1.14] | 1.03 [1.02, 1.04] | 1.07 [1.05, 1.09] | 1.13 [1.09, 1.17] |
| ADI pctl. 41-60 | 1.09 [1.07, 1.10] | 1.22 [1.19, 1.24] | 1.06 [1.05, 1.07] | 1.13 [1.11, 1.15] | 1.19 [1.19, 1.28] |
| ADI pctl. 61-80 | 1.10 [1.09, 1.12] | 1.29 [1.29, 1.31] | 1.06 [1.05, 1.07] | 1.20 [1.18, 1.22] | 1.34 [1.30, 1.39] |
| ADI pctl. 81-100 | 1.14 [1.13, 1.16] | 1.38 [1.35, 1.41] | 1.09 [1.07, 1.10] | 1.30 [1.28, 1.32] | 1.49 [1.44, 1.54] |
Notes: All comparisons were statistically significant (<.0001). Modified Poisson generalized estimating equations models adjusted for age, race/ethnicity, gender (electronic health record–defined sex), rurality, marital status, copay status, economic/housing hardship, state, year. CI = confidence interval; HED = heavy episodic drinking; AUD = alcohol use disorder; ADI = Area Deprivation Index; pctl. = percentile.
Figure 2.
Adjusted predicted prevalence and 95% confidence interval (CI) of outcomes across quintiles of Area Deprivation Index. AUDIT-C = Alcohol Use Disorders Identification Test-Consumption; Dx = diagnosis.
When examining moderation, we observed the presence of statistically significant multiplicative interactions between neighborhood disadvantage and race/ethnicity and rural residence for nearly all outcomes (Table 3). However, gender was a less consistent moderator, and, notably, neighborhood disadvantage had a more pronounced association with past-year AUD diagnosis for men than for women, but we observed the opposite pattern for unhealthy alcohol use. In a post hoc analysis examining moderation by age, mixed findings were also observed (Supplemental Table 2). When comparing across racial/ethnic groups, association estimates for neighborhood disadvantage were largest for Black or AI/AN patients for all outcomes except alcohol-specific conditions, and, when comparing across urban–rural categories, associations were strongest for patients living in the most urban areas.
Discussion
We identified that neighborhood disadvantage was associated with higher rates of all alcohol-related outcomes and that effect estimates were consistently larger for Black and AI/AN patients (compared with patients of other races/ethnicities) and urban patients (compared with patients living in more rural areas). This study is the first, to our knowledge, to use EHR and alcohol screening data to examine the role of neighborhood disadvantage in patterns of unhealthy alcohol use and related outcomes in an integrated national health care system. This study builds on prior studies by using a neighborhood-level index that captures multiple dimensions of disadvantage (Karriker-Jaffe, 2011) and by examining outcomes such as AUD and alcohol-specific conditions that have been infrequently studied in relation to neighborhood disadvantage (Ahern et al., 2015; Cambron et al., 2017; Rhew et al., 2018). Furthermore, EHR data facilitated examination of moderation by gender, race/ethnicity, and rurality.
Our main findings support previous studies across varying populations using twin-matched (Rhew et al., 2018) and longitudinal designs (Brenner et al., 2015; Cambron et al., 2017; Cerdá et al., 2010; Rhew et al., 2020) that have found that neighborhood disadvantage is modestly positively associated with alcohol consumption, heavy drinking, and alcohol-related problems among adults. We found pronounced associations between neighborhood disadvantage and unhealthy alcohol use for Black and AI/AN patients and for patients living in the most urban areas, whereas findings related to moderation by gender were mixed. The most notable differences were across race/ethnicity, corroborating the results of other studies that have identified larger effect estimates between neighborhood disadvantage and alcohol-related outcomes for marginalized racial/ethnic groups (Jones-Webb et al., 1997; Karriker-Jaffe et al., 2012; Zemore et al., 2016). Living in a disadvantaged area may subject Black or AI/AN persons to substantially more discriminatory experiences, which could elevate stress and distress in ways that could relate to patterns of alcohol use. Additional studies are needed to understand the place-based inequities in conjunction with historical trauma and social norms (Ehlers et al., 2013) in influencing patterns of alcohol use among AI/ANs.
Furthermore, findings across the urban–rural continuum suggest that conditions present in disadvantaged urban neighborhoods may be distinct in their relationship with alcohol-related outcomes, potentially because of issues specific to urban environments such as safety and policing concerns (Shmool et al., 2015), gentrification (Izenberg et al., 2018), and high alcohol outlet density (Trangenstein et al., 2020). Reasons are unclear for inconsistent moderation by gender for two outcomes and the nonpresence of moderation for three other outcomes; additional research is needed on neighborhood factors and experiences among women with unhealthy alcohol use served by the VA (Cucciare et al., 2016).
The associations we identified between neighborhood disadvantage and patterns of alcohol use and alcohol-specific conditions should be interpreted with attention to the alcohol harm paradox. The alcohol harm paradox (Bellis et al., 2016) is the repeat finding that alcohol use may be especially harmful to more disadvantaged communities than to more advantaged communities even at similar levels of alcohol use (Katikireddi et al., 2017; Sadler et al., 2017). Notably, similar patterns have been observed across race/ethnicity in U.S. contexts. For example, Hispanic, Black, and AI/AN persons face disproportionate negative consequences of alcohol compared with Whites, unexplained by differences in the volume of alcohol consumed (Zemore et al., 2018).
Thus, higher levels of unhealthy alcohol use observed among VA patients residing in more disadvantaged neighborhoods may be amplified, leading to disproportionately more alcohol-related harm. This is a reason why association sizes between neighborhood disadvantage and alcohol-related outcomes tended to be the largest for more severe outcomes. The alcohol harm paradox is understudied (Boyd et al., 2021) and may exist in part because of interactions between alcohol use and other exposures, quantity and type of alcohol consumed, as well as worse access to health care (Bellis et al., 2016). Future theory-focused studies could be important for clarifying the contribution of modifiable factors in alcohol-related disparities.
This study has several limitations. First, VA patients are not representative of the broader U.S. population (Wong et al., 2016). Unmeasured confounding may be present because of limited individual-level data on SES (e.g., no data on individual-level income) as well as alcohol policy conditions and health care quality differences unaccounted for by state fixed effects. Despite the VA’s extensive efforts to identify and treat unhealthy alcohol use, underdiagnosis of AUD, under-identification of unhealthy alcohol use because of variation in screening techniques, and inability to ascertain chronic versus acute unhealthy alcohol use may be limitations of using EHR data. For example, past-year AUD prevalence based on standardized assessment is approximately 14% in the general population (Grant et al., 2015) and 10% in the VA patient population (Hoggatt et al., 2021), yet was substantially lower in the present study based on documented diagnosis. Temporal order cannot be established given a cross-sectional design. Therefore, patterns of unhealthy alcohol use could precede or even induce selection into more disadvantaged neighborhoods (Oakes, 2004).
Finally, the ADI measure of neighborhood disadvantage used does not allow for the isolation of mechanisms, and our use of this administratively defined measure of neighborhood at the census block group level could result in bias related to the modifiable areal unit problem, where boundary definitions could bias observed associations (Wong, 2004). Alternative strategies, such as latent class approaches (Rhew et al., 2017) and approaches to defining neighborhoods that account for the racialized historical factors (e.g., redlining) that shape them (Lee et al., 2020; Trangenstein et al., 2020), could help clarify mechanisms and interventions (Riley, 2018).
Nonetheless, this study adds to a growing literature on place-based inequities in health among VA patients (Hatef et al., 2019; Nelson et al., 2017; Wong et al., 2020) and highlights that socioeconomic gradients in alcohol-related health outcomes persist across patients served by a universal health care system with extensive efforts to address unhealthy alcohol use. Responsible for addressing its patients’ medical and nonmedical needs, the VA is increasingly interested in addressing upstream social determinants of health. The VA could leverage neighborhood disadvantage data and other SES measures to document inequities and ensure equitable care. For example, the VA is examining place-based interventions to enhance social support for patients with cardiovascular diseases (Nelson et al., 2018). Similar approaches to alcohol-related care could be developed, given that increased social support may disrupt associations between neighborhood disadvantage and unhealthy alcohol use (Karriker-Jaffe et al., 2017).
Furthermore, the socioeconomic gradients in unhealthy alcohol use observed underscore that enhanced medical care that addresses individual social needs is, alone, insufficient to address social determinants of health (Castrucci & Auerbach, 2019). Targeted policy strategies, such as Federal Housing Choice Voucher programs—including those administered in partnership with the VA—could be leveraged to promote affordable housing in higher-opportunity areas (Patterson et al., 2014), and broader population-level strategies such as expansion of social safety net programs could have important influences on poverty and health among residents of disadvantaged areas (Allen et al., 2019; Berube, 2006; Wicks-Lim & Arno, 2017). Future research is needed to evaluate targeted health care and population-level approaches to addressing unhealthy alcohol use and alcohol-related racial/ethnic, gender, and geographic inequities.
Footnotes
The parent study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (R21 AA025973; Emily C. Williams/John R. Blosnich, principal investigators) to the University of Washington. This work was supported in part with resources and the use of facilities at the VA Puget Sound Health Care System in Seattle, WA. However, the contents of this manuscript do not represent the views of the U.S. Department ofVeterans Affairs or the United States Government.
References
- Ahern J., Balzer L., Galea S. The roles of outlet density and norms in alcohol use disorder. Drug and Alcohol Dependence. 2015;151:144–150. doi: 10.1016/j.drugalcdep.2015.03.014. doi:10.1016/J.DRUGALCDEP.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahern J., Galea S., Hubbard A., Midanik L., Syme S. L. “Culture of drinking” and individual problems with alcohol use. American Journal of Epidemiology. 2008;167:1041–1049. doi: 10.1093/aje/kwn022. doi:10.1093/aje/kwn022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen H. L., Eliason E., Zewde N., Gross T. Can Medicaid expansion prevent housing evictions? Health Affairs. 2019;38:1451–1457. doi: 10.1377/hlthaff.2018.05071. doi:10.1377/hlthaff.2018.05071. [DOI] [PubMed] [Google Scholar]
- Barr P. B. Neighborhood conditions and trajectories of alcohol use and misuse across the early life course. Health & Place. 2018;51:36–44. doi: 10.1016/j.healthplace.2018.02.007. doi:10.1016/j.healthplace.2018.02.007. [DOI] [PubMed] [Google Scholar]
- Barrington W. E., Stafford M., Hamer M., Beresford S. A. A., Koepsell T., Steptoe A. Neighborhood socioeconomic deprivation, perceived neighborhood factors, and cortisol responses to induced stress among healthy adults. Health & Place. 2014;27:120–126. doi: 10.1016/j.healthplace.2014.02.001. doi:10.1016/j.healthplace.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis M. A., Hughes K., Nicholls J., Sheron N., Gilmore I., Jones L. The alcohol harm paradox: Using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health. 2016;16:111. doi: 10.1186/s12889-016-2766-x. doi:10.1186/s12889-016-2766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berke E. M., Tanski S. E., Demidenko E., Alford-Teaster J., Shi X., Sargent J. D. Alcohol retail density and demographic predictors of health disparities: A geographic analysis. American Journal of Public Health. 2010;100:1967–71. doi: 10.2105/AJPH.2009.170464. doi:10.2105/AJPH.2009.170464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berube A.Using the Earned Income Tax Credit to stimulate local economies. Living Cities Policy Series. 2006. p. 2. Retrieved from https://www.brookings.edu/wp-content/uploads/2016/06/berube20061101eitc.pdf.
- Blosnich J. R., Marsiglio M. C., Dichter M. E., Gao S., Gordon A. J., Shipherd J. C., Fine M. J. Impact of social determinants of health on medical conditions among transgender veterans. American Journal of Preventive Medicine. 2017;52:491–498. doi: 10.1016/j.amepre.2016.12.019. doi:10.1016/J.AMEPRE.2016.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boardman J. D., Finch B. K., Ellison C. G., Williams D. R., Jackson J. S. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42:151–165. doi:10.2307/3090175. [PubMed] [Google Scholar]
- Bottomley C., Kirby M. J., Lindsay S. W., Alexander N. Can the buck always be passed to the highest level of clustering? BMC Medical Research Methodology. 2016;16:29. doi: 10.1186/s12874-016-0127-1. doi:10.1186/s12874-016-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd J., Bambra C., Purshouse R. C., Holmes J. Beyond behaviour: How health inequality theory can enhance our understanding of the ‘alcohol-harm paradox’. International Journal of Environmental Research and Public Health. 2021;18:6025. doi: 10.3390/ijerph18116025. doi:10.3390/ijerph18116025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley K. A., DeBenedetti A. F., Volk R. J., Williams E. C., Frank D., Kivlahan D. R. AUDIT C as a brief screen for alcohol misuse in primary care. Alcoholism: Clinical and Experimental Research. 2007;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. doi:10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Brenner A. B., Borrell L. N., Barrientos-Gutierrez T., Diez Roux A. V. Longitudinal associations of neighborhood socioeconomic characteristics and alcohol availability on drinking: Results from the Multi-Ethnic Study of Atherosclerosis (MESA) Social Science & Medicine. 2015;145:17–25. doi: 10.1016/j.socscimed.2015.09.030. doi:10.1016/J.SOCSCIMED.2015.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryden A., Roberts B., McKee M., Petticrew M. A systematic review of the influence on alcohol use of community level availability and marketing of alcohol. Health & Place. 2012;18:349–357. doi: 10.1016/j.healthplace.2011.11.003. doi:10.1016/J.HEALTHPLACE.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Cambron C., Kosterman R., Rhew I. C., Catalano R. F., Guttmannova K., Hawkins J. D. An examination of alcohol use disorder symptoms and neighborhood disorganization from age 21 to 39. American Journal of Community Psychology. 2017;60:267–278. doi: 10.1002/ajcp.12160. doi:10.1002/ajcp.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A., Deaton A. Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity. 2017;2017:397–476. doi: 10.1353/eca.2017.0005. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/29033460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey J. A., Schwartz B. S., Stewart W. F., Adler N. E. Using electronic health records for population health research: A review of methods and applications. Annual Review of Public Health. 2016;37:61–81. doi: 10.1146/annurev-publhealth-032315-021353. doi:10.1146/annurev-publhealth-032315-021353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castrucci B., Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Policy & Practice. 2019;77:25–27. doi:10.1377/hblog20190115.234942. [Google Scholar]
- Centers for Disease Control and Prevention. Alcohol-related disease impact (ARDI) application. 2013 Retrieved from https://nccd.cdc.gov/DPH_ARDI/default/default.aspx. [Google Scholar]
- Cerdá M., Diez-Roux A. V, Tchetgen E. T., Gordon-Larsen P., Kiefe C. The relationship between neighborhood poverty and alcohol use: Estimation by marginal structural models. Epidemiology. 2010;21:482–489. doi: 10.1097/EDE.0b013e3181e13539. doi:10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan P., Ahern J., Galea S., Keyes K. M. Neighborhood context and binge drinking by race and ethnicity in New York City. Alcoholism: Clinical and Experimental Research. 2016;40:785–793. doi: 10.1111/acer.13011. doi:10.1111/acer.13011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W., Qian L., Shi J., Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Medical Research Methodology. 2018;18:63. doi: 10.1186/s12874-018-0519-5. doi:10.1186/s12874-018-0519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D. A., Scribner R. A., Farley T. A. A structural model of health behavior: A pragmatic approach to explain and influence health behaviors at the population level. Preventive Medicine. 2000;30:146–154. doi: 10.1006/pmed.1999.0609. doi:10.1006/PMED.1999.0609. [DOI] [PubMed] [Google Scholar]
- Cucciare M. A., Lewis E. T., Hoggatt K. J., Bean-Mayberry B., Timko C., Durazo E. M., Frayne S. M. Factors affecting women’s disclosure of alcohol misuse in primary care: A qualitative study with U.S. military veterans. Women’s Health Issues. 2016;26:232–239. doi: 10.1016/j.whi.2015.07.010. doi:10.1016/j.whi.2015.07.010. [DOI] [PubMed] [Google Scholar]
- Dawson D. A., Goldstein R. B., Saha T. D., Grant B. F. Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug and Alcohol Dependence. 2015;148:56–61. doi: 10.1016/j.drugalcdep.2014.12.016. doi:10.1016/J.DRUGALCDEP.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A. V., Mair C.Neighborhoods and health; Annals of the New York Academy of Sciences,; 1186; 2010. pp. 125–145. doi:10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Duncan D. T., Kawachi I. Oxford, UK: Oxford University Press; 2018. Neighborhoods and health. [Google Scholar]
- Durfey S. N. M., Kind A. J. H., Buckingham W. R., DuGoff E. H., Trivedi A. N. Neighborhood disadvantage and chronic disease management. Health Services Research. 2019;54:206–216. doi: 10.1111/1475-6773.13092. doi:10.1111/1475-6773.13092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers C. L., Gizer I. R., Gilder D. A., Ellingson J. M., Yehuda R. Measuring historical trauma in an American Indian community sample: Contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug and Alcohol Dependence. 2013;133:180–187. doi: 10.1016/j.drugalcdep.2013.05.011. doi:10.1016/j.drugalcdep.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass J. E., Williams E. C. The future of research on alcohol health disparities: A health services research perspective. Journal of Studies on Alcohol and Drugs. 2018;79:322–324. doi: 10.15288/jsad.2018.79.322. doi:10.15288/jsad.2018.79.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass J. E., Williams E. C., Bucholz K. K. Psychiatric comorbidity and perceived alcohol stigma in a nationally representative sample of individuals with DSM-5 alcohol use disorder. Alcoholism: Clinical and Experimental Research. 2014;38:1697–1705. doi: 10.1111/acer.12422. doi:10.1111/acer.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon D.2003Area-based deprivation measures: A U.K. perspective Neighborhoods and Healthpp. 179–208.Oxford, UK: Oxford University Press; doi:10.1093/acprof:oso/9780195138382.003.0008 [Google Scholar]
- Grant B. F., Chou S. P., Saha T. D., Pickering R. P., Kerridge B. T., Ruan W. J., Hasin D. S. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74:911–923. doi: 10.1001/jamapsychiatry.2017.2161. doi:10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Saha T. D., Chou S. P., Jung J., Zhang H., Hasin D. S. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. doi:10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. American Journal of Epidemiology. 2004;160:301–305. doi: 10.1093/aje/kwh221. doi:10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- Hatef E., Searle K. M., Predmore Z., Lasser E. C., Kharrazi H., Nelson K., Sylling P., Weiner J. P. American Journal of Preventive Medicine. Vol. 56. Elsevier Inc; 2019. The impact of social determinants of health on hospitalization in the Veterans Health Administration; pp. 811–818. doi:10.1016/j.amepre.2018.12.012. [DOI] [PubMed] [Google Scholar]
- Hoggatt K. J., Harris A. H. S., Washington D. L., Williams E. C. Prevalence of substance use and substance-related disorders among US Veterans Health Administration patients. Drug and Alcohol Dependence. 2021;225:108791. doi: 10.1016/j.drugalcdep.2021.108791. doi:10.1016/j.drugalcdep.2021.108791. [DOI] [PubMed] [Google Scholar]
- Hu J., Kind A. J. H., Nerenz D. Area deprivation index predicts readmission risk at an urban teaching hospital. American Journal of Medical Quality. 2018;33:493–501. doi: 10.1177/1062860617753063. doi:10.1177/1062860617753063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard A. E., Ahern J., Fleischer N. L., Van der Laan M., Lippman S. A., Jewell N., Satariano W. A. To GEE or not to GEE: Comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21:467–474. doi: 10.1097/EDE.0b013e3181caeb90. doi:10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Izenberg J. M., Mujahid M. S., Yen I. H. Gentrification and binge drinking in California neighborhoods: It matters how long you’ve lived there. Drug and Alcohol Dependence. 2018;188:1–9. doi: 10.1016/j.drugalcdep.2018.03.018. doi:10.1016/J.DRUGALCDEP.2018.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson N., Denny S., Ameratunga S. Social and socio-demographic neighborhood effects on adolescent alcohol use: A systematic review of multi-level studies. Social Science & Medicine. 2014;115:10–20. doi: 10.1016/j.socscimed.2014.06.004. doi:10.1016/j.socscimed.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Jané-Llopis E., Matytsina I. Mental health and alcohol, drugs and tobacco: A review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug and Alcohol Review. 2006;25:515–536. doi: 10.1080/09595230600944461. doi:10.1080/09595230600944461. [DOI] [PubMed] [Google Scholar]
- Jones-Webb R., Snowden L., Herd D., Short B., Hannan P. Alcohol-related problems among Black, Hispanic and White men: The contribution of neighborhood poverty. Journal of Studies on Alcohol. 1997;58:539–545. doi: 10.15288/jsa.1997.58.539. doi:10.15288/jsa.1997.58.539. [DOI] [PubMed] [Google Scholar]
- Joshi S., Mooney S. J., Rundle A. G., Quinn J. W., Beard J. R., Cerdá M. Pathways from neighborhood poverty to depression among older adults. Health & Place. 2017;43:138–143. doi: 10.1016/j.healthplace.2016.12.003. doi:10.1016/J.HEALTHPLACE.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K. J. Areas of disadvantage: A systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug and Alcohol Review. 2011;30:84–95. doi: 10.1111/j.1465-3362.2010.00191.x. doi:10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K. J., Au V., Frendo M., Mericle A. A. Offsetting the effects of neighborhood disadvantage on problem drinking. Journal of Community Psychology. 2017;45:678–684. doi: 10.1002/jcop.21881. doi:10.1002/jcop.21881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K. J., Room R., Giesbrecht N., Greenfield T. K. Alcohol’s harm to others: Opportunities and challenges in a public health framework. Journal of Studies on Alcohol and Drugs. 2018;79:239–243. doi: 10.15288/jsad.2018.79.239. doi:10.15288/jsad.2018.79.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K. J., Zemore S. E., Mulia N., Jones-Webb R., Bond J., Greenfield T. K. Neighborhood disadvantage and adult alcohol outcomes: Differential risk by race and gender. Journal of Studies on Alcohol and Drugs. 2012;73:865–873. doi: 10.15288/jsad.2012.73.865. doi:10.15288/JSAD.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katikireddi S. V., Whitley E., Lewsey J., Gray L., Leyland A. H. Socioeconomic status as an effect modifier of alcohol consumption and harm: Analysis of linked cohort data. The Lancet Public Health. 2017;2:e267–e276. doi: 10.1016/S2468-2667(17)30078-6. doi:10.1016/S2468-2667(17)30078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K. S., Gardner C. O., Hickman M., Heron J., Macleod J., Lewis G., Dick D. M. Socioeconomic status and alcohol-related behaviors in mid- to late adolescence in the Avon Longitudinal Study of Parents and Children. Journal of Studies on Alcohol and Drugs. 2014;75:541–545. doi: 10.15288/jsad.2014.75.541. doi:10.15288/jsad.2014.75.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K. S., Ohlsson H., Karriker-Jaffe K. J., Sundquist J., Sundquist K. Social and economic consequences of alcohol use disorder: A longitudinal cohort and co-relative analysis. Psychological Medicine. 2017;47:925–935. doi: 10.1017/S0033291716003032. doi:10.1017/S0033291716003032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K. M., Hatzenbuehler M. L., McLaughlin K. A., Link B., Olfson M., Grant B. F., Hasin D. Stigma and treatment for alcohol disorders in the United States. American Journal of Epidemiology. 2010;172:1364–1372. doi: 10.1093/aje/kwq304. doi:10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind A. J. H., Buckingham W. R. Making neighborhood-disadvantage metrics accessible—The neighborhood atlas. New England Journal of Medicine. 2018;378:2456–2458. doi: 10.1056/NEJMp1802313. doi:10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind A. J. H., Jencks S., Brock J., Yu M., Bartels C., Ehlenbach W., Smith M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Annals of Internal Medicine. 2014;161:765–774. doi: 10.7326/M13-2946. doi:10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kneebone E., Holmes N.U.S. concentrated poverty in the wake of the Great Recession. 2016. Mar 31, Retrieved from https://www.brookings.edu/research/u-s-concentrated-poverty-in-the-wake-ofthe-great-recession/
- Lapham G. T., Achtmeyer C. E., Williams E. C., Hawkins E. J., Kivlahan D. R., Bradley K. A. Increased documented brief alcohol interventions with a performance measure and electronic decision support. Medical Care. 2012;50:179–187. doi: 10.1097/MLR.0b013e3181e35743. doi:10.1097/MLR.0b013e3181e35743. [DOI] [PubMed] [Google Scholar]
- Lee J. P., Ponicki W., Mair C., Gruenewald P., Ghanem L. What explains the concentration of off-premise alcohol outlets in Black neighborhoods? SSM - Population Health. 2020;12:100669. doi: 10.1016/j.ssmph.2020.100669. doi:10.1016/j.ssmph.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C., Frankeberger J., Gruenewald P. J., Morrison C. N., Freisthler B. Space and place in alcohol research. Current Epidemiology Reports. 2019;6:412–422. doi: 10.1007/s40471-019-00215-3. doi:10.1007/s40471-019-00215-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A. H., Ballestros K., Echko M., Glenn S., Olsen H. E., Mullany E., Murray C. J. L. The State of US Health, 1990-2016: Burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319:1444–1472. doi: 10.1001/jama.2018.0158. doi:10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller C. J., MacLehose R. F. Estimating predicted probabilities from logistic regression: Different methods correspond to different target populations. International Journal of Epidemiology. 2014;43:962–970. doi: 10.1093/ije/dyu029. doi:10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson K., Fennell T., Gray K. E., Williams J. L., Lutton M. C., Silverman J., Vanderwarker C. Veteran peer Coaches Optimizing and Advancing Cardiac Health (Vet-COACH); design and rationale for a randomized controlled trial of peer support among Veterans with poorly controlled hypertension and other CVD risks. Contemporary Clinical Trials. 2018;73:61–67. doi: 10.1016/j.cct.2018.08.011. doi:10.1016/j.cct.2018.08.011. [DOI] [PubMed] [Google Scholar]
- Nelson K., Schwartz G., Hernandez S., Simonetti J., Curtis I., Fihn S. D. The association between neighborhood environment and mortality: Results from a national study of veterans. Journal of General Internal Medicine. 2017;32:416–422. doi: 10.1007/s11606-016-3905-x. doi:10.1007/s11606-016-3905-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson K. M., Starkebaum G. A., Reiber G. E. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Reports. 2007;122:93–100. doi: 10.1177/003335490712200113. doi:10.1177/003335490712200113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes J. M. The (mis)estimation of neighborhood effects: Causal inference for a practicable social epidemiology. Social Science & Medicine. 2004;58:1929–1952. doi: 10.1016/j.socscimed.2003.08.004. doi:10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Patterson K. L., Nochajski T., Wu L. Neighborhood outcomes of formally homeless veterans participating in the HUD-VASH program. Journal of Community Practice. 2014;22:324–341. doi:10.1080/10705422.2014.929605. [Google Scholar]
- Petteway R., Mujahid M., Allen A. Understanding embodiment in place-health research: Approaches, limitations, and opportunities. Journal of Urban Health. 2019:1–11. doi: 10.1007/s11524-018-00336-y. doi:10.1007/s11524-018-00336-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Gmel G. E., Gmel G., Hasan O. S. M., Imtiaz S., Popova S., Probst C., Shuper P. A. The relationship between different dimensions of alcohol use and the burden of disease—An update. Addiction. 2017;112:968–1001. doi: 10.1111/add.13757. doi:10.1111/add.13757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhew I. C., Fleming C. B., Tsang S., Horn E., Kosterman R., Duncan G. E. Neighborhood deprivation moderates shared and unique environmental influences on hazardous drinking: Findings from a cross-sectional co-twin study. Substance Use & Misuse. 2020;55:1625–1632. doi: 10.1080/10826084.2020.1756332. doi:10.1080/10826084.2020.1756332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhew I. C., Kosterman R., Duncan G. E., Mair C. Examination of cross-sectional associations of neighborhood deprivation and alcohol outlet density with hazardous drinking using a twin design. Journal of Studies on Alcohol and Drugs. 2018;79:68–73. doi: 10.15288/jsad.2018.79.68. doi:10.15288/jsad.2018.79.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhew I. C., Kosterman R., Lee J. O. Neighborhood typologies associated with alcohol use among adults in their 30s: A finite mixture modeling approach. Journal of Urban Health. 2017;94:542–548. doi: 10.1007/s11524-017-0161-2. doi:10.1007/s11524-017-0161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro A., Amaro J., Lisi C., Fraga S. Neighborhood socioeconomic deprivation and allostatic load: A scoping review. International Journal of Environmental Research and Public Health. 2018;15:1092. doi: 10.3390/ijerph15061092. doi:10.3390/ijerph15061092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A. R. Neighborhood disadvantage, residential segregation, and beyond—Lessons for studying structural racism and health. Journal of Racial and Ethnic Health Disparities. 2018;5:357–365. doi: 10.1007/s40615-017-0378-5. doi:10.1007/s40615-017-0378-5. [DOI] [PubMed] [Google Scholar]
- Room R., Babor T., Rehm J. Alcohol and public health. The Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. doi:10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- Rubinsky A. D., Kivlahan D. R., Volk R. J., Maynard C., Bradley K. A. Estimating risk of alcohol dependence using alcohol screening scores. Drug and Alcohol Dependence. 2010;108:29–36. doi: 10.1016/j.drugalcdep.2009.11.009. doi:10.1016/J.DRUGALCDEP.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph K. E., Stuart E. A., Glass T. A., Merikangas K. R. Neighborhood disadvantage in context: The influence of urbanicity on the association between neighborhood disadvantage and adolescent emotional disorders. Social Psychiatry and Psychiatric Epidemiology. 2014;49:467–475. doi: 10.1007/s00127-013-0725-8. doi:10.1007/s00127-013-0725-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadler S., Angus C., Gavens L., Gillespie D., Holmes J., Hamilton J., Meier P. Understanding the alcohol harm paradox: An analysis of sex- and condition-specific hospital admissions by socio-economic group for alcohol-associated conditions in England. Addiction. 2017;112:808–817. doi: 10.1111/add.13726. doi:10.1111/add.13726. [DOI] [PubMed] [Google Scholar]
- Schinasi L. H., Auchincloss A. H., Forrest C. B., Diez Roux A. V. Using electronic health record data for environmental and place based population health research: A systematic review. Annals of Epidemiology. 2018;28:493–502. doi: 10.1016/j.annepidem.2018.03.008. doi:10.1016/J.ANNEPIDEM.2018.03.008. [DOI] [PubMed] [Google Scholar]
- Shmool J. L. C., Yonas M. A., Newman O. D., Kubzansky L. D., Joseph E., Parks A., Clougherty J. E. Identifying perceived neighborhood stressors across diverse communities in New York City. American Journal of Community Psychology. 2015;56:145–155. doi: 10.1007/s10464-015-9736-9. doi:10.1007/s10464-015-9736-9. [DOI] [PubMed] [Google Scholar]
- Singh G. K. Area deprivation and widening inequalities in US mortality, 1969-1998. American Journal of Public Health. 2003;93:1137–1143. doi: 10.2105/ajph.93.7.1137. doi:10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn M.-W., Zhang H., Arnold N., Stroupe K., Taylor B. C., Wilt T. J., Hynes D. M. Transition to the new race/ethnicity data collection standards in the Department of Veterans Affairs. Population Health Metrics. 2006;4:7. doi: 10.1186/1478-7954-4-7. doi:10.1186/1478-7954-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillane S., Shiels M. S., Best A. F., Haozous E. A., Withrow D. R., Chen Y., Freedman N. D. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Network Open. 2020;3:e1921451. doi: 10.1001/jamanetworkopen.2019.21451. doi:10.1001/jamanetworkopen.2019.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahre M., Roeber J., Kanny D., Brewer R. D., Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Preventing Chronic Disease. 2014;11:130293. doi: 10.5888/pcd11.130293. doi:10.5888/pcd11.130293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trangenstein P. J., Gray C., Rossheim M. E., Sadler R., Jernigan D. H. Alcohol outlet clusters and population disparities. Journal of Urban Health. 2020;97:123–136. doi: 10.1007/s11524-019-00372-2. doi:10.1007/s11524-019-00372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs Information Resource Center. 2015 Edition. Hines IL: Author; 2016. VIReC Research User Guide: PSSG Geocoded Enrollee Files. [Google Scholar]
- VanderWeele T. J., Knol M. J. A tutorial on interaction. Epidemiologic Methods. 2014;3:33–72. doi:10.1515/em-2013-0005. [Google Scholar]
- Wicks-Lim J., Arno P. S. Improving population health by reducing poverty: New York’s Earned Income Tax Credit. SSM - Population Health. 2017;3:373–381. doi: 10.1016/j.ssmph.2017.03.006. doi:10.1016/j.ssmph.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams E. C., Lapham G. T., Hawkins E. J., Rubinsky A. D., Morales L. S., Young B. A., Bradley K. A. Variation in documented care for unhealthy alcohol consumption across race/ethnicity in the Department of Veterans Affairs Healthcare System. Alcoholism: Clinical and Experimental Research. 2012;36:1614–1622. doi: 10.1111/j.1530-0277.2012.01761.x. doi:10.1111/j.1530-0277.2012.01761.x. [DOI] [PubMed] [Google Scholar]
- Wong D. W.2004The modifiable areal unit problem (MAUP) In World-Minds: Geographical perspectives on 100 problemspp. 571–575.Dordrecht, Germany: Springer [Google Scholar]
- Wong E. S., Wang V., Liu C.-F., Hebert P. L., Maciejewski M. L. Do Veterans Health Administration enrollees generalize to other populations? Medical Care Research and Review. 2016;73:493–507. doi: 10.1177/1077558715617382. doi:10.1177/1077558715617382. [DOI] [PubMed] [Google Scholar]
- Wong M. S., Steers W. N., Hoggatt K. J., Ziaeian B., Washington D. L. Relationship of neighborhood social determinants of health on racial/ethnic mortality disparities in US veterans—Mediation and moderating effects. Health Services Research. 2020;55:851–862. doi: 10.1111/1475-6773.13547. doi:10.1111/1475-6773.13547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S. H., Chapman D. A., Buchanich J. M., Bobby K. J., Zimmerman E. B., Blackburn S. M. Changes in midlife death rates across racial and ethnic groups in the United States: Systematic analysis of vital statistics. BMJ. 2018;362:k3096. doi: 10.1136/bmj.k3096. doi:10.1136/bmj.k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore S. E., Karriker-Jaffe K. J., Mulia N., Kerr W. C., Ehlers C. L., Cook W. C., Greenfield T. K. The future of research on alcohol-related disparities across U.S. racial/ethnic groups: A plan of attack. Journal of Studies on Alcohol and Drugs. 2018;79:7–21. doi: 10.15288/jsad.2018.79.7. doi:10.15288/jsad.2018.79.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore S. E., Ye Y., Mulia N., Martinez P., Jones-Webb R., Karriker-Jaffe K. Poor, persecuted, young, and alone: Toward explaining the elevated risk of alcohol problems among Black and Latino men who drink. Drug and Alcohol Dependence. 2016;163:31–39. doi: 10.1016/j.drugalcdep.2016.03.008. doi:10.1016/J.DRUGALCDEP.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou G. A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159:702–706. doi: 10.1093/aje/kwh090. doi:10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]