Abstract
Confronting COVID-19 pandemic, one's health belief and behavior are essential to mental well-being. Thus conceived, this study applied the Health Belief Model to test the mediating effect of risk perception and coping strategies on the relationship between self-efficacy and mental health problems. Six hundred and eighteen participants aged 17–52 (117 males and 501 females) completed our web-based survey from February 7 to April 10, 2020. 12.6–15.1% of participants were affected by COVID-19 outbreak in varying degrees. The mediating effects of risk perception and active coping were significant, so was the serial mediating effect of risk perception and passive coping. Individuals with higher general self-efficacy were more likely to have lower risk perception, less passive coping strategies, more active coping strategies, and subsequently had less mental health problems. In conclusion, application of the HBM would help understand how mental health problems happen during an infectious disease epidemic, and the relationships among the HBM constructs need further investigation.
Keywords: COVID-19, Self-efficacy, Mental health, Risk perception, Coping strategies, Health Belief Model
1. Introduction
Public health emergencies often seriously affected public mental health (Tian et al., 2020). During the Severe Acute Respiratory Syndrome (SARS) pandemic, a survey in Hong Kong found that close to two-thirds of the respondents felt horrified, apprehensive, or helpless to SARS (Lau et al., 2006). A recent survey showed that 70% of participants in China reported moderate to severe mental health symptoms during COVID-19 pandemic (Tian et al., 2020). These symptoms could last longer time and have greater prevalence than the pandemic itself (Ornell et al., 2020). Thus, it is urgent to understand how mental health problems have happened during the COVD-19 pandemic.
Applying the Health Belief Model (HBM) to COVID-19 might help to reduce coping behaviors that might provoke anxiety and fear, and shape a person's risk perception through perceived self-efficacy (Mukhtar, 2020). The present study aims to provide a process explanation for the effect of general self-efficacy on adult mental health problems during the COVID-19 pandemic. Furthermore, based on the associations among several constructs of the HBM, the present study examined the mediating effects of risk perception and coping strategies in this relation.
1.1. Self-efficacy and mental health problems
As a construct in the HBM, self-efficacy was considered to be an important determinant of health (Chao et al., 2019), since self-efficacy is a key factor for the initiation and execution of disease-coping behaviors (Bandura, 1977) . During the COVID-19 pandemic, several studies also reported that general self-efficacy was related to mental health problems in several populations (e.g., Bidzan et al., 2020; Mo et al., 2021). Moreover, higher self-efficacy was also reported to be associated with fewer mental health problems during the SARS pandemic (Mak et al., 2009).
1.2. Coping strategies as a mediator
The HBM is one of the most common models for explaining individual differences in coping behaviors related to health problems (Pearlman et al., 2020; Skinner et al., 2008). Coping was considered as thoughts and actions used to manage the external and internal demands of stressful situations (Folkman & Moskowitz, 2004), including active coping and passive coping (Main et al., 2011). Researchers believed that people tended to use active coping to manage daily stressors with controllable outcomes, while using passive coping to manage uncontrollable events (Cheng & Tang, 2004), such as the Wenchuan Earthquake in China (Yang et al., 2010) and SARS-related stress (Gan et al., 2004).
Self-efficacy allows individuals to seek efficient coping strategies on the encountered difficulties (Bidzan et al., 2020), such as the COVID-19 pandemic (Ezati et al., 2021). A meta-analysis study indicated that general self-efficacy was specified as the main predictor of health behaviors (Sheeran et al., 2016). Some studies found that self-efficacy was positively related to active coping (e.g., McBride & Ireland, 2016; Yang et al., 2010) and negatively related to passive coping (e.g., Chen et al., 2020; Ding et al., 2015). Furthermore, a recent study reported that coping style mediated the relationship between general self-efficacy and psychological stress in children with malignant tumor (Liu et al., 2020).
1.3. Risk perception as a mediator
Risk perception is central to the HBM (Rosenstock, 1974). Risk perception could be defined as “people's judgments about the likelihood of negative outcomes such as an illness, injury, disease and death”, and psychometric assessment of risk perception might cover a wide range of features of a certain risk (Winters et al., 2020), including perceived susceptibility, likelihood and severity (Brewer et al., 2007), as well as perceived uncontrollability of potential fatal harm (Winters et al., 2020). Some studies showed that risk perceptions were positively related to mental health problems (Imai et al., 2020; Miura et al., 2017; Suzuki et al., 2015), especially during the SARS pandemic (Wu et al., 2009). A recent study also found that perceived susceptibility and severity were positively related to state anxiety during the COVID-19 pandemic (Lin et al., 2020). However, risk perceptions might not be always negative, since other studies found higher risk perceptions were associated with more protective behaviors to cope (Bruine de Bruin & Bennett, 2020; Chou et al., 2020).
Self-efficacy would influence how threats were perceived (McBride & Ireland, 2016). However, the relationship between self-efficacy and risk perception received little attention, and inconsistent conclusions were obtained on the relationship (Lemée et al., 2019; McBride & Ireland, 2016). An Italian study found that general self-efficacy was a significant predictor of perceived personal susceptibility for the COVID-19 pandemic (Commodari et al., 2020).
1.4. Risk perception and coping strategies as serial mediators
Previous studies have found that risk perception was related to coping strategies in clinical settings (e.g., Nilsson et al., 2013). According to a recent commentary on HBM, risk perception might also modify one's coping strategies for the prevention of COVID-19 (Mukhtar, 2020). Furthermore, a recent study found that coping strategies mediated the association between risk perception and mental health among Healthcare Personnel during COVID-19 epidemic (Krok & Zarzycka, 2020).
1.5. Research question and hypothesis
Based on previous studies, this study tried for the first time to apply the HBM to explain coping strategies and mental health in Chinese adults during COVID-19 pandemic. We aimed to test the mediating effects of risk perception and coping strategies between self-efficacy and mental health problems. Three hypotheses were proposed for this study:
Hypothesis 1
Risk perception mediates the relationship between self-efficacy and mental health problems.
Hypothesis 2
Coping strategies mediate the relationship between self-efficacy and mental health problems.
Hypothesis 3
Risk perception and coping strategies operate as serial mediators between self-efficacy and mental health problems.
2. Method
2.1. Participants
A total of 798 adults from 30 cities in China took part in our online survey from February 7 to April 10, 2020. Participants received invitation of the survey through their personal contacts in Wechat or the webpage of a massive opening online psychology course. Our sample consisted of 618 participants (501 females). The average age of the participants was 22.7 years (SD = 4.9).
2.2. Measures
2.2.1. Mental health problems
Mental health problems related to COVID-19 pandemic were measured by the Psychological Questionnaires for Emergent Events of Public Health (PQEEPH). The PQEEPH consists of 25 items of five subscales, depression, neurasthenia, fear, compulsion/anxiety, hypochondria (Gao et al., 2004). Each item was scored according to the degree of emotional response (0 = “none” to 3 = “severe”) and frequency (0 = “seldom” to 3 = “always”). Average scores of items on each dimension were considered as low-risk, medium-risk, and high-risk based on mean plus one standard deviation or two standard deviations (Chen et al., 2020). Cronbach's α for the PQEEPH was 0.93 in this study. The content validity index (CVI) of the PQEEPH was 0.95 and the CVI of items ranged from 0.83–1.00.
2.2.2. Risk perception
Risk perception was measured by the Public Risk Perception Scale for Public Health Emergencies (PRPS) designed by Dai et al. (2020). The scale consists of 10 items, including four dimensions, severity of pandemic, uncontrollability, severity of health effects, likelihood. Each item was rated on a 5-point scale (1 = “completely not true” to 5 = “completely true”), with higher scores representing higher levels of risk perception. In this study, Cronbach's α for the scale was 0.76. The CVI of the PRPS was 0.97 and the CVI of items ranged from 0.83–1.00.
2.2.3. General self-efficacy
The Chinese version (Wang et al., 2001) of the General Self-Efficacy Scale (GSES, Jerusalem & Schwarzer, 1986) was used to measure people's perceived self-efficacy, which consists of 10 items. Items were rated on a 4-point Likert scale, ranging from “strongly disagree” (scored 1) to “strongly agree” (scored 4), with higher total scores representing the stronger ability and confidence to cope with stressful events. Cronbach's α calculated in this study was 0.92. The CVI of the GSES was 1.00 and the CVI of all items was 1.00.
2.2.4. Coping strategies
Individuals' coping strategies were measured by the Simplified Coping Style Questionnaire (SCSQ) developed by Xie (1998). It consists of 20 items with two subscales assessing an individual's active coping and passive coping. Each item was rated on a 4-point Likert scale (0 = “never” to 3 = “often”). In this study, Cronbach's α for active coping was 0.86 and passive coping was 0.73. The CVI of the SCSQ was 0.89 and the CVI of items was 0.67–1.00.
2.3. Data analysis
SPSS Statistic v26.0 and Mplus v7.0 were employed in our data analyses. Kolmogorov-Smirnov test showed that none of the variables was normally distributed (all p < 0.001). To evaluate the content validity of the questionnaires, six experts, including four psychologists, a mental health education specialist, and a public health physician, were asked to rate each item for relevance on a four-point Likert questionnaire. The CVI of each scale was calculated by averaging method according to Polit et al. (2007). Contingency table analyses and Mann-Whitney U tests were used to examine gender differences. Spearman correlation analyses were performed. Structural equation modeling (SEM) was performed in Mplus to test the hypotheses in a structural equation model. Self-efficacy, coping style, and the components of risk perception and mental health were used as manifest variables, and risk perception, mental health were used as latent variables. 95% bias-corrected confidence interval (CI) was used to estimate indirect effects with 5000 resample. Statistical significance is considered if the 95% CI does not contain zero.
3. Results
3.1. Preliminary analyses
The psychological impacts of COVID-19 pandemic are displayed in Table 1 . Respectively, 8.6%, 7.9%, 10.4%, 8.9% and 7.9% of participants were at medium-risk for depression, neurasthenia, fear, compulsion/anxiety, and hypochondria, and 6.5%, 4.9%, 3.2%, 4.9% and 4.7% of participants were at high-risk for these problems respectively. Table 1 also displayed descriptive statistics and differences for variables. Gender difference was found only in fear (p = 0.014), i.e., male participants had lower fear than female participants.
Table 1.
Descriptive statistics and differences for all variables.
| Gender |
||||
|---|---|---|---|---|
| Male |
Female |
χ2 or Z | p | |
| (N = 161) | (N = 457) | |||
| Age (years) | 23.36 ± 5.42 | 22.51 ± 4.71 | −2.14 | 0.032 |
| Survey time (no new cases, %) | 11.8 | 5.7 | 6.59 | 0.010 |
| Region (cumulative confirmed cases >500, %) | 70.8 | 76.8 | 2.30 | 0.129 |
| Identity (student, %) | 73.9 | 74.6 | 0.03 | 0.860 |
| Education (bachelor degree or above, %) | 97.5 | 98.5 | 0.19 | 0.660 |
| Risk perception | ||||
| Total scores | 3.35 ± 0.57 | 3.49 ± 0.54 | −2.77 | 0.006 |
| Severity of pandemic | 3.68 ± 0.62 | 3.78 ± 0.57 | −2.24 | 0.025 |
| Uncontrollability | 3.64 ± 0.82 | 3.75 ± 0.78 | −1.56 | 0.118 |
| Severity of health effects | 3.50 ± 0.95 | 3.70 ± 0.90 | −2.32 | 0.020 |
| Likelihood | 2.29 ± 0.83 | 2.44 ± 0.78 | −2.10 | 0.035 |
| Mental health | ||||
| Depression | 0.45 ± 0.64 | 0.38 ± 0.55 | −0.66 | 0.510 |
| Neurasthenia | 0.45 ± 0.59 | 0.43 ± 0.58 | −0.55 | 0.580 |
| Fear | 1.03 ± 0.57 | 1.15 ± 0.56 | −2.46 | 0.014 |
| Compulsion/anxiety | 0.24 ± 0.43 | 0.22 ± 0.39 | −0.10 | 0.920 |
| Hypochondriasis | 0.27 ± 0.44 | 0.30 ± 0.45 | −0.47 | 0.636 |
| Self-efficacy | 2.74 ± 0.59 | 2.54 ± 0.56 | −3.67 | <0.001 |
| Active coping | 1.93 ± 0.53 | 2.04 ± 0.49 | −2.10 | 0.036 |
| Passive coping | 1.34 ± 0.55 | 1.38 ± 0.51 | −0.65 | 0.518 |
Note. N = 618 (except Age, because this variable has 81 missing values). Results are rendered M ± SD except for special notes.
3.2. Correlational analyses
Correlations among the variables are displayed in Table 2 . Spearman correlation analyses showed that risk perception total scores were negatively related to self-efficacy (p = 0.002), and were positively related to passive coping as well as all dimensions of mental health problems (all p < 0.001). Self-efficacy was positively related to active coping (p < 0.001), and was negatively related to passive coping (p = 0.025) as well as all dimensions of mental health problems (all p < 0.050). Besides, active coping was negatively related to depression, neurasthenia, and compulsion/anxiety (all p < 0.001). Passive coping was positively related to all dimensions of mental health problems (all p < 0.001).
Table 2.
Correlations for main variables and their dimensions.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| Risk perception | 1 | – | |||||||
| Mental health problems | |||||||||
| Depression | 2 | 0.16⁎⁎⁎ | – | ||||||
| Neurasthenia | 3 | 0.22⁎⁎⁎ | 0.64⁎⁎⁎ | – | |||||
| Fear | 4 | 0.39⁎⁎⁎ | 0.41⁎⁎⁎ | 0.45⁎⁎⁎ | – | ||||
| Compulsion/anxiety | 5 | 0.20⁎⁎⁎ | 0.66⁎⁎⁎ | 0.64⁎⁎⁎ | 0.51⁎⁎⁎ | – | |||
| Hypochondriasis | 6 | 0.20⁎⁎⁎ | 0.34⁎⁎⁎ | 0.36⁎⁎⁎ | 0.53⁎⁎⁎ | 0.42⁎⁎⁎ | – | ||
| Self-efficacy | 7 | −0.13⁎⁎ | −0.19⁎⁎⁎ | −0.25⁎⁎⁎ | −0.12⁎⁎ | −0.20⁎⁎⁎ | −0.09⁎ | – | |
| Active coping | 8 | −0.03 | −0.21⁎⁎⁎ | −0.25⁎⁎⁎ | −0.06 | −0.20⁎⁎⁎ | −0.05 | 0.46⁎⁎⁎ | – |
| Passive coping | 9 | 0.18⁎⁎⁎ | 0.26⁎⁎⁎ | 0.27⁎⁎⁎ | 0.16⁎⁎⁎ | 0.33⁎⁎⁎ | 0.17⁎⁎⁎ | −0.09⁎ | 0.12⁎⁎ |
Note. N = 618.
p < 0.05.
p < 0.01.
p < 0.001.
3.3. Testing multiple mediation models
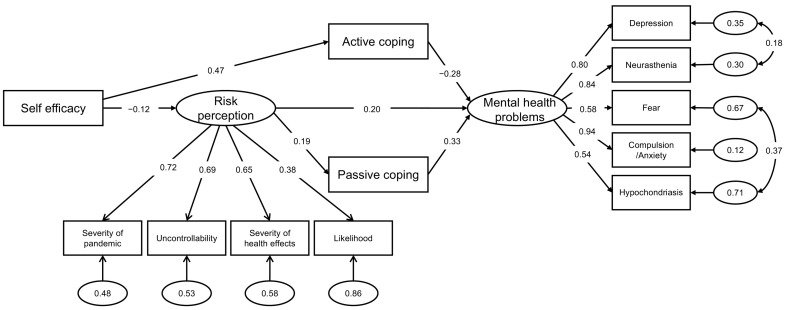
As outlined by (Walker & Smith, 2017), the χ2 test statistic was sensitive to both sample size and multivariate non-normality. Therefore, this statistic would not be taken into account in this study. The results of the initial model indicated that two indices of the initial model were not acceptable (CFI = 0.91, TLI = 0.87, SRMR = 0.07, RMSEA = 0.09, 90% CI = [0.080, 0.100]). However, considering significant correlations between depression and neurasthenia, fear and hypochondria in this study (all p < 0.010), three covariance pathways between the error terms respectively associated with active coping and passive coping, depression and neurasthenia, fear and hypochondria were added. The final model (Fig. 1 ) fit the data moderately well (CFI = 0.93, TLI = 0.90, SRMR = 0.07, RMSEA = 0.08, 90% CI = [0.068, 0.088]).
Fig. 1.
The structural equation model of direct and indirect effects on mental health problems. Note. Statistically insignificant paths between variables are not presented.
The direct and indirect effects among the variables are displayed in Table 3 . A review of the indirect effects of self-efficacy on health mental problems showed that the mediating effects of risk perception (b = −0.02, 95% CI = [−0.045, −0.002]) and active coping (b = −0.13, 95% CI = [−0.171, −0.092]) were significant, providing whole support for H1 and partial support for H2. The serial mediating effect of risk perception and passive coping remained significant (b = −0.01, 95% CI = [−0.014, −0.001]), providing partial support for H3.
Table 3.
Testing the pathways of the multiple mediation models.
| Effect | Estimate | 95% CI |
|
|---|---|---|---|
| Lower | Upper | ||
| Direct effect | |||
| Active coping → health mental problems | −0.28 | −0.347 | −0.181 |
| Passive coping → health mental problems | 0.33 | 0.229 | 0.371 |
| Risk perception → active coping | 0.05 | −0.036 | 0.147 |
| Risk perception → passive coping | 0.19 | 0.127 | 0.363 |
| Risk perception → health mental problems | 0.20 | 0.111 | 0.342 |
| Self-efficacy → risk perception | −0.12 | −0.149 | −0.022 |
| Self-efficacy → active coping | 0.47 | 0.359 | 0.464 |
| Self-efficacy → passive coping | −0.07 | −0.131 | 0.003 |
| Self-efficacy → health mental problems | 0.00 | −0.068 | 0.070 |
| Indirect effect | |||
| Self-efficacy → risk perception → health mental problems | −0.02 | −0.045 | −0.002 |
| Self-efficacy → active coping → health mental problems | −0.13 | −0.171 | −0.092 |
| Self-efficacy → passive coping → health mental problems | −0.02 | −0.048 | 0.002 |
| Self-efficacy → risk perception → active coping → health mental problems | 0.00 | −0.001 | 0.005 |
| Self-efficacy → risk perception → passive coping → health mental problems | −0.01 | −0.014 | −0.001 |
Note. N = 618. Standardized estimates are shown.
4. Discussion
Based on the HBM, the present study investigated multiple mediation models of mental health problems in a sample of the non-infected general Chinese public during COVID-19 pandemic. The main findings are: (1) 12.6–15.1% of participants were affected by COVID-19 outbreak in varying degrees; (2) risk perception mediated the relationship between self-efficacy and mental health problems; (3) active coping mediated the association between self-efficacy and mental health problems; (4) risk perception and passive coping operated as serial mediators between self-efficacy and mental health problems.
4.1. Public mental health during COVID-19 pandemic
In this study, 15.1% of participants were at medium-risk or high-risk for depression. This finding echoed three recent studies that 16.5–20.1% of the participants reported moderate or severe depressive symptoms (Choi et al., 2020; Huang & Zhao, 2020; Wang et al., 2020). Besides, 13.8% of participants were at risk for compulsion/anxiety, which is also consistent with an existing study reporting that 14% of the respondents had anxious symptoms (Choi et al., 2020). Moreover, 13.6% of participants were at risk for fear. Another similar study also showed that fear was present in 18.1% of the general population in Bosnia and Herzegovina (Šljivo et al., 2020). By and large, the proportions of COVID-19-related mental health problems in this study seemed relatively low. The reason might be that most participants of this study were young and middle-aged adults, who might have fewer mental health problems than other age groups during the COVID-19 pandemic (Tian et al., 2020).
4.2. The mediating effect of risk perception
As predicted in Hypothesis 1, risk perception mediated the association between general self-efficacy and mental health problems. Risk perception was found to be positively related to mental health problems in our study, echoing findings of a recent Italian study (Germani et al., 2020). On the other hand, general self-efficacy was found to be negatively related to risk perception. This suggests that application of the HBM (higher general self-efficacy and possibly moderate risk perception) should receive more attention in a public health emergency, such as the COVID-19 pandemic.
4.3. The multiple mediating effects of active coping and passive coping
We found that active coping was negatively related to mental health problems, whereas passive coping was positively related to mental health problems. These results are consistent with prior findings (Cohen-Louck & Levy, 2020; Yang et al., 2010; Lemée et al., 2019). More importantly, our results also indicated that active coping mediated the effect of self-efficacy on mental health problems, and risk perception and passive coping jointly mediated the effect of self-efficacy on mental health problems. This might be due to that information that increases confidence in behavioral activation, were more likely to motivate people to change health behaviors than information that increases perceived threat of diseases (Noar et al., 2007). Notably, a prior study indicated that individuals were more likely to use passive coping in dealing with pandemic-related stress (Gan et al., 2004).
4.4. Limitations
Several limitations should be noted in our study. First, this is a cross-sectional investigation, so further studies should be conducted to examine causal links among these variables. Second, the sample size is relatively small with an unbalanced gender proportion. Third, our data were collected by a self-report questionnaire through the Internet due to quarantine measures across the country; as such the indicated levels of mental health problems may not be in accord with the assessments of mental health professionals. The online questionnaire also limited the availability of the survey to elder adults.
5. Conclusions
From the perspective of the HBM, our study investigated mental health problems and underlying mechanisms among the non-infected people during COVID-19 pandemic. We found that risk perception and coping strategies were mediators in the association of self-efficacy and mental health problems. Our findings have important implications for understanding the mechanism of mental health during an infectious disease pandemic in view of health psychology. First, general self-efficacy may play a crucial role in coping behaviors and mental health during the infectious disease pandemic. Second, shaping adaptive risk perceptions through various media may benefit public mental health, and the assessment of risk perception needs more investigation in the future.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the institutional and/or national research committee's ethical standards and with The 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Research Ethics Committee of the first corresponding author' university approved this study.
Informed consent
Informed consent was obtained from all individual participants in the study.
CRediT authorship contribution statement
Chenhao Zhou: Methodology, Software, Formal analysis, Data curation, Writing – original draft, Visualization, Writing – review & editing. Xiao Dong Yue: Visualization, Writing – review & editing. Xingli Zhang: Methodology, Writing – review & editing. Fangfang Shangguan: Conceptualization, Writing – original draft, Methodology, Project administration, Resources, Investigation, Validation, Writing – review & editing. Xiang Yang Zhang: Resources, Writing – review & editing.
Declaration of competing interest
All authors declared no conflicts of interest.
Acknowledgments
This research was supported by the Shenzhen-Hongkong Institute of Brain Science-Shenzhen Fundamental Research Institutions (NYKFKT 2020002), China; the National Natural Science Foundation of China (Grant No. 31771223), and Beijing Municipal Education Commission (SZ201810028014), China.
References
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bidzan M., Bidzan-Bluma I., Szulman-Wardal A., Stueck M., Bidzan M. Does self-efficacy and emotional control protect hospital staff from covid-19 anxiety and ptsd symptoms? Psychological functioning of hospital staff after the announcement of covid-19 coronavirus pandemic. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.552583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- Bruine de Bruin W., Bennett D. Relationships between initial COVID-19 risk perceptions and protective health behaviors: A National Survey. American Journal of Preventive Medicine. 2020;59(2):157–167. doi: 10.1016/j.amepre.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao C.Y., Lemieux C., Restellini S., Afif W., Bitton A., Lakatos P.L.…Bessissow T. Maladaptive coping, low self-efficacy and disease activity are associated with poorer patient-reported outcomes in inflammatory bowel disease. Saudi Journal of Gastroenterology. 2019;25(3):159–166. doi: 10.4103/sjg.SJG_566_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Liu T., Luo J., Ren S. Data for teenagers’ stressor, mental health, coping style, social support, parenting style and self-efficacy in South China. Data in Brief. 2020;29 doi: 10.1016/j.dib.2020.105202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C., Tang C.S. The psychology behind the masks: Psychological responses to the severe acute respiratory syndrome outbreak in different regions. Asian Journal of Social Psychology. 2004;7(1):3–7. doi: 10.1111/j.1467-839X.2004.00130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi E.P.H., Hui B.P.H., Wan E.Y.F. Depression and anxiety in Hong Kong during COVID-19. International Journal of Environmental Research and Public Health. 2020;17(10) doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.P., Wang P.W., Chen S.L., Chang Y.P., Wu C.F., Lu W.H., Yen C.F. Risk perception, protective behaviors, and general anxiety during the coronavirus disease 2019 pandemic among affiliated health care professionals in Taiwan: Comparisons with frontline health care professionals and the general public. International Journal of Environmental Research and Public Health. 2020;17(24):9329. doi: 10.3390/ijerph17249329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Louck K., Levy I. Risk perception of a chronic threat of terrorism: Differences based on coping types, gender and exposure. International Journal of Psychology. 2020;55(1):115–122. doi: 10.1002/ijop.12552. [DOI] [PubMed] [Google Scholar]
- Commodari E., La Rosa V. L., Coniglio M.A. Health risk perceptions in the era of the new coronavirus: Are the Italian people ready for a novel virus? A cross-sectional study on perceived personal and comparative susceptibility for infectious diseases. Public Health. 2020;187:8–14. doi: 10.1016/j.puhe.2020.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai, Y., Hao, Y., Wu, Q., Xu, W., Wang, X., & Wang, X. (2020). Establishment and evaluation on reliability and validity of public risk perception scale for public health emergencies. Chinese Journal of Public Health, (02), 227–231. [in Chinese].
- Ding Y., Yang Y., Yang X., Zhang T., Qiu X., He X.…Sui H. The mediating role of coping style in the relationship between psychological capital and burnout among Chinese nurses. Public Library of Science one. 2015;10(4) doi: 10.1371/journal.pone.0122128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezati R.R., Mohseni S., Kamalzadeh T.H., Hassani A.M., Shahabi N., Aghamolaei T., Norozian F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: A cross-sectional study. BMC Public Health. 2021;21(1):466. doi: 10.1186/s12889-021-10500-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S., Moskowitz J.T. Coping: Pitfalls and promise. Annual Review of Psychology. 2004;55(1):745. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- Gan Y., Liu Y., Zhang Y. Flexible coping responses to severe acute respiratory syndrome-related and daily life stressful events. Asian Journal of Social Psychology. 2004;7(1):55–66. [Google Scholar]
- Gao, Y., Xu, M., Yang, Y., & Yao, K. (2004). Discussion on the coping style of undergraduates and the correlative factors during the pandemic period of SARS. Chinese Medical Ethics, (02), 60–63. [in Chinese].
- Germani A., Buratta L., Delvecchio E., Mazzeschi C. Emerging adults and COVID-19: The role of individualism-collectivism on perceived risks and psychological maladjustment. International Journal of Environmental Research and Public Health. 2020;17(10):3497. doi: 10.3390/ijerph17103497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288, 112954 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai H., Furukawa T.A., Hayashi S.U., Goto A., Izumi K., Hayashino Y., Noda M. Risk perception, self-efficacy, trust for physician, depression, and behavior modification in diabetic patients. Journal of Health Psychology. 2020;25(3):350–360. doi: 10.1177/1359105317718057. [DOI] [PubMed] [Google Scholar]
- Jerusalem M., Schwarzer R. Freie Universität. Institut für Psychologie; Berlin: 1986. Self-efficacy. Scales for mental state and personality; pp. 15–28. [Google Scholar]
- Krok D., Zarzycka B. Risk perception of covid-19, meaning-based resources and psychological well-being amongst healthcare personnel: The mediating role of coping. Journal of Clinical Medicine. 2020;9(10):3225. doi: 10.3390/jcm9103225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T., Yang X., Tsui H.Y., Pang E., Wing Y.K. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. Journal of Infection. 2006;53(2):114–124. doi: 10.1016/j.jinf.2005.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemée C., Fleury-Bahi G., Navarro O. Impact of place identity, self-efficacy and anxiety state on the relationship between coastal flooding risk perception and the willingness to cope. Frontiers in Psychology. 2019;10:499. doi: 10.3389/fpsyg.2019.00499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y., Hu Z., Alias H., Wong L.P. Knowledge, attitudes, impact, and anxiety regarding COVID-19 infection among the public in China. Frontiers in Public Health. 2020;8:236. doi: 10.3389/fpubh.2020.00236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Mo L., Huang X., Yu L., Liu Y. Path analysis of the effects of social support, self-efficacy, and coping style on psychological stress in children with malignant tumor during treatment. Medicine. 2020;99(43) doi: 10.1097/MD.0000000000022888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main A., Zhou Q., Ma Y., Luecken L.J., Liu X. Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. Journal of Counseling Psychology. 2011;58(3):410–423. doi: 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Mak W.W., Law R.W., Woo J., Cheung F.M., Lee D. Social support and psychological adjustment to SARS: The mediating role of self-care self-efficacy. Psychology & Health. 2009;24(2):161–174. doi: 10.1080/08870440701447649. [DOI] [PubMed] [Google Scholar]
- McBride H., Ireland C. The impact of coping style, self-efficacy, emotional reaction and resilience on trauma related intrusive thoughts. Journal of Forensic Practice. 2016;18(3):229–239. [Google Scholar]
- Miura I., Nagai M., Maeda M., Harigane M., Fujii S., Oe M.…Abe M. Perception of radiation risk as a predictor of mid-term mental health after a nuclear disaster: The Fukushima health management survey. International Journal of Environmental Research and Public Health. 2017;14(9):1067. doi: 10.3390/ijerph14091067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo, Y., Deng, L., Zhang, L., Lang, Q., Pang, H., Liao, C., Wang, N., Tao, P., & Huang, H. (2021). Anxiety of nurses to support Wuhan in fighting against covid-19 epidemic and its correlation with work stress and self-efficacy. Journal of Clinical Nursing, 30(3–4), 397–405. [DOI] [PubMed]
- Mukhtar S. Mental health and emotional impact of COVID-19: Applying Health Belief Model for medical staff to general public of Pakistan. Brain, Behavior, and Immunity. 2020;87:28–29. doi: 10.1016/j.bbi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson M., Forsberg A., Lennerling A., Persson L.O. Coping in relation to perceived threat of the risk of graft rejection and health-related quality of life of organ transplant recipients. Scandinavian Journal of Caring Sciences. 2013;27(4):935–944. doi: 10.1111/scs.12007. [DOI] [PubMed] [Google Scholar]
- Noar S.M., Benac C.N., Harris M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: Mental health burden and strategies. Brazilian journal of psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlman, R.L., Patel, V., Davis, R.E., Ferris, T.S., Gruszynski, K., Elledge, T., Bhattacharya, K., & Nahar, V.K. (2020). Effects of health beliefs, social support, and self-efficacy on sun protection behaviors among medical students: Testing of an extended Health Belief Model. Archives of Dermatological Research. Advance online publication. [DOI] [PubMed]
- Polit D.F., Beek C.T., Owen S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Research in Nursing and Health. 2007;30(4):459–467. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- Rosenstock I. The Health Belief Model and preventive behavior. Health Education Monographs. 1974;2:354–386. [Google Scholar]
- Sheeran P., Maki A., Montanaro E., Avishai-Yitshak A., Bryan A., Klein W.M.P.…Rothman A.J. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychology. 2016;35(11):1178–1188. doi: 10.1037/hea0000387. [DOI] [PubMed] [Google Scholar]
- Skinner C.S., Tiro J., Champion V.L. The Health Belief Model. Health Education Quarterly. 2008;11(1):1–47. [Google Scholar]
- Šljivo A., Kačamaković M., Quraishi I., Džubur Kulenović A. Fear and depression among residents of Bosnia and Herzegovina during covid-19 outbreak-internet survey. Psychiatria Danubina. 2020;32(2):266–272. doi: 10.24869/psyd.2020.266. [DOI] [PubMed] [Google Scholar]
- Suzuki Y., Yabe H., Yasumura S., Ohira T., Niwa S., Ohtsuru A.…Abe M. Psychological distress and the perception of radiation risks: The Fukushima health management survey. Bulletin of the World Health Organization. 2015;93(9):598–605. doi: 10.2471/BLT.14.146498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker D.A., Smith T.J. Computing robust, bootstrap-adjusted fit indices for use with nonnormal data. Measurement and Evaluation in Counseling and. Development. 2017;50(1–2):131–137. [Google Scholar]
- Wang, C., Hu, Z., & Liu, Y. (2001). Evidences for reliability and validity of the chinese version of general selfefficacy scale. Chinese Journal of Applied Psychology, (01), 37–40. [in Chinese].
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters M., Jalloh M.F., Sengeh P., Jalloh M.B., Nordenstedt H. Risk perception during the 2014-2015 ebola outbreak in sierra leone. BMC Public Health. 2020;20(1539) doi: 10.1186/s12889-020-09648-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z.…Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, Y. (1998). Reliability and validity of Simplified Coping Style Questionnaire. Chinese Journal of Clinical Psychology, (02), 3–5. [in Chinese].
- Yang J., Yang Y., Liu X., Tian J., Zhu X., Miao D. Self-efficacy, social support, and coping strategies of adolescent earthquake survivors in China. Social Behavior & Personality An International Journal. 2010;38(9):1219–1228. [Google Scholar]